Abstract
In order to assess the immunotherapeutic potential on canine visceral leishmaniasis of the Leishmune® vaccine, formulated with an increased adjuvant concentration (1 mg of saponin rather than 0.5 mg), 24 mongrel dogs were infected with Leishmania (L.) chagasi. The enriched-Leishmune® vaccine was injected on month 6, 7 and 8 after infection, when animals were seropositive and symptomatic. The control group were injected with a saline solution. Leishmune®-treated dogs showed significantly higher levels of anti-FML IgG antibodies (ANOVA; p < 0.0001), a higher and stable IgG2 and a decreasing IgG1 response, pointing to a TH1 T cell mediated response. The vaccine had the following effects: it led to more positive delayed type hypersensitivity reactions against Leishmania lysate in vaccinated dogs (75%) than in controls (50%), to a decreased average of CD4+ Leishmania-specific lymphocytes in saline controls (32.13%) that fell outside the 95% confidence interval of the vaccinees (41.62%, CI95% 43.93–49.80) and an increased average of the clinical scores from the saline controls (17.83) that falls outside the 95% confidence interval for the Leishmune® immunotherapy-treated dogs (15.75, CI95% 13.97–17.53). All dogs that received the vaccine were clustered, and showed lower clinical scores and normal CD4+ counts, whereas 42% of the untreated dogs showed very diminished CD4+ and higher clinical score. The increase in clinical signs of the saline treated group was correlated with an increase in anti-FML antibodies (p < 0.0001), the parasitological evidence (p = 0.038) and a decrease in Leishmania-specific CD4+ lymphocyte proportions (p = 0.035). These results confirm the immunotherapeutic potential of the enriched-Leishmune® vaccine. The vaccine reduced the clinical symptoms and evidence of parasite, modulating the outcome of the infection and the dog's potential infectiosity to phlebotomines. The enriched-Leishmune® vaccine was subjected to a safety analysis and found to be well tolerated and safe.
Keywords: FML-vaccine, Immunotherapy, Leishmune® vaccine, Canine visceral leishmaniasis, Leishmania chagasi, Kala-azar, Saponin, Quillaja saponaria Molina, QS21
1. Introduction
Leishmania (L.) chagasi and Leishmania (L.) infantum are the ethological agents of human kala-azar in America, the Mediterranean basin, Middle East and Asian Countries. Kala-azar is a severe and frequently lethal disease if untreated after the onset of symptoms. In these regions, it results from canid zoonoses. These parasites are found exposed on the skin of foxes, wild canids and dogs, and transmitted to humans through a sand fly's bite. Zoonotic visceral leishmaniasis (ZVL) is then a re-emergent canid zoonoses, the epidemiological control of which involves: the elimination of seropositive infected dogs, insecticide treatment within domestic and peri-domestic habitations, and the systematic treatment of human cases [1]. Brazil is one of the four countries responsible for 90% of the total human cases (500,000 all over the world) [1]. As a tool for epidemiological control, the killing of seropositive dogs is widely practised in Brazil and China but unacceptable in Europe. Canine surveillance programs are very laborious, expensive and require continual vigilance [1] and sensitive serological diagnostic methods [2], [3], [4] to be effective. Furthermore, since many seropositive infected dogs are asymptomatic, owner compliance is complicated [1] even though the infectivity of asymptomatic dogs to sand flies has already been proven [5].
The sacrifice of seropositive animals for epidemiological control is still performed, because chemotherapy of infected dogs using pentavalent antimonial has been mostly unsuccessful and has been accused of exacerbating the disease [5], [6], [7], [8]. Reports about an increase in survival rate [9] and a possible cure potential [10], however, stimulated research into dog therapy against ZVL. Treatment of infected dogs is now usual practise in Europe and is now being adopted in Brazil. Dogs therapies are still not recommended by WHO since both the human and canine treatment are performed with the same drugs and this fact raises the risk of rise in number of drug-resistant parasites [11]. Treatment promotes a clinical cure and better quality of life but amastigotes remain present [12], [13] meaning that dogs might remain infectious for sand flies, even several months after treatment [5], [14]. The presence of latent infections in dogs is typical and important in maintaining the long-term presence of the parasite in endemic regions [15].
The development of a protective vaccine against canine visceral leishmaniasis has been recommended by WHO as a possible tool for an effective eradication of the disease [1], [16], reducing the offer of parasites to sand fly vectors and consequently the number of human kala-azar cases. While data about an effective prophylactic vaccine against human kala-azar is still preliminary [17], partial protection against canine visceral leishmaniasis has been reported in kennel studies [18], [19], [20].
Leishmune® vaccine is a prophylactic formulation against canine visceral leishmaniasis recently licensed in Brazil for vaccination of dogs. It is the first registered vaccine against leishmaniasis. It is composed of the FML (Fucose-Mannose Ligand) antigen of Leishmania donovani and Riedel de Haen saponin which contains the QS21 and deacylated saponins of Quillaja saponaria as the main adjuvant components [21], [22], [23], [24]. This formulation obtained under laboratory conditions and proved to be safe protective and highly immunogenic for hamsters [25], mice [26] and dogs [27], [28]. In a Brazilian area endemic for both human and dog visceral leishmaniasis, recent Phase III trials of efficacy using the FML-saponin in dogs induced 92% [27] and 95% [28] protection for dogs exposed to the disease (76% and 80% of vaccine efficacy, respectively). Protection induced by the FML-QuilA vaccine lasted up to 3.5 years after vaccination. At this time, vaccinees showed higher seropositivities and intradermal reactions, with no Leishmanial DNA nor parasites in bone marrow punctures. The FML-QuilA vaccine, then, induced a significant, long-lasting and strong protective effect against canine visceral leishmaniasis in the field [28]. On the other hand, dogs which received saline were PCR positive for Leishmania DNA, had amastigotes in bone marrow and FML-serology with no intradermal reaction [28].
The industrially produced Leishmune® vaccine has recently demonstrated acceptable safety [29] and immunogenicity characteristics [21], [22]. In a highly exposed endemic area, healthy dogs vaccinated with Leishmune® remained free of parasites and noninfectious to sand flies, by parasitological criteria [21], 11 months after vaccination. Sand flies fed in vivo with serum of dogs vaccinated with Leishmune® 12 months before, showed a 79.3% reduced infection in comparison to sand flies fed on pre-immune dog's sera [30] indicating that Leishmune® is a transmission blocking vaccine (TBV) with a potential important impact on the interruption of the epidemiological cycle of visceral leishmaniasis.
Considering the relative failure of chemotherapy against canine visceral leishmaniasis and its negative impact on the epidemiological control of the disease, the possible use of a protective vaccine in the immunotherapy of the already infected dogs is highly encouraging and would have broader community acceptance than a control effort based instead on killing infected dogs. The impressive protection achieved by the FML-vaccines in the field Phase III assays [27], [28] and by Leishmune® to date [22] raise the perspective of their use in immunotherapeutic canine trials. This hypothesis is further supported by the recent results showing that the FML-saponin vaccine, among few others [31], [32], has been shown to be immunotherapeutic in mice [33] and in seropositive asymptomatic dogs from Brazilian endemic areas [34].
Different from the vaccine previously used with healthy dogs [27], [28], the infected dogs received the FML-saponin vaccine with an increased adjuvant concentration (1 mg saponin) in the same schedule (three doses with a month interval) and annual boosters [34]. The treated dogs showed stable anti-FML IgG1 levels, increasing IgG2 levels and 79–95% of positive DTH response, during the whole experiment [34]. Twenty-two months after complete vaccination, no deaths due to visceral leishmaniasis were recorded and 90% of the dogs were still asymptomatic, healthy and parasite free [34]. The dogs remain healthy up until five years after initial vaccination. On the other hand, 37% (17/46 dogs) kala-azar deaths were recorded in a control group that received no treatment during the 22-month period. All these dogs were FML-seropositive and asymptomatic at the beginning of the study. Our results indicate that the FML-vaccine was effective in the immunotherapy against visceral leishmaniasis of asymptomatic infected dogs. Normal proportions of CD4 and CD21 lymphocytes were detected in PBMC by FACS analysis, in dogs submitted to immunotherapy, suggesting their non infectious condition. As expected, treated animals showed significantly increased percentages of CD8 lymphocytes typical for a Quillaja saponin (QuilA) vaccine treatment [34].
In this investigation, we report on the potential use of an industrialized formulation of the FML-saponin vaccine, Leishmune® with an increased concentration of saponin (1 mg); its immunotherapeutic effect was investigated in infected, seropositive and symptomatic dogs with experimental canine visceral leishmaniasis.
2. Material and methods
2.1. Immunotherapy against experimental canine visceral leishmaniasis with the saponin enriched-Leishmune® vaccine
Twenty-four mongrel dogs (5-month old) from six different litters were vaccinated against rabies (Rai-vac I) and canine distemper, Type 2 Adenovirus, Coronavirus, Parainfluenza, Parvovirus and Leptospira (Duramune DA2PP+CvK/Lci, Fort Dodge Animal Health, IA, USA) and treated with anti-helminthic drugs (Drontal Plus, Bayer). All dogs were healthy and seronegative for Leishmania antibodies in the FML-ELISA assay [35] and were further experimentally infected, by the i.v. route, with 2 × 108 amastigotes obtained from Leishmania (L.) chagasi MHOM/BR/1972/BH46 from infected hamster's spleens [36]. All animals became seropositive to the FML antigen, between months 5–6. Randomization of each one of the six litters was performed by draft in order to divide them into two balanced groups. One half of each litter received the saline control and the second half the vaccine. The saline control was then composed of: dogs 1,2,3 from family A; 7,8,9,10 from family B; 15,17 from family C; 20, 21 from family D; and dog 25 from family E. The vaccinated group included: dogs 4,5,6 from family A; 11,12,13 from family B; 14,16 from family C; 19,22,23 from family D; and dog 24 from family E. The control group was treated with sterile 0.9% NaCl saline solution, while the immunotherapy group received the Leishmune® enriched vaccine containing 1.5 mg of the FML industrialized antigen (Fort Dodge Animal Health) and 1 mg of Riedel de Haen saponin. The vaccine was given in three doses, injected through the sc route on the back, with a 20–30 days interval (essentially months 6, 7, 8). This formulation differed in adjuvant concentration from the Leishmune® vaccine formulation which contains only 0.5 mg of the saponin and is industrialized and registered in Brazil as a prophylactic vaccine against canine visceral leishmaniasis (Patent: INPI number: PI1100173-9 (18.3.97). Federal University of Rio de Janeiro, Brazil). All dogs were monitored for the following parameters: anti-FML IgG antibody levels, delayed type of hypersensitivity (DTH) against LD1S f/t promastigote lysate antigen, PBMC lymphocyte phenotyping and clinical signs. Animals were clinically evaluated on a monthly basis for: alopecia; onycogryphosis; cachexia; anorexia; isolation; apathy; skin lesions, popliteal and cervical lymph node enlargement, and loss of weight. A score system of clinical signs of infection was based on a series of factors including: the diameters of small (up to 1 cm), medium (1–1.5 cm), and large (≥2 cm) lymph nodes. Weight loss was also considered mild (MW = 0–2 kg) or severe (SW = 2–5 kg). While to detection of alopecia; onycogryphosis; cachexia; anorexia; isolation; apathy or skin lesions was attributed value = 1, the scores for normal undetectable, small, medium, and enlarged lymph nodes were 0,1,2,3, respectively. Also, a score of 2 was attributed to mild loss of weight and 3 to a severe loss of weight.
