Abstract
Background
Inclusion of reusable respirators, such as elastomeric half-face respirators (EHFRs) and powered air-purifying respirators (PAPRs), in hospital respiratory protection inventories may represent 1 solution to the problem of N95 respirator shortages experienced during pandemics. User acceptance of these devices is 1 potential barrier to implementing such a strategy in respiratory protection programs.
Methods
To assess user attitudes toward various respirators, health care workers enrolled in respiratory protection programs in a medical system using EHFRs, N95s, and PAPRs and completed an online questionnaire that addressed attitudes, beliefs, and respirator preferences under different risk scenarios. Responses were compared between user groups.
Results
Of 1,152 participants, 53% currently used N95s, 24% used EHFRs, and 23% used PAPRs. N95 users rated their respirators more favorably compared with EHFR and PAPR users (P < .001) regarding comfort and communication, however, EHFR users rated their respirators much more highly regarding sense of protection (P < .001). For all user groups, reusable respirators were significantly more likely (odds ratios 2.3-7.7) to be preferred over N95 filtering facepiece respirators in higher risk scenarios compared to “usual circumstance” scenarios.
Conclusions
Despite somewhat less favorable ratings on comfort and communication, experienced EHFR and PAPR users still prefer reusable respirators over N95s in certain higher risk scenarios. This suggests that reusable respirators are an acceptable alternative to N95 respirators in health care and offer 1 viable solution to prevent pandemic-generated respirator shortages.
Key Words: Elastomeric respirator, N95 respirator, Powered air-purifying respirator, Comfort, Preference, Protection
Health care workers (HCWs) face potentially hazardous occupational exposures to infectious organisms, many of which are spread through an airborne or aerosol route.1 In these situations, respirators are required as 1 of the mechanisms to protect HCWs from exposure. Conventionally, most health care settings employ the use of N95 filtering facepiece respirators (N95-FFRs) to protect their HCWs.2 These respirators are meant to be disposable, provide protection against 95% of airborne particles as low as 0.3 microns in size, and rely on creation of a seal between the HCW's face and the mask.3 N95-FFRs have been used in health care to protect HCWs from exposure to various pathogens, including tuberculosis (TB), severe acute respiratory syndrome (SARS) coronavirus, and others.1
Over the last 20 years, all major infectious disease pandemic threats have prompted the use of respiratory protection as 1 element of a comprehensive approach to minimize risk of transmission to HCWs caring for infected patients. These events created a high demand for N95-FFRs and led to local, or even global, shortages in every case.4, 5 During the SARS 2002 outbreak, 25% of respondents at a facility that treated at least 1 possible or confirmed SARS case experienced N95-FFR shortages.4 With the 2009 H1N1 influenza pandemic, hospital managers r eported shortages and many HCWs reported that N95-FFRs were not readily available.5 The 2014 Ebola pandemic led to actual and perceived shortages of personal protective equipment overall.6, 7, 8, 9 These shortages left HCWs less protected and, therefore, more vulnerable to the risk of occupationally acquired infection.
Current respirator manufacturer and distributor supply chain flow structure may lead to future shortages with high product demand periods, such as those occurring during global pandemics.10 As expressed by a major US respirator distributor representative to a committee of the National Academies of Science in 2016 (previously known as the Institute of Medicine [IOM]), the order of magnitude of increased use of and, therefore, demand for respirators to prevent airborne pathogen transmission “is so great that none of the traditional supply chain strategies that are available would ever be sufficient to meet the demand and the expectations that our 6,000 or so health care customers would have.”10
Proposed solutions to addressing N95-FFR shortages include stockpiling of these respirators and permitting extended and limited reuse of these often single-use disposable respirators in some cases. However, each of these solutions also has drawbacks or violates other infection control precepts.5 , 11, 12, 13, 14, 15 An additional solution to this challenge of providing adequate respiratory devices during a national or global outbreak would be to include the use of reusable respirators as part of a facility-based supply.
In this approach, reusable respirators would be assigned and fit tested for each HCW and already be present and available when required. Because they are reusable, they would not be disposed of after use and, therefore, would not contribute to creating a supply shortage, mitigating a demand for new respirators. One such alternative product is the reusable elastomeric half-face respirator (EHFR), a tight-fitting device with the same assigned protection factor (APF) as an N95-FFR.16 Another example is a powered air-purifying respirator (PAPR), a loose-fitting device with a higher APF than an N95-FFR.16
Although EHFRs are often used in other industries outside of health care (eg, manufacturing or construction) where significant airborne hazards are present, they are less familiar to most HCWs.16 These devices are somewhat larger than N95-FFRs, made of synthetic materials such as silicone, and contain filter-bearing cartridges. Their size and appearance present challenges to user acceptance, given this unfamiliarity and perceptions related to possible discomfort during use, difficulty with communication, interference with work tasks, and potential fear experienced by patients.17
Yet, some health care settings have used EHFRs as part of their routine or emergency protocols for respiratory protection.2 , 18, 19, 20 Understanding the experience of workers in these environments would provide insight quantifying the potential concerns about user acceptance and could guide actions to best address these concerns.
Loose-fitting PAPRs are often used as alternatives to N95-FFRs among HCWs, who typically are unable to wear a tight-fitting N95-FFR, whether because of their inability to obtain an acceptable fit (eg, the presence of facial hair or facial structure) or because of a medical inability to wear a tight-fitting mask. In addition, loose-fitting PAPRs are appropriate when fit testing has not occurred, and some health care facilities may exclusively rely on PAPRs as their primary form of respiratory protection to avoid the need for fit testing. PAPRs are recommended for use during certain high-hazard tasks, such as aerosol-generating procedures in patients suspected to have an aerosol-transmissible disease, as they provide a higher level of protection (APF ≥ 25) and have an added benefit of including facial protection.21 These features may make PAPRs a preferred from of respiratory protection during pandemics. Although loose-fitting PAPR use does not require fit testing, training that includes appropriate donning, doffing, and use technique is still required. PAPRs have higher initial costs and may require use of product-specific auxiliary components, such as hoods. In health care, PAPR hoods are often reused among individuals for care of specific patients, but frequently are disposed of subsequently. A 2015 survey of US occupational health nurses revealed that 77% had used PAPRs in their health care facilities over the past year.2 Therefore, PAPR users represent an important group whose comparative preferences should also be examined to understand acceptance of these devices in health care.
