Abstract
Further attenuated measles vaccines were developed more than 50 years ago and have been used throughout the world. Recombinant measles vaccine candidates have been developed and express several heterologous virus protective antigens. Immunogenicity and protective actions were confirmed using experimental animals: transgenic mice, cotton rats, and primates. The recent development of measles vaccine-based vectored vaccine candidates has been reviewed and some information on recombinant measles vaccines expressing respiratory syncytial virus proteins has been shown and discussed.
Keywords: AIK-C measles vaccine, Reverse genetics, Recombinant virus, Respiratory syncytial virus
1. Introduction
The measles virus is a member of the genus Morbillivirus, the family Paramyxoviridae, order Mononegavirales and consists of 15,894 nucleotides that encode six major structural proteins. The nucleoprotein (N), phosphoprotein (P), large protein (L), and genomic RNA constitute the ribonucleoprotein complex (RNP) as transcription and replication units. Two envelope spike glycoproteins, hemagglutinin (H) and fusion (F), are present on the surface of infectious particles and execute the process of virus attachment and cell fusion. The M protein contributes to viral assembly and maturation [1]. Measles virus was first isolated in 1954 by Enders and Peebles from a patient and the Edmonston strain was further propagated in human kidney or alantoic fluid fibroblastic cells [2]. The AIK-C measles vaccine strain was developed from the wild-type Edmonston strain through small plaque cloning in sheep kidney cells and chick embryonic cells at 32.5 °C [3], [4]. The AIK-C strain is one of the candidate vaccine strains for the Expanded Programme on Immunization (EPI) to overcome maternally conferred immunity, thereby resulting in a high sero-conversion rate in young infants at 6 months of age [5], [6], [7]. Over 20 million doses have been administered mainly in Japan, and no serious adverse events have been reported in post marketing surveillance.
2. Characteristics of the AIK-C strain
The AIK-C strain shows optimal virus growth at 33 °C with small plaques, but extremely poor or no growth at 39–40 °C, demonstrating temperature sensitivity (ts). These biological markers have been used to validate vaccine production and some responsible genes were identified [3], [4]. The AIK-C vaccine strain was developed from the Edmonston strain and its full-length sequence was reported, in which 31 amino acid substitutions were found relative to the Edmonston wild-type [8]. The recent development of molecular genomic analysis has allowed reverse genetics to be performed in order to generate the infectious measles virus [9]. The reverse genetics of the AIK-C vaccine strain was explored to investigate the specific genome regions responsible for its unique biological characteristics. F and HA protein expression experiments revealed that Leu at position 278 of the F protein was responsible for the formation of small plaques in Vero cells and Phe at position 278 of the F protein of the Edmonston strain induced large plaques in Vero cells [10]. Infectious cDNA clones having F278Leu and F278Phe were generated: a recombinant virus having F278Leu induced small plaques, whereas large plaques were generated by a virus having F278Phe. However, this position did not influence the ts characteristics [10].
The replication and transcription of the measles virus are regulated by interactions between the N, P, and L proteins, and a measles mini-genome system, in which the luciferase reporter gene was inserted between the measles leader and trailer sequences, was developed to investigate transcription and replication activities [11]. Limited or no luciferase activity was observed when the P protein expression plasmid from the AIK-C strain was used in the mini-genome assay at 37 °C or higher temperatures, whereas the P expression plasmid from the Edmonston strain did not influence luciferase activity at 37 °C or higher temperatures. The P protein of the AIK-C strain was responsible for the ts characteristics and Pro at position 439 of the P protein was a critical point for the ts phenotype based on the findings of a mini-genome assay using the chimerical P expression plasmids constructed from the AIK-C and parental Edmonston strains. A recombinant measles virus having Pro at position 439 of the P protein was generated, and showed the ts phenotype. However, a recombinant measles virus having Leu at position 439 of the P protein did not [11].
3. Development of recombinant vaccines
Currently available vaccines are categorized into two types: live attenuated and inactivated vaccines. Inactivated vaccines principally induce humoral antibodies, whereas both humoral and cellular immune responses are induced by live attenuated vaccines. Therefore, a live attenuated vaccine has clinical benefits in addition to strong immunity: a basically single or two-dose immunization provides long-term immunity with a relatively lower cost. Clinical adverse events are more frequently observed with live vaccines than with inactivated vaccines because of the growth of the vaccine strain in the body. Numerous difficulties are associated with developing a new live vaccine by conventional procedures through consecutive passages in primary cell cultures. Immunogenicity and safety profiles are confirmed in experimental animal models. Final availability is established in a large-scale phase III clinical trial; however, the number of participants can be limited. Many effective live attenuated vaccines are known to be effective and safe through a long history of clinical use. Therefore, currently available live vaccine-based vectored vaccines are also expected to be theoretically safe and immunogenic.