The evaluation of the presence of parasites was performed by in vitro culture of blood and bone marrow dog's samples in a biphasic culture media (NNN blood supplemented agar solid phase and 10% Fetal Calf Serum supplemented Brain Heart infusion, with 10 mg/ml Hemin and 20 mg/ml Folic acid as the liquid phase) microscopically monitored during three culture passages (21 days), and by the in vivo culture of dog's blood and bone marrow samples in CB hamsters, inoculated through the intracardiac route. In this case, the presence of parasites was assayed by microscopy analysis of liver and spleen Giemsa stained smears, on day 90, or by survival analysis. Furthermore, PCR analysis for Leishmania DNA of bone marrow samples (month 9) was performed, and Giemsa stained dog's popliteal lymph node smears, obtained after fine needle biopsies [37] (month 11), were also microscopically evaluated. Fifteen months after infection, all animals were sacrificed by anaesthesia with 3–10 ml of T-61 euthanasia (Intervet, SP, Brazil) via i.v. and the presence of Leishmania amastigotes was assessed in Giemsa stained touch biopsies of spleen, liver, and lymph nodes smears. All the animals included in this investigation were treated following the guidelines for animal experimentation of the USA National Institute of Health, and experiments were done in accordance with the institutional guidelines in order to minimize animal suffering.
2.2. Safety and reactogenicity of the saponin enriched-Leishmune® vaccine
All three vaccines doses were injected subcutaneously on the neck. A veterinarian recorded the presence or absence of the potential vaccine adverse events: local pain, local swelling, anorexia, apathy, vomit, and diarrhoea. Reactions were observed 1,2,4 and 9 days after injection. We observed pain reactions after touching in the injection site. We recorded as pain reaction when dogs looked at the injection site, or when a skin contraction was observed, or when the dog whined or tried to bite the hand of the observer. Local swelling at the injection site was detected by palpation and ranged between 2–5 cm diameter in most animals. If the dog ate less than usual and/or rejected the food, anorexia was recorded. If the dogs did not stand up or approach to the observer, apathy was recorded.
2.3. FML-ELISA assay
Dog sera were evaluated monthly for the presence of total anti-Leishmania donovani antibodies by the FML-ELISA assay [35] using the FML antigen (2 μg/well) solubilized in carbonate buffer (pH 9.6) coated on flat-bottom 96-well plates (Corning 25805-96, cat. number 430480, highly absorbent). Total antibodies were detected by using peroxidase-labeled protein-A (Kirkegaard & Perry Laboratories, Gaithersburg, Maryland) at a 1:16,000 dilution, in blocking buffer. The cut-off of the FML-ELISA assay, as determined by the Youden test calculation [38] is Abs 492 ηm: 0.450 (mean average of absorbance values of normal healthy serum plus 2 standard deviations). Results were expressed as mean values of the triplicates. The absorbance values at 492 ηm were compared using a 1:100 dilution of the individual serum samples. Furthermore, goat anti-dog IgG1 heavy chain specific (1:1000) or IgG2 (1:8000) (Bethyl Laboratories, Inc., Montgomery, TX, USA) conjugated with horseradish-peroxidase were used for the IgG subtype determination of each pool of total sera over time.
2.4. Delayed type hypersensitivity (intradermal reaction to promastigote lysate)
This was determined by injecting dogs intradermally, in month 9 and 11 after infection. Dogs were injected in the inner side of the right hind leg, with 0.1 ml of L. donovani freeze-thawed antigen containing 200 μg protein in NaCl 0.9% sterile saline solution (108 stationary phase promastigotes/ml). The left hind leg received only 0.1 ml saline. Measure of the increase of intradermal reaction was performed 48 h after antigen injection. Indurate areas were marked, and each time the values of the saline control were subtracted from the reaction due to the Leishmania antigen. Reactions showing diameters ≥5 mm were considered positive [27], [28], [34].
2.5. Flow cytometry analysis of PBMC
In the twelve month after infection, PBMC counts of each dog were obtained from 3 ml of the cephalic vein blood collected in heparin-tubes. For ex-vivo analysis, 30 μl of blood were incubated for 30 min at room temperature, with 30 μl of each one of the following monoclonal antibodies diluted in Facs dil solution (10% FCS supplemented PBS buffer): anti-Thy-1 (Rat-IgG2b-clone YKIX337.217) (1:800), anti-CD5 (Rat-IgG2a-clone YKIX322.3) (1:800), anti-CD4 (Rat-IgG2a-clone YKIX302.9) (1:12500), anti-CD8 (Rat-IgG1-clone YCATE55.9) (1:100). Thirty microliters of anti-rat serum (1:600) (Serotec, Oxford, UK). PBS was used as negative control. After this period, 2 ml of PBS-W (PBS buffer with 0.5% Bovine Serum Albumin and 0.1% Sodium Azide) were added to each tube and the mixture was homogenised and centrifuged at 1300 rpm, at room temperature, for 7 min. The supernatants were aspirated and pellets homogenised and added of 60 μl of anti-rat FITC conjugate (1:200) (Serotec, UK) except for the PBS cell control. At this time, 4 μl of the FITC-labelled mouse anti-human-CD21 (Mouse-IgG1-clone IOB1a) monoclonal antibody (Immunotech Co. Marseille, France) was used in a direct immunofluorescence procedure. All suspensions were homogenised, incubated for 30 min at room temperature in the dark and treated with 2 ml of the 1/10 diluted lysis solution during Vortex homogenization (Becton & Dickinson, USA). The mixtures were further incubated for 10 min at room temperature in the dark and further centrifuged at 1300 rpm for 7 min. Supernatants were discarded and the pellet-containing tubes were inverted on to absorbent paper. All these procedures were repeated twice after the addition of 2 ml PBS. The pellets were homogenised carefully and finally fixed with 300 μl of 2.8% formaldehyde-PBS.
Alternatively, the PBMC Leishmania-specific lymphocytes were analysed after in vitro proliferation with Leishmania antigens. One milliliter of the cephalic vein blood was diluted in 1 ml RPMI medium (Sigma, Co.), cushioned on 2 ml Histopaque (cat. Number 1077, Sigma Co.) and centrifuged at 2400 rpm for 20 min, at room temperature. The fraction containing PBMC was aspirated and washed three times with RPMI, at 1800 rpm for 10 min at 4 °C. The cells were counted in haemocytometer. Twenty-four well plates (Nunc Nunclon, Denmark) were platted with 2 × 106 cells in 10% FCS supplemented RPMI, and incubated for five days at 37 °C and 5% CO2 in the presence of the lysate of 106 stationary phase promastigotes of Leishmania (L.) chagasi. After this period, cells were harvested and washed twice with PBS at 1500 rpm for 10 min. The pellets were labelled with 30 μl of the primary monoclonal antibodies, as described above, washed twice, incubated with the conjugates, washed twice and finally fixed in 2.8% formaldehyde-PBS. Ten thousand cells were analyzed by flow cytometry on a Becton Dickinson FACScalibur apparatus, and further analyzed using WinMDI (Windows Multiple Document Interface Flow Cytometry Application) Version 2.8 software.
2.6. PCR for Leishmanial DNA
One milliliter of peripheral blood from the cephalic vein or of bone marrow sternum aspirates were collected into EDTA tubes and stored at −20 °C. For DNA extraction, 0.7 ml samples were thawed, washed with 0.5 ml of TE buffer (10 mM Tris, 1 mM EDTA), centrifuged at 14,000 × g and treated with lysis buffer (10% sodium dodecyl sulphate- SDS in 0.2 M sodium acetate and 20 μg/ml proteinase K) at 56 °C for one hour. The lysates were further treated with 400 μl of phenol/chloroform/iso-amilic alcohol, and the DNA precipitated with ethanol, dried, and ressuspended in 50 μl of TE buffer. PCR analysis was performed using primers 13A (5′ GTG GGG GAG GGG CGT TCT 3′) and 13B (5′ ATT TTA CAC CAA CCC CCA GTT 3′) that amplify the conserved region of the kinetoplast minicircle DNA of the Leishmania genus (120bp), as previously described by Rodgers et al. [39]. This PCR assay is able to detect a minimum of 25 Leishmania parasites. The amplified products were analyzed on a 2% agarose gel containing 0.5 μg/ml ethidium bromide (Sigma Co.), and a 100bp DNA ladder (Invitrogen™) was used as a marker. The gels were visualized under UV light with a transilluminator.
2.7. Statistical analysis
Means were compared by the ANOVA analysis simple factorial test and by one-way ANOVA, Tukey's honestly significant difference method using SPSS for windows. To test the significance of the differences between groups we also used the 95% confidence interval of the averages. Proportions were compared by the χ 2 test. Correlation coefficient analysis was determined on a Pearson bivariate, two-tailed test of significance (SPSS).