One hospital setting, with more than 5,000 employees enrolled in its respiratory protection program (RPP), has used EHFRs as 1 form of respiratory protection since the 2009 H1N1 pandemic, when they were incorporated into the RPP for several reasons, including (1) N95-FFR shortages that ensued subsequent to requirements by the Occupational Safety and Health Administration (OSHA) for use during care for patients with pandemic influenza-like illness,22 and (2) professional expertise by the occupational safety staff, who were familiar with the respirators from previous employment outside of health care.19 In the fall of 2016, HCWs from this facility and its affiliated institutions were surveyed about their experiences with the use of respirators. The primary objective of this study was to understand whether EHFRs are acceptable alternatives to N95-FFRs among HCWs based on user preferences and perceptions of comfort, communication, and protection afforded by the mask. The secondary objective was to understand similar user acceptability outcomes about PAPRs compared to N95-FFRs. This study sought to determine whether regular EHFR and PAPR users have different preferences, when given a choice of respirator, and to compare respirators with respect to comfort, communication, and sense of protection from disease, compared to regular N95-FFR users.
Methods
Setting
A cross-sectional survey was conducted of HCWs enrolled in RPPs at 5 sites within a single medical system, where collectively 3 different forms of respiratory protection (N95-FFR, EHFR, and PAPR) were in use. Partner sites were recruited, after conversations with directors of employee health, safety, and their supervising leadership. Site A was a large, urban teaching hospital where all 3 forms of respiratory protection were in use during the study period. Sites B and D were suburban and urban community hospitals, respectively, where the primary form of respiratory protection was N95-FFR. Site C was a suburban rural-based community hospital, where the primary form of respiratory protection used was PAPR. Site E was a collection of urban ambulatory practices affiliated with site A, where the primary form of respiratory protection was EHFR. Each site had existing RPP policies and procedures for training and fit testing as needed that complied with the OSHA Respiratory Protection Standard (29 CFR 1910.134). The study was approved by the University of Maryland-Baltimore institutional review board.
Survey design
The survey feedback was provided by HCWs who participated in a focus group about respiratory protection during an earlier qualitative phase of this study.19 Additionally, survey questions designed to address issues raised by RPP leadership during key informant interviews also performed in this earlier qualitative study phase were included.19 Additional questions focused more generally about respiratory protection were included that were adapted from prior respiratory protection surveys and research, including the National Institute for Occupational Safety and Health Respirator Use Evaluation in Acute Care Hospitals study and from research conducted by the Workers’ Compensation Board of British Columbia.17, 23
An online survey consultant administered and hosted the survey. The draft survey was converted into a web-based platform and then pilot-tested for readability, ease of use, and length. After incorporation of revisions after pilot-testing, the survey was structured to take 15-20 minutes to complete, able to be completed in intervals, and accessible in multiple browser options, both on desktop and mobile electronic options devices.
Recruitment and survey deployment
To facilitate recruitment, study team members made announcements at nursing unit shift changes, unit “huddles,” academic divisional meetings, and at nurse managers meetings, describing the purpose of the survey, the voluntary nature of completion, and the method of survey dissemination. Flyers were also posted on bulletin boards in common areas in nursing units. Participants who completed the survey received $20 electronic gift cards as reimbursement for their participation.
The study team obtained rosters of HCWs included in the RPP at each of the 5 sites with their e-mail addresses, when available. The online survey consultant delivered individual messages to all e-mail addresses included on the RPP rosters. The content included (1) an introductory e-mail, announcing the forthcoming, voluntary survey, (2) an invitation e-mail containing a personalized link to the survey, and (3) up to 3 reminder e-mails over a 6-week period to those participants who had not completed the survey. Incorrect or incomplete e-mail addresses were resolved if possible on a case-by-case basis, but represented only a small portion of the e-mail addresses (<1%).
Because some HCWs did not have e-mail addresses on file with employee health rosters, study staff also scheduled clinical unit visits with study-supplied laptops to facilitate on-site survey completion. Clinical units that historically had been designated to use EHFRs were prioritized (emergency department, medical intensive care unit, medicine and pediatric units, respiratory therapy, radiology, and phlebotomy units). The study staff visited clinical units at 3 of the 5 participating sites: A, C, and D. At sites where e-mail addresses were available for all HCWs on RPP rosters (sites B and E), the study staff did not visit units to facilitate on-site completion.
The survey was administered over a 6-week period between August 2016 and October 2016. Participants were eligible to complete the survey if they were assigned to wear a respirator, they were at least 18 years old, they had worked for their current employer for at least 3 months, and if they had worn a respirator at least once in the last year outside of training.
At the time of study design, approximately 35% of site A's and site E's RPP participants (the only locations where EHFRs were in use) were assigned to use EHFRs, with only 2.5% in N95-FFRs and the remaining 62.5% in PAPR. As the primary objective of the study was to compare attitudes and beliefs of EHFR users to N95-FFR users, HCWs from additional sites primarily using N95-FFRs were recruited, and EHFR users were oversampled. The study budget was structured to provide participant payments to 1,000 survey respondents, and enrollment was structured to end after recruitment of 1,000 respondents.
