Highlights
-
•
After decades of investment in public health emergency response system in terms of infrastructure, equipment, inter-organizational communication and other areas, China has claimed that a sound public health emergency response system was established. Despite this, lack of qualified front-line staff that equipped with sufficient knowledge and emergency response skills has crippled the efficient action of emergency response. Although this problem is grave, there is paucity of studies in China exploring this issue.
-
•
This study identified the weakest skill areas perceived by participants among key skills highly demanded during public health emergency response.
-
•
Totally fourteen key emergency response skills and techniques were highlighted by responders. The five top weakest skill deficiency areas to be addressed were as follows: field epidemiological investigation skills, personal protective skills, nuclear and radioactive emergency handling skills, psychological intervention skills and risk assessment skills.
-
•
Major obstacles hindering the efficient promotion and mastery of those key skills among front-line emergency responders were as follows: insufficient funding of technical application, lack of operability, disqualified training and drills, delays in skill updating.
-
•
Determinants associated with the self-rated overall skill proficiency of public health emergency responders were explored: the multivariate logistic regression revealed personal protective skills as the most important factor contributing to self-rated overall skill proficiency of public health emergency responders (OR = 2.171), then field epidemiological investigation skills (OR = 1.510). Followed by emergency preparedness plan skills, coping with emergency drills, crisis communication skills, besides, field sampling skills and the professional title.
Key Words: Public health emergency, Chinese Centers for Disease Control and Prevention
Abstract
Background
To identify the weakest skill areas perceived by participants among key skills highly demanded during emergencies and to explore factors influencing the self-rated overall skill proficiency of public health emergency responders.
Methods
The participants were selected by a multistage, stratified cluster sampling method in Heilongjiang CDC to complete questionnaires that assessed their perceptions of health emergency response skills and techniques. A final sample of 1,740 staff members was obtained and analyzed.
Results
The 5 top skill deficiency areas perceived by participants were field epidemiologic investigation, personal protection, effective nuclear and radioactive response as well as psychological interventio (for these two areas gain the equal score), and risk assessment. The logistic regression revealed personal protective skills as the most important factor contributing to the self-rated overall skill proficiency of public health emergency responders, followed by field epidemiologic investigation skills.
Conclusions
More attention should be given to emergency response skill training and education programs. Major obstacles hindering the promotion of key skills and techniques among front-line emergency responders should be addressed urgently. Continuous efforts should be made to remove the financial, technical, and resource obstacles to improve public health emergency response capacity.
With advancing industrialization, increasing urbanization, and growing awareness of complicating factors, all nations will be challenged by public health emergencies that have the capacity to adversely influence the security of populations, in terms of both social cohesion and population health.1, 2, 3, 4 Here in China, severe acute respiratory syndrome (SARS) was a sobering reminder of the importance of preparation in relation to public health emergencies. In retrospect, we learned that our response mechanisms to public health emergencies, despite the best of intentions, were imperfect and our ability to cope with such crises required improvement.5, 6, 7, 8 In response to the SARS experience, the Chinese government at all levels accelerated the reform of emergency response systems to enhance capacity and effectiveness.9, 10, 11, 12
The Chinese Centers for Disease Control and Prevention (CDC) is responsible for the surveillance and management of public healthemergencies through the detection, prevention, and control of diseases. It plays a key role in protecting people from health, safety, and security threats, both in China and in other regions of the world. It is therefore reasonable to conclude that health emergency response skills and techniques adopted by CDC staff directly influence their effective response to public health emergencies.13, 14, 15 China aimed to establish a comprehensive public health system in recent years; however, an overemphasis on infrastructure might have overlooked problems associated with staff development and skill training that might exert more influence on the consequences of emergency responses.16, 17 The recent Ebola virus disease epidemic of 2013-2015 tested the efficacy of emergency response mechanisms: Despite extensive preparatory work, 2 nurses were infected by Ebola virus disease in the United States due to their incorrect use of personal protective equipment (PPE). This highlighted the human error factor in response to public health emergencies.18
Research associated with emergency responses and, in particular those charged with health emergency response skills and techniques, is a relatively new area and studies in China are limited. Liang et al's study,19 Xiang et al's study,20 Zhang et al's study,21 and Bo and Li's study22 focused on the quantity, allocation, and construction of emergency teams, but the weak competencies of emergency responders turned out to be the key impediment to improving emergency response capacity. These weak competencies could include low levels of technical efficiency; poor field epidemiologic investigation skills; and perhaps most importantly, a lack of staff who had explicit experience and skills in relation to appropriate emergency responses.23, 24, 25 This study aimed to explore opportunities for enhancing the response capacity of emergency responders by reviewing participants' knowledge, and identify factors associated with the self-rated overall skill proficiency of public health emergency responders.
