Abstract
High ventilation rate is shown to be effective for reducing cross-infection risk of airborne diseases in hospitals and isolation rooms. Natural ventilation can deliver much higher ventilation rate than mechanical ventilation in an energy-efficient manner. This paper reports a field measurement of naturally ventilated hospital wards in Hong Kong and presents a possibility of using natural ventilation for infection control in hospital wards. Our measurements showed that natural ventilation could achieve high ventilation rates especially when both the windows and the doors were open in a ward. The highest ventilation rate recorded in our study was 69.0 ACH. The airflow pattern and the airflow direction were found to be unstable in some measurements with large openings. Mechanical fans were installed in a ward window to create a negative pressure difference. Measurements showed that the negative pressure difference was negligible with large openings but the overall airflow was controlled in the expected direction. When all the openings were closed and the exhaust fans were turned on, a reasonable negative pressure was created although the air temperature was uncontrolled.
The high ventilation rate provided by natural ventilation can reduce cross-infection of airborne diseases, and thus it is recommended for consideration of use in appropriate hospital wards for infection control. Our results also demonstrated a possibility of converting an existing ward using natural ventilation to a temporary isolation room through installing mechanical exhaust fans.
Keywords: Natural ventilation, Isolation room, Ventilation rate, Infection control
1. Introduction
Air environment control in hospitals has received increasing attention since the 2003's severe acute respiratory syndrome (SARS) epidemics and due to the expected threat of influenza pandemic. There were various reports of large nosocomial SARS outbreaks [1], [2], [3], [4], [5], [6], [7], [8], and some of them suggested the possible roles played by air environment in hospital wards. To minimize the cross-infection risk, engineering control methods were suggested in the so-called AII (airborne infection isolation) rooms [9]. The most well-known is the imbalanced mechanical ventilation system to achieve negative pressure relative to the corridor [9]. These mechanical negative pressure isolation rooms are expensive to build and operate, and the ventilation flow rate is limited to 12 air change/h [9]. Li et al. reviewed studies of ventilation and infections and found that there was lack of strong scientific evidence for recommending a minimum ventilation flow rate for infection control [10]. It is known that a higher ventilation rate is able to provide a higher dilution capability. However, use of higher ventilation rates also means a higher energy cost for mechanical ventilation. Alternative ventilation control systems have also been considered, e.g. when there is an immediate need for reconfiguring existing patient rooms to serve as airborne isolation rooms. Exhaust fans were installed in the windows of an air-conditioned ward to create negative pressure during the SARS epidemics [11], [12], [13], [14]. Temporary isolation rooms were also created during the SARS epidemic from the existing hospital wards.
The risk of infection with an exposure can be calculated from the classical Wells–Riley equation [15], which was developed for predicting the risk of airborne transmission diseases; see Eq. (1):
| (1) |
where P is the risk of airborne transmitted diseases, p is the pulmonary ventilation rate of each susceptible per minute (m3/h), n is the air change rate (ACH), q is the quanta produced by one infector (quanta/h); a quantum of infection is the dose which is necessary to cause infection to a new susceptible and may be one or more airborne particles, V is the volume of enclosed space (m3), and t is the duration of exposure (h).
The effectiveness of high ventilation rate in infection risk reduction can be demonstrated by Fig. 1 , which shows the relationship between the ventilation rate and the infection risk, parameterized in relation to the quanta generation in an enclosed space with 108 m3 volume in 1 h.
Fig. 1.
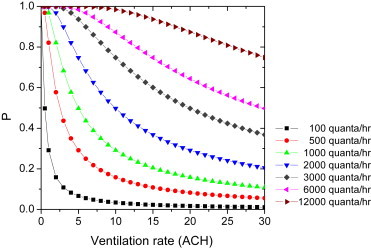
The relationship between infection risk, and the ventilation rate and the quanta generation. The unit of quanta generation is quanta per hour.
Maximizing natural ventilation was suggested for infection control in resource-limited regions [16], but without providing any technical details. To our knowledge, Escombe et al. was the first recent publication of suggesting the use of natural ventilation for infection control with field measurement data [17], and a full paper was published in 2007 [18]. Natural ventilation was shown to be effective in reducing nosocomial transmission of tuberculosis in Peru, although no epidemiological data were available. This finding is not new as it was revealed more than 100 years ago that the outdoor treatment of tuberculosis might be more effective [19]. Jiang et al. also found that large ventilation windows in two hospital buildings reduced the infection risk by the healthcare workers during the 2003 SARS outbreak in Guangdong [20]. The ultimate acceptance of natural ventilation for isolation and infection control purposes will be helpful for creating temporary isolation room as the supplementary of standard isolation room when emergency infectious epidemic broke out. And it is hoped to be helpful for making isolation wards available to their patients with low costs in resource-limited countries [21].
