Abstract
Background
The 2015 Middle East respiratory syndrome (MERS) outbreak in South Korea was a serious threat to public health, and was exacerbated by the inappropriate responses of major institutions and the public. This study examined the sources of confusion during the MERS outbreak and identified the factors that can affect people's behavior.
Methods
An online survey of the risk perception of university students in South Korea was performed after the epidemic had peaked. The questionnaire addressed the major social determinants in South Korea during the MERS epidemic. The analysis included data from 1,470 subjects who provided complete answers.
Results
The students had 53.5% of the essential knowledge about MERS. Women showed higher risk perception than men, and trust in the media was positively associated with risk perception (P < .001). Additionally, risk perception was positively associated with overreaction by the public (odds ratio, 2.80; 95% confidence interval, 2.17-3.60; P < .001). These findings suggest that media content affected the public's perception of MERS risk and that perception of a high level of risk led to overreaction.
Conclusions
Risk perception was associated with most of the social factors examined and overreaction by the public. Therefore, providing accurate information and data to the public, establishing trust, and facilitating the development of an attitude will all be important in future crises.
Key Words: MERS, Risk perception, Risk communication, Infectious disease, Trust, Overreaction
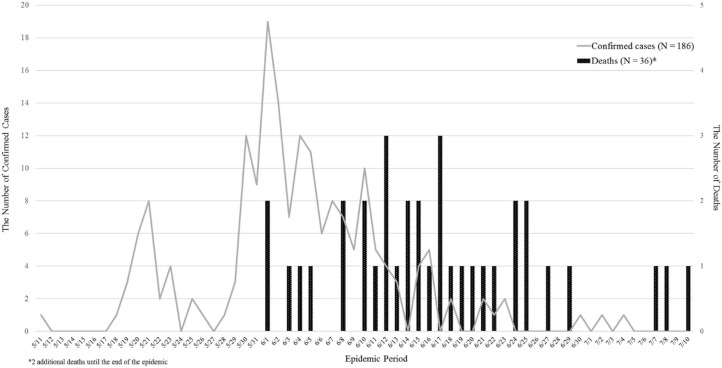
The first Middle East respiratory syndrome (MERS) case was confirmed in South Korea on May 20, 2015. The last case was diagnosed on July 4 and summed up to a total of 186 confirmed cases, almost half of which were in Seoul. After that, South Korea officially declared the end of the MERS epidemic on December 23, 2015. During the MERS outbreak, 38 died and 16,752 had been quarantined (Fig 1).1 The case fatality rate of MERS in South Korea was approximately 20.4%, lower than that on the Arabian Peninsula (approximately 45%).2
Fig 1.
Epidemic curve of Middle East respiratory syndrome in South Korea from May 11-July 10, 2015.
Public apprehension was exacerbated because the government did not disclose timely information about the status of the epidemic or hospitals' names and procedures related to MERS infection. Therefore, the public were unaware of the appropriate actions to take, but were provided with relevant information by the media. Indeed, several citizens created Web sites that listed confirmed and suspected MERS patients.3 However, the public also received inaccurate information from the Internet and social media; this increased the level of concern over MERS and resulted in rumors. The government of South Korea stated that any person who disseminated an untrue rumor would be prosecuted, but this failed to reduce the level of panic.
Although this action was supposed to prevent secondary damage, it was similar to the censorship of the media in China, where the propaganda departments of the Chinese Communist Party directly supervised the media flow when the severe acute respiratory syndrome (SARS) outbreak occurred in 2003.4 The Chinese government attempted to maintain political, social, and economic stability by minimizing the SARS crisis through the withholding of information; however, a reverse effect occurred. Nevertheless, the Chinese government assigned responsibility for censorship of the media, including the Internet, to local agencies.5 In the new media age, in which social media (including the Internet, short message services, and mobile applications) are centralized, the government restricts freedom of expression in the same way as it has restricted such freedom among traditional media sources, such as newspapers, radio, and television.6 The control of the acquisition of information is more difficult in this new age because social media are tools not only for the dissemination, sharing, and seeking of health information but also for the expression of feelings and the sharing of personal experiences and opinions.7, 8 Therefore, organizations need to build effective communication tools to respond to emerging infectious disease (EID) outbreaks because the public may express scientific skepticism about scientific topics and participation in decision-making.9
During epidemics, people usually require guidance on how to behave from a trusted source. The government and public institutions are the ideal sources because people tend to rely on the national administration. For this reason, trust in these institutions plays a main role in the public's acceptance of policies and actions.10 The World Health Organization suggested that outbreak communication should incorporate the following 5 key factors: (1) building, maintaining, or restoring trust; (2) announcing early; (3) maintaining transparency; (4) understanding the public; and (5) planning of all aspects of the response to an outbreak.11 Therefore, risk communication enhances the decision-making ability of laypeople, and can be examined by assessing risk perception.12 Trust in not only the government and public agencies but also in the media and other institutions may be associated with risk perception. Therefore, the instigation of fear among the public by the media may contribute to social panic, particularly in emergency situations.
The term risk perception usually refers to individuals' judgments about and evaluations of hazards to which they might be exposed.13 Therefore, risk perception might be among the social phenomena related to exposure to the risk of disease. In addition, perceived risk influences health behavior both positively and negatively.14 During the MERS outbreak in South Korea, negative behaviors were observed, such as oversensitive or inappropriate reactions. Some children of health care workers at hospitals treating MERS patients were prevented from attending school. Meanwhile, self-quarantined subjects occasionally escaped out of their homes until the level of infection subsided. These reactions of citizens reflect distrust in the government and accelerated noncompliance with the directions provided by the Korea Centers for Disease Control and Prevention. This finding is important because overreaction is an indicator of the level of trust in the government among the public and may provoke another social problem related to moral panic.15
Fear causing the behaviors described previously mentioned is likely related to risk perception and a low level of trust in the government and society. However, because risk perception may be related to a number of unknown determinants, it is important to identify factors that may affect risk perception. Sjöberg examined risk perception using several approaches,16 and reported that 30%-40% of risk perception could be explained by risk sensitivity, attitude, and a specific fear model. In other models, <20% of risk perception was explained. There were also some studies regarding risk perception. Previous studies of risk perception related to nuclear explosions and infectious diseases addressed the relationship between perceived risk and various social predictors, such as knowledge, social trust, and attitude.17, 18 However, previous literature on the determinants of risk perception has been limited.
