Highlights
-
•
Indoor air is an important vehicle for a variety of human pathogens.
-
•
Review of airborne transmission of infectious agents from experimental and field studies, predisposing to establish air-surface-air nexus and possible ways of transmission to susceptible hosts.
-
•
An overview of the methods for experimentally generating and recovering airborne human pathogens and environmental factors affecting their survival in air.
-
•
Current and emerging technologies for decontamination of indoor air for human pathogens.
-
•
Design, establishment, and validation of a room-size aerobiology chamber meeting the U.S. Environmental Protection Agency guidelines (2012) that can be used for assessment of air-decontamination technologies.
Key Words: Indoor air microbiome, Airborne pathogens, Microbial aerosols, Aerosolized pathogens, Air-surface-air nexus, Aerobiologic testing chamber, Air decontamination technologies
Abstract
Indoor air can be an important vehicle for a variety of human pathogens. This review provides examples of airborne transmission of infectious agents from experimental and field studies and discusses how airborne pathogens can contaminate other parts of the environment to give rise to secondary vehicles leading air-surface-air nexus with possible transmission to susceptible hosts. The following groups of human pathogens are covered because of their known or potential airborne spread: vegetative bacteria (staphylococci and legionellae), fungi (Aspergillus, Penicillium, and Cladosporium spp and Stachybotrys chartarum), enteric viruses (noro- and rotaviruses), respiratory viruses (influenza and coronaviruses), mycobacteria (tuberculous and nontuberculous), and bacterial spore formers (Clostridium difficile and Bacillus anthracis). An overview of methods for experimentally generating and recovering airborne human pathogens is included, along with a discussion of factors that influence microbial survival in indoor air. Available guidelines from the U.S. Environmental Protection Agency and other global regulatory bodies for the study of airborne pathogens are critically reviewed with particular reference to microbial surrogates that are recommended. Recent developments in experimental facilities to contaminate indoor air with microbial aerosols are presented, along with emerging technologies to decontaminate indoor air under field-relevant conditions. Furthermore, the role that air decontamination may play in reducing the contamination of environmental surfaces and its combined impact on interrupting the risk of pathogen spread in both domestic and institutional settings is discussed.
Air, a universal environmental equalizer, affects all living and nonliving forms on planet earth. For humans, it has profound health implications in all indoor environments where we normally spend most of our time.1, 2, 3 Air quality is also forever changing because of the influence of many controllable and uncontrollable factors that are virtually everywhere. Indoor air, in particular, can expose us to noxious chemicals, particulates, and a variety of infectious agents, as well as pollen and other allergens.4, 5
Emerging pathogens, such as noroviruses6 and Clostridium difficile,7 have also been detected in indoor air, with a strong potential for airborne dissemination. Pathogens discharged into the air may settle on environmental surfaces, which could then become secondary vehicles for the spread of infectious agents indoors.8 The possible transmission of drug-resistant bacteria by indoor air adds another cause for concern.9 A combination of on-going societal changes is adding further to the potential of air as a vehicle for infectious agents.10, 11, 12 The quality of indoor air is therefore a prominent public health concern13, 14 that requires a clear understanding of the transmission processes for the development and implementation of targeted infection prevention and control measures.15
Although direct and indirect exposure to pathogens in the air can occur by other means, infections from the inhalation and retention, including translocation and ingestion after inhalation of droplet nuclei, are generally regarded as true airborne spread. Aerosols of various sizes that contain infectious agents can be emitted from a variety of sources, such as infected or colonized individuals16 or flushing toilets, and may expose susceptible persons either directly (droplet transmission) or by remaining suspended in the air for inhalation (airborne transmission).17, 18 Contrary to the conventionally held belief, modeling work has redefined the Wells evaporation-falling curve,19, 20 revealing that expelled large droplets could be carried >6 m away by exhaled air at a velocity of 50 m/s (sneezing), >2 m away at a velocity of 10 m/s (coughing), and <1 m away at a velocity of 1 m/s (breathing), leading to potential transmission of short-range infectious agents that contain aerosols.21
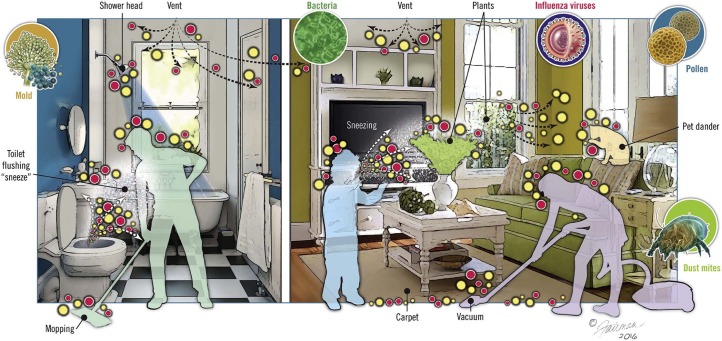
Airborne transmission requires that pathogens survive the process of aerosolization and persist in the air long enough to be transmitted to a susceptible host.22 Aerosolized pathogens may settle onto environmental surfaces in the immediate vicinity, leading to genesis of secondary vehicles (Fig 1 ).23 This review provides current information on the spread of human pathogens by indoor air, with a focus on the major classes of human pathogens from experimental and field studies, and on emerging air decontamination technologies, including test protocols developed to assess their performance under field-relevant conditions.
Fig 1.
Sources of airborne pathogens indoors and potential for environmental surface contamination. These sources may include humans; pets; plants; plumbing systems, such as operational toilets and shower heads; heating, ventilation, vacuuming, mopping, and air-conditioning systems; resuspension of settled dust; and outdoor air. The yellow and red dots represent human pathogens or harmless microorganisms.
Adapted with permission from BioMed Central.23
Methods for studying airborne human pathogens
The study of aerosolized human pathogens requires the ability to produce them experimentally at the appropriate size, store them, and sample them for residual infectious content over a predetermined time period.13 The equipment must also simulate naturally occurring environmental conditions and the duration of exposure to accurately assess aerosol survivability.24 Various analytical methods and air samplers have been used to characterize airborne pathogens and overcome the challenges of collecting and analyzing them. Relevant studies have been reviewed in detail elsewhere.13, 25, 26
Environmental factors that influence airborne microbial survival
Aerosolized microbes must survive the prevailing environmental conditions to potentially infect a susceptible host.22 Multiple factors affect airborne survival of microbes indoors (Table 1 ).13, 31 The effect of these factors on different types of microbes varies, and generalizations can be difficult because of differences in the experimental methodologies used.27 Air temperature, relative humidity (RH), and turbulence are among the more important factors affecting the fate and spread of infectious agents indoors.
Table 1.
| Environmental factor | Viruses | Bacteria | Fungi |
|---|---|---|---|
| Temperature |
|
|
|
| RH* |
|
|
|
| Atmospheric gases |
|
|
|
| Light and irradiation |
|
|
|
| Surrounding organic material (eg, saliva, mucus) |
|
|
|
CO, carbon monoxide; RH, relative humidity; UV, ultraviolet.
RH is a measure of the amount of water vapor in the air at a specific temperature; therefore, temperature and RH always interact to affect survival.
