Abstract
Background
We studied the efficacy of different time-interval applications of alcohol hand gel as a strategy for the prevention of influenza-like illness (ILI) in preschool-age children.
Methods
We performed a classroom-based cluster randomization at a kindergarten school in Bangkok, Thailand. A total of 1437 children were placed into 3 test groups, based on the frequency of alcohol hand gel use for hand hygiene: only before lunch (q lunch), every 120 minutes (q 120), and every 60 minutes (q 60). The primary outcome was a change in the school absenteeism rate caused by ILI.
Results
The rates of absenteeism from confirmed ILI (sick days/present days) were 0.026 in the q lunch group, 0.025 in the q 120 group, and 0.017 in the q 60 group. Significant reductions in absenteeism rates were seen when comparing the q 60 group with the q 120 group (rate difference, 0.009; 95% confidence interval [CI], −0.002 to 0.015; P = .008) and comparing the q 60 group with the q lunch group (rate difference, 0.0096; 95% CI, 0.004-0.016; P = .002). No such differences were detected between the q 120 and q lunch groups (rate difference, 0.001; 95% CI, 0.005-0.007; P = .743).
Conclusions
The compulsory hourly use of alcohol gel as classroom hand disinfection could significantly reduce the rate of absenteeism from ILI in preschool-age children.
Key Words: School outbreak, Antiseptic hand gel, School disinfection, Hand hygiene
Influenza-like illnesses (ILI), including the common cold, influenza, and hand, foot, and mouth disease, are typically self-limited. Nevertheless, these illnesses are highly contagious and can have a significant societal impact. In particular, the high infection rate seen in children and young adults, with a sparing of the elderly population, in the 2009 H1N1 pandemic suggests an urgent need for updated infection control policies.1 A feasible school disinfection program could be valuable, especially in kindergarten schools, where children interact closely throughout the day.
The number of 3- and 4-year-olds enrolled in preschool increased steadily between 1970 and 1985.2 The trend toward earlier preschool enrollment has continued, and it is now common for children as young as age 2 years to attend preschool programs. This transition presents a major challenge to schools, which must meet the needs of their changing student bodies and prepare for school outbreaks.
Various infection control programs for kindergartens have been studied; however, most published studies used multiple interventions, including teaching student hand etiquette, regular handwashing and the use of alcohol hand gel, to achieve the maximum possible reduction in transmission rates.3, 4 Implementation of multiple practices usually is not practical, however, especially in very young children.
Although frequent handwashing has been recommended as an effective practice for the prevention of disease transmission, preschool-age children are not easily induced to wash their hands thoroughly and frequently. Alcohol hand gel presents a good alternative because of its convenience and effective disinfection.5, 6 The present study aimed specifically to evaluate the appropriate time interval for the use of alcohol hand gel as a single strategy to reduce the rate of ILI in preschool-age children. Our results may aid the development of practicable infection control guidelines for kindergarten schools.
Methods
Study design and population
We chose Denla Kindergarten, a large private school in suburban Bangkok, Thailand, as our single study center. This school included 1441 children and 68 classrooms. In Thailand, kindergartens generally divide children into 4 levels, designated as preschool year (PY) 1 for children aged 2-3 years, PY 2 for children aged 3-4 years, PY 3 for children aged 4-5 years, and PY 4 for children aged 5-6 years.
We performed a cluster-randomized, controlled trial to assess the effectiveness of 3 disinfection interventions: application of alcohol hand gel every 60 minutes (q 60 group), every 120 minutes (q 120 group), and once before lunch, the current school standard for hand hygiene (q lunch group), as shown in Table 1 . We hypothesized that children enrolled in the intervention groups would have significantly lower rates of absenteeism from ILI compared with the children in the control group.
Table 1.
Number of children in each study arm
| q 60 group | q 120 group | q lunch group | |
|---|---|---|---|
| PY1, n (%) | 93 (6.45) | 93 (6.45) | 118 (8.19) |
| PY2, n (%) | 149 (10.41) | 139 (9.65) | 167 (11.59) |
| PY3, n (%) | 107 (7.43) | 116 (8.05) | 163 (11.31) |
| PY4, n (%) | 103 (7.22) | 101 (6.87) | 92 (6.38) |
| Total (n = 1441), n | 452 | 449 | 540 |
We collected data from December 2009 to February 2010, in the peak season for ILI in Thailand.7 Approval from school authorities was acquired before the start of the study. We described other risk factors for ILI in a leaflet distributed through the school to each participating family after written informed consent was obtained. The study was reviewed and approved by Siriraj Hospital’s Institutional Review Board, and the research protocol was approved by Siriraj Hospital’s Research Ethics Committee. The sole inclusion criterion was parental consent to participate in the study, and the sole exclusion criterion was an allergy to alcohol hand gel.
