Abstract
Objective
To assess weight and HbA1c changes in the Healthier You: National Health Service Diabetes Prevention Programme (NHS DPP), the largest DPP globally to achieve universal population coverage.
Research Design and Methods
A service evaluation assessing intervention effectiveness for adults with non-diabetic hyperglycaemia (HbA1c 42-47 mmol/mol (6.0-6.4%)) or fasting plasma glucose 5.5-6.9 mmol/l) between programme launch in June 2016 and December 2018, using prospectively collected national service-level data in England.
Results
By December 2018, 324,699 people had been referred, 152,294 had attended initial assessment and 96,442 had attended at least one of 13 group-based intervention sessions. Allowing sufficient time to elapse: 53% attended initial assessment; 36% attended at least one group-based session; and 19% completed the intervention (attended over 60% of sessions). Of the 32,665 that attended at least one intervention session and had sufficient time to finish, 17,252 (53%) completed: intention-to-treat analyses demonstrated mean weight loss 2.3 (95% CI: 2.2-2.3) kg and HbA1c reduction 1.26 (1.20-1.31) mmol/mol (0.12 (0.11-0.12) %); completer analysis demonstrated mean weight loss 3.3 (3.2-3.4) kg and HbA1c reduction 2.04 (1.96-2.12) mmol/mol (0.19 (0.18-0.19) %). Younger age, female sex, Asian and black ethnicity, lower socioeconomic status and normal baseline BMI were associated with less weight loss. Older age, female sex, black ethnicity, lower socioeconomic status and baseline overweight and obesity were associated with smaller HbA1c reduction.
Conclusions
Reductions in weight and HbA1c compare favourably to those reported in recent meta-analyses of pragmatic studies and suggest likely future reductions in participant type 2 diabetes incidence.
The increase in prevalence of Type 2 diabetes is a threat to the sustainability of health systems internationally. There is good evidence from randomised controlled trials that behavioural interventions to support people with impaired glucose tolerance to lose weight, adopt a healthy diet and increase physical activity, can significantly decrease the incidence of type 2 diabetes (1–3).
Recent systematic reviews and meta-analyses of trials assessing the effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes in routine practice have demonstrated relative risk reductions in incidence of 26% and 29% (4–6).
There is limited experience in the implementation of diabetes prevention programmes (DPP) at scale. The US DPP reported on 14,747 participants (7), the Australian lifestyle intervention programme “Life!” on 8,412 participants (8), and the Finnish “FIN-D2D” on 2,798 participants (9).
In 2016 the National Health Service (NHS) in England established The Healthier You: NHS Diabetes Prevention Programme (NHS DPP) and just over two years later has seen England achieve universal population coverage. The NHS DPP was developed to prevent or delay onset of type 2 diabetes in adults already identified to be at high risk, defined as having non-diabetic hyperglycaemia (NDH) (HbA1c 42-47 mmol/mol (6.0–6.4%) or fasting plasma glucose (FPG) 5.5-6.9 mmol/l). The rationale, justification, development and early implementation of the Programme have been described previously (10), and an impact analysis has demonstrated the potential for realising return on investment within 12 years (11). The approach is based on guidance on type 2 diabetes prevention in those at high risk from the National Institute of Health and Care Excellence (NICE PH38) (12) and is complemented by primary preventative interventions to tackle obesity, the major modifiable risk factor for Type 2 diabetes, such as a levy on sugar-sweetened beverages, outlined in the UK Government’s Childhood Obesity Plan (13–14).
Using data from the first two and half years of activity, we aimed to assess weight and HbA1c changes in the NHS DPP, and to assess whether these changes are comparable to uncontrolled pre-post summary effect sizes reported in the most recent meta-analyses of pragmatic studies, on which some of the assumptions in the impact analysis were based. We also aimed to quantify access through uptake and programme completion, and to assess impacts of age, sex, ethnicity, baseline BMI, and socioeconomic status.
Research Design and Methods
Study design
A service evaluation in England evaluating the effectiveness of the NHS DPP using prospectively collected national service-level data relating to all those referred from programme launch in June 2016 to the end of December 2018.
Intervention
The NHS DPP delivers behavioural interventions that encourage: weight loss, or the maintenance of a healthy weight; achievement of UK dietary recommendations related to fibre, fruit and vegetables, oily fish, saturated fat, salt and free sugars (15); and achievement of the UK Chief Medical Officers’ physical activity recommendations (16). The intervention is delivered according to a national service specification by one of four service providers selected through a national competitive process: Reed Momenta Ltd (London, UK), ICS Health and Wellbeing (Leeds, UK), Ingeus UK Ltd (London, UK), and Living Well Taking Control LLP (Birmingham, UK). The specification was developed by an expert group, based on the evidence for clinical and cost effectiveness and on the suggested mechanisms for achieving behaviour change described in NICE PH38 (12). These include: information provision to raise awareness of the benefits of and types of lifestyle changes needed to achieve and maintain a healthy weight; exploration and reinforcement of participants' reasons for wanting to change and their confidence about making changes; goal setting; action planning; coping plans and relapse prevention.
Each provider’s service follows the same broad structure of an initial assessment, core sessions, and maintenance sessions, with a minimum total of 13 face-to-face group-based sessions, over at least 9 months, constituting a least 16 hours contact time. Each provider must utilise a known framework for behaviour change.
Participants
Individuals are eligible if they have a blood test indicating NDH conducted within the previous 12 months, are 18 years of age or over, not pregnant and not previously diagnosed with Type 2 diabetes. Individuals are identified following an NHS Health Check (17), through retrospective searches of general practice records, or through routine clinical practice. Individuals referred are invited to attend an Initial Assessment at which further programme details are provided, and participants are assigned to a group for intervention delivery.
