Abstract
There is increasing research on posttraumatic growth after life-threatening illnesses such as cancer and HIV/AIDS, although it is unclear whether growth confers any psychological or physical benefits in such samples. Consequently, this meta-analysis explored the relationship between posttraumatic growth and psychological and physical wellbeing in adults diagnosed with cancer or HIV/AIDS and examined potential moderators of these relationships. Analysis of 38 studies (N = 7927) of posttraumatic growth after cancer or HIV/AIDS revealed that growth was related to increased positive mental health, reduced negative mental health and better subjective physical health. Moderators of these relationships included time since the event, age, ethnicity, and type of negative mental health outcome. It is hoped that this synthesis will encourage further examination of the potentially complex relationship between posttraumatic growth and adjustment in individuals living with life-threatening medical conditions.
Keywords: Posttraumatic growth, Benefit finding, Adjustment, Cancer, HIV/AIDS, Illness
1. Introduction
The diagnosis and treatment of a life-threatening illness is a major stressor for most individuals. Cancer and HIV/AIDS have shown to parallel other traumatic stressors in many ways. The diagnosis may be sudden and unexpected, the disease and treatment may pose threats to one's life, and the experience may evoke intense emotional responses of fear and helplessness. At the same time living with a life-threatening illness is not an acute, singular stressful experience, but rather a series of unfolding threats and stressors (Cordova, 2008). Cumulatively, these experiences can constitute a traumatic stressor for many individuals with cancer or HIV/AIDS. Experiencing a life-threatening illness was first recognised as an event that could precipitate posttraumatic stress disorder (PTSD) in the DSM-IV (American Psychiatric Association [APA], 1994). Rates of PTSD in cancer patients range from 5% to 35% (Kangas, Henry, & Bryant, 2002) and in HIV/AIDS patients from 30% to 64% (Botha, 1996, Kelly et al., 1998, Martinez et al., 2002).
Over the past decade there has been an important shift in emphasis of research from a nearly exclusive focus on the negative aftermath of such events to consideration of possible positive outcomes (Linley, 2003). Researchers have used a number of different terms to describe individuals' reports of benefits in the face of adversity, including posttraumatic growth, adversarial growth, benefit-finding, and thriving. Throughout this paper Tedeschi, Park, and Calhoun's (1998) term posttraumatic growth (PTG) will be used to describe a positive change in one's previous level of functioning as a result of the struggle with highly challenging life circumstances. This term differs from resilience, optimism, hardiness, which describe individuals who have adjusted successfully despite adversity (O'Leary & Ickovics, 1995), whereas individuals experiencing PTG are transformed by their struggle with adversity.
A rapidly increasing literature now testifies to the prevalence of positive life changes and personal growth following cancer and HIV/AIDS. Equally high rates of positive changes have been reported across both illnesses. Between 59% and 83% of people living with HIV/AIDS have been shown to report positive changes since diagnosis (*Milam, 2004, *Milam, 2006b, Siegel and Schrimshaw, 2000). Likewise, data suggest that between 60% and 90% of cancer survivors also report positive changes (Collins et al., 1990, Fromm et al., 1996, *Petrie et al., 1999, Rieker et al., 1985). Within the general PTG literature three common categories of growth outcomes have been identified (Joseph and Linley, 2006, Tedeschi et al., 1998). First, individuals often report that their relationships are enhanced in some way. For example many individuals with cancer or HIV/AIDS require practical and emotional support, and positive interpersonal experiences may strengthen a person's appreciation of some relationships. Second, people change their views of themselves in some way. For example patients may develop a greater sense of personal resilience and strength, an acceptance of their vulnerabilities and limitations, which are typified by a heightened awareness of their own mortality and the fragility of life. Third, there are often reports of changes in life philosophy. For example people diagnosed with cancer or HIV/AIDS are faced with the concern that their disease might progress and shorten their life and these concerns may lead to a shift in priorities and values, and to a different appreciation and approach to day-to-day life. Together these positive changes in psychological well-being can lead to a whole new way of living. Finally certain changes have been identified specific to individuals facing a serious illness. A recent focus of the PTG research has been the relationship between PTG and health behaviours (*Milam, 2004, Milam et al., 2004). Luszczynska, Sarkar and Knoll (2007) found that PTG significantly predicted adherence to antiretroviral therapy in individuals diagnosed with HIV. Furthermore, women with breast cancer have described making positive changes in health related behaviours and engaging in more careful cancer surveillance as a result of their experience (Sears, Stanton, & Danoff-Burg, 2003). Studies that compare PTG in cancer and HIV/AIDS patients suggest that growth is experienced in the same multidimensional manner across both illnesses (Lechner & Weaver, 2009). Therefore, alongside psychological, interpersonal, and life orientation changes, positive changes in health behaviours may also occur following a life-threatening illness diagnosis.
Several models have now been proposed regarding the occurrence of PTG. The three most detailed models to date include Tedeschi and Calhoun, 1995, Tedeschi and Calhoun, 2004 Functional Descriptive Model, Linley and Joseph's (2005) Organismic Valuing Theory and Christopher's (2004) Biopsychosocial–Evolutionary Theory. Although with some variation, most models hypothesize that the experience of a highly stressful or traumatic event violates an individual's basic beliefs about the self and the world and that some type of meaning making or cognitive processing to rebuild these beliefs and goals occurs, resulting in perceptions that one has grown through the process (Horowitz, 1986, Janoff-Bulman, 2004, Tedeschi and Calhoun, 2004). Although offering different levels of explanation at both the social cognitive and biological evolutionary levels, they are complimentary in that they are underpinned by the notion that people are intrinsically motivated towards growth (Joseph & Linley, 2006).
An important issue to be addressed in the literature is whether PTG following the diagnosis of a life-threatening illness is associated with psychological and physical benefits (Zoellner & Maercker, 2006). However, the current literature is unclear. For example some studies report there is no significant relationship between PTG and distress (Cordova et al., 2001, *Schulz and Mohamed, 2005), and other studies suggest distress and PTG can co-exist (Tomich & Helgeson, 2004). For example Barakat, Alderfer, and Kazak (2006) found that PTG and posttraumatic stress symptoms were positively correlated in adolescent survivors of cancer. However, other studies have reported an inverse relationship between measures of PTG and psychological distress (Linley and Joseph, 2004, *Updegraff et al., 2002, *Urcuyo et al., 2005).
Therefore, it remains to be established whether the experience of PTG in relation to a life-threatening illness confers any benefit in terms of psychological or physical health. Given the discrepant findings on this relationship a systematic integration of the literature is needed, and a meta-analysis is an ideal tool to do this. A previous meta-analysis conducted by Helgeson, Reynolds, and Tomich (2006) investigated the association between PTG and adjustment after a wide range of events such as sexual assault, natural disaster, bereavement, childhood abuse and illness. They found that PTG was related to more positive affect and less depression, but also to more intrusive thoughts about the event. PTG was unrelated to anxiety, distress, quality of life and subjective physical health. As such the aim of the current paper is to present a meta-analysis of the existing literature that will aim to objectively summarize PTG and its relation to adjustment in individuals living with a life threatening illness (cancer or HIV/AIDS) and to examine potential moderators of this relationship.
One possible explanation for the inconsistency between PTG and adjustment is that the relationship is moderated by other variables. Therefore five possible moderators will be examined that might attenuate or accentuate the growth–adjustment relationship. These were chosen because they are commonly assessed within the literature, and have prior empirical and theoretical foundations. The first variable that might moderate the relationship between PTG and adjustment is the length of time since the diagnosis. Research and theory suggest that PTG is unlikely to occur shortly after the critical event, but rather takes time to occur and is more likely to be reported in hindsight (Joseph and Linley, 2005, Tedeschi and Calhoun, 1995, Tedeschi and Calhoun, 2004). Therefore it is hypothesized that PTG is associated with positive adjustment when a longer time since the health event has elapsed. Three characteristics of the sample will also be examined as moderators: age, gender, and ethnicity. Past research has indicated that women (Bellizzi, 2004, *Milam, 2004), younger participants (Kinsinger et al., 2006; Linley and Joseph, 2004, *Milam, 2004, *Widows et al., 2005), and ethnic minorities are more likely to report PTG. However, it is not clear if and how these individual differences differentially relate to PTG and adjustment (Helgeson et al., 2006). Therefore no specific predictions about directionality regarding how these variables might moderate the growth–adjustment relationship will be made. It is also possible that the quality of the study might moderate the relationship between growth and health. For example studies that use a valid measure of growth should reflect actual PTG, and distinguish from other processes such as self-enhancement, positive illusion, and “pseudo-growth” (Lechner & Antoni, 2004; Park & Lechner, 2006). Less validated measures may fail to capture PTG, and therefore account for some of the variation in the research. Through examination of these moderators it is hoped that the meta-analysis will identify subgroups of adults whose experience of PTG is likely to be positively or negatively related to mental and physical health.
In summary, the purpose of the present study is two-fold. Primarily it is concerned with estimating the overall effect size of the relationship between PTG following a life threatening illness (cancer or HIV/AIDS) and various indicators of adjustment. Secondly, this analysis hopes to identify the variability amongst studies and explore potential moderators of the growth and adjustment relationship. It is hoped that such a review of the extant literature will lead to an enhanced understanding of the impact of PTG on the adjustment process in individuals living with life-threatening illnesses.
