Highlights
-
•
Performance of SPs knowledge improved significantly after mixed media education.
-
•
Performance of SPs attitude improved significantly after mixed media education.
-
•
Performance of SPs compliance improved significantly after mixed media education.
-
•
Hands cleaning rate was significantly improved after mixed media education.
-
•
The mixed media education intervention was efficient.
Key Words: Compliance, China, Health care-associated infections, Infection control, Clinical trial, Health hazards, Teaching hospital
Abstract
Background
Standard precautions (SPs) are considered fundamental protective measures to manage health care-associated infections and to reduce occupational health hazards. This study intended to assess the effectiveness of a mixed media education intervention to enhance nursing students' knowledge, attitude, and compliance with SPs.
Method
A randomized controlled trial with 84 nursing students was conducted in a teaching hospital in Hubei, China. The intervention group (n = 42) attended 3 biweekly mixed media education sessions, consisting of lectures, videos, role-play, and feedback with 15-20 minutes of individual online supervision and feedback sessions following each class. The control group learned the same material through self-directed readings. Pre- and posttest assessments of knowledge, attitudes, and compliance were assessed with the Knowledge with Standard Precautions Questionnaire, Attitude with Standard Precautions Scale, and the Compliance with Standard Precautions Scale, respectively. The Standard Bacterial Colony Index was used to assess handwashing effectiveness.
Results
At 6-week follow-up, performance on the Knowledge with Standard Precautions Questionnaire, Attitude with Standard Precautions Scale, and Compliance with Standard Precautions Scale were significantly improved in the intervention group compared with the control group (P < .01). The hand hygiene standard in the intervention group (38 passed) outperformed the control group (23 passed) (P < .01).
Conclusions
A mixed media education intervention is effective in improving knowledge, attitude, and compliance with SPs.
Health care-associated infections are serious public health issues because they contribute to patients' mortality and morbidity,1 increase patient hospital stays, and present a significant health hazard for health care workers and patient family members.2 Infection rates in low- and middle-income countries may exceed 25%3 and place a significant economic burden on an already taxed health care system.4, 5 Standard precautions (SPs) are considered fundamental protective measures to manage health care-associated infections and to reduce occupational health hazards.6 SPs are motivated by the principal that all patients are potentially infectious, and therefore precautions should be used to manage risk. SPs guidelines suggest hand hygiene procedures; the use of protective barriers, such as gloves, masks, and goggles; appropriate handling and disposal of sharps and other contaminated or infectious waste; and use of aseptic techniques.6 Studies suggest that use of SPs in low- and middle-income countries is low.7
Nurses' adherence with SPs has an effect on reducing health care-associated infections, cross-infections between nurses and patients, and among patients, which in turn maximizes efficiency of health care resources.8, 9 Nurses are frontline health care workers and therefore have the most direct contact with patients.10
Globally, the level of SPs compliance, knowledge, and attitudes among health care workers is low.11, 12, 13 Previous research indicated that the compliance rates of SPs among nurses ranged from 9.1%-73%,14, 15 indicating a pressing need for improvement. The compliance rate was 69.4% among 560 nurses in Brazil and 57.4% among 260 nurses in Hong Kong.16 Inadequate adherence to SPs includes failure to follow hand hygiene guidelines, failure to use barrier devices during exposures to body fluids, and performing needle recapping.6
Lack of knowledge of SPs is directly related to nurses' noncompliance.17 Ideally, SPs training should be completed early in nurses' training as part of a formal education curriculum. The majority of nursing students do not receive comprehensive SPs and occupational exposure education in China. One survey of 1,444 nursing students indicated that 722 students (50%) did not receive any SPs education.12 A survey of 246 nursing students reported 1,144 needlestick injuries during internship, which revealed universal exposure in this study to bloodborne pathogens and possible infection.18 Educational programs are needed to improve SPs compliance, knowledge, and attitudes among nursing professionals. Studies also suggest that compliance of nursing students with SPs significantly improves after education interventions.19, 20 However, few SPs education intervention studies with nursing students are conducted in mainland China. The current study assessed the effectiveness of a mixed media education intervention for nursing students to enhance their knowledge, attitude, and compliance with SPs.
We made the following hypotheses: Compared with controls, nurses who complete the intervention will:
-
1.
Have a higher level of knowledge on SPs,
-
2.
Report a more positive attitude to SPs,
-
3.
Report greater compliance with SPs, and
-
4.
Have a higher hand hygiene passing rate.
Methods
This study received approval from the ethics committee of the nursing school and the target hospital. The research process and objectives were explained to the participants. Written informed consent was obtained from all study participants. Permission was obtained from the authors of all questionnaires and scales used in this study.