Data collection
All programme providers are contractually required to collect a minimum dataset including demographic and clinical information. Age, sex, postcode, and referral HbA1c or FPG measurement are recorded at referral receipt. Ethnicity, weight and height are recorded at Initial Assessment. Body weight is measured by coaches employed by the provider in light indoor clothing at each intervention session using class 3 scales. Providers assess HbA1c values for each participant at Initial Assessment if the referral HbA1c or FPG is more than 3 months old, at six months after the first intervention session and at the end of the programme for those still attending. This service evaluation involves assessment of anonymised data collected during routine service delivery; NHS England has published an information governance framework setting out the legal basis for data collection and data flows, ensuring that the service and it’s evaluation are delivered in compliance with data protection legislation (18).
Programme moderators
Individual factors (age, sex, ethnicity, socioeconomic status, baseline BMI and number of sessions attended) and programme factors (provider) were identified as potential outcome moderators.
Sex was recorded as male, female or indeterminate. Participants were grouped into 5-year age-bands and self-reported ethnicity as white, Asian, black, mixed or other. Socioeconomic status was measured using quintiles of Index of Multiple Deprivation associated with the Lower Super Output Area derived from participant postcode (19). All variables also include an unknown category where either the participant declined to give the relevant information, or a value was not recorded. BMI was calculated and participants were classified as healthy-weight/underweight, overweight or obese, defined according to their reported ethnicity, or if their ethnicity was not known or not recorded, according to the white ethnicity group in-line with World Health Organisation thresholds (20).
Outcomes
The primary outcomes for the evaluation were change in weight and change in HbA1c analysed on the basis of intention-to-treat. In secondary analyses data from those who completed the programme were assessed separately.
Weight change, percentage weight change and the proportion of participants who achieved a weight loss of ≥ 5%, were calculated for all participants associated with cohorts that had had time to finish the programme. The baseline measurement was defined as the weight measured at the first intervention session attended to avoid including weight change during the period between Initial Assessment and intervention commencement. Weight change greater than five standard deviations from the mean was deemed erroneous and recorded as missing.
All providers elected to assess point-of-care tested (POCT) HbA1c values. POCT devices used by providers were the Siemens DCA Vantage (Siemens Healthcare Ltd, Guildford, UK), Afinion (Abbott Diagnostics, Maidenhead, UK) and A1C Now+ (BHR Pharmaceutical Ltd, Nuneaton, UK). The same device was used for repeated measures within individuals. Consistent with a recent systematic review and meta-analysis (21), there was a significant negative bias for POCT HbA1c values compared to referral, laboratory-measured HbA1c values, greater than could be attributed to regression to the mean and greater than concurrent weight change would suggest was attributable to behaviour change between referral and Initial Assessment. Therefore, mean HbA1c change was calculated only for the subgroup of participants who had had their HbA1c measured at Initial Assessment, so that all values for the same individual had been derived using the same device.
Programme retention was assessed by following cohorts of participants who attended at least one intervention session: those associated with cohorts where sufficient time had elapsed to have reached the final session, were defined as having finished the programme. “Completion” of the programme was defined as attendance of at least 60% of sessions – at least 8 sessions for three providers that offered 13 sessions, at least 11 sessions for one provider that offered 18 sessions. This aligns with the a priori criterion used for provider payment, where providers were paid for participants who attend 60% or more at each of 5 milestones. Completion rates were calculated with the number of people who had attended at least one intervention session as the denominator.
Statistical analyses
Intention-to-treat weight change analysis was conducted and included participants for whom all data fields, except HbA1c, were complete, with weight change calculated as the weight difference between the first and last sessions attended. HbA1c change analysis was conducted and included the subset of these participants who also had an HbA1c measurement at Initial Assessment, with HbA1c change calculated as the HbA1c difference between Initial Assessment and the last value recorded. Data for programme completers was assessed in secondary analyses.
Sensitivity analyses were conducted using multiple imputation, employing multivariate chained equations to impute missing data and then comparing the results to the primary analyses. Both univariate and multivariate analyses were repeated using multiple imputation datasets and results compared to ensure that missing data did not introduce bias.
Due to time delays between referral and attendance at Initial Assessments and first intervention sessions, the proportion of participants who attended either Initial Assessment or at least one intervention session were calculated using the number of referrals received up to December 2017 as the denominator, with numbers of corresponding attendees at either Initial Assessment or at an intervention session respectively by December 2018 as numerators.
A mixed-effects logistic regression model was used to identify characteristics associated with programme completion. Age, sex, ethnicity, baseline BMI, deprivation and Provider were considered as fixed effects and local referral area as a random effect with the contribution of the random effect quantified using the Intraclass Correlation Coefficient (ICC). Local referral areas are only associated with a single provider and therefore incorporate the same facilities and facilitators used by that provider. Variation between the four providers was directly accounted for by a fixed effect in the model. Mixed-effects linear regression models were used to identify factors associated with change in weight and change in HbA1c. The number of sessions attended, provider and participant characteristics were considered as fixed effects and local referral area as a random effect.
Statistical significance was defined as p-value <0.05 and confidence intervals (CI) were set at 95%. All data were analysed using Stata version 15.