2. Method
2.1. Selection of studies for the meta-analysis
A systematic search was conducted to identify studies of PTG in individuals following cancer or HIV/AIDS. The primary search method for the selection of studies was a review of the psychological and medical literature using the following computerized databases up to October 2009: Medline, PsychArticles, PsychInfo, PubMed, and Web of Science. Relevant key words were used to search for articles within these databases. Search terms included key words related to PTG: posttraumatic growth, post-traumatic growth, benefit finding, stress related growth and adversarial growth. These terms were crossed with the following health-related key terms: health, illness, disease, life-threatening, chronic, medical, terminal, cancer, HIV, AIDS. Additional studies were located through the inspection of the reference sections of obtained papers and reviews. Relevant journals were also manually searched to locate papers that may not have been identified in the databases. These journals were: Psycho-Oncology, Psychology and Health, Journal of Traumatic Stress, British Journal of Health Psychology and Journal of Consulting and Clinical Psychology. In addition, active researchers in the field of psychological growth in health samples were contacted to ask for recent papers in the field and for unpublished research to reduce the effect of publication bias. A search of abstracts from relevant conferences was also conducted to locate additional unpublished work in the area. However, no unpublished studies were retrieved. This literature search yielded a preliminary database of 193 published papers.
2.2. Inclusion and exclusion criteria
These 193 papers were examined to determine eligibility for inclusion in the meta-analysis. Studies had to meet eight criteria for inclusion. First, studies were included only if the sample were adults aged 18 or over. This decision was made because the current literature is unclear whether children or adolescents differentially experience PTG in comparison to adults (Ickovics et al., 2006a, *Ickovics et al., 2006b, Milam et al., 2004), and also only a small number of studies have explored PTG in children and adolescents following illness (too few to include adult vs. child as a moderator variable). This resulted in the exclusion of nine studies. Second, the studies had to use a quantitative measure of PTG, which was assessed in relation to a measure of positive psychological adjustment, negative psychological adjustment or physical health. Studies that included a purely qualitative assessment of PTG, or papers that were reviews of the literature were excluded from the analysis. This resulted in the exclusion of 87 studies. Third, PTG must be measured in cancer or HIV/AIDS patients. This criterion resulted in the exclusion of 16 studies. Fourth, intervention studies were excluded from the analysis unless they measured PTG at baseline prior to manipulation and effect sizes could be extracted. This resulted in the exclusion of 20 studies. Fifth, controlled comparison studies that did not report relevant data for the patient sample were excluded. This resulted in the exclusion of nine studies. Longitudinal studies which measured PTG at different time points to adjustment measures were excluded. However, when longitudinal studies reported cross-sectional relationships these were included in the analysis. This resulted in the exclusion of seven studies. Studies needed to include the relevant effect sizes (namely the correlation coefficient r) or sufficient statistical information that could be used to compute this statistic. Authors of papers with unclear statistical information were contacted to enquire about further information and if this was unable to be provided these papers were excluded from the analysis.1 Only two papers were excluded as a result of this criterion. Finally, the authors of five non-English articles were contacted for copies of their papers but these were not provided. Fig. 1 summarizes the results of the systematic search.
Fig. 1.

Flow chart of systematic search.
2.3. Data coding
Of the 193 articles yielded by the literature search 38 studies met all of the requirements for inclusion and were therefore used in the meta-analysis. Studies included in the meta-analysis are identified with an asterisk in the reference section and a detailed list of the studies is provided in Table 1 . From these papers a number of variables were extracted for analysis: i) sample size, ii) sex composition, iii) ethnicity, iv) mean age, v) time since event, vi) health event vii) adjustment outcome, and viii) effect sizes for these relationships. The methodological quality of each study was also assessed based on a checklist developed by Mirza and Jenkins (2004). The five criteria that were assessed were: 1) clear study aims, 2) sample representative of population, 3) clear inclusion and exclusion criteria, 4) validated measure of PTG, and 5) appropriate statistical analysis. The studies were then given a total score of quality with the highest possible being eight (1 = Yes, 0 = No). Table 1 displays the quality scores for each individual study. Quality scores ranged from 2–5; however most studies were of good quality with over 50% of studies scoring 4 or more.
Table 1.
Characteristics of studies included in the meta-analysis.
| Study | N | Health event | Mean age (range) | Sex composition | Racial composition | Mean time since occurrence | Measure of growth | Quality |
|---|---|---|---|---|---|---|---|---|
| Bellizzi, Miller, Arora, & Rowland (2007) | 308 | Non-Hodgkins Lymphona | 60 (23–85) | 51.3% male, 48.7% female | 30% Hispanic | 42 months | Close ended | 3 |
| Bower et al. (2005) | 763 | Breast cancer | 56 (3 0–87) | 100% female | 83.7% White, 8.7% Black, 7.6% Other | 40.8 months | Close ended | 3 |
| Carrico et al. (2006) | 264 | HIV/AIDS | 40 | 49% male, 51% female | 49% African American, 25% Caucasian, 13% Hispanic | 7.7 years | BFS (a) | 4 |
| Cole, Hopkins, Tisak, Steel, and Carr (2008) | 253 | Cancer (Mixed) | 58 (28–86) | 78% female, 22% male | 95% White | 7 months | Spiritual transformation scale | 4 |
| Cordova, Cunningham, Carlson, and Andrykowski (2001) | 70 | Breast cancer | 55 (27–87) | 100% female | 90% White, 9% Black, 1% Other | 24 months | PTGI | 4 |
| Cordova et al. (2007) | 92 | Breast cancer | 52 (25–72.8) | 100% female | 86% White | 9.4 months | PTGI | 4 |
| Curbow, Somerfield, Baker, Wingard and Legro (1993) | 135 | Bone marrow transplant | 31 (18–53) | 61% male, 39% female | 91% White | 47 months | Open ended | 4 |
| Fromm et al. (1996) | 90 | Bone marrow transplantation | 39 | 58% male, 42% female | NR | 49.5 months | Open ended | 3 |
| Harrington, McGurk, and Llewellyn (2008) | 76 | Head and neck cancer | 66.9 (32–97) | 51% female, 49% male | 93% White, 7% Other | 34% 73–121 months, 25% 48–72 months, 41% < 48 months posttreatment | BFS (a) | 4 |
| Ho, Chan, and Ho (2004) | 188 | Cancer (Mixed) | 49 (26–69) | 17% male, 83% female | Chinese | > 5 years disease free | PTGI Chinese version | 3 |
| (Ickovics, Milan, et al., 2006) | 773 | HIV/AIDS | 36 (19–55) | 100% women | 60% Black, 20% Latina, 20% White/Other | NR | Close ended | 3 |
| Jaarsma, Pool, Sanderman, and Ranchor (2006) | 294 | Cancer | 56 (21–84) | 28% male, 72% female | NR | 3.90 years | PTGI (in Dutch) | 4 |
| Katz, Flasher, Cacciapaglia, and Nelson (2001) | 87 | Cancer and lupus | 53 | 13% male, 87% female | 73% White, 6% Black, 2% Asian, 12% Hispanic, 8% Other | 9 years | BFS (b) | 3 |
| Kinsinger et al. (2006) | 250 | Prostate cancer | 65 | 100% male | 41% White, 17% Black, 42% Hispanic | 15.7 months | BFS (a) | 4 |
| Klauer, Ferring, and Filipp (1998) | 100 | Cancer (mixed) | 53 | 42% female, 58% male | NR | 40% 1 year, 20% 2 years, 25% 2–5 years, 15% 5+ years | Close ended | 2 |
| Littlewood, Vanable, Carey and Blair (2008) | 221 | HIV/AIDS | 40 (22–59) | 44% female, 56% male | 42% African American, 46% Caucasian, 4% Native American, 4% Asian Pacific Islander, 4% Other | 7 years | BFS (a) | 4 |
| Luszczynska et al. (2007) | 104 | HIV/AIDS | 35 (18–54) | 36% male, 64% female | 100% Indian | < 5 years | BFS (a) | 3 |
| Milam (2004) | 835 | HIV/AIDS | 38 | 87% male, 13% female | 40% White, 37% Hispanic, 17% Black, 7% Other | 6.4 years | Items from PTGI | 4 |
| *Milam, 2006b, Milam, 2006a | 412 | HIV/AIDS | 39 | 88% male, 12% female | 39% White, 40% Hispanic, 15% African American, 6% Other | 6.4 years | Items from PTGI | 4 |
| Mols, Vingerhoets, Coebergh and Poll-France (2009) | 183 | Breast cancer | 100% female | NR | NR | PTGI | 3 | |
| Morrill et al. (2008) | 161 | Breast cancer | 59 (36–87) | 100% female | 85% White, 12% African American | 4 years | PTGI | 3 |
| (Mystakidou, Parpa, et al., 2007) | 54 | Cancer | 60 (36–84) | 27.6% male 72.4% female | NR | 55.2% < 3 years, 44.8 ≥ 3 years | PTGI | 4 |
| (Mystakidou, Tsilika, et al., 2007) | 100 | Breast cancer | 58.2 (31–81) | 100% female | NR | 6.1 years | PTGI | 4 |
| Park, Edmondson, Fenster, and Blank (2008) | 172 | Cancer (mixed) | 45.2 | 69% female, 31% male | 88% White, 5% Latino, 3% Black/African American, 2% Native American | 23.4 months since primary treatment | PBS | 5 |
| Petrie et al. (1999) Study 2 | 52 | Breast cancer | 54 | 100% female | 92% European, 4% Maori, 4% other | 3 months posttradiation | Open ended | 3 |
| Salmon, Manzi, and Valori (1996) | 200 | Cancer (mixed) | 17% < 50, 45% 50–65, 38% > 75 | 58% male, 42% female | NR | Median = 52 weeks | Close ended | 3 |
| Salsman, Segerstorm, Brechting, Carlson, and Andrykowski (2009) | 55 | Colorectal cancer | 65.9 | 58.9% female, 41.1% male | NR | 12 months | PTGI | 4 |
| Schroevers and Teo (2008) | 113 | Cancer (mixed) | 51.8 (17–85) | 66.4% female, 33.5% male | 82.3% Chinese, 11.5% Malay | 45 months | PTGI | 3 |
| Schulz and Mohamed (2004) | 105 | Cancer (mixed) | 62 (19–86) | 61% male 39% female | NR | 1 month postsurgery | BFS (a) | 3 |
| Schwarzer, Luszczynska, Boehmer, Taubert, and Knoll (2006) | 117 | Cancer surgery | 62 | 62% male 38% female | NR | NR | Close ended | 3 |
| Sears, Stanton, and Danoff-Burg (2003) | 60 | Breast cancer | 52 (28–76) | 100% female | 87% White, 7% Black, 3% Latina, 1% Asian American, 1% Native American | 80 weeks | PTGI | 3 |
| Siegel, Scrimshaw and Pretter (2005) | 138 | HIV/AIDS | 38 (22–48) | 100% female | 38% African American, 34% Puerto Rican, 28% White | 87.6 months | Thriving scale | 4 |
| Thornton and Perez (2006) | 82 | Prostate cancer | 61 (41–78) | 100% male | 90% White | NR | PTGI | 4 |
| Tomich and Helgeson (2004) | 364 | Breast cancer | 48 (25–75) | 100% female | 93% White, 6% Black, 1% Hispanic | 4 months | BFS (a) | 3 |
| Updegraff et al. (2002) | 189 | HIV | 37 (19–62) | 100% female | 48% Black, 33% White, 20% Latina | 4.65 years | Open ended | 3 |
| Urcuyo et al. (2005) | 230 | Breast cancer | 54 (27–87) | 100% female | 63% White, 27% Hispanic, 10% Black | 3–12 months post surgery | BFS (a) | 4 |
| Widows et al. (2005) | 72 | Cancer–Bone marrow transplantation | 48 (25–66) | 26% male, 74% female | 85% White, 7% Black, 8% Hispanic | 24.05 | PTGI | 4 |
| Yanez et al. (2009) Study 2 | 165 | Cancer (mixed) | 45.7 (22–55) | 33% male, 67% female | 89% White | 3.5 years | BFS (a) | 5 |
NR = Not reported in the study; PTGI = Posttraumatic Growth Inventory; SRGS – Stress Related Growth Scale; PBS – Perceived Benefits Scale; BFS (a) = Benefit Finding Scale (Antoni et al., 2001); BFS (b) = Benefit Finding Scale (Mohr et al., 1990); SLQ – Silver Lining Questionnaire.
