Abstract
Vaccines produced in plant systems are safe and economical; however, the extensive application of plant-based vaccines is mainly hindered by low expression levels of heterologous proteins in plant systems. Here, we demonstrated that the post-transcriptional gene silencing suppressor p19 protein from tomato bushy stunt virus substantially enhanced the transient expression of recombinant SARS-CoV nucleocapsid (rN) protein in Nicotiana benthamiana. The rN protein in the agrobacteria-infiltrated plant leaf accumulated up to a concentration of 79 μg per g fresh leaf weight at 3 days post infiltration. BALB/c mice were intraperitoneally vaccinated with pre-treated plant extract emulsified in Freund's adjuvant. The rN protein-specific IgG in the mouse sera attained a titer about 1:1,800 following three doses of immunization, which suggested effective B-cell maturation and differentiation in mice. Antibodies of the subclasses IgG1 and IgG2a were abundantly present in the mouse sera. During vaccination of rN protein, the expression of IFN-γ and IL-10 was evidently up-regulated in splenocytes at different time points, while the expression of IL-2 and IL-4 was not. Up to now, this is the first study that plant-expressed recombinant SARS-CoV N protein can induce strong humoral and cellular responses in mice.
Keywords: SARS-CoV, Nucleocapsid protein, Plant-based vaccine, Humoral response, Cytokines regulation
1. Introduction
Severe acute respiratory syndrome (SARS) is an infectious disease caused by a newly evolved coronavirus (SARS-CoV) [1]. SARS was first detected in the Guangdong Province of China in late 2002. It rapidly spread across the world, and more than 8000 cases have been recorded thus far, with 10% mortality [2]. SARS-CoV infection may cause fever, pneumonia, diarrhea, respiratory lesions, or even death [3]. SARS-CoV was a zoonotic coronavirus in bats [4] or civets [5], [6] that transcended the species barrier and then infected humans [7]. The SARS-CoV genome is a polyadenylated RNA of 29,727 nucleotides which encodes the 5′-replicase (rep) and at least 7 structural proteins, namely, the spike (S), 3a, envelope (E), membrane (M), 7a, 7b, and nucleocapsid (N) proteins [8], [9], [10]. Among these structural proteins, the S, E, M, and N proteins are common in all known coronaviruses [1]. The S protein of SARS-CoV binds to the cellular receptor ACE2 and then mediates viral entry and cell fusion; thus, the S protein is expected to be the most important candidate for vaccines [11], [12], [13]. In animal models, only S protein but not N, M, or E proteins can induce a high titer of SARS-CoV-neutralizing antibodies [14], [15]. The N protein is the structural component of the helical nucleocapsid, and it plays an important role in the viral pathogenesis, replication, RNA binding, cell cytokinesis and proliferation [16], [17], [18]. Antibodies against N and S proteins were evidently detected in SARS patients on the early stage of SARS infection [19], [20], which indicated that N protein of SARS-CoV was highly immunogenic in human. DNA vaccination of animal with SARS-CoV N gene led to the production of N-specific antibodies and specific cytotoxic T lymphocytes (CTLs) response, or even the replicon inhibition of vaccinia virus expressing N protein [21], [22], [23]. A DNA vaccine encoding N epitope stimulated cytotoxic T cells to kill N protein-expressing cell [24]. N protein expressed from recombinant measles and baculovirus resulted in strong humoral and cellular immune response in mice [25], [26]. Furthermore, the SARS-CoV N protein induced not only a temporal specific T-cell response but also a long-term memory T-cell response that persisted for 2 years in recovered SARS patients [27], [28], [29]. Although N protein alone cannot elicit the production of neutralizing antibodies against SARS-CoV, the fused peptide of N and S protein was more efficient in stimulating the production of neutralizing antibodies than S peptide alone in BALB/c mice [30]. All these data suggested that N protein was an effective elicitor of humoral and cellular response.
In addition, the pathological changes in SARS patients were associated with complicated cytokines dysregulation; moreover, the Th1/Th2 cytokine imbalance was closely correlated with the severity and outcome of SARS-CoV infection [31], [32], [33], [34]. Zhang et al. had reported that IL-6 was positively correlated with SARS severity while IL-8 and TGF-β were negatively correlated with SARS severity in patient serum, and furthermore, IL-4, IL-10, and IFN-γ only showed changes in convalescent SARS patients [31], [35]. However, another report showed that IFN-γ, IL-1, IL-6, IL-12 but not IL-2, IL-10, and IL-4 were up-regulated in SARS patients before and after treatment [35]. A serum analysis of acute SARS patients (n = 98) showed substantial elevation of IFN-γ, IL-6, IL-8, IL-10, IL-12, but not IL-2, IL-4, and TNF-α before any treatment [34]. As a key immunogen of SARS-CoV, the regulatory function of N protein on cytokines also showed complex pattern in animal system. For example, the vaccination of mice with recombinant baculovirus expressing SARS N protein resulted in augment of IFN-γ- and IL-4- secreting CD4+ cells, though IFN-γ secretion level was much high than that of IL-4, which indicated predominant Th1 response [25]. However, prior immunization of mice with recombinant vaccinia virus expressing SARS-CoV N protein and later SARS-CoV virus challenge caused significant expansion of both Th1 (IFN-g, IL-2) and Th2 (IL-4, IL-5) cytokines, reduction of anti-inflammatory cytokines (IL-10, TGF-β), as well as severe pneumonia [36], [37]. The induction of IFN-γ [25], [28], [29], IL-6 [37], IL-11 [38] and other cytokines was also observed to related with SARS-N protein. Therefore, it is worthy to evaluate the cytokine changes in our system specially regarding of Th1 and Th2 response.