Natural ventilation uses natural forces, i.e. wind and density difference to drive airflow within and around the buildings. Generally, natural ventilation can provide a high ventilation rate more economically than mechanical ventilation, and its airflow and temperature are difficult to predict and control. However, modern natural ventilation is also a technology-dependent solution similar to mechanical systems. Unlike traditional natural ventilation systems, natural ventilation today depends on modern computer control system, modern design of ventilation openings, assisting fan design, etc. Thus, if properly designed, natural ventilation can also be reliable, in particular if combined with a mechanical system using the hybrid ventilation principle [22]. It should be mentioned here that the cost of hybrid and modern designed natural ventilation systems could be high for resource-limited countries, which is similar to those of mechanical ventilation system.
The purpose of this paper is to evaluate the possibility of using natural ventilation for infection control using the measurement data in Hong Kong. We carried out a field measurement study in a naturally ventilated outpatient clinic and a naturally ventilated TB hospital in Hong Kong. Unlike the field measurement of Escombe et al. [18], we investigated the ventilation performance of natural ventilation with and without exhaust fans and discussed the implications of the airflow-direction control. The results were used to evaluate the possibility of applying natural ventilation in hospitals for infection control.
2. Materials and methods
Located in the Hong Kong Island, both a TB hospital GH and an outpatient clinic SYP with naturally ventilated wards were selected for the study. Hospital GH, the only one existing naturally ventilated TB hospital in Hong Kong, is located on a hillside surrounded by green environments. Various design alternations were done since then to cater for the hot and humid summer, e.g. installing spot air cooling when needed. There were exhaust fans installed in the doorway between the corridor and the ward, between the ward and the balcony, and also between the toilet and the ambient. One exhaust fan between the corridor and the ward was installed above the doorway and two exhaust fans were installed at the top of the windows to exhaust air from the ward to the outdoor. Outpatient clinic SYP is located in the Western District of Hong Kong Island surrounded by high buildings. The outpatient clinic includes consultation rooms and a waiting area. Each consultation room has exterior windows and a door connected to the corridor. A window air conditioner was installed in the windows in each consultation room. We measured the waiting area and a consultation room.
During our measurement, a tested ward was first vacated by the hospital. Thermal manikins were used to simulate thermal buoyancy flows of the inpatients. The heat generation of each thermal manikin was 76 W corresponding to an adult at rest. The field measurement was carried out in four TB wards in Hospital GH on 9–10 November 2005 and 28 August 2006, and in the outpatient clinic SYP on 5 November 2005. Literature shows that short-term airing by natural ventilation shows high ventilation efficiency, especially for the first 10 min [23]. In this study, it needs more than half an hour to dose and mix the tracer gas in the ward in each test. So in spite of that the short period of measurement in this study may not reflect the average yearly or monthly natural ventilation rate accurately. But it still can indicate the performance of natural ventilation in typical weather conditions and evaluate the influence of size of openings, wind speed, and direction.
Pressure difference, airflow direction through doorways and windows, and air change rate were measured. Pressure difference and air velocity was measured by VELOCICAL Plus air velocity meter (8386A) (TSI Inc., Shoreview, MN, USA). A small hand-hold smoke generator (CH25301) (Drager, Germany) was used to visualize the local airflow direction. A hood flow rate meter (APM 150) (TSI Inc., Shoreview, MN, USA) was used to measure the airflow rate of the exhaust fans.
The decay method was employed to measure the air change rate. A tracer gas sulfur hexafluoride (SF6) was injected continually in the ward until the concentration of the tracer gas became steady, then the injecting was stopped, and the concentration decay was measured. Two electrical fans were used to make the air mixed in the ward during the measurement, one of the mixing fans was placed behind the doser and the other one, an oscillating fan, on top of the ceiling. The injection of SF6 was controlled by multi-gas sampler and doser type 1303 (Bruel&Kjar, Denmark), and the concentration of SF6 was measured by the single-gas monitor 3425 (Bruel&Kjar, Denmark). Those two machines were controlled by a laptop through software 7620 (Bruel&Kjar, Denmark). The concentration of the tracer gas was measured continuously. According to the concentration decay curve, the ventilation rate can be determined according to the following equation:
| (2) |
where C(τ) is the tracer gas concentration at τ time and n is the air change rate (ACH).
