Abstract
Chronic, progressive, and irreversible loss of lung function is the major medium-term and long-term complication after lung transplantation and the leading cause of death. Over the past decade, progress has been made in understanding the pathogenesis of bronchiolitis obliterans. Alloimmune factors and nonalloimmune factors may contribute to its development. Understanding the precise mechanism of each type of chronic allograft dysfunction may open up the field for new preventive and therapeutic interventions. This article reviews major new insights into the clinical aspects, pathophysiology, risk factors, diagnosis, and management of chronic allograft dysfunction after lung transplantation.
Keywords: Lung transplantation, Chronic lung allograft dysfunction, Bronchiolitis obliterans, Bronchiolitis obliterans syndrome, Neutrophilic reversible allograft/airways dysfunction, Macrolides
Bronchiolitis obliterans (BO) in the context of lung transplantation was first described in 1984 at Stanford University in a patient who developed progressive airflow obstruction after heart-lung transplantation.1 Lung biopsies revealed intraluminal polyps of fibromyxoid granulation tissue, which tended to obliterate the lumen of terminal bronchioles, and dense submucosal eosinophilic fibrous scars (Fig. 1 ). Since this early report, BO has been recognized as the major complication and the leading cause of death after lung transplantation.2
Fig. 1.
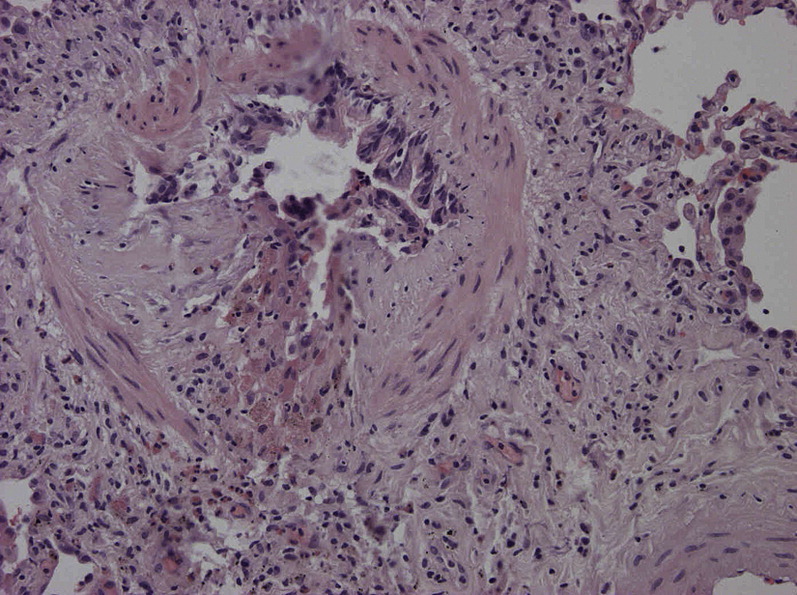
Histological picture of post-transplant BO. The lumen of the bronchiole is almost totally occluded by fibromyxoid granulation tissue.
Because the small airway lesions have a patchy distribution, they can hardly be demonstrated by transbronchial lung biopsies (TBBs), which have a low sensitivity (28%) and specificity (75%).3 As a result, in order to establish the diagnosis of BO without the need for open lung biopsy, the International Society for Heart and Lung Transplantation (ISHLT) proposed in 1993 a clinical definition based on pulmonary function criteria. The term, bronchiolitis obliterans syndrome (BOS), was coined to identify patients with a progressive and irreversible decline in forced expiratory volume in one second (FEV1). In the initial classification, BOS was divided into 4 stages based on the degree of loss in FEV1 compared with the best postoperative value. In the updated classification proposed in 2002, a potential BOS (BOS 0-p) stage—defined by a decline in FEV1 or in midexpiratory flow rates (FEF25-75)—was added to detect early but potentially important changes in pulmonary function (Table 1 ).4 Several conditions needed to be satisfied for a patient to be classified in the staging system: (1) the functional loss had to be present for at least 3 weeks to exclude an acute, reversible process; (2) the loss had to include a decrease in both FEV1 and FEV1/vital capacity ratio (ie, patients with a loss in FEV1 in the context of a restrictive ventilatory defect are not considered as having BOS), and (3) confounding conditions that may produce a decrease in FEV1 (eg, infection, acute rejection, anastomotic complications, disease recurrence, and progression of native lung hyperinflation in patients with single-lung transplantation [SLT] for emphysema) needed to be excluded.
Table 1.
Bronchiolitis obliterans syndrome classification system
| 1993 Classification | 2002 Classification | ||
|---|---|---|---|
| FEV1 80% or more of baseline | FEV1 >90% of baseline and FEF25-75 >75% of baseline | BOS 0 | |
| FEV1 81% to 90% of baseline and/or FEF25-75 = or <75% of baseline | BOS 0-p | ||
| BOS 1 | FEV1 66% to 80% of baseline | FEV1 66% to 80% of baseline | BOS 1 |
| BOS 2 | FEV1 51% to 65% of baseline | FEV1 51% to 65% of baseline | BOS 2 |
| BOS 3 | FEV1 50% or less of baseline | FEV1 50% or less of baseline | BOS 3 |
Data from Estenne M, Maurer JR, Boehler A, et al. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant 2002;21:297–310.
Transplant centers worldwide have adopted this staging system as a descriptor of chronic lung allograft dysfunction. This proved useful because it provided a common language to classify patients and compare results between programs. Several limitations, however, have become apparent in recent years. First, many patients who have confounding conditions cannot be staged for BOS. Second, as the experience with lung transplantation accrued, an increasing number of patients presented with forms of chronic allograft dysfunction that did not comprise all the characteristic features of BOS. Several types of chronic allograft dysfunction, which differ from BOS, were identified in the past years. These include (1) a reversible phenotype characterized by airway neutrophilia and functional improvement with azithromycin (AZM), (2) a phenotype characterized by a restrictive ventilatory impairment associated with upper lobe fibrosis or persistent parenchymal or pleural abnormalities, (3) exudative or follicular bronchiolitis, and (4) large airway stenosis/malacia. This review deals primarily with classical BOS, which has been more extensively studied, but other recently described presentations of chronic allograft dysfunction also are addressed.
The clinical spectrum of chronic allograft dysfunction
Classical BOS
In the registry report of the ISHLT published in 2010,2 freedom from BOS in a cohort of 12,058 patients followed between April 1994 and June 2009 was 89.7% at 1 year, 67.4% at 3 years, 51.2% at 5 years, and 24.8% at 10 years after surgery. These percentages represent a clear decrease in the prevalence of the complication compared with earlier series. Yet BOS remains by far the most significant long-term complication and the leading cause of late death after lung transplantation, accounting for 20% to 30% of all deaths after the third postoperative year.2
BOS may affect all lung transplant recipients irrespective of donor and recipient characteristics, type of transplantation, and pretransplant disease. The clinical presentation of BOS is heterogeneous.5 The type of presentation, the time from transplantation to onset, and the rate of progression are all variable between patients (Fig. 2 ). BOS may present as an acute illness and imitate a respiratory infection,5 but in most patients it starts as an asymptomatic process that produces an insidious decline in lung function. In approximately 20% of patients, BOS develops within 2 years of transplantation (early-onset BOS), but the vast majority of patients develop the complication at a later point in time.2, 6 Some patients present with a substantial loss of lung function and are already in BOS stage 2 or 3 (high-grade onset) at presentation whereas others show a slow decline over time.6 In a study by Jackson and colleagues5 56% of 204 patients who developed BOS showed a sudden drop in FEV1, whereas 18% presented with a smooth linear decline; time to BOS onset was longer in the latter group. Acute rejection during the first 6 months was significantly associated with acute onset of BOS. Auscultation of the lungs is often normal, but squeaks and coarse crackles may be heard. High-resolution CT may reveal air trapping (Fig. 3 ) and bronchiectasis,7, 8 without significant parenchymal infiltrate. As the disease progresses, permanent airway colonization with pathogens, such as Pseudomonas aeruginosa and Aspergillus fumigatus, frequently develops. Survival at 5 years after diagnosis ranges from 26% to 43%,6, 9, 10, 11 and survival at 5 years after transplantation is 20% to 40% lower in patients with, compared to patients without, BOS.11 There is also evidence that the number of respiratory infections and the aggressiveness with which they are treated have an impact on BOS progression.9 In addition to representing a major obstacle to long-term survival, BOS causes significant morbidity and loss of health-related quality of life.12
Fig. 2.
Changes in FEV1 over time elapsed since transplantation in 3 patients with BOS. Stages refer to the BOS classification, and horizontal lines indicate transitions between stages 0 and 1, stages 1 and 2, and stages 2 and 3. The figure illustrates the highly variable pattern of functional evolution between patients affected by BOS.
(From Estenne M, Maurer JR, Boehler A, et al. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant 2002;21:297–310; with permission.)
Fig. 3.
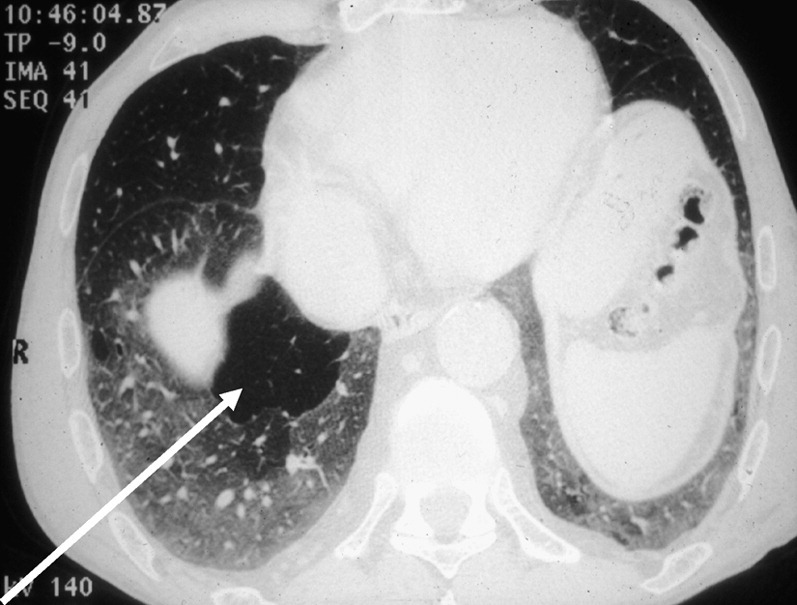
Expiratory CT scan in a transplant recipient with BOS. The arrow indicates lobules with low attenuation, a sign of the presence of air trapping.