Early survey data feeds after the first week of e-mail distribution revealed that no participants from site C had accessed the survey. We learned that an organizational “spam” filter was active and impeding the ability of that site's participants to complete the survey. This created an unfair advantage to participants at the other 4 sites in being able to complete the survey before the recruitment limit of 1,000 was reached. After problem resolution in collaboration with the site's information technology staff and after institutional review board approval, enrollment was extended for an additional 2 weeks specifically at the site that had faced a systemic e-mail blockade. Thus, total participation exceeded 1,000 because of this unexpected issue.
The electronic survey was sent to the e-mail addresses of 9,687 HCWs among the 5 institutions. A total of 1,152 participants completed the survey, yielding a total participation rate of 12%.
Data analysis
Analyses compared current EHFR users, current N95-FFR users, and current PAPR users (user groups). Differences in frequency of responses for categorical variables among these groups were tested using the Pearson χ² test. For continuous variables, we used analysis of variance to look for significant differences between the groups. Demographic variables found to be significantly different between the 3 groups were included as covariates in subsequent multivariable group comparisons about comfort, communication, sense of protection, and confidence in fit testing and training outcomes, along with other variables thought to be important in influencing responses. These covariates included sex, age, race, education level, site, job category, primary unit setting, frequency of use, frequency of training, years worked in health care, years worked for current employer, assigned respirator, respirator status prior to the 2009 H1N1 pandemic, and supervisor status.
For the 5-point Likert-type scale questionnaire responses, 2 different types of analyses were performed. First, the distribution of responses between the 3 groups were compared with unadjusted means and standard deviations and graphically using diverging stacked bar charts, with the neutral point centered at 0. Second, to formally compare differences between groups, 5-point Likert scale responses were analyzed as continuous variables, ranging from 1 (representing the most negative response) to 5 (representing the most positive response). An overall F test from analysis of covariance was used to identify whether there were any significant differences between the groups while adjusting for covariates, followed with pairwise comparisons using Tukey's honestly significant difference tests.
Finally, preferences for respirator types (3 options) under different threat levels were compared within 3 respirator user groups. First, for each group, the percentage of the group endorsing a respirator preference was calculated under different threat-level scenarios: (1) rule-out TB, also considered “usual circumstances,” (2) active TB, and (3) pandemic H1N1 influenza or SARS. Then, multinomial logistic regression modeling was used to estimate the relative odds of preferring EHFR and PAPR (vs N95-FFR) between 2 increased threat-level scenarios versus the usual circumstances scenario. Generalized estimating equations were used for this analysis to account for intraindividual correlation of responses to the 3 threat scenario questionnaire items.
For the data analysis of preferences within each user group, the number of covariate terms in each generalized estimating equation multinomial regression model was limited by the distribution of the 3-level categorical outcome. Following guidelines outlined in Babyak24 and Harrell,25 we determined overall that the maximum number of covariate terms would ideally be no more than 12. We devised a strategy to: (1) identify a potentially critical set of covariates, (2) collapse categorical covariates where stratification was not critical, and (3) fit the regression models and reduce the number of covariate terms to a maximum of 12 (highest P values first), as long as there was a <10% change in the beta coefficients of interest (ie, for threat scenario). The a priori identified initial critical set of covariates were: age, sex, race (white or nonwhite), assigned respirator, employer (binary), primary unit (3 levels), job category (3 levels), percent of time wearing a respirator (3 levels), and years working in health care. The maximum change in the beta coefficients for threat level from covariate reduction in the 3 user group models was 1.4%
Analyses were conducted using SAS version 9.4 (SAS Institute Inc, Cary, NC). Diverging stacked bar charts were constructed using R software (R Foundation for Statistical Computing, Vienna, Austria) HH.26
Results
Eleven hundred fifty-two participants completed the survey, 280 of whom were currently using EHFRs. The majority of participants in each group were women. Current EHFR users differed from current N95-FFR users and PAPR users by several demographic and occupational characteristics as shown in Table 1 .
Table 1.
Demographic and occupational characteristics of EHFR, N95-FFR, and PAPR users (N = 1,152)
| N and % of user group† |
||||||||
|---|---|---|---|---|---|---|---|---|
| EHFR users |
N95-FFR users |
PAPR users |
||||||
| Characteristic | N = 280 | 24% | N = 606 | 53% | N = 266 | 23% | P value* | |
| Sex | .033 | |||||||
| Female | 239 | 85% | 484 | 80% | 204 | 77% | ||
| Age (y) | .198 | |||||||
| <30 | 93 | 33% | 164 | 27% | 87 | 33% | ||
| 30-40 | 91 | 33% | 206 | 34% | 73 | 27% | ||
| 40+ | 96 | 34% | 236 | 39% | 106 | 40% | ||
| Race‡ | .002 | |||||||
| Black/African American | 68 | 24% | 126 | 21% | 33 | 12% | ||
| White | 175 | 63% | 366 | 60% | 185 | 70% | ||
| All others | 37 | 13% | 114 | 19% | 48 | 18% | ||
| Job category | <.001 | |||||||
| RN | 131 | 47% | 256 | 42% | 165 | 62% | ||
| RT | 20 | 7% | 36 | 6% | 9 | 3% | ||
| Provider (attending or resident Dr, NP, PA) | 24 | 9% | 162 | 27% | 30 | 11% | ||
| Pt support/other§ | 105 | 38% | 152 | 25% | 62 | 23% | ||
| Site | <.001 | |||||||
| A | 226 | 81% | 411 | 68% | 193 | 73% | ||
| B | 6 | 2% | 109 | 18% | 6 | 2% | ||
| C | 1 | 0% | 33 | 5% | 56 | 21% | ||
| D | 1 | 0% | 40 | 7% | 4 | 2% | ||
| E | 46 | 16% | 13 | 2% | 7 | 3% | ||
| Primary unit setting | <.001 | |||||||
| Higher risk inpatient units | 186 | 66% | 318 | 52% | 86 | 32% | ||
| Lower risk inpatient units | 22 | 8% | 183 | 30% | 152 | 57% | ||
| Radiology/lab | 37 | 13% | 49 | 8% | 6 | 2% | ||
| Ambulatory | 27 | 10% | 21 | 3% | 8 | 3% | ||
| Nonfixed | 8 | 3% | 35 | 6% | 14 | 5% | ||
| Percentage of time wearing a respirator | .019 | |||||||
| 0%-1% | 124 | 44% | 326 | 54% | 147 | 55% | ||
| 1%-10% | 99 | 35% | 199 | 33% | 84 | 32% | ||
| >10%-25% | 57 | 20% | 81 | 13% | 35 | 13% | ||
| Tenure | mean in y (SD) | P value¶ | ||||||
| Worked in health care (y) | 12.04 | (9.98) | 13.94 | (10.90) | 13.96 | (11.43) | <.001 | |
| Worked for current employer (y) | 7.14 | (8.11) | 8.17 | (9.34) | 9.01 | (9.04) | .075 | |
Dr, doctor; EHFR, elastomeric half-face respirator; lab, laboratory; N95-FFR, N95 filtering facepiece respirator; NP, nurse practitioner; PA, physician's assistant; PAPR, powered air-purifying respirator; PT, patient; RN, registered nurse; RT, respiratory therapist.