3. Results
3.1. Air change rate
Table 1 summarizes the measured results of ventilation rates for different situations including the situations when the doors and the windows were closed or not, and the exhaust fans were turned on or off.
-
●
Effect of surrounded environments of hospital
Table 1.
The measured ventilation rates due to natural ventilation.
| Test | Date | Location | Windows/doors to outdoor | Door to corridor | Fans | Room type | Outdoor conditions |
ACH (average value) | |
|---|---|---|---|---|---|---|---|---|---|
| Wind speed/direction (°) | Temperature (°C) | ||||||||
| 1a | 9-11, 2005 | Cubicle 7; 6/F,GH | 100% open | 100% open | Off | 2 beds ward | 3.2/160 | 28.7 | 30.3 |
| 2 | 9-11, 2005 | Cubicle 7; 6/F,GH | 100% open | Close | Off | 2 beds ward | 2.9/150 | 29.4 | 17.6 |
| 3 | 9-11, 2005 | Cubicle 7; 6/F,GH | 50% open | Close | Off | 2 beds ward | 2.8/170 | 29.4 | 14.6 |
| 4 | 9-11, 2005 | Cubicle 4; 6/F,GH | 100% open | 100% open | Off | 2 beds ward | 3/160 | 29.3 | 42.2 |
| 5 | 9-11, 2005 | Cubicle 4; 6/F,GH | 100% open | Close | Off | 2 beds ward | 2.4/170 | 29.1 | 15.4 |
| 6 | 9-11, 2005 | Cubicle 4; 6/F,GH | 50% open | Close | Off | 2 beds ward | 2.2/160 | 27.0 | 10.7 |
| 7 | 9-11, 2005 | Cubicle 4; 6/F,GH | 100% open | Close | On | 2 beds ward | 1.8/200 | 26.5 | 22.5 |
| 8a, b | 10-11, 2005 | Cubicle 0; 2/F,GH | 100% open | 100% open | Off | 2 beds ward | 2.5/150 | 28.3 | 60.2 |
| 9b | 10-11, 2005 | Cubicle 0; 2/F,GH | 100% open | Close | Off | 2 beds ward | 3.4/150 | 28.5 | 16.0 |
| 10b | 10-11, 2005 | Cubicle 0; 2/F,GH | 50% open | Close | Off | 2 beds ward | 4.1/165 | 28.7 | 12.9 |
| 11b | 10-11, 2005 | Cubicle 7; 2/F,GH | 100% open | 100% open | Off | 5 beds ward | 3.2/160 | 29.2 | 69.0 |
| 12 | 10-11, 2005 | Cubicle 7; 2/F,GH | 100% open | Close | Off | 5 beds ward | 3.2/135 | 28.9 | 31.6 |
| 13 | 10-11, 2005 | Cubicle 7; 2/F,GH | 50% open | Close | Off | 5 beds ward | 3.1/110 | 29.2 | 23.5 |
| 14 | 10-11, 2005 | Cubicle 7; 2/F,GH | Close | 100% open | Off | 5 beds ward | 2.4/130 | 28.2 | 8.7 |
| 15 | 28-08, 2006 | Cubicle 4; 6/F,GH | Close | Close | Off | 2 beds ward | 2.7/150 | 29.3 | 0.71 |
| 16 | 28-08, 2006 | Cubicle 4; 6/F,GH | 100% open | Close | Off | 2 beds ward | 4.8/90 | 30.4 | 14.0 |
| 17 | 28-08, 2006 | Cubicle 4; 6/F,GH | 100% open | 100% open | Off | 2 beds ward | 4.5/95 | 29.3 | 18.5 (8.8)c |
| 18 | 28-08, 2006 | Cubicle 4; 6/F,GH | Close | Close | On | 2 beds ward | 2.7/140 | 28.4 | 12.6 |
| 19 | 28-08, 2006 | Cubicle 4; 6/F,GH | 100% open | Close | On | 2 beds ward | 4.1/120 | 29.9 | 14.6 |
| 20 | 28-08, 2006 | Cubicle 4; 6/F,GH | 100% open | 100% open | On | 2 beds ward | 4.1/100 | 29.5 | 29.2 |
| 21a | 6-11, 2005 | Cubicle 4; 2/F, SYP | 100% open | 100% open | Off | Single room | 1.9/165 | 28.7 °C | 18.8 |
| 22a | 6-11, 2005 | Cubicle 4; 2/F, SYP | 50% open | 100% open | Off | Single room | 2.3/135 | 29.1 °C | 12.8 |
| 23a | 6-11, 2005 | Cubicle 4; 2/F, SYP | Close | Close | Off | Single room | 1.3/220 | 27.4 °C | 0.6 |
| 24a | 6-11, 2005 | Cubicle 4; 2/F, SYP | Close | 100% open | Off | Single room | 1.6/220 | 26.9 °C | 3.4 |
| 25 | 7-11, 2005 | Waiting Area, 2/F, SYP | 100% open | 100% open | Off | – | 2.4/140 | 27.5 °C | 11.9 |
| 26 | 7-11, 2005 | Waiting Area, 2/F, SYP | 50% open | 50% open | Off | – | 3.2/135 | 27.6 | 8.45 |
| 27 | 7-11, 2005 | Cubicle 20, 2/F, SYP | 50% open | 50% open | Off | Single room | 2.9/140 | 27.3 | 11.5 |
| 28 | 7-11, 2005 | Cubicle 20, 2/F, SYP | 100% open | 100% open | Off | Single room | 2.7/140 | 26.9 | 22.5 |
The window air conditioner is on in the ward during the experiment.