The aim of this study was to determine whether risk perception was associated with personal and social variables, including trust in the media, the health care field, and government. Additionally, we sought to identify the associations of risk perception and social variables with compliance with self-quarantine guidelines and overreaction during the MERS epidemic. In this study, knowledge, trust, personal characteristics, and other social determinants were considered the main factors affecting risk perception and overreaction.
Methods
Questionnaire
We developed a questionnaire based on previous studies of perception of the risk of SARS and Ebola conducted outside of South Korea.19, 20, 21 The questionnaire comprised the following 5 components: knowledge of MERS (9 items), risk perceptions about MERS (7 items), trust in society and governmental health policy(5 items), preventive behavior (11 items), and particular situations relating to MERS (7 items). Sociodemographic information was also obtained. Korean- and English-language versions of the questionnaire were developed to enable inclusion of foreign students in the survey (Supplementary Appendix S1). The English-language version of the questionnaire was backtranslated into Korean for quality control purposes.
Questions regarding knowledge of MERS were used to estimate the level of accuracy of the following information: the self-recognized level of knowledge, the concept of MERS, route of transmission, the concept of close contact, symptoms, the concept of the incubation period, characteristics of MERS, self-quarantine, and treatment of MERS. Evidence for these questions was from the MERS response guidelines of the Korea Centers for Disease Control and Prevention.22 The cumulative knowledge score of the participants was calculated (range, 0-8; 1 point for each correct response [ie, in agreement with the evidence]). Because all questions referred to information provided in governmental guidelines, the survey was regarded as providing an estimate of respondents' essential knowledge.
Risk perceptions were assessed using revised versions of the Ebola risk perception surveys conducted in Germany20 and Israel.21 Risk perception was assessed using levels of agreement with the following statements: “I think that I will contract MERS if I come into contact with a MERS patient (risk perception 1),” “I think that I might contract MERS even if I do not come into contact with a MERS patient (risk perception 2),” “My health will be severely damaged if I contract MERS (risk perception 3),” “I think MERS is more severe than other respiratory diseases (risk perception 4),” “Even if I fall ill with another disease, I will not go to hospital because of MERS (risk perception 5),” “MERS will inflict serious damage on my community (risk perception 6),” and “MERS may spread in Korea again someday (risk perception 7).” The questions were responded to on a 5-point Likert scale. In addition, because risk perception is a continuous variable, it was classified into 4 groups according to quantile (very high, high, low, and very low).
A revised questionnaire regarding trust in society, media, and health policy was developed from the Korean General Social Survey (KGSS). The KGSS has been validated in South Korea and is conducted periodically nationwide. Several questions in the KGSS estimate the levels of trust among respondents in society, the media, central and local government, the national assembly, the medical profession, and nongovernmental organizations (NGOs). Such trust was expected to be associated with trust in health policy because governmental actions tend to reflect governmental policies.
Finally, questions regarding particular situations related to MERS were classified into the following 2 categories: overreaction and compliance with self-quarantine. A large proportion of the population of South Korea was unaware of the appropriate actions during the MERS epidemic. These categories measure the characteristics of individuals not inclined to abide by the self-quarantine guidelines. Therefore, this section assessed the following personal characteristics: degree of optimism about the health policies of South Korea, willingness to sacrifice for society, responsiveness to an emergency situation, and attitude toward self-quarantine and overreaction. Attitude toward self-quarantine was measured with a question asking whether respondents were willing to prioritize quarantine adherence above all personal needs (responses were categorized as yes and no). The overreaction section comprised the following 2 questions: (1) How would you react if you realized your children were in the same class as those of someone suspected (or confirmed) to have MERS (including school and extracurricular activities)?; and (2) How would you react if you realized your children were in the same class as those of medical workers at hospitals with MERS patients (including school and extracurricular activities)? The responses to the formerly involved overreactions, for example, “(Do not) Allow my relatives or children of my family to attend school,” and those to the latter were the opposite, such as “I think children of medical workers at hospitals with MERS patients should (not) be allowed to attend school.” Each question was assumed to indicate overreaction to the behavior of oneself and others.
A presurvey including 152 participants was performed to assess the reliability and validity of the questionnaire and the direction of the responses. The presurvey was conducted both in the field using a tablet personal computer or laptop and online using an online survey application (SurveyMonkey, San Mateo, CA). Data for the main survey were collected by e-mailing students at Seoul National University. The Cronbach α values for the 2 new measures developed for this study, trust and risk perception, were 0.8307 and 0.6755, respectively, in the main survey.
Participants
Students at Seoul National University were selected for the study. We considered this population appropriate for several reasons. First, they are not likely to include people associated with hospitals. Second, younger individuals tend to have access to up-to-date information through smartphones or the Internet. Third, the subjects had similar levels of academic attainment and demographic characteristics. Finally, because of the need for a timely investigation, this setting assured the benefit of accessibility and cost-efficiency.
For the main survey, e-mails containing the link connected to the online survey setting were sent to all of the 30,727 students at Seoul National University, including undergraduates, postgraduates, and foreign students. Survey e-mails were sent on 3 occasions at weekly intervals from October 6-23, 2015. Of the 30,727 students, 1,487 (4.8%) provided a complete response. After exclusion of those with missing responses, a total of 1,470 subjects were included in the study. This survey and research were approved by the Institutional Review Board of Seoul National University (No. 1508/002-003).
