Abstract
Background
Traditional infection control policies have focused on engineering controls, specific protocols, and personal protective equipment (PPE). In light of the variable success in protecting health care workers (HCWs) from Severe Acute Respiratory Syndrome (SARS) in 2003, organizational and individual factors related to self-protective behavior in health care settings may also play an important role.
Methods
A critical review of the literature was conducted, directed at understanding what organizational and individual factors are important in protecting HCWs from infectious diseases at work.
Results
Organizational factors, such as a positive safety climate, have been associated with increased HCW adherence to universal precautions. There is some evidence that appropriate training of HCWs could be effective in changing HCW behavior if appropriate follow-up is applied. Very little research into these factors has been conducted with regard to preventing exposures to respiratory tract pathogens, but there was evidence from the SARS outbreaks that training programs and the availability of adequate PPE were associated with a decrease risk of infection.
Conclusion
Variations in organizational and individual factors can explain much of the variations in self-protective behavior in health care settings. It is likely that these factors were also important determinants during the SARS outbreaks, but they have not been extensively studied.
Background
Severe Acute Respiratory Syndrome (SARS) emerged as a new cause of severe pneumonia in late 2002 and early 2003, which was quickly determined to be caused by a novel coronavirus.1 The virus spread internationally along travel routes and caused the well-documented nosocomial outbreaks in Canada, China, Hong Kong, Vietnam, and Singapore. The Canadian outbreak resulted in 438 cases, with 51% of these being health care workers (HCWs),2 3 of whom died from SARS-related causes.3
Traditional infection control practice has focussed on training individual HCWs to follow standard procedures and instruction in the use of personal protective equipment (PPE). Prior to SARS, it was already understood that the ability of HCWs to adhere to infection control guidelines varied substantially and was often less than ideal. For example, a recent study of 3 US hospitals over 3 years founds that HCWs wore appropriate respiratory protection with tuberculosis patients 44% to 97% of the time.4 Similarly, compliance with universal precautions for blood and body fluids (BBF) has been shown to range from 16% to 44%.5, 6, 7 During the SARS outbreaks of 2003, the implementation of basic infection control procedures appeared effective in controlling the outbreaks in most circumstances8, 9, 10; however, in other situations, HCWs became infected despite apparent adherence to recommended guidelines.11 Clearly, factors other than individual knowledge and motivation must be at work to give such variation in effectiveness.
A theoretic model that has been used to explain self-protective behavior at work and could account for this variation derives from the PRECEDE (Predisposing, Reinforcing and Enabling Factors in Educational Diagnosis and Evaluation) model of health promotion,12 as modified by DeJoy.13 Predisposing factors can be seen as the characteristics of the individual (beliefs, attitudes, values) that facilitate self-protective behavior. Enabling factors can refer to the environmental factors that block or promote self-protective behavior, including skills, knowledge, and availability and accessibility of PPE and other resources. Reinforcing factors involve the organizational factors, such as communication, training, performance feedback, social approval or disapproval from coworkers or management, and other safety climate dimensions. This model has previously been used to explain the variation of compliance with universal precautions to prevent exposures to bloodborne pathogens by HCWs.14 These factors can be seen to interact as shown in Fig 1.
Fig 1.
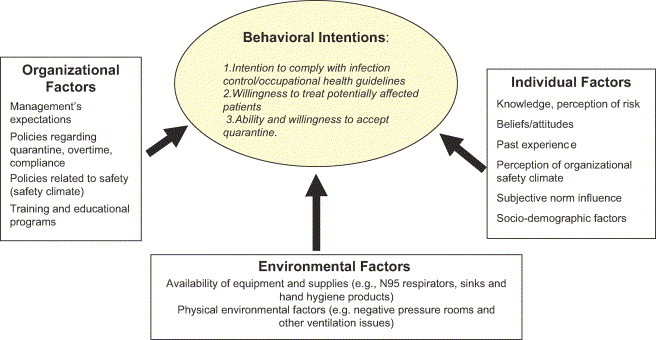
Theoretical model to explain self-protective behaviour at work. Adapted from DeJoy D. A behavioral-diagnostic model for fostering self-protective behavior in the workplace. In: Karwowski W, editor. Trends in ergonomics/human factors III. North-Holland: Elsevier Science Publishers B.V.; 1986. p. 907-17.13
The goal of this project was to review the scientific evidence on what is already known about protecting HCWs from hospital-acquired infections, using this theoretic model as a guide. This paper will review the organizational and individual factors that have been shown to be important determinants of protecting health care workers from infectious hazards.
Methods
A 16-member research team in Vancouver, Canada, composed of experts in occupational medicine, occupational hygiene, infection control, public health, and epidemiology and clinicians and frontline care providers reviewed the current scientific knowledge on the efficacy of PPE in preventing the transmission of respiratory infections and the effectiveness of these protective measures when used in clinical practice under working conditions. Literature searches were conducted in 5 databases (Medline, EMBASE, CINAHL, Web of Science, and OSHROM) for articles published in English in the last 15 years that related to infection control practices, occupational health and safety issues, and environmental factors and other issues of importance in protecting workers against infections in health care settings. This produced an initial list of 841 publications. From the initial literature search results, a series of research topics were developed under 3 broad categories: (1) basic science and efficacy of facial protective equipment, (2) the effectiveness of specific infection control procedures, and (3) organizational and individual factors that influence infection control and occupational health in health care settings.