Methods
Study population and data collection
The self-assessment of participants was facilitated by researchers from the Department of Social Medicine of Harbin Medical University. Heilongjiang is located in northeast China, with a population of more than 38 million. In 2015, the gross domestic product per capita in Heilongjiang reached 39,352.20 (Yuan), ranking in the lowest range of all provinces.26 Considering the geographic and jurisdictional diversity, a stratified cluster sampling method was adopted. All 13 municipalities in Heilongjiang were involved in the study. In each municipality, there are 5-10 counties; we selected 2-4 sampled counties at random in the same proportion (40%). Finally, 40 CDC institutions were sampled. The researchers traveled to 40 CDC institutions to conduct the face-to-face survey, and all the CDC staff were invited to participate, except nonprofessional staff. The study protocol was reviewed and approved by the Research Ethics Committee of Harbin Medical University. Each participant was interviewed by an interviewer following a structured questionnaire. All participants indicated his or her willingness to take part both verbally and in consent forms signed before the commencement of interviews. In total, 1,889 individuals completed the questionnaires.
The survey questionnaires, which were developed by the researchers, collected basic demographic information, the participants' level of confidence in achieving effective self-protection, use of PPE, and various health emergency response skills and techniques used by emergency responders. A pilot study of the survey tool was carried out and it was revised after several rounds of focus group discussions. In addition to the questionnaire survey, face-to-face interviews were conducted by qualified investigators and quality control was implemented by supervisors throughout the study.
Variables
The survey questionnaire involved dependent and independent variables. The dependent (outcome) variable was self-rated overall skill proficiency of public health emergency responders. In this study, participants were asked to choose 1 answer for each statement (1 = very poor, 2 = poor, 3 = average, 4 = good, or 5 = very good). The answers were grouped into 2 categories: not good and good (the first 3 items were “not good” and the latter 2 were “good”). The question was: “What do you think of your overall proficiency of health emergency response skills and techniques?”
Independent variables involved demographic information such as gender; age; highest educational level attained; professional title; and work experience and emergency practical experience, such as frequency of dealing with public health emergencies. In addition, self-rated health emergency response skills and techniques information was collected. This included field epidemiologic investigation skills, risk assessment skills, emergency preparedness plan making skills, emergency training and drills skills, sampling skills, detection skills, isolation skills, disinfection skills, nuclear and radioactive materials handling skills, health education skills, and crisis communication skills. Participants were asked to rate their own health emergency response skills and techniques (listed above) as (1 = very poor, 2 = poor, 3 = average, 4 = good, or 5 = very good). The answers also were grouped into 2 categories: not good and good (the first 3 items as “not good” and the latter 2 as “good”). The question was: “How do you rate your own skill level in field epidemiologic investigation, risk assessment, and other 10 important emergency handling skills?”
Statistical analysis
We excluded 149 samples because of incompleteness, so a final sample of 1,740 staff was used. Descriptive statistics were calculated to describe the demographic characteristics. Univariate analysis found the associations that demonstrated statistical significance (P < .05) and then were analyzed with the multivariate logistic regression that was adopted to predict the outcome of the self-rated overall skill proficiency of public health emergency responders. The outcome variable was treated as a nominal measure—not good versus good—and the independent variables are shown in Table 1 . Odds ratios (ORs) and their 95% confidence intervals were estimated to assess the relationship between the predictors and the outcome variable. All statistical analyses were performed using SPSS 22.0 (IBM-SPSS Inc, Armonk, NY).
Table 1.