(From Bankier AA, Muylem AV, Knoop C, et al. BOS in heart-lung transplant recipients: diagnosis with expiratory CT. Radiology 2001;218:533–9; with permission.)
BOS is used as a surrogate marker of BO but does not equal BO. Therefore, as expected for any functional marker, a drop in FEV1 is likely to have a low specificity for the diagnosis of BO (this is why exclusionary criteria were added to the definition of BOS). This lack of specificity is difficult to assess because a gold standard is rarely available. Yet in a study of lungs explanted at the time of retransplantation for BOS,13 pathology examination always showed at least some degree of BO, but a wide range of other pathologic processes of potential clinical significance was also evident in half of the specimens.
Other Forms of Chronic Allograft Dysfunction
In contrast to classical BOS, which is characterized by a progressive, irreversible airflow obstruction and few, if any, parenchymal or pleural abnormalities, recently described new phenotypes of chronic allograft dysfunction may include one or more of the following features: partial reversibility of airway obstruction, restrictive ventilatory impairment, parenchymal/pleural abnormalities, and large airway stenosis/malacia.
Neutrophilic reversible allograft/airways dysfunction
Because it is well known that macrolide antibiotics are effective in treating airway diseases which, like BOS, are associated with neutrophilic inflammation (eg, panbronchiolitis and cystic fibrosis), Gerhardt and colleagues14 performed an open trial with AZM in lung transplant recipients. In this study, AZM (250 mg 3 times a week) was added to the current immunosuppressive treatment in 6 patients with BOS; 5 patients responded with a mean improvement in the FEV1 of 21.6% after 14 weeks. One patient even had a complete restoration of FEV1 to peak post-transplant values. This landmark study was followed by at least 6 studies,15, 16, 17, 18, 19, 20 of which 4 confirmed the results published by Gerhardt and colleagues.14 One study by Benden and colleagues21 also reported a positive effect of clarithromycin on FEV1. Taking these publications together, approximately 35% of all patients in different BOS stages responded to macrolide treatment by a mean increase in FEV1 of approximately 14%. Furthermore, a higher bronchoalveolar lavage (BAL) fluid neutrophilia was associated with a greater likelihood of functional response.18 Based on these observations, Verleden and colleagues22 suggested that BOS might be dichotomized into an AZM-responsive phenotype characterized by airway neutrophilia and functional improvement with AZM (the so-called neutrophilic reversible allograft/airways dysfunction [NRAD]), and an AZM-unresponsive phenotype, which corresponds to the classical, fibroproliferative form of BO. These two phenotypes might have different pathophysiology, clinical presentation, and prognosis; for example, NRAD might start earlier after transplantation and progress slower than fibroproliferative BOS; and crackles, increased sputum production, bronchiectasis, and mucus plugging might be more prominent in the former than in the latter.
Upper lobe fibrosis
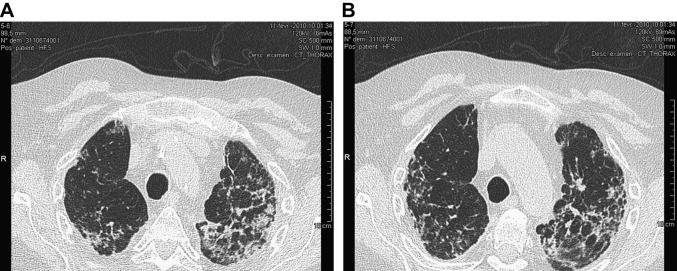
In 2005, a joint retrospective study by the Toronto General Hospital and the Duke University Hospital identified 13 of 686 lung transplant recipients who developed upper lobe fibrosis.23 Radiographic changes started initially as nonspecific interstitial markings in the upper lobes and slowly progressed to honeycombing, traction bronchiectasis, and volume loss (Fig. 4 ). Most patients had a restrictive ventilatory defect, with some eventually developing concomitant airflow obstruction. Open lung biopsy specimens revealed dense interstitial fibrosis, with occasional features of BO, acute fibrinous and organizing pneumonia, bronchiolitis obliterans organizing pneumonia, and aspiration. The rate of progression of clinical symptoms ranged from slow to rapid but, overall, the condition had a poor prognosis. The prevalence and cause of this form of chronic allograft dysfunction are still unclear.
Fig. 4.
CT scans obtained at two different levels (A and B) in a lung transplant recipient showing the peculiar pattern of upper lobe fibrosis. Culture for infectious agents of BAL specimens were repeatedly negative in these zones and transbronchial biopsies showed nonspecific inflammation and fibrotic changes.
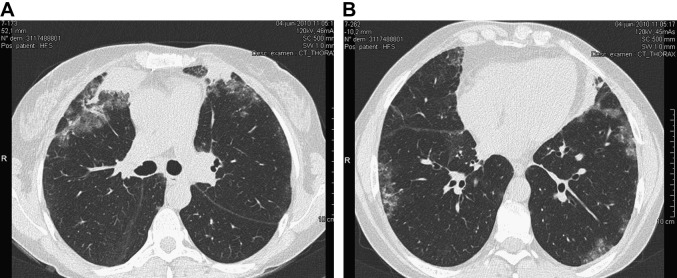
Recently, Woodrow and colleagues24 reported on lung transplant recipients who had a decline in lung function associated with persistent parenchymal (alveolar, nodular, ground-glass, or interstitial) abnormalities on chest CT—not specifically involving the upper lobes (Fig. 5 ). No precise cause was found for the parenchymal infiltrates and the patients showed a functional deterioration over time that paralleled the course of patients with classical BOS. A similar proportion of patients (approximately 50%) had a restrictive ventilatory defect in the group with, and in the group without, parenchymal infiltrates.
Fig. 5.
This patient with CF had been transplanted for 10 years when she developed an acute, rapidly progressive, and completely therapy-resistant drop in lung function. CT scan of the lungs repeatedly showed peripheral infiltrates in the upper (A) but also lower (B) lung zones. BAL showed prominent neutrophilia but also—even if to a lesser extent—eosinophilia. No infectious agents could be incriminated; in particular, there were no diagnostic criteria for invasive pulmonary aspergillosis. She, eventually, could undergo redo-double lung transplantation. The explanted lungs showed zones of nonspecific interstitial fibrosis with pneumocyte hyperplasia and fibroblast proliferation in the areas of the parenchymal abnormalities, and advanced BO lesions in other lung regions.
Chronic pleural inflammation
In a study by Woodrow and colleagues,24 36% of the radiographic abnormalities were pleural, and another study showed that at 1 year after transplantation, 50 of 58 patients (86%) had pleural abnormalities (most frequently pleural thickening) on chest CT.25 Such abnormalities may obviously restrict lung volumes, but their relationship with a process of chronic rejection and their long-term impact remain to be clarified.
Exudative/follicular bronchiolitis
In 2008, McManus and colleagues26 reported on 13 of 99 transplant recipients who presented with exudative bronchiolitis, which appeared on high-resolution CT as a tree-in-bud pattern (centrilobular nodules and branching lines). This condition was associated with early infection post-transplant and a history of Aspergillus infection. Neutrophil count in bronchial washing was increased and most patients improved clinically and radiologically with AZM. Yet, exudative bronchiolitis increased markedly the likelihood of developing BOS. Recently, Vos and colleagues27 described a patient who developed follicular bronchiolitis characterized by abundant peribronchiolar lymphoid follicules; this condition was also associated with the development of BOS.
Large airway stenosis/malacia
A recent article by Akindipe and colleagues28 reported on 5 patients who had to be retransplanted for severe recurrent airway narrowing. In all patients, allograft lung pathology revealed evidence of BO. This observation suggests a possible link between airway ischemia/hypoxia, large airway stenosis/malacia, and the development of BO.
