Abstract
Background
Noncontact forehead temperature measurement by handheld infrared thermometer was used as a screening tool for fever. However, the accuracy data and normal range of forehead temperature determined by this method were not available.
Methods
The temperature readings from 3 handheld infrared thermometers were validated against an electronic thermometer. Normal range of forehead temperature was determined by measuring the forehead temperature in 1000 apparently healthy subjects.
Results
Significant differences were detected in readings obtained by the 3 different handheld infrared thermometers (analysis of covariance, P < .001) The most accurate one was chosen, and the normal range of forehead temperature in 1000 subjects detected by this method was 31.0°C to 35.6°C.
Conclusions
Our study shows that commercially available, handheld infrared thermometers require individual validation. Forehead temperature in excess of 35.6°C is suggestive of fever. Further studies are required to confirm accuracy of this value in detecting fever.
Severe acute respiratory syndrome (SARS) poses a serious threat to the general population. Fever is the cardinal sign in SARS.1 In 2003, noncontact forehead temperature (FT) measurement by handheld infrared thermometer (HIT) was introduced in Hong Kong hospitals for screening visitors for fever.2 HITs were used extensively in industrial process for temperature monitoring. Because of the noncontact nature of an HIT, FT measurement by HIT became a very popular means of infection control measure in various institutions in Hong Kong.
We found no literature related to the usage of an HIT to measure FT as a method of fever screening nor the normal range of the FT as determined by HIT. Thus, the current study was undertaken to investigate both the accuracy of using an HIT as a method of temperature measurement and to determine the normal range of FT.
Materials and methods
Accuracy of HIT as a thermometer of surface temperature
The HIT used in our hospital is a STANDARD ST-8812 (Standard Instrument, Guang Dong, China). We included 3 new HITs in this study. The 3 units of HITs were used to measure the surface temperature of a water bath, which ranged from 32°C to 42°C (98.6°F to 107.6°F), simultaneously against an electronic thermometer (MAXIMUMTHERMOMETER GT-131; Geratherm Medical AG, Geswchwenda, Germany). Measurement of surface temperature of the water bath by HIT and electronic thermometer was made directly from the surface of the water bath with no extra treatment (eg, addition of floating reflective device). The surface temperature of the water bath was estimated by HIT with assessment of the amount of infrared emission from the surface of water. All readings were obtained by a single observer. Regression analysis was done to determine the comparability of surface temperature measured by HIT and electronic thermometer. The units of HITs used for measurement were also entered into the regression model as a categoric covariance. The agreement of surface temperature determined by HIT and electronic thermometer was assessed by the method suggested by Bland and Altman.3 Ninety-five percent limits of agreement were reported.
Normal range of FT
After the validation of reading, we determined the normal range of FT measured by HIT. Staff and visitors of our hospital were invited to join the study. Subjects aged over 18 years and below 65 years were enrolled in this study. Individuals with a history of fever, ingestion of antipyretic, and immunization within the preceding 7 days or those with symptoms such as cough, runny nose, or sore throat were excluded. The HIT was placed 5 cm away from the center of the forehead and perpendicular to the forehead. FT was recorded when a steady reading was shown. We recorded the FT, sex, and race of the subjects. All temperature readings were measured by a single observer with the same HIT in an air-conditioned environment. The unpaired Student's t test was used to compare group means. Statistical analysis was performed with SPSS 10.0.1 (SPSS Inc., Chicago, IL). Approval was granted by the ethnic committee, and verbal consent was obtained from the subjects.
Results
Accuracy of HIT as a thermometer of surface temperature
The number of readings obtained by HIT 1, HIT 2, and HIT 3 were 24, 35, and 37, respectively. In these 96 pairs of readings, readings from HIT and electronic thermometer were convertible. (Simple linear regression, R2 = 0.892, P < .001) However, we detected a significant difference in HIT readings obtained by different HITs for a given surface temperature (analysis of covariance, F = 651.63, degree of freedom = 2, P < .001). For example, the surface temperatures detected by HIT1, HIT2, and HIT3 were 37.4°C (99.32°F), 35.4°C (95.72°F), and 36.0°C (96.80°F), respectively, for a known temperature of 35.6°C (96.08°F).
By using the method suggested by Bland and Altman3 for assessing agreement ( Fig 1), the average difference of electronic thermometer readings and HIT readings was 0.56°C (1.01°F) (95% limits of agreement were −1.00°C to 2.12°C or −1.8°F to 3.82°F). The difference of these 2 readings tended to increase with an increase of surface temperature as indicated by the significant positive correlation between the difference and the average values of these 2 readings. (Pearson's correlation, r = 0.301, P = .003) Each HIT tested in the current study had a different offset as shown by the lack of overlap of the 3 HIT delta-plots (Fig 1).
Fig 1.
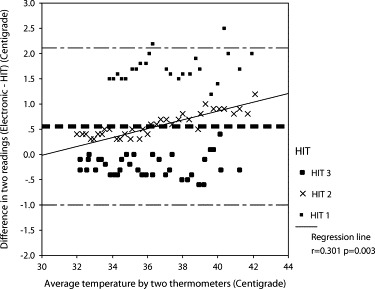
Difference against average of readings from HIT and electronic thermometer, with 95% limit of agreement (thin broken lines), mean difference (thick broken line), and regression line (solid line).
Normal range of FT
We selected an HIT with an average offset of 0.2°C (−0.36°F) from actual temperature to determine the normal range. We made 1000 observations with equal sex distribution. All subjects were Chinese.