Calculated using the Pearson χ² test.
Total may be >100 because of rounding.
Hispanic evaluated by ethnicity, not race. No significant differences among groups. There were only 35 total participants who were Hispanic.
Patient support includes patient care technicians, nurse's aides, speech/occupational/physical therapists, licensed vocational nurses, housekeeping, maintenance/facilities/safety staff, pharmacy staff, and administration/management staff.
Calculated using analysis of variance.
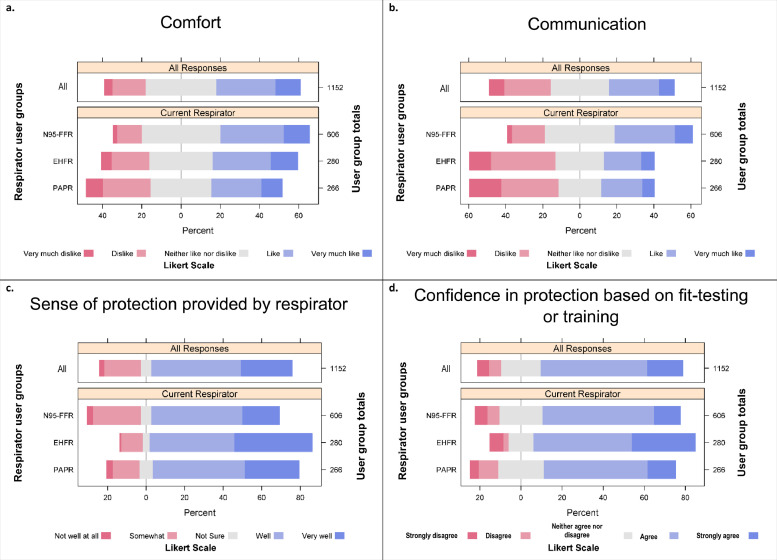
When asked, “With regard to comfort, how much do you like your respirator?” most responses were neutral to favorable (Fig 1 Panel a). N95-FFR users rated their respirators significantly more favorably than did either EHFR (P < .001) or PAPR users (P < .001) (Table 2 ). Similarly, when asked “With regard to communication, how much do you like your respirator?” N95-FFR users again rated their respirators more favorably in comparison to EHFRs (P < .001) or PAPRs (P < .001), which were both rated similarly in the neutral to negative categories (Fig 1 Panel b and Table 2).
Fig 1.
Likert scale responses of respirator users regarding how much they liked the comfort of the respirator (Panel a), communication while wearing the respirator (Panel b), how well they believe the respirator protects them (Panel c), and how confident they were that the respirator would protect them based on their fit testing or respirator training experiences (Panel d).
Table 2.
Mean Likert scale responses about respirator attributes among user groups, N = 1,152
| EHFR users (N = 280) | N95-FFR users (N = 606) | PAPR users (N = 266) | Overall comparison* | |
|---|---|---|---|---|
| Respirator attribute | mean (SD) | mean (SD) | mean (SD) | Unadjusted P value |
| Comfort | ||||
| How much do you like your respirator? † | ||||
| 3.28 (1.08) | 3.42 (0.93) | 3.06 (1.12) | <.001 | |
| Communication | ||||
| How much do you like your respirator?† | ||||
| 2.76 (1.1) | 3.29 (0.94) | 2.70 (1.18) | <.001 | |
| Sense of protection | ||||
| How well do you think your respirator protects you?‡ | ||||
| 4.12 (0.97) | 3.55 (1.15) | 3.84 (1.08) | <.001 | |
| Confidence from training or fit testing | ||||
| I am confident that my respirator will protect me based on the fit testing or training I have gone through.§ | ||||
| 3.94 (1.05) | 3.62 (0.98) | 3.60 (0.98) | <.001 | |
EHFR, elastomeric half-face respirator; N95-FFR, N95 filtering facepiece respirator; PAPR, powered air-purifying respirator.
Significance level unchanged after adjustment for sex, race, education level, employer, assigned respirator, respirator status prior to 2009 H1N1 pandemic, unit setting, supervisor status, frequency of use, frequency of training, years in health care.
1 = “very much dislike,” 2 = “dislike,” 3 = “neither like nor dislike,” 4 = “like,” and 5 = “very much like.”
1 = “not well at all,” 2 = “somewhat,” 3 = “not sure,” 4 = “well,” and 5 = “very well.”
1 = “strongly disagree,” 2 = “disagree,” 3 = “neither agree nor disagree,” 4 = “agree,” and 5 = “strongly agree.”
