Abstract
In this study, we were interested in determining if high titered egg adapted modified live infectious bronchitis virus (IBV) vaccines contain spike gene related quasispecies that undergo selection in chickens, following vaccination. We sequenced the spike glycoprotein of 12 IBV vaccines (5 different serotypes from 3 different manufacturers) directly from the vaccine vial, then compared that sequence with reisolated viruses from vaccinated and contact-exposed birds over time. We found differences in the S1 sequence within the same vaccine serotype from different manufacturers, differences in S1 sequence between different vaccine serials from the same manufacturer, and intra-vaccine differences or quasispecies. Comparing the sequence data of the reisolated viruses with the original vaccine virus, we were able to identify in vivo selection of viral subpopulations as well as mutations. To our knowledge, this is the first report showing selection of a more fit virus subpopulation as well as mutations associated with replication of modified live IBV vaccine viruses in chickens. This information is important for our understanding of how attenuated virus vaccines, including potential vaccines against the SARS-CoV, can ensure long-term survival of the virus and can lead to changes in pathogenesis and emergence of new viral pathogens. This information is also valuable for the development of safer modified live coronavirus vaccines.
Keywords: Coronavirus, Avian infectious bronchitis virus, Vaccine virus adaptation, Selection, Mutation, Molecular typing, Spike gene sequence, Serotype, Quasispecies
Introduction
Coronaviruses are an important group of enveloped single stranded RNA viruses that cause highly contagious respiratory and enteric diseases in a variety of animals and in humans. Coronaviruses belong to the order Nidovirales, family Coronaviridae, and are separated into 3 groups based on genetic and antigenic characteristics [1]. Avian infectious bronchitis virus (IBV) belongs to the group 3 coronaviruses along with the other avian coronaviruses, whereas coronaviruses in groups 1 and 2 produce disease in many species of mammals and in humans. Confusion around the origin of severe acute respiratory syndrome coronavirus (SARS-CoV) has lead to a proposed group 4; however, genetic studies suggest that SARS-CoV diverged from the group 2 viruses, thus a group 2b classification was suggested [2].
Avian infectious bronchitis virus has an enormous economic impact on commercial poultry causing highly contagious disease in chickens of all ages. Since IBV was first described by Schalk and Hawn in the 1930s, reviewed in ref. [3], many serotypes have been identified worldwide. There are currently 4 reported structural proteins associated with the IBV virion; nucleocapsid, membrane, small membrane and spike. The spike glycoprotein on the outside of the virus contains epitopes associated with serotype differences and binding of neutralizing antibodies, and it plays a role in attachment and entry into the host cell.
Coronaviruses including IBV have been shown to exist as a mixture of genetic mutants within an isolate [4], [5]. These so called quasispecies are generated through genetic mutations and recombination events that occur when the viral RNA-dependent RNA-polymerase, which lacks proofreading capabilities, replicates the viral genome [6]. For SARS-CoV, non-synonymous and synonymous substitution rates have been estimated to be as high as 3.3 × 10−3 and 4.67 × 10−3 per site per year, respectively [7]. Evolutionary and mutation rates for IBV in the face of vaccination were determined to be 2.5 and 1.5% per year, respectively, in the hypervariable region of the spike glycoprotein; however, in the absence of vaccines, IBV lineages appear to evolve at a much slower rate (0.3%) [8]. The group 3 coronaviruses, which exist only in avian species were found to have a relatively recent divergence date (1925) and exponential population growth [2]. In general, constant population size is associated with natural reservoirs of the virus, which remain largely asymptomatic in the host, whereas a change from constant to exponential population growth indicates emergence of a relatively new virus associated with interspecies transmission and disease [2].
An actively changing genetic population allows rapid adaptation to the host through selection of the most fit viral subpopulation. Selection ensures long-term survival of the virus at the cell, organism, and host population level, and can lead to changes in pathogenesis and emergence of new viral pathogens [9]. For economic reasons, vaccine manufacturers attempt to produce high titered (>1 × 108 embryo infectious dose50 (EID50)/ml) IBV vaccines so they can be packaged in 5000 or even 10,000 dose vials. The average IBV vaccine dose can vary but is generally approximately 1 × 104 EID50. Since the number of intra-isolate genome subpopulations are reported to increase dramatically when the virus titer increases [9], we were interested in determining if quasispecies of high titered modified live IBV vaccines contain specific spike gene mutations that undergo selection in chickens, following vaccination. In addition, we wanted to determine if molecular changes were solely the result of selection or if mutations also occur following vaccination.
To study the dynamics of IBV vaccine genetic adaptation to the host, we sequenced the spike glycoprotein of 12 IBV vaccines (5 different serotypes from 3 different manufacturers) directly from the vaccine vial. Then, we vaccinated chickens with those viruses and examined the spike glycoprotein sequence of the vaccines reisolated from vaccinated and from contact-exposed birds over time. Comparing the sequence data of the reisolated viruses with the original vaccine virus, we were able to access in vivo selection of subpopulations and genetic mutations.
Materials and methods
Vaccines
Twelve IBV commercial vaccines were obtained from three different manufacturers designated A, B and C herein, and had a titer of at least 1 × 108 EID50/ml. The vaccines used in this study from manufacturer A were Ark-DPI (Ark/A), GA98 (GA/A) and Mass (Mass/A). Vaccines from manufacturer B were Ark-DPI (Ark/B), Mass (Mass/B) and a mixture of Mass and Conn (Conn/B). The vaccines from manufacturer C were Ark-DPI (Ark/C), DE072 (Del/C), GA98 (GA/C), Mass (Mass/C), a mixture of Mass and Conn (Conn/C), and MassD (MassD/C). The lyopholyzed vaccines were resuspended in 10 ml of diethylpyrocarbonate (DEPC) treated water. The DE072 vaccine, stored in liquid nitrogen, was thawed and diluted using 1 ml of DEPC treated water.