Statistical analysis
Relationships between levels of risk perception and demographic factors were evaluated by the χ2 test, and the mean and SE values were estimated. To evaluate correlations among independent variables, Spearman correlation coefficients were calculated. Correlation coefficients among explanatory variables were all <0.5, which was regarded as not having multicollinearity.23 Variables were selected for inclusion by stepwise calculation of the Akaike information criterion. Moreover, to prevent multicollinearity, a test of variation inflation factors was performed for each analysis. To assess the associations of demographic factors, knowledge, trust in social organizations, intention to sacrifice, and responsiveness to emergency situations with risk perception, multiple linear regression analyses were used. Each question regarding risk perception was aggregated to produce a cumulative score indicative of the overall effect of risk perception. Prior to analysis, the variables were tested using a Q-Q plot to verify the normality of their distribution and—with the exception of knowledge—were confirmed to be continuous because the ordinal values differed only slightly from a normal distribution.24 Risk perception was estimated on a scale of 1-7, and its relationship with predictors was assessed. In addition, to identify the association of risk perception with overreaction to the epidemic and compliance with self-quarantine, multiple logistic regression analyses were performed. Odds ratios (ORs) were calculated for self-quarantine and overreaction. Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Risk perception
Sociodemographic variables and levels of risk perception are shown in Table 1 . More than half of the participants were men (57.01%), 24-26 years of age (30.54%), citizens of South Korea (95.51%), and postgraduate students (52.04%). A high frequency of risk perception was detected in women (n = 152; 52.6%), those 24-26 years of age (n = 97; 33.56%), students from South Korea (n = 281; 97.23%), and postgraduate students (n = 166; 57.44%). The mean knowledge score was 5.35 ± 1.41 out of 10. Therefore, respondents had approximately 53.5% of the essential knowledge about MERS. The mean score for trust in the medical profession was higher than those for other social components (3.63 ± 0.95); the mean score for trust in the central government was lowest (2.37 ± 1.03) (Table 2 ). In terms of the media section, the item regarding trust in newspapers was excluded from the analysis because of its lack of validity according to the variable selection process.
Table 1.
Risk perception by sociodemographic characteristics (N = 1,487)
| Characteristic | Risk perception | P value | ||||
|---|---|---|---|---|---|---|
| Total | Very low (Q1) | Low (Q2) | High (Q3) | Very high (Q4) | ||
| Sex | ||||||
| Male | 838(57.01) | 180(67.16) | 248(65.09) | 273(51.32) | 137(47.40) | <.0001 |
| Female | 632(42.99) | 88(32.84) | 133(34.91) | 259(48.68) | 152(52.60) | |
| Age (y) | ||||||
| 18-20 | 228(15.51) | 41(15.30) | 64(16.80) | 83(15.60) | 40(13.84) | .1092 |
| 21-23 | 362(24.63) | 64(23.88) | 113(29.66) | 128(24.06) | 57(19.72) | |
| 24-26 | 449(30.54) | 86(32.09) | 114(29.92) | 152(28.57) | 97(33.56) | |
| 27-30 | 253(17.21) | 46(17.16) | 55(14.44) | 102(19.17) | 50(17.30) | |
| ≥30 | 178(12.11) | 31(11.57) | 35(9.19) | 67(12.59) | 45(15.57) | |
| Country | ||||||
| South Korea | 1,404(95.51) | 254(94.78) | 361(94.75) | 508(95.49) | 281(97.23) | .4157 |
| Foreign | 66(4.49) | 14(5.22) | 20(5.25) | 24(4.51) | 8(2.77) | |
| Education | ||||||
| Undergraduate | 705(47.96) | 127(47.39) | 206(54.07) | 249(46.80) | 123(42.56) | .0245 |
| Graduate | 765(52.04) | 141(52.61) | 175(45.93) | 283(53.20) | 166(57.44) | |
NOTE. Values are n (%) or as otherwise indicated. Q, quantile.
Table 2.
Risk perception, knowledge, trust, and personal characteristics
| Characteristic | Mean | Median | SE |
|---|---|---|---|
| Risk perception | 3.14 | 3.14 | 0.58 |
| Knowledge* | 5.35 | 5.00 | 1.41 |
| Trust (media, television) | 2.69 | 3.00 | 0.97 |
| Trust (medical) | 3.63 | 4.00 | 0.95 |
| Trust (central government) | 2.37 | 2.00 | 1.03 |
| Trust (local government) | 2.63 | 3.00 | 0.96 |
| Trust (NGO) | 2.79 | 3.00 | 0.95 |
| Trust (society) | 2.45 | 2.00 | 0.86 |
| Trust (health policy) | 2.72 | 3.00 | 0.90 |
| Optimism (health policy) | 3.20 | 3.00 | 0.86 |
| Willingness to sacrifice† | 2.54 | 3.00 | 0.67 |
| Responsiveness to emergency‡ | 2.06 | 2.00 | 0.62 |
NGO, nongovernmental organization.
Ten-point scale.
Four-point scale.
Three-point scale.
Women had a higher risk perception score than men, not only overall (by 0.17/5 points; β = 0.17; P < .001), but also in all other risk perceptions from 1-7 (Table 3 ). Older age was negatively associated with risk perception 2 (concern over contracting MERS through indirect contact) (β = −0.07; P = .004) and positively associated with risk perceptions 4 (considering MERS to be more severe than other respiratory diseases) (β = 0.09; P < .001), 6 (concern over damage to the community because of MERS) (β = 0.05; P = .026), and 7 (future reemergence of MERS) (β = 0.06; P < .001). In addition, only risk perception 6 (damage to the community) was significantly positively associated with Korean ethnicity (β = 0.44; P < .001).
Table 3.