Titles and abstracts were screened to refine the citation list to include only those articles with direct application to these topics, and secondary sources were added from these primary references. The research topics were divided among the research committee members (subgroups) to summarize, using articles from the second iteration of the original citation list. Secondary reference materials, derived from these initial references, were added. Articles were critically evaluated based on the study design (descriptive, analytic, or intervention), the population under study, and the outcomes of interest. This resulted in 168 publications being used in the final report. Drafts from each subgroup were merged, and the compiled version was reviewed by the team as a whole. The results of the organizational and individual factors are presented here. The existing knowledge was then summarized, and recommendations for further research were developed through consensus by the research team.
Results
Organizational factors in self-protective behavior at work
Organizational factors, in this context, refer to determinants that range in scope from very broad issues such as workplace culture and safety climate to specific policies and procedures, such as policies that restrict individual nurses to working with either ill or well residents during an influenza outbreak. The majority of research conducted in this area has been exploring HCW compliance with universal precautions (UP). UP were introduced in the 1980s in response to the risk of transmission of bloodborne pathogens to HCWs from patients, in particular HIV, and now are more generally referred to standard precautions (in the United States) or routine practices (in Canada). Although the research does not directly examine the compliance of HCWs with protection from respiratory tract infections, the determinants of adherence to UP are likely applicable to many types of self-protective behavior.
Safety climate
The safety climate refers to the perceptions that workers share about safety in their organization and derives from a multidimensional, systems approach to worker health and safety.15 It has generally been measured by asking workers how they rate their organization's commitment to safety and has been positively correlated to good safety performance in non-health care settings.16, 17, 18, 19 In health care, it has been postulated as a determinant of improved worker safety, in general,20 and the use of UP, in particular.21 There is general agreement that the safety-related attitudes and actions of management play an important role in creating a good or bad safety climate.22, 23
Studies in health care settings have shown that safety climate has an important influence on the transfer of training knowledge.24, 25 Rivers et al in a survey of 742 nurses regarding predictors of nurses' acceptance of an intravenous catheter safety device26 concluded that a positive institutional safety climate was more important than individual factors in predicting acceptance of these devices.
Gershon et al27 found that, in 1716 hospital-based HCWs, respondents who perceived a strong commitment to safety at their institution were over 2.5 times more likely to be compliant with UP than those who did not. Similar results were found for a group of 216 HCWs from a state correctional facility.28 A later study by this group14 examined the relative importance of safety climate, the availability of PPE (an environmental factor), and individual worker characteristics (individual factors) in determining compliance with UP. They found that safety climate had the greatest association with compliance behavior of the 3 groups of variables. However, the amount of variation predicted by the model was small, suggesting the existence of other important determinants of safety-related behavior that were not accounted for in the model.
Another study conducted with 482 nurses29 found that the worker's perception that the use of UP interfered with their work (job hindrance) was the strongest predictor of failure to comply with UP. However, this study also found that perceived safety climate was the best predictor of this perceived job hindrances. Thus, it seems that safety climate underlies other important perceptions and reveals how some of these factors may interact. Other factors that seemed to predict worker perceptions of a strong safety climate included safety performance feedback and availability of PPE.
The most comprehensive attempt to describe the underlying components of the safety climate in health care institutions found 6 different components23: (1) senior management support for safety programs, (2) absence for workplace barriers to safe work practices, (3) cleanliness and orderliness of the worksite, (4) minimal conflict and good communications among staff, (5) frequent safety-related feedback and training by supervisors, and (6) availability of PPE and engineering controls.23 In addition, 2 of these factors, senior management support for safety programs and frequent safety-related feedback and training, were significantly associated with lower rates of exposures to blood and body fluids. Although it seems that we have a good understanding of what specific elements contribute to the safety climate, no studies have attempted to implement measures to try to improve a safety climate where a poor climate exists. The study cited above recommended that safety climate surveys sponsored jointly by the infection control and occupational health and safety committees should be administered in hospitals using the safety climate scale.23 The authors made several suggestions as to how they could be used. None of the recommendations, however, have been evaluated in terms of their ability to improve worker safety, once applied.
Another challenge to improving safety climates in hospitals comes with the recent emphasis on downsizing organizations and outsourcing of the workforce. Studies in the United States have shown that hospital-based HCWs are having to work faster and harder than ever in an environment of higher patient acuity and increased patient turnover and with less time for training and education.30, 31, 32, 33, 34 This is likely happening in Canada, and other countries, as well. How these larger organizational changes affect safety climate remains to be studied.