3. Results
In order to assess the immunotherapeutic potential of the Leishmune® vaccine on canine visceral leishmaniasis, formulated with an increased adjuvant concentration (from 0.5 to 1 mg of saponin), 24 mongrel dogs were infected with 2 × 108 amastigotes of L. (L.) chagasi BH46 obtained from hamsters spleens. The animals were monitored monthly for their anti-FML IgG antibodies (Fig. 1A and B). Until month 5 after infection, no antibodies were detected; between month 5–6 (150–180 days of infection), all animals started to give positive results in the FML-ELISA assay (cut-off Abs 492ηm = 0,450) and in month 6, the first clinical signs were noted. At this point, the enriched-Leishmune® vaccine was injected in the immunotherapy group (months 6, 7 and 8), while the control group received only saline. Starting from month 7, soon after the first vaccine dose, and as expected for a saponin-containing vaccine, a rapid increase of IgG anti-FML antibodies was observed in vaccinees, while control dogs showed lower and stable titters (Fig. 1A). The ANOVA analysis revealed significant differences both between times (p < 0.0001) and between treatments (p < 0.0001). Differences started in month 5 (Student-Newman-Keuls method-SPSS for windows). In Fig. 1B, we observed the evolution of the individual anti-FML IgG absorbencies in each saline-treated control dog. Four control dogs (number 1,2,3 and 10) turned to seronegative at month 7, indicating the control and spontaneous resolution of infection. We further determined the isotype of the antibodies produced against the FML antigen in each group of dogs. Fig. 1C shows the IgG2 (TH1 T-cell response) and IgG1 (TH2 T-cell response) absorbencies with regard to anti-FML antibodies. The animals vaccinated with the enriched-Leishmune® vaccine, that induced high levels of specific IgG antibodies (Fig. 1A) also showed increased IgG2 and IgG1 responses over the saline control. Both groups showed the same antibody levels by the time of infection (month 0). While immunotherapy treatment induced a higher and stable IgG2 response in vaccines (TH1 type of immune response), the IgG2 response decreased in the untreated controls with the progression of infection. On the other hand, the IgG1 antibodies diminished after vaccination and showed a mild trend to increase in the untreated infected animals (TH2 immune response) (Fig. 1C).
Fig. 1.
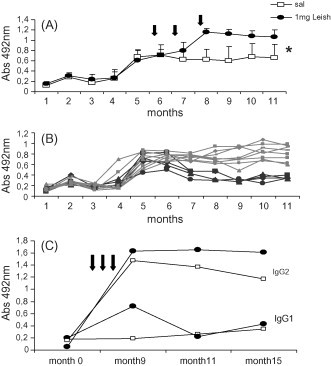
Evolution of the anti-FML antibody absorbency values with time in Leishmania (L.) chagasi experimentally infected dogs treated with saline or with Leishmune® vaccine. (A) All infected animals became seropositive between month 5 and 6 (cut-off value = Abs 492 ηm = 0.450), and after that, were treated at months 6,7 and 8 either with 3 sc doses of the adjuvant enriched-Leishmune® vaccine (arrows; n = 12) or with saline (n = 12). Results are expressed as the average ±S.D. of triplicates of each dog serum sample. * indicates a significant difference between treatments and between times (ANOVA, p < 0.0001). (B) The monitoring of the individual evolution of anti-FML antibodies of the saline treated dogs showed that four animals (number 1,2,3 and 10; black labels) became seronegative at month 7, indicating their control and spontaneous resolution of infection. (C) Goat anti-dog IgG2 (curves above) or IgG1 (curves below) specific antibodies conjugated with horseradish-peroxidase were used for the anti-FML IgG subtype determination of each pool of sera along the time.
The cellular immune response was first assayed by the analysis of the DTH response against the L. (L.) donovani lysate. The individual DTH reactions were monitored at month 9 and 11 and are summarized in Fig. 2 . The immunotherapy treatment leads to a protective effect showing more positive reactions in vaccinated dogs than the untreated controls. In month 9, just after complete vaccination, 75% of the vaccinees (9/12) and only 50% of the controls (6/12) showed positive DTH responses (above 5 mm diameters) (Fig. 2A). Also, at month 11, reactions were positive in 84% of those which received the vaccine (10/12) and 75% of controls (9/12) (Fig. 2B). Neither the differences in percentages of positive reactions (χ 2 square test) nor in the size of skin swelling were significant (ANOVA; p = 0.778 for differences between treatments and p = 0.09 differences in times) and this is probably because of the heterogeneity of the reactions (5–15 mm). The control dogs 1,2 and 3 that spontaneously lost the antibody response (Fig. 1B) showed, as expected, high IDR values (12 mm), confirming their resistant condition to infection and natural protection.
Fig. 2.

Induration size after injection of Leishmanial promastigote lysate in Leishmania (L.)chagasi infected dogs treated with saline, or after immunotherapy with Leishmune® vaccine. Data represent the individual delayed type of hypersensitivity responses in millimeter in month 9 (A) and in month 11 after infection (B). DTH reaction was determined by injecting dogs intradermally in the inner aspect of the right hind leg, with 0.1 ml of L. (L.) donovani freeze-thawed antigen (108 stationary phase promastigotes/ml). The left hind leg received only 0.1 ml saline. Data represent the increase of intradermal reaction performed 48 h after antigen injection. The values of the saline control were subtracted from the reaction due to the Leishmania antigen. Reactions ≥5 mm were considered positive. The horizontal line represents the cut-off.
The cellular immune response was also evaluated by means of the relative proportions of PBMC lymphocyte subsets at month 12, after infection. The T cell immunosuppression and reduction of CD4+ and CD21+ lymphocyte populations are expected to occur in severe kala-azar and are positively related to the infective status of dogs for the insect vector [40]. The relative average of individual proportions of T cell lymphocytes, assessed by the counts of THY-1+ and CD5+ cells, both in the ex-vivo and the in vitro analysis, ranged within the normal levels (62–79% and 77–83%) (results not shown), for treated and untreated dogs, indicating the global sustained cellular immune response and no severe impact of the infection. Despite the long period of Leishmania (L.) chagasi infection and confirming the low virulence of the strain, the detailed ex-vivo analysis of the CD4+, CD8+ and CD21+ populations (Table 1 ), showed no alterations neither in saline controls nor in vaccinated dogs. The in vitro analysis after incubation with the Leishmania antigen was however, more sensitive and showed in the saline controls, an expected and significantly decreased proportion of Leishmania-specific CD4+. Indeed, the average of CD4+ of saline controls (32.13%) falls outside the 95% confidence interval for the Leishmune® immunotherapy-treated dogs 46.87 (CI95% 43.93–49.80). Eight among 12 saline controls showed lower values (39.95, 7.71, 16.32, 42.91, 27.65, 6.5, 39.29 and 8.04%), revealing the kala-azar expected suppression of the Leishmania-specific CD4+ lymphocyte subset and confirming the immunoprotective potential of the enriched-Leishmune® vaccine (Table 1).
Table 1.
T cell phenotypes in Leishmania-specific peripheral blood mononuclear cells of dogs infected with L. (L.) chagasi submitted to immunotherapy with the enriched-Leishmune® vaccine
| Treatment | Dog number | Saline |
Dog number | 1 mg-Leishmune® |
||||
|---|---|---|---|---|---|---|---|---|
| CD4 (%) | CD8 (%) | CD21 (%) | CD4 (%) | CD8 (%) | CD21 (%) | |||
| ex-vivo PBMC phenotyping saline controls | 1 | 44.58 | 30.30 | 11.87 | 4 | 42.46 | 28.17 | 9.71 |
| 2 | 36.13 | 24.85 | 15.90 | 5 | 36.24 | 23.91 | 12.22 | |
| 3 | 41.57 | 32.96 | 11.66 | 6 | 37.67 | 31.45 | 9.43 | |
| 7 | 38.19 | 24.37 | 18.09 | 11 | 45.98 | 30.94 | 4.57 | |
| 8 | 38.93 | 32.69 | 16.38 | 12 | 44.19 | 27.10 | 9.09 | |
| 9 | 41.85 | 17.24 | 15.68 | 13 | 46.29 | 20.84 | 3.59 | |
| 10 | 54.35 | 23.88 | 7.96 | 14 | 42.45 | 17.38 | 15.48 | |
| 15 | 44.6 | 28.54 | 10.06 | 16 | 40.58 | 22.12 | 9.21 | |
| 17 | 37.08 | 27.97 | 11.58 | 19 | 46.91 | 31.90 | 5.89 | |
| 20 | 45.39 | 26.06 | 19.23 | 22 | 40.36 | 17.77 | 29.69 | |
| 21 | 46.31 | 23.36 | 16.23 | 23 | 40.47 | 25.50 | 24.07 | |
| 25 | 45.67 | 30.78 | 11.66 | 24 | 35.89 | 18.19 | 28.96 | |
| Mean | 42.88 | 26.97 | 13.86 | CI(95%) | 41.62 (39.38–43.86) | 24.60 (21.40–27.79) | 13.49 (8.07–18.00) | |
| in vitro Leishmania-specific lymphocytes phenotyping | 1 | 45.74 | 18.41 | 8.38 | 4 | 42.07 | 29.67 | 19.70 |
| 2 | 39.95 | 16.53 | 6.72 | 5 | 37.45 | 22.78 | 7.65 | |
| 3 | 50.42 | 34.75 | 8.49 | 6 | 43.17 | 35.62 | 14.50 | |
| 7 | 7.71 | 33.82 | 38.32 | 11 | 52.09 | 38.22 | 19.04 | |
| 8 | 16.32 | 36.09 | 15.49 | 12 | 43.87 | 33.01 | 14.32 | |
| 9 | 42.91 | 33.04 | 11.98 | 13 | 46.05 | 23.64 | 16.54 | |
| 10 | 27.65 | 41.18 | 29.55 | 14 | 46.66 | 25.41 | 26.41 | |
| 15 | 6.5 | 38.85 | 13.16 | 16 | 48.86 | 37.3 | 18.86 | |
| 17 | 50.45 | 38.35 | 23.11 | 19 | 53.61 | 37.29 | 17.76 | |
| 20 | 39.29 | 21.62 | 8.48 | 22 | 45.05 | 37.50 | 8.76 | |
| 21 | 50.61 | 23.16 | 23.58 | 23 | 49.77 | 21.59 | 10.01 | |
| 25 | 8.04 | 36.28 | 19.55 | 24 | 53.84 | 20.07 | 27.69 | |
| Mean | 32.13 | 31.01 | 17.23 | CI(95%) | 46.87 (43.93–49.80) | 30.17 (25.98–34.36) | 16.77 (13.05–20.49) | |
Data correspond to the proportions of blood peripheral mononuclear cell of saline controls or Leishmune®-treated dogs, after ex-vivo and in vitro incubation with Leishmania (L.) chagasi promastigote lysate, 12 months after infection.