Birds and housing
Specific-pathogen-free (SPF) white leghorn chicks (Merial, Gainesville, GA) were housed in positive-pressure Horsfal isolation units. Feed and water were provided ad libitum, and the birds were examined twice daily.
Experimental design
To guard against potential cross-contamination, the 12 vaccines were assigned to 4 different groups ensuring that there were no vaccines of the same serotype in each group. Two different experiments were conducted with vaccine groups 1 and 2 in the first experiment and vaccine groups 3 and 4 in the second experiment. Vaccines used in experiment 1 were for group 1 Del/C, GA/C, Mass/A, and for group 2 Ark/C, GA/A, and Mass/C. Vaccines used in experiment 2 were for group 3 Ark/B, Conn/B, Mass/B, and for group 4 Ark/A, Conn/C, and MassD/C. Each vaccine group was tested in a separate filtered air positive pressure room containing the isolators. One-week old chicks were randomly divided into groups of 10 birds for each vaccine type. Five birds in each group were inoculated by eye-drop with 30 μl of vaccine (equal to one dose, according to the manufacturers recommendation), the other 5 birds served as contact-exposed birds. A negative control group of 5 birds was included for each group of vaccines tested.
Tracheal swabs from all birds were collected at 3, 6 and 9 days post-vaccination (dpv), and at necropsy. Birds in experiment 1 were necropsied at 14 dpv while birds in experiment 2 were necropsied at 13 dpv. Swabs from 5 vaccinated birds and 5 contact-exposed birds for each of the vaccine types were pooled separately in 1 ml PBS (pH 7.4). The swabs were stored at −80 °C until they were analyzed for IBV RNA by RT-PCR.
Passage in embryonating eggs
The last positive tracheal swab by RT-PCR from each vaccinated and contact-exposed group of birds was passaged a maximum of ten times in 9–11 day old specific pathogen free (SPF) embryonating eggs. Three eggs per group were inoculated with 0.1 ml of PBS from the tracheal swabs into the chorioallantoic sac (CAS) as described [10]. The eggs were incubated at 37 °C and allantoic fluid was harvested from all eggs with live embryos at 48 h post-inoculation, pooled and kept at −80 °C. Subsequent passage was done by inoculating 0.2 ml of allantoic fluid from the previous passage into the CAS of 9–11 day old embryonating eggs and the allantoic fluid was harvested at 48 h post-inoculation as above.
Viral RNA extraction
Viral RNA was extracted from allantoic fluid, rehydrated or diluted vaccine, and tracheal swabs using the High Pure RNA Isolation Kit (Roche Diagnostics, Indianapolis, IN) according to manufacturer's protocol.
RT-PCR amplification and cloning of the S1 gene
Reverse transcriptase-polymerase chain reaction was carried out using the Titan One Tube RT-PCR kit (Roche Diagnostics, Indianapolis, IN) according to manufacturer's protocol with primers NEWS1OLIGO5′ [11] and Degenerate3′ [12]. Primers specific for the Conn serotype [13] were used to screen for the presence of that virus in swabs collected from birds vaccinated with vaccine containing both the Mass and Conn types and in swabs from the corresponding contact birds. The PCR products were agarose gel purified using the QIAquick gel extraction kit (Qiagen, Valencia, CA) according to the manufacturer's protocol. To aid in sequence analysis, purified PCR products from Conn/B and Conn/C, which were mixtures of Mass and Conn vaccines, and Ark/B were cloned into the TOPOXL vector using TOPOXL cloning kit (Invitrogen, Carlsbad, CA) according to manufacturer's protocol. The IBV real-time RT-PCR analysis on tracheal swabs was performed as previously described [4], [14].
Sequencing and sequence analysis of the S1 gene
Viral S1 gene sequence was determined for two different production lots for each IBV vaccine examined. The S1 gene of reisolated viruses from the first and last RT-PCR positive tracheal swabs only was also sequenced for both vaccinated and contact-exposed birds. The S1 gene of reisolated virus from Ark/A vaccinated birds was only positive by real time RT-PCR. The pooled tracheal swabs collected from the 13 dpv vaccinated birds were sequenced. In addition, each embryo passaged virus was sequenced to determine if genetic changes in the reisolated vaccine viruses would revert to the original vaccine sequence. Purified RT-PCR products or at least 4 cloned RT-PCR products for each virus were sequenced using the BigDye® Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems, Foster City, CA) according to manufacturer's protocol. Sequencing reactions were purified using Centri-Sep Columns (Princeton Separations, Inc, Adelphia, NJ) or with the Performa DTR Ultra Dye Terminator removal system (Edge BioSystems, Gaithersburg, MD). Sequence reactions were examined at the Molecular Genetics Instrumentation Facility (University of Georgia, Athens, GA).
The S1 sequences from each virus were compiled using the EditSeq and MegAlign program (DNASTAR, Inc. Madison, WI) and open reading frames were predicted using ORF finder at National Center for Biotechnology Information (NCBI, http://www.ncbi.nlm.nih.gov/gorf/gorf.html). The BlastX program (http://www.ncbi.nlm.nih.gov/BLAST/) was used to search GenBank (National Center for Biotechnology Information, http://www.ncbi.nlm.nih.gov/) for homologous IBV S1 sequences.
Results
S1 sequence analysis of vaccine viruses
All nucleotide sequences reported herein have been submitted to NCBI, GenBank (http://www.ncbi.nlm.nih.gov/) and the accession numbers are listed in Table 1 . To determine if mutations or selection of a more fit virus subpopulation was responsible for the changes observed when IBV adapts to an in vivo environment, we first needed to establish the exact sequence of the vaccine viruses directly from the manufacturer. The S1 gene deduced amino acid sequence for different production lots of the Ark/A and Ark/C vaccine viruses were the same, whereas Ark/B vaccine production lots had 1 amino acid difference (Pro524Ser) in the S1 gene. In addition, sequence differences were observed between Arkansas vaccines from the different manufacturers (Table 2 ).
