Abstract
Background
To determine if hot, humid ambient conditions impact filtering facepiece respirators' (FFRs') fit, and to evaluate differences in physiologic and subjective responses between N95 FFRs and P100 FFRs.
Methods
Twelve subjects had physiologic monitoring and subjective perceptions monitored over 1 hour of treadmill exercise (5.6 km/h) in an environmental chamber (35°C, relative humidity 50%) wearing an N95 FFR, P100 FFR, or no respirator. Respirator quantitative fit testing was done before and after exercise.
Results
There was no significant difference in pass rates for both FFRs on initial fit testing, but subjects who passed were more likely to fail the postexercise test with N95 FFRs (P = .01). Wearing FFRs increased the temperature of facial skin covered by the FFR (P = .009) and breathing discomfort (P = .002). No significant differences were noted in other measured variables (heart rate, respiratory rate, oxygen saturation, transcutaneous carbon dioxide level, rectal temperature, global skin temperature, core temperature, and subjective perceptions) between controls and FFRs and between FFR models.
Conclusion
After 1 hour of exercise in hot, humid ambient conditions, P100 FFRs retained better fit than N95 FFRs, without additional physiologic or subjective impact. Wearing FFRs under these conditions does not add to the body's thermophysiologic or perceptual burdens.
Key Words: Filtering facepiece respirators, P100, N95, Hot humid environment, Fit factors, Thermophysiologic and subjective responses
Highlights
-
•
P100 filtering facepiece respirators (FFRs) retained their fit better than N95 FFRs in hot, humid environments.
-
•
At low to moderate work rates, P100 filtering facepiece respirators' (FFRs') physiologic impact was similar to N95 FFRs.
-
•
At low to moderate work rates, exhalation valves appeared to offer no benefit.
-
•
Filtering facepiece respirator (FFR) use in hot, humid environments did not add to body heat burden or perceptions.
Filtering facepiece respirators (FFRs) are worn to prevent the inhalation of toxic and infectious airborne particles. The National Institute for Occupational Safety and Health (NIOSH) certifies FFRs and classifies them according to 3 letter designations that refer to the respirator's oil resistance (N [not resistant], R [somewhat resistant], and P [strongly resistant]) and 3 numerical designations (95, 99, and 100) that indicate the percent filtration efficiency of the respiratory filter.1 Employers mandated by the U.S. Occupational Safety and Health Administration (OSHA) to provide respiratory protection in the form of FFRs are required to provide employee fit testing (qualitative or quantitative) annually to ensure that the FFR fits the user appropriately to provide the expected level of protection.2 In ambient conditions of high heat and humidity, there is concern that FFR moisture accumulation from the combined effects of ambient humidity, retained moisture from the exhaled breath, and facial sweat accumulation can result in a loosening of the seal of the FFR to the face (with resultant ingress of contaminants) and a potential increase in breathing resistance as a result of blockage of pores in the FFR filter that could increase the work of breathing.3, 4 In recent years, these concerns have been amplified in relation to highly publicized environmental events (eg, Gulf oil spill on the Louisiana coast) and infectious disease outbreaks (eg, Ebola, Middle East respiratory syndrome) associated with the use of respiratory protective equipment in hot and humid environments. This study was undertaken to evaluate the effect of a hot, humid environment on the fit of class N95 FFRs, the most widely used FFR in industry and health care, and on class P100 FFRs used for protection from toxic airborne particulates in an industrial environment where oil may be encountered. A secondary objective of the study was to determine any differences in physiologic and subjective responses between the N95 and P100 classes of respirators in the aforementioned ambient environment.
Materials and methods
Twelve healthy, nonsmoking men were recruited for the study. Subject mean demographics were as follows: age was 23.5 ± 1.6 years, height was 181 ± 6 cm, weight was 81.8 ± 8.1 kg, and body mass index was 24.9 ± 2.3 kg/m2. The study was approved by the NIOSH Institutional Review Board, and all subjects provided written and verbal consent. Prior to exercising, subjects were first instrumented with a 4,600 Precision rectal thermistor (YSI Temperature, Dayton, OH) for core temperature monitoring, wired skin sensors (Grant Industries, Surrey, UK) for skin temperature measurements at 4 sites (shoulder, chest wall, thigh, and calf) to determine mean global skin temperature,5 2 wireless iButton sensors (Maxim, San Jose, CA) for facial skin temperature and respirator microenvironment (ie, respirator dead space, identified as the airspace between the respirator's internal surface and the wearer's face that is not occupied by any part of the facial anatomy) temperature and humidity measurements, a Tosca (Radiometer America, Westlake, OH) combination pulse oximeter-transcutaneous carbon dioxide sensor attached to an earlobe for pulse-derived oxygen saturation (SpO2)–transcutaneous carbon dioxide (tcpCO2)–heart rate (HR) monitoring, and a BioHarness physiologic monitoring chest strap (Zephyr, Annapolis, MD) for respiratory rate (RR) determination.