Factors that affect risk perception according to multiple regression
| Characteristic | Cumulative (overall) risk perception* | Riskperception 1 | Riskperception 2 | Riskperception 3 | Riskperception 4 | Riskperception 5 | Riskperception 6 | Riskperception 7 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | P value | β | P value | β | P value | β | P value | β | P value | β | P value | β | P value | β | P value | |
| (Intercept) | 2.64 | <.001* | 2.83 | <.001* | 2.74 | <.001* | 2.86 | <.001* | 1.82 | <.001* | 2.62 | <.001* | 2.32 | <.001* | 3.27 | <.001* |
| Female | 0.17 | <.001* | 0.10 | .037† | 0.18 | .002* | 0.15 | .005* | 0.25 | <.001* | 0.16 | .005* | 0.18 | <.001* | 0.15 | <.001* |
| Age (per 3-y increase)‡ | 0.02 | .086 | 0.00 | .860 | −0.07 | .004* | 0.02 | .271 | 0.09 | <.001* | −0.01 | .810 | 0.05 | .026† | 0.06 | <.001* |
| Korean | 0.11 | .111 | −0.04 | .727 | 0.27 | .050 | −0.02 | .866 | −0.05 | .706 | 0.07 | .591 | 0.44 | <.001* | 0.12 | .264 |
| Knowledge | 0.01 | .308 | 0.04 | .015† | −0.04 | .055 | 0.01 | .650 | 0.02 | .366 | −0.01 | .596 | 0.01 | .563 | 0.05 | .004* |
| Trust (media) | 0.06 | <.001* | 0.10 | <.001* | 0.03 | .360 | 0.08 | .018† | 0.07 | .019† | 0.06 | .083 | 0.11 | <.001* | −0.01 | .790 |
| Trust (medical) | −0.04 | .027† | 0.06 | .044† | −0.10 | .003* | −0.05 | .086 | −0.13 | <.001* | −0.04 | .172 | −0.04 | .146 | 0.05 | .085 |
| Trust (central government) | −0.05 | .014† | −0.06 | .076 | 0.01 | .711 | 0.01 | .714 | −0.02 | .566 | −0.09 | .022† | −0.11 | .002* | −0.10 | .002* |
| Trust (local government) | 0.04 | .046‡ | −0.03 | .376 | 0.07 | .075 | 0.00 | .991 | 0.03 | .433 | 0.10 | .006* | 0.08 | .012† | 0.02 | .566 |
| Trust (NGO) | 0.06 | <.001* | 0.09 | .001* | 0.03 | .330 | 0.08 | .008† | 0.13 | <.001* | −0.03 | .402 | 0.07 | .013† | 0.02 | .330 |
| Trust (society) | −0.03 | .211 | −0.03 | .372 | −0.02 | .593 | 0.01 | .876 | 0.04 | .270 | −0.03 | .408 | −0.11 | .002* | −0.04 | .265 |
| Trust (health policy) | −0.05 | .014† | 0.00 | .992 | −0.12 | .002* | −0.01 | .815 | −0.03 | .443 | −0.05 | .159 | −0.04 | .280 | −0.09 | .002* |
| Optimism (health policy) | −0.04 | .024† | −0.04 | .210 | −0.03 | .487 | −0.09 | .009† | −0.06 | .066 | −0.02 | .505 | 0.00 | .904 | −0.05 | .079 |
| Willingness to sacrifice | −0.06 | .004* | −0.11 | .003* | −0.07 | .112 | −0.09 | .022* | 0.01 | .818 | −0.10 | .018† | −0.06 | .125 | −0.03 | .363 |
| Responsiveness to emergency | 0.18 | <.001* | 0.16 | <.001* | 0.18 | <.001* | 0.22 | <.001† | 0.24 | <.001* | 0.06 | .191 | 0.27 | <.001* | 0.11 | .003* |
NGO, nongovernmental organization; Risk perception 1, “I think that I will contract MERS if I come into contact with a MERS patient”; Risk perception 2, “I think that I might contract MERS even if I do not come into contact with a MERS patient”; Risk perception 3, “My health will be severely damaged if I contract MERS”; Risk perception 4, “I think MERS is more severe than other respiratory diseases”; Risk perception 5, “Even if I fall ill with another disease, I will not go to the hospital because of MERS”; Risk perception 6, “MERS will inflict serious damage on my community”; Risk perception 7, “MERS may spread in Korea again someday.”
P < .01.
P < .05.
Minimum age, 18 years; maximum age, >30 years.
Knowledge
Knowledge influenced only risk perceptions 1 and 7. That is, knowledge was related to concern over contracting MERS through direct contact (β = 0.04; P = .015) and reemergence of MERS (β = 0.05; P = .004). Knowledge was associated with risk perception, which does not support the hypothesis of this work.
Trust in social organizations
Trust in the media (broadcasting) was positively associated with cumulative risk perception (β = 0.06; P < .001) and risk perceptions 1 (concern over contracting MERS through direct contact), 3 (severity of MERS), 4 (considering MERS to be more severe than other respiratory diseases), and 6 (concern over damage to the community because of MERS). However, trust in the medical profession (β = −0.04; P = .027) and the central government of South Korea (β = −0.05; P = .014) was negatively associated with overall risk perception. Risk perceptions 2 and 4 (relevant to disease traits) were related to trust in the medical profession. In addition, risk perceptions 5, 6, and 7 (relevant to community traits) were related to trust in the central government. In contrast, trust in local government (β = 0.04; P = .046) and NGOs (β = 0.06; P < .001) was positively associated with risk perception. Trust in local government and NGOs was associated with risk perceptions 5 and 6 and risk perceptions 1, 3, 4, and 6, respectively. Compared with the results for trust in the central government, those for trust in local government seemed to have similar effect sizes, but with a different direction of estimates. However, trust in NGOs was associated with the perception of the risk of transmission and that to personal health. This suggests that NGOs are believed to contribute to communities in various ways, including by providing medical services. Trust in society was not associated with the overall risk perception but was negatively associated with concern over damage to the community (β = −0.11; P = .002). Finally, trust in health policy was negatively associated with risk perception (β = −0.05; P = .014). Risk perceptions 2 and 7 were related to trust in the health policy of the government of South Korea.
Personal characteristics
Optimism about future health policy (β = −0.04; P = .024), willingness to sacrifice (β = −0.06; P = .004), and active responsiveness to an emergency (β = 0.18; P < .001) were associated with risk perception. Only risk perception 3 was associated with optimism regarding health policy (β = −0.09; P = .009). Willingness to sacrifice was negatively associated with risk perceptions 1, 3, and 5. In addition, responsiveness to an emergency was positively associated with risk perceptions 1, 2, 3, 4, 6, and 7. Therefore, respondents who were pessimistic about health policy and unlikely to sacrifice themselves in specific situations and respond actively to an emergency exhibited a higher perception of risk.