Pathogenesis and risk factors
Pathogenesis
In the earlier days of lung transplantation, BOS/BO was believed to be equivalent to chronic allograft rejection (ie, a process caused by an alloimmune reaction). The lung is uniquely exposed to the environment, however, and thus to recurrent nonalloimmune insults, such as infections, inhalation of toxic fumes, or gastroesophageal reflux. Furthermore, recent studies suggest a possible role of autoantibodies developed against specific epithelial proteins and of airway hypoxia in the pathogenesis of BOS/BO. The current view is that these insults, acting alone or in combination, up-regulate dendritric cells in the airway epithelium, leading to epithelial damage and inflammation with production of chemokines and cytokines by airway epithelium and smooth muscle cells, macrophages, and neutrophils. Activated neutrophils further increase epithelial damage via the production of reactive oxygen species and metalloproteinases. After the initial inflammatory phase, a fibroproliferative phase occurs, driven by growth factors and leading to proliferation of smooth muscle cells and myofibroblasts. This process eventually results in aberrant collagen deposition, excessive fibroproliferation, and small airway obliteration. BO would thus represent a final common pathway lesion secondary to multiple, repetitive insults to the airway epithelium.29, 30
Alloimmune Risk Factors
Ninety-five percent of patients receive grafts with 3 or more HLA mismatches. Using the Collaborative Transplant Study database, 5-year graft outcome according to HLA mismatch was examined in 8020 lung transplants performed during 1989 through 2009. Graft survival rates showed a stepwise decrease as the combined number of HLA-A+B+DR mismatches increased from 1 to 6, with a high number of HLA mismatches having an unfavorable impact on survival.31 Because of the average high number of mismatches, studies to examine the effect of HLA mismatching on the incidence of acute rejection have proved difficult and their results have been inconsistent. Most of them have, however, identified some negative impact of HLA mismatching.32, 33 Multivariate logistic regression analyses of data on 3549 adult lung transplant recipients retrieved from the United Network for Organ Sharing/ISHLT registry demonstrated an association between mismatching at the HLA-A locus (but not at the HLA-B or HLA-DR loci) and acute rejection episodes requiring hospital admission.34 Several studies have confirmed that the development of anti-HLA class I and class II antibodies after surgery is associated with a risk for acute rejection and BOS.35, 36, 37, 38, 39 Binding of these antibodies to airway epithelial cells may induce epithelial injury and proliferation.40
Acute vascular rejection histology graded greater than or equal to A2 has been identified in many studies as a statistical risk factor for BOS. Yousem41 reported in 1996 that untreated acute vascular rejection grade A2 leads to the development of BOS in 50% of patients. Several studies have shown that the risk of BOS increases when acute vascular rejection is histologically severe or persistent or recurs after treatment (studies reviewed by Knoop and Estenne42). The impact of minimal acute rejection (grade A1) on the development of BOS, however, has been long neglected. Recently, in a study by Hopkins and colleagues43 less than10% of grade A1 rejections were associated with clinical symptoms but 34% of the asymptomatic patients progressed to higher-grade acute rejection or lymphocytic bronchiolitis (LB) within 3 months. In this report also, patients with multiple A1 episodes during the first 12 months post-transplant had a significantly higher risk of developing BOS, and this occurred earlier than in patients with 1 or less grade A1 episode.43 Khalifa and colleagues44 retrospectively examined data from 228 lung transplant patients followed over a 7-year period and confirmed that grade A1 rejection is a distinct risk factor for BOS. Hachem and colleagues45 from the same group determined that even a single episode of A1 rejection, without recurrence or subsequent progression to a higher rejection grade, was a significant risk factor for the development of BOS. Treatment of grade A1 rejection with diverse approaches in order to augment the net immunosuppression decreased the risk for subsequent progression to BOS stage 1.44
LB in the absence of acute vascular rejection may also predate BOS.46, 47 Glanville and colleagues48 retrospectively assessed data from 1770 TBB specimens obtained from 341 patients over a period of 10 years and showed that the cumulative incidence of BOS was significantly associated with the severity of LB. Another retrospective analysis of 2697 TBB specimens obtained from nearly 300 consecutive patients followed during the first 2 postoperative years at the University of Copenhagen showed that the cumulative incidences of LB (≥ B2) were 33%, 53%, 62%, and 68% at 1 month, 3 months, 6 months, and 12 months, respectively. Approximately 25% and 50% of patients had a second episode graded B2 or higher within 3 months and 2 years of transplantation, respectively. In this study, LB during the first 2 years was independently associated with the frequency and/or severity of acute rejection, and LB grade B2 or higher was associated with an increased risk of BO.49
The concept of acute or chronic antibody-mediated rejection is still controversial after lung transplantation.50 There are now well documented reports that this type of rejection exists,51 however, and data on its possible contribution to chronic allograft dysfunction are beginning to appear.52 The observation that patients developing HLA antibodies fare less well than those who do not and the novel data on self-antibodies directed against epithelial antigens in patients with BOS/BO (discussed later) lend some credibility to this hypothesis.
Autoimmune Risk Factors
Recently, the development of autoimmune processes directed against epithelial-specific proteins has been incriminated in the development of BOS/BO. In one study, collagen type V-reactive CD4+ T cells were associated with a nearly 10-fold increase in the risk of BOS in clinical lung transplantation.53 In another study, anti-K–α1 tubulin antibodies were present in a significant number of patients with BOS.54 Anti-K–α1 tubulin circulating antibodies may induce profibrotic growth factors from airway epithelial cell lines, thus providing evidence that autoimmunity—like alloimmunity—may induce fibrosis.55 Conversely, it has also been shown that alloimmune responses in the lung can promote the development of collagen type V and K-α1-tubulin autoimmunity.56 Thus, the picture has become more complex: alloimmunity, autoimmunity, and the innate immune system (discussed later) may all trigger allograft airway fibrosis, and these processes are moreover likely intertwined.57
Other Risk Factors
As discussed previously, the association between acute rejection and BOS has been reported for both early and late rejection episodes. Yet many patients with acute rejection do not develop BOS, and some patients with BOS have never experienced acute rejection. One possible explanation is that the use of intense induction and maintenance immunosuppression and of aggressive treatment of rejection might uncouple the association between acute rejection and BOS. Another potential explanation, however, is that BOS/BO might be triggered by nonalloimmune–dependent factors. These may directly injure the airways—as is the case for gastric aspiration—and/or augment the alloimmune response via activation of the innate immune system, as is the case for respiratory bacterial and viral infections.58
Bacterial colonization of the graft was formerly believed to be the consequence of BOS/BO. It has been recently reported, however, that bacterial colonization, notably with Pseudomonas aeruginosa, might be one of the possible alloimmune-independent risk factors for BOS/OB. In a study by Botha and colleagues,59 including 155 lung transplant recipients, the development of allograft colonization with Pseudomonas was strongly associated with the development of BOS within 2 years of transplant (23.4% and 7.7% in those colonized and not colonized, respectively). The isolation of Pseudomonas predated the diagnosis of BOS in more than 75% of affected patients by a median exceeding 200 days. Similar findings have been reported for Aspergillus colonization.60 Valentine and colleagues61 analyzed the role of bacterial and fungal respiratory tract infections in the development of BOS in a single-center study comprising 161 lung recipients who had survived at least 180 days. Multivariate analysis indicated that gram-negative, gram-positive, and fungal pneumonias were associated with the development of BOS. Gram-positive pneumonia and fungal pneumonia in the first 100 days conferred hazard ratios of 3.8 and 2.1, respectively. They concluded that early recognition and treatment of these pathogens might improve long-term outcomes.
Kumar and colleagues62 screened serial surveillance and diagnostic BAL specimens obtained from 93 lung transplant recipients over 3 years for community-acquired respiratory viral infections (CARVIs) using sensitive molecular methods that simultaneously detected 19 respiratory viral types/subtypes. Respiratory viruses—rhinovirus, parainfluenza virus 1 to 4, coronavirus, influenza, metapneumovirus, and respiratory syncytial virus—were isolated in 48 of 93 (51.6%) patients in at least one BAL sample. Biopsy-proven acute rejection (≥ A2) or decline in FEV1 greater than or equal to 20% occurred in 33.3% of CARVI-positive patients (within 3 months of CARVI) compared with only 6.7% of CARVI-negative patients. No significant difference was seen in the incidence of acute rejection between symptomatic and asymptomatic patients. Biopsy-proved BO was diagnosed in 10 of 16 (62.5%) patients within 1 year of infection, indicating that symptomatic or asymptomatic viral infection may trigger acute rejection and/or BOS/BO. In contrast, Gottlieb and colleagues63 found that only symptomatic CARVI increases the risk of BOS. Chlamydia pneumoniae 64, 65 and human herpesvirus 6 respiratory infections66 are also known to increase the risk of BOS.
CMV mismatching (ie, seronegative recipients receiving organs from seropositive donors) and CMV pneumonitis have been associated with BOS in several series, but others found only a marginal or no relationship at all. These differences might be accounted for, at least in part, by the different strategies used to match recipients with regard to CMV status and to prevent and treat CMV illness over the decades. Valentine and colleagues61 reported that CMV pneumonitis within the first 100 days conferred a hazard ratio of 3.1 to develop BOS. The same group reported on their experience with ganciclovir (GCV) prophylaxis in 130 patients surviving at least 100 days. CMV pneumonitis occurred in 16%, 8%, 17%, and 19% of patients in the D+R+, D−R+, D+R− and D−R− groups, respectively. Ninety patients received indefinite GCV prophylaxis whereas 40 patients discontinued the prophylaxis (STOP). Cumulative incidences of CMV pneumonitis in the indefinite GCV prophylaxis and STOP groups at 5 years were 2% and 57%, respectively. In the STOP cohort, 15 of 40 patients developed CMV pneumonitis after GCV was stopped, and 10 of these developed BOS. The risk of CMV pneumonitis in the STOP cohort was significantly higher when GCV prophylaxis was discontinued within the first year. BOS-free survival and survival were, however, similar across groups.67 On the contrary, Tamm and colleagues68 showed in their series that CMV pneumonitis, when treated with GCV, is not a risk factor for BOS and does not affect survival.
Gastroesophageal reflux disease (GERD) is thought to be a risk factor for the development or progression of BOS/OB. GERD is observed in approximately half of all lung transplant patients.69 The prevalence of delayed gastric emptying is also high.69 In addition, these patients have an impaired cough reflex because of lung denervation and have altered mucociliary clearance. Taken together, these factors increase the likelihood of aspiration and subsequent airway injury. Pepsin70 and bile acids71 can be readily found in the BAL fluid of many lung transplant recipients, which confirms the frequent occurrence of gastric aspiration. The finding of increased bile acids in BAL fluid (a marker of nonacidic reflux) correlates with the presence of BOS/BO.70, 71 Exposure of the airway epithelium to bile acids may predispose to colonization with Pseudomonas aeruginosa and airway neutrophilia. Because of concern that GERD increases the risk of BOS, the general trend has been to propose a surgical solution, namely gastric fundoplication, to all recipients presenting with significant GERD. Supportive evidence for this strategy is derived from retrospective studies in which gastric fundoplication within 3 months after transplant was associated with greater freedom from BOS and increased survival.72 Another study from the same center showed that fundoplication improved lung function in many patients with established BOS.73 Before adopting this radical approach for every single lung transplant recipient, however, it is important to be aware that (1) the best way to diagnose GERD in lung transplant recipients—pH monitoring versus impedance monitoring—is at present controversial; (2) GERD—as well as the cough reflex—may improve over time; (3) fundoplication may have serious side effects (eg, significant weight loss, which can be of importance in recipients with significant malnutrition); (4) the protective function of the surgical sleeve may wane over time; (5) the precise indications, timing, and choice of fundoplication technique are yet to be defined; and (6) the overall impact on lung function and survival are unknown because there are no controlled studies to date.74
Allograft ischemia may arise during the period of warm ischemia during explantation, because of the absence of bronchial arterial reanastomosis at implantation, or through small airway microvascular damage at later time points.75 In a study of 334 lung transplant recipients of whom 65 developed primary graft dysfunction (which is a severe form of ischemia/reperfusion lung injury), this complication was an independent risk factor for BOS.76 Allograft ischemia might result in hypoxic inflammatory conditions leading to vascular remodeling and angiogenesis, which may in turn be a potent stimulus for airway fibrosis.77, 78 By gaining a better understanding of the complex interaction between airway ischemia, vascular remodeling and angiogenesis-mediated airway fibroproliferation, it might become increasingly possible to rationally design therapies that can halt conditions of maladaptive fibrosis79 and, possibly, decrease the risk of BOS/BO.