Although a number of recombinant virus vectors derived from the vaccinia virus Ankara strain, poxviruses, adeno-associated viruses, and human parainfluenza virus type III have been developed, some virus vectors were not derived from the licensed vaccine strains, without clinical experience [12], [13], [14], [15], [16]. There is no predictable biomarker relevant to the vaccine safety in experimental animals. Thus, large-scale clinical trials should be conducted for these vectors in order to assure the safety of the vector. Virus vectors derived from currently available vaccines are theoretically considered to be safe and effective. Among the currently licensed vaccines, the yellow fever vaccine has been used as a live attenuated vaccine-virus vector for the development of recombinant Japanese encephalitis, dengue, and West Nile virus vaccines [17], [18], [19]. The pre M + E region of the yellow fever vaccine was replaced by that of the other flaviviruses. Of these, the yellow fever vaccine-based Japanese encephalitis virus vaccine (ChimeriVax-JE) has been licensed.
The live attenuated measles vaccine is a more popular than the yellow fever vaccine. It induces efficient humoral and cellular immunity and its long clinical use has guaranteed its safety [20]. In addition, the measles virus theoretically replicates in the cytoplasm and there is no evidence to suggest that the genome is integrated into host DNA. Recent developments in the reverse genetics of the measles virus have allowed recombinant measles virus cDNA to be artificially manipulated, thereby, contributing to a better understanding of the mechanisms underlying virus replication, transcription, and pathogenesis. The live attenuated measles vaccine has been investigated for the recombinant virus vector besides the yellow fever vaccine. Several strains are now available throughout the world and attenuation mechanisms are supposedly different for each strain [21]. Two groups are now extensively working on recombinant measles vaccine candidates using licensed measles vaccine strains from Dr. Naim, Berna Biotech [22], [23], [24], [25], Dr. Tangy, Pasteur Institute [26], [27], [28], [29], [30], [31], [32], and others [33], [34]. Their construction strategies, targets, and experimental models are summarized in Table 1 . They targeted the unmet needs of the vaccines against HIV, SARS corona, West Nile, dengue, Nipah, chikungunya, and hepatitis C viruses. Through conventional strategy, effective live or inactivated vaccines were not developed against these targets. The targeted genome regions were inserted at the N/P, P/M, or H/L junctions. Most popular insertion site is at the P/M junction. When a heterologous gene was inserted at the N/P junction, amounts of mRNA of the P gene decreased, causing poor virus growth. Mourez et al. [31] reported a different strategy by which the F and H genome regions of the measles virus were replaced by the chimeric DNA fragment of the simian immunodeficiency virus (SIV) gp160 genome fused with the cytoplasmic region of measles F protein genome, which interacted with the M protein. The immunogenicity of the recombinants was examined in transgenic mice expressing human CD46 with the deletion of the IFN-α/β receptor or non-human primates. There is no proper experimental animal for evaluating immune responses for measles. Transgenic mice depleted of IFN systems are not appropriate to investigate the immunogenicity following administration of recombinant measles-vectored vaccine candidates. In our preliminary experiments, cotton rats (Sigmodon hispidus) were susceptible for measles virus infection. Measles virus genome was detected from regional draining lymph nodes and virus was isolated. Neutralizing antibodies were produced in cotton rats three weeks after immunization of AIK-C measles vaccine strain [35].
Table 1.