Study design
A 2-arm randomized controlled trial with pretest and posttest assessment was used. The study was conducted between May 2013 and June 2014. A random number table was used to assign participants to intervention and control groups. The intervention group received 3 biweekly mixed media education sessions, which consisted of lectures, videos, role-playing, and feedback. Participants also received 15-20 minutes of individual online supervision and feedback sessions from researchers on their practice following each class. The control group learned about SPs through self-study. The study materials were sent via e-mail by researchers to members of the control group twice—after the intervention group's first session and after the second session. They also had regular access to their clinical teachers for SPs instruction and general clinical guidance. For pretest, nursing students were invited to complete the demographic questionnaire and scales. Hand hygiene swab cultures were obtained after handwashing before nursing procedures during their work time. For posttest, after the intervention nursing students were invited to complete the scales during the break time of their clinical practice. Hand hygiene swab culture procedures were repeated for the posttest.
Sample and setting
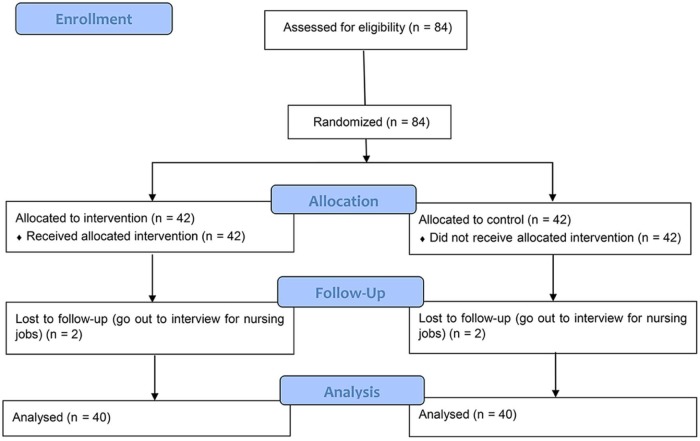
Internship for nursing students in China usually lasts from the final summer of training to the following spring (at least 8 months). It is the final year of nursing education, which involves rotations through different clinical departments in the general hospital.21 Eighty-four nursing students from 1 nursing school were recruited from the inpatient units at a large teaching hospital in Hubei, China. The teaching hospital we chose is affiliated with among the best universities in China. It is a Grade-III Class-A facility (the largest and most comprehensive research and teaching hospitals according to the Chinese Hospital Ranking System) with a 3,300-bed hospital. Eligible participants were nursing students at the beginning of clinical training. Half of the sample (n = 42) was randomly assigned to the intervention group and another half to the control group. Previous studies of the effectiveness of mixed education programs for nursing students used a target effect size of 0.35.22, 23 G*Power 3 (http://www.gpower.hhu.de/en.html) was used to calculate the sample size.24 At a statistical power of 0.80, a sample size of 70 was necessary to assess pre–post mean group differences with effect size of 0.35 and a significance level of 0.05.25 Considering a 20% dropout rate,26 a total of 84 participants was needed, with 42 in each group. Two participants from each group were lost to follow-up during the study due to interviewing for nursing jobs.
Intervention
The intervention was carried out during 3 biweekly sessions (Fig 1 ). During the first session (2 hours), the researcher (PX) gave lectures to review the principles of SPs; basic principles of infection control, including recognized interventions to break the chain of transmission of infectious agents; the biology of the hepatitis viruses and HIV; routes of transmission of bloodborne pathogens; occupational risks; and potentially risky personal behaviors. During the second session (2 hours), the researcher (PX) showed videos to demonstrate correct SPs procedures, such as how to properly wash hands, wear sterile gloves, and wear isolation gowns and personal protective equipment. The third session (2 hours) consisted of small group (6-7 participants per group) discussions focusing on the principles of SPs and their application in clinical practice. Role-playing exercises were facilitated during this session. The nursing students played the roles of teachers and students in small groups to assess and demonstrate correct SPs procedures with each other. The SPs procedures script, which included handwashing, wearing sterile gloves, wearing isolation gowns, and wearing personal protective equipment, was prepared by researchers and hospital infection management office staff members. The nursing students in the intervention group attended these 3 sessions at the same time.
Figure 1.
Flowchart.
The researchers also set up an online learning group for the intervention group using Tencent QQ (a popular communication platform in China; Tencent Inc., Shenzhen, China). Lecture slides, videos, and documents from the Ministry of Health in China and World Health Organization Guidelines on SPs and hand hygiene were uploaded. Tencent QQ also served as a discussion platform to facilitate learning. The researcher answered questions from the nursing students on this online platform. For each participant, a 15-20 minute one-on-one telephone call was made to review the session material and collect feedback following each session of the intervention. The following question was asked by the researcher of each nursing student: “How do you feel about implementing SPs during these 2 weeks?” “Did you review the materials I uploaded?” “Do you have difficulties understanding these procedures?” “Did you perform your nursing procedures using standard precautions?” and, “Do you think it's useful for you? If so, please continue. If not, could you share your thoughts with me?”