Subjects were given instructions in donning FFRs, performed negative and positive user seal checks to assess the seal of the FFR to the face,2 and then underwent respirator quantitative fit testing of a 3M model 1870 N95 FFR (3M, St Paul, MN) with the PortaCount Plus Model 8020. Fit testing of the N95 FFR was carried out with the N95-Companion Model 8095 fit tester (TSI, Shoreview, MN), a condensation nucleus particle counter that measures the concentrations of ambient particles outside and inside the FFR during successive 1-minute OSHA standard exercises (normal breathing, deep breathing, head movement side-to-side, head movement up and down, talking out loud, bending over, and normal breathing) and one 15-second exercise (grimace) that is not included in the calculation of the fit factor.2 The fit factor is the ratio of the outside and inside particles and is calculated as follows:
where FF is the fit factor, Cb is the particle concentration in the ambient sample before the respirator sample, Ca is the particle concentration in the ambient sample after the respirator sample, and Cr is the particle concentration in the respirator sample. The subjects then donned a 3M model 8293 P100 FFR (3M, St Paul, MN), adjusted the straps, and underwent quantitative fit testing using the PortAcount Plus Model 8020 (the N95 Companion is not used for P99 and P100 respirators). Fit factors with the PortaCount with N95 Companion are normally reported up to 200, and if they surpass this level, they are reported as 200+ because they exceed the manufacturer's recommended operating range,6 whereas the PortaCount Plus can record fit factors as high as 10,000 (for ease of data comparisons between the N95 FFR and P100 FFR in the current study, scores >200 for the P100 FFR were recorded as 200+). A passing score on an OSHA quantitative fit test is ≥100, indicating ≤1% penetration of particles into the dead space of the respirator. The 3M 1870 N95 FFR and 8293 P100 FFR models (see Fig 1 and Table 1 for FFR features) were fit tested immediately before (pre-exercise) and after (postexercise) 1 hour of treadmill walking (5.6 km/h, 0° incline) in an environmental chamber with ambient conditions of 35°C and relative humidity 50% (equivalent to a heat index of 40.7°C).
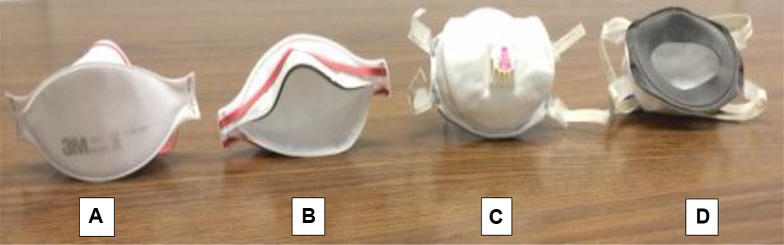
Fig 1.
Anterior and posterior views of 3M model 1870 N95 filtering facepiece respirator (A and B) and 3M model 8293 P100 filtering facepiece (C and D).
Table 1.
Filtering facepiece respirator features
| Parameters | 3M 1870 N95 FFR | 3M 8293 P100 FFR |
|---|---|---|
| Sizes available | Standard | Standard |
| Shape | Flat fold | Cup |
| Dimensions (cm) | 21.0 × 23.8 × 8.6 | 20.3 × 26.6 × 5.0 cm |
| Weight (gm) | 9.3 | 29.3 |
| Exhalation valve | No | Yes |
| Tethering devices | Two narrow, nonadjustable polyisoprene bands | Two adjustable, wide, braided polyester straps with multiple parallel polyisoprene bands |
| Layers | Three hydrophobic layers | Three hydrophobic layers |
| Other features | Pliable nose bar | Pliable nose bar, inner foam face seal |
| Static dead space volume (mL) | 325 | 240 |
| Filter resistance (mm H2O)∗ | 6.3 ± 0.5 | 17.4 ± 0.8 |
FFR, filtering facepiece respirator.