Results
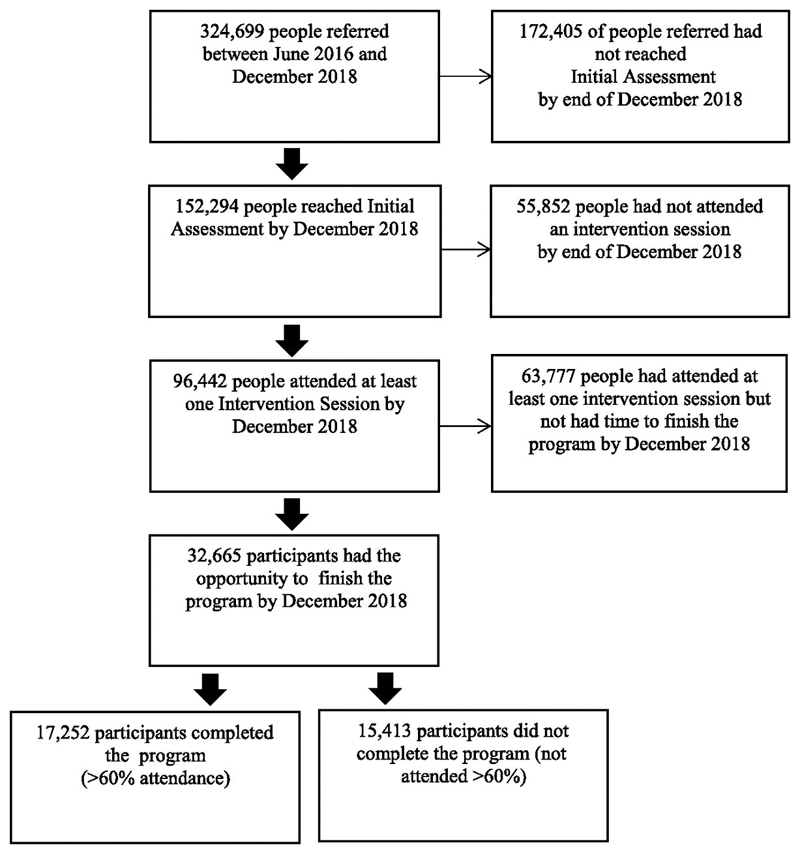
Between June 2016 and end of December 2018, 324,699 people were referred into the programme. Of these, 152,294 had attended an Initial Assessment and 96,442 had attended at least one of the group-based intervention sessions. Including only those referred up until the end of December 2017 in order to allow sufficient time to have joined a group, 53% attended an Initial Assessment and 36% attended an intervention session. There were 32,665 participants who had attended an intervention session and had had sufficient time to finish the programme. Among these participants 17,252 (53%) attended at least 60% of sessions, an overall completion rate of 19% of those referred. Figure 1 outlines numbers of people at each stage of the programme.
Figure 1.
Flowchart of people at each stage in the programme
Characteristics of people at each programme stage are shown in Table 1: 46% of people referred were male, the mean (standard deviation (SD)) age was 62 (13) years and there was broadly equal representation from all deprivation quintiles at referral. Mean HbA1c at referral was 43.7 (1.5) mmol/mol (6.1 (0.1) %). Ethnicity and weight were not recorded until the Initial Assessment; at which point 20% of participants were of black, Asian, mixed or other ethnicity, 69% white and 11% unknown. The mean weight was 83.9 (19.1) kg at Initial Assessment and the mean BMI 30.3 (6.1) kg/m2. The largest decrease in the proportions of people retained was between referral and Initial Assessment, where there were significant decreases in the proportions of males, of people aged under 60 years, and of people from the most deprived quintile (all p<0.001). Except for the proportion of males (p=0.52), these decreases continued between Initial Assessment and programme completion (all p<0.001).
Table 1. Characteristics of people at each stage in the programme, between June 2016 and December 2018.
| People referred | People referred that have attended an Initial Assessment (IA) | People who have attended at least 1 group-based intervention session (IV) | Participants associated with cohorts that have finished the programme | Participants that have completed the programme (finished, and attended more than 60% of sessions) | Chi-squared p-value (reached IA vs referred) | Chi-squared p-value (attended at least 1 IV vs reached IA) | Chi-square p-value (completed vs finished) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |||||
| Overall | 324,699 | 100% | 152,294 | 100% | 96,442 | 100% | 32,665 | 100% | 17,252 | 100% | n/a | n/a | n/a | |
| Sex | Male | 147,890 | 46% | 68,780 | 45% | 43,517 | 45% | 14,487 | 44% | 7,700 | 45% | <0.001 | <0.001 | 0.52 |
| Female | 172,252 | 53% | 82,637 | 54% | 52,511 | 54% | 18,017 | 55% | 9,465 | 55% | ||||
| Indeterminate / Unknown* | 4,557 | 1% | 877 | 1% | 414 | 0% | 161 | 0% | 87 | 0% | ||||
| Age band | <40 | 17,797 | 5% | 5,818 | 4% | 2,781 | 3% | 832 | 3% | 228 | 1% | <0.001 | <0.001 | <0.001 |
| 40-44 | 15,811 | 5% | 5,593 | 4% | 2,841 | 3% | 903 | 3% | 301 | 2% | ||||
| 45-49 | 22,604 | 7% | 8,449 | 6% | 4,602 | 5% | 1,469 | 4% | 525 | 3% | ||||
| 50-54 | 32,021 | 10% | 12,735 | 8% | 7,256 | 8% | 2,388 | 7% | 967 | 6% | ||||
| 55-59 | 37,938 | 12% | 16,647 | 11% | 10,016 | 10% | 3,383 | 10% | 1,655 | 10% | ||||
| 60-64 | 40,880 | 13% | 19,656 | 13% | 12,743 | 13% | 4,247 | 13% | 2,305 | 13% | ||||
| 65-69 | 46,787 | 14% | 25,481 | 17% | 17,517 | 18% | 6,205 | 19% | 3,710 | 22% | ||||
| 70-74 | 48,106 | 15% | 26,616 | 17% | 18,229 | 19% | 6,244 | 19% | 3,684 | 21% | ||||
| 75+ | 62,641 | 19% | 31,281 | 21% | 20,457 | 21% | 6,994 | 21% | 3,877 | 22% | ||||
| Unknown | 114 | 0% | 18 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | ||||