Table 1.
NCBIa accession numbers for IBV S1 gene sequences obtained directly from virus in vaccine vials, and reisolated vaccine virus from vaccinated and contact-exposed birds
| IBV vaccine virus | S1 sequence source | NCBI accession number |
|---|---|---|
| Ark/A | First vaccine lot | EU283045 |
| Second vaccine lot | EU283046 | |
| 13 dpvb vaccinated birds | EU283047 | |
| Ark/B | First vaccine lot | EU283048 |
| Second vaccine lot | EU283049 | |
| 3 dpv vaccinated | EU283050 | |
| 9 dpv vaccinated | EU283051 | |
| 6 dpv contact birds | EU283052 | |
| 13 dpv contact birds | EU283053 | |
| Ark/C | First vaccine lot | EU283054 |
| Second vaccine lot | EU283055 | |
| 6 dpv vaccinated birds | EU283056 | |
| Conn/B | First vaccine lot | EU283057 |
| Second vaccine lot | EU283058 | |
| 6 dpv contact birds | EU283059 | |
| 13 dpv contact birds | EU283060 | |
| Conn/C | First vaccine lot | EU283061 |
| Second vaccine lot | EU283062 | |
| Del/C | First vaccine lot | EU283063 |
| Second vaccine lot | EU283064 | |
| Reisolated vaccine virusc | EU283065 | |
| GA/A | First vaccine lot | EU283066 |
| Second vaccine lot | EU283067 | |
| 3 dpv vaccinated birds | EU283068 | |
| 9 dpv vaccinated birds | EU283069 | |
| GA/C | First vaccine lot | EU283070 |
| Second vaccine lot | EU283071 | |
| Reisolated vaccine virus | EU283072 | |
| Mass/A | First vaccine lot | EU283073 |
| Second vaccine lot | EU283074 | |
| Reisolated vaccine virus | EU283075 | |
| Mass/B | First vaccine lot | EU283076 |
| Second vaccine lot | EU283077 | |
| 3 dpv vaccinated | EU283078 | |
| 9 dpv vaccinated | EU283079 | |
| 6 dpv contact birds | EU283080 | |
| 13 dpv contact birds | EU283081 | |
| Mass/C | First vaccine lot | EU283082 |
| Second vaccine lot | EU283083 | |
| Reisolated vaccine virus | EU283084 | |
| MassD/C | First vaccine lot | EU283085 |
| Second vaccine lot | EU283086 | |
| 3 dpv vaccinated birds | EU283087 | |
| 6 dpv contact birds | EU283088 | |
NCBI = National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov/).
dpv = day post-vaccination.
Reisolated vaccine virus indicates that all viruses reisolated from vaccinated and contact-exposed birds had the same sequence.
Table 2.
Pairwise comparisons of amino acids between Ark vaccines from different manufacturers
| Residue position | Ark/A | Ark/B | Ark/C |
|---|---|---|---|
| 43 | Tyr | His | Tyr |
| 171 | Tyr | His | Tyr |
| 213 | Ser | Ala | Ser |
| 249 | Phe | Ser | Phe |
| 323 | Arg | Arg | Tyr |
| 410 | Lys | Glu | Lys |
| 524 | Ser | Pro (Ser)a | Ser |
Amino acid in brackets indicates the residue observed in vaccine vial 2.
There were 26 amino acid differences in the S1 sequences between the two production lots for the Conn/B vaccine (Table 3 ). For the Conn/C vaccine, we observed 5 amino acid differences between the different production lots. In addition, one of the Conn/C vaccine production lots had a deletion of amino acid Asn at position 58.
Table 3.
Pairwise comparisons of amino acids between Conn vaccines from different manufacturers
| Residue position | Conn/B vial 1 | Conn/B vial 2 | Conn/C vial 1 | Conn/C vial 2 |
|---|---|---|---|---|
| 10 | Ala | Thr | Thr | Thr |
| 58 | Asn | Asn | Asn | Deleted |
| 74 | Ser | Asn | Asn | Asn |
| 81 | Thr | Ser | Thr | Thr |
| 88 | Asp | Asp | Gly | Asp |
| 114 | His | His | Tyr | His |
| 161 | Leu | Phe | Phe | Phe |
| 188 | Lys | Asn | Asn | Asn |
| 214 | Asp | Asn | Asp | Asp |
| 243 | Ile | Thr | Thr | Thr |
| 260 | Val | Ile | Ile | Ile |
| 264 | Phe | Leu | Leu | Leu |
| 265 | Thr | Lys | Lys | Lys |
| 268 | Tyr | Asn | Asn | Asn |
| 270 | Ser | Thr | Thr | Thr |
| 281 | Pro | Leu | Leu | Leu |
| 309 | Ser | Gly | Gly | Gly |
| 330 | Leu | Pro | Pro | Pro |
| 331 | Glu | Lys | Glu | Glu |
| 343 | Ser | Leu | Ser | Ser |
| 373 | Glu | Gly | Gly | Gly |
| 376 | Leu | Ser | Ser | Ser |
| 381 | Val | Val | Ile | Val |
| 383 | Ser | Leu | Leu | Leu |
| 387 | Asp | Lys | Lys | Lys |
| 388 | His | Ser | Ser | Ser |
| 389 | Asn | Asp | Asp | Asp |
| 402 | Gly | Asp | Asp | Asp |
| 406 | Ile | Ile | Thr | Thr |
| 430 | Asp | Asp | Gly | Asp |
| 460 | Leu | Met | Met | Met |
| 478 | Tyr | Tyr | Cys | Tyr |
| 481 | Asn | Thr | Thr | Thr |
There were no differences observed between the S1 sequences obtained from the two vaccine production lots for the Del/C, GA/A, GA/C, Mass/A, Mass/B, and Mass/C. There were 13 amino acid sequence differences between the two production lots of the MassD/C vaccine virus (Table 4 ). MassD/C vial 1 was closest to Mass/A with only 1 amino acid sequence difference between them, whereas MassD/C vial 2 was closest to Mass/C and Mass/B with 6 and 7 amino acid sequence differences, respectively. In addition, there were differences in the amino acid sequences between the Mass vaccines from the different manufacturers. We observed 14 and 11 amino acid sequence differences between Mass vaccines from manufacturer A and the Mass vaccines from manufacturers B and C, respectively. We also found 2 amino acid sequence differences between Mass vaccines from manufacturers B and C. Finally, there were 28 amino acid sequence differences and one deletion between the GA vaccines from manufacturers A and C (Table 5 ).