Measured at 85 L/min of constant airflow.
Three randomly allocated exercise sessions were carried out on separate days: 2 sessions involved wearing either model of FFR, and 1 involved a control session (no FFR). Subjects were not allowed to make any adjustments to the respirators after the initial adjustment just prior to the pre-exercise fit test, so the postexercise fit test reflected only the impact of the exercise and environment. All fit testing was performed outside of the environmental chamber. During the treadmill exercise, subjective measurements were taken at baseline and then every 20 minutes using visual analog numerical scales for exertion (Borg Rating of Perceived Exertion Scale, a 15-grade scale ranging from no exertion at all to maximal exertion),7 thermal comfort (Frank Comfort Scale, a 10-point scale ranging from the coldest you have ever been to the hottest you have ever been),8 and a 7-point respiratory scale of overall breathing discomfort (ranging from no discomfort to intolerable discomfort).9 Respirators were weighed immediately pre- and post-testing on an accu-6201 calibrated analytical balance (Fisher Scientific, Waltham, MA) to determine moisture retention.
Statistical analysis
The χ2 test with Yates correction for continuity was used to analyze any difference in the pass rate of the 2 respirators on the pre-exercise fit test. The McNemar test was used to analyze changes in fit factors after 1 hour of use in a hot, humid environment (postexercise) for subjects who passed the pre-exercise fit. Physiologic and subjective data were analyzed using 2-way repeated-measures analysis of variance to determine the main effect of the FFRs (3 conditions) over time (4 time points over 1 hour), with the Greenhouse-Geisser correction for the violation of sphericity. A statistical significance was accepted when P < .05, and all analyses were performed using a statistical software package (SPSS version 19; IBM, Somers, NY).
Results
There was no significant difference in the pass rate on the pre-exercise fit test between N95 and P100 FFRs (χ2 = 0.2526, P = .61). Of subjects who passed both pre-exercise fit tests, a significant number failed the postexercise fit test with the N95 FFR (P > .99), but not with the P100 FFR (P = 1.0) (Table 2 ).
Table 2.
Respirator quantitative FF at FF 1 in a neutral ambient environment and FF 2 at ambient conditions of 35°C and relative humidity 50%
| Respirator | Subjects |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| N95 FFR | ||||||||||||
| FF 1 | 85 | 107 | 66 | 200+ | 191 | 148 | 132 | 104 | 200+ | 200+ | 119 | 146 |
| FF 2 | 118 | 28 | 24 | 77 | 146 | 22 | 109 | 69 | 107 | 47 | 75 | 79 |
| P100 FFR | ||||||||||||
| FF 1 | 7.7 | 71 | 4.7 | 200+ | 200+ | 200+ | 200+ | 200+ | 200+ | 200+ | 200+ | 200+ |
| FF 2 | 15 | 66 | 6.4 | 200+ | 108 | 158 | 12 | 200+ | 107 | 200+ | 200+ | 200+ |
FF, fit factors; FF 1, fit factors at baseline; FF 2, fit factors after 1 hour of treadmill exercise; FFR, filtering facepiece respirator.
There was no significant difference in mean values between controls and respirators for rectal temperature (F = 0.560, P = .519), global skin temperature (F = 0.350, P = .654), SpO2 (F = 1.461, P = .25), tcpCO2 (F = 1.829, P = .19), HR (F = 0.413, P = .625), RR (F = 0.209, P = .79), thermal sensation (F = 0.478, P = .57), perception of exertion (F = 1.495, P = .25), and microenvironment temperature (F = 2.421, P = .14) or humidity (F = 2.747, P = .12). There were also no significant differences for these same variables when comparing the N95 FFR with the P100 FFR. There was a significant difference with FFR wear in the temperature of the facial skin covered by the FFR (F = 7.460, P = .009) and breathing comfort (F = 8.634, P = .002) when compared with controls. Time approached statistical significance for tcpCO2 (P = .05) and had a significant effect (P = .02 for SpO2, P < .001 for all other variables) on measured subjective and physiologic parameters (Table 3, Table 4, Table 5 ).
Table 3.