Self-quarantine and overreaction
ORs were calculated to estimate the associations among risk perception, knowledge, personal characteristics, and compliance with self-quarantine (Table 4 ). The proportions of men and women who indicated they would comply with the self-quarantine guideline were 82.7% and 87.2%, respectively. Women were more likely to comply with self-quarantine (OR, 1.50; 95% confidence interval [CI], 1.10-2.06; P = .010), as were older subjects (OR, 1.22; 95% CI, 1.01-1.46; P = .037) and those with a greater level of knowledge (OR, 1.22; 95% CI, 1.10-1.35; P < .001). Additionally, subjects with more trust in the medical profession (OR, 1.35; 95% CI, 1.14-1.60; P = .001) and those who were willing to sacrifice (OR, 1.50; 95% CI, 1.20-1.88; P < .001) and actively respond to emergencies (OR, 1.31; 95% CI, 1.03-1.67; P = .028) were also more likely to comply with a self-quarantine order.
Table 4.
Associations of risk perception, knowledge, and personal characteristics with self-quarantine
| Characteristic | Compliance with self-quarantine | ||
|---|---|---|---|
| Odds ratio | 95% CI | P value | |
| Female (vs male) | 1.50 | 1.10-2.06 | .010* |
| Age (per 3-y increase)† | 1.22 | 1.01-1.46 | .037* |
| Korean (vs foreigner) | 0.60 | 0.25-1.46 | .263 |
| Undergraduate (vs graduate) | 1.04 | 0.67-1.62 | .867 |
| Knowledge | 1.22 | 1.10-1.35 | <.001‡ |
| Trust (media) | 0.95 | 0.80-1.14 | .605 |
| Trust (medical) | 1.35 | 1.14-1.60 | .001‡ |
| Trust (central government) | 0.88 | 0.71-1.10 | .262 |
| Trust (local government) | 1.15 | 0.93-1.42 | .194 |
| Trust (NGO) | 1.03 | 0.87-1.22 | .730 |
| Trust (society) | 1.03 | 0.83-1.27 | .823 |
| Trust (health policy) | 0.96 | 0.78-1.17 | .654 |
| Optimism (health policy) | 1.13 | 0.93-1.37 | .228 |
| Willingness to sacrifice | 1.50 | 1.20-1.88 | <.001‡ |
| Responsiveness to emergency | 1.31 | 1.03-1.67 | .028* |
| Risk perception | 1.18 | 0.90-1.54 | .233 |
CI, confidence interval; NGO, nongovernmental organization.
P < .05
Minimum age, 18 years; maximum age, >30 years.
P < .01.
The proportions of positive responses to items about overreactions in one's own behavior (self-behavior) and overreactions in response to the behavior of others were 79.9% and 42.9%, respectively. Knowledge (OR, 0.90; 95% CI, 0.82-0.99; P = .037) and trust in society (OR, 0.81; 95% CI, 0.66-0.98; P = .029) were negatively associated with overreaction in self-behavior (Table 5 ). However, responsiveness to an emergency (OR, 1.32; 95% CI, 1.05-1.66; P = .016) and risk perception (OR, 2.80; 95% CI, 2.17-3.60, P < .001) were positively associated with overreaction in self-behavior.
Table 5.
Associations of risk perception, knowledge, and personal characteristics with overreaction in one's own behavior
| Characteristic | Overreaction (self) | ||
|---|---|---|---|
| Odds ratio | 95% CI | P value | |
| Female (vs male) | 1.20 | 0.90-1.60 | .212 |
| Age (per 3-y increase)* | 0.92 | 0.78-1.08 | .295 |
| Korean (vs foreigner) | 1.72 | 0.94-3.15 | .079 |
| Undergraduate (vs graduate) | 1.16 | 0.78-1.73 | .473 |
| Knowledge | 0.90 | 0.82-0.99 | .037† |
| Trust (media) | 1.17 | 0.99-1.37 | .060 |
| Trust (medical) | 0.95 | 0.81-1.11 | .529 |
| Trust (central government) | 1.08 | 0.89-1.31 | .428 |
| Trust (local government) | 1.06 | 0.88-1.28 | .516 |
| Trust (NGO) | 1.04 | 0.89-1.21 | .611 |
| Trust (society) | 0.81 | 0.66-0.98 | .029† |
| Trust (health policy) | 1.00 | 0.84-1.20 | .992 |
| Optimism (health policy) | 0.98 | 0.82-1.17 | .817 |
| Willingness to sacrifice | 0.95 | 0.78-1.17 | .646 |
| Responsiveness to emergency | 1.32 | 1.05-1.66 | .016† |
| Risk perception | 2.80 | 2.17-3.60 | <.001‡ |
CI, confidence interval; NGO, nongovernmental organization.
Minimum age, 18 years; maximum age, >30 years.
P < .05.
P < .01.
In terms of overreaction to the behavior of others (Table 6 ), Korean respondents (OR, 0.486; 95% CI, 0.28-0.84; P = .010), those with a greater level of knowledge (OR, 0.79; 95% CI, 0.73-0.86, P < .001), and those with a higher level of trust in the medical profession (OR, 0.70; 95% CI, 0.61-0.80, P < .001) were unlikely to overreact to the behavior of others. However, respondents with a higher level of trust in local government (OR, 1.19; 95% CI, 1.02-1.38; P = .024) and higher risk perception (OR, 1.86; 95% CI, 1.52-2.28, P < .001) were more likely to overreact to the behavior of others. Therefore, risk perception was associated with a change in behavior during an epidemic.
Table 6.
Associations of risk perception, knowledge, and personal characteristics with overreaction to the behavior of others
| Characteristic | Overreaction to behavior of others | ||
|---|---|---|---|
| Odds ratio | 95% CI | P value | |
| Female (vs male) | 1.03 | 0.83-1.29 | .777 |
| Age (per 3-y increase)* | 0.97 | 0.85-1.10 | .602 |
| Korean (vs foreigner) | 0.49 | 0.28-0.84 | .010† |
| Undergraduate (vs graduate) | 1.20 | 0.86-1.66 | .283 |
| Knowledge | 0.79 | 0.73-0.86 | <.001‡ |
| Trust (media) | 1.19 | 1.04-1.36 | .012† |
| Trust (medical) | 0.70 | 0.61-0.80 | <.001‡ |
| Trust (central government) | 1.01 | 0.86-1.18 | .949 |
| Trust (local government) | 1.19 | 1.02-1.38 | .024† |
| Trust (NGO) | 0.99 | 0.88-1.13 | .977 |
| Trust (society) | 1.01 | 0.86-1.19 | .894 |
| Trust (health policy) | 1.01 | 0.87-1.17 | .926 |
| Optimism (health policy) | 0.93 | 0.81-1.08 | .342 |
| Willingness to sacrifice | 0.92 | 0.78-1.09 | .325 |
| Responsiveness to emergency | 1.19 | 0.99-1.43 | .058 |
| Risk perception | 1.86 | 1.52-2.28 | <.001‡ |
CI, confidence interval; NGO, nongovernmental organization.