As expected, the concept of adjustment was operationally defined in a number of ways across individual studies. In our analysis measures were combined and a separate analysis was conducted for positive psychological adjustment, negative psychological adjustment and subjective physical health. Psychological adjustment was defined in this paper as the psychological outcome, either positive or negative, following illness. Specific adjustment measures associated with each adjustment outcome were also examined as moderators to explore how they might explain variability within the growth–adjustment relationship. These adjustment measures were coded as follows: a) positive psychological adjustment was coded either as psychological health (e.g. positive affect, mental health) or general well-being (e.g. life satisfaction), b) negative psychological adjustment was coded as specific symptoms (e.g. depression, anxiety, PTSD) or general distress, and c) subjective physical health was coded as either general physical health, physical symptoms, or functional ability.
To examine the role of possible moderators in the growth–adjustment relationship, the following information in each paper was coded and used in the analysis as follows: (i) time since diagnosis was examined as a continuous moderator by using the mean time in months, (ii) sample gender composition was examined as continuous variable coded as percentage of female participants, (iii) sample age was examined as a continuous moderator by using the mean time in years, (iv) it was decided to code ethnicity as a categorical variable, either as < 75% White or ≥ 75% White, as this strategy minimized data exclusion, and (v) the methodological quality of each study was examined as a continuous moderator.
2.4. Computation and analysis of effect sizes
All analyses in this paper were carried out on SPSS (Version 15) using syntax specified in Field and Gillett (in press). A separate meta-analysis was carried out for each adjustment outcome. In the present study the correlation coefficient (r) was chosen as the effect size estimate for a number of reasons. First, this was a common metric for which the greatest number of effect sizes could be reported or converted; second, it is easily computed from either chi-square, t, F, and d; and third it is readily interpretable (Rosenthal & DiMatteo, 2001).
A number of papers reported correlation coefficients only for the subscales of PTG. Therefore to guarantee the independence assumption among effect sizes the coefficients were averaged to produce a single effect size associated with overall PTG. When a study did not report the effect size or probability value but stated only the relationship was nonsignificant an effect size of zero was assigned to that relationship. This is a conservative strategy because it generally underestimates the true magnitude of effect sizes (Durlak and Lipsey, 1991, Rosenthal, 1995). However, this approach is preferable to excluding nonsignificant results from the meta-analysis, because this would result in an overestimation of combined effect sizes (Rosenthal, 1995). The authors of these papers were contacted for further information and there was only one study where an effect size of zero assumed.2 In meta-analysis two common statistical procedures are used: fixed- and random-effect models (Hedges, 1992, Hedges and Vevea, 1998, Hunter and Schmidt, 2000, Hunter and Schmidt, 2000). Real social science data have been shown to contain variability in effect sizes as the norm, which indicates variable population parameters (Field, 2003, Field, 2005, Field and Gillet, in press, Hunter and Schmidt, 2000, Hunter and Schmidt, 2000). For this reason, and so the results can be generalized beyond the studies included in the meta-analysis, a random effects model was carried out. Hedges and Vevea's (1998) method was applied using Fisher-transformed correlation coefficients with results reported after the back transformation to the Pearson product–moment correlation coefficient (see Field, 2005, Overton, 1998). Using this method, each effect size is weighted by a value reflecting both the within study variance (1/n − 3 for correlation coefficients in which n is the sample size) and the between study variance (τ 2). The exact weight function for each effect size is (see Field & Gillet, in press for a guide to using Hedges and Vevea's method).
Moderator analyses were conducted also using a random-effects general linear model in which each z-transformed effect size can be predicted from the transformed moderator effect (represented by regression coefficient, β). The moderator effect, β, is estimated using generalised least squared (GLS). In both the main analysis and moderator analyses, between study variance was estimated noniteratively (e.g. Dersimonian & Laird, 1986). For a technical overview of the GLS moderator analysis that we employed see Overton, 1998, Field and Gillet, in press.
2.5. Publication bias
In any meta-analysis publication bias is a concern. This bias refers to the tendency that the decision to publish a paper is determined by the results of the study (Begg, 1994). For example studies with nonsignificant findings are less likely to be published than those with significant outcomes, which could result in a positive bias within the literature. There are different approaches to estimating publication bias: Rosenthal's (1979) fail-safe N, funnel plots and sensitivity analysis. The fail safe N estimates the number of unpublished, nonsignificant studies that would have to exist for the obtained probability value of the population effect size estimate to be rendered nonsignificant. This measure is problematic because its emphasis is on significance testing the population effect size rather than estimating the population effect size itself. Therefore, we have chosen to report measures that specifically address bias in the population effect size estimate. First, we produce funnel plots of the effect found in each study against the standard error (Light & Pillemer, 1984). An unbiased sample will show a cloud of data points that is symmetric around the population effect size and has the shape of a funnel (reflecting greater variability in effect sizes from studies with small sample sizes/less precision). Second, we performed a sensitivity analysis, which is a method that uses weights to model the process through which the likelihood of a study being published varies (usually based on a criterion such as the significance of a study). We applied the methods proposed by Vevea and Woods (2005) because they can be applied to relatively small samples of studies such as we have.
3. Results
3.1. Study characteristics
There were 38 studies included in the meta-analysis; with a total of 7927 participants. Sample sizes from individual studies ranged from 52 to 835. 78.0% of the studies focused on individuals with a cancer diagnosis and 21.1% included individuals with a HIV/AIDS diagnosis. Length of time since treatment/diagnosis varied and ranged from 0 to 108 months (M = 41.65, SD = 31.86). Mean age of the sample was 50.66 (SD = 9.9). Of the studies that provided information on ethnicity, the majority (n = 15) included samples predominantly composed of white participants.
3.2. Growth and adjustment
Table 2, Table 3, Table 4 graphically represent the effect sizes included in each adjustment meta-analysis by means of a stem and leaf plot. The stem identifies the first digit of an effect size and the leaf identifies the final digit of an effect size. For positive mental health (Table 2), the bulk of effect sizes were in the range of 0 to .26, but the range was quite wide (−.23 to .49) suggesting the influence of moderator variables. For negative mental health (Table 3), the distribution of effect sizes is relatively symmetrical and is centered around 0 to −.1. Again, the range of effect sizes was quite large (−.44 to .25) suggesting that moderator variables might usefully explain some of this variability. Finally, for physical health (Table 4) the effect size distribution looks skewed and is centered around 0 to −.07. Three studies appeared to have relatively large positive effect sizes that were inconsistent with the bulk of studies.
Table 2.
Stem and leaf plot of effect sizes for positive mental health (rs).
| Stem | Leaf |
|---|---|
| .4 | 4, 9 |
| .3 | 2 |
| .2 | 0, 3, 5, 5, 6 |
| .1 | 2 |
| .0 | 0, 3, 4, 4, 5, 9 |
| −.0 | 1, 9, 9 |
| −.1 | |
| −.2 | 3 |
Table 3.