Communication, training, and feedback
There is very little information regarding which formative training and continuing education strategies are most effective in implementing and maintaining good infection control practices or on which methods of feedback are best. In one study that examined the adherence to UP in 451 nurses employed in a large US hospital center, feedback on compliance was found to be one of the predictors of adherence, along with job hindrance and the availability and accessibility of PPE.29 Again, the variance in adherence predicted by the model was modest. This study, however, did not look specifically at the type of feedback or communication used.
A study conducted in emergency room (ER) HCWs found that compliance with barrier precautions (use of cap, gown, mask, gloves, protective eyewear) improved when staff was notified of the arrival of patients by ambulance staff.35 This prenotification resulted in 92% of ER staff using appropriate protection compared with 63% when patients arrived unannounced.
A study of Thai health care workers36 demonstrated higher compliance with glove use and handwashing during a peer feedback intervention (83% compliance vs 49% compliance during baseline). However, compliance fell to 73% in the postintervention phase. The authors noted that other techniques, including in-service educational sessions, computer-assisted learning, and provision of education and group feedback by researchers also failed to show long-term effectiveness. The authors suggested that ongoing observation and feedback are likely needed because the effectiveness of programs diminishes over time.
Another study showed that an educational intervention consisting of lecture and practice sessions for operating room staff increased compliance with use of protective eyewear from 54% to 66% and double gloving from 28% to 55%.37 It was unclear, however, how much of this effect was due to awareness by staff that they were being observed. Another study on UP found that, even when HCWs have adequate information and knowledge, they still need to enhance their skills by practicing how to use PPE.14
The DeJoy study, which showed that safety climate was a strong predictor of perceived job hindrance, also offers some insight into what kind of training programs are needed.29 If perceived job hindrance is an important predictor of compliance with UP, then training programs may need to focus less on knowledge-based training and more on helping workers overcome or reduce the barriers associated with compliance. There are no studies examining the effectiveness of measures that emerge from these suggestions.
In a recent review of the effectiveness of various interventions aimed at changing the clinical practice of physicians,38 the authors reported that there was evidence that educational outreach visits, posted reminders, interactive educational meetings, and other multifaceted interventions were effective in improving the transfer of new information into clinical practice. Passive interventions, such as mailing out new recommendations, were generally not found to be effective, even though they are the methods most commonly applied. Interventions that relied on audits or other forms of feedback were found to have variable effectiveness. Grol et al39 characterized the features that were more likely to be associated with a change in primary care practice by physicians. An important finding was that recommendations with a strong evidence base were more likely to be effective than consensus statements.
During the SARS outbreak in Hong Kong, Lau et al40 showed that having received less than 2 hours of infection control training was strongly associated with developing SARS, in addition to the inconsistent use of PPE and perceiving the amount of available PPE to be inadequate. The latter factors may be concrete examples of poor safety climates. Of note, no studies were found that examined different communication strategies used in health care institutions to improve worker safety.
Individual factors in self-protective behavior at work
Knowledge acquired through training and personal experience
Knowledge of the appropriate use of PPE is necessary but not sufficient for HCWs to adopt safe work practices.41 The study by Gershon et al from 199527 found that most HCWs surveyed had high levels of knowledge regarding UP practices but that this knowledge did not lead to high levels of compliance. Repeated exposures without consequences may also decrease compliance. In a study examining this issue, HCWs who had repeated exposures to blood and body fluids and did not acquire infection perceived a decreased risk of acquiring infection than those who had not been exposed. This experience may lead to a false sense of invulnerability and therefore increased risk taking.14
Another study found that HCWs who were younger than 40 years of age were more likely to comply with UP.28 The authors suggested that this may reflect more recent training, rather than a direct effect of age. HCWs surveyed were found to have realistic risk perceptions about exposure to BBF: Few were fearful of contagion. The level of experience did not necessarily lead to a lack of understanding of risks involved. Nurses who were educated in a more disease-driven infection control model, in which precautions were used only when the patient was known to be infected by a given pathogen, appear to be less comfortable with the UP model, as compared with recent graduates.42
Students and other HCWs may look to attending physicians as role models. However, younger physicians, house staff, and medical students have been found to be more complaint with UP than senior physicians.37 The increased compliance again probably reflects more recent training. Another study found that compliance with methicillin-resistant Staphylococcus aureus (MRSA) precautions (which included use of gloves and gowns and handwashing) was related to the occupational group, with physicians showing the lowest compliance (22%) and physiotherapists and occupational therapists having the highest compliance (89%).43 Compliance with gown and glove requirements was 65% and for hand hygiene, 35%. Angtuaco et al44 found that fewer gastroenterologists than GI endoscopy nurses used face shields for all procedures (14% vs 21%). Gershon et al has observed that physicians are “out of the loop” with regard to safety climate within hospitals and that special efforts need to be made to involve them in training, safety programs, and safety committees.28
Nurses have reported confusion at the ward level and uncertainty concerning the rationale for the uses of PPE recommended in infection control guidelines and perceive existing guidelines to lack specificity to their practice.45 They also may doubt the effectiveness of isolation precautions to prevent disease transmission and report frustration with the lack of adherence by allied professionals.45 Jeffe et al cited the need to teach medical students the importance of the use of PPE before they become set in their ways.46 Teaching medical students early in their clinical training about the risk of exposure to BBF and specific prevention measures may be associated with more positive attitudes and better compliance with precautions.