Plants are now considered as promising bioreactors for pharmaceutical protein due to their safety, low cost, high output, simple storage requirement, and benefits of eukaryotic posttranslational modifications [39]. Transient expression of target protein can be easily achieved by agrobacteria infiltration, thereby saving the time spent on generation of transgenic plants. Recombinant strains of Agrobacterium tumefaciens can be intermediator of transient expression of exogenous protein in plant by inserting the gene of interest into the T-DNA region of modified A. tumefaciens plasmid and then introducing the transformed agrobacteria into plant leaves [40]. However, the utility of this system was limited because ectopic protein expression was often down-regulated by post-transcriptional gene silencing (PTGS), which operates as a natural defense mechanism against viral accumulation or foreign DNA invasion in plants [41]. In plant host, exogenous RNA was likely to be formed into short RNA duplex intermediates (siRNA or miRNA) though multiple step process, and then the duplex RNA was unwound into single strand RNA before incorporation into RISC (RNA-induced silencing complex). Finally, the selected RNA strand bound to cognate host mRNA, resulting in target mRNA cleavage or translational repression [42]. However, for the maximum accumulation of viral proteins in plant, many viruses have developed mechanisms to suppress PTGS in different steps [43], [44], [45]. For example, the tomato bushy stunt virus (TBSV) p19 protein dimer and beet yellow virus (BYV) p21 protein can bind to the siRNA or miRNA duplex, and thus block the RNA duplex dissociation and downstream action [46]. Using this strategy, high expression of exogenous proteins had been accomplished in Nicotiana benthamiana based on suppression of gene silencing by p19 protein [45].
Plant-based vaccines exhibited immunogenicity and protection against different infectious diseases [47], [48]. For example, the potato-expressed S1 protein of the coronavirus infectious bronchitis virus (IBV) protected chickens from virulent IBV infection when administered intramuscularly or orally [48]. However, among the SARS structural proteins, only S protein had been expressed in plants [49], [50]. The transgenic tomato expressing S1 protein stimulated IgA secretion in oral vaccination; but IgG secretion was not detected in parental vaccination until commercial S peptide was injected as booster in immunization [50]. In our study, the viral PTGS suppressor p19 protein was enrolled to boost the transient expression of recombinant SARS-CoV N protein (rN) in N. benthamiana. The rN protein accumulated up to an average amount of 79 μg per g fresh tobacco leaves at 3 days post infiltration (dpi). Soluble extract of plant leaves containing rN protein was emulsified with Freund's adjuvant and then used to immunize BALB/c mice. Specific IgG (IgG1 and IgG2a) antibodies were effectively induced in mice vaccinated with plant-expressed rN protein. Meanwhile, the expression profiles of IL-10 and IFN-γ were altered in splenocytes of vaccinated mice.
2. Material and methods
2.1. Cloning of the SARS-CoV N gene into plant expression vector
The N gene of SARS-CoV (Urbani strain, GenBank accession no. AY278741) is 1269 bp in length and encodes a 423-aa protein. The cDNA fragment encoding the complete N protein was amplified from a bacterial artificial chromosome (BAC) vector (kindly provided by Dr. Luis Enjuanes, CNB-CSIC, Spain) carrying the whole SARS-CoV cDNA sequence. The following primers were used for the PCR amplification of SARS CoV N gene: forward, 5′-AAGCATGCGTCGACATGTCTGATAATGGACC-3′ and reverse, 5′-ATACGCGTTTATGCCTGAGTTGAATC-3′. The amplified product carried recognition sites for the restriction enzymes SphI and MluI at the 5′ and 3′ ends, respectively. This N-gene PCR product was cloned into the pGEM-T vector to generate the new pGEM-T-N plasmid. The 1.5 kb fragment containing the SARS-CoV N gene was cleaved from pGEM-T-N with enzymes SphI and MluI and subsequently inserted into the SphI- MluI-digested pBAL vector which is a derivative of the empty plant binary vector pBA002 [51]. The new plant expression vector thus obtained was designated as pB-35S-rN. Its expression cassette contained the strong constitutive 35S promoter, the DNA sequence coding for 6 × His fusion tag, the cleavage site for the protease factor Xa, and SARS-CoV N protein. The 47 kDa recombinant N protein expressed from plasmid pB-35S-rN was referred to as rN protein. At the same time, the SARS-CoV N gene was cloned into the prokaryotic expression vector pET-32a (+) and then expressed in Escherichia coli. The purified product from E. coli, a 64-kDa recombinant N protein with Trx tag, S tag, and 6 × His tags at the N-terminus, was designated as sN protein [52]. The cDNA sequence corresponding to the p19 protein of TBSV (GenBank accession no. AJ288942) was sub-cloned into the binary vector pCambia1300-221 downstream of the 35S promoter, resulting in the new plant binary vector pC-35S-p19.
All the generated plant expression constructs were individually transformed into cells of A. tumefaciens EHA105 strain for infiltrating host plants.
2.2. Expression and preparation of recombinant SARS-CoV N protein in tobacco
Wild-type tobacco plants (N. benthamiana) were grown until 8–10 weeks old. Agrobacterium cells transformed with target plasmid were cultured at 28 °C for 20 h, centrifuged at 3200 × g, and resuspended in 10 mM MgCl2 solution supplemented with 200 μM acetosyringone. The density of the agrobacteria suspension was then optimized for infiltration (OD600 = 1.5 for pB-35S-rN and control vector pBA002; OD600 = 1.0 for pC-35S-p19). The agrobacterium strain harboring plasmid pB-35S-rN or pBA002 was mixed with that harboring plasmid pC-35S-p19 in a 1:1 ratio, and the mixture was infiltrated into young tobacco leaves with a syringe. The sample leaves were collected at different days post infiltration, immediately frozen in liquid nitrogen, and stored at −80 °C until assay. The leaf proteins were extracted with a strong denaturing buffer in order to measure rN protein expression in Western blot, using serially diluted sN protein as standard. Fresh leaf samples (50 mg) were ground in liquid nitrogen and homogenized in 100 μl extraction buffer (modified from ref. [53]) that contained 150 mM Tris–HCl (pH 7.5), 6 M urea, 2% SDS, and 2% β-mercaptoethanol. The extract was boiled for 10 min, centrifuged at 10,000 × g for 20 min at 4 °C and the supernatant was harvested. In Western blot, the rN protein in the samples were detected by a SARS-CoV N protein-specific monoclonal antibody in mouse ascites (kindly provided by Zhihong Hu, WIV, CAS, China) as primary antibody and horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (Jackson ImmunoResearch Laboratories) as secondary antibody. The blotting signal was developed with a chemiluminescent HRP substrate (Immobilon™ Western, Millipore) and finally exposed to an X-ray film.
Besides the above-mentioned strong denaturing buffer, total soluble proteins (TSP) from tobacco leaves were isolated with a non-denaturing buffer for animal immunization. The leaves were ground in liquid nitrogen, homogenized in native extraction buffer (50 mM Tris-Cl (pH 8.0), 0.5 M sucrose, 1 mM MgCl2, 10 mM EDTA, 5 mM DTT, 1 mM phenylmethylsulfonyl fluoride (PMSF), 1 mg/ml benzamidine), and then was stirred at 4 °C for 16 h. The consequent supernatant was ultra-filtrated to get rid of compounds of low molecular mass (especially deleterious alkaloids) with an Amicon Ultra-15 membrane (10 kDa, Millipore). The concentrated extract was resuspended in PBS and either injected into mice within 2 h or stored at −80 °C until use.