Stem and leaf plot of effect sizes for negative mental health (rs).
| Stem | Leaf |
|---|---|
| .2 | 3, 4, 5, |
| .1 | 0, 1, 1, 3, 3, 4, 6, 6, |
| .0 | 0, 1, 2, 2, 2, 2, 3, 3, 4, 5, 5, 9, 9, 9 |
| −.0 | 1, 4, 4, 4, 5, 8, 9, 9 |
| −.1 | 0, 0, 1, 1, 1, 2, 2, 3, 3, 3, 7, 7, 9 |
| −.2 | 0, 0, 2, 3, 3, 4, 7, 7 |
| −.3 | 3, 4, 5, 6 |
| −.4 | 2, 4, |
Table 4.
Stem and leaf plot of effect sizes for subjective physical health (rs).
| Stem | Leaf |
|---|---|
| .6 | 4 |
| .5 | |
| .4 | 5, 7 |
| .3 | |
| .2 | 5 |
| .1 | 1, 4 |
| .0 | 0, 0, 4, 8, 9 |
| −.0 | 2, 1, 1, 7 |
| −.1 | 3, 7 |
Table 5 shows the individual meta-analyses for each adjustment outcome. PTG was significantly related to higher levels of positive psychological adjustment (PTG explained 1.7% of the variance), lower levels of negative psychological adjustment (PTG explained only 0.3% of the variance), and higher reported levels of physical health (PTG explained 1.4% of the variance). The results suggest considerable variation in effect sizes for the three adjustment outcomes, and it is therefore important to examine factors that moderate these relationships. The funnel plots shown in Fig. 2, Fig. 3, Fig. 4 suggest publication bias might be present in the data, as indicated by the non-funnel like and asymmetric distribution of data points around the estimated mean, typical of biased data sets. In particular, for positive mental health (Fig. 1) and physical health (Fig. 3), the data cloud is relatively sparse for small studies (the bottom part of the figure). This pattern is indicative of one-tailed publication bias (Vevea & Woods, 2005). For negative mental health (Fig. 2) the cloud is a little sparse around zero for small studies, which indicates two-tailed publication bias (Vevea & Woods, 2005). We calculated several publication-bias corrected estimates based on our interpretation of the funnel plots of the overall population effect sizes on positive mental health, negative mental health and physical health. We used Vevea and Woods' (2005) weight function model of publication bias to calculate population effect size estimates under different selection bias scenarios. Based on the funnel plots, for positive mental health and physical health we assumed moderate (MOT) or severe (SOT) one-tailed selection bias, and for negative mental health we assumed moderate (MTT) and severe (STT) two-tailed selection bias. The values corrected for selection bias were as follows: for positive mental adjustment, the original population estimate of .13 was reduced to .08 (MOT), −.40 (SOT); for negative mental adjustment, the original estimate of −.05 became −.05 (MTT) and −.04 (STT); for physical health the original estimate of .12 became .06 (MOT), −.47 (SOT). As such, the estimate of population effect size for negative mental health was unaffected by publication bias. If we assume moderate publication bias, then estimates for positive mental health and physical health were slightly reduced, but if severe publication bias is assumed then the estimates change quite dramatically. As such, our conclusions come with the caveat that if severe publication bias was, in reality, present in the literature then our conclusions would be quite different for positive mental health and physical health outcomes.
Table 5.
Meta-analysis results for each adjustment outcome.
| Adjustment | k | τ2 | Q | 95% confidence interval for r |
z | ||
|---|---|---|---|---|---|---|---|
| Lower | Mean | Upper | |||||
| Positive mental health | 19 | .027 | 119.04*** | .04 | .13 | .21 | 3.00 ⁎⁎ |
| Negative mental health | 60 | .029 | 360.58*** | −.10 | −.05 | −.01 | − 2.17 ⁎ |
| Subjective physical health | 17 | .053 | 219.51*** | .00 | .12 | .23 | 1.95 ⁎ |
k = number of effect sizes, Q = homogeneity statistic.
p < .05.
p < .01.
p < .001.
Fig. 2.
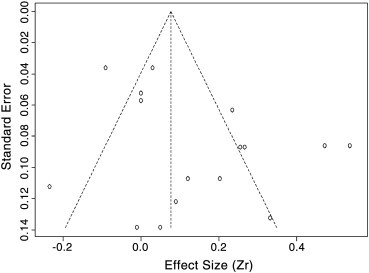
Funnel plot of positive mental health. The vertical line is the population effect size and the diagonal line displays the 95% confidence interval.
Fig. 3.
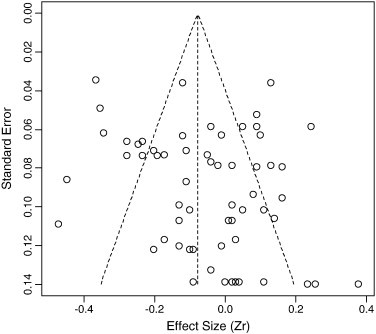
Funnel plot of negative mental health. The vertical line is the population effect size and the diagonal line displays the 95% confidence interval.
Fig. 4.

Funnel plot of subjective physical health. The vertical line is the population effect size and the diagonal line displays the 95% confidence interval.
3.3. Moderator analyses
Five moderators that might explain significant amounts of effect size variation for each adjustment outcome were examined. Subcategories of each adjustment outcome were also initially explored as moderators.
3.3.1. Positive mental health
Categories of positive psychological adjustment did not significantly moderate the relationship between PTG and positive mental health (p > .05). Time emerged as a significant moderator of positive psychological adjustment (β = .005, p < .001), implying the longer the time since the event, the stronger the relationship between PTG and positive mental health. The age of the sample emerged as a significant moderator (β = −.011, p < .01), indicating that samples with younger participants, showed a stronger relationship between PTG and positive adjustment. Ethnicity also moderated the relationship between PTG and positive mental health, χ 2 (1) = 4.77, p < .05, indicating that samples comprised of more than 25% non-white participants demonstrated a stronger relationship between PTG and positive psychological adjustment. Gender (β = .001, p > .05) and quality (β = .148, p > .05) did not significantly moderate the relationship between PTG and positive psychological adjustment.
3.3.2. Negative mental health
Categories of negative mental health moderated the relationship between PTG and negative psychological adjustment. Dummy coding revealed that PTSD symptoms had a stronger negative relationship with PTG in comparison to depression (χ 2 (1) = 4.29, p < .05), but not in comparison to anxiety (χ 2 (1) = 0.28, p > .05) and general distress (χ 2 (1) = 0.18, p > .05). Time since the health event, measured in months, moderated negative mental health (β = −.003, p < .01), indicating the shorter the time since the event, the stronger the relationship between PTG and negative adjustment. Ethnicity was also a significant moderator, χ 2 (1) = 34.16, p < .001, indicating that samples with more than a 75% white composition demonstrated a stronger negative relationship between PTG and negative adjustment. Age also appeared as a moderator (β = .009, p < .001), indicating that samples with older participants demonstrated a stronger negative relationship between PTG and negative adjustment. Quality of the study (β = .021, p > .05) and participant's gender (β = .001, p > .05) did not moderate the relationship between growth and negative mental health.
3.3.3. Subjective physical health
Categories of physical health did not significantly moderate the relationship between PTG and physical health (p > .05). Ethnicity moderated the relationship between PTG and physical health (χ 2 (1) = 4.75, p < .05), indicating that samples comprised of more than 25% non-white participants demonstrated a stronger relationship between PTG and physical health. Furthermore, time (β = .003, p > .05), gender (β = −.001, p > .05), age (β = .003, p > .05), and study quality (β = −.013, p = .05) did not significantly moderate the relationship between PTG and physical health.
4. Discussion
This meta-analytic review summarized the findings from 38 studies examining the association between PTG following cancer or HIV/AIDS and positive psychological adjustment, negative psychological adjustment, and subjective physical health. Despite variability in effect sizes this analysis demonstrated a small positive relationship between PTG and positive mental health. Therefore, individuals who perceive PTG following cancer or HIV/AIDS also report enhanced psychological well-being. Furthermore, a small negative relationship was found between PTG and negative mental health. Individuals who perceive PTG following cancer or HIV/AIDS also report reduced symptoms of negative mental health. Finally, PTG displayed a small positive relationship with measures of subjective physical health, implying that PTG may also confer some physical benefit. These findings suggest that PTG is associated with positive adaptive consequences, and is therefore an important construct to be studied in clinical and health research.
4.1. Summary of effect size moderators
An additional aim of the study was to examine factors that might moderate the relationship between PTG and adjustment, and therefore provide further insight by accounting for variability in effect sizes reported previously. Study quality and gender were the only variables that did not moderate the relationship between PTG and outcomes. Therefore the implications of these findings are that studies of differing quality do not account for differences in the growth–adjustment relationship and that there are no significant differences between men and women in the growth-outcome relationship. Other moderators examined had varying effects on relationships between PTG and different outcomes; each of which will be discussed in turn.
Subcategories of positive mental health, and subjective physical health did not significantly moderate their relationship with PTG. However, subcategories of negative mental health did moderate the growth-negative mental health relationship. Specifically, in comparison to depression, PTSD symptoms showed a stronger negative relationship with PTG.
Time since the illness emerged as a significant moderator for positive and negative mental health. In the short term, there was a stronger relationship between PTG and negative mental health, but over time there was an increased relationship between PTG and positive mental health. These results are consistent with the results from a previous meta-analysis looking at PTG following a range of traumas (Helgeson et al., 2006). Together these findings suggest that in the short-term PTG is influential in reducing negative symptoms, but in the long-term PTG is more instrumental in enhancing positive well-being. This is consistent with Tedeschi and Calhoun, 1995, Tedeschi and Calhoun, 2004 functional-descriptive model of PTG, which states that the management of emotional distress is essential in the initial stages post-trauma. On the other hand, PTG reported later might reflect more substantive life changes that have positive consequences for quality of life (Tomich & Helgeson, 2004). Time since the health event did not moderate the relationship between PTG and physical health.