In contrast, when participants were asked “How well do you think your respirator protects you?” EHFR users rated their respirators most favorably (Fig 1 Panel c and Table 2). Both EHFR (P < .001) and PAPR users (P = .012) rated their respirators significantly more favorably than did N95-FFR users. EHFR users were more confident that their respirator would protect them based on their fit testing or training in contrast to either N95-FFR users (P = .003), who would require similar fit testing, or in comparison to PAPR users (P = .005), who still require training despite not needing to undergo fit testing (Fig 1 Panel d and Table 2). Multivariable analysis, including adjustment for frequency of fit testing or training, did not decrease the significance level of these comparisons.
To understand respirator preference and the impact of escalated threat levels on preference, users were asked to select their preferred respirator given 3 choices (EHFR, N95-FFR, or PAPR). First, the question, “What respirator would you prefer to wear under usual circumstances, such as caring for a patient who is being ruled-out for TB?” was asked. The risk scenario was then escalated to caring for a patient with known, active TB and finally to a setting of pandemic H1N1 or SARS. The majority of each user group preferred to stay with their current respirator type under usual circumstances (Table 3 ). As risk increased to exposure to active TB, however, the percentage staying with or switching to EHFR or PAPR increased in each user group. When exposure was to pandemic H1N1 or SARS, the propensity to stay with or switch to EHFR was not as strong as with exposure to active TB, but propensity to prefer PAPR was higher. For all user groups, reusable respirators were significantly more likely to be preferred over N95-FFRs in higher risk scenarios compared to usual circumstance scenarios (Table 4 ). Adjustment for covariates increased the odds of preferring either EHFR or PAPR compared to N95-FFR in all user groups and in each threat scenario compared to usual circumstances.
Table 3.
Preferences for respirator type under hypothetical risk scenarios (unadjusted)
| Current EHFR users (N = 280) | Current N95-FFR users (N = 606) | Current PAPR users (N = 266) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Preferred respirator |
Preferred respirator |
Preferred respirator |
|||||||
| Scenario | EHFR | N95-FFR (%) | PAPR | EHFR | N95-FFR (%) | PAPR | EHFR | N95-FFR (%) | PAPR |
| Rule out TB (usual circumstance) | |||||||||
| 56 | 37 | 6 | 11 | 78 | 12 | 10 | 40 | 50 | |
| Active TB | |||||||||
| 69 | 15 | 16 | 29 | 44 | 28 | 16 | 18 | 66 | |
| Pandemic H1N1 or SARS | |||||||||
| 61 | 18 | 21 | 23 | 46 | 31 | 18 | 21 | 62 | |
EHFR, elastomeric half-face respirator; N95-FFR, N95 filtering facepiece respirator; PAPR, powered air-purifying respirator; TB, tuberculosis; H1N1, H1N1 influenza; SARS, severe acute respiratory syndrome.
Table 4.
Odds ratios (unadjusted* and adjusted†) comparing respirator preference under hypothetical increased threat scenarios versus “rule out TB” (usual circumstance) scenario
| Current EHFR users (N = 280) | Current N95-FFR users (N = 660) | Current PAPR users (N = 266) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Preference for: |
Preference for: |
Preference for: |
|||||||
| Scenario | EHFR | PAPR | N95-FFR | EHFR | PAPR | N95-FFR | EHFR | PAPR | N95-FFR |
| Active TB | |||||||||
| uOR | 3.0 (2.2-4.2) | 6.3 (4.0-10.1) | (ref) | 4.9 (3.8-6.3) | 4.1 (3.3-5.2) | (ref) | 3.7 (2.4-5.6) | 2.9 (2.2-3.9) | (ref) |
| aOR | 3.2 (2.3-4.6) | 7.0 (4.4-11.2) | (ref) | 5.4 (4.1-7.0) | 4.4 (3.4-5.6) | (ref) | 4.0 (2.6-6.1) | 3.1 (2.3-4.1) | (ref) |
| Pandemic H1N1 or SARS | |||||||||
| uOR | 2.3 (1.7-3.2) | 7.0 (4.1-11.7) | (ref) | 3.7 (2.8-4.9) | 4.4 (3.4-5.7) | (ref) | 3.5 (2.4-5.2) | 2.4 (1.8-3.2) | (ref) |
| aOR | 2.4 (1.8-3.4) | 7.7 (4.6-13.0) | (ref) | 4.0 (3.0-5.3) | 4.7 (3.5-6.1) | (ref) | 3.8 (2.5-5.8) | 2.5 (1.8-3.3) | (ref) |
NOTE. Unadjusted odds ratio point estimates were calculated using multinomial regression, however these can be calculated directly from the percentages in Table 3 (subject to rounding error). For example, the first uOR estimate in this Table, 3.0, equals (69%/15%) divided by (56%/37%).
EHFR, elastomeric half-face respirator, N95-FFR, N95 filtering facepiece respirator; PAPR, powered air-purifying respirator; ref, reference comparison; TB, tuberculosis; uOR, unadjusted odds ratio; aOR, adjusted odds ratio; H1N1, H1N1 influenza; SARS, severe acute respiratory syndrome.
uOR = probability of preferring EHFR (or PAPR) divided by probability of preferring N95-FFR under an active TB (or pandemic H1N1) scenario divided by the same probability ratio under a usual circumstance scenario.
aORs were estimated adjusting for a limited set of critical covariates (see Data analysis section for details).
To understand whether EHFR and PAPR users perceived their susceptibility differently than N95-FFR users, we asked participants how likely they believed they would be to contract various communicable diseases from caring for an infected patient while not wearing a respirator. Whereas most respondents reported their belief that it would be likely or very likely that they would contract TB, H1N1, SARS, or Ebola, there were no significant differences in the frequency of reporting of the different responses among the user groups (data not shown).