Measures
Knowledge with Standard Precautions Questionnaire
Knowledge was defined as understanding the definition and application of SPs, safety procedures, and precautions when using sharp objects. There are 42 items on the Knowledge with Standard Precautions Questionnaire (KSPQ).27 Responses are “yes,” “no,” or “not sure.” A score of 1 is given for each correct answer. Total score ranged from 0-42. Content validity was rated by an expert panel to be good (content validity index [CVI] = 0.92).28 Two-week test–retest reliability was excellent (Cronbach's α = 0.94) in the original scale development study.27 Alpha in the current study was 0.76.
Attitude with Standard Precautions scale
Attitude was defined as how participants react to implementing SPs procedures according to the infection control principles at a suitable time.29 The Attitude with Standard Precautions (ASPS) scale was developed in Chinese to measure nursing students' attitudes on 5 dimensions of SPs.27 A total of 34 items assessed the following dimensions: Risk Perception, Efficacy of SPs, Barriers to Implementing SPs, Favorable Conditions for Action, and Assessment of Self-Efficacy. All items were scored on a 5-point Likert scale from 1 = “strongly disagree” to 5 = “strongly agree.” Total score ranged from 34-170. Content validity was rated by an expert panel to be good (CVI = 0.89)28 and 2-week test–retest reliability was good (Cronbach's α = 0.88) in the original study.27 Alpha in the present study was 0.84.
Compliance with Standard Precautions Scale
Compliance in health care settings was defined as following the prescription guidance, instructions, and advice from physicians.30 The Compliance with Standard Precautions (CSPS) scale was an English-version scale developed to measure nurse compliance with infection control practices outlined by the Centers for Disease Control and Prevention.31 In total there are 20 items on a Likert-type scale ranging from 1 = “never” to 4 = “always” and the total score ranged from 20-80. It was validated among nursing students.32 Internal validity index was 0.90, and Cronbach's α was 0.73. The scale author granted permission for translation and validation. The Chinese validation process of the CSPS was that the original English scale was translated into Chinese by 2 bilingual translators. The Chinese translation was reviewed and revised by a study author (XW) and the translators and another 2 bilingual translators back-translated the revised Chinese translation into English. The back-translated English scale was then reviewed and finalized by another study author (JZ) and the translators. Finally, the author of the CSPS was invited to assess the quality of the Chinese translation by looking at the back-translated scale and the original. A pilot study was done with 30 nursing students (participation rate and recovery rate were both 100%). Cronbach's α was 0.88 and CVI was 0.95 by a panel of 5 nursing experts, indicating good reliability and validity of the scale.33
Bacterial colony measurement
The Bacterial Colony Index34 is an indication of the effectiveness of handwashing. According to the Chinese Center for Disease Control and Prevention, qualified total aerobic bacterial counts should be lower than 10 CFU/cm2 in general units and lower than 5 CFU/cm2 in operating rooms.34 The following steps were employed to measure hand hygiene:34 the researchers asked participants to wash their hands using their usual handwashing habit before nursing procedures; as soon as their hands were dry, with palms facing up, the researchers used 1 sterile cotton swab to sample 5 fingers of both hands from top to bottom; the cotton swabs were put into sterile tubes within 2 hours of collection; the swab cultures were sent to a microbiology lab to test for bacteria growth; and results were available after 48 hours.
Participant characteristics
Age, gender, education level, history of SPs education, motivation to be trained, history of hepatitis B vaccine, history of needle puncture exposure during clinical rotation, and willingness to report needlestick incidents.
Data analysis
STATA 14.0 (StataCorp, College Station, TX) was used in the analysis. Descriptive statistics, including frequency, mean, and standard deviation were used to summarize demographic data and study outcome measures. Repeated measures mixed model approach was performed to evaluate the intervention efficacy of the KSPQ, ASPS, and CSPS. The χ2 test and Fisher exact test were used to evaluate the passing rate of hand hygiene after the intervention. The statistically significant level was set as P < .05 with 2-tailed tests.
Results
Participant characteristics
Average age of participants was 20.31 ± 0.78 years, and 82 nursing students had an associate's degree or beyond. Ninety-two percent were full-time nursing students. Only 23.81% of nursing students received related infection control information. A strong desire to receive training was reported by 54.76%. Among nursing students, 33.33% did not have the hepatitis B vaccine before participating in this study and only 12 students stated that their hepatitis B antibody was positive. Nearly half (47.62%) were exposed to needle puncture during their clinical rotation. The majority of those exposed (85.71%) indicated that they were willing to report a needle puncture incident if it occurred. Characteristics are presented in Table 1 .
Table 1.