| Mean age | 62 | - | 64 | - | 65 | - | 65 | - | 67 | - | ||||
| SD of age | 13.4 | - | 12.4 | - | 11.7 | - | 11.5 | - | 10.2 | - | ||||
| Ethnicity | Asian | n/a | n/a | 17,364 | 11% | 10,249 | 11% | 3,381 | 10% | 1,382 | 8% | n/a | <0.001 | <0.001 |
| Black | n/a | n/a | 9,567 | 6% | 5,402 | 6% | 2,099 | 6% | 959 | 6% | ||||
| Mixed | n/a | n/a | 2,539 | 2% | 1,673 | 2% | 559 | 2% | 249 | 1% | ||||
| Other | n/a | n/a | 1,432 | 1% | 765 | 1% | 220 | 1% | 82 | 0% | ||||
| White | n/a | n/a | 105,315 | 69% | 69,477 | 72% | 23,113 | 71% | 13,006 | 75% | ||||
| Unknown | n/a | n/a | 16,077 | 11% | 8,876 | 9% | 3,293 | 10% | 1,574 | 9% | ||||
| Deprivation quintile | IMD 1 (most deprived) | 68,616 | 21% | 29,388 | 19% | 16,357 | 17% | 5,634 | 17% | 2,500 | 14% | <0.001 | <0.001 | <0.001 |
| IMD 2 | 65,469 | 20% | 29,604 | 19% | 17,472 | 18% | 6,368 | 19% | 3,222 | 19% | ||||
| IMD 3 | 62,733 | 19% | 30,141 | 20% | 19,378 | 20% | 7,038 | 22% | 3,865 | 22% | ||||
| IMD 4 | 61,798 | 19% | 30,446 | 20% | 20,300 | 21% | 6,747 | 21% | 3,725 | 22% | ||||
| IMD 5 (least deprived) | 65,108 | 20% | 32,247 | 21% | 22,721 | 24% | 6,779 | 21% | 3,888 | 23% | ||||
| Unknown | 975 | 0% | 468 | 0% | 214 | 0% | 99 | 0% | 52 | 0% | ||||
| BMI grouping at IA | Underweight/Healthy | n/a | n/a | 22,953 | 15% | 14,033 | 14% | 4,373 | 13% | 2,558 | 14% | n/a | <0.001 | <0.001 |
| Overweight | n/a | n/a | 50,850 | 33% | 32,640 | 34% | 10,393 | 32% | 5,938 | 34% | ||||
| Obese | n/a | n/a | 67,390 | 44% | 43,370 | 45% | 13,516 | 41% | 6,809 | 39% | ||||
| Unknown | n/a | n/a | 11,101 | 7% | 6,399 | 7% | 4,383 | 13% | 1,947 | 11% | ||||
| Mean BMI at IA | n/a | n/a | 30.3 | - | 30.3 | - | 30.3 | - | 29.9 | - | ||||
| SD of BMI at IA | n/a | n/a | 6.1 | - | 6.0 | - | 5.9 | - | 5.7 | - | ||||
| Mean Weight at IA (kg) | Mean weight at IA (kg) | n/a | n/a | 83.9 | - | 84 | - | 83.6 | - | 82.6 | - | |||
| SD of weight at IA (kg) | n/a | n/a | 19.1 | - | 18.9 | - | 18.7 | - | 18.1 | - |
Indeterminate and unknown grouped together due to suppression of small numbers
Completion, weight change and HbA1c change were assessed for participants associated with cohorts that had finished the programme. Of those, 26,753 (82%) participants had no missing or unknown data (excluding HbA1c). There were no missing data for age, provider, local referral area and the number of sessions attended. Data were missing for: participant postcode (and therefore deprivation quintile) (0.3%), sex (0.5%), BMI (7%) and ethnicity (10%). Data on weight was missing at either baseline or end of programme for 7% of participants. There were 19,891 (61%) participants who had their HbA1c measured using a POCT device at Initial Assessment, of whom 16,083 had no missing data (49% of all participants).
Univariate analyses of primary outcomes are provided in Table 2 (with secondary outcomes in supplementary material, Table S1). The mean number of days on the programme was 179.8 (136) days and the mean number of intervention sessions attended was 8.2 (4.6) sessions. For the providers offering a total of 13 sessions, the mean number attended was 7.6 (3.8) and, for the provider offering 18 sessions, the mean number attended was 9.6 (5.8). The regression analysis indicated that participants who were older, up to 70 years, from less deprived backgrounds and with a lower BMI were more likely to complete the programme, but there was no effect of sex. Relative to white groups, Asian and mixed ethnic groups had lower completion rates, with no significant differences for other ethnic groups. There were significant differences in completion by provider (supplementary material, Tables S2 and S3). Clustering by local referral area made a proportionately small contribution to the outcomes (ICC 3.9 (2.1-7.2) %).