The role of other risk factors for BOS, such as graft ischemic time, donor-recipient gender or size mismatch, and type of surgical procedure, is currently controversial.
The Role of Neutrophils
It is widely accepted that BOS/BO involves a neutrophilic airway inflammation, although this feature is lacking in a substantial proportion of patients. Recent studies (summarized by Verleden and colleagues22) have shown that interleukin (IL)-17 may have an important role in the development of BOS/BO. IL-17 is a potent indirect neutrophil-attracting chemokine through its ability to induce IL-8 secretion from different cell types in the airways. IL-17 is increased in the airways of patients with BOS/BO and induces production of IL-8 by airway smooth muscle and epithelial cells, which, in turn, promotes airway neutrophilia. The IL-17/IL-8 axis may be triggered by both alloimmune and autoimmune mechanisms, airway bacterial colonization, and GERD,22 but the reasons why BOS is accompanied by airway neutrophilia in some patients and not in others remain unclear. The effect of AZM on this inflammatory process is likely primarily accounted for by its ability to inhibit the IL-17/IL-8 pathway; other potential mechanisms include a positive effect of AZM on GERD (AZM is a known agonist of motilin) as well as its inhibitory effect on bacterial growth.
Open Questions and Controversial Issues
It is important to stress that BOS and the newly described phenotypes of chronic allograft dysfunction are syndromes defined by clinical criteria, changes in pulmonary function, radiographic features, and analysis of BAL cellularity, alone or in combination. These entities are merely descriptive and do not sort by specific pathogenic pathways, risk factors, pathology, or prognosis. Patients may have more than one phenotype at a time or over time, and different pathogenic pathways and pathology may coexist (discussed previously). More work is required to understand the clinical relevance and pathogenesis of each entity as well as the mechanisms by which the different risk factors produce one phenotype or another.
For the time being, we still have to work with the current definition of BOS (ie, a progressive and irreversible airflow obstruction due to a loss of small airway function attributed to BO) although the difficulties associated with a staging system based on a retrospective diagnosis and exclusionary criteria are acknowledged. BOS should probably no longer be presumed to reflect specifically a process of chronic rejection because nonalloimmune insults likely often contribute to the development of the small airway lesions. Finally, whether or not NRAD should be considered a subtype of BOS or a distinct entity is currently debated in the transplant community (discussed later).
Diagnosis
To the extent that current therapies work to stop or slow down the progression of BOS, they do so mostly by an anti-inflammatory, not an antifibrotic, effect. Therefore, they are more likely to be effective in the early stage of the disease. For this reason, various parameters have been evaluated as early biomarkers of BOS.
Lung Function
Spirometry is appealing as an early marker because it is widely available, noninvasive, reproducible, and relatively inexpensive. Two studies have assessed the predictive value of BOS stage 0-p for the diagnosis of BOS stage 1. In the study by Hachem and colleagues,80 which included 203 adult bilateral lung transplant (BLT) recipients, the FEV1 criterion had a sensitivity, specificity, positive predictive value, and negative predictive value of 74%, 86%, 79%, and 82%, respectively; corresponding values for the modified FEF25-75 criterion (computed using baseline values obtained at the time of the two highest FEV1 measurements) were 66%, 88%, 81%, and 76%, respectively. In the 197 SLT recipients studied by Lama and colleagues,81 the FEV1 criterion was also predictive of BOS 1; its predictive value was superior to that of the FEF25-75 criterion and was superior in patients with underlying restrictive as opposed to obstructive physiology.
Exhaled Biomarkers
Distribution of ventilation
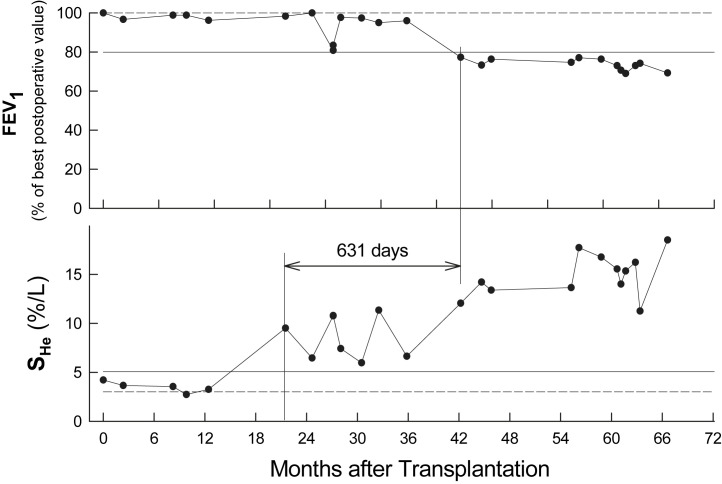
The slope of the alveolar plateau of the single-breath washout test reflects the homogeneity of ventilation distribution and increases as ventilation becomes more heterogeneous. The single-breath test can be performed using an inspiration of pure oxygen and measuring the concentration of nitrogen during expiration; a gas mixture containing inert gases (for example helium) can also be used during inspiration, and the concentration of these gases be measured during expiration. Two prospective studies have assessed the usefulness of the single-breath test for the early detection of BOS in BLT recipients. In these studies, nitrogen slope became abnormal 17882 and 15183 days before the criterion for BOS 1 was met. The positive predictive value of the test was 70% to 80% and the negative predictive value approximately 100%. Furthermore, 2 studies by Estenne and colleagues82 and Van Muylem and colleagues84 showed that helium slope is an even earlier marker than nitrogen slope (Fig. 6 ).
Fig. 6.
In patients presenting BOS, the slope of the alveolar plateau for helium increases as ventilation becomes more heterogeneous and this early marker of BOS becomes abnormal before spirometric criteria for BOS 1 are fulfilled. This figure shows changes in FEV1 and in the slope of the alveolar plateau for helium obtained during a single-breath washout test (She) in one heart-lung transplant recipient. In the upper panel, the dashed line corresponds to 100% of the two best postoperative values and the continuous line indicates a 20% decrease (BOS stage 1). In the lower panel, the dashed line corresponds to the average of the two lowest postoperative values, and the continuous line is the upper limit of the 97.5% CI computed from data obtained in 10 stable transplant patients. Note that a significant change in She is observed 631 days before the 20% drop in FEV1.
(From Van Muylem A, Knoop C, Estenne M. Early detection of chronic pulmonary allograft dysfunction by exhaled biomarkers. Am J Respir Crit Care Med 2007;175:731–6; with permission.)
Two recent studies in recipients of SLT for emphysema or fibrosis suggested that when performed in lateral decubitus, the single-breath test may also provide information on ventilation distribution in the graft in this patient population.85, 86
Exhaled gases
Exhaled nitric oxide (eNO) is a well-recognized biomarker of airway inflammation. In stable lung transplant recipients and patients with BOS, eNO reflects the expression of bronchial epithelial inducible NO synthase and positively correlates with airway neutrophilia.87, 88, 89, 90 Carbon monoxide (CO) is produced endogenously by the stress protein heme oxygenase, which is increased in a variety of oxidant/inflammatory-mediated injuries. In BO lesions, heme oxygenase staining correlates with myeloperoxidase expression (reflecting oxidant load) and with neutrophilic infiltration of the bronchial wall. Heme oxygenase degrades heme with the production of iron, biliverdin, and CO. Therefore, both eNO87, 88, 89 and exhaled CO (eCO)90 may reflect airway neutrophilia and, hence, be used as surrogate markers of BOS.
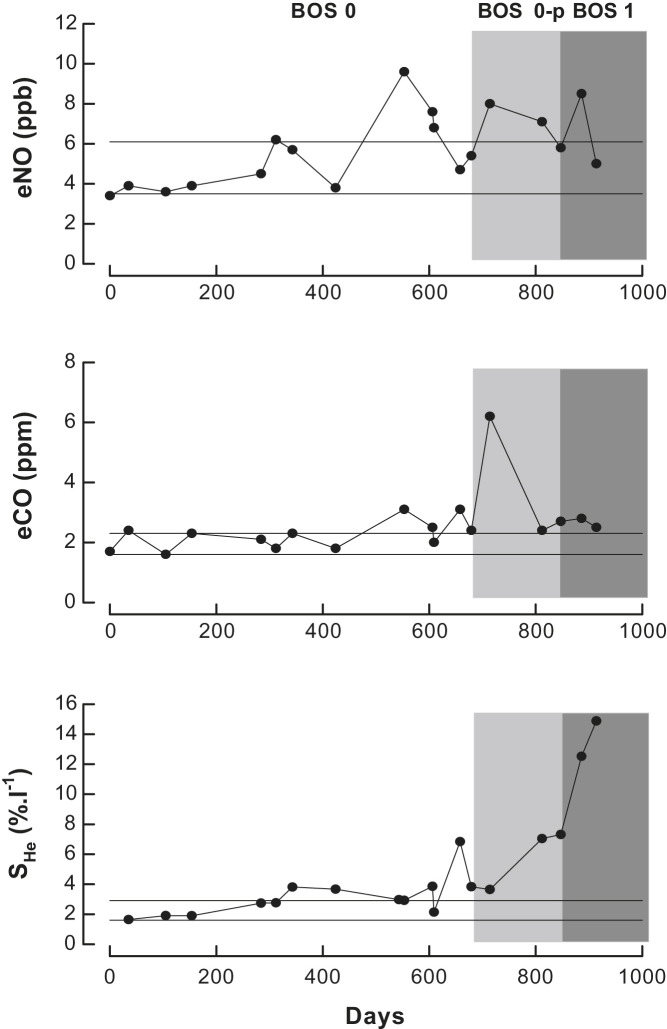
Four studies have shown that eNO is increased in patients with BOS compared with patients without BOS,89, 91, 92, 93 independent of the type of surgical procedure. The potential contribution of serial eNO measurements to the early detection of BOS, however, was difficult to assess from these studies. In a recent study of 65 recipients of bilateral grafts who were followed for approximately 1250 days, Van Muylem and colleagues84 found that eNO and eCO only transiently increased in BOS 0-p and then returned to baseline as BOS progressed (Fig. 7 ). The sensitivity of exhaled gases for the diagnosis of BOS 0-p was only 50% to 60%, but it increased to approximately 80% when values of eNO and eCO were combined; yet, on average, the increase in exhaled gases did not precede the diagnosis of BOS 0-p. This may be due, at least in part, to a significant proportion of patients with early BOS having no increase in airway neutrophilia.