Recombinant measles vaccine-based virus expressing heterologous antigens.
| MV vector | Insertion site | Inserted targets | Experimental animals | Authors [ref. No.] | |
|---|---|---|---|---|---|
| Edm. Zagreb | P/M | SARS-Corona virus | Nucleocapsid, Spike | CD46+, IFN-receptor- mice | Liniger et al. [22] |
| Berna Moraten | P/M | HPV | L1 | CD46+, IFN-receptor- mice | Cantarella et al. [23] |
| P/M, H/L | HIV | gp140, Gag-pol, | CD46+, IFN-receptor- mice | Liniger et al. [24] | |
| Edmonston B | P/M, H/L | Mumps virus, SIV | Mumps F, HN, SIV env, etc. | CD46+, IFN-receptor- mice | Wang et al. [25] |
| Schwarz | P/M | SARS Corona virus | Spike | CD46+, IFN-receptor- mice | Escriou et al. [26] |
| P/M | HIV | HIV Gag, RT, Nef | Cynomolgus macaques | Stebbings et al. [27] | |
| P/M | West Nile virus | Envelope | Squirrel monkey | Brandler, et al. [28] | |
| P/M | Dengue viruses I-IV | Envelope + partial M | CD46+, IFN-receptor- mice | Brandler et al. [29] | |
| P/M, H/L | HIV | Gag (P/M), Env (H/L) | CD46+, IFN-receptor- mice | Guerbois et al. [30] | |
| F and H: replaced | SIV | gp160+MVF cytoplasmic | ND | Mourez et al. [31] | |
| P/M | Chikungunya virus | C-E3-E2-6K-E1 | CD46+, IFN-receptor- mice | Brandler et al. [32] | |
| Edmonston B, Wild | N/P | Nipah virus | G | African green monkey | Yoneda et al. [33] |
| Moraten/Schwarz | P/M | Hepatits C, | E1, E2 | CD46+, IFN-receptor- mice | Reyes-del Valle et al. [34] |
| Edm. Zagreb | P/M | RSV, EB virus | SV F, EB gp350 | Cotton rats, Rhesus Macaques | Mok et al. [39] |
| AIK-C | P/M | RSV | F, G | Cotton rats | Sawada et al. [40] |
| AIK-C | P/M | RSV | NP, M2, F | Cotton rats | Yamaji et al. [41] |
MV: measles virus, Edm. Zagreb: Edmonston Zagreb, HIV: human immunodeficiency virus, HPV: human papilloma virus, SIV: simian immunodeficiency virus, RSV: respiratory syncytial virus, EB: Epstein Barr virus, CD46+, IFN-receptor- mice: human CD46 transgenic and interferon receptor knockout mice.
4. History of the respiratory syncytial virus (RSV) vaccine
The RSV vaccine has been anticipated for many years, among the many unmet needs of vaccines. RSV is one of the most common causes of lower respiratory tract infections in infants and young children worldwide. The peak age for serious RSV infections is less than 6 months and most children have had an RSV infection by two years of age. Serious complications have been reported especially in newborn babies born prematurely with lung diseases, or those with congenital heart diseases. RSV also causes lower respiratory tract infections in the elderly and immuno-compromised hosts, as well as in the pediatric population [36], [37].
The formalin-inactivated RSV vaccine (FI-RSV) was developed after the discovery of RSV. However, it failed to induce protective immunity and resulted in a paradoxical tragedy of increasing the severity of subsequent RSV infections [36]. Since then, many challenges were performed. The classical biological selection of cold-adapted or ts mutants or reverse genetically engineered vaccine candidates were not appropriately attenuated, and subunit vaccines of the fusion (F) or glycoprotein (G) did not provide long-term protective immunity [38]. The reasons for the serious outcome of FI-RSV were extensively investigated, and FI-RSV was found to induce a skewed Th2 response. A balanced Th1 and Th2 response is essential for the development of a RSV vaccine [38]. Therefore, live-vectored vaccine candidates have been investigated using human parainfluenza, bovine parainfluenza, and Sendai viruses [38]. The measles vaccine-vectored RSV vaccine has also been reported. Mok et al. [39] reported recombinant measles virus cDNA with the insertion of RSV F at the P/M junction and Epstein–Barr (EB) virus gp350 protein at the H/L junction. The infectious virus was recovered and induced neutralizing antibodies against RSV but not against EBV.