Age appeared to differentially affect the relationship between PTG and adjustment. Younger adults demonstrated a stronger positive relationship between PTG and positive mental health. In comparison older adults displayed a stronger negative relationship between PTG and negative mental health. One explanation is that core beliefs of young people may be more affected than those of older people. For example younger people tend to view the world as less just and less benevolent, and the older groups tend to view the world as luckier and more controllable (Calhoun, Cann, Tedeschi, & McMillan, 1998). Being diagnosed with cancer or HIV/AIDS when young might shatter more natural and social rules or beliefs which would generate a greater possibility of reconstructing these core beliefs and therefore promote PTG. Another explanation might be that younger people may be more capable and adept at making changes to their lives, which results in enhanced well-being. Whereas, older participants may be dealing with other significant life events and be less adaptable compared with younger samples, and therefore PTG may be more useful in reducing and managing distress. Age did not act as a significant moderator between PTG and self-reported physical health.
Ethnicity was a significant moderator of the relationship PTG and all three adjustment measures. Specifically, non-white samples displayed a larger effect size for the relationship between PTG and positive mental health and also subjective physical health, compared to samples composed primarily of white participants. In comparison samples composed of predominantly white participants showed a stronger relationship between PTG and negative mental health. This variability may be explained by differences in culture e.g. family, religion, spirituality, which has shown to be important or associated with PTG following stressful life events (Shaw et al., 2005, Milam, 2006a, Tedeschi and Calhoun, 1995). Because of these differences, growth in ethnic minority samples may reflect more fundamental and existential changes resulting in enhanced well-being. In comparison, growth in predominantly white samples may be used more as a strategy to reduce distress.
4.2. Methodological issues
The results of this study should be interpreted with the following limitations in mind. Though the present findings indicate that PTG and positive mental health, negative mental health, and subjective physical health are associated (albeit modestly), only cross-sectional data were included in the analysis, which constrains causal inference. For example it is not clear if PTG leads to better psychological and physical health, or if these factors result in an enhanced perception of PTG. Furthermore, even though studies were included in the analysis only if they used a clear measure of PTG the final data set consisted of studies that used varying conceptions of PTG, which could be problematic. For example, past research has indicated that benefit finding and PTG are related but distinct constructs, and might therefore have unique predictors and outcomes (Sears et al., 2003). Therefore, future research in the area should ascertain if such constructs are theoretically and empirically interchangeable.
The present study did not examine type of illness as a moderator because there were not enough studies of HIV/AIDS to include cancer vs. HIV/AIDS as a moderator variable. Although research suggests that people with HIV/AIDS report similar levels and areas of PTG compared to individuals with cancer, there are unique differences between the illnesses, particularly in social responses to individuals with HIV/AIDS compared to those with cancer (Lechner & Weaver, 2009). For example HIV/AIDS is an infectious disease and people who are HIV positive may face more stigma because of fear, lack of knowledge concerning transmission, and greater perceived accountability (Lechner & Weaver, 2009). This may hinder opportunities for emotional processing and therefore may not facilitate PTG and positive adjustment as readily as cancer and other illnesses.
Furthermore, meta-analysis, like any other procedure, has its advantages and disadvantages, and this study is no exception. First, where authors of papers reported significant findings but did not include enough statistical information to calculate the effect size, these effect sizes were coded as zero. This is a conservative approach and therefore may have lowered the effect size estimate for each meta-analysis conducted. Second, as with many meta-analytic studies, the current findings may over represent those studies that are published and have significant results, preventing the generalization of the current findings to unpublished reports (Rosenthal, 1979). For the overall effects, our publication bias analysis showed that the population effect size estimates were relatively unaffected when corrected for moderate selection bias. This finding gives us some confidence that the results are not idiosyncratic to our sample of studies. However, when correcting for severe publication bias the effect of growth on positive mental adjustment and physical health became strongly negative (the opposite direction to the population effects). Although this is a correction for severe publication bias, the current findings should be viewed within the context of these results.
4.3. Theoretical and clinical implications
Despite these limitations, this study has significant implications for research and practice. A weakness in the literature is the lack of consensus between theorists as to whether PTG is best conceptualized as an adaptive coping strategy that people use following a challenging life event, or as an outcome of the struggle with a traumatic event (Affleck and Tennen, 1996, Park and Helgeson, 2006, Tedeschi and Calhoun, 1995, Tedeschi and Calhoun, 2004). The findings from this study suggest that shortly after the event PTG may be used as a coping strategy to manage and reduce emotional distress associated with the illness threat. However over time PTG grows and is more significant in enhancing positive well-being. This implies that adjustment to serious illness is an ongoing process that occurs over time (Helgeson et al., 2006, Bellizzi, 2004). As recognized by Butler (2007) a challenge of future work is to psychometrically separate these processes so they can be reliably investigated.
The results suggest that PTG is associated with a reduction in negative mental health, which was particularly prominent when PTSD symptoms were the outcome. This supports Joseph and Linley's (2005, 2008) conceptualization of how PTG and PTSD relate to each other. Traumatic events are thought to shatter assumptions about the self and the world and lead to the symptoms of PTSD. These experiences of reexperiencing, avoidance and arousal are viewed as the cognitive emotional processing of the new trauma related information as individuals search for new meaning in life (Joseph & Linley, 2008). As these new meanings are found, and the person's view of themselves and the world is reconstructed, PTG should occur and symptoms of distress should decrease. Therefore PTG should be predictive of lower distress, because as people find new meaning they can overcome the cognitive disruption and confusion characterized by PTSD (Joseph & Linley, 2005). Support for this has been reported by Frazier, Conlon and Glaser (2001) who found that among sexual assault survivors who reported PTG over 12 months were the least distressed.
However, Joseph and Linley (2006) note that this does not mean to imply that the alleviation of distress should automatically lead to the enhancement of growth. According to their Organismic Valuing Theory of growth, PTG should only relate to reduced distress through accommodation (i.e., changing one's global meaning to incorporate the stressor) as opposed to assimilation (i.e., changing one's view of the stressor so that it is consistent with one's global meaning). As such they caution that therapeutic work may impede or disrupt the cognitive processes that are necessary for accommodation and therefore PTG.
Nonetheless these findings suggest PTG may be a useful target for therapeutic intervention in health care and clinical settings, where the aim is long-term emotional and physical adjustment. Psychotherapy for traumatic events such as a serious illness has predominantly focused on the negative effects of trauma, and the goal of therapeutic intervention to promote growth as opposed to alleviate distress will be a major paradigm shift. It is therefore important to raise clinician's awareness of the possibility of positive change. For example, clinicians might recognize the patient's struggle to understand the impact of the illness not only as a posttraumatic response but also as a potential precursor to growth (Zoellner & Maercker, 2006).
The empirical study of ways to facilitate PTG is in its infancy and only a few intervention studies have included PTG as an endpoint (Antoni et al., 2001, 2006; Penedo et al., 2006). Nonetheless some interventions, which contain techniques aimed at promoting growth, have shown to successfully improve outcomes. For example Antoni et al. (2001) found that a psychosocial intervention that taught participants broad cognitive behavioural stress management techniques, served to increase reports of perceived benefits from having had breast cancer, and simultaneously reduced levels of depression. This study demonstrates that PTG can be altered and can be incorporated easily within cognitive behavioural stress-management interventions. However, the findings from the meta-analysis suggest that clinicians should be sensitive to the timing of PTG discussions. For example the present analysis suggests that PTG might be a useful target in the short-term to reduce distress, but in order to enhance well-being PTG should be targeted later on in the adjustment process.
However, in agreement with Park and Helgeson (2006) it is cautioned that large scale interventions to facilitate PTG in cancer and HIV/AIDS patients should be avoided until researchers understand more about the origins of PTG, the conditions under which PTG is verdical, the best methods to assess PTG, and its relations to psychological and physical health, are fully understood. Care should also be taken to avoid imposing an expectation of PTG in the face of serious illness. Patients with cancer or HIV/AIDS often report feeling burdened with the pressure to stay positive and encouraging the identification of positive changes from their illness may be potentially offensive to patients, serve to minimise their experience and lead them to suppress reports of distress (Bellizzi and Blank, 2006, Cordova, 2008).
4.4. Future research
This meta-analysis of growth in cancer and HIV/AIDS patients illustrates the promising and exciting nature of this area of research. However, the review also indicates much remains to be learned and highlights areas of research where future work is needed. The present study indicates that in the short term, PTG is associated with a reduction in negative mental health, whereas over longer term, PTG is associated with an enhancement in positive well-being. Therefore a clear point of focus is the use of longitudinal studies to further disentangle and clarify the temporal course of this relationship. Experimental designs, such as the interventions described earlier, will also help to reveal the causal role of PTG in adjustment and to isolate mechanisms responsible for the effects (Algoe & Stanton, 2009).
Many of the conclusions reached in this paper regarding moderators of the growth–adjustment relationship are based on theoretical considerations rather than on direct empirical evidence and future studies should attempt to validate and test these hypotheses. Moreover, to further explicate the growth–adjustment relationship studies should continue to identify additional mediators and moderators. A particularly relevant moderator to medical populations that should be investigated is the perception of the severity of an illness. A previous meta-analysis found that perceptions of the severity of a traumatic event are related to PTG (Helgeson et al., 2006). As such it might be expected that PTG may have a stronger relationship with psychological well-being and physical health for more subjectively severe illnesses and caution must therefore be taken when generalizing the current findings to less threatening illnesses characteristics and indeed wider trauma populations.