Table 2. Primary outcomes (weight change and HbA1c change) for participants who have finished the programme, including respectively those for whom all data fields, except HbA1c, were complete (N=26,753) and for those with all data fields complete (N=16,083); univariate analysis.
| Mean weight change, intention-to-treat | Mean HbA1c change, intention-to-treat | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean baseline weight (kg) | Mean weight change (kg) | 95% CI lower | 95% CI upper | P value | N | Mean baseline HbA1c (mmol/mol) | Mean HbA1c change (mmol/mol) | 95% CI lower | 95% CI upper | P value | ||
| Total | 26,753 | 83.4 | -2.3 | -2.3 | -2.2 | n/a | 16,083 | 41.8 | -1.3 | -1.3 | -1.2 | n/a | |
| Sex | Male | 11,942 | 90 | -2.5 | -2.6 | -2.5 | <0.001 | 7,065 | 41.7 | -1.4 | -1.4 | -1.3 | <0.001 |
| Female | 14,800 | 78.1 | -2 | -2.1 | -2 | 9,010 | 41.8 | -1.2 | -1.2 | -1.1 | |||
| Indeterminate | 11 | 84.7 | -2.8 | -5.1 | -0.5 | 8 | 42.1 | -0.1 | -2.9 | 2.7 | |||
| Age band | <40 | 604 | 90.3 | -1 | -1.3 | -0.8 | <0.001 | 342 | 41.1 | -0.7 | -1 | -0.3 | <0.001 |
| 40-44 | 693 | 90.6 | -1 | -1.3 | -0.8 | 388 | 41.5 | -0.7 | -1 | -0.5 | |||
| 45-49 | 1,116 | 90.4 | -1.6 | -1.8 | -1.4 | 629 | 41.5 | -0.6 | -0.8 | -0.4 | |||
| 50-54 | 1,873 | 88.8 | -1.7 | -1.9 | -1.5 | 1,082 | 41.9 | -1 | -1.2 | -0.9 | |||
| 55-59 | 2,723 | 87.8 | -2.1 | -2.2 | -1.9 | 1,599 | 41.7 | -1.1 | -1.2 | -0.9 | |||
| 60-64 | 3,489 | 85.2 | -2.4 | -2.5 | -2.3 | 2,161 | 41.7 | -1.2 | -1.4 | -1.1 | |||
| 65-69 | 5,201 | 83.8 | -2.6 | -2.7 | -2.4 | 3,216 | 41.7 | -1.4 | -1.6 | -1.3 | |||
| 70-74 | 5,161 | 81.6 | -2.6 | -2.7 | -2.5 | 3,167 | 41.8 | -1.5 | -1.6 | -1.4 | |||
| 75+ | 5,893 | 77.2 | -2.2 | -2.3 | -2.1 | 3,499 | 42 | -1.3 | -1.4 | -1.1 | |||
| Ethnicity | Asian | 3,087 | 74.8 | -1 | -1.1 | -0.9 | <0.001 | 1,844 | 42.1 | -0.9 | -1 | -0.8 | <0.001 |
| Black | 1,821 | 86.3 | -1.7 | -1.9 | -1.6 | 1,167 | 42.2 | -0.8 | -1 | -0.6 | |||
| Mixed | 513 | 84.1 | -1.7 | -2 | -1.4 | 285 | 42.2 | -1 | -1.3 | -0.7 | |||
| Other | 181 | 80.9 | -1.5 | -2 | -1.1 | 95 | 41.3 | -0.6 | -1.1 | 0 | |||
| White | 21,151 | 84.5 | -2.5 | -2.5 | -2.4 | 12,692 | 41.7 | -1.4 | -1.4 | -1.3 | |||
| Deprivation | IMD 1 (most deprived) | 4,430 | 84.8 | -1.8 | -1.9 | -1.6 | <0.001 | 2,631 | 41.9 | -0.9 | -1 | -0.7 | <0.001 |
| IMD 2 | 5,161 | 84 | -2.1 | -2.2 | -2 | 3,287 | 41.7 | -1.2 | -1.3 | -1.1 | |||
| IMD 3 | 5,922 | 83.1 | -2.2 | -2.3 | -2.1 | 3,741 | 41.9 | -1.3 | -1.4 | -1.2 | |||
| IMD 4 | 5,635 | 83.2 | -2.5 | -2.6 | -2.4 | 3,268 | 41.7 | -1.3 | -1.4 | -1.2 | |||
| IMD5 (least deprived) | 5,605 | 82.4 | -2.6 | -2.7 | -2.5 | 3,156 | 41.8 | -1.5 | -1.7 | -1.4 | |||
| BMI | Underweight/healthy | 4,205 | 62.7 | -1.4 | -1.5 | -1.3 | <0.001 | 2,630 | 41.3 | -1.4 | -1.5 | -1.3 | 0.001 |
| group | Overweight | 9,865 | 76.5 | -2.2 | -2.3 | -2.1 | 6,033 | 41.6 | -1.3 | -1.4 | -1.2 | ||