5. Development of recombinant measles vaccine expressing RSV antigens
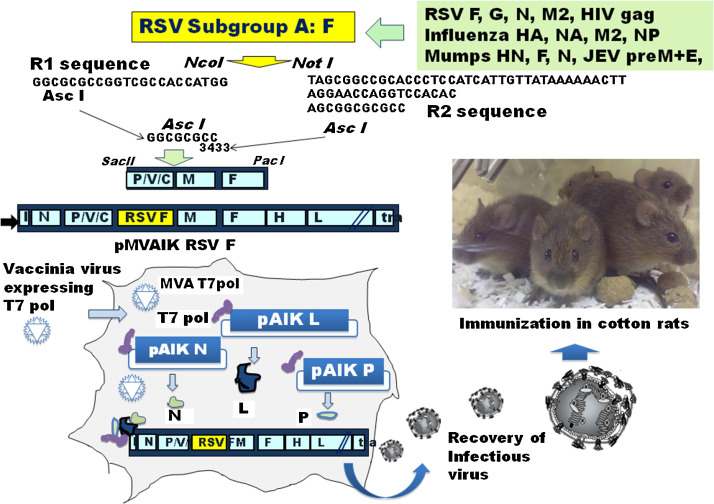
The experimental design for the construction of recombinant cDNA from the AIK-C strain and immunogenicity are shown in Fig. 1 . The Asc I restriction enzyme site was introduced by adding the GGCGCG sequence at the 3433 genome position of the P/M junction. The R1 and R2 sequences were added, and a cloning vector was constructed from nucleotide position 2040 of the Sac II site and at 7238 of the EcoT22I site. The open reading frames of the heterologous virus genome encoding the protective antigen were cloned at the restriction enzyme sites, Nco I and Not I. They were introduced into full-length infectious cDNA using Sac II and Pac I sites. They were then transfected into 293 T cells together with helper plasmids expressing the measles N, P, and L proteins under the control of T7 RNA polymerase. Infectious virus particles were rescued through blind passages in Vero cells at 32.5 °C in 5% CO2.
Fig. 1.
Experimental strategy for the recombinant measles virus expressing heterologous antigens. Three experimental steps are involved. (1) Cloning of heterologous genome: heterologous virus genomes encoding the protective antigen were cloned using Nco I and Not I. (2) Construction of measles AIK-C vector: Asc I restriction enzyme site was introduced at the 3433 genome position at the P/M junction, and the R1, R2 sequences, and Nco I and Not I sites were added. A cloning vector was constructed from nucleotide position 2040 of the Sac II site and at 7238 of the EcoT22I site. (3) Infectious virus recovery: 293T cells were infected with vaccine virus expressing T7 RNA polymerase and were transfected with full length of infectious cDNA, together with helper plasmids expressing measles N, P, and L proteins. Then, cotton rats were immunized.
Recombinant measles viruses expressing the fusion (F) or glyco (G) proteins of RSV subgroup A (MVAIK/RSV/F or MVAIK/RSV/G) were developed. These viruses induced cross protective neutralizing antibodies (NT) against RSV subgroups A and B in cotton rats. The infectious virus was not recovered from the lung tissues of the cotton rats immunized with recombinant viruses after the challenge with RSV subgroup A, but the protective effects were not sufficient after the challenge with RSV subgroup B [40]. Although no detectable RSV was recovered from immunized cotton rats after the challenge, very mild inflammatory pneumonitis was observed.
Recombinant measles viruses expressing RSV M2-1 or NP (MVAIK/RSV/M2-1 and MVAIK/RSV/NP) were generated, together with MVAIK/RSV/F. No detectable neutralizing antibody against RSV was induced in cotton rats immunized with recombinant measles virus expressing M2-1 or NP, whereas high titers of neutralizing antibody were induced after immunization with those expressing F or G protein. MVAIK/RSV/M2-1 and MVAIK/RSV/NP induced strong CTL responses, increasing the number of CD8+ IFN-γ+ cells in spleen cells stimulated with the NP, M2, and F peptides, or inactivated RSV antigen [41]. No infectious virus was recovered from lung homogenate following the challenge. A histological examination of the lung tissues demonstrated a significant reduction in inflammatory reactions without alveolar damage, despite negative for neutralizing antibodies. Both neutralizing antibody and CTL responses are essential for the protection from infection and mitigating the inflammatory responses.
When considering a clinical usage of recombinant measles vaccine candidates expressing RSV antigen in young infants, growth inhibition of vaccine virus was supposed because of maternally conferred immunity. When cotton rats were immunized beforehand with different doses of AIK-C vaccine strain, a significant antibody response was demonstrated after immunization with MVAIK/RSV/F in cotton rats with PA titer ≤320. Considering the protection for newborn or young infants in clinical setting, adult immunization of recombinant virus (MVAIK/RSV/F) would be expected before pregnancy. But, the experimental model is hardly developed because of different immunological system in rodents.