The mean FT was 33.3°C ± 1.18°C (91.94°F ± 2.12°F). The histogram showing the frequency distribution of FT measured by HIT was showed in Fig 2. The normal range for FT was 31.0°C to 35.6°C (87.8°F to 96.1°F) (mean ± 1.96° standard deviation). Those with FT higher than 35.6°C were statistically abnormal. Mean FT of female group (33.4°C, 92.1°F) and male group (33.3°C, 91.94°F) were similar (Unpaired Student's t test, P = .22).
Fig 2.
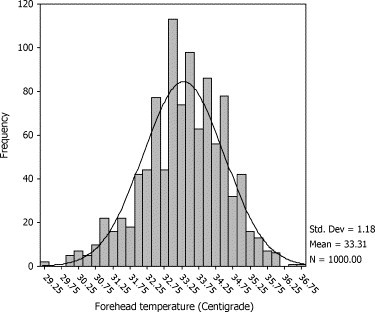
Histogram showing the frequency distribution of forehead temperature in 1000 apparently healthy adults.
Discussion
Despite its popularity, no normal values or accuracy data of noncontact measurement of FT by HIT were published in literature. In previous studies, FT was measured by different methodologies that required physical contact with the forehead. Nearly all studies found that FT was not accurate enough for fever detection.4, 5, 6, 7, 8, 9, 10
For the same surface temperatures detected by electronic thermometers, the discrepancies of surface temperatures detected by the 3 HITs could be as high as 2°C (3.6°F). Such discrepancies could lead to inaccurate and misleading recordings during disease surveillance. Institutions using similar equipment for fever screening should check the offsets before introducing them to clinical usage because each HIT may have a unique offset (Fig 1). The problems with the inaccurate readings in our study were not likely because of observer error because a single observer was deployed in this study. Hence, our study data suggested that the current brand of HIT was not accurate enough for clinical purpose. Further improvement in the quality of the product is required, and other similar HITs for assessment of FT require further studies.
With the most accurate HIT in our possession, the current study came up with a normal range of FT (31.0°C to 35.6°C or 97.8°F to 96.1°F). We suggest further studies with a larger population with different brands of handheld thermometers to confirm that forehead temperatures >35.6°C (>96.1°F) are indicative of fever. We caution readers to extrapolate this normal range to other age populations because different normal ranges of tympanic temperature in neonates, children, and adults were previously reported.11
In conclusion, our study shows that commercially available, handheld infrared thermometers require individual validation. Forehead temperature in excess of 35.6°C (96.1°F) is suggestive of fever. Further studies are required to confirm accuracy of this value in detecting fever.
Hong Kong
References
- 1.WHO Severe Acute Respiratory Syndrome (SARS) Wkly Epidemiol Rec. 2003;78:86. [PubMed] [Google Scholar]
- 2.SARS Expert Committee. SARS Expert Committee Report, appendix III, chronology of the SARS epidemic in Hong Kong. Available from: http://www.sars-expertcom.gov.hk/textonly/english/reports/reports/files/e_full_text.pdf. Accessed November 26, 2003.
- 3.Bland J.M., Altman D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;i:307–310. [PubMed] [Google Scholar]
- 4.Callanan D. Detecting fever in young infants: reliability of perceived, pacifier, and temporal artery temperatures in infants younger than 3 months of age. Pediatr Emerg Care. 2003;19:240–243. doi: 10.1097/01.pec.0000086231.54586.15. [DOI] [PubMed] [Google Scholar]
- 5.Alves J.G., Correia Jde B. Ability of mothers to assess the presence of fever in their children without using a thermometer. Trop Doct. 2002;32:145–146. doi: 10.1177/004947550203200308. [DOI] [PubMed] [Google Scholar]
- 6.Nwanyanwu O.C., Ziba C., Redd S.C., Luby S.P. Palpation as a method of fever determination in Malawian children who are less than 5 years old: how reliable is it? Ann Trop Med Parasitol. 1997;91:359–363. doi: 10.1080/00034989760978. [DOI] [PubMed] [Google Scholar]
- 7.Lewit E.M., Marshall C.L., Salzer J.E. An evaluation of a plastic strip thermometer. JAMA. 1982;247:321–325. [PubMed] [Google Scholar]
- 8.Scholefield J.M., Gerber M.A., Dwyer P. Liquid crystal forehead temperature strips: a clinical appraisal. Am J Dis Child. 1982;136:198–201. doi: 10.1001/archpedi.1982.03970390012002. [DOI] [PubMed] [Google Scholar]
- 9.Suleman M., Doufas A.G., Anka O., Ducharme M., Sessler D.I. Insufficiency in a new temporal-artery thermometer for adult and pediatric patients. Anesth Analg. 2002;95:67–71. doi: 10.1097/00000539-200207000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Ostrowsky B., Ober J., Wenzel R., Edmond M. The case of the cold thermometers. Am J Infect Control. 2003;31:57–59. doi: 10.1067/mic.2003.10. [DOI] [PubMed] [Google Scholar]
- 11.Chamberlain J.M., Terndrup T.E., Alexander D.T., Silverstone F.A., O'Donnell R., Grander J. Determination of normal ear temperature with an infrared emission detection thermometer. Ann Emerg Med. 1995;25:15–20. doi: 10.1016/s0196-0644(95)70349-7. [DOI] [PubMed] [Google Scholar]