2.3. Immunization of mice with the plant-expressed or E. coli-expressed recombinant N protein
6- to 8-week-old female BALB/c mice were divided into four groups (7 mice per group) for the immunoassay. Each mouse was intraperitoneally (i.p.) injected with either soluble plant extract derived from 500 mg fresh tobacco leaves or 10 μg of the purified sN protein from E. coli per dose. Control plant extract without rN protein or PBS was respectively administered as negative control. The injections were performed 4 times at 14-day intervals. The antigens were emulsified with complete Freund's adjuvant for the first immunization and incomplete Freund's adjuvant for the second immunization. Later, the third and fourth injections were administered without adjuvant. Serum samples were collected from each mouse 10 days after every injection, and an enzyme-linked immunosorbent assay (ELISA) was performed to determine the IgG titer. Three days after the forth injection, the mice were sacrificed and serum samples were obtained for classification of the IgG isotypes and for Western blot analysis. Meanwhile, splenocytes of three mice per group were harvested 3 days after the third and forth injection to analyze the cytokine expression levels therein.
2.4. B-cell response elicited in mice by recombinant SARS-CoV N protein
The titer of SARS-CoV N protein-specific antibodies in the serum samples was assessed by ELISA as described by Alvarez et al. [54]. In brief, 96-well plates (BioFil, Canada) were coated overnight at 4 °C with the purified sN protein (antigen) at a concentration of 500 ng per well. The serum samples were serially diluted and incubated with antigen at 37 °C for 2 h. N protein-specific IgG in the serum samples was detected by using HRP-conjugated rabbit anti-mouse IgG (Boster, China) as secondary antibody. Color was developed by using 3,3′,5,5′-tetramethylbenzidine (TMB) as substrate, and the reaction was terminated by 1N H2SO4. The optical density was measured at 450 nm on a microplate reader (Model 550, Bio-Rad). The specificity of IgG antibodies was further confirmed in Western blot analysis. The sN protein was effectively and specifically cleaved by recombinant plum pox virus (PPV) protease [52]; therefore a pure N protein without fusion tag was harvested. In Western blot, the pure N protein was employed as antigen, and serum samples of immunized mice worked as primary antibody.
Further, the titers of IgG1 and IgG2a antibody subclass were evaluated in ELISA. After the incubation of serum samples with sN antigen, SARS–CoV N-specific IgG1 or IgG2a antibodies were detected by using the following antibodies (all from Proteintech Group Inc.): goat anti-mouse IgG1 or goat anti-mouse IgG2a, and then HRP-conjugated donkey anti-goat IgG antibody.
All the assays were independently repeated three times, and the absorbance data twice above the background were considered as positive data in ELISA.
2.5. Cytokines regulation in the splenocytes of immunized mice
Splenocytes were prepared from the immunized mice 3 days after the third or fourth injection. Total RNA was isolated from the cells with RNeasy Mini kit (QIAGEN) following the manufacturer's instructions. Each RNA sample was subjected to DNase digestion, phenol-chloroform extraction, and ethanol precipitation. The mRNA was reverse-transcribed to cDNA for quantitative Real-time PCR. The analysis of mRNA level of cytokine was performed on a thermal cycler instrument (PTC-200, MJ Researcher). Sense and antisense primers were synthesized for housekeeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (forward, 5′-TGAAGCAGGCATCTGAGGG-3′ and reverse, 5′-CGAAGGTGGAAGAGTGGGA-3′), and for the cytokine genes: IFN-γ (forward, 5′-GTCAACAACCCACAGGTCCAG-3′ and reverse, 5′-CAATCTCTTCCCCACCCCGAATC-3′), IL-2 (forward, 5′-GATGAACTTGGACCTCTGCGG-3′ and reverse, 5′-CCTTTAGTTTTACAACAGTTACTCT-3′), IL-4 (forward, 5′-ACAGGAGAAGGGACGCCAT-3′ and reverse, 5′-TTAGGCTTTCCAGGAAGTCTTTC-3′), and IL-10 (forward, 5′-GCGGACTGCCTTCAGCCAG-3′ and reverse, 5′-CACAGGGGAGAAATCGATGACAGC-3′). The real-time PCR reaction system was set up as the normal PCR reaction system except for adding 1 × SYBR Green into the reaction system. The PCR programme run as following: 94 °C for 5 min → 94 °C for 30 s, 58 °C for 30 s, 72 °C for 30 s; 35 cycles; the fluorescence being read at the end of each cycle → 72 °C for 5 min. Each sample was conducted in triplicate and two independent experiments were performed. The data was analyzed using the Opticon monitor software package (Opticon Monitor, Version 3, Bio-Rad) and Microsoft excel software.
