Highlights
-
•
Contact tracing is an essential step in infectious disease control and prevention.
-
•
Using Electronic medical record (EMR) is challenging and misses a number of potential exposures.
-
•
Real time location system (RTLS) doubled the potential exposures list for pertussis disease beyond the conventional method of EMR-based contact identification
-
•
RTLS is more efficient and timely in the process of contact tracing.
-
•
Further studies with larger sample size are needed to confirm the findings.
Key Words: Infectious disease, Pertussis
Abstract
Background
Contact tracing is the systematic method of identifying individuals potentially exposed to infectious diseases. Electronic medical record (EMR) use for contact tracing is time-consuming and may miss exposed individuals. Real-time location systems (RTLSs) may improve contact identification. Therefore, the relative effectiveness of these 2 contact tracing methodologies were evaluated.
Methods
During a pertussis outbreak in the United States, a retrospective case study was conducted between June 14 and August 31, 2016, to identify the contacts of confirmed pertussis cases, using EMR and RTLS data in the emergency department of a tertiary care medical center. Descriptive statistics and a paired t test (α = 0.05) were performed to compare contacts identified by EMR versus RTLS, as was correlation between pertussis patient length of stay and the number of potential contacts.
Results
Nine cases of pertussis presented to the emergency department during the identified time period. RTLS doubled the potential exposure list (P < .01). Length of stay had significant positive correlation with contacts identified by RTLS (ρ = 0.79; P = .01) but not with EMR (ρ = 0.43; P = .25).
Conclusions
RTLS doubled the potential pertussis exposures beyond EMR-based contact identification. Thus, RTLS may be a valuable addition to the practice of contact tracing and infectious disease monitoring.
Contact tracing is a critical strategy required for timely prevention and control of infectious disease outbreaks.1, 2 However, conventional contact tracing methods are time-consuming and can miss a significant number of potential exposures.3, 4 Medical record review and staff interview methods fail to capture all potentially exposed individuals because of incomplete or missing documentation and recall bias.5, 6 Failure to identify persons in contact with infected patients increases the risk of transmission, placing many health care workers and vulnerable patients (eg, infants and comorbid patients) at risk.7 This transmission may cause significant health complications, especially for vulnerable patients, and increase morbidity and mortality.7 Failure to adequately trace infectious disease contacts disrupts routine health care services8 and results in substantial cost for health care systems.9, 10 Current contact tracing methodologies for contagious diseases are imperfect, and new technological interventions should be investigated to identify close contacts in a timely, efficient, and exhaustive manner to prevent subsequent transmission to other patients and health care workers for effective outbreak management.
Advances in technology have made tracking individuals possible and increasingly affordable using several types of real-time location system (RTLS). One such RTLS uses radiofrequency identification (RFID) tracking. RFID has been used in a variety of settings such as schools11, 12 and academic conferences13, 14 to facilitate and accelerate the process of understanding face-to-face contact, human interactions, and social networks accurately and efficiently within a very short time. In health care settings, RFID has been used to study the role of patient-health care worker networks and face-to-face contact frequency and duration in the disease transmission process15 and to identify the most and least connected health care workers with patients.16
To date, no study has compared RTLS with the standard methodology of chart review for contact tracing. In this case study, we describe a relative effectiveness comparison of contact tracing between current state (chart review) and RTLS tracking for confirmed pertussis cases in an emergency department (ED).
Materials and methods
Equipment
Our RTLS system (Quake Global, Inc, San Diego, CA) utilizes 194 in-ceiling, passive RFID readers with 734 antennas, covering 212 locations in a 54,450 sq ft ED and radiology (supporting ED services) department space. The RTLS, driven by this RFID infrastructure, was in operation and reliable for 6 months before data collection. Core ED staff wore RFID-enabled employee identification tags. In addition to physicians and nurses, staff including respiratory therapists and registration personnel had RFID-enabled badges. However, some ancillary staff serving the ED (eg, medical students and radiology technicians) did not have RFID-enabled identification tags during the time of this study.