Variable assignment note
| Variable | Description | Instructions |
|---|---|---|
| Y | The self-rated overall skill proficiency of public health emergency responders | Not good = 0 |
| Good = 1 | ||
| X1 | Centers for Disease Control and Prevention level | City = 0 |
| District = 1 | ||
| X2 | Gender | Male = 1 |
| Female = 2 | ||
| X3 | Age | ≤ 30 = 1 |
| 30-39 = 2 | ||
| 40-49 = 3 | ||
| ≥ 50 = 4 | ||
| X4 | Highest educational level attained | Junior college and below = 1 |
| Undergraduate = 2 | ||
| Graduate and above = 3 | ||
| X5 | Professional title | Junior and below = 1 |
| Intermediate title = 2 | ||
| Senior title = 3 | ||
| X6 | Work experience | 1-9 years = 1 |
| 10-19 years = 2 | ||
| 20-29 years = 3 | ||
| ≥ 30 years = 4 | ||
| X7 | The frequency of dealing with public health emergencies | 1-9 times = 1, |
| 10-19 times = 2 | ||
| ≥ 20 times = 3 | ||
| X8 | Personal protective skills | Not good = 0 |
| Good = 1 | ||
| X9 | Emergency preparedness plan skills | Not good = 0 |
| Good = 1 | ||
| X10 | Risk assessment skills | Not good = 0 |
| Good = 1 | ||
| X11 | Outcome of prior training | Not good = 0 |
| Good = 1 | ||
| X12 | Coping with emergency drills | Not good = 0 |
| Good = 1 | ||
| X13 | Field epidemiologic investigation skills | Not good = 0 |
| Good = 1 | ||
| X14 | Field sampling skills | Not good = 0 |
| Good = 1 | ||
| X15 | Disease identification and detection skills | Not good = 0 |
| Good = 1 | ||
| X16 | Application of isolation methods | Not good = 0 |
| Good = 1 | ||
| X17 | Onsite disinfection skills | Not good = 0 |
| Good = 1 | ||
| X18 | Nuclear and radioactive skills | Not good = 0 |
| Good = 1 | ||
| X19 | Effective health education skills | Not good = 0 |
| Good = 1 | ||
| X20 | Effective crisis communication skills | Not good = 0 |
| Good = 1 |
Results
Participant characteristics
Of the 1,740 eligible participants, 41.0% were men and 59.0% were women. More than two-thirds of respondents (68.4%) were aged 30-49 years and just more than half of all respondents had work experience between 10 and 29 years (55.3%). Similarly, just more than half (54.3%) reported having junior college or lower qualifications. The participants' professional titles mainly belonged to the group of junior and below (41.2%).
The perceived weakest skill areas of participants among key skills highly demanded during public health emergency response
Altogether, 14 key skills were highlighted as the most earnestly needed skills for front-line emergency responders. Among them, the 5 weakest skill deficiency areas were perceived by participants. Overall, 43.9% of responders regarded field epidemiologic investigation as the weakest skill mastered by emergency responders. The other weak skills were personal protection (25.7%), emergency psychological intervention (25.6%), effective nuclear and radioactive materials response (25.6%), and risk assessment (21.4%) (Table 2 ). In contrast, responders rated their skills in devising emergency preparedness plans at 91.1%.
Table 2.
The perceived weakest skill areas of participants among key skills highly demanded during public health emergency response
| Item | n | Constituent ratio (%) |
|---|---|---|
| Emergency psychological intervention skills | 446 | 25.6 |
| Health education skills | 223 | 12.8 |
| Event report and report processing skills | 248 | 14.3 |
| Personal protective skills | 448 | 25.7 |
| Field epidemiologic investigation skills | 580 | 43.9 |
| Isolation and onsite disinfection skills | 353 | 20.3 |
| Nuclear and radioactive response skills | 445 | 25.6 |
| Crisis communication skills | 328 | 18.9 |
| Medical rescue skills | 254 | 14.6 |
| Risk assessment skills | 373 | 21.4 |
| Training and drills skills | 274 | 15.7 |
| Emergency preparedness plan skills | 155 | 8.9 |
| Material reserves skills | 245 | 14.1 |
| Disease identification and detection skills | 322 | 18.5 |
The obstructive factors hindering the promotion of health emergency response skills and techniques
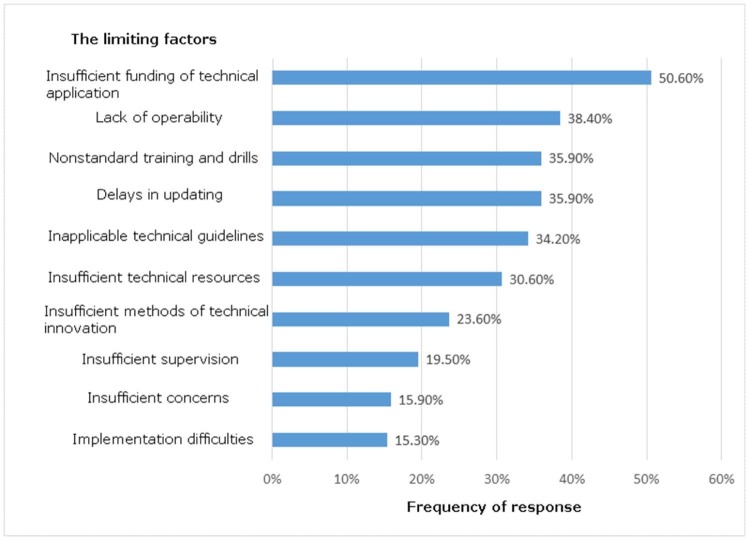
Public health emergency response skills and techniques play a critical role in emergency response work27; however, the factors hindering the promotion of these skills and techniques reduce emergency response capability. In our study, we found insufficient funding of technical application (50.6%) was the most common obstructive factor, followed by lack of operability (38.4%). In addition, the proportion of delays in skill updating and disqualified training and drills was both 35.9%, as shown in Figure 1 .