Intervention
We used cluster randomization to assign the school’s classrooms to intervention or control groups, with the classroom as the level of randomization. The rationale behind this structure was that children in a shared classroom are at similar risk for contracting diseases through airborne, droplet, and contact transmission.
To ensure the compliance of each intervention group, 2 research assistants were assigned to monitor the use of alcohol hand gel every 60 or 120 minutes for the duration of the 12-week study. Classroom teachers were required to cosign after each disinfection round.
In each classroom, the teacher received a container of alcohol hand gel from the governmental pharmaceutical organization (active ingredients: ethyl alcohol, 70%; chlorhexidine gluconate, 1%; Irgasan, 0.3%). Although the safety of alcohol hand gel use by children has been demonstrated,8 the teacher was instructed to assist each child in using 1 pump of alcohol hand gel per disinfection round. The teacher was also charged with the proper storage and refilling of the alcohol hand gel during the study period.
Students whose families declined to participate were not asked to use alcohol hand gel. These students remained in their classrooms and continued to follow the school standard for hand hygiene.
Data collection and illness definitions
Existing school rules require that a parent or guardian call to report student absences. All student absences were documented by classroom teachers according to the usual practice. Only absences caused by ILI were recorded in the case record forms. The form included the child’s name, the date of absence, whether the child saw a physician, and if so, the diagnosis. If the child was sick but was not seen by a physician, symptoms were recorded.
Outcomes
The study’s primary outcome was a change in the absenteeism rate caused by reported, physician-confirmed ILI during the study period. The rate was calculated as the number of sick days divided by the total number of school days.
The secondary outcome was a change in the rate of absenteeism caused by total reported ILI (with and without a doctor’s confirmation). If the child was sick but did not see a doctor, the parents were asked to report any of the following symptoms: runny or stuffy nose, cough, fever or chills, sore throat, headache, diarrhea, and presence of hand, foot, or mouth ulcers. If 2 or more of these symptoms were reported, then the child’s illness was documented as ILI.9, 10
Statistical analysis
Children in each study group were pooled, and the clustering effect was disregarded to compare baseline characteristics of the 3 groups. For continuous data, univariate analyses were performed to test for normality in the distribution. The Student t-test and Wilcoxon’s rank-sum test were used for normal and nonnormal distributions, respectively. Fisher’s exact test or the χ2 test was used to compare categorical or binary data, as appropriate.
Logistic regression with generalized estimating equations was used to adjust for the clustered design, in which outcome is the absenteeism rate during the trial period for each study arm. Poisson regression was used for the absenteeism rate. Based on previous unpublished studies, the anticipated absenteeism rate in the control group was 0.05. SAS Power and Sample Size 3.1 software (SAS Institute, Cary, NC) were used to calculate sample size.