Table 4.
Pairwise comparisons of amino acids between Mass vaccines from different manufacturers
| Residue position | Mass/A | Mass/B | Mass/C | MassD/C vial 1 | MassD/C vial 2 |
|---|---|---|---|---|---|
| 19 | Ala | Val | Val | Ala | Ala |
| 38 | Asp | Asn | Asn | Asp | Asn |
| 64 | Gly | Glu | Gly | Gly | Gly |
| 69 | Ile | Thr | Thr | Ile | Thr |
| 73 | Gly | Asp | Gly | Gly | Gly |
| 75 | Val | Val | Val | Val | Ala |
| 76 | Val | Val | Val | Val | Ala |
| 101 | Tyr | His | His | Tyr | His |
| 109 | Val | Val | Val | Val | Glu |
| 130 | Ser | Phe | Phe | Ser | Phe |
| 179 | Ala | Glu | Ala | Glu | Glu |
| 205 | Arg | Lys | Lys | Arg | Lys |
| 246 | Thr | Ile | Ile | Thr | Ile |
| 271 | Asn | Tyr | Tyr | Asn | Tyr |
| 273 | Thr | Ser | Ser | Thr | Arg |
| 376 | Gly | Glu | Glu | Gly | Glu |
| 479 | Ser | Gly | Gly | Ser | Gly |
Table 5.
Pairwise comparisons of amino acids between GA vaccines from different manufacturers
| Residue position | GA/A | GA/C |
|---|---|---|
| 3 | Gly | Val |
| 32 | Arg | Gly |
| 58 | Asp | Ser |
| 60 | Glu | Asp |
| 68 | Gly | Asp |
| 84 | Gly | Arg |
| 86 | Arg | Ser |
| 90 | Gln | Lys |
| 112 | Thr | Ser |
| 122 | Lys | Gln |
| 141 | Ile | Arg |
| 144 | Asn | Asp |
| 163 | Asn | Ser |
| 197 | Val | Ser |
| 198 | Met | Tyr |
| 199 | Arg | Ala |
| 200 | Asp | Arg |
| 201 | Thr | Ser |
| 257 | His | Asp |
| 282 | Glu | Asn |
| 283 | His | Gln |
| 330 | Gly | Arg |
| 389 | Asp | Glu |
| 390 | Val | Phe |
| 391 | Asn | Asp |
| 409 | Arg | Ile |
| 423 | Ile | Deletion |
| 479 | Lys | Asn |
| 481 | Thr | Ile |
Virus detection from vaccinated and contact-exposed birds
Tracheal swabs collected from vaccinated and contact-exposed birds were tested for IBV by RT-PCR and real-time RT-PCR and the results are presented in Table 6 . Tracheal swabs collected from all the negative control birds were negative for IBV by RT-PCR and real-time RT-PCR. Based on sequence data from reisolated viruses, there was no cross-contamination detected between the vaccines. The tracheal swabs from Ark/B, Ark/C, Mass/B, Mass/C, and MassD/C vaccinated birds were positive for IBV at all sampling times. The tracheal swabs from Del/C, GA/C, GA/A, and Mass/A vaccinated birds were positive on days 3, 6, and 9 dpv but not at necropsy (14 dpv Expt. 1 or 13 dpv Expt. 2). Tracheal swabs for all of the contact-exposed birds in groups Ark/B, Conn/B, Mass/A, and Mass/B were positive for IBV at all sampling times. Swabs from Del/C, GA/A, Mass/C, and MassD/C contact-exposed birds were positive for IBV by RT-PCR or real time RT-PCR except at 3 dpv. Tracheal swabs from Ark/C contact-exposed birds were negative at 3, 6, and 9 dpv but positive at necropsy (14 dpv Expt. 1 or 13 dpv Expt. 2). Using RT-PCR analysis, tracheal swabs collected from Ark/A vaccinated and contact-exposed birds were negative for IBV. However, real-time RT-PCR analysis, which is more sensitive than RT-PCR, showed that the swabs from Ark/A vaccinated birds but not contact-exposed birds were positive for virus.
Table 6.
RT-PCR and real time RT-PCR analysis of vaccine viruses reisolated from the trachea of vaccinated and contact-exposed birds at 3, 6, 9, 13 or 14 days post-vaccination
| Vaccinesa | 3 dpvb Tracheal swab |
6 dpv Tracheal swab |
9 dpv Tracheal swab |
13 or 14 dpv Tracheal swab |
||||
|---|---|---|---|---|---|---|---|---|
| Vaccinated | Contact | Vaccinated | Contact | Vaccinated | Contact | Vaccinated | Contact | |
| Ark/A | −/+c | −d | −/+ | − | −/+ | − | −/+ | − |
| Ark/B | + | −/+ | + | + | + | + | −/+ | + |
| Ark/C | −/+ | − | + | − | −/+ | − | −/+ | −/+ |
| Conn/B | + | −/+ | − | + | − | + | − | + |
| Conn/C | − | − | − | − | − | − | − | − |
| Del/C | + | − | + | + | + | + | − | −/+ |
| GA/A | + | − | −/+ | −/+ | + | −/+ | − | −/+ |
| GA/C | + | + | −/+ | + | −/+ | + | − | − |
| Mass/A | −/+ | + | + | + | + | + | − | −/+ |
| Mass/B | + | −/+ | + | + | + | + | −/+ | + |
| Mass/C | + | − | + | −/+ | + | + | −/+ | −/+ |
| MassD/C | + | − | + | + | + | + | + | + |
All samples from negative groups were negative.
dpv = days post-vaccination.