Minimum age, 18 years; maximum age, >30 years.
P < .05.
P < .01.
Discussion
The findings of this study indicate that risk perception is associated with various social factors. Risk perception was correlated with sex and the level of trust in social organizations. These findings indicate that risk perception interacts with demographic and personal attitudinal factors at a collective level, as previously suggested.25 Women had a higher risk perception than men. Trust in the media (television), local government, and NGOs exhibited positive associations with risk perception, whereas trust in central government, the medical profession, and health policy exhibited negative ones. These results suggest that people are aware of the different roles of central and local government.
Additionally, these results identify the types of determinant that affect whether people overreact when an infectious outbreak occurs. Women and those with low levels of trust in central government, the medical field, and health policy were more likely to overreact. On the other hand, people with high levels of trust in the media, local government, and NGOs may be hypersensitive when an EID outbreak occurs. Furthermore, the higher risk perception was associated with only overreaction, not compliance to self-quarantine. Hypersensitivity that leads to overreaction can be explained by perceived media dependency26; however, this may have been related only to television in this research. Moreover, differences in the effects of trust in central and local governments on risk perception may be explained by South Koreans' perceptions of the roles of these government bodies. Central and local governments do not always appear to smoothly coordinate the emergency response, and this may be related to ongoing challenges about decentralization from the central governmental system.27
Another important finding is related to the role of the media during a crisis. In this study, trust in the media positively affected risk perception and overreaction, supporting that the mass media influence perceptions of disasters and risks; however, they cannot change an epidemic event itself.4 Restrictions on the availability of information by the government can exacerbate the impact of a disaster, especially in the new media age, in which person-centered media is emphasized; this was the case in the 2003 SARS outbreak in China and the 2015 MERS outbreak in South Korea. Regardless of the political system (ie, even in democratic states), the absence of risk communication may yield unexpected results. Therefore, the World Health Organization outbreak guidelines11 regarding building public trust and establishing a transparent flow of information need to be followed.
Respondents in this study were moderately knowledgeable about MERS, possessing 53.5% of the essential knowledge. This finding may reflect a higher mean level of education of the respondents compared with the general population, but indicates that the public is not ignorant about environmental and health-related matters.28 From another point of view, this finding can be said to contradict the deficit model, which holds that the public lacks knowledge.29 On the emergence of a novel infectious disease, people tend to be receptive to health-related information conveyed by new media, including the Internet and mobile phones. For these reasons, the role of the mass media is particularly important because they usually provide widespread coverage of EIDs and convey information to the public.30 Furthermore, the level of knowledge about MERS was not associated with risk perception. This is not in agreement with a previous report of a correlation between knowledge and perception of the risk of nuclear explosions.31 Notwithstanding these considerations, knowledge of MERS was directly associated with overreaction and compliance with self-quarantine. This suggests that greater knowledge of unfamiliar diseases reduces the likelihood of undesirable behavior, which can lead to social problems.
Personal characteristics, including willingness to sacrifice and responsiveness to an emergency, were negatively and positively, respectively, associated with risk perception. In addition, while responsiveness to an emergency was associated directly with overreaction and compliance with self-quarantine, willingness to sacrifice was associated only with compliance with self-quarantine. Personal characteristics were associated with responsive behaviors; however, the reasons for these associations could not be determined. One possibility is nationalism. Individuals who regard nations as abstract communities with shared emotional bonds governed by rules and/or norms tend to be altruistic.32 Therefore, people in societies governed by established, systematic rules are less likely to exhibit unusual behaviors that may lead to social panic.
Moreover, inaccurate information is disseminated through social media platforms, such as Twitter, Facebook, and Google. The enormous influence of social media during the 2014-2015 Ebola outbreak in West Africa has led to exaggerated concerns even among the population in the United States with negligible risks.33 Indeed, the mass media can also incite panic, which is related to fear and antisocial behavior34; however, when they do their job properly, they can inform the public accurately about current conditions. Two studies in which a mobile health communication tool was used demonstrated the effectiveness of a social media–based approach in terms of changing vaccination behavior.35, 36 Furthermore, the provision of appropriate and timely public health information by social media and the mobile health tool could accelerate the detection of disease outbreaks and enhance the public's response,37 thereby minimizing adverse health and economic effects.38
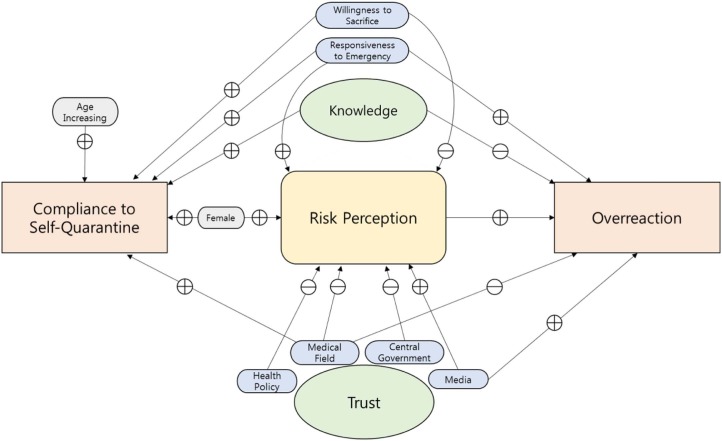
The findings of our study are depicted in schematic form in Figure 2 . In this model, risk perception was related to various factors such as sex, trust, and other personal characteristics. There was a notable aspect of risk perception: it was directly associated with overreaction, but not with compliance to self-quarantine. This suggests that risk perception motivates self-protective behavior, possibly resulting in overreaction. However, it does not automatically result in compliance to quarantine, which is generally perceived as protecting others, rather than oneself. In this sense, risk perception is a double-edged sword: at an optimal level, it helps the public protect themselves from infection and thereby deter the spread of epidemic; however, when excessive and characterized by fear, it can lead to other social problems, such as overreaction and discrimination. Sandman reported that risk perception is comprised of hazard and outrage.39 The MERS outbreak caused fear and anxiety among the population, which might have resulted in an overreaction to both the response of the government and the behaviors of themselves and others.40 Our model also points to the importance of trust in medical experts and proper knowledge. These 2 factors demonstrate the potential to maximize the benefit by promoting compliance and reducing overreaction. Therefore, risk communication should not just scare people, but should create a context in which there is trust and a flow of knowledge and clear information between the authorities and the public. These conditions should prevent adverse effects, particularly in democratic states. The existing literature emphasizes these essential components of risk management and risk communication.41, 42
Fig 2.