Discussion
This study examined whether EHFRs and PAPRs could serve as user-acceptable solutions to N95-FFR shortages. Respirator shortages have been repeatedly demonstrated during the last 3 pandemics and will predictably recur with future pandemics. Thus, the health care sector must plan to address these foreseeable shortages.
The use of a reusable respirator that could be purchased in advance and be on hand in a health care setting would avoid the need for just-in-time purchasing of N95-FFRs and reliance on an insecure supply chain during a surge in demand. EHFRs have not conventionally been used in health care, but IOM, OSHA, and others have suggested their use as an option to mitigate shortages of disposable N95-FFRs during emergencies.27 Although PAPRs may have found greatest use in health care historically among workers who are unable to use tight-fitting N95-FFRs, expanded use could also assist in limiting N95-FFR shortages.
EHFR findings
Although EHFR users rate their respirators less favorably than do N95-FFR users, with respect to comfort and communication, they rate them significantly more favorably with respect to sense of protection afforded. Despite the barriers of comfort and communication, when given a choice to wear an N95-FFR, the majority of current EHFR users would still choose to wear an EHFR under usual and escalated respiratory protection scenarios.
There are several explanations why EHFRs may be preferred over N95-FFRs. First, there may be greater confidence in obtaining a reliable fit, given the more durable design of the EHFR. Further, the mask has a larger surface area in contact with the face, which may promote a better seal or even a perception of a better seal. Second, the EHFR users may wear their respirators more frequently than the N95-FFR users, yielding a greater familiarity with the mask and assessment of how well it protects. When adjusted for frequency of use, however, there was still a pattern of preference for EHFR. Another hypothesis was that this EHFR preference may have been driven by a dominant choice by a specific worker group (eg, nurses compared to doctors). When we adjusted for job category, however, there was still a statistically significant preference for EHFR under increasing threat levels. Finally, we explored whether having an increased perception of risk susceptibility might influence preference for respirator type. To understand underlying perceptions among different respirator users, this study queried whether routine EHFR users were influenced more by fear of the potential diseases they could encounter, compared to N95-FFR users. They were not. They rated the likelihood of contracting TB, SARS, or Ebola when not wearing a respirator similarly to N95-FFR users, suggesting that they view the diseases themselves similarly as other respirator users.
Poorer comfort of EHFR masks has been anecdotally cited as a barrier to use in the health care setting.17, 19 In a Canadian pilot study where HCWs were newly assigned to wear EHFRs, HCWs reported comfort as a reason for not choosing an EHFR.17 Thus, there may be resistance from HCWs when newly introduced to these masks as a form of required respiratory protection. In the current study's population of experienced EHFR users, the comfort ratings for these devices were not dramatically different from the ratings of N95-FFRs, and mean response values fell in the neutral or positive range. This suggests that comfort of EHFRs is not an insurmountable barrier to their use in health care settings, and that experience with these devices creates familiarity and ease with use, such that the EHFR is the preferred device among the experienced user cohort.
Communication, however, was rated negatively for EHFRs. This is a challenge in health care, where staff must communicate not only with each other but also with patients. Although this does not seem to impair ultimate preference, this aspect clearly demonstrates a limitation of this device's use in the health care setting. This user rating echoes that found in the Workers’ Compensation Board of British Columbia study, where speech intelligibility test scores for workers using EHFRs were lower, but still above the minimum acceptable level according to the National Institute for Occupational Safety and Health.17 Similarly, in a study of intelligibility of words spoken when wearing EHFRs under real and simulated ambient intensive care unit noise conditions, speech intelligibility was significantly lower compared to controls and compared with other common forms of respiratory protection, but could be improved with use of a voice augmentation device.27 The results from the current study support previous recommendations from the IOM that communication interference be rectified in the next generation of respiratory protective devices developed for HCWs.27 However, in general, the familiar EHFR user cohort numbering several hundred still preferred this device for all threat scenarios for which they were queried.
PAPR findings
Responses of PAPR users in this study shared some similarities with the limited number of prior published works evaluating PAPR user acceptability in HCWs. Communication and comfort ratings among PAPR users were the lowest of the 3 respirators. With respect to communication, in a study of different types of respirators worn by HCWs, hearing clarity while wearing a PAPR was 79% compared to 90% clarity without the use of a PAPR.27 In another study of HCWs who had used 2 different PAPR models during the 2003 SARS outbreak, between 5% and 14% percent of respondents reported significant or unacceptable hearing impairment, only 5%-14% could speak normally when using the PAPR, and 25% reported having to raise their voice significantly.28 These HCWs, however, had also worn N95-FFRs underneath their PAPR hoods, per hospital policy, which may have added an additional impairment to communication. Research on comfort of PAPRs, however, has produced variable results. In the study among HCWs experienced with PAPR use during SARS, the majority of respondents found PAPRs to be “at least tolerable,” with 23%-46% reporting them to be “very comfortable,” but 9%-14% reporting to be “uncomfortable.” Other studies have reported increased perception of facial heat and eye dryness in PAPR users.29, 30
In the current study, PAPR users rated their respirators more favorably than N95-FFR users on sense of protection. Similarly, in the study of HCWs familiar with PAPR use during SARS, PAPRs were perceived to be more protective than N95-FFRs.28 Of the 3 respirators queried in the current study, PAPRs have the highest APF by OSHA. In our study population, PAPR users rated their respirators slightly lower than EHFR users on their perceived level of protectiveness. This finding suggests an opportunity for improved education among HCWs on the levels of protection provided by respiratory protective equipment in general.
PAPR users also reported higher ratings related to confidence that their respirator would protect them based on the training they had received compared to N95-FFR users, but significantly lower ratings compared to EHFR users. This may reflect differences in the content and delivery of respiratory protection training among the different user groups. In the study of HCWs experiences with PAPR use during SARS, the majority of HCWs received PAPR training by an experienced trainer, but approximately 30% received video instruction and some relied only on printed instructions.28 There may be an additional belief in the protectiveness of a respirator that is instilled during a fit testing process, which is absent in a loose-fitting PAPR training program.