Temperatures of subjects over the course of 1 hour of treadmill exercise at ambient conditions of 35°C and relative humidity 50%
| Parameters | Control | N95 FFR | P100 FFR |
|---|---|---|---|
| Rectal temperature (°C) | |||
| 0 min | 37.16 ± 0.39 | 37.15 ± 0.34 | 37.10 ± 0.30 |
| 20 min | 37.42 ± 0.34 | 37.29 ± 0.35 | 37.34 ± 0.34 |
| 40 min | 37.63 ± 0.38 | 37.50 ± 0.30 | 37.55 ± 0.33 |
| 60 min | 37.76 ± 0.39 | 37.64 ± 0.31 | 37.70 ± 0.33 |
| Mean skin temperature (°C) | |||
| 0 min | 26.3 ± 1.7 | 26.6 ± 1.5 | 26.7 ± 2.5 |
| 20 min | 30.9 ± 0.8 | 31.2 ± 0.9 | 31.1 ± 1.5 |
| 40 min | 33.3 ± 0.5 | 33.5 ± 0.4 | 33.3 ± 0.8 |
| 60 min | 34.3 ± 0.3 | 34.4 ± 0.3 | 34.3 ± 0.4 |
| Facial skin temperature under a respirator (°C) | |||
| 0 min | 32.9 ± 1.2 | 33.7 ± 1.0 | 33.8 ± 0.8∗ |
| 20 min | 34.7 ± 0.9 | 35.3 ± 0.4∗ | 35.3 ± 0.4∗ |
| 40 min | 34.6 ± 0.9 | 35.3 ± 0.5∗ | 35.4 ± 0.6∗ |
| 60 min | 34.8 ± 0.7 | 35.0 ± 0.7 | 35.1 ± 0.8 |
NOTE. Values are mean ± SD.
FFR, filtering facepiece respirator.
Significantly different from controls (P < .05).
Table 4.
Physiologic and subjective parameters over 1 hour of treadmill exercise at ambient conditions of 35°C and relative humidity 50%
| Parameters | Control | N95 FFR | P100 FFR |
|---|---|---|---|
| O2 saturation (%) | |||
| 0 min | 98.1 ± 0.7 | 98.2 ± 0.8 | 97.8 ± 0.9 |
| 20 min | 97.8 ± 0.6 | 97.8 ± 1.0 | 97.3 ± 1.0 |
| 40 min | 97.6 ± 1.0 | 97.5 ± 0.7 | 97.7 ± 1.2 |
| 60 min | 97.9 ± 1.1 | 97.8 ± 0.6 | 97.3 ± 0.8 |
| Transcutaneous CO2 (mm Hg) | |||
| 0 min | 40.8 ± 1.8 | 39.3 ± 4.0 | 41.2 ± 1.3 |
| 20 min | 41.6 ± 2.5 | 41.8 ± 2.7 | 42.8 ± 2.7 |
| 40 min | 41.6 ± 3.1 | 41.7 ± 2.4 | 42.7 ± 2.0 |
| 60 min | 40.9 ± 2.4 | 41.3 ± 2.4 | 42.6 ± 2.1 |
| Heart rate (beats/min) | |||
| 0 min | 74.0 ± 7.8 | 72.8 ± 16.1 | 68.1 ± 13.2 |
| 20 min | 100.4 ± 12.4 | 97.7 ± 10.3 | 98.7 ± 10.7 |
| 40 min | 104.3 ± 14.9 | 101.1 ± 12.2 | 101.1 ± 9.8 |
| 60 min | 106.2 ± 14.8 | 105.9 ± 11.9 | 105.1 ± 9.2 |
| Respiratory rate (breaths/min) | |||
| 0 min | 15.1 ± 6.4 | 15.4 ± 4.7 | 16.0 ± 2.6 |
| 20 min | 27.1 ± 5.1 | 27.1 ± 2.8 | 26.8 ± 8.0 |
| 40 min | 27.3 ± 6.5 | 28.8 ± 3.4 | 28.6 ± 6.8 |
| 60 min | 28.1 ± 7.1 | 28.4 ± 3.2 | 29.3 ± 6.5 |
| Breathing comfort (1 [no discomfort] to 7 [intolerable discomfort]) | |||
| 0 min | 1.0 ± 0.0 | 1.1 ± 0.3 | 1.1 ± 0.3 |
| 20 min | 1.3 ± 0.5 | 1.8 ± 0.6∗ | 1.6 ± 0.5∗ |
| 40 min | 1.6 ± 0.8 | 2.1 ± 0.5∗ | 2.0 ± 0.7∗ |
| 60 min | 1.7 ± 0.8 | 2.2 ± 0.6∗ | 2.4 ± 0.5∗ |
| Thermal sensation (0 [coldest] to 5 [neutral] to 10 [hottest]) | |||
| 0 min | 4.8 ± 0.4 | 4.8 ± 0.6 | 4.8 ± 0.4 |
| 20 min | 5.8 ± 0.5 | 5.8 ± 0.5 | 5.9 ± 0.3 |
| 40 min | 6.3 ± 0.5 | 6.3 ± 0.6 | 6.3 ± 0.5 |
| 60 min | 6.4 ± 0.5 | 6.6 ± 0.5 | 6.7 ± 0.5 |
| Exertion (Borg scale 6-20 [no exertion at all] to 11 [light exertion] to 20 [maximal exertion]) | |||
| 0 min | 6.0 ± 0.0 | 6.2 ± 0.4 | 6.0 ± 0.0 |
| 20 min | 8.1 ± 1.4 | 8.2 ± 1.6 | 8.0 ± 1.2 |
| 40 min | 9.1 ± 2.0 | 9.5 ± 1.9 | 9.6 ± 1.6 |
| 60 min | 9.3 ± 2.0 | 9.9 ± 2.1 | 10.5 ± 1.7 |
NOTE. Values are mean ± SD.
Abbreviation: FFR, filtering facepiece respirator.
Significantly different from controls (P < .05).
Table 5.
Respirator microclimate (dead space) parameters over 1 hour of treadmill exercise at ambient conditions of 35°C and relative humidity 50%
| Parameters | N95 FFR | P100 FFR |
|---|---|---|
| Microclimate temperature (°C) | ||
| 0 min | 31.8 ± 2.1 | 31.2 ± 1.9 |