The increase in clinical signs is correlated with the increase in anti-FML antibodies of the saline treated group (p < 0.0001, Pearson Two Tailed Correlation coefficient), indicating that the experimental infection reproduced the development of the natural disease. Dogs were asymptomatic at the beginning of the assay and until six months after infection, when the vaccination treatment begun (Table 2 ). While an increase in the number of symptoms was noted in both the vaccinees and untreated controls throughout the experiment, the differences in number of clinical signs were highly significant, both between treatments (ANOVA, p < 0.0001) and between times (ANOVA, p < 0.0001). The number of clinical signs was higher in saline controls. The difference in number of signs, between treatments started at month 8 (Table 2), when vaccination was completed (p < 0.05, Student-Newman-Keuls test and Tukey's honestly significant difference, SPSS for windows). Also, little difference was seen between total scores of treated and untreated animals soon after vaccination (month 6,7 and 8) while stronger differences were noticed in month 11 and 15 (scores of 42 and 60 for untreated and 30 and 45 for vaccinated dogs, respectively).
Table 2.
Correlation between the decline in CD4+ proportions and the increase in the symptoms score
| CD4+ (%) | Months |
Score | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 0–5 | 6 | 7 | 8 | 9 | 11 | 15 | |||
| Saline | |||||||||
| 1 | 45.74 | – | MW | MW | MW | – | MW | O,MW,SL | |
| 2 | 2 | 2 | 0 | 2 | 1,2,1 | 12 | |||
| 2 | 39.95 | – | MW | MW | MW | – | O,MW | O,SL | |
| 2 | 2 | 2 | 0 | 1,2 | 1,1 | 11 | |||
| 3 | 50.42 | – | O, MW | O, MW | O, MW | – | SW,O | O,SW,SL | |
| 1,2 | 1,2 | 1,2 | 0 | 3,1 | 1,3,1 | 18 | |||
| 7 | 7.71 | – | O,MW | O,MW | O,MW | O,MW | SW,O | SW,O | |
| 1,2 | 1,2 | 1,2 | 1,2 | 3,1 | 3,1 | 20 | |||
| 8 | 16.32 | – | O,MW | O,MW | O,MW | MW | SW,O | A, S,O, SW,LL | |
| 1,2 | 1,2 | 1,2 | 2 | 3,1 | 1,1,1,3,3 | 24 | |||
| 9 | 42.91 | – | O,MW | O,MW | O,MW | – | MW,O | MW,O,SL | |
| 1,2 | 1,2 | 1,2 | 0 | 2,1 | 2,1,1, | 16 | |||
| 10 | 27.65 | – | O,MW | O,MW | O,MW | O | SW,O | O,SW,ML | |
| 1,2 | 1,2 | 1,2 | 1 | 3,1 | 1,3,2 | 20 | |||
| 15 | 6.5 | – | O,MW | O,MW | O,MW | O | MW,O, OE | O,ML | |
| 1,2 | 1,2 | 1,2 | 1 | 2,1,1 | 1,2 | 17 | |||
| 17 | 50.45 | – | O,A,S | O,A,SL | O,A,SL | O | MW,O | MW,O,SL | |
| 1,1,1 | 1,1,1 | 1,1,1 | 1 | 2,1 | 2,1,1 | 17 | |||
| 20 | 39.29 | – | O,MW | O,MW | O,MW | O | MW,O | O,MW,LL | |
| 1,2 | 1,2 | 1,2 | 1 | 2,1 | 1,2,3 | 19 | |||
| 21 | 50.61 | – | O,MW | O,MW | O,MW | MW | SW,O | O,SW,ML | |
| 1,2 | 1,2 | 1,2 | 1 | 3,1 | 1,3,2 | 20 | |||
| 25 | 8.04 | – | O,MW | O,MW | O,MW | – | SW,O | SW,O,LL | |
| 1,2 | 1,2 | 1,2 | 0 | 3,1 | 3,1,3 | 20 | |||
| Total scores | 34 | 34 | 34 | 10 | 42 | 60 | 214 | ||
| CI 95% | 17.83 (19.96–15.69) | ||||||||
| Vaccinees | |||||||||
| 4 | 42.07 | – | O,MW | O,MW | O,MW | MW | O | O,SL | |
| 1,2 | 1,2 | 1,2 | 2 | 1 | 1,1 | 14 | |||
| 5 | 37.45 | – | O,MW | O,MW | O,MW | – | O | O,MW,SL | |
| 1,2 | 1,2 | 1,2 | 0 | 1 | 1,2,1 | 14 | |||
| 6 | 43.17 | – | O,MW | O,MW | O,MW | – | O, MW | SW, SL | |
| 1,2 | 1,2 | 1,2 | 0 | 1,2 | 3,1 | 16 | |||
| 11 | 52.09 | – | O,MW | O,MW | O,MW | O,MW | SW,O | SW,O,ML | |
| 1,2 | 1,2 | 1,2 | 1,2 | 3,1 | 3,1,2 | 22 | |||
| 12 | 43.87 | – | O,MW | O,MW | O,MW | O,MW | SW,O | O,MW, SL | |
| 1,2, | 1,2 | 1,2 | 1,2 | 3,1 | 1,2,1 | 20 | |||
| 13 | 46.05 | – | MW | MW | MW | O,MW | O, MW | O,LL | |
| 2 | 2 | 2 | 1,2 | 1,2 | 1,3 | 16 | |||
| 14 | 46.66 | – | MW | MW | MW | – | O,MW | O,SL | |
| 2 | 2 | 2 | 0 | 1,2 | 1,1 | 11 | |||
| 16 | 48.86 | – | O,MW | O,MW | O,MW | O,A | O | O,MW,SL | |
| 1,2 | 1,2 | 1,2 | 1,1 | 1 | 1,2,1 | 16 | |||
| 19 | 53.61 | – | MW | MW | MW | O | O,MW | MW,O,SL | |
| 2 | 2 | 2 | 1 | 1,2 | 2,1,1 | 14 | |||
| 22 | 45.05 | – | O,MW | O,MW | O,MW | – | O | MW,SL,O | |
| 1,2 | 1,2 | 1,2 | 0 | 1 | 2,1,1, | 14 | |||
| 23 | 49.77 | – | O,MW | O,MW | O,MW | O | O,MW | O,MW,ML | |
| 1,2 | 1,2 | 1,2 | 1 | 1,2 | 1,2,2 | 18 | |||
| 24 | 53.84 | – | O,MW | O,MW | O,MW | – | O,MW | O,SL | |
| 1,2 | 1,2 | 1,2 | 0 | 1,2 | 1,1 | 14 | |||
| Total scores | 33 | 33 | 33 | 15 | 30 | 45 | 189 | ||
| CI (95%) | 15.75 (17.53–13.97) | ||||||||
Animals were clinically evaluated monthly for: alopecia (A); onycogryphosis (O); skin lesions (S), oedema (OE), popliteal and cervical lymph node enlargement and loss of weight.
Three levels of lymph node enlargement were discriminated: 0 for no detection, 1 for small (SL; up to 1 cm); 2 for medium (ML; 1–1.5 cm) and 3 for large lymph nodes (LL; ≥2 cm). Loss of weight was also classified as 2 for mild weight loss (MW) when ranging from 0–2 kg, and 3 for severe weight loss (SW) when ranging from 2–5 kg. Detection of alopecia; onycogryphosis or skin lesions or oedema were considered of value = 1.
We also described the evolution of clinical signs of visceral leishmaniasis using a score that quantifies the number of signs and discriminates slight from sever symptoms (Table 2). Three levels of lymph node enlargement were discriminated: 0 for no detection, 1 for small (SL; up to 1 cm); 2 for medium (ML; 1–1.5 cm) and 3 for large lymph nodes (LL; ≥2 cm). Loss of weight was also considered as level 2 for mild loss (MW) ranging from 0–2 kg, and level 3 for severe loss (SW) ranging from 2–5 kg. Detection of alopecia (A); onycogryphosis (O) skin lesions (S) or oedema (OE) was considered of value = 1. No death or severe kala-azar cases were detected during the study period. Only dog 7 died, in month 15 by the end of experiment, but due to an accident apparently not related to the disease. The average of the scores of total clinical signs, which expresses the number and severity of visceral leishmaniasis symptoms of saline controls (17.83), falls outside the 95% confidence interval of the Leishmune® immunotherapy-treated dogs 15.75 (CI95% 13.97–17.53) confirming the protection induced by the Leishmune® immunotherapy treatment, that reduced the number and severity of the symptoms. The number of clinical signs is correlated with the decline in Leishmania-specific CD4+ lymphocyte proportions (p = 0.035, Pearson Two Tailed Correlation coefficient), which points out the onset of the kala-azar immunosuppresion. Fig. 3 correlates in a bivariate graphic, the values of the symptom's scores and the CD4+ lymphocyte counts for each dog. While all Leishmune®-vaccinees are clustered showing lower scores and normal CD4+ counts, the untreated dogs number 7,8,10,15 and 25 showed very diminished CD4+ and higher scores of clinical signs, typical of canine visceral leishmaniasis. They represent 42% of the untreated control dogs. On the other hand, untreated controls number 1,2, and 3 which spontaneously lost their antibody response (Fig. 1), sustained normal CD4+ counts and showed strong IDR reactions, displayed the lowest scores of clinical signs (Table 2 and Fig. 3). Interestingly, while control dogs 7,8 and 10 from family B, dog 15 from family C and dog 25 from family E are immunosupressed, the Leishmune®-treated dogs 11,12 and 13 (family B), dogs 14 and 16 (family C) and dog 24 (family E), despite their common genetic backgrounds are highly protected (Fig. 3).
Fig. 3.
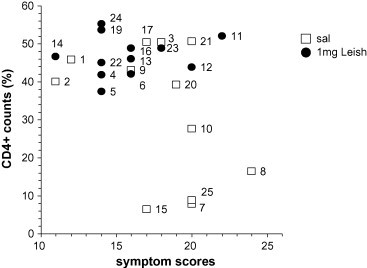
Correlation between increase in symptoms scores and decrease in CD4+ Leishmania-specific counts. Data represent in a bivariate graphic the correlation between the individual symptoḿs scores and the CD4+ Leishmania-specific lymphocyte counts. While all Leishmune®-vaccinees are clustered showing lower clinical scores and normal CD4+ counts, the untreated dogs number 7,8,10,15 and 25 showed very diminished CD4+ and higher scores of clinical signs, typical of canine visceral leishmaniasis.