Fig. 7.
Changes in eNO, in eCO, and in the slope of the alveolar plateau for helium (She) over time in one transplant recipient. The continuous lines indicate the confidence interval. Note that values of She become abnormal before BOS 0-p, and then increase progressively with the BOS stage; in contrast, values of eNO and eCO are much more variable between successive measurements and do not show a consistent trend as BOS progresses.
In summary, eNO and eCO have a fair sensitivity and nitrogen or helium slope has a good sensitivity for the detection of BOS. All biomarkers also have a high negative predictive value, but their specificity and positive predictive value are much lower. The low specificity reflects that these markers—like the FEV1—may be affected by complications other than BOS (eg, acute rejection, lymphocytic bronchiolitis, and infection). From a clinical point of view, the high negative predictive value should help detect conditions that may confound the diagnosis of BOS, because in the absence of a significant rise in exhaled biomarkers, BOS is an unlikely explanation for a decline in spirometry. Conversely, a persistent rise in slope or in eNO/eCO should be interpreted as a warning signal and prompt close monitoring of a patient’s lung function and clinical condition.
Other Markers
Several other surrogate markers of BOS have been proposed, but their clinical utility is limited by one or more of the following factors: they are invasive or potentially toxic, they are expensive, they are not widely available, or their predictive value has not been appropriately tested or is controversial. These surrogate markers include exhaled breath condensate,94 induced sputum,95 analysis of cellular composition and inflammatory markers in BAL fluid, and imaging techniques, such as CT—in particular, quantification of air trapping at full expiration (see Fig. 3),7, 8, 96 and hyperpolarized 3He MRI.97
Treatment
Optimization and/or Change in Immunosuppressive Regimen
All interventions that target risk factors and may prevent the development of BOS are valuable because therapy is often ineffective when BOS is established. In this context, optimization of the immunosuppressive regimen to prevent the occurrence of acute rejection is a critical issue (discussed previously). Several studies have looked at the effects of increasing the net level of immunosuppression (eg, by using high-dose methylprednisolone, cytolytic therapy, or methotrexate) and/or changing the maintenance regimen (eg, by shifting from cyclosporine A to tacrolimus or from azathioprine to mycophenolate mofetil, or by adding inhaled cyclosporine A) in patients with established BOS (reviewed by Knoop and Estenne42). In some patients, these modalities have been shown to stabilize lung function or decrease the rate of decline of FEV1 for short periods of time. The small number of patients studied, the mostly retrospective design of these studies, the lack of adequate control group, and the relatively short follow-up time, however, make it difficult to assess the effectiveness of these treatments. No single strategy has proved more successful than another. In addition, augmented immunosuppression increases the risk of toxicity and predisposes to intercurrent bronchopulmonary infections, which must be factored into the risk-benefit analysis as they may promote the progression of BOS (discussed previously).
Macrolides
As discussed previously, several studies with a follow-up of 12 to 40 weeks have shown that macrolide treatment improves FEV1 in approximately one-third of patients in different BOS stages. Two studies20, 98 have assessed the long-term effect of AZM. The study by Gottlieb and colleagues included 81 patients with a median follow-up of 1.3 years20 and the study by Vos and colleagues98 included 108 patients treated for a median time of 612 days. An initial response (defined as a 10% or more increase in FEV1) was observed in 30% to 40% of the patients, but 30% to 40% of these subsequently relapsed. By multivariate analysis, initial response to AZM and earlier post-transplant time of initiation of treatment were protective factors for disease progression or relapse; in contrast, the level of BAL neutrophilia had no predictive value. These longitudinal data thus show that AZM provides a sustained functional improvement in the long-term in only a small minority of patients with BOS (approximately 10%–15%). This observation suggests, therefore, that in most patients (even those with the NRAD phenotype), BOS is a condition that worsens with time.
Despite this relatively modest effect of AZM on lung function, 3 studies in patients with BOS have shown that this treatment is associated with a significant reduction in the risk of death.20, 98, 99 In studies by Gottlieb and colleagues20 and by Vos and colleagues,98 responders had significantly better overall survival compared with nonresponders; as expected, the difference between groups was more pronounced when only responders with a sustained response were taken into account.
Using AZM for the prevention of BOS (ie, when patients are still in BOS stage 0) may have an even greater clinical impact than using it as a treatment. In a recent prospective randomized trial of AZM (40 patients) versus placebo (43 patients), Vos and colleagues100 initiated treatment at discharge and followed the patients for 2 years. BOS occurred less in patients receiving AZM (12.5%) than placebo (44.2%), and BOS-free survival was better with AZM. Patients receiving AZM demonstrated better FEV1, lower BAL neutrophilia, and less systemic inflammation. There was no difference in survival between groups, but this may be due to the short follow-up time.
Statins
In a large retrospective study published in 2003, Johnson and colleagues101 found that patients who received statins during the first year after transplantation for treatment of hypercholesterolemia were at less risk of developing BOS than patients who were not treated. In addition, patients receiving statins were less likely to develop severe BOS and had better survival. Unfortunately, there have been no subsequent reports to confirm these observations nor have there been controlled studies. In vitro, it has been demonstrated that simvastatin attenuates the release of airway neutrophilic and remodeling mediators from primary bronchial epithelial cells from stable lung transplant patients and inhibits their up-regulation by transforming growth factor β and IL-17.102 In practice, many lung transplant programs systematically prescribe a statin in order to exploit this immunomodulatory effect even if the true clinical benefit is still hypothetical.
Total Lymphoid Irradiation
Fisher and colleagues103 summarized their experience with total lymphoid irradiation in 37 patients treated for progressive BOS. In the 27 recipients who completed more than 80% of the treatment, the rate of decline in FEV1 decreased from 122.7 mL/mo pre–total lymphoid irradiation to 25.1 mL/mo post–total lymphoid irradiation. Patients with a greater rate of functional decline before treatment were more likely to respond. Results of these studies are promising, but in the absence of adequately powered randomized control trials, they should be regarded as providing suggestive, rather than convincing, evidence.
Photospheresis
Two recent single-center reports document experience with extracorporeal photopheresis in the treatment of BOS. Benden and colleagues104 reported on a series of 12 patients with various stages of BOS; rate of decline in FEV1 was 112 mL/mo before photopheresis and 12 mL/mo after completion of 12 cycles. No complications related to therapy were recorded in this study. In a larger study of 60 patients with BOS, Morrell and colleagues105 documented a similarly dramatic reduction in rate of decline in FEV1 from 116 mL/mo prior to treatment to 28.9 mL/mo during the 6 months after initiation of photopheresis. Eight patients experienced catheter-related bacteremias, one patient had a catheter-associated thrombus, and one patient experienced transient hypotension during a treatment. The mechanisms by which photopheresis exerts immunomodulatory and anti-inflammatory effects remain poorly understood. In the absence of randomized trials, it is premature to endorse photopheresis as a definitive therapy for BOS.
Retransplantation
In 1998, Novick and colleagues106 reported results of 230 retransplants performed at 47 centers worldwide, 63% of which were performed for BOS. The report indicated that early survival after retransplantation was reduced compared with first transplants, but results of retransplants performed for BOS were not different than those done for other indications. In addition, recurrent BOS was observed in a frequency similar to that seen after first transplants. Subsequently, three single-center reports have confirmed this observation. Brugière and colleagues107 reported on long-term outcome in 15 single-lung retransplantations for BOS. The median time between primary lung transplantation and retransplantation was 31 months (range, 12 to 39 months). Actuarial survival rates at 1 year, 2 years, and 5 years after retransplantation were 60%, 53%, and 45%, respectively. Ten patients died during long-term follow-up, 6 of them from infection (60%). The retained graft was the initial site of the fatal infection in 4 of these patients. Two other patients experienced disabling chronic purulent expectoration arising from the old graft. Lung retransplantation thus offered a viable therapeutic option for selected SLT recipients with BOS, but given the morbidity and mortality related to the retained graft, the team now favors replacement of the primary graft when retransplantation is considered.107 Strueber and colleagues108 reported on 54 redo-transplants among 614 lung transplantation procedures performed at their institution. Retransplantation for BOS achieved 1-year and 5-year survival rates of 78% and 62%, respectively, which were not different from those observed after first-time lung transplantations. Recipients had a similar incidence of BOS after retransplantation for BOS versus after a first procedure. The same group published similar results for 7 retransplantations performed in children.109 At present, 1% to 2% of lung transplantations performed yearly worldwide are retransplantations.2 In assessing these procedures, medical issues and the issue of equitable use of scarce resources need be addressed.
Summary
Chronic allograft dysfunction, especially BOS/BO, remains the major obstacle to long-term survival after lung transplantation. Major advances in understanding the risk factors and pathogenic mechanisms leading to irreversible small airway lesions have been made and new options for the prevention and treatment of BOS/BO are available. There is no doubt that the coming years will further improve our ability to cope with this devastating complication of lung transplantation.