The majority of the studies included in the present paper measured PTG so that only positive changes were assessed. This could be problematic because participants may develop a ‘response bias’ which may lead individuals to over-report PTG, and it may also restrict our characterisation of the life changes that health events may precipitate (Tomich & Helgeson, 2004). Furthermore, a recent prospective study of severe acute respiratory syndrome (Cheng, Wong, & Tsang, 2006) found that positive associations between PTG and positive well-being are more likely to be found among individuals who perceive benefits from the event, as well as the costs. Therefore, examining positive and negative change simultaneously should be considered as a focus of future research investigating PTG and adjustment in health samples.
Particularly pertinent for this population is the possibility that PTG can serve to improve physical health. Although this paper only looked at subjective measures of physical health there is promising preliminary data which suggests that PTG may be related to better physiological functioning. For example Cruess et al. (2000) found that among women with breast cancer, cognitive behavioural stress management reduced levels of cortisol through the enhancement of PTG. Yet, no studies have addressed possible mechanisms for the relationship between PTG and physical health. A recent model proposed by Bower, Low, Moskowitz, Sepah, and Epel (2008) suggests that factors often associated with growth such as coping, positive affect and improved relationships, can lead to a state of enhanced allostasis (maintaining stability, or homeostasis, through change, Sterling & Eyer, 1988), which buffers against future stress responses. This is a promising model, which merits increased attention in future research. Furthermore, the relationship between PTG and health behaviours such as exercise, medication adherence, requires a more detailed examination; particularly regarding how these behaviours might moderate the relationship between PTG and physical health.
Finally, it is acknowledged that the ways in which PTG is manifested might contain elements that are distinctive to specific cultural environments (Calhoun & Tedeschi, 2006). This paper included only three studies conducted in non-Western countries and therefore it is clear that there is a need to examine PTG in more diverse ethnic and cultural groups to fully understand the relationship between growth and adjustment.
4.5. Summary and conclusions
On the basis of this meta-analysis it can be concluded that PTG following cancer or HIV/AIDS is related to better positive mental health and self-reported physical health, and less negative mental health. This does not preclude that many individuals might experience distress, but rather that PTG is a worthy phenomenon to be studied in clinical and health research. It is hoped that this meta-analysis will encourage further examination of the caveats addressed in this research, so that in the future PTG can perhaps become a viable therapeutic aim in individuals living with a life-threatening illness.
Footnotes
The authors of the following studies who did not report the results of analyses testing the relationship between growth and adjustment were generous enough to provide this information when contacted: Ickovics et al., 2006a, *Ickovics et al., 2006b, McGrath and Joseph, 2006, Powell et al., 2007, Tallman et al., 2007, *Tomich and Helgeson, 2004, *Yanez et al., 2009.
The analysis (PTG and positive mental health) was re-run without this study and the results remained unchanged.
References
- Affleck G., Tennen H. Construing benefits from adversity: Adaptational significance and dispositional underpinnings. Journal of Personality. 1996;64:900–922. doi: 10.1111/j.1467-6494.1996.tb00948.x. [DOI] [PubMed] [Google Scholar]
- Algoe S., Stanton L. Is benefit finding good for individuals with chronic disease? In: Park C., Lechner S., Antoni M., Stanton A., editors. Medical illness and positive life change: Can crisis lead to personal life transformation? American Psychological Association; Washington DC: 2009. pp. 185–206. [Google Scholar]
- American Psychiatric Association . 4th ed. American Psychiatric Association; Washington, D.C.: 1994. Diagnostic and Statistic Manual of Mental Disorders. [Google Scholar]
- Antoni M., Lehman J., Kilbourn K., Boyers A., Culver J., Alferi S. Cognitive-behavioural stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early stage breast cancer. Health Psychology. 2001:20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- Barakat L., Alderfer M., Kazak A. Posttraumatic growth in adolescent survivors of cancer and their mothers and fathers. Journal of Pediatric Psychology. 2006;31:413–419. doi: 10.1093/jpepsy/jsj058. [DOI] [PubMed] [Google Scholar]
- Begg C.B. Publication bias. In: Cooper H., Hedges L.V., editors. The Handbook of Research Synthesis. Russell Sage Foundation; New York: 1994. pp. 399–409. [Google Scholar]
- Bellizzi K. Expressions of generativity and posttraumatic growth in adult cancer survivors. International Journal of Aging and Human Development. 2004;58:267–287. doi: 10.2190/DC07-CPVW-4UVE-5GK0. [DOI] [PubMed] [Google Scholar]
- Bellizzi K., Blank T. Predicting posttraumatic growth in breast cancer survivors. Health Psychology. 2006;25:47–56. doi: 10.1037/0278-6133.25.1.47. [DOI] [PubMed] [Google Scholar]
- Bellizzi et al., 2007.Bellizzi K., Miller M., Arora N., Rowland J. Positive and negative life changes experienced by survivors of Non-Hodgkins Lymphona. Annals of Behavioral Medicine. 2007;34:188–199. doi: 10.1007/BF02872673. [DOI] [PubMed] [Google Scholar]
- Botha K. Posttraumatic stress disorder and illness behaviour in HIV+ patients. Psychological Reports. 1996;79:843–845. doi: 10.2466/pr0.1996.79.3.843. [DOI] [PubMed] [Google Scholar]
- Bower J., Low C., Moskowitz J., Sepah S., Epel E. Benefit finding and physical health: Positive psychological changes and enhanced allostasis. Social and Personality Psychology Compass. 2008;2:223–244. [Google Scholar]
- Bower et al., 2005.Bower J., Meyerowitz B., Desmond K., Bernaards C., Rowland J., Ganz P. Perceptions of positive meaning and vulnerability following breast cancer: Predictors and outcomes among long-term breast cancer survivors. Annals of Behavioral Medicine. 2005;29:236–245. doi: 10.1207/s15324796abm2903_10. [DOI] [PubMed] [Google Scholar]
- Butler L. Growing pains: Commentary of the field of posttraumatic growth and Hobfoll and colleagues recent contribution to it. Applied Psychology: An International Review. 2007;56:367–378. [Google Scholar]
- Calhoun L., Cann A., Tedeschi R., McMillan J. Traumatic events and generational differences in assumptions about a just world. Journal of Social Psychology. 1998;138:789–791. doi: 10.1080/00224549809603265. [DOI] [PubMed] [Google Scholar]
- Calhoun L., Tedeschi R. Foundations of posttraumatic growth. In: Calhoun L.G., Tedeschi R.G., editors. Handbook of posttraumatic growth: Research and practice. Erlbaum Associates; Mahwah, NJ: 2006. pp. 138–175. [Google Scholar]
- Carrico et al., 2006.Carrico A., Ironson G., Antoni M., Lechner S., Durán R., Kumar M. A path model of the effects of spirituality on depressive symptoms and 24-h urinary-free cortisol in HIV-positive persons. Journal of Psychosomatic Research. 2006;61:51–58. doi: 10.1016/j.jpsychores.2006.04.005. [DOI] [PubMed] [Google Scholar]
- Cheng C., Wong W., Tsang K. Perception of benefits and costs during SARS outbreak: An 18 month prospective study. Journal of Consulting and Clinical Psychology. 2006;74:870–879. doi: 10.1037/0022-006X.74.5.870. [DOI] [PubMed] [Google Scholar]
- Christopher M. A broader view of trauma: A bio-psychosocial evolutionary view of the role of the traumatic stress response in the emergence of pathology and/or growth. Clinical Psychology Review. 2004;24:75–98. doi: 10.1016/j.cpr.2003.12.003. [DOI] [PubMed] [Google Scholar]
- Cole et al., 2008.Cole B., Hopkins C., Tisak J., Steel J., Carr B. Assessing spiritual growth and spiritual decline following a diagnosis of cancer: Reliability and validity of the spiritual transformation scale. Psycho-Oncology. 2008;17:112–121. doi: 10.1002/pon.1207. [DOI] [PubMed] [Google Scholar]
- Collins R., Taylor S., Skokan L. A better world or a shattered vision? Changes in life perspectives following victimization. Social Cognition. 1990;8:263–285. [Google Scholar]
- Cordova M. Facilitating posttraumatic growth following cancer. In: Joseph S., Linley P.A., editors. Trauma, recovery and growth: Positive psychological perspectives on posttraumatic stress. John Wiley & Sons; Hoboken NJ: 2008. pp. 185–206. [Google Scholar]
- Cordova M., Cunningham L., Carlson C., Andrykowski M. Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychology. 2001;20:176–185. [PubMed] [Google Scholar]
- Cordova et al., 2007.Cordova M., Giese-Davis J., Golant M., Kronenwetter C., Chang V., Spiegel D. Breast cancer as trauma: Posttraumatic stress and posttraumatic growth. Journal of Clinical Psychology in Medical Settings. 2007;14:308–319. [Google Scholar]
- Cruess D.G., Antoni M.H., McGregor B.A., Kilbourn K.M., Boyers A.E., Alferi S.M. Cognitive behavioural stress management reduces serum cortisol by enhancing benefit finding among women being treated for early stage breast cancer. Psychosomatic Medicine. 2000;62:304–308. doi: 10.1097/00006842-200005000-00002. [DOI] [PubMed] [Google Scholar]
- Curbow et al., 1993.Curbow B., Somerfield M., Baker F., Wingard J., Legro M. Personal changes, dispositional optimism, and psychological adjustment to bone marrow transplantation. Journal of Behavioral Medicine. 1993;16:423–443. doi: 10.1007/BF00844815. [DOI] [PubMed] [Google Scholar]
- Dersimonian R., Laird N. Meta-analysis in clinical-trials. Controlled Clinical Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Durlak J.A., Lipsey M.W. A practitioner's guide to meta-analysis. American Journal of Community Psychology. 1991;19:291–332. doi: 10.1007/BF00938026. [DOI] [PubMed] [Google Scholar]
- Field A.P. The problem in using fixed-effects models of meta-analysis on real-world data. Understanding Statistics. 2003;2:77–96. [Google Scholar]
- Field A.P. Is the meta-analysis of correlation coefficients accurate when population effect sizes vary? Psychological Methods. 2005;10(4):444–467. doi: 10.1037/1082-989X.10.4.444. [DOI] [PubMed] [Google Scholar]
- Field, A. P. & Gillet, R. (in press). How to do a meta-analysis. British Journal of Mathematical and Statistical Psychology.