The analysis of air samples for microbes now includes methods that are based on the polymerase chain reaction (PCR). However, PCR-based methods typically cannot differentiate between viable and nonviable microbes.32 A recent study found that PCR substantially overestimated the quantity of infectious airborne influenza virus, but the differences in infectious versus noninfectious virus over time were similar to data from quantification by plaque-forming units, which determined that virus losses were evident within 30-60 minutes postaerosolization.32 Generally, enveloped viruses survive better at lower RH, but there are many exceptions.28 Other factors that affect aerosol activation in relation to RH include evaporative activity (ie, dehydration, rehydration), surface areas of particles, and pH.28
Airborne spread of major classes of human pathogens
Although studies with experimental animals have determined the susceptibility to airborne pathogens and the minimal infective inhalation dose of a given pathogen,25 there are wide variations in their test design. First, the number of inhaled microbes may not be known or it may be unrealistically high. Second, the test protocol may not have fully excluded microbial exposure by means other than inhalation. Third, there may be incomplete recording of the environmental conditions (eg, RH, air temperature) to assess their impact on microbial viability. Fourth, pertinent differences may exist between laboratory-adapted strains of the tested microbe compared with strains in the field. Studies using the actual pathogen aerosolized in body fluids provide the strongest evidence of pathogen survivability.18
In contrast, field studies face their own set of challenges, which include the noise, bulk, and expense of inefficient air collection devices.25 Moreover, passive impingers may not adequately collect low concentrations of pathogens found in the clinical environment.33 Slit sampling does not impose size exclusion and may be more effective at recovering viable pathogens of any size.33 From a methodologic perspective, field studies also must control for potential variables, such as air turbulence or human activity in areas proximate to sampling, such that sampling occurs before, during, and after an area is occupied and should include functioning ventilation systems.34
We have previously reviewed published studies on the airborne spread of viruses of animals and humans.13, 25 Table 2 summarizes key human pathogens with evidence of aerosol transmission. A number of these pathogens causes severe disease, and their classification as high risk by the U.S. Centers for Disease Control and Prevention and the World Health Organization emphasizes the need for appropriate control measures.18
Table 2.
Key human pathogens with evidence of aerosol transmission18
| Viruses | Bacteria |
|---|---|
Enteric
Respiratory
Neurologic
Skin
|
|
| Fungi | |
|---|---|
|
Aspergillus spp Penicillium spp Cladosporium spp Stachybotrys chartarum |
MRSA, methicillin-resistant Staphylococcus aureus; SARS, severe acute respiratory syndrome.
Viruses
Experimental studies have used surrogates for human pathogenic enveloped and nonenveloped viruses, such as Cystovirus (ϕ6) and bacteriophage MS-2, respectively.35 Enteric viruses are transmitted primarily by the fecal-oral route, but airborne transmission has been reported.13 Airborne transmission of norovirus may be possible via aerosolization of vomitus and toilet flushing, which are regarded as potential sources of both indoor air and environmental surface contamination. Enteric bacteria and viruses have been recovered from indoor air and environmental surfaces in areas surrounding toilets.18, 36, 37 We reported that aerosolized simian rotavirus SA-1138 survived best at midrange RH.39, 40 These results contradicted a prior study by Moe and Harper,41 in which the UK strain of calf rotavirus was reported to survive best at low and high RH, but not at high temperature.41 Subsequent studies on human rotavirus,39 murine rotavirus, and a UK strain of calf rotavirus, aerosolized under the same experimental setup, confirmed the behavior of all strains of rotaviruses are similar in airborne state.39, 40 Furthermore, studies of different picornaviruses (poliovirus type 1 [Sabin] and human rhinovirus) and a human coronavirus (an enveloped virus) that used the same experimental conditions produced results that were consistent with the published literature, suggesting that the experimental design did not introduce bias toward the behavior of aerosolized rotaviruses.39, 42, 43
Among the respiratory viruses, influenza virus is present in the air around infected individuals, and airborne transmission via droplet nuclei has been demonstrated in experimental models and in reports of influenza spread on-board aircrafts.15 Low RH favors airborne survival and transmission; however, high air exchange rates facilitate dilution of virus-containing aerosols, regardless of their size.12 A recent study confirmed recovery of influenza virus from the air emitted by infected persons at distances of 0.5-1.5 m, which could reach the breathing zone of susceptible individuals, including health care workers.44
Surprisingly, and in spite of much study, the exact mode of and the relative importance of various types of vehicles for transmission of rhinoviruses, which are the most frequent cause of the common cold, remain shrouded in mystery.45, 46 The behavior of experimentally aerosolized rhinovirus type 14, which represents typical picornaviruses (as previously mentioned),43 coupled with rhinovirus recovery from both indoor air47 and outdoor air,48 substantiate the role of air as a vehicle in spread of some of these picornaviruses. Taken together, an overall assessment of the available evidence suggests a role for airborne spread49 and for the role of contaminated hands and environmental surfaces in rhinovirus dissemination.50
Coronaviruses are the second leading cause of the common cold and are also responsible for the severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome.37 SARS is thought to be transmitted via direct contact, but airborne transmission is also suspected because the virus has been detected in air samples that were collected from rooms where a patient was recovering from SARS.18, 33 The virus is spread through droplets and can remain viable on surfaces for several days at room temperature. The use of aerosol-generating procedures, such as intubation, bronchoscopy, and oxygen delivery vents, may promote dispersal of SARS via enhanced release in mists of exhaled pulmonary gases.34, 51 Our earlier work on the behavior of aerosolized human coronaviruses 229E further substantiates the potential role of air in their aerial spread.39
Aerosol transmission of the Ebola virus is biologically plausible.18 The virus is present in saliva, stool, blood, and other body fluids; therefore, it could be aerosolized through symptoms associated with infection or via health care procedures. The Ebola virus has been shown to survive in the air when the half-life of the virus ranged from 15 (Zaire Ebola virus) to 24 minutes (Reston Ebola virus), and the time for 99% biologic decay of the aerosolized virus held in rotating drum (at 50%-55% RH and 22°C ± 3°C) was estimated to be between 104 and 162 minutes. Additionally, infection of rhesus monkeys via experimentally aerosolized Ebola virus has also been reported.52 These findings raise concerns for aerosol transmission and control of this serious pathogen; however, thus far, there is no clear evidence for the airborne spread of this virus in humans.18 Epidemiologic evidence indicates transmission is associated with direct physical contact or contact with body fluids; however, the possibility of aerosolized spread has been postulated by Ebola virologists.18, 53
Bacteria
Approximately one-third of humans carry Staphylococcus aureus, with the anterior nares as a common site of colonization,54 and environmental contamination plays an important role in the transmission of methicillin-resistant S aureus. Shedding of the bacteria is highly variable, but transmission likely occurs via skin squames that settle out on environmental surfaces in the vicinity. Smaller particles may remain airborne, particularly if there is air turbulence.54, 55 An important characteristic of the staphylococci is their ability to survive over a wide range of temperatures, RH, and exposure to sunlight.54
Mycobacterium tuberculosis is transmitted via droplet nuclei expectorated from infected persons during coughing, sneezing, and talking.18, 34 Control measures include expensive negative-pressure ventilation and less expensive, but climate-dependent, natural ventilation.56 Upper-room ultraviolet (UV) light or negative air ionization may help reduce the airborne spread of M tuberculosis.56