3. Results
3.1. Expression of recombinant SARS-CoV N protein in tobacco boosted by the viral PTGS suppressor p19 protein
It has been reported that if the 35S:green fluorescent protein (GFP) transgene was expressed along with a virus-encoded PTGS suppressor p19 protein, GFP expression was not silenced [45]. We adopted a similar system to obtain high expression of heterologous protein in plant by the assistance of p19 protein. As expected, the rGFP expression was abundant in tobacco with the help of p19 at 3 dpi (Fig. 1A, lane 5), while the expression of rGFP was very weak in the no p19 control due to PTGS (Fig. 1A, lane 4). At 6 dpi, approximately 40- to 50-fold of translated product was achieved in the p19 group as compared with no p19 control. Furthermore, the expressed rGFP protein remained un-degraded for at least 10 days in this system (Fig. 1A). Similarly, when two agrobacterium culture that respectively harbored SARS-CoV N protein-expressing plasmid (B-35S-rN) and p19 protein-expressing plasmid (C-35S-p19) were co-infiltrated into tobacco leaves, the yield of recombinant SARS-CoV N (rN) protein was clearly boosted at 3 dpi (Fig. 1B-lane 3). By using a harsh denaturing buffer containing SDS and urea, most of the proteins in plant leaves were extracted; therefore, the concentration of the rN protein expressed in the tobacco leaves could be measured as compared with a serially quantified sN protein (1.5 × 10−14 mol to 7 × 10−12 mol). The plant-expressed rN protein reached an average level of 79 μg/g leaf fresh weight at 3 dpi under the p19 environment (Fig. 1D). While in the control without p19, the expression level of rN protein was intensely reduced by 3–5 times (Fig. 1B-lane 2, 1D). Meanwhile, the agrobacteria containing empty plasmid (BA002) did not result in any sign of rN production when co-injected with the p19-containing agrobacteria (Fig. 1B-lane 1 and 1D). Dissimilar to rGFP protein, the accumulation of rN protein markedly diminished at 6 dpi, regardless of whether p19-containing agrobacteria were co-infiltrated or not (Fig. 1B-lane 5 and 6, 1D). A reason for the decreased yield of rN protein may lie on the unstable character of the plant-expressed rN protein as compared to rGFP protein. A non-denaturing buffer was used to extract the TSP for immunoassays in animals. Western blot analysis showed strong rN protein signal was detected in the soluble supernatant, though more than 50% of the rN protein remained in the insoluble pellet (Fig. 1C). The soluble rN protein accounted for 0.8–1% of the TSP at 3 dpi. In most of the reported data, the recombinant proteins usually account for less than l% of the TSP in plant expression systems. Due to the deleterious effects of alkaloids in tobacco, an ultra-filtration membrane allowing the passage of molecules less than 10 kDa was selected to remove the small lethal compounds, especially nicotine (1.6 kDa).
Fig. 1.
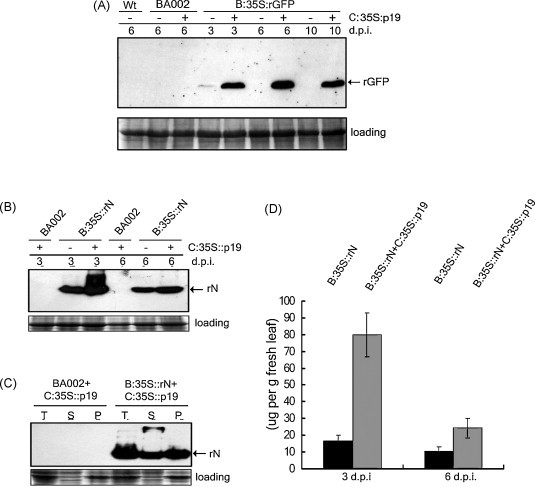
The PTGS suppressor TBSV p19 protein enhanced the transient expression of exogenous protein in N. benthamiana. Different agrobacterium cells carrying different binary vectors are infiltrated into tobacco with or without agrobacteria carrying p19-expressing vector. The infiltrated tobacco leaves were collected at 3 to 10 dpi. (A) The transient expression of recombinant GFP (rGFP) protein in N. benthamiana by Western blot using a monoclonal antibody against the 6 × His fusion tag (Santa Cruz). Wt: wild type tobacco protein; BA002: empty vector. (B) The transient expression of recombinant SARS N (rN) protein in N. benthamiana by Western blot. (C) The soluble rN protein in infiltrated-tobacco leaves at 3 dpi by Western blot analysis. T: total crude material; S: supernatant; P: pellet. (D) Quantitation of the expressed rN protein in tobacco by Western blot and then by Quantity One software, using quantified sN protein as standard.
3.2. B-cell response elicited in mice by recombinant SARS-CoV N protein
To analyze the immunogenicity of plant-expressed rN protein, the above-described soluble extract of plant leaves was emulsified in Freund's adjuvant and then injected into BALB/c mice intraperitoneally (i.p.). The mice in groups I and II were respectively immunized with control plant extract (Fig. 1C-lane 2) or plant extract that contained 2–4 μg rN protein (Fig. 1C-lane 4) for each injection. The mice in groups III and IV were respectively immunized with PBS control or 10 μg of E. coli-derived sN protein per injection. Using sN protein as antigen in ELISA, the IgG antibodies provoked by plant-derived rN protein obtained a low titer of 1:2.6 × 102 after the second injection (Fig. 2A, group II, day 24), while IgG antibodies against E. coli-derived sN protein already reached a high titer of 1:3.9 × 104 (Fig. 2A, group IV, day 24). Following the third immunization, the antibody titer of sera from group II mice rapidly accelerated and achieved an average value of 1:1.78 × 103 (Fig. 2A, group II, day 38). SARS-CoV N-specific IgG antibodies were not detected in the control group I and III during the vaccination period. In addition, the specificities of the immunoglobulins were confirmed after the fourth boost by performing Western blot, using pure N protein without fusion tag as the antigen. The 46 kDa pure N protein antigen interacted with the antisera from groups II and IV, but not with those from groups I and III (Fig. 2B). This eliminated the possibility that the serum antibodies in group II and IV mice were secreted in response to unspecific proteins other than SARS-CoV N protein. These results revealed that vaccination of BALB/c mice with tobacco-expressed rN protein successfully led to specific B-cell response.
Fig. 2.

Antibody elicited by plant-expressed rN protein in mice. (A) The IgG titers in the mouse antisera detected in ELISA. The mice in each group were i.p. administered with different antigens as following: group I-control plant extract; group II-plant extract containing rN protein; group III-PBS control; group IV-purified recombinant sN protein from E. coli. The IgG titer was indicated as the mean ± standard deviation (SD) at different time points of vaccination (day 0, 10, 24, 38, and 45). (B) The specificity of IgG antibodies was confirmed by Western blot assay. The antiserum from each group was independently used as antibody to interact with the pure N protein antigen (50 ng per lane) in Western blot. I-1 and I-2: sera from mice Nos. 1 and 2 in group I at a 1:1000 dilution; II-6 and II-8: sera from mice Nos. 6 and 8 in group II at a 1:1000 dilution; III-1 and III-2: sera from mice Nos. 1 and 2 in group III at a 1:40,000 dilution; IV-4 and IV-6: sera from mice Nos. 4 and 6 in group IV at a 1:40,000 dilution.