Tests 8 and 11: The ventilation rates of Tests 8 and 11 were so high that the sampler failed to sample adequate data. The ventilation rate is calculated according to the inadequate data.
Test 17: The measured ventilation rate for Test 17 is about 18.5 ACH. However, an unknown disturbance was also recorded by the equipment during a short unstable period with the ventilation rate as low as 8.8 ACH.
One of the nature forces to drive airflow around buildings is due to wind. The surrounding environments influence the building to acquire fresh air driven by wind. The comparison of ventilation rate of wards in two natural ventilated building is demonstrated in Fig. 2 , when the electric fans were all switched off. Results show that the ventilation rate of the ward in Hospital GH is higher than Clinic SYP when doors or windows are fully or partially open. The Hospital GH is located on hillside surrounded by green trees, while Clinic SYP is surrounded by high buildings, indicating that the hospitals surrounded by green environments may get higher ventilation rate than the hospitals surrounded by high buildings.
-
●
Effect of opening windows and doors
Fig. 2.
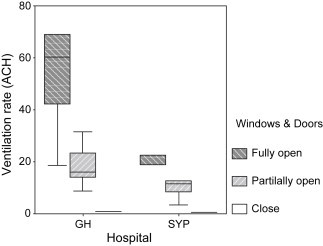
Comparison of the measured ventilation rate at Hospital GH and Outpatient Clinic SYP when all the fans were switched off.
It is obvious that the ventilation rate increases with the opening area increase, as demonstrated by Fig. 2.
When all the openings were closed in the ward, the measured ventilation rate due to infiltration was only 0.60 and 0.71 ACH (Test 15 and Test 23). When the openings connected to the corridor were fully open, the window to the outdoor was closed and the exhaust fans were off; the ventilation rate was between 3.4 ACH (Test 24) and 8.7 ACH (Test 14). The observed airflow pattern is shown in Fig. 3A. The measured airflow pattern seemed unsatisfactory because there was an exchange flow between the corridor and the room air. The measured air change rate was also unsatisfactory in this case. When we fully opened the windows to the outdoor and closed the door to the corridor, as illustrated in Fig. 3B, the measured ventilation rate was between 14.0 and 31.6 ACH, which is higher than the current required ventilation rate as specified by ASHRAE and CDC guidelines for isolation rooms [9], [24]. When all the openings of the ward were open, the so-called cross-ventilation occurred as shown in Figs. 3C and D. The measured ventilation rate was between 11.9 and 69.0 ACH. The maximum ventilation rate recorded might be due to the existence of a strong wind at the time of measurement.
-
●
Effect of wind
Fig. 3.
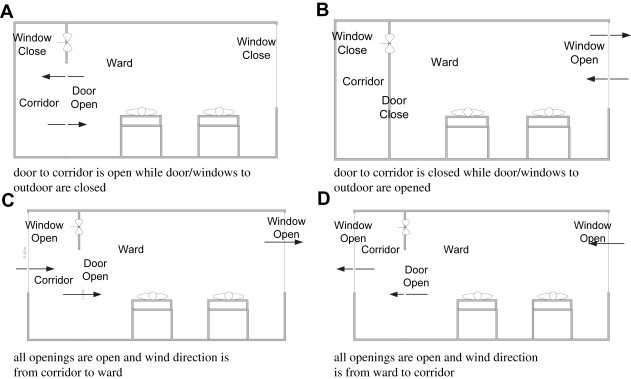
Illustrated airflow direction for four scenarios: (A) the door to the corridor is open, while the door/windows to outdoor are closed; (B) the door to the corridor is closed, while the door/windows to outdoor are opened; (C) all the openings are open, and the wind direction is from the corridor to the ward, and (D) all the openings are open and the wind direction is from the ward to the corridor.