| 20 min | 35.0 ± 0.4 | 34.7 ± 0.8 |
| 40 min | 35.0 ± 0.6 | 34.9 ± 0.5 |
| 60 min | 35.0 ± 1.0 | 35.1 ± 0.8 |
| Microclimate relative humidity (%) | ||
| 0 min | 56.0 ± 12.8 | 62.5 ± 9.6 |
| 20 min | 76.0 ± 14.7 | 81.2 ± 8.4 |
| 40 min | 79.2 ± 15.2 | 86.3 ± 7.5 |
| 60 min | 82.8 ± 16.6 | 89.9 ± 5.6 |
NOTE. Values are mean ± SD. There was no significant difference in FFR moisture retention after 1 hour of treadmill exercise (N95 FFR = 4.13 ± 3.05 g, P100 FFR = 5.45 ± 4.31; P = .44).
FFR, filtering facepiece respirator.
Discussion
Our data indicate no statistically significant differences between FFR models passing the pre-exercise fit tests; the pass rates (FF ≥100) are in line with those of other reported studies.10, 11, 12 The failures of both models on the initial fit tests reflect the recognition that there is high variability in obtaining a good fit with the FFR13, 14 as a result of numerous factors (facial anthropometrics, respirator style and features, material quality, training, experience, etc); therefore, no single FFR model is likely to obtain a passing score each time it is tested. However, of subjects passing the pre-exercise fit test, a significant number failed on the postexercise test with the N95 FFR, but not with the P100 FFR (Table 2). Facial sweat has been reported to interfere with the fit of some respirators,3 and all subjects in the current study were observed to be sweating profusely during the 1 hour of exercise in the hot, humid environment. The impact of the hot, humid ambient environment is further supported by the significantly higher retained moisture of both respirators compared with that previously reported for the N95 FFR over 1 hour at a similar work rate in temperate ambient conditions.15, 16 In addition to possible effects on face seal and breathing resistance, significant moisture retention in nonrigid protective facemasks can lead to facemask collapse on inspiration that impedes breathing; therefore, rigid FFRs, such as the P100, may retain their shape better in hot, humid conditions of prolonged FFR wear.17, 18 It may be that the better postexercise fit factor performance of the P100 FFR was, at least in part, related to its inner gasket-like flange (face seal) (Table 1, Fig 1D), which offers a larger sealing surface area than that of the N95 FFR.19 The adjustable straps of the P100 FFR (Table 1) might also offer an advantage of tailoring the face seal pressure to compensate for the variability in facial anthropometrics among respirator users and thereby may enhance fit. The 2 individuals who failed the initial fit testing with the N95 FFR and the 1 individual who barely passed (FF = 107) are the same 3 individuals who also failed the initial fit testing with the P100 FFR (Table 2), suggesting that they shared some common features that impact fit (anthropometrics, etc). Of further (but possibly related) note, the 2 respirator models studied are available commercially only in 1 size (that is expected to fit most, but not all, faces) rather than the multiple sizes offered for most FFRs (ie, small, medium, medium-large, large) to accommodate recognized differences in facial sizes. Having a 1-size FFR model that fits most users well offers certain commercial and logistical advantages, but the fact that it cannot fit all users in a given respirator protection program is an important consideration.