Participants' characteristics
| Items | Participants (n = 84) (%) |
Control group (n = 42) (%) |
Intervention group (n = 42) (%) |
|---|---|---|---|
| Age (y) | 20.31 ± 0.78 | 20.24 ± 0.85 | 20.38 ± 0.70 |
| Gender | |||
| Female | 84(100) | 42(100) | 42(100) |
| Education level | |||
| Bachelor | 1(1.19) | 1(2.8) | |
| Associate | 81(96.40) | 42(100) | 39(92.86) |
| Diploma | 2(2.38) | 2(4.76) | |
| Education type | |||
| Full-time | 77(91.67) | 39(92.86) | 38(90.48) |
| Part-time | 7(8.33) | 3(7.14) | 4(9.52) |
| Ever received related infection control courses | |||
| Yes | 20(23.81) | 12(28.57) | 8(19.05) |
| No | 64(76.19) | 30(71.43) | 34(80.95) |
| Motivation to be trained | |||
| Very | 46(54.76) | 23(54.76) | 23(54.76) |
| General | 34(40.48) | 17(40.48) | 17(40.48) |
| No | 1(1.19) | 1(2.38) | |
| Don't care | 3(3.57) | 1(2.38) | 2(4.76) |
| Ever received hepatitis B vaccine | |||
| Yes | 56(66.67) | 29(69.05) | 27(64.29) |
| No | 28(33.33) | 13(30.95) | 15(35.71) |
| Hepatitis B antibody | |||
| Positive | 12(14.29) | 5(11.90) | 7(16.67) |
| Negative | 21(25.00) | 12(28.57) | 9(21.43) |
| Don't know | 51(60.71) | 25(59.52) | 26(61.90) |
| Needlestick exposure | |||
| Yes | 40(47.62) | 23(54.76) | 17(40.48) |
| No | 44(52.38) | 19(45.24) | 25(59.52) |
| Willingness to report the needstick incident | |||
| Yes | 72(85.71) | 37(88.10) | 35(83.33) |
| No | 12(14.29) | 5(11.90) | 7(16.67) |
NOTE. Values are presented as mean ± standard deviation or n(%). Bachelor's degree is 4-year nursing program after senior high school education, associate's degree is 3-year nursing program after senior high school education, and diploma is 3-year nursing program after junior high school education. “Motivation to be trained” was assessed by asking question, “Do you have willingness to get standard precautions training?”
Baseline assessment
Average baseline score in the control group for knowledge was 34.57 ± 3.78 on the KSPQ (range, 0-42), attitude was 128.36 ± 7.19 on the ASPS (range, 34-170), and compliance was 61.64 ± 5.93 on the CSPS (range, 20-80). Average baseline score for the intervention group for knowledge was 34.50 ± 4.62 on the KSPQ, attitude was 128.81 ± 7.34 on the ASPS, and compliance was 62.67 ± 5.88 on the CSPS. Only 31 (36.9%) out of 84 nursing students passed the hand hygiene standard. Results are presented in Table 2, Table 3 .
Table 2.
Intervention data (knowledge, attitude, and compliance with standard precautions)
| Items | Control group | Intervention group | P value overall† | P1 | P2 | P3 | ||
|---|---|---|---|---|---|---|---|---|
| Pretest (n = 42) |
Posttest (n = 40) |
Pretest (n = 42) |
Posttest (n = 40) |
|||||
| Knowledge with Standard Precautions Questionnaire‡ | 34.57 ± 3.78 | 35.98 ± 3.87 | 34.50 ± 4.62 | 41.28 ± 0.93 | .000** | .051 | .000** | .000** |
| Attitude with Standard Precautions Scale§ | 128.36 ± 7.19 | 129.83 ± 8.64 | 128.81 ± 7.34 | 136.65 ± 6.47 | .000** | .372 | .000** | .000** |
| Dimension 1 | 20.00 ± 2.07 | 20.80 ± 2.21 | 20.64 ± 1.92 | 21.95 ± 1.91 | .000** | .075 | .004 | .011* |
| Dimension 2 | 32.40 ± 3.25 | 33.23 ± 3.29 | 32.29 ± 3.32 | 36.98 ± 1.56 | .000** | .209 | .000** | .000** |
| Dimension 3 | 23.90 ± 4.30 | 23.20 ± 5.17 | 23.62 ± 5.04 | 22.83 ± 3.92 | .720 | .470 | .422 | .727 |
| Dimension 4 | 32.38 ± 3.15 | 32.98 ± 3.32 | 32.24 ± 3.43 | 34.40 ± 2.73 | .006** | .393 | .001** | .045* |
| Dimension 5 | 19.67 ± 2.01 | 19.63 ± 2.79 | 20.02 ± 2.04 | 20.50 ± 1.89 | .252 | .932 | .329 | .076 |
| Compliance with Standard Precautions Scale|| | 61.64 ± 5.93 | 62.63 ± 6.52 | 62.67 ± 5.88 | 72.55 ± 3.46 | .000** | .445 | .000** | .000** |
NOTE. Values are presented as mean ± standard deviation.
P overall is the effect of repeated measures mixed model; P1, P2, and P3 is the effect of intervention at each time and in each group with contrast command. P1 compares the pre- and posttest in the control group, P2 compares the pre- and posttest in the intervention group, and P3 compares the posttest between control group and intervention group.
Score ranges from 0 to 42.