References
- 1.Burke C.M., Theodore J., Dawkins K.D. Post-transplant obliterative bronchiolitis and other late lung sequelae in human heart-lung transplantation. Chest. 1984;86:824–829. doi: 10.1378/chest.86.6.824. [DOI] [PubMed] [Google Scholar]
- 2.Christie J.D., Edwards L.B., Kucheryavaya A.Y. The Registry of the International Society for Heart and Lung Transplantation: twenty-seventh official adult lung and heart-lung transplant report—2010. J Heart Lung Transplant. 2010;29:1004–1018. doi: 10.1016/j.healun.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Glanville A.R. Bronchoscopic monitoring after lung transplantation. Semin Respir Crit Care Med. 2010;31:208–221. doi: 10.1055/s-0030-1249117. [DOI] [PubMed] [Google Scholar]
- 4.Estenne M., Maurer J.R., Boehler A. Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria. J Heart Lung Transplant. 2002;21:297–310. doi: 10.1016/s1053-2498(02)00398-4. [DOI] [PubMed] [Google Scholar]
- 5.Jackson C.H., Sharples L.D., McNeil K. Acute and chronic onset of bronchiolitis obliterans syndrome (BOS): are they different entities? J Heart Lung Transplant. 2002;21:658–666. doi: 10.1016/s1053-2498(02)00381-9. [DOI] [PubMed] [Google Scholar]
- 6.Finlen Copeland C.A., Snyder L.D., Zaas D.W. Survival after bronchiolitis obliterans syndrome among bilateral lung transplant recipients. Am J Respir Crit Care Med. 2010;182:784–789. doi: 10.1164/rccm.201002-0211OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bankier A.A., Muylem A.V., Knoop C. BOS in heart-lung transplant recipients: diagnosis with expiratory CT. Radiology. 2001;218:533–539. doi: 10.1148/radiology.218.2.r01fe09533. [DOI] [PubMed] [Google Scholar]
- 8.de Jong P.A., Dodd J.D., Coxson H.O. Bronchiolitis obliterans following lung transplantation: early detection using computed tomographic scanning. Thorax. 2006;61:799–804. doi: 10.1136/thx.2005.053249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heng D., Sharples L.D., McNeil K. Bronchiolitis obliterans syndrome: incidence, natural history, prognosis, and risk factors. J Heart Lung Transplant. 1998;17:1255–1263. [PubMed] [Google Scholar]
- 10.Bando K., Paradis I.L., Similo S. Obliterative bronchiolitis after lung and heart-lung transplantation. An analysis of risk factors and management. J Thorac Cardiovasc Surg. 1995;110:4–13. doi: 10.1016/S0022-5223(05)80003-0. [DOI] [PubMed] [Google Scholar]
- 11.Valentine V.G., Robbins R.C., Berry G.J. Actuarial survival of heart-lung and bilateral sequential lung transplant recipients with obliterative bronchiolitis. J Heart Lung Transplant. 1996;15:371–383. [PubMed] [Google Scholar]
- 12.van den Berg J.W., Geertsma A., van de Bij W. Bronchiolitis obliterans syndrome after lung transplantation and health-related quality of life. Am J Respir Crit Care Med. 2000;161:1937–1941. doi: 10.1164/ajrccm.161.6.9909092. [DOI] [PubMed] [Google Scholar]
- 13.Martinu T., Howell D.N., Davis R.D. Pathologic correlates of bronchiolitis obliterans syndrome in pulmonary retransplant recipients. Chest. 2006;129:1016–1023. doi: 10.1378/chest.129.4.1016. [DOI] [PubMed] [Google Scholar]
- 14.Gerhardt S.G., McDyer J.F., Girgis R.E. Maintenance azithromycin therapy for bronchiolitis obliterans syndrome: results of a pilot study. Am J Respir Crit Care Med. 2003;168:121–125. doi: 10.1164/rccm.200212-1424BC. [DOI] [PubMed] [Google Scholar]
- 15.Verleden G.M., Dupont L.J. Azithromycin therapy for patients with bronchiolitis obliterans syndrome after lung transplantation. Transplantation. 2004;77:1465–1467. doi: 10.1097/01.tp.0000122412.80864.43. [DOI] [PubMed] [Google Scholar]
- 16.Yates B., Murphy D.M., Forrest I.A. Azithromycin reverses airflow obstruction in established bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2005;172:772–775. doi: 10.1164/rccm.200411-1537OC. [DOI] [PubMed] [Google Scholar]
- 17.Shitrit D., Bendayan D., Gidon S. Long-term azithromycin use for treatment of bronchiolitis obliterans syndrome in lung transplant recipients. J Heart Lung Transplant. 2005;24:1440–1443. doi: 10.1016/j.healun.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Verleden G.M., Vanaudenaerde B.M., Dupont L.J. Azithromycin reduces airway neutrophilia and IL-8 in patients with bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2006;174:566–570. doi: 10.1164/rccm.200601-071OC. [DOI] [PubMed] [Google Scholar]
- 19.Porhownik N.R., Batobara W., Kepron W. Effect of maintenance azithromycin on established bronchiolitis obliterans syndrome in lung transplnat patients. Can Respir J. 2008;15:199–202. doi: 10.1155/2008/158681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gottlieb J., Szangolies J., Koehnlein T. Long-term azithromycin for bronchiolitis obliterans syndrome after lung transplantation. Transplantation. 2008;85:36–41. doi: 10.1097/01.tp.0000295981.84633.bc. [DOI] [PubMed] [Google Scholar]
- 21.Benden C., Boehler A. Long-term clarithromycin therapy in the management of lung transplant recipients. Transplantation. 2009;87:1538–1540. doi: 10.1097/TP.0b013e3181a492b2. [DOI] [PubMed] [Google Scholar]
- 22.Verleden G.M., Vos R., De Vleeschauwer S.I. Obliterative bronchiolitis following lung transplantation: from old to new concepts? Transpl Int. 2009;22:771–779. doi: 10.1111/j.1432-2277.2009.00872.x. [DOI] [PubMed] [Google Scholar]
- 23.Pakhale S.S., Hadjiliadis D., Howell D.N. Upper lobe fibrosis: a novel manifestation of chronic allograft dysfunction in lung transplantation. J Heart Lung Transplant. 2005;24:1260–1268. doi: 10.1016/j.healun.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 24.Woodrow J.P., Shlobin O.A., Barnett S.D. Comparison of bronchiolitis obliterans syndrome to other forms of chronic lung allograft dysfunction after lung transplantation. J Heart Lung Transplant. 2010;29:1159–1164. doi: 10.1016/j.healun.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 25.Ferrer J., Roldan J., Roman A. Acute and chronic pleural complications in lung transplantation. J Heart Lung Transplant. 2003;22:1217–1225. doi: 10.1016/s1053-2498(02)01230-5. [DOI] [PubMed] [Google Scholar]
- 26.McManus T.E., Milne D.G., Whyte K.F. Exudative bronchiolitis after lung transplantation. J Heart Lung Transplant. 2008;27:276–281. doi: 10.1016/j.healun.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 27.Vos R., Vanaudenaerde B.M., De Vleeschauwer S.I. Follicular bronchiolitis: a rare cause of bronchiolitis obliterans syndrome after lung transplantation: a case report. Am J Transplant. 2009;9:644–650. doi: 10.1111/j.1600-6143.2008.02518.x. [DOI] [PubMed] [Google Scholar]
- 28.Akindipe O., Fernandez-Bussy S., Jantz M. Obliterative bronchiolitis in lung allografts removed at retransplant for intractable airway problems. Respirology. 2009;14:601–605. doi: 10.1111/j.1440-1843.2009.01513.x. [DOI] [PubMed] [Google Scholar]
- 29.Halloran P.F., Homik J., Goes N. The “injury response”: a concept linking nonspecific injury, acute rejection, and long-term transplant outcomes. Transplant Proc. 1997;29:79–81. doi: 10.1016/s0041-1345(96)00015-2. [DOI] [PubMed] [Google Scholar]
- 30.Egan J.J. Obliterative bronchiolitis after lung transplantation: a repetitive multiple injury airway disease. Am J Respir Crit Care Med. 2004;170:931–932. doi: 10.1164/rccm.2408010. [DOI] [PubMed] [Google Scholar]
- 31.Opelz G., Süsal C., Ruhenstroth A. Impact of HLA compatibility on lung transplant survival and evidence for an HLA restriction phenomenon: a collaborative transplant study report. Transplantation. 2010;90:912–917. doi: 10.1097/TP.0b013e3181f2c981. [DOI] [PubMed] [Google Scholar]
- 32.Keogh A., Kaan A., Doran T. HLA mismatching and outcome in heart, heart-lung and single lung transplantation. J Heart Lung Transplant. 1995;14:444–451. [PubMed] [Google Scholar]
- 33.Schulman L.L., Weinberg A.D., McGregor C. Mismatches at the HLA-DR and HLA-B loci are risk factors for acute rejection after lung transplantation. Am J Respir Crit Care Med. 1998;157:1833–1837. doi: 10.1164/ajrccm.157.6.9707007. [DOI] [PubMed] [Google Scholar]
- 34.Quantz M.A., Bennett L.E., Meyer D.M. Does human leukocyte antigen matching influence the outcome of lung transplantation? An analysis of 3,549 lung transplantations. J Heart Lung Transplant. 2000;19:473–479. doi: 10.1016/s1053-2498(00)00081-4. [DOI] [PubMed] [Google Scholar]
- 35.Girnita A.L., McCurry K.R., Iacono A.T. HLA-specific antibodies are associated with high-grade and persistent-recurrent lung allograft acute rejection. J Heart Lung Transplant. 2004;23:1135–1141. doi: 10.1016/j.healun.2003.08.030. [DOI] [PubMed] [Google Scholar]
- 36.Girnita A.L., Duquesnoy R., Yousem S.A. HLA-specific antibodies are risk factors for lymphocytic bronchiolitis and chronic lung allograft dysfunction. Am J Transplant. 2005;5:131–138. doi: 10.1111/j.1600-6143.2004.00650.x. [DOI] [PubMed] [Google Scholar]
- 37.Jaramillo A., Smith M.A., Phelan D. Development of ELISA-detected anti-HLA antibodies precedes the development of bronchiolitis obliterans syndrome and correlates with progressive decline in pulmonary function after lung transplantation. Transplantation. 1999;67:1155–1156. doi: 10.1097/00007890-199904270-00012. [DOI] [PubMed] [Google Scholar]