Similar to that reported by the EHFR users, despite the less favorable responses on comfort and communication, PAPR users expressed preference for use of PAPR over N95-FFR in increased threat scenarios, as compared to usual circumstances. This response pattern is similar to the findings among HCWs using PAPRs during SARS, where 84% of respondents agreed or strongly agreed to the statement, “for potential SARS cases, routine use of the PAPR….is preferable to using the N-95 respirator, despite the significantly higher cost of the PAPR.”28 Interestingly, only 51% of that population believed that routine use of the PAPR was preferable for infectious cases, such as TB. Similar to that seen among EHFR users, however, when given a choice to wear an N95-FFR, the majority of current PAPR users would still choose to wear a PAPR under escalated respiratory protection scenarios.
Strengths and limitations
This study has several strengths. First, these findings, to our knowledge, represent the largest collection of user acceptance data from EHFR and PAPR users specifically focused on respirator use to date. Second, these results come from a large population of HCWs familiar with the use of EHFRs over more than 8 years of use. Elastomeric respirators were first introduced in this setting in 2009 during the H1N1 pandemic and had continued in routine use since that time. At least 13% of the current EHFR respondents had used these devices since their debut in this setting, reflecting familiarity with use of this device. The mean age of EHFR users was 37 years, and they had worked an average of 12 years in health care, with an average of 6 years at their current sites.
The survey included photos for each question that required a response about a specific type of respirator, which likely increased surety that the responses refer to the intended respirator. Another strength is the high number of responses from outpatient clinical HCWs and patient support staff, who often are not included in HCW research. They represent a vitally important component of the care team and must be considered with respect to personal protective equipment.
Prior to initiation of this survey, we had become aware that some HCWs engaged in a practice of wearing different respirators than what they were assigned to use (ie, some HCWs who were assigned to wear an EHFR would usually use an N95-FFR instead). Our additional research into respirator availability, storage, and cleanliness will help to understand why some EHFR users wear different respirators than what they are assigned to use. Our findings here suggest that user acceptance is not a significant driver of this practice.
This study has limitations as well. Participants worked at different sites, each with different respiratory protection training programs, all of which complied with established protocols to meet the expectations of the OSHA respiratory protection standard. The analyses in this study incorporate frequency of respiratory protection training as a potential confounder, but are unable to differentiate between organizational differences in content or approach to respiratory protection training. By incorporating site, job category, and primary clinical unit, however, influences imparted by training content and delivery likely were captured. Also, the preference odds ratios indicate a preference for EHFR or PAPR in comparison to preference for N95-FFR. The methodology does not allow a head-to-head comparison of EHFR compared to PAPR and should not be interpreted in this way.
Finally, our participation rate was 12%, but this was expected based on study design. We aimed to recruit at least 1,000 participants and provided gift cards for participation on a rolling basis. HCWs may have been less motivated to participate after the gift cards were exhausted. The breadth of job categories of our participants, however, suggests that an appropriately representative sample of HCWs engaged in respiratory protection activities was assembled. The number of current EHFR users is smaller than that originally anticipated and on which power calculations were based. Some of this is owing to changes in respirator assignment surrounding the time of survey deployment. For example, out of 1,152 participants, 153 reported using EHFRs in the past but were no longer using them (data not shown). Also, participants were asked what respirator they were most recently assigned to use and what respirator they usually use. To account for the small group of respondents who usually used respirators that were different from their respirator assignment, we adjusted for assigned respirator in all of our analyses, and the unadjusted outcomes did not change significantly. Because we wanted to focus on the experiences of current users, we have a smaller sample size than originally anticipated. Despite this smaller sample size, we still saw significant differences between the respirator user groups, suggesting that we were not underpowered to detect important differences.
Conclusions
User acceptance has been cited as a barrier to wide-scale implementation of the use of reusable respirators, such as EHFRs in health care. Based on the experience of 1 health system, user acceptance does not appear to be as important a barrier as potentially anticipated. Even when given a choice to use a standard N95-FFR, most current EHFR users will still elect to use an elastomeric respirator under increasing risk levels, despite perceptions of somewhat lower comfort and communication. This suggests that EHFRs are an acceptable alternative to N95 respirators in health care and offer 1 viable solution to prevent pandemic-generated respirator shortages. Similar patterns were observed among PAPR users. These results suggest that user acceptance should not uncritically continue to be cited as a major barrier to widespread adoption of reusable respirator use in health care.
Acknowledgments
The authors appreciate the visual analytic design input of Mr Zoran Ivankovich.
Footnotes
Funding/support: This work was supported by a grant (1R21OH010868-01) from the Centers for Disease Control and Prevention-National Institute for Occupational Safety and Health.
Conflicts of interest: None to report.
