Abstract
The sudden emergence of 2009 H1N1 influenza in the spring of that year sparked a surge in visits to emergency departments in New York City and other communities. A larger, second wave of cases was anticipated the following autumn. To reduce a potential surge of health system utilization without denying needed care, we enlisted the input of experts from medicine, public health, nursing, information technology, and other disciplines to design, test, and deploy clinical algorithms to help minimally trained health care workers and laypeople make informed decisions about care-seeking for influenza-like illness. The product of this collaboration, named Strategy for Off-Site Rapid Triage (SORT) was disseminated in 2 forms. Static algorithms, posted on the Centers for Disease Control and Prevention's Web site, offered guidance to clinicians and telephone call centers on how to manage adults and children with influenza-like illness. In addition, 2 interactive Web sites, http://www.Flu.gov and http://www.H1N1ResponseCenter.com, were created to help adults self-assess their condition and make an informed decision about their need for treatment. Although SORT was anchored in a previously validated clinical decision rule, incorporated the input of expert clinicians, and was subject to small-scale formative evaluations during rapid standup, prospective evaluation is lacking. If its utility and safety are confirmed, SORT may prove to be a useful tool to blunt health system surge and rapidly collect epidemiologic data on future disease outbreaks.
Introduction
The emergence of a novel strain of H1N1 influenza (“2009 H1N1”) in North America in spring 2009 caught public health authorities by surprise. Because many people were susceptible and a vaccine would not be available for many months, experts predicted that the virus could rapidly infect 30% to 50% of the population.
In this article, we describe how a large number of clinical and public health experts came together to rapidly create, refine, and deploy the Strategy for Off-Site Rapid Triage (SORT), a set of clinical algorithms designed to help minimally trained health care workers and laypeople make informed decisions about care-seeking in the setting of a hypothetical influenza pandemic. Ultimately, SORT was adopted, with minor modifications, by the Centers for Disease Control and Prevention (CDC) and offered free to the public through interactive Web sites supported by the US Department of Health and Human Services (http://www.Flu.gov) and the Microsoft Corporation (http://www.H1N1ResponseCenter.com). The rapid emergence and spread of 2009 H1N1 precluded prospective evaluations of SORT before its deployment. Now that the immediate crisis is past, prospective studies are needed to affirm SORT's safety and utility and to further explore the feasibility of using the Web and other bidirectional technologies to reduce surge and collect real-time epidemiologic information about rapidly emerging public health threats.
Background
The 2009 H1N1 influenza pandemic is the first the world has faced in 40 years.1 Four previous flu pandemics have been studied in detail: 1889 to 1892, 1918 to 1920, 1957 to 1960, and 1968 to 1970. In each, localized, often mild outbreaks were followed some months later by massive waves of illness and mortality, often in younger age groups.2 Virulence varied widely; the 1918 to 1920 pandemic (also caused by an H1N1 strain) was by far the worst, killing 20 to 40 million people worldwide. The 1968 to 1970 pandemic was the mildest of the 4. But in each instance, the toll of deaths and illness substantially exceeded that of a typical flu season.3
Because pandemic monitoring was primarily focused on Asia, public health officials were caught by surprise when a novel strain of H1N1 influenza suddenly emerged in the Western Hemisphere at the end of a regular flu season. Initially, the high number of reported fatalities relative to hospitalized cases in Mexico suggested that the virus was highly lethal. This prompted Mexican health authorities to close schools, cancel public events, and impose other community disease mitigation strategies in hopes of limiting the outbreak's effects.
As 2009 H1N1 quickly spread across the United States, epidemiologists determined that the virus was not particularly virulent.4 Unlike most influenza strains, it tended to spare the elderly, perhaps because many older Americans have some degree of preexisting immunity to H1N1 viruses. But the virus greatly affected children and young adults. Many who died in the first wave of illness had underlying medical problems, but some were previously healthy individuals.5, 6 Word of these deaths provoked widespread anxiety and prompted many to seek immediate medical attention, regardless of the nature or severity of their symptoms.
In August 2009, the President's Council of Advisors on Science and Technology (PCAST) reported on preparations for 2009 H1N1 influenza.7 Although it was generally understood by that point that the virus was less dangerous than first feared, PCAST concluded that it still represented a serious public health threat. “The issue” PCAST warned, “is not that the [2009 H1N1] virus is more deadly than other flu strains, but rather that it is likely to infect more people than usual because it is a new strain against which few people have immunity. This could mean that doctors' offices and hospitals may get filled to capacity.”7
The PCAST predicted that 2009 H1N1 could infect 30% to 50% of the population and produce symptoms in 20% to 40%. If even half that number sought medical attention, the pandemic would send 30 to 60 million Americans into an already heavily burdened emergency care system.8 Early experience appeared to justify the council's concern. Between May 15 and June 15, more than 44,000 people with influenza-like illness had visited New York City emergency departments (EDs) compared with 4,267 the year before. Total ED visits increased by 32%, from 325,135 the previous year to more than 428,000.9 In some communities, ED use surged by 50% to 100%.10 Because the second wave of influenza pandemics is typically larger than the first, officials worried at the time that a sustained surge of ED visits could worsen already dangerous waits for emergency care,11 overload EDs, and promote iatrogenic transmission of influenza from individuals with flu to medically fragile patients nearby.