Furthermore, the titers of IgG1 and IgG2a subclasses were measured in the sera obtained from in groups II and IV mice three days after the forth injection, using E. coli-expressed sN protein as antigen in ELISA (Fig. 3 ). The titer of IgG1 (1:3 × 103) was approximately 10-fold higher than that of IgG2a (1:1.5 × 102 to 1:3.5 × 102) in the group II mice that were immunized with plant-expressed rN protein emulsified in Freund's adjuvant. The titer of IgG1 (1:4 × 105) was approximately 50-fold higher than that of IgG2a (1:7 × 103) in the group IV mice that were immunized with the E. coli-expressed sN protein emulsified in Freund's adjuvant. A previous report indicated that vaccination of recombinant SARS-CoV N protein purified from E. coli with incomplete Freund's adjuvant also mainly preferred the production of IgG1 than that of IgG2a in mice [28].
Fig. 3.

Titers of antibodies belong to IgG1 and IgG2a subclasses in the serum samples from group II and group IV mice. Four mice each from groups II and IV were selected for ELISA measurement. The mixture of sera obtained from mice Nos. 1 and 2 in group II was designated as II-A; II-B indicated sample from mice Nos. 6 and 8 in group II; IV-A indicated sample from mice Nos. 1 and 3 in group IV; IV-B indicated sample from mice Nos. 4 and 6 in group IV. The data were indicated as the mean ± SD.
3.3. Cytokines regulation in the splenocytes of immunized mice
Cytokines are widely recognized as important mediators of many immune and inflammatory responses. To investigate the impact of plant-derived rN protein on the regulation of cytokines, the relative mRNA levels of Th1 type (IFN-γ, IL-2), Th2 type (IL-4) and immunosuppressive type (IL-10) cytokines were evaluated in the splenocytes of Group II mice 3 days after the third and fourth vaccination (day 31 and 45) while group I mice was analyzed as control (Fig. 4 ). The expression of these four cytokines exhibited different pattern in splenocytes. When compared with group I mice, IFN-γ expression level in group II mice was significantly increased to 3.0-fold (P < 0.05) at day 31; then gradually reduced to 1.8-fold at day 45. The expression of regulatory cytokine IL-10 in group II mice was rapidly increased from 1.2-fold (day 31) to 3.7-fold (P < 0.05) (day 45). Under the influence of rN protein, IL-4 expression level diminished to 0.39-fold (P < 0.05) of the control mice after the 4th vaccination. Compared with group I mice, the IL-2 mRNA level in group II mice was weakly up-regulated to 1.6-fold (P < 0.05) after the fourth injections.
Fig. 4.

The relative expression levels of cytokines in vaccinated mouse splenocytes (n = 3). The relative mRNA levels were evaluated at day 31 and day 45 by real-time PCR analysis. The relative mRNA levels of four different cytokines in the group II mice were compared with those in group I mice. The result had been demonstrated as the value of 2−(ΔCt of group II−ΔCt of group I) (Note: ΔCt = Cttarget gene − CtGAPDH). The statistics P-value was calculated by Prism programme and indicate as * when P < 0.05.
4. Discussion
SARS-CoV infection causes disastrous aftermath; therefore, enormous efforts have been undertaken to develop effective and safe vaccines against this newly emerged virus [2]. Humoral and cellular responses had been evidently detected in animal models in response to vaccines developed with the SARS-CoV N protein or N DNA [22], [28], [55], [56]. In our study, the PTGS suppressor p19 protein enhanced the expression of the recombinant SARS-CoV N protein in tobacco. The accumulation of rN protein was brought to a maximal output of 100 μg/g fresh leaf weight at 3 dpi with the help of p19 protein. The soluble rN protein from tobacco extract provoked evident secretion of specific IgG in mice following three doses of intraperitoneal injections. Furthermore, the expression levels of cytokines in splenocytes of vaccinated mice were altered. Our study illustrated the potent immunogenicity conferred by recombinant SARS-CoV N protein expressed in tobacco. It is worthy to note that most of the mice survived after five doses of injections with tobacco leaf extract without low-molecule-mass molecules, which suggested the pre-treated tobacco crude extract can conveniently serve as immunogen carrier for animal vaccination study.
In the reported case of plant-expressed S protein, no specific IgG antibodies were detected in mice when the transgenic tobacco material was administered orally or parenterally, even after three doses [50]. In our study, the IgG antibodies specific for the plant-derived rN protein were significantly increased after the third parental injection, indicating effective stimulatory effect of rN protein on B-cell differentiation and maturation in mice. This may imply that (1) the N protein is the key immunogenic component of SARS-CoV; and (2) a large amount of the rN protein (2–4 μg rN protein per injection per mice) in the plant soluble extract enabled the switching on of antigen recognition and presentation. Compared with E. coli-expressed sN protein, plant-expressed rN protein exhibited much weaker immunogenicity (1.57 × 105 Vs 1:1.78 × 103 of antiserum titer after the 3rd immunization), which may be due to the lower amount of presented immunogen (10 μg sN protein Vs 2–4 μg rN protein per dose); the interference of high concentration of tobacco proteins injected into mice; and the usage of sN but not pure N protein as antigen in ELISA measurement.
Considering the increased IFN-γ expression, the slightly up-regulated IL-2 and down-regulated IL-4 expression in mouse splenocytes, our result indicated potential Th1 response by plant-derived rN protein in mice, as indicated by baculovirus-expressed [25] or E. coli-expressed N protein [28] in mice. Th1 response can lead to cytotoxic T cell response and virus clearance. SARS-CoV N DNA or protein vaccination in mice also repressed the replication of N-expressing cell [24] or virus [23]. However, it should be noted that N protein-vaccinated mice developed severe lung inflammation upon SARS-CoV infection [36], [57], as well as the up-regulation of Th1 and Th2 type cytokines in mice. Another concern is that mice age also affected the cytokine secretion (IFN-γ and TNF-α) and lung inflammation upon SARS-CoV infection [36], [58]. Therefore, caution should be taken in interpreting the immunologic mechanism of SARS-CoV N protein. IFN-γ may play an important role in N protein-mediated T cell response since it was commonly reported to be increased after N protein vaccination in mice and the elevation of IFN-γ was also found on the early stage of SARS patients and considered to be related with the Th1-type immunity as well as inflammatory response in SARS [35], [59]. Inflammatory cytokines such as IL-6, TNF-α were reported to be up-regulated in early SARS patient [60] and IL-6 activation was closely related to SARS N-protein but not S, M, E protein [61]. However, we found that the expression levels of IL-6 and TNF-α in rN-vaccinated mice were respectively about 1.28- and 0.89-fold of the levels in the control mice without significance (P > 0.05). IL-10 has important regulatory function in immune response, such as suppressing secretion of Th1-type cytokine, inhibiting inflammatory response and effector CD4+ cell proliferation [62]. Similar to our result, intratracheal administration of rat with SARS-CoV N protein caused significant increased IL-10 secretion in serum [63], and yet, the finding that increased IL-10 expression was induced by SARS-CoV N protein need to be studied further in order to illustrate the mechanism better.