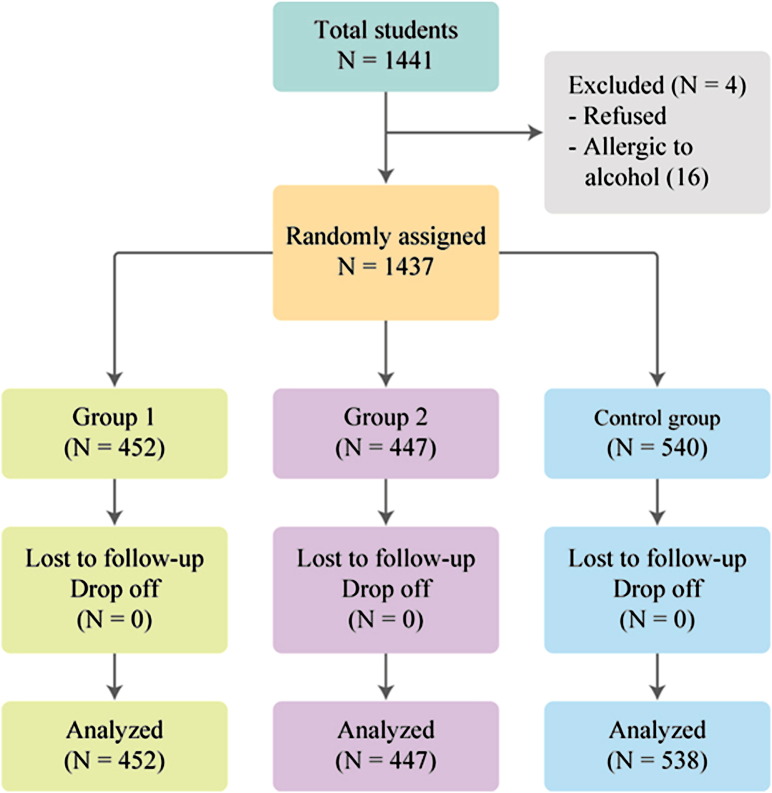
Results
A total of 1437 of the 1441 students provided written informed consent and were randomly assigned to a test group (Fig 1 ). Among these students, 16 children reported a history of alcohol hand gel allergy. These children remained in their classrooms but did not use alcohol hand gel. No students were lost to follow-up or discontinued the intervention during the study period. Baseline characteristics of all participants after randomization were similar across the intervention groups (Table 2 ). More than half of the children were aged <4 years, and most had been breast-fed and adequately immunized.
Fig 1.
Study flow.
Table 2.
Baseline characteristics
| % | q 60 group (group 1) | q 120 group (group 2) | q lunch group (control group) | Missing | |
|---|---|---|---|---|---|
| Boy (n = 801) | 55.66 | 211 | 255 | 335 | 0 |
| Girl (n = 638) | 44.34 | 241 | 192 | 205 | |
| Age, months | 0 | ||||
| 0-24 | 1.81 | 5 | 4 | 17 | |
| 25-36 | 14.47 | 58 | 56 | 94 | |
| 37-48 | 36.40 | 205 | 182 | 136 | |
| 49-60 | 28.04 | 81 | 116 | 206 | |
| >60 | 19.28 | 133 | 121 | 123 | |
| Mean age, months | 50.68 | 51.37 | 49.85 | ||
| Breast-feeding history | 51 | ||||
| Never | 7.72 | 44 | 24 | 39 | |
| <3 months | 36.08 | 167 | 143 | 190 | |
| >3 months | 56.20 | 239 | 237 | 303 | |
| Atopy/allergic rhinitis | 0 | ||||
| Yes | 37.37 | 159 | 169 | 209 | |
| No | 62.63 | 293 | 276 | 331 | |
| Immunization history | 32 | ||||
| Not completed | 4.77 | 13 | 21 | 33 | |
| Completed | 54.95 | 236 | 244 | 292 | |
| Completed with additional self-paid program | 40.28 | 195 | 172 | 199 | |
| Chicken pox | 74 | 68 | 84 | ||
| IPD | 60 | 57 | 69 | ||
| Meningitis | 13 | 8 | 7 | ||
| Influenza | 116 | 108 | 116 | ||
| Rota | 34 | 21 | 26 | ||
| Household smoker | |||||
| Yes | 17.25 | 74 | 84 | 85 | 28 |
| No | 82.75 | 370 | 355 | 441 | |
| Allergic to alcohol gel | 7 | 4 | 5 | 24 | |
| Other school age member in household | |||||
| Yes | 147 | 152 | 195 | 620 | |
| No | 103 | 116 | 114 | ||
| Mall | |||||
| <4/month | 59.43 | 276 | 256 | 303 | 32 |
| >4/month | 40.57 | 167 | 183 | 220 |
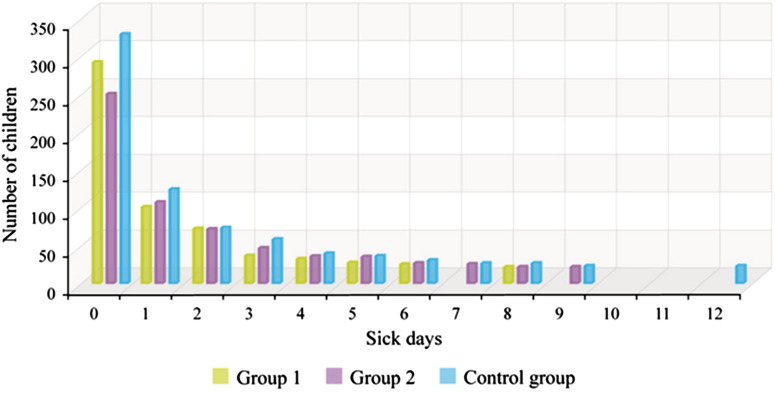
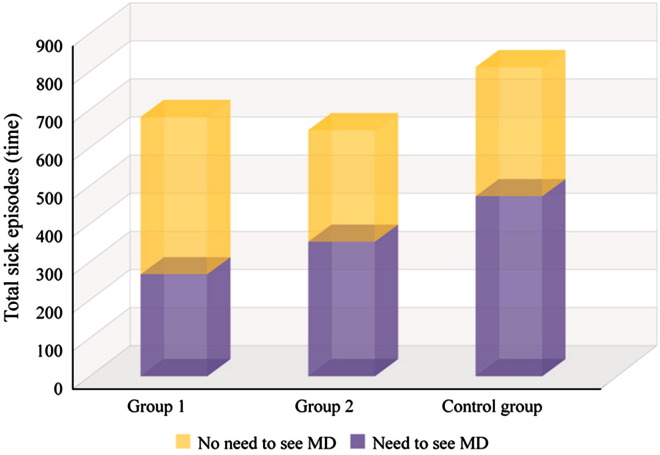
The number of days missed because of ILI ranged from 0 to 13 days per illness episode. Children who missed more than 1 day accounted for one-fourth of all absences (Fig 2 ). Compared with the control group, the intervention groups also had fewer doctor visits during the study period (Fig 3 ).
Fig 2.
Number of children and length of sick episodes.
Fig 3.
Proportion of the need to see MD of each group sick episodes.