There were no significant differences between controls and FFRs with respect to measured physiologic variables, save for the temperature of the facial skin under the respirator, a finding that was not unexpected because of the FFR barrier effects on facial skin heat dissipation (eg, convection, radiation, evaporation) that has been previously reported with N95 FFR use.20 The findings of no significant differences between controls and FFRs with respect to overall skin temperature, rectal temperature, and thermal perceptions indicate that the use of FFRs in hot, humid environments does not add to the body's thermophysiologic or perceptual burdens. The lack of significant physiologic impact of N95 FFR use compared with controls was also not unexpected because comparable findings have been previously reported with N95 FFRs having similar filter resistances.15, 16 This is the result of decreased breathing resistance that is the result of the incorporation of electrostatic charges into the filter that allows for improved particle capture without increasing filter density. This is also related to the fact that workload intensity (low to moderate in the current study) has a greater impact physiologically (eg, HR, RR) than the magnitude of inspiratory resistance.9 The lack of significant difference between the 2 FFR models with respect to measured physiologic variables was, however, somewhat unanticipated given the roughly 3-fold difference in filter resistance of the P100 FFR (Table 1). The similarity in the RR between the 2 FFRs and controls suggests that the FFR filter resistances were compensated for by an increase in the respective respiratory duty cycles (the portion of the respiratory cycle spent in inhalation), a feature that may be imperceptible to the FFR wearer at the study's low to moderate work rate.21 Therefore, the significant subjective perception of increased breathing discomfort with either FFR compared with controls may have been related to other issues, such as the significantly greater facial skin heat, associated respirator microenvironment (respirator dead space) moisture and heat, or temperature of the inhaled air (determined by the composite of the temperature of the entrained ambient air and respirator dead space air temperature). The finding of no significant beneficial impact on study variables attributable to the exhalation valve of the P100 FFR has previously been reported for N95 FFR use over 1 and 2 hours, at the same work rate as the current study, and attributed to the lack of development of the streamlined airflows required for exhalation valve activation at low to moderate work rates.22, 23 The lack of significant difference in the increased temperature of the facial skin covered by either of the FFRs further supports that the P100 exhalation valve was likely not sufficiently activated.23 The impact of an exhalation valve could be evaluated through the use of an infrared camera to determine surface temperatures of different models of FFRs (with and without an exhalation valve) at similar work rates.24 The absence of significant differences in thermal perceptions between controls and FFRs suggests that global skin temperature in a hot, humid environment is the major contributor to perceptions of thermal discomfort rather than the FFR itself.
Limitations of this study include the relatively small subject numbers (n = 12). However, all subjects were experienced FFR users; therefore, the data are likely to be reliable. We only tested subjects for 1 hour of exercise at a low to moderate work rate and cannot comment on findings with more prolonged FFR use or higher work rates. Only 1 model each of the N95 FFR and P100 FFR from a single manufacturer was tested, and we cannot comment on other FFR classes (eg, P99 FFR, N99 FFR), models (eg, cup shaped, duck bill, pleated), other exhalation valve-equipped models, or FFRs from different manufacturers. Although the tested N95 FFR and P100 FFR were of different design styles (flat fold and cup-shaped, respectively), prior investigations comparing flat-fold and cup-shaped N95 FFRs have reported no statistically significant differences in fit factors between designs.19, 25 It may be that anthropometric features, selecting the appropriate respirator size, and certain respirator features (eg, adjustable straps) are more important to respirator fit than respirator style.25 Some of the subjects who failed a fit test (ie, score <100) nonetheless still attained a score (≥10) that correlated with the OSHA-assigned protection factor of 10 for FFRs (the workplace level of respiratory protection that a respirator or class of respirators is expected to provide to employees when the employer implements a continuing, effective respiratory protection program as specified by the OSHA).