In Table 3 , we further summarized the results of parasite evidence from each dog at month 6, 9 and 11 after infection, and the results of parasite detection in liver, spleen and lymph nodes obtained after autopsy in month 15. No positive results were seen at month 6, in the in vitro culture analysis of blood and bone marrow samples (results not shown). On the other hand, the in vivo parasite amplification of blood, bone marrow and lymph node samples in hamsters (months 6 and 11), and the bone marrow PCR analysis (month 9) showed higher sensitivity (Table 2). We recorded as positive, hamsters infected with dog samples 90 days before that either died of visceral leishmaniasis or had parasites in spleen or liver. Taking into the account the proportion of positive results among the total of evaluations, the saline treated group showed a higher percent of parasite evidence (35/93; 37.6%) than the Leishmune® treated group (28/96; 29.2%) (Table 3) indicating that for the saline treated animals the disease was in progress, whereas the vaccinated animals controlled their parasitaemia and probably their potential infectiousness to insects. This difference however, was not statistically significant. Of note, dogs 1,2,3 from the saline control and dogs 4 and 5 from the vaccinated group which did not show any parasite evidence belong to the same family and litter suggesting a possible genetic background for the resistance of these animals.
Table 3.
Parasitologycal evidence of Leishmania infection in control and Leishmune® immunotherapy-treated dogs with time
| S | 6 m | 9 m | 11 m |
15 m |
L | 6 m | 9 m | 11 m |
15 m |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMh | BM PCR | BMh | Bh | Ln | l | S | Ln | BMh | BM PCR | BMh | Bh | Ln | L | s | Ln | ||
| 1 | − | − | − | − | − | − | − | − | 4 | − | − | − | − | − | − | − | − |
| 2 | − | − | − | − | − | − | − | − | 5 | − | − | − | − | − | − | − | − |
| 3 | − | − | − | + | − | − | − | − | 6 | D | − | − | − | − | − | − | − |
| 7 | − | + | + | D | + | Nd | Nd | Nd | 11 | − | + | + | − | + | − | + | + |
| 8 | + | + | + | − | + | − | + | + | 12 | − | − | − | − | − | − | − | − |
| 9 | + | + | − | D | − | − | − | − | 13 | + | + | + | − | − | − | − | − |
| 10 | − | − | + | − | − | − | − | − | 14 | − | − | + | + | − | − | − | − |
| 15 | − | + | + | + | + | − | + | − | 16 | + | − | D | D | − | − | − | − |
| 17 | D | − | D | − | − | − | − | − | 19 | D | − | + | − | + | − | + | + |
| 20 | − | − | D | + | + | − | + | + | 22 | − | − | − | + | − | − | − | + |
| 21 | + | − | D | D | + | − | + | + | 23 | + | + | + | − | + | + | + | + |
| 25 | − | − | − | − | − | + | − | + | 24 | − | − | − | − | − | − | − | − |
| Signs | 4 | 4 | 7 | 6 | 5 | 1 | 4 | 4 | 5 | 3 | 6 | 3 | 3 | 1 | 3 | 4 | |
| Total | 12 | 12 | 12 | 12 | 12 | 11 | 11 | 11 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | 12 | |
The Leishmania infection was confirmed in saline (S) or Leishmune®-treated dogs (L) by hamster's in vivo culture of bone marrow (BMh), blood (Bh) or by Giemsa stained lymph node (Ln) samples and by PCR analysis for Leishmanial DNA in bone marrow (BM PCR). The presence of Leishmania amastigotes was confirmed after dog's autopsy in liver (l), spleen (s) and lymph nodes (Ln) by microscopy analysis of Giemsa stained smears in month 15. D = hamsters that died of clinically and parasitologycally confirmed visceral leishmaniasis. m = months after infection; Nd = not determined.
A significant positive correlation was found between the evolution of the number of symptoms and the number of parasitological evidences with time (p = 0.038), starting from month 9 after infection, soon after complete vaccination. This confirms the protective potential of the enriched-Leishmune® vaccine that reduced the clinical symptoms, parasite evidence and infectiousness of vaccinated dogs, modulating the outcome of the infection.
The safety and reactogenicity of the 1 mg saponin-Leishmune® vaccine were also assessed. The incidence of adverse effects in dogs vaccinated with 1 mg-Leishmune® vaccine was quantified as the percentage of dogs showing any sign of pain, local swelling, apathy, anorexia, diarrhoea or vomit (Table 4 ), recorded after one or more injections of the vaccine. The number of dogs showing pain (25%), significantly increased from the 1st to the 3rd dose (p < 0.001, ANOVA). The pain after each vaccination dose only lasted for 48 h (p = 0.006). Local swelling was the most commonly noticed adverse effect (63%), and although the number of reactive dogs was apparently increased after the first dose (Table 4), no significant differences between doses 1,2 and 3 were noted. Also, in 92% of the animals, the swelling reaction was transient, declining after the first 24 h after each dose and completely disappearing fourth days after injection (Table 4). Apathy reactions (11%), significantly decreased (p = 0.039) after the first 24 h hours after each dose (p < 0.05; Tukey's honestly significant difference method, SPSS for windows). No deaths, anorexia, vomit, diarrhoea, allergy or anaphylactic effects were registered indicating that the adverse effects were mild and that the vaccine was very tolerable.
Table 4.
Percentage of dogs showing pain, local swelling, apathy, anorexia, diarrhoea or vomit after vaccination with 1 mg Leishmune® and decline of the adverse reactions along the time
| Adverse effects | Reactive dogs (%)a | Number of dogs with adverse reaction along the time |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1st dose |
2nd dose |
3rd dose |
||||||||
| Day 1 | Day 2 | Day 4 | Day 1 | Day 2 | Day 4 | Day 1 | Day 2 | Day 4 | ||
| Pain | 25 | 1 | 0 | 0 | 2 | 1 | 0 | 5 | 1 | 0 |
| Local swelling | 63.3 | 6 | 0 | 0 | 8 | 4 | 1 | 8 | 2 | 1 |
| Apathy | 11 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Anorexia | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Diarrhoea | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Vomit | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Data refers to the percent of dogs among the total sample (n = 12) which showed any adverse effect at any time after vaccination.
The results of evolution of: anti-FML IgG antibodies, IDR to L. (L.) donovani lysate, CD4+ Leishmania-specific lymphocytes counts in blood (in vitro), parasite or DNA evidence and clinical signs point to the positive immunotherapeutic potential of the 1 mg saponin-Leishmune® vaccine on the development of canine visceral leishmaniasis and its potential effect on dog's infectiousness to phlebotomines. The toxicity analysis revealed that the vaccine was safe and with acceptable reactogenicity.
4. Discussion
Phase IIa trials are designed to check the vaccine-induced protection against an experimental challenge. Although they are needed in order to standardize the vaccine dosage, route and schedule previous to a field test, they have a main limitation: the questionable representativity of artificial challenges [41]. Indeed, results obtained from challenges using laboratory-adapted parasite strains challenges differ from those induced by parasite in nature. This effect is particularly striking in the case of a typical insect-borne disease such as visceral leishmaniasis.
Although the Leishmania (L.) chagasi strain used in this work was isolated from a human kala-azar case and was previously used as challenge in two kennel studies (106 promastigotes) [18], [42], it did not induce any death nor severe cases of visceral leishmaniasis among the infected controls. Indeed, using a high inoculum (2 × 108 amastigotes), considered two million times higher than that delivered in nature [19], [43], three untreated control dogs (1,2 and 3) and three vaccined animals (dogs 4,5 and 6) only developed a mild infection. The heterogeneity in the outcome of canine visceral leishmaniasis infection and the spontaneous remission is well described in the literature, so finding dogs that were asymptomatic and spontaneously cured was expected to occur in both groups [2], [5], [42]. Interestingly, dogs 1,2,3,4,5,6 belong to the same family and the same litter, suggesting a genetically based resistance to the infection (recently proved in dogs [42], [43]), more than the low infectivity of the Leishmania strain. Being aware of that fact, we purposely randomized the SRD animals according to their family origin, distributing half of each litter in the saline control and the other half in the vaccine group. The determination of which dog composed each group was done by draft. This natural resistance did not impede however, the significant increase in the symptomatology and decrease in Leishmania-specific CD4+ counts of the saline controls, whose averages fell outside the IC95% of vaccinated dogs disclosing the protective effect of the immunotherapy treatment. Ramiro et al. [19] justified the use a higher inoculum to assure that the lack of infection in protected animals is due to the immune response achieved by vaccination and not to natural resistance to the disease. The absence of severe clinical signs and deaths, both in this investigation and in the work of Ramiro et al. [19], and the presence of animals resistant to infection, prove however, that the high inoculum does not itself guarantee susceptibility. This should be probably associated to natural inoculation through the phlebotomine bite [44] or to the variation in dog's genetic background associated to the described NRAMP1 gene [42] and/or the MHC classII DLA-DRB1 genotype, significantly associated with levels of anti-Leishmania IgG and parasite status assessed by PCR [43]. In any case, the mongrel dogs participating in the present Phase IIa trial indeed represent the susceptibility of a heterogenic dog population to the disease found in larger natural populations.
The study of the immunotherapeutic effect of an anti-Leishmania vaccine in mice [31], [32], [33] and dogs is very preliminary [34]. The development of an immunotherapeutic tool against visceral leishmaniasis is particularly important in Brazil, where the control campaign against human kala-azar is based on the removal and sacrifice of the infected dogs and where chemotherapy is not recommended, as it is not completely efficient and maintains the parasite reservoir [1], [15], [16]. The potential effect of the FML (Fucose-Mannose Ligand)-vaccine on immunotherapy of canine visceral leishmaniasis was first demonstrated in 21 L. (L.) chagasi naturally infected dogs that were seropositive to FML but completely asymptomatic at the beginning of vaccination [34]. While 37% of the untreated controls died, the vaccinees remained 90% asymptomatic, healthy, with normal CD4+ and CD21+ lymphocyte proportions until month 22, after vaccination [34]. These dogs also received the FML-saponin preparation (1 mg adjuvant) and remained healthy and asymptomatic for five years (unpublished results). We used an increased saponin concentration based on our previous effective results of immunotherapy in the murine model [33].