Score ranges from 34 to 170. ASPS has the 5 dimensions. Dimension 1 is “risk perception,” 5 items, score ranges from 5 to 25; dimension 2 is “efficacy of SPs,” 8 items, score ranges from 8 to 40; dimension 3 is “barriers to implementing SPs,” 8 items, score ranges from 8 to 40; dimension 4 is “favorable conditions for action,” 8 items, score ranges from 8 to 40; and dimension 5 is “assessment of self-efficacy,” 5 items, score ranges from 5 to 25.
Score range from 20 to 80.
P < .05.
P < .01.
Table 3.
Intervention data (hand hygiene)
| Item | Control group | Intervention group | P1† | P2† | P3† | ||
|---|---|---|---|---|---|---|---|
| Pretest (n = 42) |
Posttest (n = 40 |
Pretest (n = 42) |
Posttest (n = 40) |
||||
| Passed | 13(31.0) | 23(57.5) | 18(42.9) | 38(95.0) | .015* | .000** | .000** |
| Failed | 29(69.0) | 17(42.5) | 24(57.1) | 2(5.0) | |||
NOTE. Values are presented as n (%).
P1 compares the pre- and posttest in control group, P2 compares the pre- and posttest in intervention group, and P3 compares the posttest between control group and intervention group.
P < .05.
P < .01.
The 3 items of the KSPQ with lowest scores were: “Do you know what SPs are?” for which 9.52% answered correctly; “We only need to take SPs when we take care of hepatitis C or syphilis patients,” for which 46.43% answered correctly; and, “We should wear gloves when we are drawing blood and doing venipuncture,” for which 47.62% answered correctly.
The 3 items of the ASPS with lowest scores were in the dimension Barriers to Implementing SPs. The specific items were, “Some blood and body fluids are unpredictable,” for which the mean score was 1.88 ± 0.73; “I could not always follow SPs because the patients' needs came first,” for which the mean score was 2.55 ± 0.99; and, “I had not enough time to follow SPs because I was busy,” for which the mean score was 2.81 ± 0.89.
The 3 items of the CSPS with lowest scores were: “The sharps box is disposed only when it is full,” for which the mean score was 1.90 ± 1.01; “I wear a gown or apron when exposed to blood, body fluids, or any patient excretions,” for which the mean score was 2.42 ± 1.07; and, “I recap used needles after giving an injection,” for which the mean score was 2.45 ± 1.03.
Intervention result
Pre- and post intervention within-group comparisons were analyzed (see Table 2, Table 3). Nursing students in the intervention group reported significantly increased scores on knowledge (KSPQ, from 34.50 ± 4.62 to 41.28 ± 0.93; P < .01), attitudes (ASPS, from 128.81 ± 7.34 to 136.65 ± 6.47; P < .01), and compliance (CSPS, from 62.67 ± 5.88 to 72.55 ± 3.46; P < .01), whereas no significant change was found in the control group. For hand hygiene, both the intervention group (42.9%-95%) and the control group (31.0%-57.5%) performed better at week 6 than the pre intervention level (P < .01 and P < .05, respectively).
Posttest comparison between groups was also conducted. At the end of the third session (week 6), the intervention group had significantly higher scores than did the control group on knowledge (KSPQ, 41.28 ± 0.93 vs 35.98 ± 3.87; P < .01), attitudes (ASPS, 136.65 ± 6.47 vs 129.83 ± 8.64; P < .01), and compliance (CSPS, 72.55 ± 3.46 vs 62.63 ± 6.52; P < .01). For hand hygiene, the passing rate in the intervention group (95.0%) was significantly higher than that of the control group (57.5%; P < .01).
Discussion
The present study demonstrated the significant effect of a mixed media intervention for nursing students at the beginning of clinical training. Compliance with the intervention was high. Our study also indicated that nursing students demonstrated low levels of knowledge and application of SPs, which further highlights the need to implement interventions to improve SPs uptake.
Infectious disease rates in China may in part be driven by poor infection control in hospitals, presenting a critical public health challenge. For example, 7.2% of the population younger than age 59 years are hepatitis B positive,35 the estimated rate of hepatitis C virus range from 1.0%-2.9% in China.36, 37 In this study, approximately one-third of nursing students did not receive hepatitis B vaccines and only one-sixth knew their hepatitis B antibody status. It was well known that injuries from sharp objects could cause transmission of hepatitis B and C, HIV, syphilis, brucellosis, malaria, and other infectious diseases.38 This knowledge among our study participants did not prevent their direct exposure. A needlestick incident during clinical practice was reported by 47.62% of the students, compared with another study documenting 1,144 needlestick injuries among 246 Chinese nursing students during internship.18 Mixed media education interventions may help to improve this situation.