The Origin of SORT
Four months before 2009 H1N1 emerged, the Emory University Department of Emergency Medicine and Emory Office of Critical Event Preparedness and Response in Atlanta, GA, convened an interdisciplinary expert group to devise a clinical algorithm for use in future influenza pandemics (Figure). Their goal was to create a simple but accurate tool that could help minimally trained health care workers screen large numbers of patients with influenza-like illness. The meeting was sponsored by the Georgia Division of Public Health as part of its pandemic influenza preparedness activity.12 Supplemental funding was provided by the Robert W. Woodruff Foundation and later by the de Beaumont Foundation. The group named the product of their deliberations Strategy for Offsite Rapid Triage, or SORT.
Figure.
Participants* in the SORT development meeting: December 10 to 11, 2008.
Before the meeting, 3 group members (A.P.I., B.D., T.C.B.; see acknowledgements) conducted an adjudicated literature search to identify clinical decision rules that are designed to identify patients who are severely ill with pneumonia or other conditions. Candidate clinical decision rules were presented to the full group. After a period of discussion, all agreed that the United Kingdom's CRB-65 (4 components of the score: Confusion, Respiratory rate greater than 24 breaths per minute, systolic Blood pressure less than 100 millimeters of mercury and age greater than or equal to 65 years) score was best suited to anchor the proposed influenza-like illness algorithm. The CRB-65 score was selected because it uses simple signs and symptoms, does not require diagnostic testing, and accurately quantifies illness severity in patients with pneumonia.13
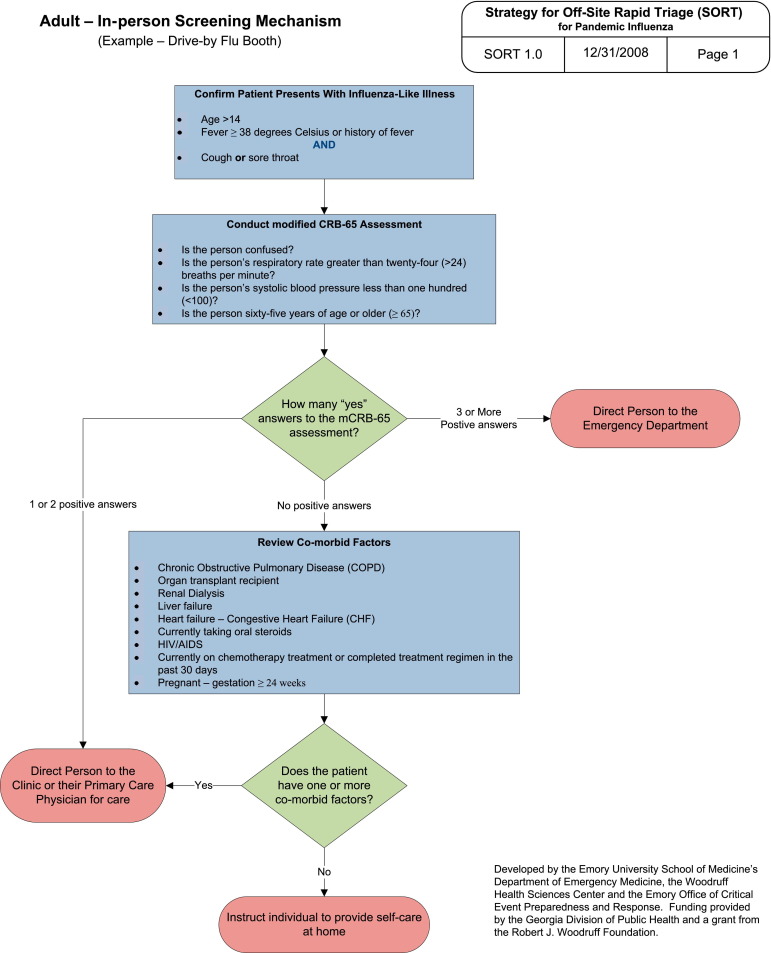
The group then developed an efficient, 3-step process to assess patients with influenza-like illness. In the first step, patients are screened to determine whether they meet CDC criteria for influenza-like illness. Those who do proceed to the second step, an assessment of illness severity using questions adopted from the CRB-65 score. Patients with influenza-like illness who have a CRB-65 score of 0 (suggesting relatively mild illness) move on to the third step, a short series of questions designed to determine whether they have a health condition that increases their risk of developing severe complications of influenza.
According to the patient's answers, SORT assigns a level of risk and recommends a specific action. Patients with “high-risk” influenza-like illness—in the group's first iteration of the algorithm, those with a CRB-65 score of 3 or more—would be sent directly to an ED. “Intermediate-risk” patients—CRB score of 1 or 2 or comorbid conditions that increase their risk of complications—would be advised to contact their physician or seek care in a walk-in clinic because early administration of antiviral medication might reduce the chance of complications. “Low-risk” patients—those with mild disease (CRB-65=0) and no comorbid conditions—would be advised to convalesce at home.