| Obese | 12,683 | 95.7 | -2.6 | -2.6 | -2.5 | 7,420 | 42.1 | -1.2 | -1.2 | -1.1 | |||
| Provider | Ingeus UK Ltd | 5,868 | 84.9 | -2.1 | -2.2 | -2 | <0.001 | 35 | 39.7 | -1 | -2.4 | 0.4 | <0.001 |
| Living Well Taking Control LLP | 3,067 | 84.2 | -1.9 | -2.1 | -1.8 | 2,066 | 40.9 | -0.5 | -0.6 | -0.4 | |||
| ICS Health and Wellbeing | 11,752 | 82.4 | -2.3 | -2.3 | -2.2 | 8,890 | 42.3 | -1.3 | -1.4 | -1.2 | |||
| Reed Momenta Ltd | 6,066 | 83.7 | -2.6 | -2.7 | -2.4 | 5,092 | 41.2 | -1.5 | -1.6 | -1.4 |
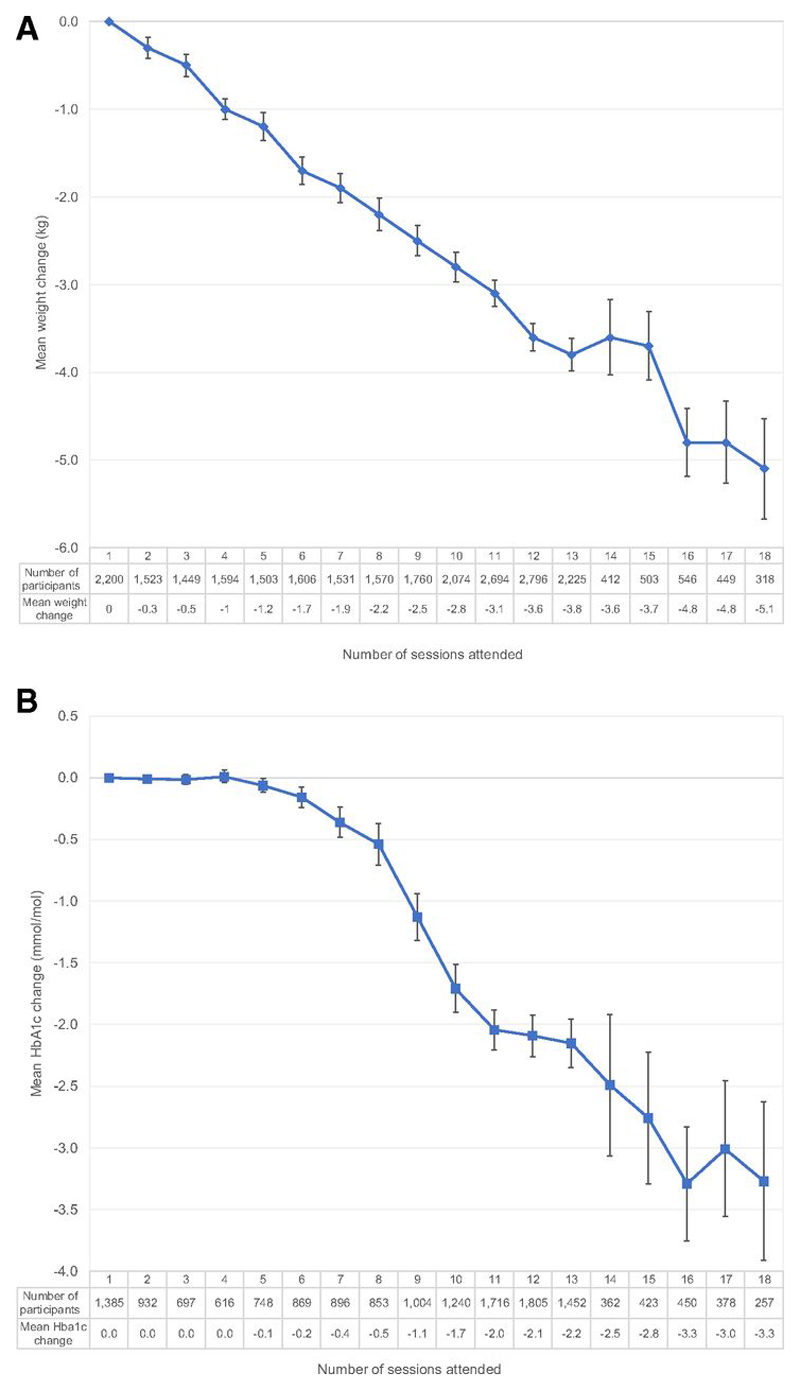
Using intention-to-treat analysis, mean baseline weight was 83.4kgs with a mean weight change of -2.3kg (-2.3kg to -2.2kg). Mean percentage weight change was -2.7% (-2.7% to -2.6%) and 24% of participants lost ≥5% of baseline weight. Weight loss increased with the number of sessions attended (Figure 2). The regression analysis indicated that for each additional session attended, there was a 0.32kg greater weight loss and for each 1kg higher baseline weight, there was an additional 0.03kg weight loss. Older people, up to 75 years, men, those from areas in the least deprived quintile and those with a higher BMI, lost more weight. Asian and black ethnic groups lost less weight, with no significant differences for other groups. There were significant differences by provider, independent of the number of sessions in their programme (supplementary material, Table S4). The ICC was 0.4 (0.2-0.8) %.
Figure 2.
A: Mean weight change (kg) by number of sessions attended, included those for whom all data fields, except HbA1c, were complete (N=26,753). B: Mean Hba1c change (mmol/mol) by number of sessions attended, included those for whom all data fields were complete (N=16,083).
Number of participants refers to the number attending exactly the given number of sessions (e.g.: Panel A; 2,200 participants attended only one intervention session before finishing the programme, 1,523 participants attended exactly two intervention sessions before finishing the programme etc.).
The mean baseline POCT HbA1c was 41.8mmol/mol (6.0%) with a mean HbA1c change of -1.26 (-1.31 to -1.20) mmol/mol (-0.12 (-0.12 to -0.11) %). HbA1c change increased with the number of sessions attended (Figure 2). The regression analysis indicated that for each additional session attended, there was an additional 0.18mmol/mol (0.02%) decrease in HbA1c and for each 1kg in weight reduction, there was a 0.15mmol/mol (0.01%) reduction in HbA1c. For each mmol/mol (0.09%) increase in baseline HbA1c there was a further corresponding decrease of 0.32mmol/mol (0.03%). There were significantly smaller HbA1c reductions for older participants, women, those from the most deprived deprivation quintile and for those with a higher BMI. There was a significantly smaller HbA1c reduction for black participants with no significant differences for other ethnic groups (supplementary material, Table S4). The ICC was 1.3 (0.7-2.3) %.