- 38.Palmer S.M., Davis R.D., Hadjiliadis D. Development of an antibody specific to major histocompatibility antigens detectable by flow cytometry after lung transplant is associated with bronchiolitis obliterans syndrome. Transplantation. 2002;74:799–804. doi: 10.1097/00007890-200209270-00011. [DOI] [PubMed] [Google Scholar]
- 39.Girnita A.L., McCurry K.R., Zeevi A. Increased lung allograft failure in patients with HLA-specific antibody. Clin Transpl. 2007:231–239. [PubMed] [Google Scholar]
- 40.Jaramillo A., Smith C.R., Maruyama T. Anti-HLA class I antibody binding to airway epithelial cells induces production of fibrogenic growth factors and apoptotic cell death: a possible mechanism for bronchiolitis obliterans syndrome. Hum Immunol. 2003;64:521–529. doi: 10.1016/s0198-8859(03)00038-7. [DOI] [PubMed] [Google Scholar]
- 41.Yousem S.A. Significance of clinically silent untreated mild acute cellular rejection in lung allograft recipients. Hum Pathol. 1996;27:269–273. doi: 10.1016/s0046-8177(96)90068-4. [DOI] [PubMed] [Google Scholar]
- 42.Knoop C., Estenne M. Acute and chronic rejection after lung transplantation. Semin Respir Crit Care Med. 2006;27:521–533. doi: 10.1055/s-2006-954609. [DOI] [PubMed] [Google Scholar]
- 43.Hopkins P.M., Aboyoun C.L., Chhajed P.N. Association of minimal rejection in lung transplant recipients with obliterative bronchiolitis. Am J Respir Crit Care Med. 2004;170:1022–1026. doi: 10.1164/rccm.200302-165OC. [DOI] [PubMed] [Google Scholar]
- 44.Khalifah A.P., Hachem R.R., Chakinala M.M. Minimal acute rejection after lung transplantation: a risk for bronchiolitis obliterans syndrome. Am J Transplant. 2005;5:2022–2030. doi: 10.1111/j.1600-6143.2005.00953.x. [DOI] [PubMed] [Google Scholar]
- 45.Hachem R.R., Khalifah A.P., Chakinala M.M. The significance of a single episode of minimal acute rejection after lung transplantation. Transplantation. 2005;80:1406–1413. doi: 10.1097/01.tp.0000181161.60638.fa. [DOI] [PubMed] [Google Scholar]
- 46.Ross D.J., Marchevsky A., Kramer M. Refractoriness of airflow obstruction associated with isolated lymphocytic bronchiolitis/bronchitis in pulmonary allografts. J Heart Lung Transplant. 1997;16:832–838. [PubMed] [Google Scholar]
- 47.Husain A.N., Siddiqui M.T., Holmes E.W. Analysis of risk factors for the development of bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 1999;159:829–833. doi: 10.1164/ajrccm.159.3.9607099. [DOI] [PubMed] [Google Scholar]
- 48.Glanville A.R., Aboyoun C.L., Havryk A. Severity of lymphocytic bronchiolitis predicts long-term outcome after lung transplantation. Am J Respir Crit Care Med. 2008;177:1033–1040. doi: 10.1164/rccm.200706-951OC. [DOI] [PubMed] [Google Scholar]
- 49.Burton C.M., Iversen M., Scheike T. Is lymphocytic bronchiolitis a marker of acute rejection? An analysis of 2,697 transbronchial biopsies after lung transplantation. J Heart Lung Transplant. 2008;27:1128–1134. doi: 10.1016/j.healun.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 50.Glanville A.R. Antibody-mediated rejection in lung transplantation: myth or reality? J Heart Lung Transplant. 2010;29:395–400. doi: 10.1016/j.healun.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 51.Morrell M.R., Patterson G.A., Trulock E.P. Acute antibody-mediated rejection after lung transplantation. J Heart Lung Transplant. 2009;28:96–100. doi: 10.1016/j.healun.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 52.Magro C.M., Abbas A.E., Seilstad K. C3d and the septal microvasculature as a predictor of chronic lung allograft dysfunction. Hum Immunol. 2006;67:274–283. doi: 10.1016/j.humimm.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 53.Burlingham W.J., Love R.B., Jankowska-Gan E. IL-17-dependent cellular immunity to collagen type V predisposes to obliterative bronchiolitis in human lung transplants. J Clin Invest. 2007;117:3498–3506. doi: 10.1172/JCI28031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goers T.A., Ramachandran S., Aloush A. De novo production of K-alpha1 tubulin-specific antibodies: role in chronic lung allograft rejection. Hum Immunol. 2008;180:4487–4494. doi: 10.4049/jimmunol.180.7.4487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tiriveedhi V., Angaswamy N., Weber J. Lipid raft facilitated ligation of K-alpha1-tubulin by specific antibodies on epithelial cells: role in pathogenesis of chronic rejection following human lung transplantation. Biochem Biophys Res Commun. 2010;399:251–255. doi: 10.1016/j.bbrc.2010.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nath D.S., Basha H.I., Mohanakumar T. Antihuman leukocyte antigen antibody-induced autoimmunity: role in chronic rejection. Curr Opin Organ Transplant. 2010;15:16–20. doi: 10.1097/MOT.0b013e3283342780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shilling R.A., Wilkes D.S. Immunobiology of chronic lung allograft dysfunction: new insights from the bench and beyond. Am J Transplant. 2009;9:1714–1718. doi: 10.1111/j.1600-6143.2009.02690.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kastelijn E.A., van Moorsel C.H., Rijkers G.T. Polymorphisms in innate immunity genes associated with development of bronchiolitis obliterans after lung transplantation. J Heart Lung Transplant. 2010;29:665–671. doi: 10.1016/j.healun.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 59.Botha P., Archer L., Anderson R.L. Pseudomonas aeruginosa colonization of the allograft after lung transplantation and the risk of bronchiolitis obliterans syndrome. Transplantation. 2008;85:771–774. doi: 10.1097/TP.0b013e31816651de. [DOI] [PubMed] [Google Scholar]
- 60.Weigt S.S., Elashoff R.M., Huang C. Aspergillus colonization of the lung allograft is a risk factor for bronchiolitis obliterans syndrome. Am J Transplant. 2009;9:1903–1911. doi: 10.1111/j.1600-6143.2009.02635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Valentine V.G., Gupta M.R., Walker J.E., Jr. Effect of etiology and timing of respiratory tract infections on development of bronchiolitis obliterans syndrome. J Heart Lung Transplant. 2009;28:163–169. doi: 10.1016/j.healun.2008.11.907. [DOI] [PubMed] [Google Scholar]
- 62.Kumar D., Husain S., Chen M.H. A prospective molecular surveillance study evaluating the clinical impact of community-acquired respiratory viruses in lung transplant recipients. Transplantation. 2010;89:1028–1033. doi: 10.1097/TP.0b013e3181d05a71. [DOI] [PubMed] [Google Scholar]
- 63.Gottlieb J., Schulz T.F., Welte T. Community-acquired respiratory viral infections in lung transplant recipients: a single season cohort study. Transplantation. 2009;87:1530–1537. doi: 10.1097/TP.0b013e3181a4857d. [DOI] [PubMed] [Google Scholar]
- 64.Glanville A.R., Gencay M., Tamm M. Chlamydia pneumoniae infection after lung transplantation. J Heart Lung Transplant. 2005;24:131–136. doi: 10.1016/j.healun.2003.09.042. [DOI] [PubMed] [Google Scholar]
- 65.Kotsimbos T.C., Snell G.I., Levvey B. Chlamydia pneumoniae serology in donors and recipients and the risk of bronchiolitis obliterans syndrome after lung transplantation. Transplantation. 2005;79:269–275. doi: 10.1097/01.tp.0000149839.87843.64. [DOI] [PubMed] [Google Scholar]
- 66.Neurohr C., Huppmann P., Leuchte H. Human herpesvirus 6 in bronchalveolar lavage fluid after lung transplantation: a risk factor for bronchiolitis obliterans syndrome? Am J Transplant. 2005;5:2982–2991. doi: 10.1111/j.1600-6143.2005.01103.x. [DOI] [PubMed] [Google Scholar]
- 67.Valentine V.G., Weill D., Gupta M.R. Ganciclovir for cytomegalovirus: a call for indefinite prophylaxis in lung transplantation. J Heart Lung Transplant. 2008;27:875–881. doi: 10.1016/j.healun.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 68.Tamm M., Aboyoun C.L., Chhajed P.N. Treated cytomegalovirus pneumonia is not associated with bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2004;170:1120–1123. doi: 10.1164/rccm.200310-1405OC. [DOI] [PubMed] [Google Scholar]
- 69.Davis C.S., Shankaran V., Kovacs E.J. Gastroesophageal reflux disease after lung transplantation: pathophysiology and implications for treatment. Surgery. 2010;148:737–744. doi: 10.1016/j.surg.2010.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Blondeau K., Mertens V., Vanaudenaerde B.A. Gastro-oesophageal reflux and gastric aspiration in lung transplant patients with or without chronic rejection. Eur Respir J. 2008;31:707–713. doi: 10.1183/09031936.00064807. [DOI] [PubMed] [Google Scholar]
- 71.D’Ovidio F., Mura M., Tsang M. Bile acid aspiration and the development of bronchiolitis obliterans after lung transplantation. J Thorac Cardiovasc Surg. 2005;129:1144–1152. doi: 10.1016/j.jtcvs.2004.10.035. [DOI] [PubMed] [Google Scholar]
- 72.Cantu E., 3rd, Appel J.Z., 3rd, Hartwig M.G. Early fundoplication prevents chronic allograft dysfunction in patients with gastroesophageal reflux disease. Ann Thorac Surg. 2004;78:1142–1151. doi: 10.1016/j.athoracsur.2004.04.044. [DOI] [PubMed] [Google Scholar]
- 73.Davis R.D., Jr., Lau C.L., Eubanks S. Improved lung allograft function after fundoplication in patients with gastroesophageal reflux disease undergoing lung transplantation. J Thorac Cardiovasc Surg. 2003;125:533–542. doi: 10.1067/mtc.2003.166. [DOI] [PubMed] [Google Scholar]