SORT was initially envisioned for use by minimally trained health care workers at off-site flu assessment stations and walk-in clinics. But the development group quickly realized that a slightly modified version—one that substitutes symptoms for measured respiratory rate and blood pressure—could be used by call centers or even self-administered through an interactive Web site. Ultimately, both versions were included in the group's work product (Figure E1, available online at http://www.annemergmed.com).
Figure E1.
SORT version 1.0.
Refinement and Validation
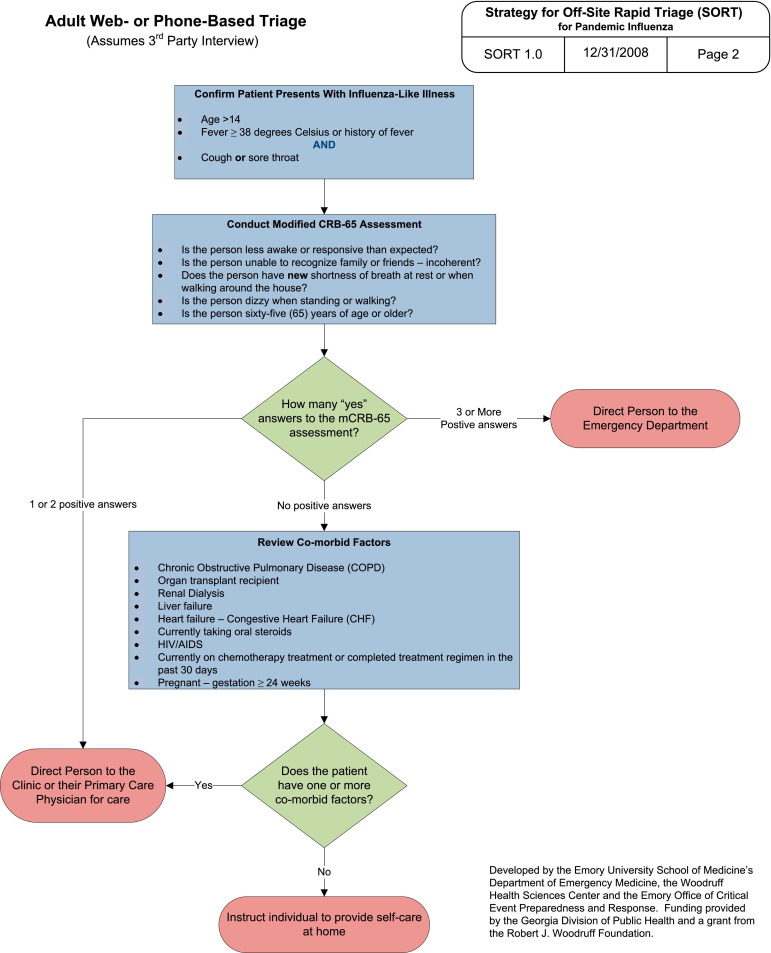
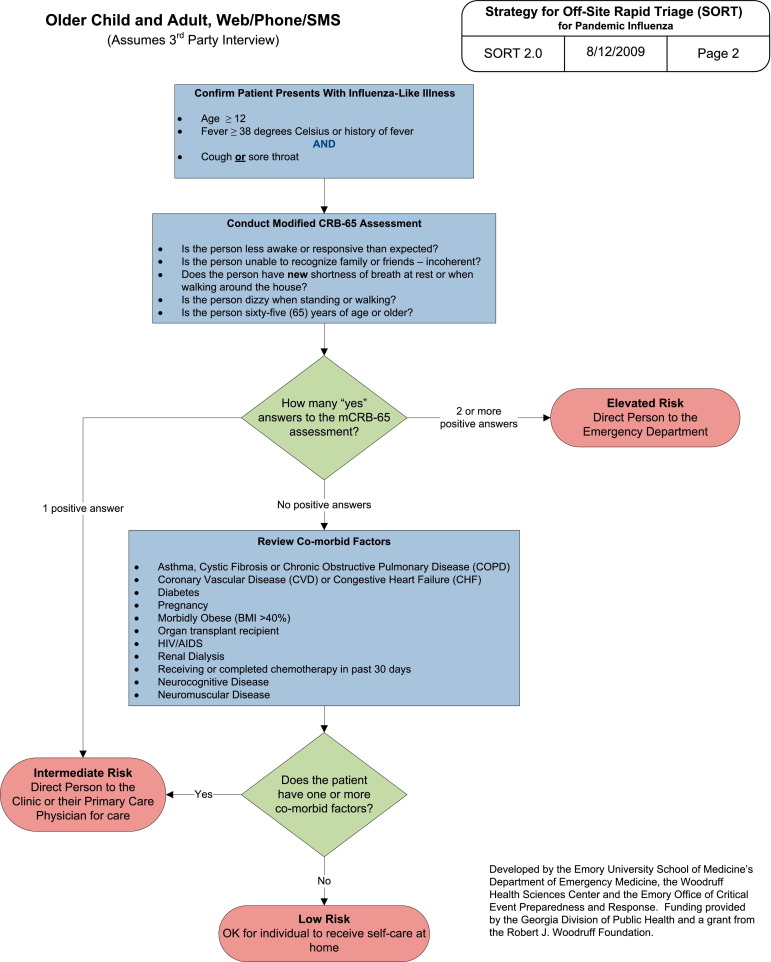
When 2009 H1N1 influenza emerged 4 months later, we reexamined SORT 1.0 in light of what was being learned about the new virus.14, 15 According to early reports from the CDC and the World Health Association (WHO), we added several risk factors to our list: pregnant, morbidly obese (body mass index >40%), asthma, cystic fibrosis, coronary vascular disease, and neuromuscular or neurocognitive disease. We also decreased the threshold for being categorized as high risk from a CRB-65 score of 3 to 2 (Figure E2, available online at http://www.annemergmed.com).