Attitudes and beliefs
Demographic factors such as gender, education levels, shift work, or occupation have not consistently found to be associated with compliance with infection control procedures.27 Compliance is affected by attitudes and perception of risk; however, having a positive attitude toward the patients, lower risk-taking tendencies, and greater knowledge of modes of transmission have been shown to lead to greater compliance.14 Use of PPE only when there is visible blood may demonstrate that HCWs make personal judgements concerning their own potential risk instead of following a consistent policy.47 HCWs do not appear to dismiss or underestimate their personal risk of acquiring an occupational infectious disease48, 49, 50; in fact, HCWs are more likely to overestimate their risk. However, several studies suggest that adherence may often be poorest when the risk of exposure is highest.22
Perceived barriers may be one of the most important factors affecting compliance. Godin et al found that HCW perceptions of their ability to adopt the use of PPE into their practice affected their level of compliance.51 If they believe that the barriers to their adherence to recommended use of PPE cannot be circumvented, they will not comply. Actual working conditions resulting in overwork, lack of time with patients, and having to deal with emergencies were reported to have significant negative affects on compliance. HCWs are influenced by the subjective norm, ie, the perception of social expectation to adopt a given behavior.51 This suggests that, if HCW believe that key persons in their work and social environment expect them to be compliant with the use of PPE, they are more likely to do so.
Certainly, organizational issues impact individual attitudes considerably. For example, workload issues are thought to affect HCW willingness to comply with recommendations for PPE use. Workers who feel stressed and overloaded at work are much less likely to be attendant to safety needs and precautions.23 Helfgott et al found that knowledge of how to prevent occupational exposure did not appear to correlate with compliance with UP.41 The most common reasons why HCWs in this study did not comply were time constraints, interference with performing specific tasks, and lack of risk-based information to assist HCWs in identifying infectious patients. It was also noteworthy that this study also found that level of compliance was inversely proportional to level of experience of the HCW. Osborne determined that mean compliance rates among Australian operating room nurses were 55.6% with always double gloving during surgical procedures and 92% with always wearing adequate eye protection.52 The variable that had the most influence on compliance was the perception of barriers to compliance, specifically, that adhering to UP interfered with duties. Nickell et al found in their study of 2001 HCWs during the SARS outbreak in Toronto that the most commonly cited difficulty with complying with precautionary measures, especially masks, was that wearing one for any extended period of time was very uncomfortable.53
Dejoy et al, in their 2000 study, demonstrated the importance of easy access to the correct PPE when needed as an influence on compliance.14 Presumably, the greater perceived availability of PPE may lead to stronger beliefs in their effectiveness for prevention among HCWs. It is interesting that the case-control study conducted by Lau et al during the SARS outbreak in Hong Kong also found that perceiving that adequate PPE was unavailable was associated with an increased risk of acquiring disease.40
The perception that the use of PPE may lead to decreased quality in the therapeutic relationship between patients and HCWs has been shown to be a significant factor that influences HCW compliance.5, 54, 55 Interference with the practitioner-patient relationship and decreased dexterity were the most frequently cited reasons for noncompliance in one study.54 Nickell et al found that, during the Toronto SARS outbreak, HCWs found that wearing of masks made communication difficult and led to a sense of social isolation.53 Others have found that the wearing of PPE places barriers between 2 people, negatively altering interpersonal dynamics and complicating the performance of tasks and treatment.14 Respirators cover the face and mouth, hampering communication, especially for the elderly population and those with hearing loss. Use of respirators may lead to increased isolation and fear among patients.56 Prieto and Clark also cited concerns among nurses that isolation of patients could lead to depression from lack of social contacts.45
Conclusion
SARS was a disease largely spread by respiratory droplets. The lack of spread within the community and the recent information on relatively low natural transmission rates for SARS coronavirus indicate that SARS is less contagious than influenza and other similar respiratory infections.1 The consistent application of basic infection control precautions terminated outbreaks in Vietnam,10 Taiwan,57 Singapore, Hong Kong,58 and, eventually, Toronto.59 Large outbreaks occurred when the causative agent was not recognized, generally early in the course of the epidemic, and basic infection control procedures were not in place. As such, attention to understanding why there was a failure to implement appropriate precautions, and how best to promote compliance in future, is an important topic for study.
This literature review has shown that variations in organizational and individual factors can explain much of the variations in self-protective behavior in health care settings, especially with respect to applying universal precautions (now called standard precautions, or routine practices). It seems likely that these factors were also important safety determinants during the SARS outbreaks but that they have not been extensively studied. The priorities for further research, which have derived from this review, are presented in Table 1. A qualitative study conducted in parallel with this review has found that organizational factors are considered to be important from the perspective of HCWs themselves.60 These broader determinants of effective infection control practices have not traditionally been addressed when policies and procedures for protecting HCWs from nosocomial infections have been designed.
Table 1.