Nontuberculous mycobacteria are found in soil and water sources and can form biofilms under domestic environments, such as shower heads.57 Transmission to humans is uncertain, but droplet aerosolization is a suspected route of pulmonary disease, with shower heads considered a common source.57, 58 Contamination of hospital water supplies and medical equipment are suspected in nosocomial outbreaks of disease.59 Similarly, Legionella spp become airborne by active aerosolization of contaminated water and form biofilms in air conditioning systems.34 Legionella-like amoebal pathogens are a subset of bacteria that grow within amoebae and often are coinfectious agents with other bacteria and fungi.60
Clostridium difficile spores have been recovered from the air near symptomatic patients, especially those with recent-onset diarrhea.61 Air samples were positive for C difficile in 70% of patients, and the highest levels of surface recovery were in areas closest to the patient.7 The isolates recovered from the air were indistinguishable from those recovered from fecal samples and from the environment in the same settings.7 Additionally, C difficile has been recovered after toilet flushing, and leaving the lid open when flushing increases contamination of surrounding environmental surfaces.61
Airborne infection of Bacillus anthracis is affected by environmental factors that include room size, ventilation rate, and host factors, such as pulmonary ventilation rate.62 Secondary aerosolization of viable B anthracis spores was reported after contamination of a U.S. Senate office, with >80% of particles being in the respirable size range of 0.95-3.5 µm.14
Fungi
As ubiquitous microorganisms, fungi pose a health threat in indoor environments.29 Fungal infections can be particularly serious in immunocompromised patients,63 especially airborne spores of Aspergillus spp that are blown in from natural ventilation sources.27 Fungal spores are aerosolized from municipal water supplies and dust and can be effectively transported over long distances by wind and air currents.63, 64 The evolution of the fungal spore has enabled them to travel long distances and be more capable of withstanding environmental insults.27 The most important factor of fungal growth in indoor environments is humidity65; therefore, control measures include dehumidification of the air and high-efficiency particulate arrestor filtration.27
Recent research suggests that airborne fungal particles are heterogeneous and comprise spores and submicrometer fragments.66, 67 These fragments are of significant interest with regard to health because they remain in the air longer and are easily inhaled. There are also a variety of fungal components that have been identified in air, including mycotoxins, ergosterols, glucans, and microbial volatile organic compounds, and these require unique analysis methods.64 Taken together, these findings provide a foundation for the definition of sick building syndrome.68 High humidity within sick houses and buildings allows for growth of fungi indoors, particularly species of Aspergillus, Penicillium, and Cladosporium and Stachybotrys chartarum, an indoor mold that was associated with sick building syndrome several decades ago.64, 68, 69 These fungi can be found in dust, furniture, carpets, and ventilation systems at concentrations ranging from 0-1,000 colony-forming unit (CFU)/m3.64 In fact, carpet has been described as a sink for fungi, but it is also a source for resuspension of fungal particles into the air.64 Various respiratory conditions (eg, wheeze, cough, asthma) have been linked to fungi and their biologic components in the indoor environment.64 Fungal species found outdoors include Cladosporium and Alternaria spp, which are responsible for triggering hypersensitivity reactions, including rhinitis, sinusitis, and asthma.27, 64
Current and emerging air decontamination technologies
The clear recognition of indoor air as a vehicle for pathogens has incurred a corresponding upsurge in the marketing of products and technologies with claims for safe and effective decontamination of air.70 Although many technologies are available for environmental surface decontamination, the number and variety of those for decontamination of indoor air remain limited and of questionable veracity (Table 3 ). The air-decontaminating claims of many such technologies are not based on testing under field-relevant conditions with pathogens relevant to human health, and scientifically valid and standardized protocols to generate field-relevant data for label claims for review by regulatory and public health agencies and the public at large remain unavailable. Here, we address this gap in the development of a test platform for standardized testing of commercially available devices for decontaminating indoor air of vegetative bacteria that represent airborne human pathogens. We know of only one guideline that directly relates to this topic.71 It specifies the size of a sealed enclosure for experimental contamination of the air with aerosols of vegetative bacteria to assess technologies for their temporary reduction. Therefore, the text that follows relates directly to that guideline.
Table 3.
Current and emerging technologies for decontamination of indoor air for human pathogens
| Technology | Description | Pathogen tested | Remarks |
|---|---|---|---|
| UV irradiation | |||
| Microgenix air purification system | Chemical-coated filter and UV source for reducing microbes in HVAC systems | Aerosolized MS-2 phage as surrogate for viruses |
|
| Upper-room 254 nm UVC light | Exposure to UV light (254 nm) field separated by manifolds at 4 levels of temperature and RH | Porcine reproductive and respiratory syndrome virus |
|
| UV light (254 nm) at 3 levels of RH | Influenza A virus (H1N1, PR-8) |
|
|
| UV light (254 nm) under real-world conditions of convection, mixing, temperature, and RH | Vaccinia virus as a surrogate for smallpox |
|
|
| UV light (254 nm) | Respiratory adenovirus, murine hepatitis virus, a coronavirus as surrogate for SARS, and bacteriophage MS-2 |
|
|
| UV germicidal irradiation (8 lamps emitting peak 253.7 nm UVC light) | Airborne virus was passed through a cylinder that was 0-30 cm from UV source | Four bacteriophages (a single strand each of RNA and DNA and a double strand each of RNA and DNA) |
|
| Oxygen-based technologies | |||
| Hydroxyl/Odorox product | Claims to inactivate all types of pathogens on surfaces and in the air |
|
|
| Phocatox | Combination of HEPA filtration, hydroxyl radical production, purified O3, and vaporized gas-phase hydrogen peroxide plus UVC | Claims to decontaminate air and surfaces of a wide range of pathogens—viruses, bacteria (including MRSA and Clostridium difficile), and fungi |
|
| TriAir T250 | Hydroxyl radicals | Gram-positive and gram-negative bacteria; enveloped and nonenveloped viruses |
|
| Inov8 Air Disinfection unit | Hydroxyl radicals | All types of pathogens |
|
| Ozone generator | Gaseous ozone and aerosolized virus were generated continuously into the chamber | Bacteriophages: single-strand RNA and DNA, double-strand RNA and DNA |
|
| Cold oxygen plasma | Viruses nebulized into tunnel with phosphate-buffered saline | Human parainfluenza virus-3, respiratory syncytial virus, influenza virus H5N2 |
|
| Nonthermal plasma reactors | Air flows in near the floor and is filtered with plasma and exhausted from top | H5N2 avian flu strain as surrogate for H1N1 |
|
| Sharp air purifier | Combination of plasmacluster ion technology and multiple layers of filtration | Bacteria and viruses |
|
HEPA, high-efficiency particulate arrestor; HVAC, heating, ventilation, air conditioning; MRSA, methicillin-resistant Staphylococcus aureus; RH, relative humidity; SARS, severe acute respiratory syndrome; UV, ultraviolet; UVC, energy-rich ultraviolet light with a wavelength of 200-400 nanometers (nm).
Adapted with permission from Elsevier.25
Basic experimental design and operation of an aerobiology chamber
The studies of microbial survival in indoor air, as well as proper assessment of methods for its decontamination, emphasize numerous challenges and highlight the need for specialized equipment and protocols. Proper expertise and suitable experimental facilities for such investigations remain uncommon. Several of the available sites with testing claims are neither experienced in, nor equipped to conforming with, the U.S. Environmental Protection Agency's (EPA) guidelines on testing the sanitization of indoor air.71 Based on our considerable experience in the study of airborne human pathogens,13, 25, 39, 43, 72 we have built an aerobiology chamber (Fig 2 ) designed to meet the requirements of the EPA guidelines and have used this to study the effects that a variety of air decontamination technologies have on the airborne survival and inactivation of vegetative bacteria, viruses (bacteriophage), and bacterial spore-formers (Sattar et al, unpublished data). Additional details about the operational aspects of the aerobiology chamber, described elsewhere,73 are discussed briefly.
Fig 2.