Figure E2.
SORT version 2.0.
To assess the utility and safety of the revised algorithm, colleagues in New York City and Los Angeles agreed to retrospectively assess how SORT 2.0 would have performed had it been used to screen patients with influenza-like illness in their EDs earlier that spring. Because a primary objective of SORT is to identify patients with influenza-like illness who can safely recover at home, we were particularly interested in assessing its negative predictive value. These audits did not require individual identifiers, sought no sensitive information, involved no therapeutic interventions, and analyzed data in aggregate, so they were determined to be exempt by Emory's institutional review board.
Colleagues at the Montefiore ED reported that SORT 2.0 would have classified 60 of 102 influenza-like illness visits (60%) as low risk. Five of the low-risk patients were hospitalized, mainly for social reasons. (J. Gallagher, personal communication, August 11, 2009). At the New York University Langone Medical Center ED, SORT 2.0 classified 40 of 87 patients with influenza-like illness (47%) as low risk. One low-risk patient was admitted. Although he was afebrile, had normal vital signs, and had normal oxygenation, he was found to have pneumonia and a WBC count of 1,500 (I. Portelli and S. Smith, personal communication, August 18, 2009). At UCLA/Olive View Medical Center, 2 of 36 patients with low-risk influenza-like illness were hospitalized. Both had intractable vomiting (L. Baraff, personal communication, August 20, 2009).
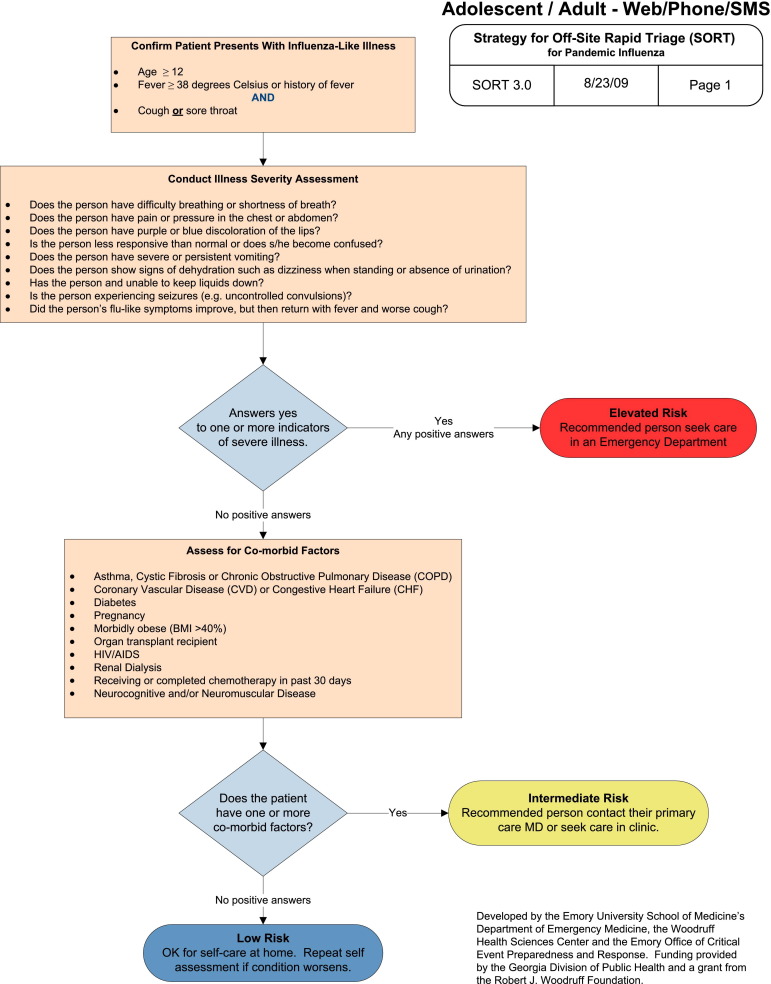
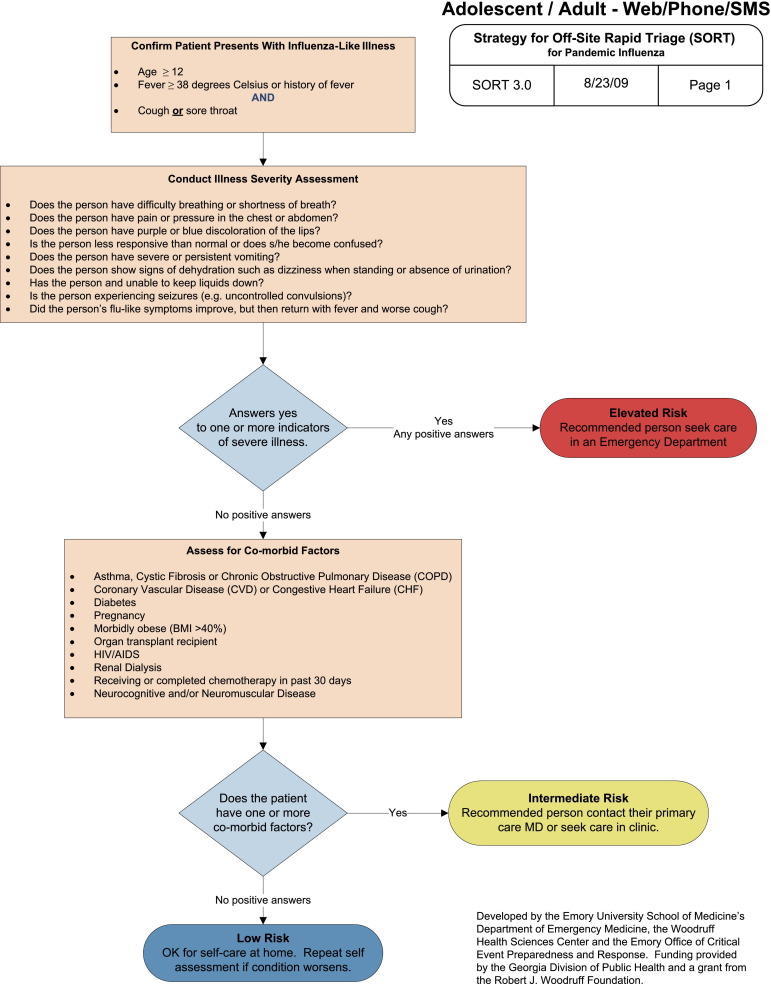
According to these observations and additional epidemiologic data from the CDC and WHO, we added intractable vomiting, chest pain, and recrudescence as high-risk symptoms. To minimize the risk of false-negative results, we recalibrated the algorithm to send patients with even one high-risk symptom to the ED (Figure E3, available online at http://www.annemergmed.com). The Kaiser Permanente Colorado Institute for Health Research agreed to perform a retrospective assessment, using their health system's computerized records, to determine how well SORT 3.0 would have performed had it been used to screen patients with influenza-like illness. Between April 1 and June 30, 2009, 2,758 outpatients with influenza-like illness visited the Kaiser Permanente Colorado health system. SORT 3.0 categorized 1,540 of these encounters (56%) as low risk. During the next 2 weeks, 7 low-risk patients were hospitalized, but only 2 had problems that were related to the index visit (negative predictive value 99.9%). Intermediate-risk patients were much more likely to be admitted within 2 weeks than low-risk patients (odds ratio 11.9; 95% confidence interval 5.29 to 26.9) (D. Magid, personal communication, August 23, 2009).