Fig 1.
The factors hindering the promotion of health emergency response skills and techniques.
Self-determined confidence in achieving effective self-protection and the proficient use of PPE, including protective glasses, masks, footwear, and clothing
To ensure an effective public health emergency response, responders must be able to protect themselves from the effect of public health emergencies wherever possible. For this reason, familiarity and effective use of personal protective apparel and equipment is paramount. We found that 62.2% of interviewees reported a lack of confidence in their ability to achieve effective self-protection when encountering biologic or nuclear and radiation emergencies. More than half of the staff members (59.4%) revealed that they were unaware of how to deal with disease outbreaks of unknown etiology. In terms of PPE safety, more than 80% of the sampled staff claimed proficiency in the use of protective glasses, medical protective masks, latex gloves, protective clothing, protective footwear, and isolation gowns; however, 76.2% reported the proficient use of a N95 or FFP3 mask, but only 56.4% reported proficiency with respiratory protective devices (Table 3 ).
Table 3.
Self-determined confidence in achieving effective self-protection and the proficient use of personal protective equipment (PPE)
| Item | n | Constituent ratio (%) |
|---|---|---|
| Self-determined confidence in achieving effective self-protection | ||
| Infectious disease | 615 | 35.3 |
| Occupational poisonings | 452 | 26.0 |
| Diseases outbreaks of unknown etiology | 1,033 | 59.4 |
| Environmental pollution | 421 | 24.2 |
| Biological or nuclear and radiation | 1,083 | 62.2 |
| PPE | ||
| Protective glasses | 1,640 | 94.3 |
| Respiratory protective devices | 981 | 56.4 |
| Medical protective masks | 1,665 | 95.7 |
| Latex gloves | 1,681 | 96.6 |
| Protective clothing | 1,562 | 89.8 |
| Protective footwear | 1,547 | 88.9 |
| Isolation gowns | 1,465 | 84.2 |
| N95 or FFP3 masks | 1,326 | 76.2 |
Determinants associated with the self-rated overall skill proficiency of public health emergency responders
Univariate analysis showed that the self-rated overall skill proficiency of public health emergency responders was associated with age, highest education level attained, professional title, work experience, the frequency of dealing with public health emergencies, personal protective skills, devising emergency preparedness plans skills, risk assessment skills, coping with emergency drills, field epidemiologic investigation skills, field sampling skills, disease identification and detection skills, application of isolation methods, onsite disinfection skills, nuclear and radioactive emergency handling skills, effective health education, and crisis communication skills.
Multivariate logistic regression revealed that personal protective skills were identified as the most important factor contributing to the self-rated overall skill proficiency of public health emergency responders (OR, 2.171), followed by field epidemiologic investigation skills (OR, 1.510). Skills related to making emergency preparedness plans, coping with emergency drills, performing crisis communication, conducting field sampling, and having a professional title also played significant roles in public health emergencies (Table 4 ).
Table 4.
Determinants associated with the self-rated overall skill proficiency of public health emergency responders
| Variable | β | Standard error | Wald | P value | Odds ratio (95% confidence interval) |
|---|---|---|---|---|---|
| Professional title | 0.258 | 0.103 | 6.269 | .012 | 1.295(1.058-1.585) |
| Personal protective skills | 0.775 | 0.105 | 54.063 | .000 | 2.171(1.766-2.669) |
| Emergency preparedness plan skills | 0.350 | 0.097 | 13.070 | .000 | 1.419(1.174-1.715) |
| Competency in coping with emergency drills | 0.337 | 0.125 | 7.305 | .007 | 1.401(1.097-1.788) |
| Field epidemiologic investigation skills | 0.412 | 0.112 | 13.529 | .000 | 1.510(1.212-1.881) |
| Field sampling skills | 0.268 | 0.115 | 5.444 | .020 | 1.307(1.044-1.637) |
| Crisis communication skills | 0.316 | 0.091 | 12.111 | .001 | 1.372(1.148-1.640) |
Discussion
Public health emergency response skills and techniques are directly related to comprehensive detection and prevention measures. The response to public health emergencies plays a crucial if not decisive role in predicting likely outcomes.28 Determining key deficits and identifying opportunities for improvement can help strengthen emergency response capacity. Our research suggests that health emergency response skills and techniques are the essential precondition for coping with public health emergencies.