The rates of absenteeism due to confirmed ILI (sick days/present days) were 0.017 in the q 60 group, 0.025 in the q 120 group, and 0.026 in q lunch group. The absenteeism rate due to confirmed ILI was significantly higher in the control group compared with the q 60 group (rate difference, 0.0096; 95% confidence interval [CI], 0.004-0.016; P = .002) and also in the q 120 group compared with the q 60 group (rate difference, 0.009; 95% CI, 0.002-0.015; P = .008). No significant difference was found between the q 120 group and the control group (rate difference, 0.001; 95% CI, 0.005-0.007; P = 0.743).
The rates of absenteeism from ILI both with and without a doctor’s confirmation were 0.069 in the q 60 group, 0.065 in the q 120 group, and 0.070 in q lunch groups. No significant effect was found across rates.
On multivariate analysis, only intervention group and patient age were found to be significant risk factors for ILI (P = .012 and .000, respectively). No significant effect was detected for other variables, including sex, breast-feeding history, presence of underlying disease, immunization history, frequency of visits to public places (eg, malls), and presence of a smoker in the household.
Discussion
We found that using alcohol hand gel every 60 minutes significantly reduced the rate of absenteeism due to confirmed ILI in kindergarten classrooms, whereas using alcohol hand gel every 120 minutes or only before lunch was not as effective. In the children with ILI, the need for physician visits was also lower in the intervention groups than in the control group.
In Thailand, the 2009 H1N1 influenza pandemic resulted in 14,976 cases and 119 deaths by August 22, 2009.11 At that time, several schools had been closed to control school outbreaks. These closures were traumatic for both the schools and the communities.12, 13 Health care authorities face challenges in preventing ILI transmission, as for the spread of severe acute respiratory syndrome in 2003, avian influenza in 2006, and hand, foot, and mouth disease in 2008.14, 15, 16 There is an urgent need for a practicable infection control program designed specifically for young children and their schools.
At the time of this study, no other concurrent infection control measures in place in the school or nationally could have affected the overall infection and illness rates, given that the study commenced before the H1N1 pandemic. The acceptability of facemasks in Thailand was low compared with that in several other countries.17 In contrast, the application of alcohol hand gel was already widely accepted as a convenient and effective disinfection agent for ILI that reduces viral inoculation, replication, and transmission from contaminated hands.18, 19, 20 The alcohol hand gel formulation used in this study provided broader antibacterial activity against gram-positive and gram-negative bacteria, as well as a longer sustained antibacterial effect, compared with commercially available products in the United States, which typically contain 60% ethanol, with no chlorhexidine or Irgasan.21, 22 This could limit the generalizability of our findings to other countries.