(−/+) Samples negative by RT-PCR/and positive by real time RT-PCR.
(−) Samples negative by RT-PCR and by real time RT-PCR.
The Conn/B vaccine virus was only reisolated from the swab taken at 3 dpv, from vaccinated birds while the virus was reisolated from all four sampling times from the contact-exposed birds (Table 6). From the birds that were vaccinated with Conn/C vaccine, which also contains the Mass virus, we detected IBV by RT-PCR, but Conn specific primers failed to amplify the Conn virus indicating that the viruses detected in the vaccinated and contact-exposed birds were not Conn virus (data not shown). Sequence analysis confirmed that only the Mass virus was reisolated.
S1 sequence analysis of reisolated vaccine viruses
The S1 amino acid sequences from the reisolated viruses were compared to the sequence from the same vaccine virus that was used for vaccination. Analysis of the virus reisolated from Del/C, GA/C, Mass/A and Mass/C vaccinated and contact-exposed birds showed that the S1 gene amino acid sequence did not change after the virus replicated in birds.
The S1 amino acid sequence analysis of vaccine viruses reisolated from Ark vaccinated and contact birds showed a consistent amino acid change of Tyr326 to Asn326 and a deletion of Asn345 (Table 7 ) in the vaccine virus obtained from all three manufacturers. Analysis of the original vaccine sequences revealed minor nucleotide peaks in otherwise clean sequence at Tyr326Asn, as shown in Fig. 1 as well as for Tyr43His and Ser213Ala, indicating multiple RNA species in the Ark/A and Ark/C vaccines. The deletion at amino acid residue 345 was not detected in the original vaccines. In addition, amino acid changes Ser130Gly (Ark/A and Ark/C) and Thr323Arg (Ark/C) detected in the reisolated vaccine viruses appeared to result from in vivo mutations since minor peaks were not detected in the original vaccine sequences, although selection cannot be excluded.
Table 7.
Sequence of reisolated vaccine viruses that showed S1 gene sequence differences from the original vaccine sequence
| Vaccine | Nucleotide position | Nucleotide change | Amino acid change | Amino acid deletion |
|---|---|---|---|---|
| Ark/Aa | 127† | T → C | Tyr43His | |
| 388† | A → G | Ser130Gly | ||
| 637† | T → G | Ser213Ala | ||
| 976† | T → A | Tyr326Asn | ||
| 1033–1035† | AAT deletion | Asn345 | ||
| Ark/Bb | 976†,‡ | T → A | Tyr326Asn | |
| 1033–1035†,‡ | AAT deletion | Asn345 | ||
| Ark/Cc | 127† | T → C | Tyr43His | |
| 388† | A → G | Ser130Gly | ||
| 637† | T → G | Ser213Ala | ||
| 968† | C → G | Thr323Arg | ||
| 976† | T → A | Tyr326Asn | ||
| 1033–1035† | AAT deletion | Asn345 | ||
| Conn/Bd | 172–174‡ | AAT deletion | Asn58 | |
| 238‡ | T → A | No | ||
| 241† | T → A | No | ||
| 1033‡ | T → C | Ser345Pro | ||
| GA/Ae | 662† | G → T | Ser221Thr | |
| 988† | G → A | Gly330Arg | ||
| 1152† | C → T | No | ||
| 1438† | G → T | Lys479Asn | ||
| Mass/Bf | 191†,‡ | A → G | Glu64Gly | |
| 313‡ | T → C | Ser105Pro | ||
| 1469‡ | C → T | Pro490Leu | ||
Virus isolated at 13 days post-vaccination (dpv).
Virus isolated from vaccinated birds at 9 dpv and from contact birds at 13 dpv.
Virus isolated at 6 dpv.
Virus isolated from vaccinated birds at 3 dpv and from contact birds at 6 and 13 dpv.
Virus isolated at 3 and 9 dpv.
Virus isolated from vaccinated birds at 3 and 9 dpv and from contact birds at 6 and 13 dpv.
Vaccinated birds.
Contact birds.
Figure 1.
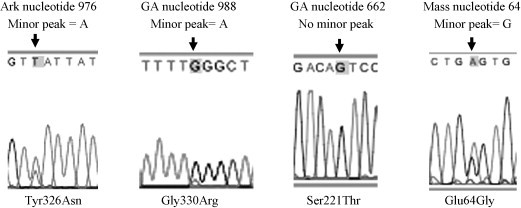
Chromatograms of vaccine viruses showing major and minor peaks (Tyr326Asn, Gly330Arg, and Glu64Gly) indicating subpopulation selection associated with the reisolated vaccine viruses, and a single peak (Ser221Thr) indicating a mutation was associated with the reisolated vaccine virus.
The S1 amino acid sequence for the virus reisolated from Conn/B vaccinated birds had no changes when compared to the virus in the vaccine vial. The Conn/B virus obtained from contact-exposed birds had an amino acid change of Ser345Pro, a deletion of Asn58 as well as two synonymous nucleotide changes (Table 7). Only one change, Ser345Pro in Conn/B appeared to result from in vivo mutations since no minor peaks were observed in the sequence chromatogram.
The GA/A vaccinated birds had four nucleotide changes that resulted in three amino acid changes, Ser221Thr as shown in Fig. 1, as well as Gly330Arg and Lys479Asn. The Gly330Arg change resulted from selection of a subpopulation since a minor A peak was observed in the chromatogram (Fig. 1), whereas the other changes appear to be the result of in vivo mutations. We also observed a synonymous C to T nucleotide change at position 1152.