Staff development and training
The Chinese CDC is a highly technical and professional institution and its comprehensively prepared staff are critical to effective emergency response.29 Previous studies have showed that a lack of opportunities for advanced or continuing education and qualified staff meant the agency could not meet the demand for actual public health emergency work in China.30, 31 These results were consistent with ours. Our study found that low preparatory education and inadequate numbers of qualified personnel existed in Heilongjiang. The United States attaches great importance to the continuing education of CDC staff through a variety of training approaches. For example, CDC staff can participate in short-term training or promote corresponding knowledge by network and distance education.32 We suggest that there is a need to improve the preparedness of existing staff in China through formal advanced education, and to review the entry-level requirements for new staff. Consideration may be given to offer senior staff, such as experienced health managers in related areas, an opportunity to undergo additional training and be offered redeployment to improve emergency response capacity. In addition, developing a multidisciplinary public health specialist workforce is also very necessary in China. The UK public health policy has emphasized the importance of a multidisciplinary background among the public health specialist workforce since 1997.33 In 1999, the Public Health Department of the UK National Health System received other related professional background personnel.34 Reinforcing skills by developing existing staff training and a multidisciplinary public health specialist workforce should become the priority in the process of health emergency preparedness in the Chinese CDC.
The weak skills and techniques perceived by participants in public health emergency response
Field epidemiologic investigation is at the heart of planning for public health emergency responses and is a deciding factor in the outcomes to a large extent.35 In our study, our sampled population conceded they were not proficient in the most important skills needed by people managing public health emergencies. Other studies show that the lack of experienced and senior staff, laboratory support, and insufficient ongoing funding influenced personnel's capacity to master field epidemiologic investigation skills.36, 37 The other, weaker skill in public health emergency response shown in this study was personal protection. PPE use is essential to prevent skin and mucous membranes from becoming contaminated.38 PPE serves as the last physical barrier between a health care provider and infectious agents. In previous outbreaks, health care personnel infections were substantially reduced with the institution of barrier precautions39; however, our survey found that not all the responders were confident in the proficient use of PPE. This was especially problematic in the use of respiratory protective devices and apparatus. The safety of emergency response personnel is dependent upon the prior investment of training in the correct use of PPE.40 Our survey showed that in some public health emergencies, such as biological or nuclear and radiation accidents, the capacity of personal protection was low. Although this may be related to the sudden and unexpected onset of accidents with resultant environmental contamination in many complex and diverse ways,41 it seems that proper planning and preparation should prevent poor performance.
Major problems hindering the promotion of health emergency response skills and techniques
Promotion of health emergency response skills and techniques is a key factor in public health emergencies.42 Our study found that insufficient funding was the main limiting factor to the promotion of health emergency response skills and techniques. Effective promotion is predicated upon financial support, appropriate equipment, and flexible thinking among Chinese CDC staff. Another survey, conducted by Dredger et al,43 also reported that there was an increased need for financial support to ensure effective emergency response.
Contributory factors to the self-rated overall skill proficiency of public health emergency responders
The multivariate regression results showed that mastering personal protective skills (or not) was found to have the greatest influence (OR, 2.171) on outcome. During the SARS outbreak, health care providers accounted for 20% of all infected persons. Similarly, the Ebola virus disease crisis that devastated West Africa also resulted in high mortality rates among health care providers. It is pertinent to ask why so many health care providers using PPE and with no history of direct contact became infected.44, 45 These examples demonstrate the importance of personal protective skills. In our study, field epidemiologic investigation skills were the second highest contributory factor identified that influenced the self-rated overall skill proficiency of public health emergency responders. Epidemiologic investigations are usually conducted in outbreak situations and serve as the key step for stipulating appropriate responses to public health emergencies that influenced the outcome of communicable diseases.39 Therefore, effective implementation of epidemiologic investigation is a prerequisite to ensure that emergency work is carried out smoothly. Competency in coping with emergency drills is also a key element in the self-rated overall skill proficiency of public health emergency responders (OR, 1.401). For any country, public health emergencies necessitate emergency drills to simulate real emergency experiences to develop and improve skills and to assess emergency response capacity.46 The US Federal Emergency Management Agency describes 6 levels of emergency drills, increasing in complexity from informational seminars to simulations to implementing emergency response functions.47 However, emergency drills started relatively late in China and the country has not yet established an effective emergency drill system. So, how to ensure the emergency drill capacity to cope with public health emergencies promptly and properly will be the primary focus of China in the future. With regard to crisis communication skills associated with the self-rated overall skill proficiency of public health emergency responders (OR, 1.372), they are not limited to effective team management, but also include providing public information in a calm and sensitive manner to avoid civil unrest during a public health emergency. People charged with management must take in information, process it, and act on it, often in the absence of all facts or ideal situations being open for consideration.48 Governments and health agencies worldwide should acknowledge the importance of effective and appropriate communication during public health emergencies.49 Meanwhile, the availability of experienced staff, the ability to devise an emergency preparedness plan, and field sampling skills were other factors that contributed to the self-rated overall skill proficiency of public health emergency responders.