Aerobiology chamber with essential components (length × width × height: 320.0 × 360.6 × 211.0 cm—24.3 m3 [860 ft3]). Reprinted with permission from Elsevier.73
Experiments using the aerobiology chamber
Testing microbial survival
Any meaningful assessment of air decontamination requires that the aerosolized challenge microbe remain viable in the experimentally contaminated air long enough to allow for proper differentiation between its biologic decay or physical fallout and inactivation or removal by the technology being assessed. Therefore, initial testing is required to determine the rate of biologic decay of the test microorganism(s) under the experimental conditions to be used for testing potential air decontamination technologies. For this, the test microorganism(s) was aerosolized into the chamber, and 2-minute air samples were collected at different intervals using a slit-to-agar (STA) sampler over an 8-hour period. The culture plates were incubated at 36°C ± 1°C, the CFU on them was recorded, and the data were analyzed to determine the rate of biologic decay.
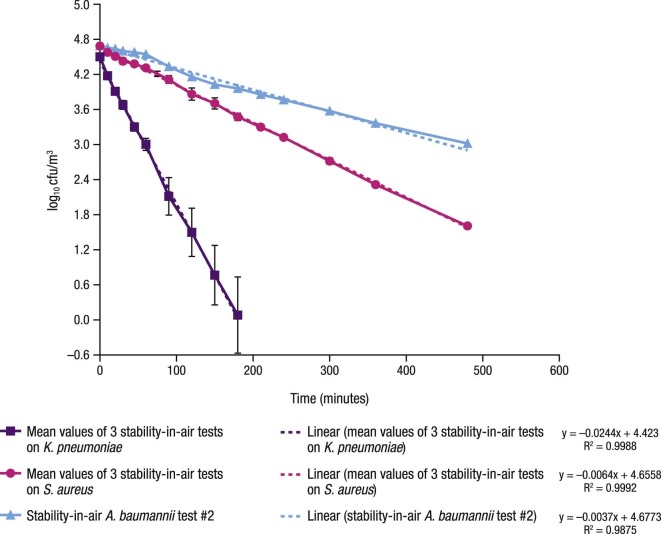
The results of the tests on the airborne survival of 3 types of vegetative bacteria are shown in Figure 3 . Acinetobacter baumannii (ATCC 19606; ATCC, Manassas, VA) proved to be the most stable in air, followed by S aureus (ATCC 6538; ATCC) and Klebsiella pneumoniae (ATCC 4352; ATCC).
Fig 3.
Comparative rates of biologic decay of aerosolized A. baumannii, S. aureus, and K. pneumoniae held within the aerobiology chamber. A. baumannii, Acinetobacter baumannii; cfu, colony forming units; K. pneumoniae, Klebsiella pneumoniae; S. aureus, Staphylococcus aureus.
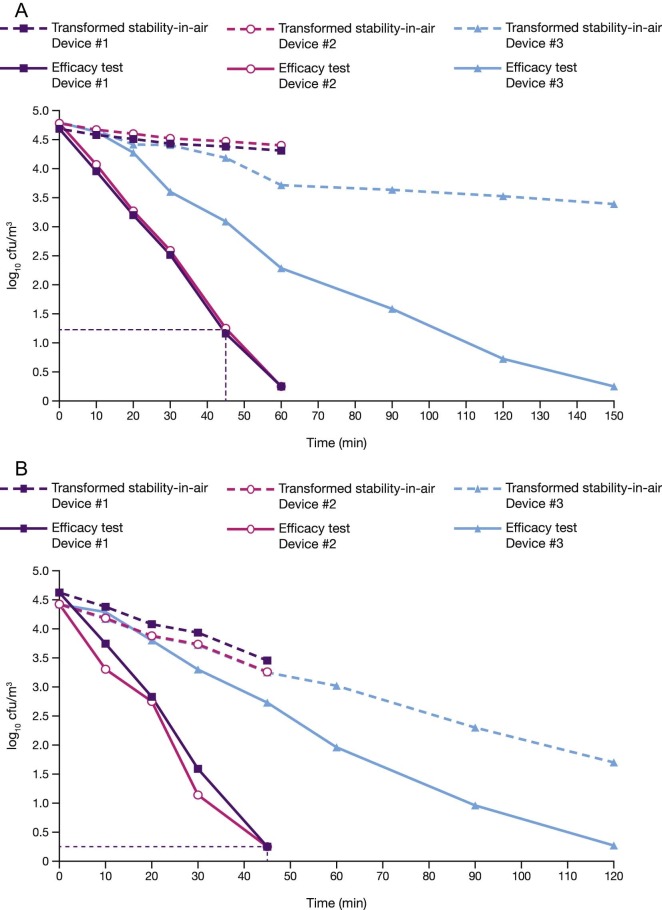
Testing of 3 types of indoor air decontamination devices
Three types of commercially available indoor air decontamination devices that were based on UV light and high-efficiency particulate arrestor filtration were tested for their ability to reduce the levels of viable bacteria in the air of the chamber (Table 4 ). The air within the chamber was first experimentally contaminated with aerosolized test bacterium suspended in a soil load. The test device, placed inside the chamber, was remotely operated, and samples of the chamber air were collected directly onto Petri plates using STA and were incubated for CFU determinations.
Table 4.
Specifications of 3 devices that were tested for their ability to decontaminate experimentally aerosolized microbial challenge within the aerobiology chamber
| Device no. | Flow rate, ft3/min (m3/min) | Time to expose entire contents of the chamber once | Theoretical no. of exposures of an aerosol particle in 8 h | UV light bulb wattage |
|---|---|---|---|---|
| 1 | 100(2.831) | 0.143 h(8.594 min) | 55.94 | 5(LB4000) |
| 2 | 120(3.398) | 0.12 h(7.16 min) | 66.67 | 8(LB5000) |
| 3 | 60(1.699) | 0.239 h(14.32 min) | 33.47 | 9(ZW6S12W) |
UV, ultraviolet.
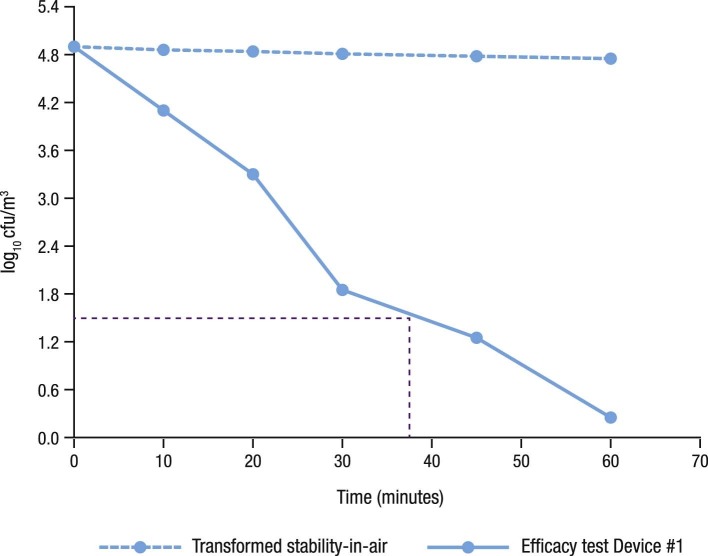
As shown in Fig 4, Fig 4 , the air decontamination devices that were tested could achieve a 3-log10 reduction in viability of S aureus and K pneumoniae in 38-45 minutes (Table 5). So far, such testing has been conducted only once with A baumannii using device 1, and as the data presented in Figure 5 show, it reduced the viability of A baumannii by 3 log10 in 38 minutes (Table 5).