The occurrence of a high ventilation rate depends on the wind speed, the wind, and the direction and area of the openings. This explained the difference in measured ventilation rates in Tests 4 and 17 which were carried out in a same ward; see Figs. 4(A) and (B). Fig. 4(B) shows the measured temperature, wind speed, and the direction from the Hong Kong observatory during the tests. Test 4 was done at 15:19–15:30 on November 9, 2005, when the wind speed and the wind direction were 3.6 m/s and 150°, respectively, at 15:00, and 2.4 m/s and 170°, respectively, at 16:00. Test 17 was done at 17:42–18:04 on August 28, 2006, when the wind speed and the direction were 4.1 m/s and 100°, respectively, at 17:00, and 4.8 m/s and 90° at 18:00. In spite of that recorded wind speed during Test 17 being much higher than that during Test 4, the measured ventilation rate of Test 17 (18.5 ACH) was much lower than that of the ventilation rate of Test 4 (42.2 ACH). The reason is due to the wind direction; see Fig. 4(A). The angle between the wind direction and the tables and windows of Test 17 was less than 10°, while the angle of Test 4 was almost 75°. The effective wind speed flow to the windows was 3.0 × sin(75°) = 2.9 m/s for Test 4, while the effective wind speed was less than 4.5 × sin(10°) = 0.78 m/s. In the two tests, the experiment settings including the heat source inside the ward were set similar. Large ventilation rates make temperature in outdoor and indoor close, i.e. 0.019 °C in Test 4 and 0.87 °C in Test 17. So the wind dominates the ventilation rate in this test. So the results show the significance of wind speed and the wind direction to the ventilation rate.
Fig. 4.
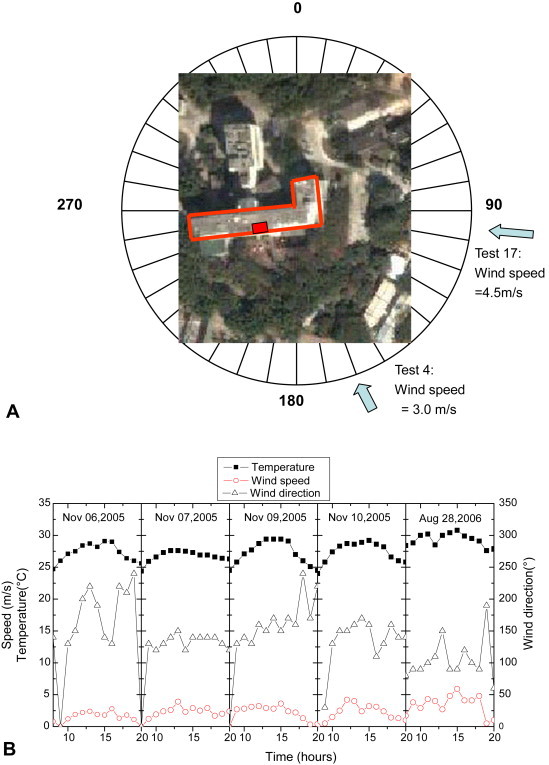
(A) An illustration of wind speed and wind direction of Tests 4 and 17. In Test 17, the recorded wind speed was 4.5 m/s and the wind direction 95°. In Test 4, the recorded wind speed was 3.5 m/s and the wind direction 160°, refer to (B). The satellite photo of Hospital GH was obtained from http://www.maps.google.com. (B) The ambient air temperature, wind speed, and the direction measured by the Hong Kong Observatory at Wong Chuk Hang weather station, close to the TB Hospital GH.