Limitations
This study has several limitations. First, data were collected using self-assessment tools, and therefore, the perceptions of public health emergency response skills and techniques may be overestimated. Second, because we surveyed the participants in 1 province due to time and resource restrictions, these findings may not be generalizable to other regions in China. To get a more accurate estimation of the emergency response capacity, further studies are recommended to develop a more comprehensive evaluation tool and enhance the skills and techniques of responders during public health emergencies.
Conclusions
Following several rounds of heavy investment in public health emergency system construction in China, poor emergency response skills and techniques of front-line responders turns out to be the key impediment to this system. Policy intervention should be targeted to equip emergency responders with needed skills and techniques and address the weakest links in their skill mix. More attention should be given to emergency response skills training and education programs and providing grassroots-level CDC staff with more opportunities to master the skills of epidemiologic investigation, personal protection, emergency preparedness planning, emergency drills, and crisis communication. Major obstacles hindering the efficient promotion of key skills and techniques among front-line emergency responders should be addressed urgently. Continuous efforts should be made to remove the financial, technical, and resource obstacles to improve the public health emergency response capacity.
Acknowledgments
The authors thank all of the participating organizations and participants. Without their cooperation and suggestions, there was no way to complete this academic research.
Footnotes
JR, HS, and DD contributed equally to this work.
JR participated in design of the research, conducted analysis of the data, and edited the manuscript; QW and YH were responsible for the overall design of the research, organized and conducted the survey, designed the analysis frameworks, and drafted and edited the manuscript; AF provided language help and contributed to the final revision; DD and NN were responsible for the data analysis process; HS and YC participated in the process of data collection and the manuscript revision.
This study was funded by the Scientific Research of Ministry of Health of China (grant No.201002028), the National High Technology Research and Development Program of China (grant No.2006AA02Z460), and the Natural Science Foundation of China (grant No.71173064).
Conflicts of interests: None to report.
Contributor Information
Qunhong Wu, Email: wuqunhong@163.com.
Yanhua Hao, Email: hyhyjw@126.com.
References
- 1.Martinot A., Thomas J., Thiermann A., Dasgupta N. Prevention and control of avian influenza: the need for a paradigm shift in pandemic influenza preparedness. Vet Rec. 2007;160:343–345. doi: 10.1136/vr.160.10.343. [DOI] [PubMed] [Google Scholar]
- 2.Khardori N., Kanchanapoom T. Overview of biological terrorism: potential agents and preparedness. Clin Microbiol Newsl. 2005;27:1–8. [Google Scholar]
- 3.Nicoll A., Wilson D., Calvert N., Borriello P. Managing major public health crises. BMJ. 2001;323:1321–1322. doi: 10.1136/bmj.323.7325.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang X. The present situation and countermeasure of preventing and curing infectious diseases. J Public Health Prev Med. 2004;15:4–7. [Google Scholar]
- 5.Huang J.W., Hou T.W. Design and prototype of a mechanism for active on-line emerging/ notifiable infectious diseases control, tracking and surveillance, based on a national healthcare card system. Comput Methods Programs Biomed. 2007;8:161–170. doi: 10.1016/j.cmpb.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang W. The main problems and challenges of the current disease control in China. Chin Health Econ Mag. 2005;24:73. [Google Scholar]
- 7.Yu J., Yu M., Su H., Wang H., Zhang Y., Liu L. A brief introduction to the study concerning constructing disease prevention and control system of China. Chin Health Resour. 2006;9:115–117. [Google Scholar]