Figure E3.
SORT version 3.0.
Buoyed by these findings, we developed a demonstration Web site with branching logic to depict how patients could use SORT to self-assess their need for care. To ensure that the site was comprehensible to laypeople, we asked experts in health literacy at our institution to translate SORT's clinical terms into plain language.16 More than 100 lay volunteers of widely varying age, race, and socioeconomic status reviewed draft text and offered suggestions on how to make the content understandable and actionable. Some had an influenza-like illness when they participated; others had recently recovered from the flu.
On September 3 to 4, 2009, we presented draft adult and pediatric SORT algorithms and our demonstration Web site at a hastily convened Institute of Medicine workshop titled “Assessing the Severity of Influenza-Like Illnesses: Clinical Algorithms to Inform and Empower Health Care Professionals and the Public.”17 The event, which was sponsored by UnitedHealth Group, attracted national leaders from academia, major clinical societies, public health, law, government, and private industry. Feedback was highly favorable.
Deployment
From that point forward, the pace of events accelerated. On October 2, 2009, the CDC adopted a slightly modified version of SORT 3.0 and posted it on the agency's Web site at http://cdc.gov/h1n1flu/clinicians/pdf/adultalgorithm.pdf. In an accompanying disclaimer, the CDC stated that the algorithm was intended for use “by physicians and those working under their supervision.” It was also limited to patients older than 18 years. Five days later, US Department of Health and Human Services (HHS) secretary Katherine Sibelius announced the posting of an H1N1 self-evaluation application at http://www.Flu.gov. It closely adheres to the CDC's adult algorithm and used many of the terms and phrases we devised for our demonstration Web site. It is intended for use by adults older than 18 years. The same day (October 7, 2009), Microsoft Corporation unveiled its own flu self-assessment application at http://www.H1N1ResponseCenter.com. Like Flu.gov's application, Microsoft's site closely adheres to the CDC's adult algorithm and uses health-literate language licensed, at no charge, from Emory University. Both HHS and Microsoft encouraged health departments, nongovernmental organizations, private health plans, employers, and other organizations to link to their Web sites free. Many chose to do so.