Relationships among risk perception, compliance, and overreaction.
To date, there are a limited number of studies on risk perception of infectious diseases (including MERS); therefore, this work makes an important contribution to the field. Several factors affecting perceived risk were evaluated (eg, trust in the media or health policy, personal characteristics), which were not assessed in previous studies. Although knowledge and trust have been previously reported to be associated with perceived risk,17, 18 this study further explored possible effects of risk perception and their implications in responding to an epidemic. EIDs are unfamiliar to the general public and are likely to be overestimated in the risk,31 possibly leading to social panic. To prevent this, it is important to boost the risk communication with fostering trust and relevant knowledge, which requires transparency.
This study had limitations. First, the survey involved students at a university; therefore, the participants might have different levels of concern about the epidemic compared with the general public. However, the participants represented the younger population with a homogeneous educational level with fewer confounding factors. Therefore, the findings were still likely meaningful for understanding the characteristics of risk perception in the essence. Second, the response rate was rather low (4.8%). Most online surveys have much lower response rates than person-to-person interviews.43 The students who had a greater perception of the risk might have been better motivated to participate in the study. Even if the associations found in this study may be weaker in a larger population, it is informative to identify the direction and structure of the interrelationships among the factors.
Future studies should investigate whether the findings from this study are applicable in more diverse populations. Furthermore, developing and testing more specific approaches to building trust and sharing knowledge during an epidemic would be needed. In responding to the public health emergency, collaboration is important among various social institutions, such as central and local governments, media, and medical community. More research is needed to explore the roles and relationships of these agents for effective risk communication.
In conclusion, risk perception was found to be associated with social trust and personal attitudes toward emergency situations in this study. Risk perception was associated with overreaction, possibly by fear-induced changes in behavior. However, knowledge about the nature of disease mitigated this possibility and enhanced compliance to quarantine guidelines. Understanding the determinants of risk perception contributes to effective communication. Building trust and sharing knowledge are important to ensure a rapid response to disease outbreaks, and to prevent unnecessary behaviors among members of the public.
Acknowledgments
We thank all members, Hye-rin Park, Jee-eun Yi, Kang-jin Kim, Nam-kyu Cho, Nara Lee, and Yunisa Astiarani who participated in conducting the survey together in Community Health Field Training, one of the programs of a Master's course at the Graduate School of Public Health. We also thank the supporting from BK21 Plus.
Footnotes
Funding/support: Supported by the Community Health Field Training Program, the Graduate School of Public Health, Seoul National University.
Conflicts of interest: None to report.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.ajic.2017.02.013.
Appendix. Supplementary data
The following is the supplementary data to this article:
Middle East respiratory syndrome questionnaire
References
- 1.Korea Centers for Disease Control and Prevention MERS portal. http://www.mers.go.kr/mers/html/jsp/main.jsp Available from. Accessed October 2016.
- 2.Penttinen P.M., Kaasik-Aaslav K., Friaux A., Donachie A., Sudre B., Amato-Gauci A.J., et al. Taking stock of the first 133 MERS coronavirus cases globally–Is the epidemic changing? Euro Surveill. 2013;18:1–5. doi: 10.2807/1560-7917.es2013.18.39.20596. [DOI] [PubMed] [Google Scholar]
- 3.Fung I.C., Tse Z.T., Chan B.S., Fu K.W. Middle East respiratory syndrome in the Republic of Korea: transparency and communication are key. Western Pac Surveill Response J. 2015;6:1–2. doi: 10.5365/WPSAR.2015.6.2.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma R. Media, crisis, and SARS: an introduction. Asian J Commun. 2005;15:241–246. [Google Scholar]
- 5.King G., Pan J., Roberts M.E. How censorship in China allows government criticism but silences collective expression. Am Polit Sci Rev. 2013;107:326–343. [Google Scholar]
- 6.Keane M., Donald S.H. Routledge; London, UK: 2014. Convergence, content industries and media governance. Media in China: consumption, content and crisis. [Google Scholar]
- 7.Tausczik Y., Faasse K., Pennebaker J.W., Petrie K.J. Public anxiety and information seeking following the H1N1 outbreak: blogs, newspaper articles, and Wikipedia visits. Health Commun. 2012;27:179–185. doi: 10.1080/10410236.2011.571759. [DOI] [PubMed] [Google Scholar]
- 8.Chew C., Eysenbach G. Pandemics in the age of Twitter: content analysis of Tweets during the 2009 H1N1 outbreak. PLoS ONE. 2010;5:e14118. doi: 10.1371/journal.pone.0014118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gesser-Edelsburg A., Shir-Raz Y. Routledge; New York (NY): 2016. Risk communication and infectious diseases in an age of digital media. [Google Scholar]
- 10.Cvetkovich G., Winter P.L. Trust and social representations of the management of threatened and endangered species. Environ Behav. 2003;35:286–307. [Google Scholar]
- 11.World Health Organization . WHO; Geneva, Switzerland: 2005. Outbreak communication: best practices for communicating with the public during an outbreak. [Google Scholar]
- 12.Fischhoff B., Bostrom A., Quadrel M.J. Risk perception and communication. Annu Rev Public Health. 1993;14:183–203. doi: 10.1146/annurev.pu.14.050193.001151. [DOI] [PubMed] [Google Scholar]