Different from previous results of experimental infection with L. (L.) donovani and natural infection with L. (L.) chagasi (90–120 days) [18], [34], [45], [46], the anti-Leishmania antibodies in this investigation only became evident between 150 to 180 days. The literature estimates that seroconversion in nature occurs on average 94 days after infection and it takes more 105 days for the dog to become symptomatic and infectious for the insect vector (199 days) [2]. Our results indicate lower virulence of the L. (L.) chagasi strain that showed a delay in seroconversion [46]. Significant correlations however were found in untreated dogs, between the increase in anti-FML antibodies and the increase in clinical signs which itself is correlated with the increase in number of parasitological evidence and the decrease in Leishmania-specific CD4+ lymphocyte proportions. Both variables are highly associated with infectiousness to phlebotomine [2], [40]. This means that, in spite of use of a strain that shows a delay in seroconversion, the dog's infection simulated the natural infection in the field. On the other hand, after vaccination, a rapid and significant increase of IgG anti-FML antibodies was observed in vaccinees, as described first for the immunoprophylactic vaccine [27], [28] and as was expected for the use of a vaccine composed of QuilA saponin [47] and glycoproteins antigens [26], [48]. The higher anti-FML IgG2 response detected in dogs treated with the Leishmune® together with the reduction of the IgG1 antibodies indicate the induction of a protective/curative TH1 response [2], [19], [34], [49], [50], [51]. The response induced by Leishmune® was similar to that achieved in naturally infected dogs after immunotherapy with a FML-saponin vaccine, [34] and seems to be stronger than that reported by Ramiro et al. [19] for dogs vaccinated with LACK formulations, which only showed higher IgG2/IgG1 ratios between days 28–42, after infection. In the present study the maximal IgG2 predominance was sustained from month 9 to month 15.
Significant immunological responses and clinical protection were demonstrated in this investigation. Significant positive correlation was found between the evolution of the number of symptoms and the number of parasitological evidences with time, while negative correlation was found between the increase in clinical signs and the decrease in CD4+ populations disclosing the curative potential of the saponin enriched-Leishmune® vaccine. Although the clinical cure was not complete in the vaccinated dogs, the accumulated scores were much higher in untreated than in treated animals. Indeed, the scores of untreated animals increased from month 11, while they were low and stable in vaccines until month 15, suggesting that the protective effect lasted throughout the study period.
Cellular immune response was evaluated by the DTH response and the CD4+, CD8+ and CD21+ lymphocyte-specific proliferation against the Leishmania antigen. While saline controls showed significant decrease in the CD4+ Leishmania-lymphocyte specific population, expected for kala-azar immunosupression, the increase in intradermal response and the sustained CD4+ Leishmania-lymphocyte population, achieved in vaccinees revealed a TH1 mediated immune response. Different from our previous results [34], and although expected to be enhanced in immunity against parasite protozoa [52] and in animals treated with Quillaja saponaria saponin adjuvants [47], no significant increase in CD8+ populations was observed in Leishmune® vaccines.
In previous work, dogs prophylactically vaccinated with Leishmune® (0.5 mg saponin) showed absence of parasites through their correlated negative reactions in lymph node PCR, skin immunohistochemistry, blood PCR analysis and absence of symptoms [21]. In the present investigation, significant reduction in the number of clinical signs was correlated with the decrease in parasitological signs, sustained normal CD4+ proportions, increase in levels of anti-FML IgG and IgG2 antibodies, confirming the immunotherapeutic potential of the formulation on canine visceral leishmaniasis. In both the immunoprophylactic and the immunotherapeutic vaccine, our results suggest the reduced infectivity of the vaccinated dogs. Very similar results were obtained in the first immunotherapy with the enriched-Leishmune® vaccine on asymptomatic naturally infected dogs from a Brazilian endemic area [34], which remain healthy until now, five years after the beginning of vaccine treatment. On the other hand, in this work, the increase in symptomatology of saline controls correlated with the increase in IgG antibodies, parasite evidence and with the decrease in CD4+ Leishmania–specific lymphocyte populations confirmed the recent literature [2], [21], [45], [53], [54] indicating that, despite the mild infection, there is an increase in infectiousness for phlebotomines.
Leishmune® prophylactic formulation is a transmission blocking vaccine (TBV). Dog's antibodies present in sera, even 12 months after vaccination, led to 79.3% inhibition of sand fly infection [30]. The TBV property of Leishmune® vaccine might have been enhanced in the immunotherapeutic formula used in this study by the increase in saponin concentration. The lack of infectiousness of Leishmune®-treated dogs to sand flies is suggested by the normal levels of CD4+ specific lymphocytes [40], [53], the lower proportions of parasitological evidences and the high and consistent anti-FML IgG2 antibody response that would lead to the decline or interruption of the epidemy in nature [30].
Two studies in literature report kennel experiments of dog's prophylactic vaccination against visceral leishmaniasis due to Leishmania (L.) infantum. Ramiro et al. [19] used a prime boost with DNA plasmid and recombinant vaccinia virus expressing the LACK antigen (rVV-LACK) from L. (L.) infantum in dogs challenged with L. (L) infantum. IgG antibodies and clinical symptoms were found in 5/5 untreated controls, 4/5 LACK-DNA and 2/5 LACK-DNA + rVV-LACK treated dogs. The rVV-LACK formulation was also the best in decreasing liver and spleen parasite burden and enhancing in vitro lymphocyte proliferation against the LACK antigen. This group however, produced coincidental IFNγ and IL4 peaks that disappeared one month after infection [19]. The statistical significance of these results is however not available, probably due to the small number of animals. Rafati et al. [20] used a prime boost with DNA and recombinant protein of the Cistein proteinases a and b of L. (L.) infantum in combination with Montanide 720 and CPG on ten dogs further challenged with L. (L.) infantum. The vaccinated group showed IgG, IgG1 and IgG2 antibody synthesis, stimulation of lymphocyte proliferation, IFNγ/IL10 secretion and DTH response enhanced over controls, with less positive results in culture and PCR for Leishmania DNA. No clinical signs were reported in neither group, probably due to the very low infective challenge (5 × 106 promastigotes) [20]. The main contribution of that study was the analysis of the immunogenicity of the vaccine and not of the efficacy. The immunogenic potential detected in the formulation was expected for the use of Montanide 720 and CpG sequences. Knowing the highly heterogenic degree of infection observed in canine visceral leishmaniasis [42], [43] no significant conclusion might be drawn from the study which used ten vaccinated dogs and only two control untreated dogs.
The saponin adjuvant concentration of the therapeutic Leishmune® vaccine is the double (1 mg) of that composing the prophylactic formulation (0.5 mg) [27], [28] and was very tolerable and effective in the previous immunotherapy assay [34]. Each prophylactic Leishmune® dose contains about 90 μg of QS21 saponin, as the main adjuvant active compound [24]. The therapeutic formula then includes 180 μg of QS21/dose. The use of 100 μg of QS21 showed perfect tolerability in mice vaccinated with the FML-saponin vaccine [26], [23], [55], [56]. Also, doses of 100 μg are considered tolerable and now recommended for use in humans submitted to melanoma immunotherapy [57]. A Babesia canis vaccine composed of parasite antigen and 1 mg of QuilA adjuvant that contains about 400 μg of QS21 Quillaja saponaria saponin [26] was reported [58]. This vaccine contains 2.2 times the QS21 concentration of the immunotherapic Leishmune® vaccine and led to 100% local pain, 20% of anorexia, 33% of listlessness and 93% of swelling. In spite of these results, its use has been reported since 1992 [58].
The Leishmune® prophylactic vaccine containing 0.5 mg saponin induced transient reactions of local pain (40.87%), anorexia (20.48%), apathy (24.17%), local swelling reactions (15.90%), vomit (2.4%) and diarrhoea (1.5%). No dead by anaphylaxis occurred, and only two dogs (0,1%) showed allergic reactions (facial oedema and itching) [29]. Transient alopecia on injection site occurred in only 0.28% of the dogs with total recovery and no need of treatment. All the mild adverse events in response to Leishmune® injection were transient and disappeared before the injection of the following vaccine dose [29]. In spite of the double adjuvant concentration used in the present work, the number of dogs showing pain (25%) and apathy (11%) were lower. No deaths, anaphylaxis, anorexia, allergy, vomit or diarrhoea events were detected indicating that reactogenicity did not increase in a dose-response. The difference in the reactogenicity of the 0.5 and the 1 mg vaccine might be related to the different evaluation protocols. While the 0.5 mg formulation was evaluated on a daily basis for 14 days after each injection by the dog owners [29], the immunotherapeutic vaccine was evaluated in experimental kennel dogs, by veterinarians on day 1,2,4 and 9 after each dose. Also, in the vaccination with the 0.5 mg vaccine, different sites for injections were used showing that subcutaneous injections in the neck induced less reactions [29]. In the present study, the neck was the injection site. This might explain the detected lower reactogenicity reported. In both studies, most of the adverse effects were mild and mostly disappeared within five days after injection. The only increased adverse effect of the immunotherapeutic formulation was the local swelling (from 15.9% in the 0.5 mg vaccine to 63% in the 1 mg vaccine), characteristic of the expected inflammatory response subsequent to the Quillaja saponaria saponin injection [23], [26], [58], which was in spite of that, mostly reverted by the fourth day after injection.
The safety assay of the 0.5 mg industrial Leishmune® vaccine [29] is the first one in literature which actually describes the reactogenicity of a Quillaja saponaria vaccine (Leishmune®) in more than 600 dogs. The vaccine was considered tolerable and non toxic [29]. No other studies about dog vaccines reported such information. Of note and different from [29], here we report on the analysis of a new experimental vaccine. Regarding the cost-benefit analysis, one must keep in mind that treatment with the 1 mg saponin vaccine might be worthwhile, for its therapeutic potential and in spite of some undesirable side effects, especially given that zoonotic visceral leishmaniasis is a fatal human and canine disease increasing in endemic areas and whose epidemiological control involves culling and euthanasia of Leishmania-infected dogs.
In the present investigation, we have analysed the effect of the adjuvant-enriched-Leishmune® vaccine against experimental canine visceral leishmaniasis. We concluded that the significantly increased IgG2 antibody response, the increase in intradermal response and the sustained CD4+ Leishmania-lymphocyte population together with the decrease in clinical and parasitological signs of disease achieved for those vaccinated confirm the significant immunotherapeutic potential of the enriched-Leishmune® vaccine, its TH1-mediated immune response and its potential use for the control of canine visceral leishmaniasis in endemic areas.