Acknowledgments
This work was supported by grants from the European Commission Sixth Framework Program (No. SP22-CT-2004-511060). We thank Dr. Luis Enjuanes from CNB-CSIC Spain for kindly providing the SARS-CoV cDNA clone, Dr. Zhihong Hu for the monoclonal anti-SARS-CoV N protein antibody, Dr. David Baulcombe for p19 clone, and Dr. Namhai Chua for pBA002 vector. Q. X. is supported by Chinese Academy of Sciences.
References
- 1.Rota P.A., Oberste M.S., Monroe S.S., Nix W.A., Campagnoli R., Icenogle J.P. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003 May;300(5624):1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 2.Enjuanes L., Dediego M.L., Alvarez E., Deming D., Sheahan T., Baric R. Vaccines to prevent severe acute respiratory syndrome coronavirus-induced disease. Virus Res. 2007;(April) doi: 10.1016/j.virusres.2007.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peiris J.S., Yuen K.Y., Osterhaus A.D., Stohr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349(December (25)):2431–2441. doi: 10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- 4.Lau S.K., Woo P.C., Li K.S., Huang Y., Tsoi H.W., Wong B.H. Severe acute respiratory syndrome coronavirus-like virus in Chinese horseshoe bats. Proc Natl Acad Sci USA. 2005;102(September (39)):14040–14045. doi: 10.1073/pnas.0506735102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang M., Yan M., Xu H., Liang W., Kan B., Zheng B. SARS-CoV infection in a restaurant from palm civet. Emerg Infect Dis. 2005;11(December (12)):1860–1865. doi: 10.3201/eid1112.041293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kan B., Wang M., Jing H., Xu H., Jiang X., Yan M. Molecular evolution analysis and geographic investigation of severe acute respiratory syndrome coronavirus-like virus in palm civets at an animal market and on farms. J Virol. 2005;79(September (18)):11892–11900. doi: 10.1128/JVI.79.18.11892-11900.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li W., Shi Z., Yu M., Ren W., Smith C., Epstein J.H. Bats are natural reservoirs of SARS-like coronaviruses. Science. 2005;310(October (5748)):676–679. doi: 10.1126/science.1118391. [DOI] [PubMed] [Google Scholar]
- 8.Huang C., Ito N., Tseng C.T., Makino S. Severe acute respiratory syndrome coronavirus 7a accessory protein is a viral structural protein. J Virol. 2006;80(August (15)):7287–7294. doi: 10.1128/JVI.00414-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang C., Narayanan K., Ito N., Peters C.J., Makino S. Severe acute respiratory syndrome coronavirus 3a protein is released in membranous structures from 3a protein-expressing cells and infected cells. J Virol. 2006;80(January (1)):210–217. doi: 10.1128/JVI.80.1.210-217.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schaecher S.R., Mackenzie J.M., Pekosz A. The ORF7b protein of severe acute respiratory syndrome coronavirus (SARS-CoV) is expressed in virus-infected cells and incorporated into SARS-CoV particles. J Virol. 2007;81(January (2)):718–731. doi: 10.1128/JVI.01691-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He Y., Zhou Y., Liu S., Kou Z., Li W., Farzan M. Receptor-binding domain of SARS-CoV spike protein induces highly potent neutralizing antibodies: implication for developing subunit vaccine. Biochem Biophys Res Commun. 2004;324(November (2)):773–781. doi: 10.1016/j.bbrc.2004.09.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dimitrov D.S. The secret life of ACE2 as a receptor for the SARS virus. Cell. 2003;115(December (6)):652–653. doi: 10.1016/S0092-8674(03)00976-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao J., Wang W., Yuan Z., Jia R., Zhao Z., Xu X. A study on antigenicity and receptor-binding ability of fragment 450–650 of the spike protein of SARS coronavirus. Virology. 2007;359(March (2)):362–370. doi: 10.1016/j.virol.2006.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buchholz U.J., Bukreyev A., Yang L., Lamirande E.W., Murphy B.R., Subbarao K. Contributions of the structural proteins of severe acute respiratory syndrome coronavirus to protective immunity. Proc Natl Acad Sci USA. 2004;101(Junuary (26)):9804–9809. doi: 10.1073/pnas.0403492101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bisht H., Roberts A., Vogel L., Bukreyev A., Collins P.L., Murphy B.R. Severe acute respiratory syndrome coronavirus spike protein expressed by attenuated vaccinia virus protectively immunizes mice. Proc Natl Acad Sci USA. 2004;101(April (17)):6641–6646. doi: 10.1073/pnas.0401939101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Narayanan K., Kim K.H., Makino S. Characterization of N protein self-association in coronavirus ribonucleoprotein complexes. Virus Res. 2003;98(December (2)):131–140. doi: 10.1016/j.virusres.2003.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou B., Liu J., Wang Q., Liu X., Li X., Li P. The nucleocapsid protein of severe acute respiratory syndrome coronavirus inhibits cell cytokinesis and proliferation by interacting with translation elongation factor 1alpha. J Virol. 2008;82(July (14)):6962–6971. doi: 10.1128/JVI.00133-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Surjit M., Lal S.K. The SARS-CoV nucleocapsid protein: a protein with multifarious activities. Infect Genet Evol. 2008;8(July (4)):397–405. doi: 10.1016/j.meegid.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang L.R., Chiu C.M., Yeh S.H., Huang W.H., Hsueh P.R., Yang W.Z. Evaluation of antibody responses against SARS coronaviral nucleocapsid or spike proteins by immunoblotting or ELISA. J Med Virol. 2004;73(July (3)):338–346. doi: 10.1002/jmv.20096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Y., Chang Z., Ouyang J., Wei H., Yang R., Chao Y. Profiles of IgG antibodies to nucleocapsid and spike proteins of the SARS-associated coronavirus in SARS patients. DNA Cell Biol. 2005;24(August (8)):521–527. doi: 10.1089/dna.2005.24.521. [DOI] [PubMed] [Google Scholar]