- 8.Lei F., Zhao W. The discussion of the current situation and existing problems of the junior center for disease control and prevention. Chin Prim Health Care. 2007;21:53. [Google Scholar]
- 9.Perrone L.A., Tumpey T.M. Reconstruction of the 1918 pandemic influenza virus: how revealing the molecular secrets of the virus responsible for the worst pandemic in recorded history can guide our response to future influenza pandemics. Infect Disord Drug Targets. 2007;7:294–303. doi: 10.2174/187152607783018772. [DOI] [PubMed] [Google Scholar]
- 10.Moye P.K., Pesik N., Terndrup T., Roe J., Weissman N., Kiefe C. Bioterrorism training in U.S. emergency medicine residencies: has it changed since 9/11? Acad Emerg Med. 2007;14:221–227. doi: 10.1197/j.aem.2006.10.102. [DOI] [PubMed] [Google Scholar]
- 11.Hu Y.Y., Adams R.E., Boscarino J.A., Laraque D. Training needs of pediatricians facing the environmental health and bioterrorism consequences of September 11th. Mt Sinai J Med. 2006;73:1156–1164. [PubMed] [Google Scholar]
- 12.Murphy F.A. Emerging zoonoses: the challenge for public health and biodefense. Prev Vet Med. 2008;86:216–223. doi: 10.1016/j.prevetmed.2008.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xie H., Luo L., Su Z., Wang W., Wang Y., Sun M. Human resources allocation in centers of disease prevention and control in China. J Hyg Res. 2005;34:390–392. [PubMed] [Google Scholar]
- 14.Wang Y., Luo L., Sun M., Su Z., Ma N., Xie H. Factors and indicators which should be considered in calculating human resources allocation criteria of the centers of disease prevention and control in China. J Hyg Res. 2005;34:513–515. [PubMed] [Google Scholar]
- 15.The Ministry of health . 2005. Some provisions on the construction of the disease prevention and control system. Ministry of public health of the people's Republic of China. [Google Scholar]
- 16.Boedigheimer S.F., Gebbie K.M. Currently employed public health administrators: are they prepared? J Public Health Manag Pract. 2001;7:30–36. doi: 10.1097/00124784-200107010-00007. [DOI] [PubMed] [Google Scholar]
- 17.Allegrante J.P., Moon R.W., Auld M.E., Gebbie K.M. Continuing-education needs of the currently employed public health education workforce. Am J Public Health. 2001;91:1230–1234. doi: 10.2105/ajph.91.8.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacIntyre C.R., Chughtai A.A., Seale H., Richards G.A., Davidson P.M. Uncertainty, risk analysis and change for Ebola personal protective equipment guidelines. Int J Nurs Stud. 2015;52:899–903. doi: 10.1016/j.ijnurstu.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang L., Hao Y., Sun H., Zhang Y., Wu Q. Analysis on personnel's emergency capacities of CDCs in Heilongjiang Province. Chin Health Resour. 2013;16:18–20. [Google Scholar]
- 20.Xiang H., Wang C., Xu Y., Nie S. Current situation and analysis of emergency responders in public health emergencies in China. Chin J Prev Med. 2007;41:9–11. [Google Scholar]
- 21.Zhang Y., Hao Y., Wu Q., Liu Y., Gao S. Studying on evaluation of public health emergency response ability and its application at home and abroad. Chin Health Serv Manag. 2009;4:220–228. [Google Scholar]
- 22.Bo T., Li S. Research status and prospect of emergency response capability of public health emergencies. Prev Med Trib. 2007;13:628–631. [Google Scholar]
- 23.Public Health Policy Research Office of the Chinese Center for Disease Control and Prevention . Peking Union Medical College Press; 2003. Reform and thinking of public health in China. [Google Scholar]
- 24.Li F., Zhang H., Cheng S., Wang L., Zhang M., Han X. The analysis of the influencing factors on public health emergency response capacity construction. Chin J Public Health. 2007;23:1235–1236. [Google Scholar]
- 25.Huang J. China should establish what kind of public health response system from SARS Crisis. Natl Med J China. 2003;83:1553–1555. [Google Scholar]
- 26.Bureau of Statistics in Heilongjiang Heilongjiang municipal GDP and per capita GDP ranking. 2015. http://www.phbang.cn/finance/data/152416.html Available from: Accessed March 4, 2016.