3.2. Pressure difference and airflow direction
Compared with mechanical ventilation, natural ventilation is difficult to control and predict. During measurement, it was found that the airflow pattern and the airflow direction were unstable, and bi-directional flows existed through an opening in Tests 1–4, 9–10, 15–17, 20, and 24–28. The pressure difference between the two openings was too small to be measured by our equipments when the windows and door were fully open. Strictly speaking, the pathogen-containing droplet residues are possible to escape from the ward to the corridor. However, the infection risk can be very low due to the existence of very high ventilation rate at the same time. Additionally, the use of exhaust fans may help us to avoid the infection risk as a design alternative. In Tests 7 and 18–20, all the exhaust fans were switched on. The airflow rate of the exhaust fans was found to differ when the doors and the windows were opened or closed. When all the fans were running and when all the openings were closed, the airflow rate for a fan was much lower than when all the openings were opened. The airflow rate of the fan to supply air from corridor to the ward was 160 l/s when all the openings were closed, while it was 80 l/s when all the openings were opened. And the airflow rate of fans to exhaust air from corridor to the balcony was 380 l/s when all the openings were closed, while it was 535 l/s when all the opening were open. It is due to the pressure difference. Negative pressure of the ward makes it easy to supply corridor air to the ward and difficult to exhaust ward air to the balcony.
The airflow direction was shown by smoke visualization, and it shows that when the fans were turned on, the airflow was always from the corridor to the ward. The measured pressure differences across different openings are shown in Fig. 5 . During the measurement, the toilet door was kept closed. When the windows and the doors were open, the pressure difference would disappear. As we switched off the exhaust fan in the toilet and switched on the exhaust fans in the ward, the airflow would go from the toilet to the ward. It is of great importance to ensure that the toilet exhaust fan was switched on when the exhaust fans in the ward were turned on. When all the doors and the openings were closed and all the exhaust fans were switched on, the resulted pressure difference seemed satisfactory. Fans may also increase the ventilation rate and control the airflow direction. It is useful for the worst weather conditions. The results indicate that the natural ventilated ward could alter to a temporary mechanical isolation room if the electric fans were properly designed and installed.
Fig. 5.
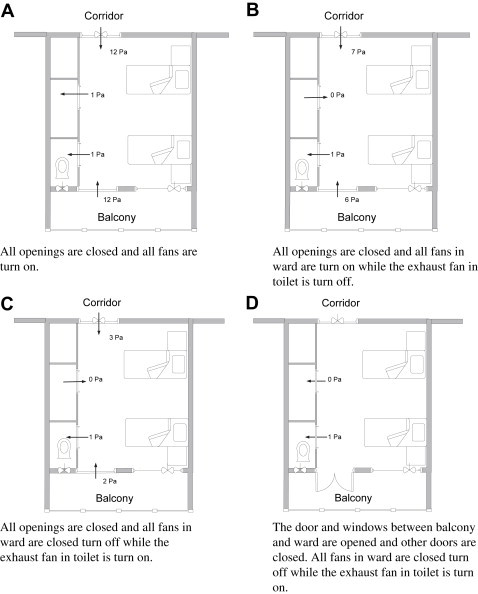
Measured pressure difference between the zones when the exhaust fans are switched on.
4. Discussions
Although there is still a need for direct epidemiological evidences to support (or refute) the use of natural ventilation for infection control, the present test results, with a satisfactory ventilation performance of natural ventilation, suggest the efficacy of nature in diluting any airborne pollutants, including the infectious airborne pathogens. One particular attracting aspect of natural ventilation is that it is available in many healthcare facilities in limited-resource regions in the world. This is in contrast with the mechanical ventilation, which can be easily controlled, but may be too expensive for some poor areas.
There are at least three major concerns with using natural ventilation for infection control. First, the ventilation rate delivered by natural ventilation may be very high for most of the period, but may be low when the natural forces are not available. This may be resolved by a better design of natural ventilation. If the resources are available, natural ventilation may be designed together with mechanical ventilation so that the latter can function when the natural forces are not available. Second, as traditionally believed, negative pressure is needed for airborne precaution and natural ventilation cannot control the airflow direction through the doorway. This may not be an issue when the quanta generation rate is not extremely high as discussed below. It may be argued that when the ventilation rate is double or triple the minimum 12 ACH recommended by CDC, the infection risk would be significantly reduced. Third, the natural ventilation cannot control the thermal comfort conditions when the outdoor air is hot and humid, as experienced in the Hospital GH. Through their many years experience operating natural ventilation for their TB wards, they have learned to use spot air conditioning and ceiling fans for achieving better thermal comfort for their patients.
Table 2 provides information about how the ventilation rates relate to the decay of droplet nuclei concentration with different ventilation rates, using the concentration decay equation. The assumptions in producing Table 2 include that the ACH remains constant and the concentration in the enclosed space is uniform (normally not the case in real-life situation). Applying the concentration decay equation, it takes 20 min to reduce the concentration to 1.8% with 12 ACH, but only 10 min with 24 ACH.