- 21.Zhu M.S., Pan Y., Chen H.Q., Shen Y., Wang X.C., Sun Y.J. Induction of SARS-nucleoprotein-specific immune response by use of DNA vaccine. Immunol Lett. 2004;92(April (3)):237–243. doi: 10.1016/j.imlet.2004.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jin H., Xiao C., Chen Z., Kang Y., Ma Y., Zhu K. Induction of Th1 type response by DNA vaccinations with N, M, and E genes against SARS-CoV in mice. Biochem Biophys Res Commun. 2005;328(March (4)):979–986. doi: 10.1016/j.bbrc.2005.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim T.W., Lee J.H., Hung C.F., Peng S., Roden R., Wang M.C. Generation and characterization of DNA vaccines targeting the nucleocapsid protein of severe acute respiratory syndrome coronavirus. J Virol. 2004;78(May (9)):4638–4645. doi: 10.1128/JVI.78.9.4638-4645.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheung Y.K., Cheng S.C., Sin F.W., Chan K.T., Xie Y. Induction of T-cell response by a DNA vaccine encoding a novel HLA-A*0201 severe acute respiratory syndrome coronavirus epitope. Vaccine. 2007;25(August (32)):6070–6077. doi: 10.1016/j.vaccine.2007.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bai B., Lu X., Meng J., Hu Q., Mao P., Lu B. Vaccination of mice with recombinant baculovirus expressing spike or nucleocapsid protein of SARS-like coronavirus generates humoral and cellular immune responses. Mol Immunol. 2008;45(February (4)):868–875. doi: 10.1016/j.molimm.2007.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liniger M., Zuniga A., Tamin A., Azzouz-Morin T.N., Knuchel M., Marty R.R. Induction of neutralising antibodies and cellular immune responses against SARS coronavirus by recombinant measles viruses. Vaccine. 2008;26(April (17)):2164–2174. doi: 10.1016/j.vaccine.2008.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gao W., Tamin A., Soloff A., D’Aiuto L., Nwanegbo E., Robbins P.D. Effects of a SARS-associated coronavirus vaccine in monkeys. Lancet. 2003;362(December (9399)):1895–1896. doi: 10.1016/S0140-6736(03)14962-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu S.J., Leng C.H., Lien S.P., Chi H.Y., Huang C.Y., Lin C.L. Immunological characterizations of the nucleocapsid protein based SARS vaccine candidates. Vaccine. 2006;24(April (16)):3100–3108. doi: 10.1016/j.vaccine.2006.01.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peng H., Yang L.T., Wang L.Y., Li J., Huang J., Lu Z.Q. Long-lived memory T lymphocyte responses against SARS coronavirus nucleocapsid protein in SARS-recovered patients. Virology. 2006;351(August (2)):466–475. doi: 10.1016/j.virol.2006.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao J., Huang Q., Wang W., Zhang Y., Lv P., Gao X.M. Identification and characterization of dominant helper T-cell epitopes in the nucleocapsid protein of severe acute respiratory syndrome coronavirus. J Virol. 2007;81(June (11)):6079–6088. doi: 10.1128/JVI.02568-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang Y., Li J., Zhan Y., Wu L., Yu X., Zhang W. Analysis of serum cytokines in patients with severe acute respiratory syndrome. Infect Immun. 2004;72(August (8)):4410–4415. doi: 10.1128/IAI.72.8.4410-4415.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chien J.Y., Hsueh P.R., Cheng W.C., Yu C.J., Yang P.C. Temporal changes in cytokine/chemokine profiles and pulmonary involvement in severe acute respiratory syndrome. Respirology. 2006;11(November (6)):715–722. doi: 10.1111/j.1440-1843.2006.00942.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheung C.Y., Poon L.L., Ng I.H., Luk W., Sia S.F., Wu M.H. Cytokine responses in severe acute respiratory syndrome coronavirus-infected macrophages in vitro: possible relevance to pathogenesis. J Virol. 2005;79(June (12)):7819–7826. doi: 10.1128/JVI.79.12.7819-7826.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li C.K., Wu H., Yan H., Ma S., Wang L., Zhang M. T cell responses to whole SARS coronavirus in humans. J Immunol. 2008;181(October (8)):5490–5500. doi: 10.4049/jimmunol.181.8.5490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wong C.K., Lam C.W., Wu A.K., Ip W.K., Lee N.L., Chan I.H. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136(April (1)):95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yasui F., Kai C., Kitabatake M., Inoue S., Yoneda M., Yokochi S. Prior immunization with severe acute respiratory syndrome (SARS)-associated coronavirus (SARS-CoV) nucleocapsid protein causes severe pneumonia in mice infected with SARS-CoV. J Immunol. 2008;181(November (9)):6337–6348. doi: 10.4049/jimmunol.181.9.6337. [DOI] [PubMed] [Google Scholar]
- 37.Zhang X., Wu K., Wang D., Yue X., Song D., Zhu Y. Nucleocapsid protein of SARS-CoV activates interleukin-6 expression through cellular transcription factor NF-kappaB. Virology. 2007;365(September (2)):324–335. doi: 10.1016/j.virol.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheng M., Chan C.W., Cheung R.C., Bikkavilli R.K., Zhao Q., Au S.W. Cross-reactivity of antibody against SARS-coronavirus nucleocapsid protein with IL-11. Biochem Biophys Res Commun. 2005;338(December (3)):1654–1660. doi: 10.1016/j.bbrc.2005.10.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maliga P., Graham I. Molecular farming and metabolic engineering promise a new generation of high-tech crops. Curr Opin Plant Biol. 2004;7(April (2)):149–151. doi: 10.1016/j.pbi.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 40.Kapila J., de Rycke R., van Montagu M., Angenon G. An Agrobacterium-mediated transient gene expression system for intact leaves. Plant Sci. 1997;122:101–108. [Google Scholar]