Compulsory hand disinfection of entire classrooms at prespecified intervals helped ensure compliance of each intervention group. During the study period, no adverse reactions to alcohol hand gel was reported, even in the children as young as 20 months. “Alcohol hand gel round” seemed to be an enjoyable activity for the children. Moreover, the application process for the children in the classroom was usually brief and did not disturb the regular classroom schedule. The cost of the use of alcohol hand gel every 60 minutes was $6.39 per child per 12-week period; however, the effect size of the intervention was substantial, considering the reduced rate of absenteeism for ILI and the associated lost time from work for parents and costs related to doctor visits and antibiotic prescriptions.
No significant effect of gel application on the absenteeism rate was detected for all reported ILI (with and without a doctor’s confirmation), however. One possible explanation for the inconsistency between the primary and secondary outcomes is misclassification of large numbers of cases due to the lack of diagnostic testing. Especially in those children who did not visit a doctor, allergy symptoms could have been easily misclassified during the telephone interview (the baseline data show that 37.37% of the students reported an allergic disorders as the underlying disease), as well as those who had ILI that attended school regardless of being ill or not.
Likewise, we cannot definitively state that the observed reduction in absenteeism is the direct effect of the school disinfection program; however, randomization should account for unknown confounders. Another limitation is that the study was conducted in a single school system in which most families were middle-to-high socioeconomic status; our results might not be applicable to other schools.
In conclusion, the use of alcohol hand gel every 60 minutes significantly reduced the absenteeism rate due to confirmed ILI in kindergarten classrooms, whereas using alcohol hand gel every 120 minutes or only before lunch was not as effective. No adverse reactions to the alcohol hand gel were observed during the study period. Day care centers and kindergartens should consider adopting this practice to reduce the spread of common illnesses among children, especially during epidemics.
Acknowledgment
We thank Thidakarn Rujipattanakul, the school, and the parents and students who participated in the study for their cooperation.
Footnotes
D.P. conceptualized the research questions, conducted the data analyses, and wrote the initial drafts of the manuscript. T.P. and E.F.C. supervised data analysis and interpretation of results and revised and contributed to the manuscript. N.V. and S.D. critically interpreted the results and reviewed drafts of the manuscript.
This research was supported by a Royal College of Physicians of Thailand research grant.
Conflict of interest: None to report.
References
- 1.Khandaker G., Dierig A., Rashid H., King C., Heron L., Booy R. Systematic review of clinical and epidemiological features of the pandemic influenza A (H1N1) 2009. Influenza Other Respi Viruses. 2011;5:148–156. doi: 10.1111/j.1750-2659.2011.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Department of Education. National Center for Education Statistics . US Government Printing Office; Washington [DC]: 1985. The condition of education, 1985 edition. [Google Scholar]
- 3.Apisarnthanarak A., Apisarnthanarak P., Cheevakumjorn B., Mundy L.M. Intervention with an infection control bundle to reduce transmission of influenza-like illnesses in a Thai preschool. Infect Control Hosp Epidemiol. 2009;30:817–822. doi: 10.1086/599773. [DOI] [PubMed] [Google Scholar]
- 4.Lennell A., Kühlmann-Berenzon S., Geli P., Hedin K., Petersson C., Cars O. Alcohol-based hand disinfection reduced children’s absence from Swedish day care centers. Acta Paediatr. 2008;97:1672–1680. doi: 10.1111/j.1651-2227.2008.01057.x. [DOI] [PubMed] [Google Scholar]
- 5.Meadows E., Le Saux N. A systematic review of the effectiveness of antimicrobial rinse-free hand sanitizers for prevention of illness-related absenteeism in elementary school children. BMC Public Health. 2004;4:50. doi: 10.1186/1471-2458-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grayson M.L., Melvani S., Druce J., Barr I.G., Ballard S.A., Johnson P.D. Efficacy of soap and water and alcohol-based hand-rub preparations against live H1N1 influenza virus on the hands of human volunteers. Clin Infect Dis. 2009;48:285–291. doi: 10.1086/595845. [DOI] [PubMed] [Google Scholar]