- Frazier P., Conlon A., Glaser T. Positive and negative life changes following sexual assault. Journal of Consulting and Clinical Psychology. 2001;69:1048–1055. doi: 10.1037//0022-006x.69.6.1048. [DOI] [PubMed] [Google Scholar]
- Fromm K., Andrykowski M., Hunt J. Positive and negative psychosocial sequelae of bone marrow transplantation: Implication for quality of life assessment. Journal of Behavioral Medicine. 1996;19:221–240. doi: 10.1007/BF01857767. [DOI] [PubMed] [Google Scholar]
- Harrington et al., 2008.Harrington S., McGurk M., Llewellyn C.D. Positive consequences of head and neck cancer. Journal of Psychosocial Oncology. 2008;26:43–62. doi: 10.1080/07347330802115848. [DOI] [PubMed] [Google Scholar]
- Hedges L.V. Meta-analysis. Journal of Educational Statistics. 1992;17:279–296. [Google Scholar]
- Hedges L.V., Vevea J.L. Fixed- and random-effects models in meta-analysis. Psychological Methods. 1998;3:486–504. [Google Scholar]
- Helgeson V., Reynolds K., Tomich P. A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology. 2006;74:797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Ho S., Chan C., Ho R. Posttraumatic growth in Chinese cancer survivors. Psycho-Oncology. 2004;13:377–389. doi: 10.1002/pon.758. [DOI] [PubMed] [Google Scholar]
- Horowitz M. Aronson; New York: 1986. Stress response syndromes. [Google Scholar]
- Hunter J.E., Schmidt F.L. Fixed effects vs. random effects meta-analysis models: Implications for cumulative research knowledge. International Journal of Selection and Assessment. 2000;8:275–292. [Google Scholar]
- Ickovics J., Meade C., Kershaw T., Milam S., Lewis J., Ethier K. Urban teens: Trauma, posttraumatic growth, and emotional distress among female adolescents. Journal of Consulting and Clinical Psychology. 2006;74:841–850. doi: 10.1037/0022-006X.74.5.841. [DOI] [PubMed] [Google Scholar]
- Ickovics et al., 2006b.Ickovics J., Milan S., Boland, Schoenbaum E., Schuman P., Vlahov D. Psychological resources preotect health: 5-year survival and immune function among HIV-infected women from four US cities. AIDS. 2006;20:1851–1860. doi: 10.1097/01.aids.0000244204.95758.15. [DOI] [PubMed] [Google Scholar]
- Jaarsma et al., 2006.Jaarsma T., Pool G., Sanderman R., Ranchor A. Psychometric properties of the Dutch version of the posttraumatic growth inventory among cancer patients. Psycho-Oncology. 2006;15:911–920. doi: 10.1002/pon.1026. [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R. Posttraumatic growth: Three explanatory models. Psychological Inquiry. 2004;15:30–34. [Google Scholar]
- Joseph S., Linley P.A. Positive adjustment to threatening events: An organismic valuing theory of growth through adversity. Review of General Psychology. 2005;9:262–280. [Google Scholar]
- Joseph S., Linley P.A. Growth following adversity: Theoretical perspectives and implications for clinical practice. Clinical Psychology Review. 2006;26:1041–1053. doi: 10.1016/j.cpr.2005.12.006. [DOI] [PubMed] [Google Scholar]
- Joseph S., Linley P.A. Wiley; Hoeboken: 2008. Trauma, recovery, and growth: positive psychological perspectives on posttraumatic stress. [Google Scholar]
- Kangas M., Henry J.L., Bryant R.A. Posttraumatic stress disorder following cancer: A conceptual and clinical review. Clinical Psychology Review. 2002;22:499–524. doi: 10.1016/s0272-7358(01)00118-0. [DOI] [PubMed] [Google Scholar]
- Katz et al., 2001.Katz R., Flasher L., Cacciapaglia H., Nelson S. The psychosocial impact of cancer and lupus: A cross validation study that extends the generality of “benefit finding” in cancer patients with chronic disease. Journal of Behavioral Medicine. 2001;24:561–571. doi: 10.1023/a:1012939310459. [DOI] [PubMed] [Google Scholar]
- Kelly B., Raphael B., Judd F., Perdices M., Kernutt G., Burnett P. Posttraumatic stress disorder in response to HIV infection. General Hospital Psychiatry. 1998;10:345–352. doi: 10.1016/s0163-8343(98)00042-5. [DOI] [PubMed] [Google Scholar]
- Kinsinger et al., 2006.Kinsinger D., Penedo F., Antoni M., Dahn J., Lechner S., Schneiderman N. Psychosocial and sociodemographic correlates of benefit-finding in men treated for localised prostate cancer. Psycho-Oncology. 2006;15:954–961. doi: 10.1002/pon.1028. [DOI] [PubMed] [Google Scholar]
- Klauer et al., 1998.Klauer T., Ferring D., Filipp S.-H. Still stable after all this…? Temporal comparison in coping with severe and chronic disease. International Journal of Behavioral Development. 1998;22:339–355. [Google Scholar]
- Lechner S., Antoni M. Posttraumatic growth and group-based interventions for persons dealing with cancer: What have we learned so far? Psychological Inquiry. 2004;15:35–41. [Google Scholar]
- Lechner S., Weaver K. Lessons learned about benefit finding among individuals with cancer or HIV/AIDS. In: Park C., Lechner S., Antoni M., Stanton A., editors. Medical illness and positive life change: Can crisis lead to personal life transformation? Washington DC; American Psychological Association: 2009. pp. 185–206. [Google Scholar]
- Light R.J., Pillemer D.B. Harvard University Press; Cambridge, MA: 1984. Summing up: The science of reviewing research. [Google Scholar]
- Linley P.A. Positive adaptation to trauma: Wisdom as both process and outcome. Journal of Traumatic Stress. 2003;16:601–610. doi: 10.1023/B:JOTS.0000004086.64509.09. [DOI] [PubMed] [Google Scholar]
- Linley P.A., Joseph S. Positive change following trauma and adversity: A review. Journal of Traumatic Stress. 2004;17:11–21. doi: 10.1023/B:JOTS.0000014671.27856.7e. [DOI] [PubMed] [Google Scholar]
- Littlewood et al., 2008.Littlewood R., Vanable P., Carey M., Blair D. The association of benefit finding to psychosocial and behaviour adaptation among HIV+ men and women. Journal of Behavioral Medicine. 2008;31:145–155. doi: 10.1007/s10865-007-9142-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luszczynska et al., 2007.Luszczynska A., Sarkar Y., Knoll N. Received social support, self-efficacy, and finding benefits in disease as predictors of physical functioning and adherence to antiretroviral therapy. Patient Education and Counseling. 2007;66:37–42. doi: 10.1016/j.pec.2006.10.002. [DOI] [PubMed] [Google Scholar]
- Martinez A., Israelski D., Walker C., Koopman C. Posttraumatic stress disorder in women attending human immunodeficiency virus outpatient clinics. AIDS Patient Care and STDs. 2002;16:283–291. doi: 10.1089/10872910260066714. [DOI] [PubMed] [Google Scholar]
- McGrath J.C., Linley P.A. Post-traumatic growth in acquired brain injury: A preliminary small scale study. Brain Injury. 2006;20:767–773. doi: 10.1080/02699050600664566. [DOI] [PubMed] [Google Scholar]
- Milam, 2004.Milam J. Posttraumatic growth among HIV/AIDS patients. Journal of Applied Social Psychology. 2004;34:2353–2376. [Google Scholar]
- Milam J. Positive changes attributed to the challenge of HIV/AIDS. In: Calhoun L.G., Tedeschi R.G., editors. Handbook of posttraumatic growth: Research and practice. Erlbaum; Mahwah, NJ: 2006. pp. 214–224. [Google Scholar]
- Milam, 2006b.Milam J. Posttraumatic growth and HIV disease progression. Journal of Consulting and Clinical Psychology. 2006;74:817–827. doi: 10.1037/0022-006X.74.5.817. [DOI] [PubMed] [Google Scholar]
- Milam J., Ritt-Olsen A., Unger J. Posttraumatic growth among adolescents. Journal of Adolescent Research. 2004;19:192–204. [Google Scholar]
- Mirza R., Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: Systematic review. British Medical Journal. 2004;328:794–797. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D., Dick L., Russo D., Pinn J., Boudewyn A., Likosky W. The psychosocial impact of multiple sclerosis: Exploring the patient's perspective. Health Psychology. 1990;18:376–382. doi: 10.1037//0278-6133.18.4.376. [DOI] [PubMed] [Google Scholar]
- Mols et al., 2009.Mols F., Vingerhoets A.J.J.M., Coebergh J.W.W., Poll-Franse L.V. Well-being, posttraumatic growth and benefit finding in long-term breast cancer survivors. Psychology and Health. 2009;24:583–595. doi: 10.1080/08870440701671362. [DOI] [PubMed] [Google Scholar]
- Morrill et al., 2008.Morrill E., Brewer N., O'Neil S., Lillie S., Dees C., Carey L. The interaction of post-traumatic growth and post-traumatic stress symptoms in predicting depressive symptoms and quality of life. Psycho-Oncology. 2008;17:948–953. doi: 10.1002/pon.1313. [DOI] [PubMed] [Google Scholar]