Research priorities for organizational and individual factors to improve self-protective behavior in health care workers
| Theme | Research questions |
|---|---|
| Safety climate | What interventions can improve the safety climate in health care institutions where it is poor? |
| How have recent changes to the health care workforce (downsizing, outsourcing, etc.) affected safety climate? | |
| Training | What are the most effective methods of formative and continuing education to improve health care worker safety behavior? |
| Feedback | What are the most effective methods of providing ongoing feedback to improve health care worker safety behavior? |
| Communication | What intrainstitutional communication strategies are most effective in improving health care worker safety behaviors, especially in outbreak situations? |
Safety climate is being increasingly recognized as one of the most important determinants of safe work practice in terms of preventing exposures to BBF but has been little studied in other types of nosocomial transmitted diseases. Respiratory tract diseases, in particular, have not been well studied in this regard, presumably because most HCWs do not develop severe or specific symptoms when infected (such as for most respiratory tract viruses) or because most HCWs are already immune to potential pathogens, either through vaccination (for influenza or measles) or through natural immunity (varicella). Other diseases, such as tuberculosis, are thought to be easily controlled through the use of specific environmental controls and PPE.61 Improving the safety climate and creating a workplace culture in which workers and their health are valued has the added potential benefit of improving HCW outcomes for many different diseases and injuries, including emerging diseases of which preexisting immunity is not present. This has particular relevance to HCWs, who will likely be placed at great risk of acquiring novel strains of influenza during a pandemic.
Clearly, HCWs do need to be trained in infection control procedures to apply them, but the available evidence indicates that knowledge deficit is not a major barrier to compliance. This suggests that a focus on training content or methods to increase knowledge may not yield much change in compliance. Feedback to workers on their adherence to precautions has been identified as an important factor in facilitating compliance with infection control practices. Unfortunately, most studies that have found positive effects on compliance levels through formal education sessions have found improvements to be short lived. The optimal type, timing, and frequency of feedback that is most effective in achieving compliance are not known. Most of the reviewed studies were observational in nature, whereas many of the research questions could be investigated using intervention-based study designs. It is particularly noteworthy that the communication strategies used by health care institutions to improve worker safety have not been researched at all.
Factors other than individual knowledge likely have more influence over worker behavior. Physicians, perhaps because they operate somewhat outside the established workplace health and safety system, are often the least compliant, despite having arguably the most knowledge. Individual attitudes and beliefs that affect adherence to infection control guidelines, such as having a positive attitude toward patients and the belief in the effectiveness of recommended guidelines, are largely influenced by organizational factors in the workplace. Even when workers have the attitudes and beliefs that facilitate adherence, workload issues and ease of incorporating infection control into usual work practices may run counter to these intentions. Time and equipment to permit compliance must be available. Reduction of job-related hindrance through analysis and modification of patient care tasks and development of skill-based training may result in better compliance.
Many authors have noted with concern that some HCWs acquired SARS when wearing what should have been adequate PPE11 and have called for the use of PPE with better efficacy versus airborne particles.62 However, in light of the wide variation in organizational factors that exist in health care settings, we feel that a closer examination of these factors is warranted before concluding that these breakthrough events were due to inadequate equipment. Some attitudes such as the use of PPE interfering with patient interactions and the discomfort associated with PPE use may not change until less obtrusive and more comfortable equipment is developed. In this regard, the use of PPE with higher protection factors, but which is less comfortable, may ultimately result in less protection for HCWs. Clearly, concerns regarding field effectiveness must be considered when recommendations are made for the use of specific PPE.
This review has also revealed the relative paucity of occupational health research conducted in health care facilities. This likely reflects the traditional lack of attention that HCWs have received in terms of protecting their own health and safety. The lessons learned from SARS should be used to improve occupational health and safety for health care workers for current nosocomially transmitted infections, as well as for future potential emerging diseases.
This project was funded by The Change Foundation as part of a project entitled “Protecting the Faces of Healthcare Workers: Knowledge Gaps and Research Priorities for Effective Protection Against Occupationally-Acquired Respiratory Infectious Diseases.”60
Acknowledgments
The authors thank Mimi Doyle-Waters of the Centre for Clinical Epidemiology and Evaluation and Wendy Hunt of the Workers' Compensation Board of BC for conducting the database searches and the staff of OHSAH, who assisted in various aspects of the project.
Vancouver, British Columbia, Canada
Footnotes
Members of the British Columbia Interdisciplinary Respiratory Protection Study Group: Bob Janssen, Laurence Svirchev, Workers' Compensation Board of British Columbia; Karen Bartlett, School of Occupational and Environmental Hygiene, UBC; Mark Fitzgerald, Tom Perry, Ron Thiessen, Vancouver General Hospital; Mark Gilbert, Department of Health Care and Epidemiology, UBC; Quinn Danyluk, Fraser Health, BC; Chun-Yip Hon, Occupational Health and Safety Agency for Healthcare in British Columbia; Phil Bigelow, Department of Environmental and Radiological Health Sciences, Colorado State University; and Sharon Saunders, BC Nurses Union.