Due to its clinical use for several decades, the measles vaccine is considered to be safe and immunogenic, thereby providing long-term memory, and maybe a promising platform for developing a new vaccine. Several issues remain to be resolved: the acceptability of DNA-engineered vaccines in public, clinical guidelines for safety profiles, and regulatory guidelines for the manufacture of these vaccines.
References
- 1.Griffin D.E. Measles virus. In: Knipe D.M., Howley P.M., editors. Fields virology. 5th ed. Wolters Kluwer, Lippincott, Williams & Wilkins; Philadelphia: 2007. pp. 1551–1585. [Google Scholar]
- 2.Strebel P.M., Papania M.J., Fiebelkorn A.P., Halsey N.A. Measles vaccines. In: Plotkin S.A., Orenstein W.A., Offit P.A., editors. Vaccines. 6th ed. Elsevier; Philadelphia: 2013. pp. 352–387. [Google Scholar]
- 3.Sasaki K. Studies on the modification of the live AIK measles vaccine I. Adaptation of the further attenuated AIK measles virus (the strain of AIK-L33) to chick embryo cells. Kitasato Arch Exp Med. 1974;47:1–12. [PubMed] [Google Scholar]
- 4.Makino S. Development and characteristics of live AIK-C measles virus vaccine: a brief report. Rev Infect Dis. 1983;5:504–505. doi: 10.1093/clinids/5.3.504. [DOI] [PubMed] [Google Scholar]
- 5.Tidjani O., Grunitsky B., Guérin N., Lévy-Bruhl D., Lecam N., Xuereff C. Serological effects of Edmonston-Zagreb Schwarz, and AIK-C measles vaccine strains given at ages 4-5 or 8-10 months. Lancet. 1989;II:1357–1360. doi: 10.1016/s0140-6736(89)91967-3. [DOI] [PubMed] [Google Scholar]
- 6.Bolotovski V.M., Grabowsky M., Clements C.J., Albrecht P., Brenner E.R., Zargaryantzs A.I. Immunization of 6 and 9 month old infants with AIK-C, Edmonston-Zagreb, eningrad-16 and Schwarz strains of measles vaccine L. Int J Epidemiol. 1994;23:1069–1077. doi: 10.1093/ije/23.5.1069. [DOI] [PubMed] [Google Scholar]
- 7.Nkrumah F.K., Osei-Kwasi M., Dunyo S.K., Koram K.A., Afari E.A. Comparison of AIK-C measles vaccine in infants at 6 months with Schwarz vaccine at 9 months: a randomized controlled trial in Ghana. Bull WHO. 1998;76:353–359. [PMC free article] [PubMed] [Google Scholar]
- 8.Mori T., Sasaki K., Hashimoto H., Makino S. Molecular cloning and complete nucleotide sequence of genomic RNA of the AIK-C strain of attenuated measles virus. Virus Genes. 1993;7:61–81. doi: 10.1007/BF01702349. [DOI] [PubMed] [Google Scholar]
- 9.Radecke F., Spielhofer P., Schneider H., Kaelin K., Huber M., Dötsch C. Rescue of measles viruses from cloned cDNA. EMBO J. 1995;14:5773–5784. doi: 10.1002/j.1460-2075.1995.tb00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nakayama T., Komase K., Uzuka R., Hoshi A., Okafuji T. Leucine at position 278 of the AIK-C measles virus vaccine strain fusion protein is responsible for reduced syncytium formation. J Gen Virol. 2001;82:2143–2150. doi: 10.1099/0022-1317-82-9-2143. [DOI] [PubMed] [Google Scholar]
- 11.Komase K., Nakayama T., Iijima M., Miki K., Kawanishi R., Uejima H. The phosphoprotein of attenuated measles AIK-C vaccine strain contributes to its temperature-sensitive phenotype. Vaccine. 2006;24:826–834. doi: 10.1016/j.vaccine.2005.06.036. [DOI] [PubMed] [Google Scholar]
- 12.Drexler I., Staib C., Sutter G. Modified vaccinia virus Ankara as antigen delivery system: how can we best use its potential? Curr Opin Biotechnol. 2004;15:506–512. doi: 10.1016/j.copbio.2004.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arlen P.M., Kaufman H.L., DiPaola R.S. Pox viral vaccine approaches. Semin Oncol. 2005;32:549–555. doi: 10.1053/j.seminoncol.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 14.Johnson P.R., Schnepp B.C., Connell M.J., Rohne D., Robinson S., Krivulka G.R. Novel adeno-associated virus vector vaccine restricts replication of simian immunodeficiency virus in macaques. J Virol. 2005;79:955–965. doi: 10.1128/JVI.79.2.955-965.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Skiadopoulos M.H., Surman S.R., Riggs J.M., Orvell C., Collins P.L., Murphy B.R. Evaluation of the replication and immunogenicity of recombinant human parainfluenza virus type 3 vectors expressing up to three foreign glycoproteins. Virology. 2002;297:136–152. doi: 10.1006/viro.2002.1415. [DOI] [PubMed] [Google Scholar]