Conclusions
A P100 FFR had a significantly greater proportion of passing scores on respirator quantitative fit testing after 1 hour of treadmill exercise at a low to moderate work rate in a hot, humid environment without significant difference in measurable physiologic stress compared with an N95 FFR. The adjustable straps that permit tailoring of face seal pressure to compensate for variability in facial dimensions, and the inner flange on the P100 FFR that allows for a greater sealing surface to the face when compared with the study N95 FFR model, may serve to maintain an acceptable fit in environments associated with increased facial moisture. At low to moderate work rates, exhalation valves on FFRs may not be activated. Wearing a FFR in hot, humid environments at low to moderate work rates does not add to the body's thermophysiologic or perceptual burdens. In hot, humid environments where respiratory protection is mandated, the use of P100 FFRs may offer some advantages over N95 FFRs in maintaining FFR fit without any additional physiologic burden over 1 hour of use at low to moderate work rates, while simultaneously offering a higher level of filtration.
Acknowledgments
We thank Andrew Palmiero, MS, Michael Bergman, MS, and W. Jon Williams, PhD, of the National Institute for Occupational Safety and Health for their manuscript reviews.
Footnotes
Funding/Support: Supported by National Personal Protective Technology Laboratory internal operating funds.
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of product names does not constitute endorsement by the authors or the National Institute for Occupational Safety and Health.
Conflicts of interest: None to report.
References
- 1.Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health: NIOSH guide to the selection and use of particulate respirators. DHHS (NIOSH) Publication No. 96-101, 1996. Available from: http://www.cdc.gov/niosh/docs/96-101/. Accessed January 21, 2015.
- 2.S. Department of Labor, Occupational Safety & Health Administration, Regulations (Standards - 29 CFR), Appendix A to § 1910.134: Fit Testing Procedures (Mandatory). Available from: https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9780. Accessed January 21, 2015.
- 3.Caretti D.M., Gardner P.D. Respirator fit factor performance while sweating. Am Ind Hyg Assoc J. 1999;60:84–88. doi: 10.1080/00028899908984425. [DOI] [PubMed] [Google Scholar]
- 4.Roberge R.J., Kim J.H., Coca A. Protective facemask impact on human thermoregulation: an overview. Ann Occup Hyg. 2012;56:102–112. doi: 10.1093/annhyg/mer069. [DOI] [PubMed] [Google Scholar]
- 5.Ramanathan N.L. A new weighting system for mean surface temperature on the human body. J Appl Phys. 1964;19:531–533. doi: 10.1152/jappl.1964.19.3.531. [DOI] [PubMed] [Google Scholar]
- 6.Rengasamy S., Eimer B.C., Shaffer R.E. Evaluation of the performance of the N95-Companion: effects of filter penetration and comparison with other aerosol instruments. J Occup Environ Hyg. 2012;9:417–426. doi: 10.1080/15459624.2012.685838. [DOI] [PubMed] [Google Scholar]
- 7.Borg C. Psychophysical basis of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- 8.Frank S.M., Raja S.N., Bulcao C.F., Goldstein D.S. Relative contribution of core and cutaneous temperatures to thermal comfort and the autonomic response in humans. J Appl Phys. 1999;86:1588–1593. doi: 10.1152/jappl.1999.86.5.1588. [DOI] [PubMed] [Google Scholar]
- 9.Antunano MJ, Baumgardner FW, Chen YT, Constable SH. Characterization of chemical defense mask breathing resistance tolerances. 1993. Available from: http://oai.dtic.mil/oai/oai?verb=getRecord&metadataPrefix=html&identifier=ADA265221. Accessed January 22, 2015.