The baseline surveys showed that most nursing students in this study did not receive any formal SPs training, despite being taught about infection control. They do not know the SPs or how to put them into practice. The main factor identified that influenced adherence to SPs were lack of SPs training in China.12 In China, there is a lack of a compulsory curriculum on SPs and infection control courses in nursing schools at associate, bachelor's, and master's degree levels. The infection control-related chapters in fundamental nursing and surgical nursing textbooks are very limited and not fully taught,39, 40 and there are no specific courses on SPs or infection control. More than 85% of nursing students receive infection control knowledge from their clinical teachers.41 The usual practice is to follow the school curriculum, which does not explicitly teach about SPs. One survey in 2010 demonstrated that half of 1,444 nursing students did not receive any SPs education at all at school.12 Most nursing students receive partial SPs knowledge when they start their clinical practice, either taught by their clinical instruction teachers or learned from other sources.
Baseline attitudes about SPs were not high and this was consistent with previous studies among clinical nurses, surgeons, and physicians.17, 42 This may be in part due to the lack of knowledge of SPs. Low scores were observed for items that measured barriers to implementing SPs. The reason for this may be that the baseline assessment occurred at the beginning of students' clinical rotations. They may not have had enough clinical experience and a lack of exposure to observe and learn in the isolation, infectious diseases, or surgical departments. Therefore, they did not recognize the importance of SPs. On the other hand, nursing students may not be able to obtain a patients' complete medical history, including the history of HIV, hepatitis B virus, or other infectious diseases. In previous studies nursing students did not pay enough attention to SPs due in part to the fact that some patients and their family members did not review or did not know their infectious status.43 Compliance with SPs should be practiced at all times during clinical practice.
The mixed media education intervention implemented at the beginning of clinical training was effective in improving knowledge, attitude, and compliance with SPs as well as hand hygiene among nursing students. After the mixed media education intervention, nursing students in the intervention group reported greater knowledge of SPs than did those in the control group, including the principles of SPs and infection control, occupational risks, and potentially risky personal behaviors. Nursing students in the intervention group also improved their positive attitude about SPs more than did those in the control group. In particular, their attitude about the “efficacy of SPs” and “favorable conditions for action” improved. Finally, nursing students in the intervention group improved their compliance with SPs more than did those in the control group. For example, washing hands, wearing gloves, donning personal protective equipment at the proper time, and putting used sharp articles into sharps boxes all improved. For hand hygiene, the control group's increase in passing rate may have been due to gaining knowledge and practice tips from their clinical teachers. However, the intervention group still outperformed the control group on hand hygiene.
Limitations
To our knowledge, this is the first intervention study where a mixed media approach with an objective outcome measure of behavior change was used to deliver SPs training in mainland China. The study used validated and reliable measures appropriate to the Chinese context, and used an objective outcome measure of behavior change.31, 32 There were several limitations. First, the sample size was small. Although this is appropriate for a pilot test of a new intervention, future studies should include a larger sample size. Relatedly, the study was conducted in 1 hospital. A multicenter study would be ideal to confirm that the comprehensive nursing intervention model is effective and scalable. Finally, the present study is limited by its pre–post design. Future studies are needed with longer-term follow-up periods to know the durability of improvements in knowledge, attitude, and compliance with SPs.
Conclusions
Mixed media education intervention can improve nursing students' level of knowledge, attitude, and compliance with SPs. Increased use of SPs is of vital importance to protect the health of nurses, patients, and other health care professionals from health care-associated infections. Improvement of SPs deficiencies is desperately needed because emergent cases of H7N9, Ebola virus disease, Middle East respiratory syndrome, and Zika virus will expose Chinese nurses to infectious disease. There is an urgent need from policy makers, nursing school teachers, and hospital trainers to reduce SPs deficiencies among nursing students. For teaching hospitals, forming a team of professional staff to serve as trainers to implement SPs is vital. Applying SPs education throughout clinical rotations allows students to strengthen their awareness and practice of SPs.
Acknowledgments
The authors thank the authors of the KSPQ and ASPS instruments (Y. J. Li, and X. L. Zhao) and the author of the CSPS (S. C. Lam) for authorizing us to use their scales. The authors also thank P. Liu, D. Luo, Y. Q. Liu, and M. Yu for contributing to translating the CSPS; X. P. Zhu and H. B. Mao for collaborating with this research; Q. L. Guo and her colleagues for culturing and analyzing the swab samples; S. H. Song, Y. B. Tan, X. L. Jin, and Y. Li for guiding and training the students on essential standard precautions-related materials; and the nursing students for participating and collaborating with this research.
Footnotes
Supported by the Research and Development Affairs Office, University of Macau, People's Republic of China, under grant No. MYRG2015-00109-FSS.
Conflicts of interest: None to report.