For completers, the mean baseline weight was 82.4kgs with a mean weight change of -3.3kg (-3.4kg to -3.2kg). The mean percentage weight change was -4.0% (-4.0% to -3.9%) and 37% of participants lost ≥5% or more of weight. The mean baseline POCT HbA1c was 41.8mmol/mol (6.0%) with a mean change of -2.04 (-2.12 to -1.96) mmol/mol (-0.19 (-0.19 to -0.18) %). Analysis of characteristics associated with outcomes gave similar results to the intention-to-treat analysis, although weight loss did not differ by sex (supplementary material, Table S5).
Sensitivity analysis using imputed data showed there were no substantive changes in direction and magnitude of the associations (supplementary material, Tables S6-S9). Statistically significant covariates in the complete-case analysis remained significant in the imputed analysis, with the exception of a single (60-64 year) age group for weight change and mixed ethnicity for completion, the latter placing some uncertainty on the significance of mixed ethnicity. A number of subcategories were significant in the imputed analysis but not in the complete-case analysis. In these cases, there were no substantial differences in the magnitude and sign of the associated coefficient, and no suggested change to the interpretation.
Conclusions
A national programme to provide behavioural support to people with NDH in England was associated with a significant reduction in weight and HbA1c among the 36% of people referred who attended at least one of the group-based intervention sessions. There was a clear dose-response relationship and people who attended more sessions experienced greater reductions in both weight and HbA1c.
Strengths and limitations
This report describes the largest cohort of people offered an intervention within a diabetes prevention programme achieving universal population coverage. It includes objective measures of weight, HbA1c, individual participant data, and flow through the programme and assesses impact on health inequalities. There is some missing data and we have taken a principled and pragmatic approach to consider the effects on data interpretation. Our sensitivity analyses do not vary in terms of the direction and broad magnitude of the findings in the primary analyses providing some reassurance that the missing data have not appreciably biased our conclusions. The uncontrolled nature of this analysis means that external confounders cannot be excluded and there may have been other factors leading to weight loss and HbA1c reductions, including secular trends.
Data on HbA1c change are only available for half the participants where a baseline measure of POCT HbA1c was performed, so that it was directly comparable to subsequent measurements. However, given the cause of these missing data, it is unlikely that this has introduced a specific bias. Moreover, the characteristics of the subset are similar to the complete dataset. At an individual level, the clinical significance of a 1.26mmol/mol (0.12%) reduction in HbA1c is difficult to gauge, as very little data is available internationally with regard HbA1c reductions in response to interventions in the non-diabetic range. However, a “left shift” in HbA1c distribution of 1.26mmol/mol is likely to be significant at population level.
A current limitation is that the last recorded weight available is that measured at the last session attended and at present we do not have data on longer-term outcomes. However, mechanisms for the acquisition of longer-term data have been established, and meanwhile, initial weight loss is a strong predictor of weight loss outcomes in subsequent years (22). From 2017/18, the National Diabetes Audit in England, which involves extracts from healthcare datasets held in primary care settings and hospitals, was expanded to include people at high risk of type 2 diabetes, including those with NDH and hence eligible for the NHS DPP (23). Data will be systematically extracted for those coded with NDH, and linked with the NHS DPP dataset, permitting tracking longitudinally of HbA1c and therefore Type 2 diabetes incidence, weight, other recorded cardiovascular risk factors including blood pressure and lipids, microvascular and cardiovascular disease incidence, and mortality. Recent 30-year follow-up data from the Da Qing Diabetes Prevention Outcome Study demonstrated that lifestyle intervention in people with impaired glucose tolerance, in addition to delaying the onset of Type 2 diabetes, also reduced the incidence of cardiovascular events, microvascular complications, and cardiovascular and all-cause mortality, and increased life-expectancy (3)
Implications of this evaluation
The NHS DPP design was based on a Public Health England commissioned systematic review and meta-analysis assessing the effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes in routine practice over 12-18 months. This found such programmes to be associated with weight loss of 2.5kg (95% CI 1.99, 2.99) and HbA1c reduction of 0.07% (95% CI 0.01, 0.14) (4,5). The pooled incidence rate ratio of Type 2 diabetes among patients attending a diabetes prevention programme compared with those receiving usual care was 0.74 (95% CI 0.58, 0.93), a reduction of 26%. A more recent global systematic review and network meta-analysis of pragmatic DPP studies reporting effects on incidence, weight, and glycaemic parameters demonstrated a similar relative risk reduction of 29%, associated with 2.5kg (95% CI 1.90, 3.00) weight loss but no evidence of a reduction in HbA1c (6). NHS DPP data demonstrate similar weight loss and greater reduction in HbA1c, providing optimism that this programme may lead to reductions in future type 2 diabetes incidence among attendees.
The US DPP reported a mean percentage weight reduction of 4.2% (7), greater than the 2.7% weight loss seen in the NHS DPP intention-to-treat analysis, although the US analysis only included participants who had attended at least 4 intervention sessions. When compared with the 4.0% weight loss seen among completers in the NHS DPP the results are similar. The Finnish DPP reported weight losses of 1.3kg in men and 1.1kg in women (9), and the Australian DPP 1.4kg for participants completing sessions 1-5 and 2.5kg for participants completing session 1-6 (8). Differences in weight loss across the four programmes may reflect differences in intensity, ranging from a median of 14 sessions in the US DPP, a mean of 6 in the Australia DPP and a mean of 2.9 in the Finnish DPP, compared to 8 in the NHS DPP (7–9). Differences in starting weight may also have been contributory; US DPP participants had a mean baseline measurement of 96.8kgs, Australia DPP participants, 87.3kg and Finnish DPP, 95.8kg men and 83.8kg women, compared 83.4kg for NHS DPP participants. None of the programmes in other countries have reported the effects on glycaemic parameters, although the Finnish DPP reported beneficial effects on Type 2 diabetes incidence and cardiovascular risk factors (9).