Supported in part by the Canada Research Council (to A.Y.).
References
- 1.World Health Organization. Consensus document on the epidemiology of severe acute respiratory syndrome (SARS): WHO, 2003.
- 2.Health Canada. Canadian SARS Numbers, September 3, 2003, 2003.
- 3.Health Canada. Learning from SARS: Renewal of Public Health in Canada: A report of the National Advisory Committee on SARS and Public Health: National Advisory Committee on SARS and Public Health; 2003.
- 4.Tokars J.I., McKinley G.F., Otten J., Woodley C., Sordillo E.M., Caldwell J. Use and efficacy of tuberculosis infection control practices at hospitals with previous outbreaks of multidrug-resistant tuberculosis. Infect Control Hosp Epidemiol. 2001;22:449–455. doi: 10.1086/501933. [DOI] [PubMed] [Google Scholar]
- 5.Kelen G., Giovanna T., Celentano D., Kelaninov D., Bisson L., Junkins E. Adherence to universal (barrier) precautions during interventions on critically ill and injured emergency department patients. J Acquir Immune Defic Syndr. 1990;3:987–994. [PubMed] [Google Scholar]
- 6.Hammond J.S., Eckes J.M., Gomez G.A., Cunningham D.N. HIV, trauma, and infection control: universal precautions are universally ignored. J Trauma. 1990;30:555–558. [PubMed] [Google Scholar]
- 7.Astbury C., Baxter P.J. Infection risks in hospital staff from blood: hazardous injury rates and acceptance of hepatitis B immunization. J Soc Occup Med. 1990;40:92–93. doi: 10.1093/occmed/40.3.92. [DOI] [PubMed] [Google Scholar]
- 8.Seto W.H., Tsang D., Yung R.W.H., Ching T.Y., Ng T.K., Ho M. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1519–1520. doi: 10.1016/S0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varia M., Wilson S., Sarwal S., McGeer A., Gournis E., Galanis E. Investigation of a nosocomial outbreak of severe acute respiratory syndrome (SARS) in Toronto, Canada. CMAJ. 2003;169:285–292. [PMC free article] [PubMed] [Google Scholar]
- 10.Ha L., Bloom S., Nguyen Q., Maloney S., Le Q., Leitmeyer K. Lack of SARS Transmission among Public Hospital Workers, Vietnam. Emerg Infect Dis. 2004;10:265–268. doi: 10.3201/eid1002.030707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ofner M., Lem M., Sarwal S., Vearncombe M., Simor A. Cluster of severe acute respiratory syndrome cases among protected health-care workers, Toronto, Canada, April 2003. JAMA. 2003;289:2788–2789. [PubMed] [Google Scholar]
- 12.Green L., Kreuter M., Deeds S., Partridge K. Mayfield Publishing Co.; Palo Alto, CA: 1980. Health education planning: a diagnostic approach. [Google Scholar]
- 13.DeJoy D. A behavioral-diagnostic model for fostering self-protective behavior in the workplace. In: Karwowski W., editor. Trends in ergonomics/human factors III. Elsevier Science Publishers B.V.; North-Holland: 1986. pp. 907–917. [Google Scholar]
- 14.DeJoy D.M., Searcy C.A., Murphy L.R., Gershon R.R. Behavioral-diagnostic analysis of compliance with universal precautions among nurses. J Occup Health Psychol. 2000;5:127–141. doi: 10.1037//1076-8998.5.1.127. [DOI] [PubMed] [Google Scholar]
- 15.Zohar D. Safety climate in industrial organizations: theoretical and applied implications. J Appl Psychol. 1980;65:96–101. [PubMed] [Google Scholar]
- 16.Simonds R., Shafai-Sahrai Y. Factors apparently affecting the injury frequency in eleven matched pairs of companies. J Saf Res. 1977;9:120–127. [Google Scholar]
- 17.Smith M., Cohen H., Cohen A., Cleveland R. Characteristics of successful safety programs. J Saf Res. 1978;10:5–15. [Google Scholar]
- 18.Cohen H., Cleveland R. Safety program practices in record-holding plants. Prof Saf. 1983;28:26–33. [Google Scholar]
- 19.Isla Diaz R., Diaz Cabrera D. Safety climate and attitude as evaluation measures of organizational safety. Accid Anal Prev. 1997;29:643–650. doi: 10.1016/s0001-4575(97)00015-8. [DOI] [PubMed] [Google Scholar]
- 20.Cox T., Leiter M. The health of health care organizations. Work Stress. 1992;6:219–227. [Google Scholar]
- 21.White C., Berger M. Using force-field analysis to promote use of personal protective equipment. Infect Control Hosp Epidemiol. 1992;13:752–755. doi: 10.1086/648350. [DOI] [PubMed] [Google Scholar]
- 22.DeJoy D.M., Gershon R.R.M., Murphy L.R. A work systems analysis of compliance with universal precautions among health care workers. Health Educ Q. 1996;23:159–174. doi: 10.1177/109019819602300203. [DOI] [PubMed] [Google Scholar]