Three major specialty societies endorsed elements of the effort. The American College of Emergency Physicians was the first major group to endorse SORT, on September 9 (N. Jouriles, personal communication). The American College of Physicians followed suit on October 19 (J. Stubbs, personal communication). The American Academy of Pediatrics worked directly with the CDC on a pediatric algorithm, which was posted on the CDC's Web site on October 16 (http://www.cdc.gov/h1n1flu/clinicians/pdf/childalgorithm.pdf). As soon as this pediatric algorithm was posted, we began drafting health-literate content to offer the guidance directly to the public through the Web. Unfortunately, the American Academy of Pediatrics opposed this effort because the algorithm was not prospectively validated. Concerns were also expressed that an interactive pediatric Web site might discourage some parents from contacting their child's medical provider.
Notwithstanding this disappointment, the overall effort to create, test, and deploy SORT was highly collaborative from beginning to end. Numerous organizations and individuals gave freely of their time and expertise (see acknowledgements). Recognizing the urgency of the effort, Emory's Office of Technology Transfer readily licensed the technology, at no charge, to any vendor who agreed to provide it free.
Initial Experience
Between October 7, 2009, and February 24, 2010, Flu.gov recorded 721,906 total page views, 320,333 visits to Flu.gov/evaluation (the opening page of the self-evaluation site), and 230,761 completed evaluations to flu.gov/evaluation/index2.html (A. Roszak, personal communication). To reassure the public that the federal government would respect each user's privacy, HHS did not retain data on site visitors. As a consequence, we have no additional information.
Between October 5 and December 13, 2009, Microsoft's Web site, http://www.H1N1ResponseCenter.com, was visited 1.6 million times. Of the 442,000 visitors (28%) who completed a self-assessment, slightly less than half (N=202,000) chose to share anonymous data with the site. Preliminary analysis indicates that 37% of these visitors provided answers that categorized them as high risk and 13% were too young to receive guidance. The other half either did not meet influenza-like illness criteria or were assessed as not requiring ED treatment. Microsoft did not identify visitors who used the site multiple times, so it is possible that some individuals repeatedly entered positive replies.
Limitations
Despite our best efforts, SORT was not deployed until early October 2009, when the pandemic's peak had nearly passed. The CDC did not actively promote the static algorithms posted on its Web site. HHS and Microsoft did not aggressively market their interactive, self-assessment Web sites. News coverage did, however, generate some “free media.”
Beyond counting Web hits, we cannot determine SORT's effect on care-seeking and patient safety. Although we received no reports of adverse events associated with use of SORT, we cannot exclude the possibility that some patients delayed care and experienced harm as a result. It is also possible that SORT was so conservative that it encouraged some patients to make an unnecessary trip to the ED. Prospective evaluations, including criterion-standard comparisons and follow-up studies, are needed to fully assess SORT's utility and safety.
Discussion
As this article goes to press, 2009 H1N1 appears to be the mildest flu pandemic on record, at least in the United States. The CDC estimates that between April 2009 and January 16, 2010, between 8,330 and 17,160 deaths related to 2009 H1N1 occurred. The midlevel estimate is 11,690 deaths.18 Although any death is tragic, this toll is less than that associated with a typical year of seasonal flu, much less a pandemic year.2, 3, 4 2009 H1N1 did, however, cause considerable morbidity. According to the CDC, between 183,000 and 378,000 H1N1-related hospitalizations occurred during the same interval. The midlevel estimate is 257,000 hospitalizations. The CDC projects that between 41 and 84 million Americans were infected with 2009 H1N1.17 The midlevel estimate is 57 million, close to the lower boundary of 60 million predicted by the PCAST in August 2009.7
Influenza is a notoriously unpredictable virus. 2009 H1N1 may remain relatively mild or it could mutate in the coming months to become more virulent. Continued vigilance is warranted.
Our experience illustrates both the opportunities and challenges of Web-based self-evaluation to limit a health system surge. In less than 12 months, a large, diverse, and highly motivated group of experts representing multiple disciplines took SORT from a hypothetical concept to reality. With the help of the US government and one of America's top technology companies, 2 static algorithms and 2 interactive Web sites were deployed nationwide. Originally envisioned to help health care workers make informed decisions about where to direct patients for treatment of influenza-like illness, SORT rapidly evolved into a decision support tool for the general public. We hoped to safely and responsibly reduce a surge of visits to EDs and other health care facilities while encouraging those who truly need care to receive it.
The Web sites we helped devise were used approximately 650,000 times. We have no way to determine how many times the CDC's adult and pediatric algorithms were used by clinicians and call centers. No adverse events were reported. Microsoft's data suggests that their Web site may have prevented as many as 100,000 ED visits, although the true total is probably less. Because HHS did not record data on visitors to Flu.gov, we cannot estimate the effect of their self-assessment tool.