- 16.Slobod K.S., Shenep J.L., Luján-Zilbermann J., Allison K., Brown B., Scroggs R.A. Safety and immunogenicity of intranasal murine parainfluenza virus type I (Sendai virus) in healthy human adults. Vaccine. 2004;22:3182–3186. doi: 10.1016/j.vaccine.2004.01.053. [DOI] [PubMed] [Google Scholar]
- 17.Monath T.P., Guirakhoo F., Nichols R., Yoksan S., Schrader R., Murphy C. Chimeric live, attenuated vaccine against Japanese encephalitis (ChimeriVax-JE): phase 2 clinical trials for safety and immunogenicity, effect of vaccine dose and schedule, and memory response to challenge with inactive Japanese encephalitis antigen. J Infect Dis. 2003;188:1213–1230. doi: 10.1086/378356. [DOI] [PubMed] [Google Scholar]
- 18.Monath T.P., Liu J., Kanesa-Thasan N., Myers G.A., Nichols R., Deary A. A live, attenuated recombinant West Nile virus vaccine. Proc Natl Acad Sci USA. 2006;103:6694–6699. doi: 10.1073/pnas.0601932103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guy B., Saville M., Lang J. Development of Sanofi Pasteur tetravalent dengue vaccine. Hum Vaccine. 2010;16 doi: 10.4161/hv.6.9.12739. [DOI] [PubMed] [Google Scholar]
- 20.Zuniga A., Wang Z., Liniger M., Hangartner L., Caballero M., Pavlovic J. Attenuated measles virus as a vaccine vector. Vaccine. 2007;25:2974–2983. doi: 10.1016/j.vaccine.2007.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bankamp B., Takeda M., Zhang Y., Xu W., Rota P.A. Genetic characterization of measles vaccine strains. J Infect Dis. 2011;204:S533–S548. doi: 10.1093/infdis/jir097. [DOI] [PubMed] [Google Scholar]
- 22.Liniger M., Zuniga A., Tamin A., Azzouz-Morin T.N., Knuchel M., Marty R.R. Induction of neutralising antibodies and cellular immune responses against SARS coronavirus by recombinant measles viruses. Vaccine. 2008;26:2164–2174. doi: 10.1016/j.vaccine.2008.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cantarella G., Liniger M., Zuniga A., Schiller J.T., Billeter M., Naim H.Y. Recombinant measles virus-HPV vaccine candidates for prevention of cervical carcinoma. Vaccine. 2009;27:3385–3390. doi: 10.1016/j.vaccine.2009.01.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liniger M., Zuniga A., Azzouz-Morin T.N., Combardiere B., Marty R.R., Wiegand M. Recombinant measles viruses expressing single or multiple antigens of human immunodeficiency virus (HIV-1) induce cellular and humoral immune responses. Vaccine. 2009;27:3299–3305. doi: 10.1016/j.vaccine.2009.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang Z., Hangartner L., Cornu T.I., Martin L.R., Zuniga A., Billeter M.A. Recombinant measles viruses expressing heterologous antigens of mumps and simian immunodeficiency viruses. Vaccine. 2001;19:2329–2336. doi: 10.1016/s0264-410x(00)00523-5. [DOI] [PubMed] [Google Scholar]
- 26.Escriou N., Callendret B., Lorin V., Combredet C., Marianneau P., Février M. Protection from SARS coronavirus conferred by live measles vaccine expressing the spike glycoprotein. Virology. 2014;452–453:32–41. doi: 10.1016/j.virol.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stebbings R., Février M., Li B., Lorin V., Koutsoukos M., Mee E. Immunogenicity of a recombinant measles-HIV-1 clade B candidate vaccine. PLoS One. 2012;7:e50397. doi: 10.1371/journal.pone.0050397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brandler S., Marianneau P., Loth P., Lacôte S., Combredet C., Frenkiel M.P. Measles vaccine expressing the secreted-form of West Nile virus envelope glycoprotein induces protective immunity in squirrel monkeys, a new model of West Nile virus infection. J Infect Dis. 2012;206:212–219. doi: 10.1093/infdis/jis328. [DOI] [PubMed] [Google Scholar]