Study protocol
During an outbreak of pertussis in the Midwest region of the United States, a retrospective case study was conducted to identify possible contacts of 9 confirmed, successive pertussis cases between June 14 and August 31, 2016. Our study was performed in the ED of a large tertiary medical center with an annual volume of approximately 74,000 patient encounters. We used both traditional electronic medical record (EMR)-based contact identification and RTLS-generated data. All pertussis cases were diagnosed 1-2 days after the ED visit and reported to institutional infection control services. None of these 9 patients were admitted to the hospital.
Per existing contact tracing protocol, a list of possible exposures for each pertussis patient was generated after review of the EMR. Nurse leadership in coordination with hospital infection control, using current Centers for Disease Control and Prevention guidelines, conducted this review. Possible disease exposure included any health care worker whose role placed them in face-to-face contact with the index patient in the exam room or triage area. The EMR identified any health care workers who documented their interactions with patients.
Subsequently, a list of possible pertussis exposures was generated using a novel RTLS event mapping program that identified patients and staff, their colocations, and movements over time and space. It took <5 minutes to generate each of these RTLS data queries. Because pertussis is spread through droplet respiratory secretions, possible exposures were limited to colocation in ED exam rooms or triage areas where droplet exposures are most likely. Hallway and waiting room colocation were excluded from the analysis because they were not considered likely to result in face-to-face exposure. All possible exposures, identified through RTLS or EMR review, were offered standard pertussis exposure prophylaxis.
Analysis
We compared the number of possible exposures identified by EMR, the number of possible exposures identified by RTLS, and the roles of the health care staff that came in contact with confirmed pertussis cases. Descriptive statistics and paired t tests were used to compare the number of contacts and the role of those identified by EMR and RTLS, with α = 0.05. In addition, a Pearson product-moment correlation between the length of stay (LOS) and the number of contacts identified by each methodology was performed.
Results
Nine patients eventually diagnosed with pertussis presented to the ED during our identified time period, with patient ages ranging from 1.6-18 years (mean, 9.6 years). The average LOS was 94 minutes (range, 62 to 294 minutes; standard deviation = 96.6).
When combining all 9 cases, EMR review (alone) identified 45 potential contacts (Table 1 and Fig 1 ). Thirteen health care workers were identified in the EMR but not identified by RTLS, including 2 physicians, 6 triage nurses, 1 discharge nurse, 1 scribe, 1 urology technician, 1 radiology technician, and 1 medical student. RTLS alone identified 77 contacts, of whom 45 were additional new contacts not identified from the EMR. Table 2 shows the roles of the health care staff identified by RTLS but not by EMR review. RTLS identified twice as many possible contact cases as those identified by EMR review (P < .01) increasing the number of potential contacts above those identified by the EMR from an average of 5 contacts per case to an average of 10 contacts per case (Fig 1 and Table 1).
Table 1.
Nine pertussis cases and potential exposure identified by electronic medical record (EMR) and real-time location system (RTLS)
| Case No. | Age, y | Emergency department length of stay, min | No. by EMR review | No. by RTLS review | No. by EMR (but not RTLS) | No. by RTLS (but not EMR) | Total unique contacts | Increase above EMR only, % |
|---|---|---|---|---|---|---|---|---|
| 1 | 1.6 | 91 | 4 | 8 | 2 | 6 | 10 | 150.0 |
| 2 | 18 | 152 | 5 | 9 | 1 | 5 | 10 | 100.0 |
| 3 | 11 | 144 | 7 | 9 | 1 | 3 | 10 | 42.9 |
| 4 | 2.1 | 68 | 5 | 8 | 2 | 5 | 10 | 100.0 |
| 5 | 17 | 121 | 5 | 5 | 1 | 1 | 6 | 20.0 |
| 6 | 17 | 62 | 3 | 3 | 0 | 0 | 3 | 0 |
| 7 | 9 | 288 | 5 | 10 | 2 | 7 | 12 | 140.0 |
| 8 | 2.8 | 287 | 5 | 14 | 2 | 11 | 16 | 220.0 |
| 9 | 8 | 294 | 6 | 11 | 2 | 7 | 13 | 116.7 |
| Total | 45 | 77 | 13 | 45 | 90 | |||
| Average | 9.6 | 94 | 5.0 | 8.6 | 1.4 | 5.0 | 10.0 | 100 |
Fig 1.