Several challenges remain. Because of the rapid emergence of 2009 H1N1, we were unable to follow the lengthy timetable normally required to methodically develop and validate a new clinical decision rule. We attempted to compensate for this fact by anchoring SORT in a previously validated clinical decision rule.
Some clinicians may question the wisdom of providing decision support directly to the public. The legal and political risks of misclassifying severely ill patients compelled us to make each generation of SORT more conservative than the last. The resulting increase in sensitivity came, no doubt, at the expense of specificity, which probably limited SORT's effect on surge. Microsoft's data suggest that their current version overtriages patients to some degree. Prospective research is needed to determine whether SORT and other Web-based tools can be made more precise without compromising safety.
Many individuals and organizations contributed time and effort to this project. However, future efforts to address the threat of health system surge should not depend on good will alone. Public health preparedness warrants the same level of societal commitment afforded to vaccine development and other disease control efforts.
Now that the immediate crisis is past, SORT should be prospectively evaluated to confirm its safety and effectiveness. Given 2009 H1N1's effect on children, it will be particularly important to assess SORT in pediatric age groups. One way to do this is to ask the parents of children with flu-like symptoms to complete a Web-based assessment immediately before their child is examined by a clinician. The 2 assessments can then be compared, with the clinical examination as the criterion standard. Existing research networks, such as the CDC's EMERGEncy ID Net19 or the Health Resources and Services Administration Pediatric Emergency Care Applied Research Network,20 are well suited to this task.
SORT is but one example of how information technology may be used to empower patients to make prudent decisions about their health. Although SORT is designed to assess patients with influenza-like illness, the 3-step approach it uses (screening, severity assessment, associated risk factors) may be used to evaluate many illnesses. SORT-like algorithms for selected public health threats such as severe acute respiratory syndrome could be even be prepared and evaluated in advance and deployed if needed. This method could help reassure a nervous public, particularly in the early phases of an outbreak when many people otherwise rush to the nearest ED.
With additional refinement, Web-based decision-support tools such as SORT may be used to collect important epidemiologic information about disease incidence and severity in nonhospitalized individuals. Information of this type is vital to quickly characterize a new disease's attack rate and virulence. Initial assessment of the 2009 H1N1 outbreak in Mexico was hindered by lack of knowledge about the number and distribution of nonhospitalized cases. As a result, Mexican officials did not know whether they were dealing with the early stages of a highly lethal outbreak (what was initially feared) or an already established epidemic with relatively few deaths (the picture that subsequently emerged in the United States). Someday, bidirectional technologies such as the World Wide Web and short messaging service21 may be used to generate “epidemic science in real time.”22
Conclusion
Advances in biomedical science have given us new vaccines, antimicrobials, and diagnostic tests. Information technology has progressed at an equal, if not greater, pace, but it has not been exploited to the same degree. SORT is but one example of how the Web and other bidirectional technologies may be used to inform and empower the public to make prudent health care decisions. In the future, information technology may revolutionize public health preparedness by providing new and powerful ways to detect, contain, and mitigate public health threats.
Acknowledgments
Numerous individuals and organizations contributed to this effort. Although their listing here does not constitute their personal endorsement of this article or every aspect of the project, we are nonetheless indebted to them for their contributions and wisdom. Contributors include, but are not limited to, Larry Baraff, MD, T. Christopher Bond, PhD, Holley Butkovich, Lorenzo DiFrancesco, MD, Barry Diner, MD, Alexandra Drane, Harvey Fineberg, MD, John Gallagher, MD, Lewis Goldfrank, MD, Lynn R. Goldman, PhD, Michael Handrigan, Kara Jacobsen, MA, John A. Jernigan, MD, Nicholas Jouriles, MD, Rebecca Katz, PhD, Priscilla Keith, JD, Naghma Khan, MD, Steve Krug, MD, Adam Landman, MD, Hal C. Lawrence, MD, Linda Lawrence, MD, Weimin Lu, MBA, Nicole Lurie, MD, Gene W. Matthews, MD, Meg McCoy, JD, John A. Mitas, MD, Arnold S. Monto, MD, Robert Nadolski, Kristine Nash-Wong, Andy Pope, PhD, Ian Portelli, MD, Lynne Richardson, MD, Andrew Roszak, JD, EMT-P, Jeffrey Runge, MD, Judith Salerno, PhD, Harold Simon, MD, Joseph Stubbs, MD, Todd Taylor, MD, Reed Tuckson, MD, Silas Smith, MD, and Charlotte Yeh, MD.
Footnotes
Supervising editor: Amy H. Kaji, MD, PhD
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article that might create any potential conflict of interest. See the Manuscript Submission Agreement in this issue for examples of specific conflicts covered by this statement. This work was supported in part by a contract from the Georgia Division of Public Health and grants from the Robert W. Woodruff Foundation and the de Beaumont Foundation.
Publication date: Available online June 3, 2010.