Fig 4.
(A) Comparative inactivation rates of airborne Staphylococcus aureus during the operation of 3 indoor air decontamination devices. cfu, colony forming units. Reprinted with permission from Elsevier.73 (B) Comparative inactivation rates of airborne Klebsiella pneumoniae during the operation of 3 indoor air decontamination devices. cfu, colony forming units. Reprinted with permission from Elsevier.73
Table 5.
Regression coefficients, P values comparing decay rates of efficacy tests with stability in air, and times required to achieve 3 log10 reductions
| Device | Slope | Intercept | P value | ≥3 log10 reduction (min) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S aureus | K pneumoniae | A baumannii | S aureus | K pneumoniae | A baumannii | S aureus | K pneumoniae | A baumannii | S aureus | K pneumoniae | A baumannii | |
| Stability in air | −0.0064 | −0.0244 | −0.0037 | 4.6471 | 4.4657 | 4.8829 | NA | NA | NA | NA | NA | NA |
| Efficacy test device 1 | −0.0752 | −0.099 | −0.079 | 4.6977 | 4.6871 | 4.7821 | 3.82 × 10−10 | 2.93 × 10−5 | NA | 45 | 45 | 38 |
| Efficacy test device 2 | −0.0766 | −0.0983 | ND | 4.8243 | 4.5763 | ND | 1.39 × 10−9 | 2.00 × 10−4 | NA | 45 | 45 | ND |
| Efficacy test device 3 | −0.0224 | −0.0369 | ND | 4.9301 | 4.4449 | ND | 2.13 × 10−10 | 2.93 × 10−5 | NA | 215 | 215 | ND |
A baumannii, Acinetobacter baumannii; K pneumoniae, Klebsiella pneumoniae; NA, not applicable; ND, not done; S aureus, Staphylococcus aureus.
Fig 5.
Inactivation of aerosolized Acinetobacter baumannii during operation of an indoor air decontamination device (device 1). cfu, colony forming units.
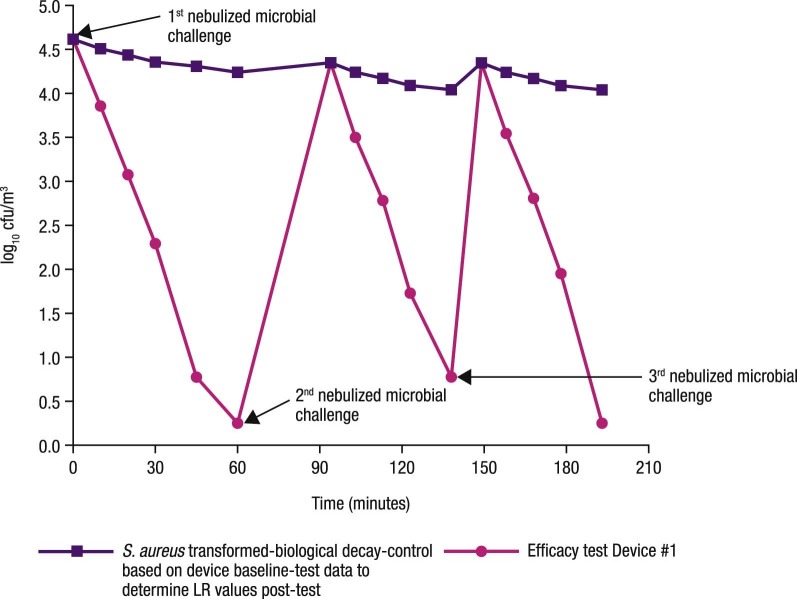
Testing with repeated microbial challenge
In this experiment, device 1 was tested for its ability to manage ongoing fluctuations in the microbiologic quality of indoor air. A suspension of S aureus was nebulized into the chamber at 3 separate time points, while the device operated continuously. As shown in Figure 6 , the device's efficacy after the 3 challenges with aerosolized bacteria was almost the same. The times at which the device demonstrated 3-log10 reductions after each nebulization were found to be 40, 39.5, and 40.9 minutes. The mean of the 3-log10 reduction times was 40.13 ± 0.71 minutes, giving an average biologic decay rate of aerosolized bacteria of 0.0753 ± 0.0024 CFU/m3/min after the 3 nebulizations.
Fig 6.
Repeated microbial challenge with aerosolized S. aureus during operation of device 1. cfu, colony forming units; LR, log10 reduction; S. aureus, Staphylococcus aureus.
Reducing microbial contamination of environmental surfaces by inactivation of airborne vegetative bacteria
As previously mentioned, larger particles of aerosolized pathogens often settle onto environmental surfaces in the immediate vicinity, leading to contamination as a secondary vehicle of transmission, or reaerosolize through human or mechanical activity, such as vacuuming. To determine if targeting aerosolized microorganisms could reduce the contamination of environmental surfaces, device 1, with proven efficacy against airborne vegetative bacteria, was tested to see if it could also reduce the level of contamination of environmental surfaces in the same setting. S aureus (ATCC 6538; ATCC) was used as the challenge microbial aerosol, and surfaces were disposable plastic Petri plates (100 mm in diameter).
Fifteen sterile plastic plates were placed in groups of 3 on the floor of the aerobiology chamber, with one set in each of the 4 corners and one in the center. The lids of the plates were removed. A suspension of S aureus in a soil load was nebulized into the chamber with the muffin fan operating for 5 minutes to evenly distribute the airborne bacterial particles. A 2-minute air sample was then collected from the chamber using an STA sampler to determine the initial level of airborne contamination. Ten minutes were allowed to elapse for circulation of the airborne bacteria in the chamber. The muffin fan was then turned off and the airborne bacteria were allowed to settle for 30 minutes. At the end of this period, the Petri plates were retrieved and eluted for CFU to determine the titer of microbial contamination deposited on each one. Such testing allowed us to determine the levels of airborne bacteria that could settle on the plates without air decontamination procedures.
The experiment was repeated in exactly the same manner, but with the test device in the chamber activated and allowed to work for 45 minutes. At the end of this period, the Petri plates were retrieved and eluted for CFU to determine the titer of microbial contamination deposited on each plate.
The results indicated that the nebulization of the microbial suspension for 10 minutes produced 4.7 log10 CFU/m3 of air in the chamber. The average level of CFU on the control and test Petri plates held in the chamber was 200 ± 110 and 8.3 ± 8.9, respectively. The device could reduce the contamination of the plates from airborne bacteria by 95% as compared with the controls.
Discussion and concluding remarks
Recognition that human pathogens can be transmitted via indoor air emphasizes the need for the development of control procedures that limit exposure and reduce the risk of infection in susceptible individuals. This need is heightened by an increase in the aging population and numbers of the immunosuppressed. We must also be prepared for an intentional or accidental release of infectious aerosols. Standardization of sampling and analytical methods is crucial to developing an understanding of airborne pathogens26 and technologies for their effective control.
We have described the creation and application of an aerobiology test chamber that complies with the relevant guideline of the EPA.71 The chamber was successfully used (1) to study the airborne survival of 3 types of vegetative bacteria under ambient conditions; (2) to test the ability of 3 commercial indoor air decontamination devices to abate experimentally generated aerosols of 3 types of vegetative bacteria; (3) to test one of the devices for its ability to deal with repeated microbial challenge with vegetative bacteria in simulation of situations in which indoor air is contaminated on an on-going basis; and (4) to test one of the air decontamination devices for its effectiveness in reducing the level of microbial contamination of environmental surfaces as a function of reducing airborne bacteria.