- Mystakidou et al., 2007.Mystakidou K., Parpa E., Tsilika E., Pathiaki M., Galanos A., Vlahos L. Traumatic distress and positive changes in advanced cancer patients. American Journal of Hospice & Palliative Medicine. 2007;24:270–276. doi: 10.1177/1049909107299917. [DOI] [PubMed] [Google Scholar]
- Mystakidou et al., 2007.Mystakidou K., Tsilika E., Parpa E., Kyriakopoulos D., Malamos N., Damigos D. Personal growth and psychological distress in advanced breast cancer. The Breast. 2007;17:382–386. doi: 10.1016/j.breast.2008.01.006. [DOI] [PubMed] [Google Scholar]
- O'Leary V., Ickovics J. Resilience and thriving in response to challenge: An opportunity for a paradigm shift in women's health. Women's Health: Research on Gender, Behavior, and Policy. 1995;1:121–142. [PubMed] [Google Scholar]
- Overton R.C. A comparison of fixed-effects and mixed (random-effects) models for meta-analysis tests of moderator variable effects. Psychological Methods. 1998;3(3):354–379. [Google Scholar]
- Park et al., 2008.Park C., Edmondson D., Fenster J., Blank T. Meaning making and psychological adjustment following cancer: The mediating roles of growth, life meaning and restored just-world beliefs. Journal of Consulting and Clinical Psychology. 2008;76:863–875. doi: 10.1037/a0013348. [DOI] [PubMed] [Google Scholar]
- Park C., Helgeson V. Introduction to the Special Section: Growth following highly stressful life events — Current status and future directions. Journal of Consulting and Clinical Psychology. 2006;74:791–796. doi: 10.1037/0022-006X.74.5.791. [DOI] [PubMed] [Google Scholar]
- Park C., Lechner S. Measurement issues in assessing growth following stressful life experiences. In: Calhoun L.G., Tedeschi R.G., editors. Handbook of posttraumatic growth: Research and Practice. Erlbaum; Mahwah, NJ: 2006. pp. 47–67. [Google Scholar]
- Penedo F.J., Molton I., Dahn J.R., Shen B.J., Kinsinger D., Traeger L. A randomized controlled trial of group-based cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine. 2006;31:261–270. doi: 10.1207/s15324796abm3103_8. [DOI] [PubMed] [Google Scholar]
- Petrie et al., 1999.Petrie K., Buick D., Weinman J., Booth R. Positive effects of illness reported by myocardial infarction and breast cancer patients. Journal of Psychosomatic Research. 1999;47:537–543. doi: 10.1016/s0022-3999(99)00054-9. [DOI] [PubMed] [Google Scholar]
- Powell T., Ekin-Wood A., Collin C. Post-traumatic growth after head injury: A long-term follow-up. Brain Injury. 2007;21:31–38. doi: 10.1080/02699050601106245. [DOI] [PubMed] [Google Scholar]
- Rieker P., Edbril S., Garnick M. Curative testis cancer therapy: Psychosocial sequelae. Journal of Clinical Oncology. 1985;3:1117–1126. doi: 10.1200/JCO.1985.3.8.1117. [DOI] [PubMed] [Google Scholar]
- Rosenthal R. The ‘File Drawer Problem’ and tolerance for null results. Psychological Bulletin. 1979;86:638–641. [Google Scholar]
- Rosenthal R. Writing meta-analytic reviews. Psychological Bulletin. 1995;118:183–192. [Google Scholar]
- Rosenthal R., DiMatteo M.R. Meta-analysis: Recent developments in quantitative methods for literature reviews. Annual Review of Psychology. 2001;52:59–82. doi: 10.1146/annurev.psych.52.1.59. [DOI] [PubMed] [Google Scholar]
- Salmon et al., 1996.Salmon P., Manzi F., Valori R.M. Measuring the meaning of life for patients with incurable cancer: The Life Evaluation Questionnaire (LEQ) European Journal of Cancer. 1996;5:755–760. doi: 10.1016/0959-8049(95)00643-5. [DOI] [PubMed] [Google Scholar]
- Salsman et al., 2009.Salsman J.M., Segerstorm S.C., Brechting E.H., Carlson C.R., Andrykowski M.A. Posttraumatic growth and PTSD symptomatology among colorectal cancer survivors: A 3 month longitudinal examination of cognitive processing. Psycho-Oncology. 2009;18:30–41. doi: 10.1002/pon.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroevers and Teo, 2008.Schroevers M.J., Teo I. The report of posttraumatic growth in Malaysian cancer patients: Relationships with psychological distress and coping strategies. Psycho-Oncology. 2008;17:1239–1246. doi: 10.1002/pon.1366. [DOI] [PubMed] [Google Scholar]
- Schulz and Mohamed, 2005.Schulz U., Mohamed N. Turning the tide: Benefit finding after cancer surgery. Social Science and Medicine. 2005;59:653–662. doi: 10.1016/j.socscimed.2003.11.019. [DOI] [PubMed] [Google Scholar]
- Schwarzer et al., 2006.Schwarzer R., Luszczynska A., Boehmer S., Taubert S., Knoll N. Changes in finding benefit after cancer surgery and the prediction of well-being one year later. Social Science and Medicine. 2006;63:1614–1624. doi: 10.1016/j.socscimed.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Sears et al., 2003.Sears S., Stanton A., Danoff-Burg S. The yellow brick road and the emerald city: Benefit-finding, positive reappraisal coping, and posttraumatic growth in women with early-stage breast cancer. Health Psychology. 2003;22:487–496. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- Shaw A., Joseph S., Linley A. Religion, spirituality, and posttraumatic growth. Mental Health, Religion, & Culture. 2005;8:1–11. [Google Scholar]
- Siegel K., Schrimshaw E. Perceiving benefits in adversity: Stress-related growth in women living with HIV/AIDS. Social Science and Medicine. 2000;51:1543–1554. doi: 10.1016/s0277-9536(00)00144-1. [DOI] [PubMed] [Google Scholar]
- Siegel et al., 2005.'Siegel K., Scrimshaw E., Pretter S. Stress-related growth among women living with HIV/AIDS: Examination of an exploratory model. Journal of Behavioral Medicine. 2005;28:403–414. doi: 10.1007/s10865-005-9015-6. [DOI] [PubMed] [Google Scholar]
- Sterling P., Eyer J. Allostasis: A new paradigm to explain arousal pathology. In: Fisher S., Reason J., editors. Handbook of Life Stress, Cognition and Health. John Wiley & Sons; New York: 1988. pp. 629–649. [Google Scholar]
- Tallman B.A., Altmaier E., Garcia C. Finding Benefit From Cancer. Journal of Counseling Psychology. 2007;54:481–487. [Google Scholar]
- Tedeschi R., Calhoun L. Sage Publications; Thousand Oaks, CA: 1995. Trauma and transformation: Growing in the aftermath of suffering. [Google Scholar]
- Tedeschi R., Calhoun L. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004;15:1–18. [Google Scholar]
- Tedeschi R., Park C., Calhoun L. Erlbaum; Mahwah, NJ: 1998. Posttraumatic growth: Positive changes in the aftermath of crisis. [Google Scholar]
- Thornton and Perez, 2006.Thornton A., Perez M. Posttraumatic growth in prostate cancer survivors and their partners. Psycho-Oncology. 2006;15:285–296. doi: 10.1002/pon.953. [DOI] [PubMed] [Google Scholar]
- Tomich and Helgeson, 2004.Tomich P., Helgeson V. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychology. 2004;23:16–23. doi: 10.1037/0278-6133.23.1.16. [DOI] [PubMed] [Google Scholar]
- Updegraff et al., 2002.Updegraff J., Taylor S., Kemeny M., Wyatt G. Positive and negative effects of HIV-infection in women in low socioeconomic resources. Personality and Social Psychology Bulletin. 2002;28:382–394. [Google Scholar]
- Urcuyo et al., 2005.Urcuyo K., Boyers A., Carver C., Antoni M. Finding benefit in breast cancer: Relations with personality, coping, and concurrent well-being. Psychology and Health. 2005;20:175–192. [Google Scholar]
- Vevea J.L., Woods C.M. Publication bias in research synthesis: Sensitivity analysis using a priori weight functions. Psychological Methods. 2005;10:428–443. doi: 10.1037/1082-989X.10.4.428. [DOI] [PubMed] [Google Scholar]
- Widows et al., 2005.Widows M., Jacobsen P., Booth-Jones M., Fields K. Predictors of posttraumatic growth following bone marrow transplantation for cancer. Health Psychology. 2005;24:266–273. doi: 10.1037/0278-6133.24.3.266. [DOI] [PubMed] [Google Scholar]
- Yanez et al., 2009.Yanez B., Edmondson D., Stanton A.L., Park C.L., Kwan L., Ganz P.A. Facets of spirituality as predictors of adjustment to cancer: Relative contributions of having faith and finding meaning. Journal of Consulting and Clinical Psychology. 2009;77:730–741. doi: 10.1037/a0015820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner T., Maercker A. Posttraumatic growth in clinical psychology — A critical review and introduction of a two component model. Clinical Psychology Review. 2006;26:626–653. doi: 10.1016/j.cpr.2006.01.008. [DOI] [PubMed] [Google Scholar]