- 7.Simmerman J.M., Chittaganpitch M., Levy J., Chantra S., Maloney S., Uyeki T. Incidence, seasonality and mortality associated with influenza pneumonia in Thailand: 2005-2008. PLoS ONE. 2009;4:e7776. doi: 10.1371/journal.pone.0007776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kinnula S., Tapiainen T., Renko M., Uhari M. Safety of alcohol hand gel use among children and personnel at a child day care center. Am J Infect Control. 2009;37:318–321. doi: 10.1016/j.ajic.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Kasper M.R., Wierzba T.F., Sovann L., Blair P.J., Putnam S.D. Evaluation of an influenza-like illness case definition in the diagnosis of influenza among patients with acute febrile illness in Cambodia. BMC Infect Dis. 2010;10:320. doi: 10.1186/1471-2334-10-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Classification Committee of the World Organization of National Colleges, Academies, and Academic Associations of General Practitioners/Family Physicians . ICHPPC-2 defined. Oxford University Press; New York [NY]: 1983. Inclusion criteria for the use of the rubrics of the International Classification of Health Problems in Primary Care; p. 487. [Google Scholar]
- 11.Simmerman J.M., Suntarattiwong P., Levy J., Gibbons R.V., Cruz C., Shaman J. Influenza virus contamination of common household surfaces during the 2009 influenza A (H1N1) pandemic in Bangkok, Thailand: implications for contact transmission. Clin Infect Dis. 2010;51:1053–1061. doi: 10.1086/656581. [DOI] [PubMed] [Google Scholar]
- 12.Koonin L.M., Cetron M.S. School closure to reduce influenza transmission. Emerg Infect Dis. 2009;15:137–138. doi: 10.3201/eid1501.081289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanvoravongchai P., Adisasmito W., Chau P.N., Conseil A., de Sa J., Krumkamp R., AsiaFluCap Project Pandemic influenza preparedness and health systems challenges in Asia: results from rapid analyses in 6 Asian countries. BMC Public Health. 2010;10:322. doi: 10.1186/1471-2458-10-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fong E., Chang L.Y. Community under stress: trust, reciprocity, and community collective efficacy during a SARS outbreak. J Community Health. 2011;36:797–810. doi: 10.1007/s10900-011-9378-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y., Tan X.J., Wang H.Y., Yan D.M., Zhu S.L., Wang D.Y. An outbreak of hand, foot, and mouth disease associated with subgenotype C4 of human enterovirus 71 in Shandong, China. J Clin Virol. 2009;44:262–267. doi: 10.1016/j.jcv.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Bourouiba L., Teslya A., Wu J. Highly pathogenic avian influenza outbreak mitigated by seasonal low pathogenic strains: insights from dynamic modeling. J Theor Biol. 2010 Dec 10 doi: 10.1016/j.jtbi.2010.11.013. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Ferng Y.H., Wong-McLoughlin J., Barrett A., Currie L., Larson E. Barriers to mask wearing for influenza-like illnesses among urban Hispanic households. Public Health Nurs. 2011;28:13–23. doi: 10.1111/j.1525-1446.2010.00918.x. [DOI] [PubMed] [Google Scholar]
- 18.Ansari S.A., Sattar S.A., Springthorpe V.S., Wells G.A., Tostowaryk W. Rotavirus survival on human hands and transfer of infectious virus to animate and nonporous inanimate surfaces. J Clin Microbiol. 1988;26:1513–1518. doi: 10.1128/jcm.26.8.1513-1518.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agolini G., Puro V., Sancin A.M., Biondi M., Clementi M., Raitano A. Pandemic influenza: rapidsanitary-hygienic measures for initial containment of diffusion. Ann Iq. 2008;20:409–420. [PubMed] [Google Scholar]
- 20.Allison M.A., Guest-Warnick G., Nelson D., Pavia A.T., Srivastava R., Gesteland P.H. Feasibility of elementary school children’s use of hand gel and facemasks during influenza season. Influenza Other Respi Viruses. 2010;4:223–229. doi: 10.1111/j.1750-2659.2010.00142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aly R., Maibach H.I. Comparative study on the antimicrobial effect of 0.5% chlorhexidine gluconate and 70% isopropyl alcohol on the normal flora of hands. Appl Environ. 1979;37:610–613. doi: 10.1128/aem.37.3.610-613.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zafar A., Butler R.C., Reese D.J., Gaydos L.A., Mennonna P.A. Use of 0.3% triclosan (Bacti-Stat) to eradicate an outbreak of methicillin-resistant Staphylococcus aureus in a neonatal nursery. Am J Infect Control. 1995;23:200–208. doi: 10.1016/0196-6553(95)90042-x. [DOI] [PubMed] [Google Scholar]