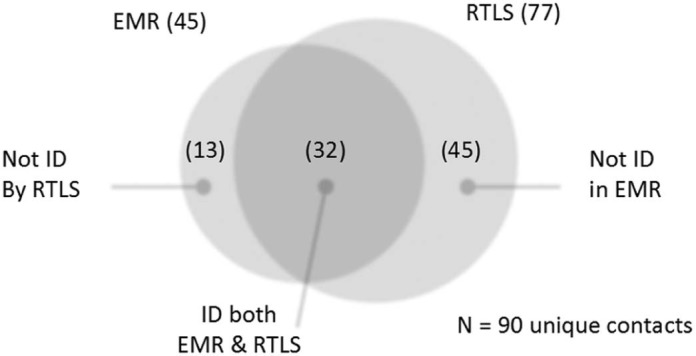
Electronic medical record (EMR) versus real-time location system (RTLS) in identifying pertussis contacts.
Table 2.
Health care staff additionally identified as potentially exposed by real-time location system
| Role | Case No. | Total, n | Total additional staff identified, % | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
| Physician | 1 | 1 | 2 | 4.4 | |||||||
| Nurse | 2 | 3 | 1 | 2 | 2 | 4 | 2 | 16 | 35.6 | ||
| Pharmacist | 1 | 1 | 2.2 | ||||||||
| Respiratory care | 1 | 1 | 1 | 3 | 6.7 | ||||||
| Care team assistant | 2 | 2 | 1 | 1 | 3 | 9 | 20.0 | ||||
| Registration | 1 | 1 | 1 | 2 | 1 | 6 | 13.3 | ||||
| Phlebotomist | 2 | 2 | 4.4 | ||||||||
| Child life specialist | 1 | 1 | 1 | 2 | 1 | 6 | 13.3 | ||||
| Total | 6 | 5 | 3 | 5 | 1 | 0 | 7 | 11 | 7 | 45 | 100 |
NOTE. Case numbers 7, 8, and 9 had the longest length of stay (4:48, 4:47, and 4:90 min, respectively) and also had the largest number of additionally identified staff by RTLS (7, 11, and 7, respectively) (Table 2). Length of stay had significant positive correlation with the total unique contacts (ρ = 0.78; P = .01). When further examined by identification method, length of stay had significant positive correlation with the total contact number identified by RTLS (ρ = 0.79; P = .01) but length of stay was not significantly correlated with the total contact number identified by EMR review (ρ = 0.43; P = .25).
Discussion
In this study, RTLS doubled the number of potential pertussis exposures identified beyond the conventional methods of EMR-based contact identification, suggesting that RTLS may be more effective than traditional EMR review alone. RTLS-generated data can be a valuable adjunct to identify additional potential disease exposures, especially health care staff who are not principal caretakers and/or those in supporting ED roles.
RTLS appears to be of greater benefit when patients have longer ED LOS. We showed statistically significant positive correlation with ED LOS and RTLS-identified contacts, but not with EMR-identified contacts. The literature has shown that the LOS of contagious patients in hospital settings increases the potential for nosocomial spread of contagious diseases,17, 18 but no study has looked into the correlation between LOS and number of identified contacts using different contact tracing methodologies. Our finding may be due to the fact that patients with longer LOS interact with more health care providers during their stay.
In addition to the increased identification of exposed health care staff, RTLS also saves time and resources in identifying potential exposures due to rapidity and can quantify exposure duration. In this study, RTLS data query took, on average, <5 minutes to generate a list of possible exposures and unlike chart review gave duration of exposure. Time to complete standard chart review was not specifically measured, but was estimated to be 30-60 minutes per patient EMR. Other studies have found that the use of chart review in contact tracing is time-consuming.3 The objective data provided by RTLS reduced the need to further verify and interview staff documented within the chart to identify additional potential exposures. In addition, RTLS may also reduce the effect of recall bias and need to contact health care staff, who must also rely on memory, in an effort to identify potential exposures.
The RTLS system failed to identify 13 health care workers who were documented in the medical record. Four were representatives of staff categories that had not been equipped with RFID-enabled badges, and 6 were triage nurses who provided care before the rooming process and their RTLS antenna was moved to increase probabilities of registering in the future. Two physicians were missed, 1 whose badge had an RFID chip that was not being read correctly by the RTLS, and the other was a resident physician who was not wearing the correct RFID-enabled badge. There was not a clear explanation why 1 discharge nurse was not picked up in the query. Further expansion of RIFD-enabled badges and analysis of system outliers is needed to ensure overall RTLS system integrity.