Each of these experiments was completed successfully, thereby demonstrating the suitability of the aerobiology chamber and the protocols for aerosol generation and sampling. The use of the STA sampler proved particularly effective for providing event-related information on the levels of viable bacteria in the air of the chamber.
The testing with A baumannii clearly demonstrated that it is more suitable than K pneumoniae as a surrogate for gram-negative bacteria. A baumannii is not only a relevant airborne pathogen that is more resistant to aerosolization, but it also is more stable in the airborne state.74 Therefore, it is recommended that it be considered as an alternative for K pneumoniae by regulatory agencies, such as the EPA, for testing and registration of air decontamination technologies.
The experimental facility and test protocols described here are suitable for work with other types of airborne human pathogens, such as viruses, fungi, and bacterial spore formers. The aerobiology chamber also could be readily adapted to assess emerging technologies of indoor air decontamination. Although the work reported here was performed in a sealed and empty chamber, as specified in the EPA guidelines, the aerobiology chamber can be modified to represent air exchanges, and furniture can be introduced to simulate a typical room under both domestic and institutional settings.
Air, in general, is crucial to the establishment and maintenance of the indoor microbiome, and the continual redistribution of microbes indoors occurs at the air-surface-air nexus. Although classic airborne spread of pathogens occurs via droplet nuclei, droplets can potentially contaminate environmental surfaces, depending on their size and prevailing environmental conditions, thereby creating secondary vehicles for pathogens. Therefore, targeting airborne pathogens could potentially provide an additional advantage by reducing environmental surface contamination. Our preliminary findings indicate that a reduction in the level of viable airborne bacteria using active air decontamination can also reduce bacterial contamination on environmental surfaces in the same setting. Therefore, targeting airborne pathogens could entail additional benefits, such as preventing or reducing the deposition of harmful microbes on secondary vehicles that include frequently touched environmental surfaces and also preventing or reducing their resuspension from these surfaces back into the air via a variety of indoor activities (Fig 1).8, 12, 17, 75, 76 Further studies should investigate the role air decontamination may play in reducing the contamination of environmental surfaces and its combined impact on interrupting the risk of pathogen spread in both domestic and institutional settings.
Acknowledgments
We thank Dr John A. Mitchell (Wordsmith Scientific and Regulatory, LLC, Bozeman, MT) and Elizabeth Bruning (RB, Montvale, NJ) for their critical review and feedback.
Footnotes
Funding/Support: This paper was presented at a workshop organized under the auspices of ASTM International's biannual meeting held in April 2016. Publication of this supplement is primarily supported by RB, Montvale, New Jersey, with additional support from MicroBioTest, a division of Microbac Laboratories, Inc., Sterling, Virginia. The City University of New York (CUNY) and the University of Ottawa, Ottawa, Canada, are academic sponsors. Editorial support was provided by Ashely O'Dunne, PhD; Shannon O'Sullivan, ELS; and Alanna Franchetti, ELS of Medergy (Yardley, PA), and funded by RB.
Conflicts of Interest: None to report.
References
- 1.Fernstrom A., Goldblatt M. Aerobiology and its role in the transmission of infectious diseases. J Pathog. 2013;2013:493960. doi: 10.1155/2013/493960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kowalski W. CRC Press; Boca Raton (FL): 2012. Hospital airborne infection control. [Google Scholar]
- 3.Traistaru E., Moldovan R., Menelaou A., Kakourou P., Georgescu C. A comparative study on the quality of air in offices and homes. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2013;48:1806–1814. doi: 10.1080/10934529.2013.823335. [DOI] [PubMed] [Google Scholar]
- 4.Mandal J., Brandl H. Bioaerosols in indoor environment–a review with special reference to residential and occupational locations. Open Environ Biol Monit J. 2011;4:83–96. [Google Scholar]
- 5.Mandin C., Derbez M., Kitchner S. Schools, office buildings, leisure settings: diversity of indoor air quality issues. Global review of indoor air quality in these settings. Ann Pharm Fr. 2012;70:204–212. doi: 10.1016/j.pharma.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Nenonen N.P., Hannoun C., Svensson L., Toren K., Andersson L.M., Westin J. Norovirus GII.4 detection in environmental samples from patient rooms during nosocomial outbreaks. J Clin Microbiol. 2014;52:2352–2358. doi: 10.1128/JCM.00266-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Best E.L., Fawley W.N., Parnell P., Wilcox M.H. The potential for airborne dispersal of Clostridium difficile from symptomatic patients. Clin Infect Dis. 2010;50:1450–1457. doi: 10.1086/652648. [DOI] [PubMed] [Google Scholar]
- 8.Gralton J., Tovey E., McLaws M.L., Rawlinson W.D. The role of particle size in pathogen transmission: a review. J Infect. 2011;62:1–13. doi: 10.1016/j.jinf.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muzlay M., Moore G., Turton J.F., Wilson A.P. Dissemination of antibiotic-resistant enterococci within the ward environment: the role of airborne bacteria and the risk posed by unrecognized carriers. Am J Infect Control. 2013;41:57–60. doi: 10.1016/j.ajic.2012.01.031. [DOI] [PubMed] [Google Scholar]
- 10.Eames I., Tang J.W., Li Y., Wilson P. Airborne transmission of disease in hospitals. J R Soc Interface. 2009;6(Suppl 6):S697–702. doi: 10.1098/rsif.2009.0407.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sattar S.A., Tetro J., Springthorpe V.S. Impact of changing societal trends on the spread of infectious diseases in American and Canadian homes. Am J Infect Control. 1999;27:S4–21. doi: 10.1016/s0196-6553(99)70037-4. [DOI] [PubMed] [Google Scholar]
- 12.Yang W., Marr L.C. Dynamics of airborne influenza A viruses indoors and dependence on humidity. PLoS ONE. 2011;6:e21481. doi: 10.1371/journal.pone.0021481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sattar S.A., Ijaz M.K. Spread of viral infections by aerosols. Crit Rev Environ Control. 1987;17:89–131. [Google Scholar]
- 14.Weis C.P., Intrepido A.J., Miller A.K., Cowin P.G., Durno M.A., Gebhardt J.S. Secondary aerosolization of viable Bacillus anthracis spores in a contaminated US Senate Office. JAMA. 2002;288:2853–2858. doi: 10.1001/jama.288.22.2853. [DOI] [PubMed] [Google Scholar]
- 15.Goldmann D.A. Transmission of viral respiratory infections in the home. Pediatr Infect Dis J. 2000;19(Suppl):S97–102. doi: 10.1097/00006454-200010001-00002. [DOI] [PubMed] [Google Scholar]
- 16.Meadow J.F., Altrichter A.E., Bateman A.C., Stenson J., Brown G.Z., Green J.L. Humans differ in their personal microbial cloud. PeerJ. 2015;3:e1258. doi: 10.7717/peerj.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Y., Tang J., Noakes C.J., Hoddson M. Engineering control of respiratory infection and low-energy design of healthcare facilities. Sci Technol Built Environ. 2015;21:25–34. [Google Scholar]