The S1 sequence in the virus obtained from Mass/B vaccinated and contact birds had a Glu64Gly change. A minor G peak was observed in the chromatogram indicating that the change resulted from selection of a subpopulation (Fig. 1). The virus isolated at necropsy from the contact-exposed birds showed additional changes of amino acid Ser105Pro and Pro490Leu (Table 7). Those changes apparently resulted from in vivo mutations.
The S1 amino acid sequence analysis of MassD/C vaccinated and contact-exposed birds were not consistent. The virus obtained from the first swabs from the vaccinated birds at 3 dpv and the contact-exposed birds at 6 dpv had amino acid changes that were not observed in the viruses isolated from subsequent swabs (data not shown).
Sequence analysis of reisolated vaccines passaged in eggs
To determine if genetic changes observed in the reisolated vaccine viruses would revert to the original vaccine sequence we passaged them a maximum of ten times in embryonating eggs and examined selected passages for genetic reversion (Table 8 ). No reversion was observed in the Ark/A, Ark/B, and Ark/C viruses reisolated from vaccinated birds following 10 passages. The Ark/B viruses reisolated from contact-exposed birds reverted from Asn to Tyr at position 326 and an additional Asn at position 345 was observed at pass 3 in embryonating eggs, which was the same as the original vaccine. The Conn/B virus reisolated from contact-exposed birds reverted to the original vaccine sequence at position Pro345Ser after 4 passages in eggs but the deletion of Asp58 in the reisolated vaccine was still present following 10 passages. None of the GA/A reisolated vaccine viruses reverted following 3 egg passages. The GA/A virus was only passaged 3 times in eggs due to contamination. The Mass/B detected by RT-PCR from vaccinated birds at 9dpv could not be rescued in embryonating eggs; thus, the 3dpv swabs were passaged in eggs. Reisolated Mass/B from vaccinated and contact-exposed birds did not revert to the original vaccine sequence at position Glu64Gly following 10 passages in eggs. Mass/B virus reisolated at 13 dpv from contact-exposed birds reverted to the original vaccine sequence at position Pro105Ser and Leu490Pro following 3 passages in eggs.
Table 8.
Subpopulations and changes following passage of reisolated virus in embryonating eggs
| Reisolated vaccine | Amino acid change | Double peaksa | Egg passage changeb |
|---|---|---|---|
| Ark/A (vaccinated 13 dpv)c | Tyr43His | Yes | No |
| Ser130Gly | No | No | |
| Ser213Ala | Yes | No | |
| Tyr326Asn | Yes | No | |
| Asn345 deletion | – | No | |
| Ark/B (contact 13 dpv) | Tyr326Asn | No | Yes (EP3)d |
| Asn345 deletion | – | Yes (EP3) | |
| Ark/B (vaccinated 9 dpv) | Tyr326Asn | No | No |
| Asn345 deletion | – | No | |
| Ark/C (vaccinated 6 dpv) | Tyr43His | Yes | No |
| Ser130Gly | No | No | |
| Ser213Gly | Yes | No | |
| Thr323Arg | No | No | |
| Tyr326Asn | Yes | No | |
| Asn345 deletion | – | No | |
| Conn/B (contact 14 dpv) | Asn58 deletion | – | No |
| Ser345Pro | No | Yes (EP4) | |
| GA/A (vaccinated 9 dpv) | Ser221Thr | No | No (EP3) |
| Gly330Arg | Yes | No (EP3) | |
| Lys479Asn | No | No (EP3) | |
| Mass/B (vaccinated 3 dpv) | Glu64Gly | Yes | No |
| Mass/B (contact 13 dpv) | Glu64Gly | Yes | No |
| Ser105Pro | No | Yes (EP3) | |
| Pro490Leu | No | Yes (EP3) | |
Major and minor chromatogram peaks observed in clean sequence data.
Viruses were passaged 10 times in 9–11-day old embryonating eggs unless otherwise noted.
Virus reisolated from vaccinated or contact-exposed birds on the day indicated (dpv = day post-vaccination).
Each egg passage was sequenced. (EP#) = Egg passage number where the change was observed.
Discussion
In this study, we examined the S1 sequence of 12 vaccines for IBV and compared that sequence data to the same vaccines reisolated from vaccinated and contact-exposed chickens. We focused on the S1 gene for this analysis because it is widely known that the S1 subunit of spike contains serotype specific epitopes, as well as epitopes that induce virus-neutralizing antibodies and S1 is directly involved in attachment to host cells. In addition, it was shown that by far, most genetic changes occur in the S1 gene during adaptation to the host [15], [16], [17]. Until now, it was not clear if mutations or selection of a more fit subpopulation was responsible for the changes observed when coronaviruses are attenuated or adapted to a particular host system [16]. Our data clearly shows that selection of a subpopulation of intra-vaccine quasispecies results from infection and replication of IBV vaccine viruses in chickens and that genetic mutation among IBV vaccines also occurs.
With a couple of exceptions where it was necessary to sequence cloned amplicons due to sequencing difficulties, we sequenced RT-PCR products because that data represents all of the genetic diversity within the population of viruses in a given isolate. Sequence ambiguities in otherwise clean sequence data can be used to identify diverse viral RNA genomes within an isolate [5]. Furthermore, the area under the peaks when two or more peaks are present at any single nucleotide position in the sequence chromatogram can be used to identify the major and minor subpopulations. Our data show differences in S1 sequence within the same vaccine serotype from different manufacturers, differences in S1 sequence between different vaccine serials from the same manufacturer, and intra-vaccine S1 differences. Differences in the S1 gene between the same vaccine serotype from different manufacturers likely reflects the source of the original virus strain used to produce the vaccine and the methods and number of passages in embryonating chicken eggs used to attenuate the virus. S1 gene differences between vaccine serials from the same manufacturer are most likely due to the generation of mutations through replication of the viral genome. The World Organization for Animal Health (OIE) guidelines (http://www.oie.int/eng/normes/mmanual/A_summry.htm) for production of IBV vaccines stipulates that no more than 5 passages beyond the master seed can be used to produce the vaccine. IBV has been reported to have a 1.5% mutation rate per year, and SARS-CoV was reported to have a non-synonymous substitution rate of 1.16–3.30 × 10−3 per site per year [7], [8]. In addition, it has been reported that IBV can adapt to cell culture following as few as 2–5 passages and as many as 25 amino acid substitutions have been documented in the S1 gene after only 7 passages in cell culture [18], [19]. Clearly, coronaviruses have the capacity for rapid genetic change, which likely accounts for sequence differences between different serials of the same vaccine.