- 23.Gershon R.R., Karkashian C.D., Grosch J.W., Murphy L.R., Escamilla-Cejudo A., Flanagan P.A. Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. Am J Infect Control. 2000;28:211–221. doi: 10.1067/mic.2000.105288. [DOI] [PubMed] [Google Scholar]
- 24.Ford J., Fisher S. The transfer of safety training in work organizations: a systems perspective to continuous learning. J Occup Med. 1994;9:241–259. [PubMed] [Google Scholar]
- 25.Goldstein I. Training in work organizations. In: Dunnette M., Hough L., editors. Handbook of industrial and organizational psychology. Consulting Psychologists Press; Palo Alto, CA: 1991. pp. 506–619. [Google Scholar]
- 26.Rivers D.L., Aday L.A., Frankowski R.F., Felknor S., White D., Nichols B. Predictors of nurses' acceptance of an intravenous catheter safety device. Nurs Res. 2003;52:249–255. doi: 10.1097/00006199-200307000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Gershon R.R.M., Vlahov D., Felknor S.A., Vesley D., Johnson P.C., Delclos G.L. Compliance with universal precautions among health care workers at three regional hospitals. Am J Infect Control. 1995;23:225–236. doi: 10.1016/0196-6553(95)90067-5. [DOI] [PubMed] [Google Scholar]
- 28.Gershon R.R.M., Karkashian C.D., Vlahov D., Kummer L., Kasting C., Green-McKenzie J. Compliance with universal precautions in correctional health care facilities. J Occup Environ Med. 1999;41:181–189. doi: 10.1097/00043764-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 29.DeJoy D.M., Murphy L.R., Gershon R.M. The influence of employee, job/task, and organizational factors on adherence to universal precautions among nurses. Int J Ind Ergon. 1995;16:43–55. [Google Scholar]
- 30.Salyer J. Environmental turbulence: impact in nurse performance. J Nurs Adm. 1995;25:12–20. [PubMed] [Google Scholar]
- 31.Boylan C., Russell G. Beyond restructuring. J Nurs Adm. 1997;27:13–20. doi: 10.1097/00005110-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Hall L., Donner G. The changing role of hospital nurse managers: a literature review. Can J Nurs Adm. 1997;10:14–39. [PubMed] [Google Scholar]
- 33.Curran C. Changing the way we do business. Nurs Econ. 1991;9:296–297. [PubMed] [Google Scholar]
- 34.Shindal-Rothschild J., Duffy M. The impact of restructuring and work design on nursing practice and patient care. Best Pract Benchmarking Healthcare. 1996;1:271–282. [PubMed] [Google Scholar]
- 35.DiGiacomo J.C., Hoff W.S., Rotondo M.F., Martin K., Kauder D.R., Anderson H.L., III Barrier precautions in trauma resuscitation: real-time analysis utilizing videotape review. Am J Emerg Med. 1997;15:34–39. doi: 10.1016/s0735-6757(97)90044-9. [DOI] [PubMed] [Google Scholar]
- 36.Moongtui W., Gauthier D.K., Turner J.G. Using peer feedback to improve handwashing and glove usage among Thai health care workers. Am J Infect Control. 2000;28:365–369. doi: 10.1067/mic.2000.107885. [DOI] [PubMed] [Google Scholar]
- 37.Kim L.E., Jeffe D.B., Evanoff B.A., Mutha S., Freeman B., Fraser J. Improved compliance with universal precautions in the operating room following an educational intervention. Infect Control Hosp Epidemiol. 2001;22:522–524. doi: 10.1086/501945. [DOI] [PubMed] [Google Scholar]
- 38.Bero L., Grilli R., Grimshaw J., Harvey E., Oxman A., Thomson M. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote implementation of research findings by health care professionals. BMJ. 1998;317:465–468. doi: 10.1136/bmj.317.7156.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grol R., Dalhuijsen J., Thomas S., Veld C., Rutten G., Mokkink H. Attributes of clinical guidelines that influence use of guidelines in general practice: observational study. BMJ. 1998;317:858–861. doi: 10.1136/bmj.317.7162.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lau J., Fung K., Wong T., Kim J., Wong E., Chung S. SARS transmission among hospital workers in Hong Kong. Emerg Infect Dis. 2004;10:280–286. doi: 10.3201/eid1002.030534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Helfgott A.W., Taylor-Burton J., Garcini F.J., Eriksen N.L., Grimes R. Compliance with universal precautions: knowledge and behavior of residents and students in a department of obstetrics and gynecology. Infect Dis Obstet Gynecol. 1998;6:123–128. doi: 10.1002/(SICI)1098-0997(1998)6:3<123::AID-IDOG5>3.0.CO;2-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Young E.W., Forti E.M., Preston D.B. Rural nurses' use of universal precautions in relation to perceived knowledge of patient's HIV status. Int J Nurs Stud. 1996;33:249–258. doi: 10.1016/0020-7489(95)00057-7. [DOI] [PubMed] [Google Scholar]