- 41.Johansen L.K., Carrington J.C. Silencing on the spot. Induction and suppression of RNA silencing in the Agrobacterium-mediated transient expression system. Plant Physiol. 2001;126(July (3)):930–938. doi: 10.1104/pp.126.3.930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chellappan P., Vanitharani R., Fauquet C.M. MicroRNA-binding viral protein interferes with Arabidopsis development. Proc Natl Acad Sci USA. 2005;102(July (29)):10381–10386. doi: 10.1073/pnas.0504439102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anandalakshmi R., Pruss G.J., Ge X., Marathe R., Mallory A.C., Smith T.H. A viral suppressor of gene silencing in plants. Proc Natl Acad Sci USA. 1998;95(October (22)):13079–13084. doi: 10.1073/pnas.95.22.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brigneti G., Voinnet O., Li W.X., Ji L.H., Ding S.W., Baulcombe D.C. Viral pathogenicity determinants are suppressors of transgene silencing in Nicotiana benthamiana. Embo J. 1998;17(November (22)):6739–6746. doi: 10.1093/emboj/17.22.6739. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 45.Voinnet O., Rivas S., Mestre P., Baulcombe D. An enhanced transient expression system in plants based on suppression of gene silencing by the p19 protein of tomato bushy stunt virus. Plant J. 2003;33(March (5)):949–956. doi: 10.1046/j.1365-313x.2003.01676.x. [DOI] [PubMed] [Google Scholar]
- 46.Scholthof H.B. The Tombusvirus-encoded P19: from irrelevance to elegance. Nat Rev Microbiol. 2006;4(May (5)):405–411. doi: 10.1038/nrmicro1395. [DOI] [PubMed] [Google Scholar]
- 47.Streatfield S.J. Oral hepatitis B vaccine candidates produced and delivered in plant material. Immunol Cell Biol. 2005;83(June (3)):257–262. doi: 10.1111/j.1440-1711.2005.01335.x. [DOI] [PubMed] [Google Scholar]
- 48.Zhou J.Y., Wu J.X., Cheng L.Q., Zheng X.J., Gong H., Shang S.B. Expression of immunogenic S1 glycoprotein of infectious bronchitis virus in transgenic potatoes. J Virol. 2003;77(August (16)):9090–9093. doi: 10.1128/JVI.77.16.9090-9093.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li H.Y., Ramalingam S., Chye M.L. Accumulation of recombinant SARS-CoV spike protein in plant cytosol and chloroplasts indicate potential for development of plant-derived oral vaccines. Exp Biol Med (Maywood) 2006;231(September (8)):1346–1352. doi: 10.1177/153537020623100808. [DOI] [PubMed] [Google Scholar]
- 50.Pogrebnyak N., Golovkin M., Andrianov V., Spitsin S., Smirnov Y., Egolf R. Severe acute respiratory syndrome (SARS) S protein production in plants: development of recombinant vaccine. Proc Natl Acad Sci USA. 2005;102(June (25)):9062–9067. doi: 10.1073/pnas.0503760102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yoo H.R., Kwon B.E., Jang Y.S., Youn H.K. Validity and reliability of an instrument for predictive nursing intention for SARS patient care. Taehan Kanho Hakhoe Chi. 2005;35(October (6)):1063–1071. doi: 10.4040/jkan.2005.35.6.1063. [DOI] [PubMed] [Google Scholar]
- 52.Zheng N., Perez J.D., Zhang Z., Dominguez E., Garcia J.A., Xie Q. Specific and efficient cleavage of fusion proteins by recombinant plum pox virus NIa protease. Protein Expr Purif. 2008;57(February (2)):153–162. doi: 10.1016/j.pep.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Valli A., Martin-Hernandez A.M., Lopez-Moya J.J., Garcia J.A. RNA silencing suppression by a second copy of the P1 serine protease of Cucumber vein yellowing ipomovirus, a member of the family Potyviridae that lacks the cysteine protease HCPro. J Virol. 2006;80(October (20)):10055–10063. doi: 10.1128/JVI.00985-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alvarez M.L., Pinyerd H.L., Crisantes J.D., Rigano M.M., Pinkhasov J., Walmsley A.M. Plant-made subunit vaccine against pneumonic and bubonic plague is orally immunogenic in mice. Vaccine. 2006;24(March (14)):2477–2490. doi: 10.1016/j.vaccine.2005.12.057. [DOI] [PubMed] [Google Scholar]
- 55.Azizi A., Aucoin S., Tadesse H., Frost R., Ghorbani M., Soare C. A combined nucleocapsid vaccine induces vigorous SARS-CD8+ T-cell immune responses. Genet Vaccines Ther. 2005;August (3):7. doi: 10.1186/1479-0556-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shin G.C., Chung Y.S., Kim I.S., Cho H.W., Kang C. Antigenic characterization of severe acute respiratory syndrome-coronavirus nucleocapsid protein expressed in insect cells: The effect of phosphorylation on immunoreactivity and specificity. Virus Res. 2007;127(July (1)):71–80. doi: 10.1016/j.virusres.2007.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Deming D., Sheahan T., Heise M., Yount B., Davis N., Sims A. Vaccine efficacy in senescent mice challenged with recombinant SARS-CoV bearing epidemic and zoonotic spike variants. PLoS Med. 2006;3(December (12)):e525. doi: 10.1371/journal.pmed.0030525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhu Y.G., Qu J.M. Differential characteristics of the early stage of lung inflammation induced by SARS-CoV Nucleocapsid protein related to age in the mouse. Inflamm Res. 2009;(February) doi: 10.1007/s00011-009-8062-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Huang K.J., Su I.J., Theron M., Wu Y.C., Lai S.K., Liu C.C. An interferon-gamma-related cytokine storm in SARS patients. J Med Virol. 2005;75(February (2)):185–194. doi: 10.1002/jmv.20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jones B.M., Ma E.S., Peiris J.S., Wong P.C., Ho J.C., Lam B. Prolonged disturbances of in vitro cytokine production in patients with severe acute respiratory syndrome (SARS) treated with ribavirin and steroids. Clin Exp Immunol. 2004;135(March (3)):467–473. doi: 10.1111/j.1365-2249.2003.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang X., Wu K., Wang D., Yue X., Song D., Zhu Y. Nucleocapsid protein of SARS-CoV activates interleukin-6 expression through cellular transcription factor NF-kappaB. Virology. 2007;(May) doi: 10.1016/j.virol.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roncarolo M.G., Gregori S., Battaglia M., Bacchetta R., Fleischhauer K., Levings M.K. Interleukin-10-secreting type 1 regulatory T cells in rodents and humans. Immunol Rev. 2006;212(August):28–50. doi: 10.1111/j.0105-2896.2006.00420.x. [DOI] [PubMed] [Google Scholar]
- 63.Hao D., He L.X., Qu J.M., Pan J., Hu B.J., Zhang J. A study of pulmonary inflammatory reaction induced by N-protein of SARS-CoV in rat models and effects of glucocorticoids on it. Zhonghua Nei Ke Za Zhi. 2005;44(December (12)):890–893. [PubMed] [Google Scholar]