To our knowledge, this is the first report where both selection of a more fit virus subpopulation and mutations are associated with replication of modified live IBV vaccine viruses in chickens. Vaccine virus subpopulation selection following vaccination, as evidenced by major and minor peaks in otherwise clean sequence data, were observed for Tyr43His, Ser213Ala, and Tyr326Asn changes in reisolated Ark/A and Ark/C vaccine, Gly330Arg in reisolated GA/A vaccine and Glu64Gly in reisolated Mass/B vaccine. Genetic mutations as evidenced by single peaks in clean sequence data and no reversion following egg passage of reisolated viruses, were observed for Ark/A at Ser130Gly, and Ark/C at Ser130Gly and Thr323Arg. Mutations were also detected for GA/A at positions Ser221Thr and Lys479Asn. However, it should be noted that existing viral RNA species could be responsible for apparent genetic mutations if that viral RNA subpopulation was below our level of detection. The level of detection for the RT-PCR test used herein is approximately 500 template copies/ml (unpublished data). No genetic subpopulations for Conn/B at position Ser345Pro were detected in the original vaccine, however; the reisolated vaccine reverted to Ser after only 4 egg passages. This was also observed for Mass/B at positions Ser105Pro and Pro490Leu, which reverted after only 3 egg passages. Reversion after only a few egg passages suggests that the genetic change is important for growth in eggs but it is not clear if selection of a subpopulation or mutations was responsible for those changes.
A deletion of 3 nucleotides (AAT) coding for Asn345 was observed in all of the reisolated Ark vaccines indicating that that genetic change is important for in vivo replication of Ark type vaccines. However, based on sequence data from cloned RT-PCR product, the reisolated Ark/B vaccine reverted following embryonating egg passage indicating that a low-level virus population retaining the 3 nucleotide sequence was being maintained in vivo, since it is unlikely, but not impossible, that the virus could acquire an AAT insertion through a recombination event or other mechanism after only a few back passages in eggs. It was necessary to clone the RT-PCR products from the Ark/B vaccine to obtain sequence data of single fragments, presumably because viruses with and without the deletion were being maintained in the population.
Amino acid sequence differences in the IBV spike glycoprotein are responsible for diverse serotypes of the virus, which do not cross-protect [20]. Some IBV vaccines, so called protectotypes, have been shown to provide more cross-protection than other similar vaccines [21]. It is likely that these protector-type vaccines have a more diverse population of viruses capable of simulating a broader immune response in the host. In addition, it has been shown that viral subpopulations can work together to invade and replicate in the host [22], [23]. Thus, it seems logical that a vaccine having a more dynamic quasispecies population ought to be more efficacious than one producing fewer mutant sequences. However, molecular evolution can lead to the selection of virulent viruses as well as the emergence of new viral pathogens [9]. A largely undocumented but widely accepted phenomenon of rolling vaccine reactions in commercial chicken flocks occurs when less than 100% of the flock receives the vaccine allowing repeated transmission of the vaccine virus from vaccinated birds to unvaccinated flock-mates. The highly infectious nature of IBV combined with vaccination and re-infection of vaccine viruses in a commercial chicken flock that can contain over 20,000 birds, likely allows the virus to undergo molecular evolution. The evidence for this can be found in the multitude of variant viruses with sequences extremely similar to the vaccines used in the flocks [24].
In summary, it appears that high-titered IBV vaccines contain a mixture of genetic variants and vaccination of chickens results in selection of the most fit viral RNA subpopulations as well as generation of mutations. This allows rapid adaptation to the host ensuring replication and stimulation of an immune response, however; accumulating evidence also indicates that it can lead to persistence and the emergence of new viral pathogens [5], [9]. Recognizing selection and mutation of vaccine viruses in the host is important for our understanding of how vaccine viruses can potentially replicate, persist and evolve to cause disease, and applies to all modified live coronavirus vaccines including potential vaccines against the SARS-CoV. This information can also be used to develop safer, higher quality, more targeted modified live vaccines containing viral subpopulations that successfully induce an efficacious immune response.
Acknowledgements
We would like to thank Dr. Mary Pantin-Jackwood and Dr. Egbert Mundt for reviewing this manuscript.