- 43.Afif W., Huor P., Brassard P., Loo V.G. Compliance with methicillin-resistant Staphylococcus aureus precautions in a teaching hospital. Am J Infect Control. 2002;30:430–433. doi: 10.1067/mic.2002.125174. [DOI] [PubMed] [Google Scholar]
- 44.Angtuaco T., Oprescu F., Lal S., Pennington J., Russell B., Co J. Universal precautions guideline: self-reported compliance by gastroenterologists and gastrointestinal endoscopy nurses–a decade's lack of progress. Am J Gastroenterol. 2003;98:2420–2423. doi: 10.1111/j.1572-0241.2003.07694.x. [DOI] [PubMed] [Google Scholar]
- 45.Prieto J., Clark J. Infection control. Dazed and confused … the implementation of infection control policies and guidelines. Nurs Times. 1999;95:49–53. [PubMed] [Google Scholar]
- 46.Jeffe D.B., Mutha S., L'Ecuyer P.B. Healthcare workers' attitudes and compliance with universal precautions: gender, occupation, and specialty differences. Infect Control Hosp Epidemiol. 1997;18:710–712. doi: 10.1086/647517. [DOI] [PubMed] [Google Scholar]
- 47.Evanoff B., Kim L., Mutha S., Jeffe D., Haase C., Andereck D. Compliance with universal precautions among emergency department personnel caring for trauma patients. Ann Emerg Med. 1999;33:160–165. doi: 10.1016/s0196-0644(99)70389-6. [DOI] [PubMed] [Google Scholar]
- 48.Cooke M. House staff attitudes towards the acquired immunodeficiency virus. AIDS Public Policy J. 1988;3:59–60. [Google Scholar]
- 49.Becker M., Janz N., Band J., Bartly J., Snyder M., Gaynes R. Noncompliance with universal precautions policy: why do physicians and nurses recap needles? Am J Infect Control. 1990;18:232–239. doi: 10.1016/0196-6553(90)90164-n. [DOI] [PubMed] [Google Scholar]
- 50.Hoffman-Terry M., Rhodes L., Reed J. Impact of human immunodeficiency virus on medical and surgical residents. Arch Intern Med. 1992;152:1788–1796. [PubMed] [Google Scholar]
- 51.Godin G., Naccache H., Morel S. Determinants of nurses' adherence to universal precautions for venipunctures. Am J Infect Control. 2000;28:359–364. doi: 10.1067/mic.2000.107594. [DOI] [PubMed] [Google Scholar]
- 52.Osborne S. Influences on compliance with standard precautions among operating room nurses. Am J Infect Control. 2003;31:415–423. doi: 10.1067/mic.2003.68. [DOI] [PubMed] [Google Scholar]
- 53.Nickell L., Crighton E., Tracy C., Al-Enazy H., Bolaji Y., Hanjrah S. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. 2004;170:793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Willy M., Dhillon G., Loewen N., Wesley R., Henderson D. Adverse exposures and universal precautions practices among a group of highly exposed health professionals. Infect Control Hosp Epidemiol. 1990;11:351–356. doi: 10.1086/646186. [DOI] [PubMed] [Google Scholar]
- 55.Linn L., Kahn K., Leake B. Physicians' perceptions about increased glove-wearing in response to risk of HIV infection. Infect Control Hosp Epidemiol. 1990;11:248–254. doi: 10.1086/646162. [DOI] [PubMed] [Google Scholar]
- 56.Fennelly K.P. Personal respiratory protection against Mycobacterium tuberculosis. Clin Chest Med. 1997;18:1–17. doi: 10.1016/s0272-5231(05)70352-x. [DOI] [PubMed] [Google Scholar]
- 57.Hsieh Y.-H., Chen C.W.-S. Severe acute respiratory syndrome–numbers do not tell whole story. BMJ. 2003;326:139–146. doi: 10.1136/bmj.326.7403.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Abdullah A.S.M., Tomlinson B., Cockram C.S., Thomas G.N. Lessons from the severe acute respiratory syndrome outbreak in Hong Kong. Emerg Infect Dis. 2003;9:1042–1045. doi: 10.3201/eid0909.030366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wallington T., Berger L., Henry B., Shahin R., Yaffe B., Mederski B. Update: severe acute respiratory syndrome, Toronto, Canada, 2003. JAMA. 2003;290:457–458. [PubMed] [Google Scholar]
- 60.Yassi A, Bryce E, Moore D, Janssen R, Copes R, Bartlett K, et al. Protecting the faces of health care workers: knowledge gaps and research priorities for effective protection against occupationally-acquired respiratory infectious diseases: The Change Foundation; 2004.
- 61.Palmore T.N., Sepkowitz K.A. Occupational risk of tuberculosis among healthcare workers. Clin Occup Environ Med. 2002;2:609–629. [Google Scholar]
- 62.Nicas M., Harrison R., Charney W., Borwegan B. Respiratory protection and severe acute respiratory syndrome. J Occup Environ Med. 2004;46:195–197. doi: 10.1097/01.jom.0000116808.46760.06. [DOI] [PubMed] [Google Scholar]