References
- 1.Jarvis W.R. Selected aspects of the socioeconomic impact of nosocomial infections: morbidity, mortality, cost, and prevention. Infect Control Hosp Epidemiol. 1996;17:552–557. doi: 10.1086/647371. [DOI] [PubMed] [Google Scholar]
- 2.Plowman R., Graves N., Griffin M.A., Roberts J.A., Swan A.V., Cookson B. The rate and cost of hospital-acquired infections occurring in patients admitted to selected specialties of a district general hospital in England and the national burden imposed. J Hosp Infect. 2001;47:198–209. doi: 10.1053/jhin.2000.0881. [DOI] [PubMed] [Google Scholar]
- 3.Pittet D., Allegranzi B., Storr J., Donaldson L. “Clean care is safer care”: the global patient safety challenge 2005-2006. Int J Infect Dis. 2006;10:419–424. doi: 10.1016/j.ijid.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Fry D.E. The economic costs of surgical site infection. Surg Infect (Larchmt) 2002;3(Suppl 1):s37–43. doi: 10.1089/sur.2002.3.s1-37. [DOI] [PubMed] [Google Scholar]
- 5.Report on the burden of endemic health care-associated infection worldwide. 2011. http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf Available from.
- 6.Siegel J.D., Rhinehart E., Jackson M., Chiarello L. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35:s65–164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vindigni S.M., Riley P.L., Jhung M. Systematic review: handwashing behaviour in low- to middle-income countries: outcome measures and behaviour maintenance. Trop Med Int Health. 2011;16:466–477. doi: 10.1111/j.1365-3156.2010.02720.x. [DOI] [PubMed] [Google Scholar]
- 8.Kim K.M., Kim M.A., Chung Y.S., Kim N.C. Knowledge and performance of the universal precautions by nursing and medical students in Korea. Am J Infect Control. 2001;29:295–300. doi: 10.1067/mic.2001.114837. [DOI] [PubMed] [Google Scholar]
- 9.Pratt R.J., Pellowe C.M., Wilson J.A., Loveday H.P., Harper P.J., Jones S.R. epic2: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2007;65(Suppl 1):S1–64. doi: 10.1016/S0195-6701(07)60002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cole M. Exploring the hand hygiene competence of student nurses: a case of flawed self assessment. Nurse Educ Today. 2009;29:380–388. doi: 10.1016/j.nedt.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 11.Kermode M., Jolley D., Langkham B., Thomas M.S., Holmes W., Gifford S.M. Compliance with Universal/Standard Precautions among health care workers in rural north India. Am J Infect Control. 2005;33:27–33. doi: 10.1016/j.ajic.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Luo Y., He G.P., Zhou J.W., Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis. 2010;14:e1106–14. doi: 10.1016/j.ijid.2009.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pan A., Domenighini F., Signorini L., Assini R., Catenazzi P., Lorenzotti S. Adherence to hand hygiene in an Italian long-term care facility. Am J Infect Control. 2008;36:495–497. doi: 10.1016/j.ajic.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 14.Efstathiou G., Papastavrou E., Raftopoulos V., Merkouris A. Compliance of Cypriot nurses with standard precautions to avoid exposure to pathogens. Nurs Health Sci. 2011;13:53–59. doi: 10.1111/j.1442-2018.2011.00576.x. [DOI] [PubMed] [Google Scholar]
- 15.Gammon J., Morgan-Samuel H., Gould D. A review of the evidence for suboptimal compliance of healthcare practitioners to standard/universal infection control precautions. J Clin Nurs. 2008;17:157–167. doi: 10.1111/j.1365-2702.2006.01852.x. [DOI] [PubMed] [Google Scholar]
- 16.Pereira F.M., Lam S.C., Chan J.H., Malaguti-Toffano S.E., Gir E. Difference in compliance with Standard Precautions by nursing staff in Brazil versus Hong Kong. Am J Infect Control. 2015;43:769–772. doi: 10.1016/j.ajic.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 17.Chan R., Molassiotis A., Chan E., Chan V., Ho B., Lai C.Y. Nurses' knowledge of and compliance with universal precautions in an acute care hospital. Int J Nurs Stud. 2002;39:157–163. doi: 10.1016/s0020-7489(01)00021-9. [DOI] [PubMed] [Google Scholar]
- 18.Yao W.X., Yang B., Yao C., Bai P.S., Qian Y.R., Huang C.H. Needlestick injuries among nursing students in China. Nurse Educ Today. 2010;30:435–437. doi: 10.1016/j.nedt.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 19.Al-Hussami M., Darawad M. Compliance of nursing students with infection prevention precautions: effectiveness of a teaching program. Am J Infect Control. 2013;41:332–336. doi: 10.1016/j.ajic.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 20.Holmen I.C., Seneza C., Nyiranzayisaba B., Nyiringabo V., Bienfait M., Safdar N. Improving hand hygiene practices in a rural hospital in sub-Saharan Africa. Infect Control Hosp Epidemiol. 2016;37:834–839. doi: 10.1017/ice.2016.71. [DOI] [PubMed] [Google Scholar]