- 27.Wang X., Yin J., Su H., Gao F., Wu Q. The investigation of health emergency capacity in the municipal CDC of Heilongjiang. Chin J PHM. 2012;28:632–634. [Google Scholar]
- 28.Xu J., Wu Q., Hao Y., Ning N., Kang Z. Screening of key techniques for public health emergency management based on TOPSIS method. Chin J Public Health. 2013;29:632–634. [Google Scholar]
- 29.Fan L., Chen L., Li L. Analysis on current manpower resources and countermeasure to management of center for disease control and prevention. Chin J Dis Control Prev. 2005;9:481–482. [Google Scholar]
- 30.Wang C., Wei S., Liu J., Liao Q., He J., Liu L. Study on current situation and influential factors on public health emergency among staff from center of disease control and prevention in Hubei province. Chin J Public Health. 2007;23:731–733. [Google Scholar]
- 31.Wei S., Liao Q., Nie S., Luo L., Hu S. Investigation on capabilities of early warning, analysis and decision making for public health emergency events. Chin J Public Health. 2007;23:347–348. [Google Scholar]
- 32.Sommer A. Toward a better educated public health workforce. Am J Public Health. 2000;90:1194–1195. doi: 10.2105/ajph.90.8.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Evans D., Dowling S. Developing a multi-disciplinary public health specialist workforce: training implications of current UK policy. J Epidemiol Community Health. 2002;56:744–747. doi: 10.1136/jech.56.10.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Horney J.A., Sollecito W., Alexander L.K. Competency-based preparedness training for public health practitioners. J Public Health Manag Pract. 2005:S147–9. doi: 10.1097/00124784-200511001-00027. [DOI] [PubMed] [Google Scholar]
- 35.Dong X., Hao Y., Wu Q., Liu J., Chen H., Cui X. Influencing factors of epidemiological investigation ability among emergency responders of CDC. Chin J Public Health. 2013;29:647–650. [Google Scholar]
- 36.Chen J., Wu Q., Hao Y., Li B., Zhao Z., Xu H. Analysis on epidemiological investigation ability and the influencing factors in CDC. Chin J PHM. 2006;22:184–187. [Google Scholar]
- 37.Ning N., Wu Q., Li B., Teng B., Liu Q., Yu D. Investigation and analysis on current status of emergency training to staffs of centers for disease control and prevention in Heilongjiang Province. Chin Health Econ. 2008;27:66–69. [Google Scholar]
- 38.Verbeek J.H., Ijaz S., Mischke C., Ruotsalainen J.H., Mäkelä E., Neuvonen K. Personal protective equipment for preventing highly infectious diseases due to contact with contaminated body fluids in health care staff. Cochrane Database Syst Rev. 2016;(4) doi: 10.1002/14651858.CD011621.pub2. CD011621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lescano A.G., Salmon-Mulanovich G., Pedroni E., Blazes D.L. Epidemiology: outbreak investigation and response training. Science. 2007;318:574–575. doi: 10.1126/science.1146837. [DOI] [PubMed] [Google Scholar]
- 40.Yao H. The role of personal protective equipment in public health emergency. Chin Pers Prot Equip. 2005;1:7–9. [Google Scholar]
- 41.Fischer W.A., 2nd, Weber D.J., Wohl D.A. Personal protective equipment: protecting health care providers in an Ebola outbreak. Clin Ther. 2015;37:2402–2410. doi: 10.1016/j.clinthera.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao Z., Wu Q., Ding D., Wang X., Kang Z., Ning N. Analysis on obstacle factors for promotion of emergency response techniques with factor analysis. Chin J Public Health. 2014;30:926–928. [Google Scholar]
- 43.Dredger S.M., Kothari A., Morrison J., Sawada M., Crighton E.J., Graham I.D. Using participatory design to develop (public) health decision support systems through GIS. Int J Health Geogr. 2007;6:53. doi: 10.1186/1476-072X-6-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cohen J. Infectious diseases. When Ebola protection fails. Science. 2014;346:17–18. doi: 10.1126/science.346.6205.17. [DOI] [PubMed] [Google Scholar]
- 45.Weber D.J., Rutala W.A., Schaffner W. Lessons learned: protection of healthcare workers from infectious disease risks. Crit Care Med. 2010;38:S306–14. doi: 10.1097/CCM.0b013e3181e69ebd. [DOI] [PubMed] [Google Scholar]
- 46.Dausey D.J., Buehler J.W., Lurie N. Designing and conducting tabletop exercises to assess public health preparedness for manmade and naturally occurring biological threats. BMC Public Health. 2007;7:92. doi: 10.1186/1471-2458-7-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Federal Emergency Management Agency Emergency management institute. http://www.training.fema.gov/EMIWEB Unit 11: Course training; Available from: Accessed January 19, 2016.
- 48.Haddow G.D., Haddow K.S. Disaster Communications in a changing media world. 2nd ed. 2014. Chapter eleven-communicating during a public health crisis; pp. 195–209. [Google Scholar]
- 49.Holmes B.J., Henrich N. Communicating with the public during health crises: experts' experiences and opinions. J Risk Res. 2009;12:793–807. [Google Scholar]