- 10.Centers for Disease Control and Prevention (CDC) Laboratory performance evaluation of N95 filtering facepiece respirators, 1996. MMWR Morb Mortal Wkly Rep. 1998;47:1045–1049. [PubMed] [Google Scholar]
- 11.Wilkinson I.J., Pisaniello D., Ahmad J., Edwards S. Evaluation of a large-scale quantitative respirator-fit testing program for healthcare workers: survey results. Infect Control Hosp Epidemiol. 2010;31:918–925. doi: 10.1086/655460. [DOI] [PubMed] [Google Scholar]
- 12.Pauli U., Karlen S., Summermatter K. The importance of fit-testing particulate filtering facepiece respirators! Appl Biosafety. 2014;19:184–192. [Google Scholar]
- 13.Clapham S.J., Stephenson D.J., Wallace D.O., Lillquist D.R., Suruda A.J. Comparison of N95 disposable filtering facepiece fits using Bitrex qualitative and TSI Portaccount® quantitative fit testing. Int J Occup Environ Health. 2000;6:50–54. doi: 10.1179/oeh.2000.6.1.50. [DOI] [PubMed] [Google Scholar]
- 14.Frost S, Mogridge R, Roff M, Health and Safety Laboratory. Review of fit test pass criteria for filtering facepieces class 3 (FFP3) respirators. 2015. Available from: http://www.hse.gov.uk/research/rrpdf/rr1029.pdf. Accessed August 24, 2015.
- 15.Roberge R.J., Coca A., Williams W.J., Powell J.B., Palmiero A.J. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care. 2010;55:569–577. [PubMed] [Google Scholar]
- 16.Roberge R.J., Coca A., Williams W.J., Palmiero A.J., Powell J.B. Surgical mask placement over N95 filtering facepiece respirators: physiological effects on healthcare workers. Respirology. 2010;15:516–521. doi: 10.1111/j.1440-1843.2010.01713.x. [DOI] [PubMed] [Google Scholar]
- 17.Roberge R.J., Kim J.H., Benson S.M. Absence of consequential changes in physiological, thermal and subjective responses from wearing a surgical mask. Respir Physiolo Neurobiol. 2012;181:29–35. doi: 10.1016/j.resp.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Roberge R. Factors impacting respirator comfort & tolerance to N95 filtering facepiece respirators: research results from Project BREATHE. 2014. Available from: http://prague.isrp.com/index.php/presentations/101-raymond-roberge-1/file. Accessed June 23, 2015.
- 19.Niezgoda G., Kim J.H., Roberge R.J., Benson S.M. Flat fold and cup-shaped N95 filtering facepiee respirator face seal area and pressure determinations: a stereophotogrammetry study. J Occup Environ Hyg. 2013;10:419–424. doi: 10.1080/15459624.2013.801246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberge R.J., Benson S., Kim J.H. Thermal burden of N95 filtering facepiece respirators. Ann Occup Hyg. 2012;56:808–814. doi: 10.1093/annhyg/mes001. [DOI] [PubMed] [Google Scholar]
- 21.Kim J.H., Roberge R.J., Powell J.B., Shaffer R.E., Ylitalo C.M., Sebastian J.M. Pressure drop of filtering facepiece respirators: how low should we go? Int J Occup Med Environ Health. 2015;28:1–10. doi: 10.13075/ijomeh.1896.00153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberge R.J., Kim J.-H., Benson S.M. N95 filtering facepiece respirator deadspace temperature and humidity. J Occup Environ Hyg. 2012;9:166–171. doi: 10.1080/15459624.2012.660428. [DOI] [PubMed] [Google Scholar]
- 23.Roberge R.J. Are exhalation valves on N95 filtering facepiece respirators beneficial at low-moderate work rates: an overview. J Occup Environ Hyg. 2012;9:617–623. doi: 10.1080/15459624.2012.715066. [DOI] [PubMed] [Google Scholar]
- 24.Monaghan W.D., Roberge M.R., Rengasamy M., Roberge R.J. Thermal imaging comparison of maximum surface temperatures achieved on N95 filtering facepiece respirators with and without exhalation valves at sedentary breathing volumes. J Int Soc Resp Protect. 2009;26:12–19. [Google Scholar]
- 25.Zhuang Z., Coffey C.C., Ann R.B. The effect of subject characteristics and respirator features on respirator fit. J Occup Environ Hyg. 2005;2:641–649. doi: 10.1080/15459620500391668. [DOI] [PubMed] [Google Scholar]