References
- 1.Masters P.S. The molecular biology of coronaviruses. Adv Virus Res. 2006;66:193–292. doi: 10.1016/S0065-3527(06)66005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vijaykrishna D., Smith G.J., Zhang J.X., Peiris J.S., Chen H., Guan Y. Evolutionary insights into the ecology of coronaviruses. J Virol. 2007;81(8):4012–4020. doi: 10.1128/JVI.02605-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fabricant J. The early history of infectious bronchitis. Avian Dis. 1998;42:648–650. [PubMed] [Google Scholar]
- 4.Jackwood M.W., Hilt D.A., Callison S.A. Detection of infectious bronchitis virus by real-time reverse transcriptase-polymerase chain reaction and identification of a quasispecies in the Beaudette strain. Avian Dis. 2003;47(3):718–724. doi: 10.1637/6075. [DOI] [PubMed] [Google Scholar]
- 5.Zhang X., Hasoksuz M., Spiro D., Halpin R., Wang S., Vlasova A. Quasispecies of bovine enteric and respiratory coronaviruses based on complete genome sequences and genetic changes after tissue culture adaptation. Virology. 2007;363(1):1–10. doi: 10.1016/j.virol.2007.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai M.M.C., Holmes K.V. Coronaviridae: the viruses and their replication. In: Knipe D.M., Howley P.M., Griffin D.E., Lamb R.A., Martin M.A., Roizman B., editors. Fields virology. 4th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2001. pp. 1163–1185. [Google Scholar]
- 7.Zhao Z., Li H., Wu X., Zhong Y., Zhang K., Zhang Y.P. Moderate mutation rate in the SARS coronavirus genome and its implications. BMC Evol Biol. 2004;4:21. doi: 10.1186/1471-2148-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee C.W., Jackwood M.W. Origin and evolution of Georgia 98 (GA98), a new serotype of avian infectious bronchitis virus. Virus Res. 2001;80(1–2):33–39. doi: 10.1016/s0168-1702(01)00345-8. [DOI] [PubMed] [Google Scholar]
- 9.Domingo E., Baranowski E., Ruiz-Jarabo C.M., Martin-Hernandez A.M., Saiz J.C., Escarmis C. Quasispecies structure and persistence of RNA viruses. Emerg Infect Dis. 1998;4(4):521–527. doi: 10.3201/eid0404.980402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gelb J.J., Jackwood M.W. Infectious bronchitis. In: Swayne D.E., Glisson J.R., Jackwood M.W., Pearson J.E., Reed W.M., editors. A laboratory manual for the isolation and identification of avian pathogens. 4th ed. American Association of Avian Pathologists; Kennett Square, PA: 1998. pp. 169–174. [Google Scholar]
- 11.Jackwood M.W., Yousef N.M., Hilt D.A. Further development and use of a molecular serotype identification test for infectious bronchitis virus. Avian Dis. 1997;41(1):105–110. [PubMed] [Google Scholar]
- 12.Lee C.W., Hilt D.A., Jackwood M.W. Redesign of primer and application of the reverse transcriptase-polymerase chain reaction and restriction fragment length polymorphism test to the DE072 strain of infectious bronchitis virus. Avian Dis. 2000;44(3):650–654. [PubMed] [Google Scholar]
- 13.Keeler C.L., Jr., Reed K.L., Nix W.A., Gelb J., Jr. Serotype identification of avian infectious bronchitis virus by RT-PCR of the peplomer (S-1) gene. Avian Dis. 1998;42(2):275–284. [PubMed] [Google Scholar]
- 14.Callison S.A., Hilt D.A., Boynton T.O., Sample B.F., Robison R., Swayne D.E. Development and evaluation of a real-time Taqman RT-PCR assay for the detection of infectious bronchitis virus from infected chickens. J Virol Methods. 2006;138(1–2):60–65. doi: 10.1016/j.jviromet.2006.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cavanagh D., Picault J.P., Gough R., Hess M., Mawditt K., Britton P. Variation in the spike protein of the 793/B type of infectious bronchitis virus, in the field and during alternate passage in chickens and embryonated eggs. Avian Pathol. 2005;34(1):20–25. doi: 10.1080/03079450400025414. [DOI] [PubMed] [Google Scholar]
- 16.Huang Y.P., Wang C.H. Sequence changes of infectious bronchitis virus isolates in the 3′ 7.3 kb of the genome after attenuating passage in embryonated eggs. Avian Pathol. 2007;36(1):59–67. doi: 10.1080/03079450601110015. [DOI] [PubMed] [Google Scholar]
- 17.Liu S., Han Z., Chen J., Liu X., Shao Y., Kong X. S1 gene sequence heterogeneity of a pathogenic infectious bronchitis virus strain and its embryo-passaged, attenuated derivatives. Avian Pathol. 2007;36(3):231–234. doi: 10.1080/03079450701338730. [DOI] [PubMed] [Google Scholar]
- 18.Shen S., Law Y.C., Liu D.X. A single amino acid mutation in the spike protein of coronavirus infectious bronchitis virus hampers its maturation and incorporation into virions at the nonpermissive temperature. Virology. 2004;326(2):288–298. doi: 10.1016/j.virol.2004.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fang S.G., Shen S., Tay F.P., Liu D.X. Selection of and recombination between minor variants lead to the adaptation of an avian coronavirus to primate cells. Biochem Biophys Res Commun. 2005;336(2):417–423. doi: 10.1016/j.bbrc.2005.08.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cavanagh D., Naqi S.A. Infectious bronchitis. In: Saif Y.M., editor. Diseases of poultry. 11th ed. Iowa State University Press; Ames, IA: 2003. pp. 101–119. [Google Scholar]
- 21.Cook J.K.A., Orbell S.J., Woods M.A., Huggins M.B. Breadth of protection of the respiratory tract provided by different live-attenuated infectious bronchitis vaccines against challenge with infectious bronchitis viruses of heterologous serotypes. Avian Pathol. 1999;28:477–485. doi: 10.1080/03079459994506. [DOI] [PubMed] [Google Scholar]
- 22.Vignuzzi M., Stone J.K., Arnold J.J., Cameron C.E., Andino R. Quasispecies diversity determines pathogenesis through cooperative interactions in a viral population. Nature. 2006;439(7074):344–348. doi: 10.1038/nature04388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pfeiffer J.K., Kirkegaard K. Bottleneck-mediated quasispecies restriction during spread of an RNA virus from inoculation site to brain. Proc Natl Acad Sci USA. 2006;103(14):5520–5525. doi: 10.1073/pnas.0600834103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nix W.A., Troeber D.S., Kingham B.F., Keeler C.L., Jr., Gelb J., Jr. Emergence of subtype strains of the Arkansas serotype of infectious bronchitis virus in Delmarva broiler chickens. Avian Dis. 2000;44(3):568–581. [PubMed] [Google Scholar]