Although the cost of the RTLS system can be justifiable in large urban EDs with diverse patient populations, some might argue against such high cost in small community EDs that are less likely to develop major infectious disease outbreaks. However, diseases like pertussis are increasingly reemerging in cycles every 3-5 years despite the high rate of vaccination,19 and lack of vaccination is an increasing concern.20 In other studies, nosocomial pertussis outbreaks resulted in substantial cost to hospitals, even when the number of pertussis cases was low.9, 10 Also, contact tracing is only 1 method to justify the cost of RTLS, and some smaller community EDs may also attain a reasonable return on investment using metrics such as reducing asset shrinkage.21
Limitations to our study include, but are not limited to, a small sample size. We tested only 1 ED, and focused on 1 specific disease, which makes it less generalizable. Also, this study did not include the mitigating effect of personal protective equipment use by health care staff members for exposure to pertussis-diagnosed patients, and did not take the cost of using each contact tracing method into account. Further multicenter comparative studies of infectious diseases using contact tracing between the RTLS and EMR, with larger sample sizes and with focus on more than 1 disease, are needed to confirm our findings and cost-effectiveness and allow for more generalizability.
Conclusions
RTLS identified more potential contacts with pertussis-diagnosed patients than EMR-based chart review. Although RTLS is not mature enough a technology to entirely replace standard chart review, this case study illustrates how an evolving technology can accelerate the process of active screening and facilitate timely cessation in the chain of transmission of infectious diseases. RTLS can be an important tool for infection control programs, especially in tertiary care medical systems with higher acuity and complex, vulnerable patients. Such hospitals are relied upon to care for patients with rare, high-risk, contagious diseases like measles, tuberculosis, and emerging infections such as Ebola virus disease, severe acute respiratory syndrome, or Middle East respiratory syndrome. Notably, several high-risk emerging infections are transmitted by airborne spread with greater contagious risk to staff and other patients, and if discharged home, to the public at large. We believe that RTLS may show a more substantial benefit in these cases, because brief exposures at a distance are clinically significant and difficult to thoroughly evaluate by traditional means, whereas event mapping using RTLS is customizable to pick up such brief exposures.
Footnotes
Supported by funds from the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery and contributions from the Mayo Clinic ED-Clinical Engineering Learning Lab.
Conflicts of interest: None to report.
References
- 1.Browne C., Gulbudak H., Webb G. Modeling contact tracing in outbreaks with application to Ebola. J Theor Biol. 2015;384:33–49. doi: 10.1016/j.jtbi.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Begun M., Newall A.T., Marks G.B., Wood J.G. Contact tracing of tuberculosis: a systematic review of transmission modelling studies. PLoS One. 2013;8 doi: 10.1371/journal.pone.0072470. e72470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dixon M.G., Taylor M.M., Dee J., Hakim A., Cantey P., Lim T. Contact tracing activities during the Ebola virus disease epidemic in Kindia and Faranah, Guinea, 2014. Emerg Infect Dis. 2015;21:2022–2028. doi: 10.3201//eid2111.150684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.England D.O., Currie M.J., Bowden F.J. An audit of contact tracing for cases of chlamydia in the Australian Capital Territory. Sex Health. 2005;2:255–258. doi: 10.1071/sh05021. [DOI] [PubMed] [Google Scholar]
- 5.Bryant K.A., Humbaugh K., Brothers K., Wright J., Pascual F.B., Moran J. Measures to control an outbreak of pertussis in a neonatal intermediate care nursery after exposure to a healthcare worker. Infect Control Hosp Epidemiol. 2006;27:541–545. doi: 10.1086/505666. [DOI] [PubMed] [Google Scholar]