- 74.Robertson A.G., Ward C., Pearson J.P. Lung transplantation, gastroesophageal reflux, and fundoplication. Ann Thorac Surg. 2010;89:653–660. doi: 10.1016/j.athoracsur.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 75.Snell G.I., Westall G.P. The contribution of airway ischemia and vascular remodelling to the pathophysiology of bronchiolitis obliterans syndrome and chronic lung allograft dysfunction. Curr Opin Organ Transplant. 2010;15:558–562. doi: 10.1097/MOT.0b013e32833e1112. [DOI] [PubMed] [Google Scholar]
- 76.Daud S.A., Yusen R.D., Meyers B.F. Impact of immediate primary lung allograft dysfunction on bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2007;175:507–513. doi: 10.1164/rccm.200608-1079OC. [DOI] [PubMed] [Google Scholar]
- 77.Belperio J.A., Keane M.P., Burdik M.D. Role of CXCR2/CXCR2 ligands in vascular remodelling during bronchiolitis obliterans syndrome. J Clin Invest. 2005;115:1150–1162. doi: 10.1172/JCI24233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Douglas I.S., Nicolls M.R. Chemokine-mediated angiogenesis: an essential link in the evolution of airway fibrosis? J Clin Invest. 2005;115:1133–1136. doi: 10.1172/JCI25193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dhillon G.S., Zamora M.R., Roos J.E. Lung transplant airway hypoxia: a diathesis to fibrosis? Am J Respir Crit Care Med. 2010;182:230–236. doi: 10.1164/rccm.200910-1573OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hachem R.R., Chakinala M.M., Yusen R.D. The predictive value of bronchiolitis obliterans syndrome stage 0-p. Am J Respir Crit Care Med. 2004;169:468–472. doi: 10.1164/rccm.200307-1018OC. [DOI] [PubMed] [Google Scholar]
- 81.Lama I.N., Murray S., Mumford J.A. Prognostic value of bronchiolitis obliterans syndrome stage 0-p in single-lung transplant recipients. Am J Respir Crit Care Med. 2005;172:379–383. doi: 10.1164/rccm.200501-097OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Estenne M., Van Muylem A., Knoop C. Detection of obliterative bronchiolitis by indexes of ventilation distribution. Am J Respir Crit Care Med. 2000;162:1047–1051. doi: 10.1164/ajrccm.162.3.9912063. [DOI] [PubMed] [Google Scholar]
- 83.Reynaud-Gaubert M., Thomas P., Badier M. Early detection of airway involvement in obliterative bronchiolitis after lung transplantation. Functional and bronchoalveolar lavage cell findings. Am J Respir Crit Care Med. 2000;161:1924–1929. doi: 10.1164/ajrccm.161.6.9905060. [DOI] [PubMed] [Google Scholar]
- 84.Van Muylem A., Knoop C., Estenne M. Early detection of chronic pulmonary allograft dysfunction by exhaled biomarkers. Am J Respir Crit Care Med. 2007;175:731–736. doi: 10.1164/rccm.200609-1301OC. [DOI] [PubMed] [Google Scholar]
- 85.Van Muylem A., Scillia P., Knoop C. Single-breath test in lateral decubitus reflects function of single lungs grafted for emphysema. J Appl Physiol. 2006;100:834–838. doi: 10.1152/japplphysiol.01307.2005. [DOI] [PubMed] [Google Scholar]
- 86.Van Muylem A., Gevenois P.A., Kallinger E. Single-breath test in lateral decubitus reflects function of single lungs grafted for interstitial lung disease. J Appl Physiol. 2008;104:224–229. doi: 10.1152/japplphysiol.00582.2007. [DOI] [PubMed] [Google Scholar]
- 87.Gabbay E., Haydn Walters E., Orsida B. In stable lung transplant recipients, exhaled nitric oxide levels positively correlate with airway neutrophilia and bronchial epithelial iNOS. Am J Respir Crit Care Med. 1999;160:2093–2099. doi: 10.1164/ajrccm.160.6.9902088. [DOI] [PubMed] [Google Scholar]
- 88.Gabbay E., Walters E.H., Orsida B. Post-lung transplant bronchiolitis obliterans syndrome (BOS) is characterized by increased exhaled nitric oxide levels and epithelial inducible nitric oxide synthase. Am J Respir Crit Care Med. 2000;162:2182–2187. doi: 10.1164/ajrccm.162.6.9911072. [DOI] [PubMed] [Google Scholar]
- 89.Zheng L., Whitford H.M., Orsida B. The dynamics and associations of airway neutrophilia post lung transplantation. Am J Transplant. 2006;6:599–608. doi: 10.1111/j.1600-6143.2006.01222.x. [DOI] [PubMed] [Google Scholar]
- 90.Vos R., Cordemans C., Vanaudenaerde B.M. Exhaled carbon monoxide as a noninvasive marker of airway neutrophilia after lung transplantation. Transplantation. 2009;87:1579–1583. doi: 10.1097/TP.0b013e3181a4e69c. [DOI] [PubMed] [Google Scholar]
- 91.Fisher A.J., Gabbay E., Small T. Cross sectional study of exhaled nitric oxide levels following lung transplantation. Thorax. 1998;53:454–458. doi: 10.1136/thx.53.6.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Verleden G.M., Dupont L.J., Van Raemdonck D.E. Accuracy of exhaled nitric oxide measurements for the diagnosis of bronchiolitis obliterans syndrome after lung transplantation. Transplantation. 2004;78:730–733. doi: 10.1097/01.tp.0000131814.44106.c0. [DOI] [PubMed] [Google Scholar]
- 93.Brugiere O., Thabut G., Mal H. Exhaled NO may predict the decline in lung function in bronchiolitis obliterans syndrome. Eur Respir J. 2005;25:813–819. [Google Scholar]
- 94.Dupont L.J., Dewandeleer Y., Vanaudenaerde B.M. The pH of exhaled breath condensate of patients with allograft rejection after lung transplantation. Am J Transplant. 2006;6:1486–1492. doi: 10.1111/j.1600-6143.2006.01331.x. [DOI] [PubMed] [Google Scholar]
- 95.Allen D.J., Fildes J.E., Yonan N. Changes in induced sputum in the presence of bronchiolitis obliterans syndrome and correlation with spirometry in single and bilateral lung transplant recipients. J Heart Lung Transplant. 2005;24:88–91. doi: 10.1016/j.healun.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 96.Bankier A.A., Van Muylem A., Scillia P. Air trapping in heart-lung transplant recipients: variability of anatomic distribution and extent at sequential expiratory thin-section CT. Radiology. 2003;229:737–742. doi: 10.1148/radiol.2293020827. [DOI] [PubMed] [Google Scholar]
- 97.Gast K.K., Zaporozhan J., Ley S. (3)He-MRI in follow-up of lung transplant recipients. Eur Radiol. 2004;14:78–85. doi: 10.1007/s00330-003-2092-4. [DOI] [PubMed] [Google Scholar]
- 98.Vos R., Vanaudenaerde B.M., Ottevaere A. Long-term azithromycin therapy for bronchiolitis obliterans syndrome: divide and conquer? J Heart Lung transplant. 2010;29:1358–1368. doi: 10.1016/j.healun.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 99.Jain R., Hachem R.R., Morrell M.R. Azithromycin is associated with increased survival in lung transplant recipients with bronchiolitis obliterans syndrome. J Heart Lung Transplant. 2010;29:531–537. doi: 10.1016/j.healun.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Vos R., Vanaudenaerde B.M., Verleden S.E. A randomized placebo-controlled trial of azithromycin to prevent bronchiolitis obliterans syndrome after lung transplantation. Eur Respir J. 2011;37:164–172. doi: 10.1183/09031936.00068310. [DOI] [PubMed] [Google Scholar]
- 101.Johnson B.A., Iacono A.T., Zeevi A. Statin use is associated with improved function and survival of lung allografts. Am J Respir Crit Care Med. 2003;167:1271–1278. doi: 10.1164/rccm.200205-410OC. [DOI] [PubMed] [Google Scholar]
- 102.Murphy D.M., Forrest I.A., Corris P.A. Simvastatin attenuates release of neutrophilic and remodeling factors from primary bronchial epithelial cells derived from stable lung transplant recipients. Am J Physiol Lung Cell Mol Physiol. 2008;294:L592–L599. doi: 10.1152/ajplung.00386.2007. [DOI] [PubMed] [Google Scholar]
- 103.Fisher A.J., Rutherford R.M., Bozzino J. The safety and efficacy of total lymphoid irradiation in progressive bronchiolitis obliterans syndrome after lung transplantation. Am J Transplant. 2005;5:537–543. doi: 10.1111/j.1600-6143.2004.00709.x. [DOI] [PubMed] [Google Scholar]
- 104.Benden C., Speich R., Wanger C. Extracorporeal photopheresis after lung transplantation: a 10-year single-center experience. Transplantation. 2008;86:1625–1627. doi: 10.1097/TP.0b013e31818bc024. [DOI] [PubMed] [Google Scholar]
- 105.Morrell M.R., Despotis G.J., Lublin D.M. The efficacy of photopheresis for bronchiolitis obliterans syndrome after lung transplantation. J Heart Lung Transplant. 2010;29:424–431. doi: 10.1016/j.healun.2009.08.029. [DOI] [PubMed] [Google Scholar]
- 106.Novick R.J., Stitt L.W., Al-Kattan K. Pulmonary retransplantation: predictors of graft function and survival in 230 patients. Pulmonary Retransplant Registry. Ann Thorac Surg. 1998;65:227–234. doi: 10.1016/s0003-4975(97)01191-0. [DOI] [PubMed] [Google Scholar]
- 107.Brugière O., Thabut G., Castier Y. Lung retransplantation for bronchiolitis obliterans syndrome: long-term follow-up in a series of 15 recipients. Chest. 2003;123:1832–1837. doi: 10.1378/chest.123.6.1832. [DOI] [PubMed] [Google Scholar]
- 108.Strueber M., Fischer S., Gottlieb J. Long-term outcome after pulmonary retransplantation. J Thorac Cardiovasc Surg. 2006;132:407–412. doi: 10.1016/j.jtcvs.2005.12.059. [DOI] [PubMed] [Google Scholar]
- 109.Müller C., Görler H., Ballmann M. Pulmonary retransplantation in paediatric patients: a justified therapeutic option? A single-centre experience. Eur J Cardiothorac Surg. 2011;39:201–205. doi: 10.1016/j.ejcts.2010.05.012. [DOI] [PubMed] [Google Scholar]