Table 2.
Decay of droplet nuclei concentration for different ventilation rates and duration of time in a room.
| Time (min) | Ventilation rate (%) |
|||
|---|---|---|---|---|
| 6 ACH | 12 ACH | 18 ACH | 24 ACH | |
| 0 | 100 | 100 | 100 | 100 |
| 5 | 60.7 | 36.8 | 22.37 | 13.5 |
| 10 | 36.8 | 13.5 | 5.0 | 1.8 |
| 15 | 22.3 | 5.00 | 1.1 | 0.3 |
| 20 | 13.5 | 1.8 | 0.3 | 0.03 |
| 25 | 8.2 | 0.7 | 0.06 | 0.00 |
| 30 | 5.0 | 0.3 | 0.01 | 0 |
| 40 | 1.8 | 0.03 | 0 | 0 |
| 50 | 0. 7 | 0 | 0 | 0 |
| 60 | 0.3 | 0 | 0 | 0 |
As shown in Fig. 1, natural ventilation may not be effective when the quanta generation is extremely high in spite of the fact that it is rare. This means that in the case of extremely high quanta generation, a correct airflow direction is important in avoiding the leakage of the pathogens-laden droplet nuclei into the public areas such as corridors. Literatures show that airborne transmitted diseases have the possibility to transmit in vertical direction, i.e. transmit between different floors in a high rise residential building due to buoyancy effects [25], [26]. So the route of vertical transmission of airborne transmitted diseases should be taken into account in controlling airborne infection. In natural ventilation, it is not easy to control its airflow direction. In some locations, prevailing wind direction may be used in the design for airflow-direction control. It may be argued that the cases with extremely high quanta generation may be exceptional. In any case, this may be one of the situations when the natural ventilation may not be effective. However, in this case, natural ventilation may reduce but not eliminate the risk of infection, and appropriate personal protection equipment (PPE) such as use of masks is recommended.
5. Conclusions
We presented a field measurement study on the performance of natural ventilation in a TB hospital and an outpatient clinic, and discussed the possibility of using natural ventilation for infection control. The measured ventilation rate was found to be much higher than the CDC recommended 12 ACH for isolation rooms. However, when all the openings are open, the pressure difference between the corridor and the ward and that between the ward and the outdoor is much less than 1 Pa, and cannot be measured by the conventional equipment. The observed airflow direction through an open door or window can be unstable during the measurement when the wind is weak.
The mechanical exhaust fans installed in the ward can create negative pressure. When all the openings were closed and the fans were turned on, the ventilation rate was as high as 12.6 ACH and the pressure difference between the ward and the corridor was also high. The measured results indicate that a naturally ventilated ward may be converted to an isolation room by installing exhaust fans when the natural forces are not sufficiently strong.
Our measurement confirmed that natural ventilation could provide a high ventilation rate, especially when all the openings in the ward were fully open. The high ventilation rate is expected to reduce the risk of cross-infection.
Acknowledgements
The work described in this paper was supported jointly by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China (Project No. HKU 7115/04E) and a Hospital Authority-commissioned project under the Research Fund for the Control of Infectious Diseases (RFCID) by the Health, Welfare and Food Bureau (Project No. HA-NS-002), Hong Kong SAR Government.
References
- 1.Chen Y.C., Huang L.M., Chan C.C. SARS in hospital emergency room. Emerg Infect Dis. 2004;10:782–788. doi: 10.3201/eid1005.030579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Christian M.D., Loutfy M., McDonald C. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect Dis. 2004;10:287–293. doi: 10.3201/eid1002.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ha L.D., Bloom S.A., Hien N.Q. Lack of SARS transmission among public hospital workers. Vietnam. Emerg Infect Dis. 2004;10:265–268. doi: 10.3201/eid1002.030707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee N., Hui D., Wu A. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;15:1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 5.Leo Y.S., Chen M., Heng B.H. Severe acute respiratory syndrome – Singapore. JAMA. 2003;25:3231–3234. doi: 10.1001/jama.289.24.3231-b. [reprinted from MMWR 2003;52:405–11] [DOI] [PubMed] [Google Scholar]
- 6.Li Y., Huang X., Yu I.T.S., Wong T.W., Qian H. Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air. 2005;15:83–95. doi: 10.1111/j.1600-0668.2004.00317.x. [DOI] [PubMed] [Google Scholar]
- 7.Shen Z., Ning F., Zhou W.G. Superspreading SARS events, Beijing, 2003. Emerg Infect Dis. 2004;10:256–260. doi: 10.3201/eid1002.030732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenbaum R.A., Benyo J.S., O'Connor R.E. Use of a portable forced air system to convert existing hospital space into a mass casualty isolation area. Ann Emerg Med. 2004;44:628–634. doi: 10.1016/j.annemergmed.2004.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC. Guidelines for environmental infection control in health-care facilities. Atlanta (GA): US Department of Health and Human Services Centers for Disease Control and Prevention (CDC); 2003.