Appendix
References
- 1.Dawood F.S., Jain S., Finelli L., Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–2615. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 2.Miller M.A., Viboud C., Balinska M. The signature features of influenza pandemics—implications for policy. N Engl J Med. 2009;360:2595–2598. doi: 10.1056/NEJMp0903906. [DOI] [PubMed] [Google Scholar]
- 3.Taubenberger J.K., Morens D.M. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. January 2006 doi: 10.3201/eid1201.050979. http://www.cdc.gov/ncidod/EID/vol12no01/05-0979.htm (Serial on the Internet.) Accessed March 13, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention CDC estimates of 2009 H1N1 influenza cases, hospitalizations and deaths in the United States, April–December 12, 2009. January 15, 2010. http://www.cdc.gov/h1n1flu/estimates/April_December_12.htm Accessed March 13, 2010.
- 5.Louie J.K., Acosta M., Winter K. Factors associated with death or hospitalization due to pandemic 2009 influenza A (H1N1) infection in California. JAMA. 2009;302:1896–1902. doi: 10.1001/jama.2009.1583. [DOI] [PubMed] [Google Scholar]
- 6.Guillermo D.-C., Lapinsky S.E., Macias A.E. Critically ill patients with 2009 influenza A(H1N1) in Mexico. JAMA. 2009;302:1880–1887. doi: 10.1001/jama.2009.1536. [DOI] [PubMed] [Google Scholar]
- 7.President's Council of Advisors on Science and Technology . Executive Office of the President; Washington, DC: 2009. Report to the President on US Preparations for 2009–H1N1 Influenza. [Google Scholar]
- 8.Committee on the Future of Emergency Care in the US Health System, Institute of Medicine . National Academies Press; Washington, DC: 2006. Hospital Based Emergency Care: At the Breaking Point. [Google Scholar]
- 9.Hartocollis A. New York Times. July 21, 2009. NY braces for swine flu return; p. A1. [Google Scholar]
- 10.Levey N. Los Angeles Times. May 11, 2009. Hospitals swamped amid flu fears. [Google Scholar]
- 11.US Government Accountability Office . Government Accountability Office; Washington, DC: 2009. Hospital Emergency Departments: Crowding Continues to Occur, and Some Patients Wait Longer than Recommended Time Frames. GAO-09-347. [Google Scholar]
- 12.Lotstein D., Leuschner K.J., Ricci K.A. RAND Corp; Santa Monica, CA: 2009. PREPARE for Pandemic Influenza: A Quality Improvement Toolkit.http://www.rand.org/pubs/technical_reports/TR598 Accessed April 4, 2010. [Google Scholar]
- 13.Bower T., Ewig S., Marre R. CRB-65 predicts death from community acquired pneumonia. J Intern Med. 2006;260:93–101. doi: 10.1111/j.1365-2796.2006.01657.x. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention CDC health update: interim guidance—children and pregnant women who may be infected with swine-origin influenza virus: considerations for clinicians. Distributed via Health Alert Network. April 28, 2009, 11:45 PM ET. CDCHAN-00285-09-04-28-UPD-N. http://www.cdc.gov/h1n1flu/HAN/042809.htm Accessed March 23, 2010.
- 15.World Health Organization WHO technical consultation on the severity of disease caused by the new influenza A (H1N1) virus infections. http://www.who.int/csr/resources/publications/swineflu/technical_consultation_2009_05_06/en/index.html Revised full report posted May 9, 2009 (short summary originally posted May 6, 2009) Accessed March 23, 2010.
- 16.Committee on Health Literacy, Institute of Medicine . National Academies Press; Washington, DC: 2004. Health Literacy: A Prescription to End Confusion. [Google Scholar]
- 17.Institute of Medicine Assessing the severity of influenza-like illnesses: clinical algorithms to inform and empower health care professionals and the public. http://www.iom.edu/Activities/PublicHealth/MedPrep/2009-SEP-03.aspx Accessed October 25, 2009.
- 18.Centers for Disease Control and Prevention CDC estimates of 2009 H1N1 influenza cases, hospitalizations and deaths in the United States, April 2009–January 16, 2010. http://www.cdc.gov/h1n1flu/estimates_2009_h1n1.htm#Table Cumulative CDC Home. Published March 3, 2010. Accessed March 5, 2010.
- 19.Talan D.A., Moran G.J., Mower W.R. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Clin Infect Dis. 1999;28:401–402. doi: 10.1086/517199. [DOI] [PubMed] [Google Scholar]
- 20.Pediatric Emergency Care Applied Research Network (PECARN) http://www.pecarn.org Accessed December 23, 2009.
- 21.Olmstead S.S., Grabenstein J.D., Jain A. Use of an electronic monitoring system for self-reported smallpox vaccine reactions. Biosecur Bioterror. 2005;3:198–206. doi: 10.1089/bsp.2005.3.198. [DOI] [PubMed] [Google Scholar]
- 22.Fineberg H.V., Wilson M.E. Epidemic science in real time. Science. 2009;324:987. doi: 10.1126/science.1176297. [DOI] [PubMed] [Google Scholar]