- 13.Renn O., Rohrmann B. Springer Science & Business Media; New York (NY): 2000. Cross-cultural risk perception: a survey of empirical studies. [Google Scholar]
- 14.Van der Pligt J. Risk perception and self-protective behavior. Eur Psychol. 1996;1:34–43. [Google Scholar]
- 15.Rohloff A., Wright S. Moral panic and social theory beyond the heuristic. Curr Sociol. 2010;58:403–419. [Google Scholar]
- 16.Sjöberg L. Factors in risk perception. Risk Anal. 2000;3:20–22. [PubMed] [Google Scholar]
- 17.Maswanya E.S., Moji K., Horiguchi I., Nagata K., Aoyagi K., Honda S., et al. Knowledge, risk perception of AIDS and reported sexual behaviour among students in secondary schools and colleges in Tanzania. Health Educ Res. 1999;14:185–196. doi: 10.1093/her/14.2.185. [DOI] [PubMed] [Google Scholar]
- 18.Van Damme W., Van Lerberghe W. Epidemics and fear. Trop Med Int Health. 2000;5:511–514. doi: 10.1046/j.1365-3156.2000.00599.x. [DOI] [PubMed] [Google Scholar]
- 19.Rubsamen N., Castell S., Horn J., Karch A., Ott J.J., Raupach-Rosin H., et al. Ebola risk perception in Germany, 2014. Emerg Infect Dis. 2015;21:1012–1018. doi: 10.3201/eid2106.150013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gesser-Edelsburg A., Shir-Raz Y., Hayek S., Lev O.S.B. What does the public know about Ebola? Am J Infect Control. 2015;43:669–675. doi: 10.1016/j.ajic.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 21.de Zwart O., Veldhuijzen I.K., Elam G., Aro A.R., Abraham T., Bishop G.D., et al. Perceived threat, risk perception, and efficacy beliefs related to SARS and other (emerging) infectious diseases: results of an international survey. Int J Behav Med. 2009;16:30–40. doi: 10.1007/s12529-008-9008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korea Centers for Disease Control and Prevention . Korea Centers for Disease Control and Prevention; Osong, South Korea: 2015. MERS response guideline 2015. [Google Scholar]
- 23.Shortell T. 2001. An introduction to data analysis & presentation.http://academic.brooklyn.cuny.edu/soc/courses/712/chap18.html Available from. Accessed April 4, 2016. [Google Scholar]
- 24.Rhemtulla M., Brosseau-Liard P.É., Savalei V. When can categorical variables be treated as continuous? A comparison of robust continuous and categorical SEM estimation methods under suboptimal conditions. Psychol Methods. 2012;17:354. doi: 10.1037/a0029315. [DOI] [PubMed] [Google Scholar]
- 25.Thomas R.K. Springer Science & Business Media; New York (NY): 2003. Society and health: sociology for health professionals. [Google Scholar]
- 26.Jackob N.G.E. No alternatives? The relationship between perceived media dependency, use of alternative information sources, and general trust in mass media. Int J Commun. 2010;4:18. [Google Scholar]
- 27.Kim S. Public trust in government in japan and south korea: does the rise of critical citizensmatter? Public Admin Rev. 2010;70:801–810. [Google Scholar]
- 28.Irwin A. Psychology Press; New York (NY): 1995. Citizen science: a study of people, expertise and sustainable development. [Google Scholar]
- 29.Dickson D. SciDev.Net. 2005. The case for a ‘deficit model’ of science communication; p. 27.http://www.scidev.net/global/communication/editorials/thecase-for-a-deficit-model-of-science-communic.html Available from. Accessed November 20, 2016. [Google Scholar]
- 30.Berry T.R., Wharf-Higgins J., Naylor P.J. SARS wars: an examination of the quantity and construction of health information in the news media. Health Commun. 2007;21:35–44. doi: 10.1080/10410230701283322. [DOI] [PubMed] [Google Scholar]
- 31.Sjoberg L., Drottzsjoberg B.M. Knowledge and risk perception among nuclear-power-plant employees. Risk Anal. 1991;11:607–618. doi: 10.1111/j.1539-6924.1991.tb00650.x. [DOI] [PubMed] [Google Scholar]
- 32.Stern P.C. Why do people sacrifice for their nations? Polit Psychol. 1995:217–235. [Google Scholar]
- 33.Fung I.C., Tse Z.T., Cheung C.N., Miu A.S., Fu K.W. Ebola and the social media. Lancet. 2014;384:2207. doi: 10.1016/S0140-6736(14)62418-1. [DOI] [PubMed] [Google Scholar]
- 34.Altheide D.L. Moral panic: from sociological concept to public discourse. Crime Media Cult. 2009;5:79–99. [Google Scholar]
- 35.Salathe M., Khandelwal S. Assessing vaccination sentiments with online social media: implications for infectious disease dynamics and control. PLoS Comput Biol. 2011;7:e1002199. doi: 10.1371/journal.pcbi.1002199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yoda L.U., Nahl D., Crosby M.E., Stage-based mHealth communication interventions for HPV education . 2013. Proceedings of the 2013 46th Hawaii International Conference on Science Systems. Wailea, Hawaii; January 7-10. [Google Scholar]
- 37.Kass-Hout T.A., Alhinnawi H. Social media in public health. Br Med Bull. 2013;108:5–24. doi: 10.1093/bmb/ldt028. [DOI] [PubMed] [Google Scholar]
- 38.Smith R.D. Responding to global infectious disease outbreaks: lessons from SARS on the role of risk perception, communication and management. Soc Sci Med. 2006;63:3113–3123. doi: 10.1016/j.socscimed.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sandman P.M. Springer; New York (NY): 1989. Hazard versus outrage in the public perception of risk. Effective risk communication. [Google Scholar]
- 40.Pangestu T. MERS-CoV outbreak in South Korea–public policy trumped by fear and politics. Asian J Public Aff. 2015;8:49–52. [Google Scholar]
- 41.Cvetkovich G., Lofstedt R.E. Routledge; New York (NY): 2013. Social trust and the management of risk. [Google Scholar]
- 42.Löfstedt R. Springer; New York (NY): 2005. Risk management in post-trust societies. [Google Scholar]
- 43.Nulty D.D. The adequacy of response rates to online and paper surveys: what can be done? Assess Eval High Educ. 2008;33:301–314. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Middle East respiratory syndrome questionnaire