Acknowledgments
This work was financially supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Recursos Humanos em Áreas Estratégicas (RHAE/CNPq), Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ-PRONEX and CNE fellowship), Ministério da Ciência e Tecnologia (MCT/PRONEX). The authors thank Andrew Macrae from the Instituto de Microbiologia Professor Paulo de Góes, Universidade Federal do Rio de Janeiro for the English language editing.
References
- 1.Tesh R. Control of zoonotic visceral leishmaniasis. Is it time to change strategies? Am J Trop Med Hyg. 1995;52:287–292. doi: 10.4269/ajtmh.1995.52.287. [DOI] [PubMed] [Google Scholar]
- 2.Courtenay O., Quinnell R.J., Garcez L.M., Shaw J.J., Dye C. Infectiousness in a cohort of Brazilian dogs: why culling fails to control visceral leishmaniasis in areas of high transmission. J Inf Dis. 2002;186:1314–1320. doi: 10.1086/344312. [DOI] [PubMed] [Google Scholar]
- 3.Palatnik-de-Sousa C.B., Melo L.M.B., Borja–Cabrera G.P., Palatnik M., Lavor C.C. Improving methods for epidemiological control of canine visceral leishmaniasis based on a mathematical model. Impact on the incidence of the canine and human disease. 2004. Ann Braz Acad Sci. 2004;76:583–593. doi: 10.1590/s0001-37652004000300012. [DOI] [PubMed] [Google Scholar]
- 4.MS-SINAN-Secretaria de Vigilância em Saúde. Manual de Vigilância e Controle da Leishmaniose Visceral. Editora MS. 2003. Brasília-DF. pp. 28.
- 5.Alvar J., Molina R., San Andrés M., Tesouro M., Nieto J., Vitutia M. Canine leishmaniasis: Clinical, parasitological and entomological follow-up after chemotherapy. Ann Trop Med Parasitol. 1994;88:371–378. doi: 10.1080/00034983.1994.11812879. [DOI] [PubMed] [Google Scholar]
- 6.Ranque J., Ranque M., Cabassu J., Cabassu H. Le diagnostic précoce de la leishmaniose canine par la ponction ganglionnaire. Réflexions à propos de soixante examens positifs obtenus en dix mois dans la région Marseillaise. Bull Acad Nat Med. 1948;132:339–340. [PubMed] [Google Scholar]
- 7.Marzochi M.C.A., Coutinho S.G., Souza W.J.S., Toledo L.M., Grimaldi G., Jr., Momen H. Canine visceral leishmaniasis in Rio de Janeiro, Brazil. Clinical, Parasitological, Therapeutical and Epidemiological findings. (1977–1983) Mem Inst Osw Cruz. 1985;80:349–357. doi: 10.1590/s0074-02761985000300012. [DOI] [PubMed] [Google Scholar]
- 8.Oliva G., Gradoni L., Cortese L., Orsini S., Ciaramella P., Scalone A. Comparative efficacy of meglumine antimoniate and aminosidine sulphate, alone or in combination, in canine leishmaniasis. Ann Trop Med Parasitol. 1998;92:165–171. doi: 10.1080/00034989860003. [DOI] [PubMed] [Google Scholar]
- 9.Lanotte G., Rioux JÁ, Pereires J., Vollhardt Y. Écologie des leishmanioses dans le sud de la France. 10. Les formes évolutives de la leishmaniose viscérale canine. Élaboration d’une typologie bio-clinique à finalité épidémiologique. Ann Parasitol. 1979;54:277–295. [PubMed] [Google Scholar]
- 10.Reiter I. Von, Kretzschmar A., Boch J., Krampitz H. Zur leishmaniose des hundes. Infektionsverlauf, diagnose un therapieversuche nach exp. Infection vom Beagles mit Leishmania donovani (st. Kalkutta) Berl Münc Tierärztl Wschr. 1985;98:40–44. [PubMed] [Google Scholar]
- 11.Organização Mundial da Saúde. Lucha contra las leishmanioses. Serie de informes técnicos 1990; 793: 1–177.
- 12.Ikeda-García F, Lopes RS, Marques FJ, Lima VMF, Morinishi CK, Bonnello FL et al. Clinical and Parasitological evaluation of dogs naturally infected by Leishmania (Leishmania) chagasi submitted to treatment with meglumine antimoniate. Vet parasitol 2006; (in press). [DOI] [PubMed]
- 13.Schettini D.A., Costa V.A.P., Souza L.F., Demichelli C., Rocha O.G., Melo M.N. Pharmacokinetic and parasitological evaluation of the bone marrow of dogs with visceral leishmaniasis submitted to multiple dose treatment with liposome-encapsulated meglumine antimoniate. Braz J Med Biol Res. 2005;38:1879–1883. doi: 10.1590/s0100-879x2005001200017. [DOI] [PubMed] [Google Scholar]
- 14.Gradoni L., Maroli M., Gramiccia M., Mancianti F. Leishmania infantum infection rates in Phlebotomus perniciosus fed on naturally infected dogs under antimonial treatment. Med Vet Entomol. 1987;1:339–342. doi: 10.1111/j.1365-2915.1987.tb00364.x. [DOI] [PubMed] [Google Scholar]
- 15.Palatnik-de-Sousa C.B., Santos W.R., França-Silva J.C., da Costa R.T., Barbosa Reis A., Palatnik M. Impact of canine control on the epidemiology of canine and human visceral leishmaniasis in Brazil. Am J Trop Med Hyg. 2001;65:510–517. doi: 10.4269/ajtmh.2001.65.510. [DOI] [PubMed] [Google Scholar]
- 16.Dye C. The logic of visceral leishmaniasis control. Am J Trop Med Hyg. 1996;55:125–130. doi: 10.4269/ajtmh.1996.55.125. [DOI] [PubMed] [Google Scholar]
- 17.Khalil E.A., El Hassan A.M., Zijlstra E.E., Ghalib H.W., Musa B., Ibrahim M.E. Autoclaved Leishmania major vaccine for prevention of leishmaniasis: a randomised, double-blind, BCG-controlled trial in Sudan. Lancet. 2000;356:1565–1569. doi: 10.1016/s0140-6736(00)03128-7. [DOI] [PubMed] [Google Scholar]
- 18.Mayrink W., Genaro O., Franca-Silva J.C., Costa R.T., Tafuri L., Toledo V.P.C.P. Phase I and II open clinical trials of a vaccine against Leishmania chagasi infections in dogs. Mem Inst Osw Cruz MEMIOC. 1996;91:695–697. doi: 10.1590/s0074-02761996000600006. [DOI] [PubMed] [Google Scholar]
- 19.Ramiro M.J., Zárate J.J., Hanke T., Rodriguez D., Rodriguez J.R., Esteban M. Protection in dogs against visceral leishmaniasis caused by Leishmania infantum is achieved by immunization with a heterologous prime-boost regime using DNA vaccine and vaccinia recombinant vectors expressing LACK. Vaccine. 2003;21:2474–2484. doi: 10.1016/s0264-410x(03)00032-x. [DOI] [PubMed] [Google Scholar]
- 20.Rafati S., Nakhaee A., Taheri T., Taslimi Y., Darabi H., Eravani D. Protective vaccination against canine visceral leishmaniasis using a combination of DNA and protein immunization with cysteine proteinases type I and Type II of L. infantum. Vaccine. 2005;23:3716–3725. doi: 10.1016/j.vaccine.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 21.Nogueira F.S., Moreira M.A.B., Borja Cabrera G.P., Santos F.N., Menz I., Parra L.E. Leishmune® vaccine blocks the transmission of canine visceral leishmaniasis. Absence of Leishmania parasites in blood, skin and lymph nodes of vaccinated exposed dogs. Vaccine. 2005;23:4805–4810. doi: 10.1016/j.vaccine.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 22.Borja Cabrera GP, Santos FN, Paraguai de Souza E, Parra LM, Menz I, Xu Z et al. Phase I safety and immunogenicity trial of Leishmune® in dogs of Brazilian endemic areas. Third World Congress on Leishmaniasis, (Worldleish III), Palermo, Italy, 2005; pp. 116.