References
- 1.Siegel JD, Rhinehart E, Jackson M, Chiarello L, Health Care Infection Control Practices Advisory Committee 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35(Suppl):65–164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wizner K, Stradtman L, Novak D, Shaffer R. Prevalence of respiratory protective devices in US health care facilities: implications for emergency preparedness. Workplace Health Saf. 2016;64:359–368. doi: 10.1177/2165079916657108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brosseau L, Berry Ann R. Centers for Disease Control and Prevention; Atlanta (GA): 2009. N95 respirators and surgical masks. [Google Scholar]
- 4.Srinivasan A, Jernign DB, Liedtke L, Strausbaugh L. Hospital preparedness for severe acute respiratory syndrome in the United States: views from a national survey of infectious diseases consultants. Clin Infect Dis. 2004;39:272–274. doi: 10.1086/421777. [DOI] [PubMed] [Google Scholar]
- 5.Beckman S, Materna B, Goldmacher S, Zipprich J, D'Alessandro M, Novak D, et al. Evaluation of respiratory protection programs and practices in California hospitals during the 2009-2010 H1N1 influenza pandemic. Am J Infect Control. 2013;41:1024–1031. doi: 10.1016/j.ajic.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schnirring L. Center for Infectious Disease Research and Policy (CIDRAP); Minneapolis (MN): 2014. WHO: medical worker infections and shortages hamper Ebola response [Internet]http://www.cidrap.umn.edu/news-perspective/2014/08/who-medical-worker-infections-and-shortages-hamper-ebola-response Available from: Accessed June 29, 2018. [Google Scholar]
- 7.Northam J. National Public Radio; Washington (DC): 2014. Ebola protective suits are in short supply.https://www.npr.org/2014/10/07/354230895/ebola-protective-suits-are-in-short-supply Available from: Accessed June 29, 2018. [Google Scholar]
- 8.Abutaleb Y. West Africa's Ebola epidemic leads to US protective gear backlog. Available from: https://www.reuters.com/article/us-health-ebola-usa-backlog/west-africas-ebola-epidemic-leads-to-u-s-protective-gear-backlog-idUSKBN0IQ2N420141107. Accessed June 29, 2018.
- 9.Hinshaw D, Bunge J. US buys up Ebola gear, leaving little for Africa: manufacturers strain to meet demand amid rising anxiety. Wall Street Journal (US Edition) November 24, 2014 [Google Scholar]
- 10.National Academies of Sciences, Engineering, and Medicine . National Academies Press; Washington (DC): 2017. [Google Scholar]
- 11.Institute of Medicine . National Academies Press; Washington (DC): 2006. [Google Scholar]
- 12.Rebmann T, Alexander S, Bartley J, Cain T, Citarella B, Cloughessy M, et al. Association for Professionals in Infection Control and Epidemiology; Washington (DC): 2009. APIC position paper: extending the use and/or reusing respiratory protection in healthcare settings during disasters. [Google Scholar]
- 13.Centers for Disease Control and Prevention . National Institute for Occupational Safety and Health; 2014. [Google Scholar]
- 14.Hines L, Rees E, Pavelchak N. Respiratory protection policies and practices among the health care workforce exposed to influenza in New York State: evaluating emergency preparedness for the next pandemic. Am J Infect Control. 2014;42:240–245. doi: 10.1016/j.ajic.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Assessment of elastomeric respirators in healthcare environments (R21). Available from: https://www.cdc.gov/niosh/oep/resrchpast.html. Accessed December 21, 2018.
- 16.Bach M. Centers for Disease Control and Prevention; Atlanta (GA): 2017. Understanding respiratory protection options in healthcare: the overlooked elastomeric. [Google Scholar]
- 17.Ciconte R, Danyluk Q. WorkSafe BC Research Services; British Columbia (Canada): 2013. Assessment and determination of practical considerations for widescale utilization of elastomeric half-facepiece respirators during a pandemic or outbreak situation. Report no.: RS2011-IG13. [Google Scholar]
- 18.Bessesen MT, Adams JC, Radonovich L, Anderson J. Disinfection of reusable elastomeric respirators by health care workers: a feasibility study and development of standard operating procedures. Am J Infect Control. 2015;43:629–634. doi: 10.1016/j.ajic.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 19.Hines SE, Mueller N, Oliver M, Gucer P, McDiarmid M. Qualitative analysis of origins and evolution of an elastomeric respirator-based hospital respiratory protection program. J Int Soc Respir Prot. 2017;34:95–110. [PMC free article] [PubMed] [Google Scholar]
- 20.Brown LM, Rogers B, Buckheit K, Curran JP. Evaluation of 9 health care organizations’ respiratory protection programs and respiratory protective device practices: implications for adoption of elastomerics. Am J Infect Control. 2018;46:350–352. doi: 10.1016/j.ajic.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 21.California Department of Public Health . Occupational Health Branch California Department of Public Health; Richmond (CA): 2015. [Google Scholar]
- 22.Occupational Safety and Health Administration . Department of Labor; Washington (DC): 2009. Report no. OSHA 3328-05R. [Google Scholar]
- 23.Peterson K, Novak D, Stradtman L, Wilson D, Couzens L. Hospital respiratory protection practices in 6 US states: a public health evaluation study. Am J Infect Control. 2015;43:63–71. doi: 10.1016/j.ajic.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66:411–421. doi: 10.1097/01.psy.0000127692.23278.a9. [DOI] [PubMed] [Google Scholar]
- 25.Harrell FE., Jr. Springer; New York (NY): 2001. Regression modeling strategies: with applications to linear models, logistic regression and survival analysis. [Google Scholar]
- 26.Heilberger RM, Robbins NB. Design of diverging stacked bar charts for Likert scales and other applications. J Stat Softw. 2014;57:1–32. [Google Scholar]
- 27.Radonovich LJ, Yanke R, Cheng J, Bender B. Diminished speech intelligibility associated with certain types of respirators worn by healthcare workers. J Occup Environ Hyg. 2010;7:63–70. doi: 10.1080/15459620903404803. [DOI] [PubMed] [Google Scholar]
- 28.Khoo K, Leng P, Ibrahim IB, Lim TK. The changing face of healthcare worker perceptions on powered air-purifying respirators during the SARS outbreak. Respirology. 2005;10:107–110. doi: 10.1111/j.1440-1843.2005.00634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Powell JB, Kim J, Roberge R. Powered air-purifying respirator use in healthcare: effects on thermal sensations and comfort. J Occup Environ Hyg. 2017;14:947–954. doi: 10.1080/15459624.2017.1358817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacDowell L, He X, Guffey S, Allen A. ProQuest LLC; Ann Arbor (MI): 2018. Preference and user experience with powered air-purifying respirators in healthcare workers in a simulated work environment: a pilot study. [Google Scholar]