- 21.Sun L., Gao Y., Yang J., Zang X.Y., Wang Y.G. The impact of professional identity on role stress in nursing students: a cross-sectional study. Int J Nurs Stud. 2016;63:1–8. doi: 10.1016/j.ijnurstu.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 22.Considine J., Botti M., Thomas S. Effect of a self-directed learning package on emergency nurses' knowledge of assessment of oxygenation and use of supplemental oxygen. Nurs Health Sci. 2005;7:199–208. doi: 10.1111/j.1442-2018.2005.00236.x. [DOI] [PubMed] [Google Scholar]
- 23.Considine J., Brennan D. Effect of an evidence-based paediatric fever education program on emergency nurses' knowledge. Accid Emerg Nurs. 2007;15:10–19. doi: 10.1016/j.aaen.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Faul F., Erdfelder E., Lang A.-G., Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 25.Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 26.Polit D.F., Beck C.T. 9th ed. Wolters Kluwer Health; 2012. Nursing research: generating and assessing evidence for nursing practice. [Google Scholar]
- 27.Zhao X.L., Li Y.J., Gao Y., Ma R.Y., Zhang L., Liao L. Study on influencing factors of nursing students: compliance of Standard Precaution. J Nurs. 2011;18:5–9. [Google Scholar]
- 28.Portney L.G., Watkins M.P. 3rd ed. Prentice Hall; London: 2009. Foundations of clinical research: application to practice. [Google Scholar]
- 29.Sax H., Perneger T., Hugonnet S., Herrault P., Chraiti M.N., Pittet D. Knowledge of standard and isolation precautions in a large teaching hospital. Infect Control Hosp Epidemiol. 2005;26:298–304. doi: 10.1086/502543. [DOI] [PubMed] [Google Scholar]
- 30.Haynes R.B., Taylor D.W., Sackett D.L. Baltimore John Hopkins University Press; 1979. Compliance in health care. [Google Scholar]
- 31.Lam S.C. Universal to standard precautions in disease prevention: preliminary development of compliance scale for clinical nursing. Int J Nurs Stud. 2011;48:1533–1539. doi: 10.1016/j.ijnurstu.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 32.Lam S.C. Validation and cross-cultural pilot testing of compliance with standard precautions scale: self-administered instrument for clinical nurses. Infect Control Hosp Epidemiol. 2014;35:547–555. doi: 10.1086/675835. [DOI] [PubMed] [Google Scholar]
- 33.Streiner D.L. Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess. 2003;80:99–103. doi: 10.1207/S15327752JPA8001_18. [DOI] [PubMed] [Google Scholar]
- 34.Ministry of Health of the People's Republic of China Standard of health workers' hand hygiene. Chin J Nosocomiol. 2009;19:I–II. [Google Scholar]
- 35.Liang X., Bi S., Yang W., Wang L., Cui G., Cui F. Epidemiological serosurvey of hepatitis B in China—declining HBV prevalence due to hepatitis B vaccination. Vaccine. 2009;27:6550–6557. doi: 10.1016/j.vaccine.2009.08.048. [DOI] [PubMed] [Google Scholar]
- 36.Sievert W., Altraif I., Razavi H.A., Abdo A., Ahmed E.A., Alomair A. A systematic review of hepatitis C virus epidemiology in Asia, Australia and Egypt. Liver Int. 2011;31(Suppl 2):61–80. doi: 10.1111/j.1478-3231.2011.02540.x. [DOI] [PubMed] [Google Scholar]
- 37.Cui Y., Jia J. Update on epidemiology of hepatitis B and C in China. J Gastroenterol Hepatol. 2013;28(Suppl 1):7–10. doi: 10.1111/jgh.12220. [DOI] [PubMed] [Google Scholar]
- 38.Himmelreich H., Rabenau H.F., Rindermann M., Stephan C., Bickel M., Marzi I. The management of needlestick injuries. Dtsch Arztebl Int. 2013;110:61–67. doi: 10.3238/arztebl.2013.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen L.H. Investigation of occupation education present situation in nursing schools. Pract Prev Med. 2004;11:406–408. [Google Scholar]
- 40.Mao X.Y., Jin D.Y., Yu L.M., Zhang H.M., Gai X.R., Xu H. Sharp injuries among nursing students in medical practices. Chin J Nosocomiol. 2003;13:110–112. [Google Scholar]
- 41.Meng F.F., Zhang X.Y., Tian S.J., Luo S.Y., Yin C., Wang Y.L. Investigation on status in quo of occupational health and safety of nursing students during the clinical internship and the curricula setting about occupational health and safety. J Nurs Sci. 2008;23:59–61. [Google Scholar]
- 42.Askarian M., McLaws M.L., Meylan M. Knowledge, attitude, and practices related to standard precautions of surgeons and physicians in university-affiliated hospitals of Shiraz, Iran. Int J Infect Dis. 2007;11:213–219. doi: 10.1016/j.ijid.2006.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yu H.L., Tian L.H., Yang Z.T. The occupational injuries and protective countermeasures in new pediatric medical staffs. J Misdiagn. 2010;10:76. [Google Scholar]