- 23.Palatnik-de-Sousa C.B., Santos W.R., Casas C.P., Paraguai de Souza E., Tinoco L.W., da Silva B.P. Protective vaccination against murine visceral leishmaniasis using aldehyde-containing Quillaja saponaria sapogenins. Vaccine. 2004;22:2470–2479. doi: 10.1016/j.vaccine.2004.01.072. [DOI] [PubMed] [Google Scholar]
- 24.Oliveira-Freitas E., Casas C.P., Borja-Cabrera G.P., Santos F.N., Nico D., Souza L.O.P. Acylated and deacylated saponins of Quillaja saponaria mixture as adjuvants for the FML-vaccine against visceral leishmaniasis. Vaccine. 2006;24:3909–3920. doi: 10.1016/j.vaccine.2006.02.034. [DOI] [PubMed] [Google Scholar]
- 25.Palatnik de Sousa C.B., Moreno M.B., Paraguai de Souza E., Borojevic R. The FML vaccine (Fucose-Mannose Ligand) protects hamsters from experimental kala-azar. Ciência e Cultura (J Braz Assoc Adv Sci) 1994;46:290–296. [Google Scholar]
- 26.Santos W.R., de Lima V.M.F., Paraguai de Souza E., Bernardo R.R., Palatnik M., Palatnik de Sousa C.B. Saponins, IL12 and BCG adjuvant in the FML-vaccine formulation against murine visceral leishmaniasis. Vaccine. 2002;21:30–43. doi: 10.1016/s0264-410x(02)00444-9. [DOI] [PubMed] [Google Scholar]
- 27.da Silva V.O., Borja-Cabrera G.P., Correia Pontes N.N., Paraguai de Souza E., Luz K.G., Palatnik M. A Phase III trial of efficacy of the FML-vaccine against canine kala-azar in an endemic area of Brazil (São Gonçalo do Amarante, RN) Vaccine. 2001;19:1082–1092. doi: 10.1016/s0264-410x(00)00339-x. [DOI] [PubMed] [Google Scholar]
- 28.Borja-Cabrera G.P., Correia Pontes N.N., da Silva V.O., Paraguai de Souza E., Santos W.R., Gomes E.M. Long lasting protection against canine kala-azar using the FML-QuilA saponin vaccine in an endemic area of Brazil (São Gonçalo do Amarante) Vaccine. 2002;20:3277–3284. doi: 10.1016/s0264-410x(02)00294-3. [DOI] [PubMed] [Google Scholar]
- 29.Parra L.E., Borja-Cabrera G.P., Santos F.N., Palatnik-de-Sousa C.B., Menz I. Safety trial using the Leishmune® vaccine against canine visceral leishmaniasis in Brazil. Vaccine. 2006;25:2180–2186. doi: 10.1016/j.vaccine.2006.11.057. [DOI] [PubMed] [Google Scholar]
- 30.Saraiva E.M., Barbosa A.F., Santos F.N., Borja-Cabrera G.P., Nico D., Souiza L.O.P. The FML-vaccine (Leishmune®) against canine visceral leishmaniasis: a transmission blocking vaccine. Vaccine. 2006;24:2423–2431. doi: 10.1016/j.vaccine.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 31.Handman E., Noormohanmmadai A.H., Curtis J.M., Baldwin T., Sjolander A. Therapy of murine cutaneous leishmaniasis by DNA vaccination. Vaccine. 2000;18:3011–3017. doi: 10.1016/s0264-410x(00)00109-2. [DOI] [PubMed] [Google Scholar]
- 32.Gamboa-León R., Paraguai de Souza E., Borja Cabrera G.P., Santos F.N., Miyashiro L.M., Pinheiro R.O. Immunotherapy against visceral leishmaniasis with the nucleoside hydrolase-DNA vaccine of L. donovani. Vaccine. 2006;24:4863–4873. doi: 10.1016/j.vaccine.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 33.Santos W.R., Aguiar I.A., Paraguai de Souza E., de Lima V.F.M., Palatnik M., Palatnik-de-Sousa C.B. Immunotherapy against murine experimental visceral leishmaniasis with the FML-vaccine. Vaccine. 2003;21(32):4668–4676. doi: 10.1016/s0264-410x(03)00527-9. [DOI] [PubMed] [Google Scholar]
- 34.Borja-Cabrera G.P., Cruz Mendes A., Paraguai de Souza W., Okada L.Y.H., Trivellato F.A.A., Kawasaki J.K.A. Effective immunotherapy against canine visceral leishmaniasis with the FML-vaccine. Vaccine. 2004;22:2234–2243. doi: 10.1016/j.vaccine.2003.11.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Borja Cabrera G.P., da Silva V.O., da Costa R.T., Barbosa Reis A., Mayrink W., Genaro O. The FML-ELISA assay in diagnosis and prognosis of canine visceral leishmaniasis. Am J Trop Med. 1999;61:296–301. doi: 10.4269/ajtmh.1999.61.296. [DOI] [PubMed] [Google Scholar]
- 36.Bradley D.J., Kirkley K. Regulation of Leishmania population within the host. The variable course of Leishmania donovani infections in the mice. Clin Exp Immunol. 1977;30:119–129. [PMC free article] [PubMed] [Google Scholar]
- 37.Cowell R.L., Tyler R.D. Cytology of cutaneous lesions. Vet Clin North Am Small Anim Pract. 1989;19:769–794. doi: 10.1016/s0195-5616(89)50083-4. [DOI] [PubMed] [Google Scholar]
- 38.Palatnik de Sousa C.B., Gomes E., Paraguai de Souza E., Palatnik M., Luz K., Borojevic R. Leishmania donovani: titration of antibodies to the Fucose-Mannose ligand as an aid in diagnosis and prognosis of visceral leishmaniasis. Trans Roy Soc Trop Med Hyg. 1995;89:390–393. doi: 10.1016/0035-9203(95)90022-5. [DOI] [PubMed] [Google Scholar]
- 39.Rodgers M.R., Popper S.J., Wirth D.F. Amplification of kinetoplast DNA as a tool in the detection and diagnosis of Leishmania. Exp Parasitol. 1990;71:267–275. doi: 10.1016/0014-4894(90)90031-7. [DOI] [PubMed] [Google Scholar]
- 40.Guarga J.L., Moreno J., Lucientes J., Gracia M.J., Peribanez M.A., Alvar J. Canine leishmaniasis transmission: higher infectivity among naturally infected dogs to sand flies is associated with lower proportions of T helper cells. Res Vet Sci. 2000;69:249–253. doi: 10.1053/rvsc.2000.0419. [DOI] [PubMed] [Google Scholar]
- 41.UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (TDR). Guidelines for the evaluation of Plasmodium falciparum vaccines in populations exposed to natural infections. TDR/MAL/VAC/97. World Health organization, Geneva, Switzerland.
- 42.Altet L., Francino O., Solano-Gallego L., Renier C., Sanchez A. Mapping and sequencing of the canine NRAMP1 gene and identification of mutations in leishmaniasis-susceptible dogs. Infect Immun. 2002;70:2763–2771. doi: 10.1128/IAI.70.6.2763-2771.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Quinnell R.J., Kennedy L.J., Barnes A., Courtenay O., Dye C., Garcez L.M. Susceptibility to visceral leishmaniasis in the domestic dog is associated with MHC class II polymorphism. Immunogenetics. 2003;55:23–28. doi: 10.1007/s00251-003-0545-1. [DOI] [PubMed] [Google Scholar]
- 44.Norsworthy N.B., Sun J., Elnaiem D., Lanzaro G., Soong L. Sand fly saliva enhances Leishmania amazonensis infection by modulating interleukin-10 production. Infect Immun. 2004;72:1240–1247. doi: 10.1128/IAI.72.3.1240-1247.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Borja-Cabrera GP. Análise do potencial diagnóstico, prognóstico e imunoprotetor do antígeno FML (Ligante de Fucose Manose) de Leishmania (L.) donovani,no calazar canino experimental e de área endêmica. PhD Thesis. Department of Experimental Pathology. Federal Fluminense University. 2000. pp. 79.
- 46.Quinnell R.J., Courtenay O., Garcez L., Dye C. The epidemiology of canine leishmaniasis: transmission rates estimated from a cohort study in Amazonian Brazil. Parasitol. 1997;115:143–156. doi: 10.1017/s0031182097001200. [DOI] [PubMed] [Google Scholar]
- 47.Marciani D.J. Vaccine adjuvants: role and mechanisms of action in vaccine immunogenicity. Drug Discov Today. 2003;8:934–943. doi: 10.1016/s1359-6446(03)02864-2. [DOI] [PubMed] [Google Scholar]
- 48.Paraguai de Souza E., Bernardo R.R., Palatnik M., Palatnik de Sousa C.B. Vaccination of Balb/c mice against experimental visceral leishmaniasis with the GP36 glycoprotein antigen of Leishmania donovani. Vaccine. 2001;19:3104–3115. doi: 10.1016/s0264-410x(01)00031-7. [DOI] [PubMed] [Google Scholar]
- 49.Deplazes P., Smith N.C., Arnold P., Lutz H., Eckert J. Specific IgG1 and IgG2 antibody responses of dogs to Leishmania infantum and other parasites. Parasite Immunol. 1995;17:451–458. doi: 10.1111/j.1365-3024.1995.tb00914.x. [DOI] [PubMed] [Google Scholar]
- 50.Solano-Gallego L., Riera C., Roura X., Inieste L., Gallego M., Valladares J.E. Leishmania infantum-specific IgG, IgG1 and IgG2 antibody responses in healthy and ill dogs from endemic areas. Evolution in the course of infection and after treatment. Vet Parasitol. 2001;96:265–276. doi: 10.1016/s0304-4017(00)00446-5. [DOI] [PubMed] [Google Scholar]
- 51.Mendes C.O., Paraguai de Souza E., Borja-Cabrera G.P., Melo Batista L.M., Santos M.A., Parra L.E. IgG1/IgG2 antibody dichotomy in sera of vaccinated or naturally infected dogs with visceral leishmaniasis. Vaccine. 2003;21/19–20:2589–2597. doi: 10.1016/s0264-410x(03)00046-x. [DOI] [PubMed] [Google Scholar]
- 52.Carvalho L.H., Sano G.-H., Hafalla J.C.R., Morrot A., Curoto de lafaille M.A., Zavala F. IL-4-secreting CD4+ T cells are crucial to the development of CD8+-cells responses against malaria liver stages. Nat Med. 2002;8:166–170. doi: 10.1038/nm0202-166. [DOI] [PubMed] [Google Scholar]
- 53.Travi B.L., Tabares C.J., Cadena H., Ferro C., Osorio Y. Canine visceral leishmaniasis in Colombia: relationship between clinical and parasitologic status and infectivity for sand flies. Am J Trop Med Hyg. 2001;64:119–124. doi: 10.4269/ajtmh.2001.64.119. [DOI] [PubMed] [Google Scholar]
- 54.Moreno J., Nieto J., Chamizo C., Gonzalez F., Blanco F., Barker F. The immune response and PBMC subsets in canine visceral leishmaniasis before and after chemotherapy. Vet Immunopathol. 1999;30:181–195. doi: 10.1016/s0165-2427(99)00096-3. [DOI] [PubMed] [Google Scholar]
- 55.Palatnik de Sousa C.B., Paraguai de Souza E., Gomes E.M., Borojevic R. Experimental murine Leishmania donovani infection: Immunoprotection by the Fucose-Mannose Ligand (FML) Braz J Med Biol Res. 1994;27:547–551. [PubMed] [Google Scholar]
- 56.Santos W.R., Paraguai de Souza E., Palatnik M., Palatnik de Sousa C.B. Vaccination with the FML antigen (Fucose-Mannose Ligand) of Leishmania donovani in the Swiss Albino model. Vaccine. 1999;17:2554–2561. doi: 10.1016/s0264-410x(99)00058-4. [DOI] [PubMed] [Google Scholar]
- 57.Slovin S.F., Ragupathi G., Fernandez C., Jefferson M.P., Diani M., Wilton A.S. A bivalent conjugate vaccine in the treatment of relapsed prostate cancer: a study of glycosylated MUC-2-KLH and Globo H-KLH conjugate vaccines given with the new semi-synthetic saponin immunological adjuvant GPI-0100 or QS21. Vaccine. 2005;23:3113–3122. doi: 10.1016/j.vaccine.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 58.Schetters T.P.M., Kleuskens J., Scholtes N., Bos H.J. Vaccination of dogs against Babesia canis infection using parasite antigens from in vitro culture. Parasite Immunol. 1992;14:295–305. doi: 10.1111/j.1365-3024.1992.tb00469.x. [DOI] [PubMed] [Google Scholar]