- 29.Brandler S., Ruffié C., Najburg V., Frenkiel M.P., Bedouelle H., Desprès P. Pediatric measles vaccine expressing a dengue tetravalent antigen elicits neutralizing antibodies against all four dengue viruses. Vaccine. 2010;28:6730–6739. doi: 10.1016/j.vaccine.2010.07.073. [DOI] [PubMed] [Google Scholar]
- 30.Guerbois M., Moris A., Combredet C., Najburg V., Ruffié C., Février M. Live attenuated measles vaccine expressing HIV-1 Gag virus like particles covered with gp160ΔV1V2 is strongly immunogenic. Virology. 2009;388:191–203. doi: 10.1016/j.virol.2009.02.047. [DOI] [PubMed] [Google Scholar]
- 31.Mourez T., Mesel-Lemoinw M., Combredet C., Najburg V., Cayet N., Tangy F. A chimeric measles virus with a lentiviral envelope replicates exclusively in CD4+/CCR5+cells. Virology. 2011;419:117–125. doi: 10.1016/j.virol.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 32.Brandler S., Ruffié C., Combredet C., Brault J.-B., Najburg V., Prevost M.-C. A recombinant measles vaccine expressing chikungunya virus-like particles is strongly immunogenic and protects mice from lethal challenge with chikungunya virus. Vaccine. 2013;31:3718–3725. doi: 10.1016/j.vaccine.2013.05.086. [DOI] [PubMed] [Google Scholar]
- 33.Yoneda M., Georges-Courbot M.-C., Ikeda F., Ishii M., Nagata N., Jacquot F. Recombinant measles virus vaccine expressing the Nipah Virus glycoprotein protects against lethal Nipah virus challenge. PLOS ONE. 2013;8:e58414. doi: 10.1371/journal.pone.0058414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reyes-del Valle J., de la Fuente C., Turner M.A., Springfeld C., Apte-Sengupta S., Frenzke M.E. Broadly neutralizing immune responses against hepatitis C virus induced by vectored measles viruses and a recombinant envelope protein booster. J Virol. 2012;86:11558–11566. doi: 10.1128/JVI.01776-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haga T., Murayama N., Shimizu Y., Saito A., Sakamoto T., Morita T. Analysis of antibody response by temperature-sensitive measles vaccine strain in the cotton rat model. Comp Immun Microbiol Infect Dis. 2009;32:309–406. doi: 10.1016/j.cimid.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 36.Anderson L.J., Parker R.A., Strikas R.L. Association between respiratory syncytial virus outbreaks and lower respiratory tract deaths of infants and young children. J Infect Dis. 1990;161:640–646. doi: 10.1093/infdis/161.4.640. [DOI] [PubMed] [Google Scholar]
- 37.Falsey A.R., Walsh E.E. Respiratory syncytial virus infection in adults. Clin Microbiol Rev. 2000;13:371–384. doi: 10.1128/cmr.13.3.371-384.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Collins P.L., Melero J.A. Progress in understanding and controlling respiratory syncytial virus: still crazy after all these years. Virus Res. 2011;162:80–99. doi: 10.1016/j.virusres.2011.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mok H., Cheng X., Xu Q., Zengel J.R., Parhy B., Zhao J. Evaluation of measles vaccine virus as a vector to deliver respiratory syncytial virus fusion protein or Epstein–Barr virus glycoprotein gp350. Open Virol J. 2012;6:12–22. doi: 10.2174/1874357901206010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sawada A., Komase K., Nakayama T. AIK-C measles vaccine expressing fusion protein of respiratory syncytial virus induces protective antibodies in cotton rats. Vaccine. 2011;29:1481–1490. doi: 10.1016/j.vaccine.2010.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yamaji Y., Nakayama T. Recombinant measles viruses expressing respiratory syncytial virus proteins induced virus-specific CTL responses in cotton rats. Vaccine. 2014;32:4529–4536. doi: 10.1016/j.vaccine.2014.06.024. [DOI] [PubMed] [Google Scholar]