- 18.Jones R.M., Brosseau L.M. Aerosol transmission of infectious disease. J Occup Environ Med. 2015;57:501–508. doi: 10.1097/JOM.0000000000000448. [DOI] [PubMed] [Google Scholar]
- 19.Wells W.F. On airborne infection. Study II. Droplets and droplet nuclei. Am J Hygeine. 1934;20:611–618. [Google Scholar]
- 20.Wells W.F. Harvard University Press; Cambridge (MA): 1955. Airborne contagion and air hygiene. [Google Scholar]
- 21.Xie X., Li Y., Chwang A.T., Ho P.L., Seto W.H. How far droplets can move in indoor environments–revisiting the Wells evaporation-falling curve. Indoor Air. 2007;17:211–225. doi: 10.1111/j.1600-0668.2007.00469.x. [DOI] [PubMed] [Google Scholar]
- 22.Cox C.S. Airborne bacteria and viruses. Sci Prog. 1989;73:469–499. [PubMed] [Google Scholar]
- 23.Prussin A.J., Marr L.C. Sources of airborne microorganisms in the built environment. Microbiome. 2015;3:78. doi: 10.1186/s40168-015-0144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verreault D., Duchaine C., Marcoux-Voiselle M., Turgeon N., Roy C.J. Design of an environmentally controlled rotating chamber for bioaerosol aging studies. Inhal Toxicol. 2014;26:554–558. doi: 10.3109/08958378.2014.928763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yates M., Nakatsu C., Miller R., Pillai S., editors. Manual of environmental microbiology. 4th ed. ASM Press; Washington (DC): 2015. p. 3.2.7-1-24. [Google Scholar]
- 26.Verreault D., Moineau S., Duchaine C. Methods for sampling of airborne viruses. Microbiol Mol Biol Rev. 2008;72:413–444. doi: 10.1128/MMBR.00002-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang J.W. The effect of environmental parameters on the survival of airborne infectious agents. J R Soc Interface. 2009;6(Suppl 6):S737–46. doi: 10.1098/rsif.2009.0227.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang W., Marr L.C. Mechanisms by which ambient humidity may affect viruses in aerosols. Appl Environ Microbiol. 2012;78:6781–6788. doi: 10.1128/AEM.01658-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haleem Khan A.A., Karuppayil S.M. Fungal pollution of indoor environments and its management. Saudi J Biol Sci. 2012;19:405–426. doi: 10.1016/j.sjbs.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Z., Reponen T., Grinshpun S.A., Gorny R.L., Willeke K. Effect of sampling time and air humidity on the bioefficiency of filter samplers for bioaerosol collection. J Aerosol Sci. 2001;32:661–674. [Google Scholar]
- 31.Roth Y., Chapnik J.S., Cole P. Feasibility of aerosol vaccination in humans. Ann Otol Rhinol Laryngol. 2003;112:264–270. doi: 10.1177/000348940311200313. [DOI] [PubMed] [Google Scholar]
- 32.Brown J.R., Tang J.W., Pankhurst L., Klein N., Gant V., Lai K.M. Influenza virus survival in aerosols and estimates of viable virus loss resulting from aerosolization and air-sampling. J Hosp Infect. 2015;91:278–281. doi: 10.1016/j.jhin.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 33.Booth T.F., Kournikakis B., Bastien N., Ho J., Kobasa D., Stadnyk L. Detection of airborne severe acute respiratory syndrome (SARS) coronavirus and environmental contamination in SARS outbreak units. J Infect Dis. 2005;191:1472–1477. doi: 10.1086/429634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Srikanth P., Sudharsanam S., Steinberg R. Bio-aerosols in indoor environment: composition, health effects and analysis. Indian J Med Microbiol. 2008;26:302–312. doi: 10.4103/0255-0857.43555. [DOI] [PubMed] [Google Scholar]
- 35.Aranha-Creado H., Brandwein H. Application of bacteriophages as surrogates for mammalian viruses: a case for use in filter validation based on precedents and current practices in medical and environmental virology. http://www.pall.com/ps/PDFGenerator?URL=http://www.pall.com/main/oem-materials-and-devices/literature-library-details-print-pdf.page?id=3624 Available from. Accessed March 24, 2016. [PubMed]
- 36.Verani M., Bigazzi R., Carducci A. Viral contamination of aerosol and surfaces through toilet use in health care and other settings. Am J Infect Control. 2014;42:758–762. doi: 10.1016/j.ajic.2014.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.La R.G., Fratini M., Della L.S., Iaconelli M., Muscillo M. Viral infections acquired indoors through airborne, droplet or contact transmission. Ann Ist Super Sanita. 2013;49:124–132. doi: 10.4415/ANN_13_02_03. [DOI] [PubMed] [Google Scholar]
- 38.Sattar S.A., Ijaz M.K., Johnson-Lussenburg C.M., Springthorpe V.S. Effect of relative humidity on the airborne survival of rotavirus SA11. Appl Environ Microbiol. 1984;47:879–881. doi: 10.1128/aem.47.4.879-881.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ijaz M.K., Sattar S.A., Johnson-Lussenburg C.M., Springthorpe V.S. Comparison of the airborne survival of calf rotavirus and poliovirus type 1 (Sabin) aerosolized as a mixture. Appl Environ Microbiol. 1985;49:289–293. doi: 10.1128/aem.49.2.289-293.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ijaz M.K., Sattar S.A., Alkarmi T., Dar F.K., Bhatti A.R., Elhag K.M. Studies on the survival of aerosolized bovine rotavirus (UK) and a murine rotavirus. Comp Immunol Microbiol Infect Dis. 1994;17:91–98. doi: 10.1016/0147-9571(94)90034-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moe K., Harper G.J. The effect of relative humidity and temperature on the survival of bovine rotavirus in aerosol. Arch Virol. 1983;76:211–216. doi: 10.1007/BF01311105. [DOI] [PubMed] [Google Scholar]
- 42.Ijaz M.K., Brunner A.H., Sattar S.A., Nair R.C., Johnson-Lussenburg C.M. Survival characteristics of airborne human coronavirus 229E. J Gen Virol. 1985;66:2743–2748. doi: 10.1099/0022-1317-66-12-2743. [DOI] [PubMed] [Google Scholar]
- 43.Karim Y.G., Ijaz M.K., Sattar S.A., Johnson-Lussenburg C.M. Effect of relative humidity on the airborne survival of rhinovirus-14. Can J Microbiol. 1985;31:1058–1061. doi: 10.1139/m85-199. [DOI] [PubMed] [Google Scholar]
- 44.Mubareka S., Granados A., Naik U., Darwish I., Cutts T.A., Astrakianakis G. Influenza virus emitted by naturally-infected hosts in a healthcare setting. J Clin Virol. 2015;73:105–107. doi: 10.1016/j.jcv.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dick E.C., Jennings L.C., Mink K.A., Wartgow C.D., Inhorn S.L. Aerosol transmission of rhinovirus colds. J Infect Dis. 1987;156:442–448. doi: 10.1093/infdis/156.3.442. [DOI] [PubMed] [Google Scholar]
- 46.Gwaltney J.M. Rhinoviruses. In: Evans A.S., Kaslow R.A., editors. Viral Infections of humans: epidemiology and control. 4th ed. Plenum Medical; New York (NY): 1997. pp. 815–838. [Google Scholar]
- 47.Myatt T.A., Johnston S.L., Rudnick S., Milton D.K. Airborne rhinovirus detection and effect of ultraviolet irradiation on detection by a semi-nested RT-PCR assay. BMC Public Health. 2003;3:5. doi: 10.1186/1471-2458-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Myatt T.A., Johnston S.L., Zuo Z., Wand W., Kebadze T., Rudnick S. Detection of airborne rhinovirus and its relation to outdoor air supply in office environments. Am J Respir Crit Care Med. 2004;169:1187–1190. doi: 10.1164/rccm.200306-760OC. [DOI] [PubMed] [Google Scholar]