- 10.Li Y., Leung G.M., Tang J.W. Role of ventilation in airborne transmission of infectious agents in the built environment – a multi-disciplinary systematic review. Indoor Air. 2007;17:2–18. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- 11.Dwosh H.A., Hong H.H.L., Austgarden D., Herman S., Schabas R. Identification and containment of an outbreak of SARS in a community hospital. Can Med Assoc J. 2003;27:1415–1420. [PMC free article] [PubMed] [Google Scholar]
- 12.Esswein E.J., Kiefer M., Wallingford K. Environmental and occupational health response to SARS, Taiwan, 2003. Emerg Infect Dis. 2004;10:1187–1194. doi: 10.3201/eid1007.030728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fung C.P., Hsieh T.L., Tan K.H. Rapid creation of a temporary isolation ward for patients with severe acute respiratory syndrome in Taiwan. Infect Control Hosp Epidemiol. 2004;25:1026–1032. doi: 10.1086/502339. [DOI] [PubMed] [Google Scholar]
- 14.Gomersall C.D., Tai D.Y.H., Loo S. Expanding ICU facilities in an epidemic: recommendations based on experience from the SARS epidemic in Hong Kong and Singapore. Intens Care Med. 2006;32:1004–1013. doi: 10.1007/s00134-006-0134-5. [DOI] [PubMed] [Google Scholar]
- 15.Riley E.C., Murphy G., Riley R.L. Airborne spread of measles in a suburban elementary school. Am J Epidemiol. 1978;107(5):421–432. doi: 10.1093/oxfordjournals.aje.a112560. [DOI] [PubMed] [Google Scholar]
- 16.WHO . World Health Organization; Geneva (Switzerland): 1999. Guidelines for the prevention of tuberculosis in healthcare facilities in resource-limiting settings. [Google Scholar]
- 17.Escombe A.R., Oeser C.C., Martinez C. Natural ventilation to reduce nosocomial transmission of tuberculosis and other airborne infections. Int J Tub Lung Dis. 2005;9:s56–s57. [Google Scholar]
- 18.Escombe A.R., Oeser C.C., Gilman R.H. Natural ventilation for the prevention of airborne contagion. Plos Med. 2007;4:309–317. doi: 10.1371/journal.pmed.0040068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waxham F.E. The outdoor treatment of tuberculosis. JAMA. 1902;39:1392–1393. [JAMA 2002;288:2754 (reprinted)] [Google Scholar]
- 20.Jiang S., Huang L., Chen X. Ventilation of wards and nosocomial outbreak of severe acute respiratory syndrome among healthcare workers. Chin Med J (Engl) 2003;116:1293–1297. [PubMed] [Google Scholar]
- 21.Apisarnthanarak A., Mundy L.M. Influenza outbreak among healthcare workers in an avian influenza (H5N1) – endemic setting. Clin Infect Dis. 2006;43:1493–1494. doi: 10.1086/508885. [DOI] [PubMed] [Google Scholar]
- 22.Heiselberg P. Hybrid Ventilation Centre Aalborg University; Aalborg (Denmark): 2000. Hybrid Ventilation Centre. Principles of hybrid ventilation. [Google Scholar]
- 23.Perino M, Heiselberg P. Short-term airing by natural ventilation – modelling and control strategies. Indoor Air [article online: Feb 7 2009, 4:37 AM]. [DOI] [PubMed]
- 24.Ashrae . American Society of Heating Refrigerating and Air-Conditioning Engineers Inc.; Atlanta (GA): 2003. HVAC design manual for hospitals and clinics. [Google Scholar]
- 25.Gao N.P., Niu J.L., Perino M., Heiselberg P. The airborne transmission of infection between flats in high-rise residential buildings: tracer gas simulation. Build Environ. 2008;43:1805–1817. doi: 10.1016/j.buildenv.2007.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gao N.P., Niu J.L., Perino M., Heiselberg P. The airborne transmission of infection between flats in high-rise residential buildings: particle simulation. Build Environ. 2009;44:402–410. doi: 10.1016/j.buildenv.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]