- 6.Daskalaki I., Hennessey P., Hubler R., Long S.S. Resource consumption in the infection control management of pertussis exposure among healthcare workers in pediatrics. Infect Control Hosp Epidemiol. 2007;28:412–417. doi: 10.1086/513121. [DOI] [PubMed] [Google Scholar]
- 7.O'Brien J.A., Caro J.J. Hospitalization for pertussis: profiles and case costs by age. BMC Infect Dis. 2005;5:57. doi: 10.1186/1471-2334-5-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ward A., Caro J., Bassinet L., Housset B., O'Brien J.A., Guiso N. Health and economic consequences of an outbreak of pertussis among healthcare workers in a hospital in France. Infect Control Hosp Epidemiol. 2005;26:288–292. doi: 10.1086/502541. [DOI] [PubMed] [Google Scholar]
- 9.Baggett H.C., Duchin J.S., Shelton W., Zerr D.M., Heath J., Ortega-Sanchez I.R. Two nosocomial pertussis outbreaks and their associated costs—King County, Washington, 2004. Infect Control Hosp Epidemiol. 2007;28:537–543. doi: 10.1086/513497. [DOI] [PubMed] [Google Scholar]
- 10.Zivna I., Bergin D., Casavant J., Fontecchio S., Nelson S., Kelley A. Impact of Bordetella pertussis exposures on a Massachusetts tertiary care medical system. Infect Control Hosp Epidemiol. 2007;28:708–712. doi: 10.1086/518352. [DOI] [PubMed] [Google Scholar]
- 11.Salathe M., Kazandjieva M., Lee J.W., Levis P., Feldman M.W., Jones J.H. A high-resolution human contact network for infectious disease transmission. Proc Natl Acad Sci USA. 2010;107:22020–22025. doi: 10.1073/pnas.1009094108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stehle J., Voirin N., Barrat A., Cattuto C., Isella L., Pinton J.F. High-resolution measurements of face-to-face contact patterns in a primary school. PLoS ONE. 2011;6 doi: 10.1371/journal.pone.0023176. e23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cattuto C., Van den Broeck W., Barrat A., Colizza V., Pinton J.F., Vespignani A. Dynamics of person-to-person interactions from distributed RFID sensor networks. PLoS ONE. 2010;5 doi: 10.1371/journal.pone.0011596. e11596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Isella L., Romano M., Barrat A., Cattuto C., Colizza V., Van den Broeck W. Close encounters in a pediatric ward: measuring face-to-face proximity and mixing patterns with wearable sensors. PLoS ONE. 2011;6 doi: 10.1371/journal.pone.0017144. e17144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gundlapalli A., Ma X., Benuzillo J., Pettey W., Greenberg R., Hales J. Social network analyses of patient-healthcare worker interactions: implications for disease transmission. AMIA Ann Symp Proc. 2009;2009:213–217. [PMC free article] [PubMed] [Google Scholar]
- 16.Hornbeck T., Naylor D., Segre A.M., Thomas G., Herman T., Polgreen P.M. Using sensor networks to study the effect of peripatetic healthcare workers on the spread of hospital-associated infections. J Infect Dis. 2012;206:1549–1557. doi: 10.1093/infdis/jis542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vincent J., Bihari D.J., Suter P.M., Bruining HA, White J, Nicolas-Chanoin MH. The prevalence of nosocomial infection in intensive care units in Europe: results of the European Prevalence of Infection in Intensive Care (EPIC) study. JAMA. 1995;274:639–644. [PubMed] [Google Scholar]
- 18.Cohen B., Hyman S., Rosenberg L., Larson E. Frequency of patient contact with health care personnel and visitors: implications for infection prevention. Jt Comm J Qual Patient Saf. 2012;38:560–565. doi: 10.1016/s1553-7250(12)38073-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bouchez V., Guiso N. Bordetella pertussis, B. parapertussis, vaccines and cycles of whooping cough. Pathog Dis. 2015;73 doi: 10.1093/femspd/ftv055. pii: ftv055. [DOI] [PubMed] [Google Scholar]
- 20.Phadke V.K., Bednarczyk R.A., Salmon D.A., Omer S.B. Association between vaccine refusal and vaccine-preventable diseases in the United States: a review of measles and pertussis. JAMA. 2016;315:1149–1158. doi: 10.1001/jama.2016.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rousek J.B., Pasupathy K., Gannon D., Hallbeck S. Asset management in healthcare: evaluation of RFID. IIE Trans Healthc Syst Eng. 2014;4:144–155. [Google Scholar]