- 49.Sun Y., Wang Z., Zhang Y., Sundell J. In China, students in crowded dormitories with a low ventilation rate have more common colds: evidence for airborne transmission. PLoS ONE. 2011;6:e27140. doi: 10.1371/journal.pone.0027140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kramer A., Schwebke I., Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect Dis. 2006;6:130. doi: 10.1186/1471-2334-6-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Somogyi R., Vesely A.E., Azami T., Preiss D., Fisher J., Correia J. Dispersal of respiratory droplets with open vs closed oxygen delivery masks: implications for the transmission of severe acute respiratory syndrome. Chest. 2004;125:1155–1157. doi: 10.1378/chest.125.3.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Johnson E., Jaax N., White J., Jarhling P. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int J Exp Pathol. 1995;76:227–236. [PMC free article] [PubMed] [Google Scholar]
- 53.Osterholm M.T., Moore K.A., Kelley N.S., Brosseau L.M., Wong G., Murphy F.A. Transmission of Ebola viruses: what we know and what we do not know. MBio. 2015;6:e00137. doi: 10.1128/mBio.00137-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dancer S.J. Importance of the environment in meticillin-resistant Staphylococcus aureus acquisition: the case for hospital cleaning. Lancet Infect Dis. 2008;8:101–113. doi: 10.1016/S1473-3099(07)70241-4. [DOI] [PubMed] [Google Scholar]
- 55.Shiomori T., Miyamoto H., Makishima K. Significance of airborne transmission of methicillin-resistant Staphylococcus aureus in an otolaryngology-head and neck surgery unit. Arch Otolaryngol Head Neck Surg. 2001;127:644–648. doi: 10.1001/archotol.127.6.644. [DOI] [PubMed] [Google Scholar]
- 56.Escombe A.R., Moore D.A., Gilman R.H., Navincopa M., Ticona E., Mitchell B. Upper-room ultraviolet light and negative air ionization to prevent tuberculosis transmission. PLoS Med. 2009;6:e43. doi: 10.1371/journal.pmed.1000043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Johnson M.M., Odell J.A. Nontuberculous mycobacterial pulmonary infections. J Thorac Dis. 2014;6:210–220. doi: 10.3978/j.issn.2072-1439.2013.12.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Falkinham J.O., III. Mycobacterial aerosols and respiratory disease. Emerg Infect Dis. 2003;9:763–767. doi: 10.3201/eid0907.02-0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Phillips M.S., von Reyn C.F. Nosocomial infections due to nontuberculous mycobacteria. Clin Infect Dis. 2001;33:1363–1374. doi: 10.1086/323126. [DOI] [PubMed] [Google Scholar]
- 60.Roig J., Rello J. Legionnaires' disease: a rational approach to therapy. J Antimicrob Chemother. 2003;51:1119–1129. doi: 10.1093/jac/dkg191. [DOI] [PubMed] [Google Scholar]
- 61.Best E.L., Sandoe J.A., Wilcox M.H. Potential for aerosolization of Clostridium difficile after flushing toilets: the role of toilet lids in reducing environmental contamination risk. J Hosp Infect. 2012;80:1–5. doi: 10.1016/j.jhin.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 62.Fennelly K.P., Davidow A.L., Miller S.L., Connell N., Ellner J.J. Airborne infection with Bacillus anthracis–from mills to mail. Emerg Infect Dis. 2004;10:996–1002. doi: 10.3201/eid1006.020738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Anaissie E.J., Stratton S.L., Dignani M.C., Lee C.K., Summerbell R.C., Rex J.H. Pathogenic molds (including Aspergillus species) in hospital water distribution systems: a 3-year prospective study and clinical implications for patients with hematologic malignancies. Blood. 2003;101:2542–2546. doi: 10.1182/blood-2002-02-0530. [DOI] [PubMed] [Google Scholar]
- 64.Nevalainen A., Taubel M., Hyvarinen A. Indoor fungi: companions and contaminants. Indoor Air. 2015;25:125–156. doi: 10.1111/ina.12182. [DOI] [PubMed] [Google Scholar]
- 65.Ayanbimpe G.M., Danjuma W.S., Okolo M.O. Relationship between fungal contamination of indoor air and health problems of some residents in Jos. http://www.intechopen.com/books/air-quality-monitoring-and-modeling/-relationship-between-fungal-contamination-of-indoor-air-and-health-problems-of-some-residents-in-jo Available from. Accessed February 18, 2016.
- 66.Mensah-Attipoe J., Saari S., Veijalainen A.M., Pasanen P., Keskinen J., Leskinen J.T. Release and characteristics of fungal fragments in various conditions. Sci Total Environ. 2016;547:234–243. doi: 10.1016/j.scitotenv.2015.12.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Afanou K.A., Straumfors A., Skogstad A., Skaar I., Hjeljord L., Skare O. Profile and morphology of fungal aerosols characterized by field emission scanning electron microscopy (FESEM) Aerosol Sci Technol. 2015;49:423–435. doi: 10.1080/02786826.2015.1040486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cabral J.P. Can we use indoor fungi as bioindicators of indoor air quality? Historical perspectives and open questions. Sci Total Environ. 2010;408:4285–4295. doi: 10.1016/j.scitotenv.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 69.Kuhn D.M., Ghannoum M.A. Indoor mold, toxigenic fungi, and Stachybotrys chartarum: infectious disease perspective. Clin Microbiol Rev. 2003;16:144–172. doi: 10.1128/CMR.16.1.144-172.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kowalski W.J., Bahnfleth W.P., Striebig B.A., Whittam T.S. Demonstration of a hermetic airborne ozone disinfection system: studies on E. coli. AIHA J (Fairfax, Va) 2003;64:222–227. doi: 10.1080/15428110308984811. [DOI] [PubMed] [Google Scholar]
- 71.Environmental Protection Agency Air sanitizers–efficacy data recommendations. 2013. http://www.noticeandcomment.com/-ocspp-810-2500-air-sanitizers-2013-03-12-epa-730-c-11-003-fn-24288.aspx Test Guideline No. #OCSPP 810.2500-Air Sanitizers-; -03-12 [EPA 730-C-11-003]; Available from. Accessed December 4, 2015.
- 72.Ijaz M.K., Karim Y.G., Sattar S.A., Johnson-Lussenburg C.M. Development of methods to study the survival of airborne viruses. J Virol Methods. 1987;18:87–106. doi: 10.1016/0166-0934(87)90114-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sattar S.A., Kibbee R.J., Zargar B., Wright K.E., Rubino J.R., Ijaz M.K. Decontamination of indoor air to reduce the risk of airborne infections: studies on survival and inactivation of airborne pathogens using an aerobiology chamber. Am J Infect Control. 2016 doi: 10.1016/j.ajic.2016.03.067. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 74.Spellberg B., Bonomo R.A. “Airborne assault”: a new dimension in Acinetobacter baumannii transmission*. Crit Care Med. 2013;41:2042–2044. doi: 10.1097/CCM.0b013e31829136c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hospodsky D., Yamamoto N., Nazaroff W.W., Miller D., Gorthala S., Peccia J. Characterizing airborne fungal and bacterial concentrations and emission rates in six occupied children's classrooms. Indoor Air. 2015;25:641–652. doi: 10.1111/ina.12172. [DOI] [PubMed] [Google Scholar]
- 76.Liu L., Wei J., Li Y., Ooi A. Evaporation and dispersion of respiratory droplets from coughing. Indoor Air. 2016 doi: 10.1111/ina.12297. [DOI] [PubMed] [Google Scholar]