Beyond the national DPPs it is unusual for behavioural programmes to take a whole-population approach. We are only aware of one randomised controlled trial of a behavioural intervention for weight loss that was offered opportunistically in primary care. The Brief interventions for Weight Loss trial (BWeL) found that 40% of people offered support attended, and 24% completed, a 12-week programme (24), similar to the proportions seen in the NHS DPP, which is a longer programme.
People from more deprived areas were less likely to complete the programme, lost less weight and had smaller reductions in HbA1c. Similarly, BWeL found that participants from lower socioeconomic backgrounds attended fewer sessions, leading to less weight loss (25).
Black, Asian, mixed and other ethnic groups are over-represented in those attending an initial assessment (26), but the adjusted odds ratio of completion amongst Asian groups is 25% lower than white groups. Asian and black groups lost less weight, and black groups had smaller reductions in HbA1c. Uniquely, the effect of ethnicity is independent of socioeconomic status.
Program engagement, retention and adherence are crucial to attain the desired effects. The findings highlight the need to actively target engagement, retention and adherence in specific groups to avoid widening inequalities. There has already been a new round of provider procurement for the NHS DPP, with newly appointed providers starting in August 2019. The payment schedule has been adjusted to provide greater incentives to providers to retain participants of black, Asian, mixed and other ethnicity, and those from more deprived backgrounds. Recognising that a large proportion declined or failed to attend the face-to-face group-based interventions, digital modes of programme delivery will be offered for those that decline or fail to attend the face-to-face interventions. Such programmes have been shown to be associated with weight loss though the effects on glycaemic control are less clear (27). A large uncontrolled pilot of digital prevention interventions conducted in live service environments in England is currently underway (28).
In summary, reductions in weight and HbA1c demonstrated in the NHS DPP are encouraging, compare favourably to those reported in recent meta-analyses of pragmatic studies, and are potentially indicative of future reductions in participant type 2 diabetes incidence.
Supplementary Material
Funding
NHS England funded programme development, implementation and evaluation.
Footnotes
Contributor and guarantor information
All authors are members or attendees of the Healthier You: NHS Diabetes Prevention Programme Expert Reference Group, chaired by JV. Members from inception (JV, SON, BY, NW, KK, SJ) were responsible for developing the service specification for the behavioural intervention and for developing the data fields for the Minimum Dataset. All authors have advised on the operational delivery of the Programme and on the interpretation of data derived via the Minimum Dataset on a quarterly basis since inception in 2015. EB and DB have performed the data analyses, and JF has advised on overall analytic design and multiple imputation. JV, EB, and DB were responsible for study design and initial manuscript drafting. JF, SJ and CB contributed to early draft development. All authors have reviewed drafts of the manuscript and provided constructive feedback and criticism. JV is the guarantor and accepts full responsibility for the work. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Competing interests
All authors have completed the ICMJE uniform disclosure form and declare: JV is the National Clinical Director for Diabetes and Obesity at NHS England and is the Clinical Lead for the Healthier You: NHS Diabetes Prevention Programme. EB is the Head of Health Intelligence (diabetes) for Public Health England and leads analysis of the Diabetes Prevention Programme. DB is an analyst for NHS England and is actively involved in analysis of the programme. JF was the diabetes evidence and evaluation lead at Public Health England until September 2018. CB is the Primary Care Advisor to the NHS Diabetes Programme. BY is Clinical Lead of the National Diabetes Audit for England and Wales and a Trustee of Diabetes UK. KK was Chair of the Programme Development Group for the National Institute for Health and Care Excellence (NICE) public health guidance on Type 2 diabetes: prevention in people at high risk (NICE PH38). KK is also Co-Director of the Leicester Diabetes Centre (LDC), and one of the Programme Providers, Ingeus UK Ltd, provide interventions based on the type 2 diabetes prevention programme developed by LDC. NW was Chair of the Programme Development Group for NICE public health guidance on Type 2 diabetes prevention: population and community-level interventions (NICE PH35). JS represents Public Health England on the NHS England Diabetes Programme Board. SON is the Clinical Director at Diabetes UK.
KK acknowledges support from National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) East Midlands and the NIHR Leicester BRC. SJ is funded by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre and Oxford NIHR Collaboration and Leadership in Applied Health Research.
Prior presentation of data and publication in abstract form
Study data has been presented at the Diabetes UK Annual Professional conference in March 2019 and at the European Association for the Study of Diabetes Annual Conference in September 2019.
References
- 1.Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of Type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 2.Diabetes Prevention Program Research Group. Reduction in the incidence of Type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gong Q, Zhang P, Wang J, et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcomes Study. Lancet Diabetes Endocrinol. 2019;6:452–461. doi: 10.1016/S2213-8587(19)30093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Public Health England. A systematic review and meta-analysis assessing the effectiveness of pragmatic lifestyle interventions for the prevention of Type 2 diabetes mellitus in routine practice. [Accessed 18th May 2019]; Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/733053/PHE_Evidence_Review_of_diabetes_prevention_programmes-_FINAL.pdf.
- 5.Dunkley AJ, Bodicoat DH, Greaves CJ, et al. Diabetes prevention in the real world: effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes and of the impact of adherence to guidelines recommendations: a systematic review and meta-analysis. Diabetes Care. 2014;37(4):922–33. doi: 10.2337/dc13-2195. [DOI] [PubMed] [Google Scholar]
- 6.Galaviz KI, Weber MB, Straus A, et al. Global Diabetes Prevention Interventions: A systematic Review and Network Meta-analysis of the Real-World Impact on Incidence, Weight and Glucose. Diabetes Care. 2018;41(7):1526–1534. doi: 10.2337/dc17-2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ely EK, Gruss SM, Luman ET, et al. A national effort to prevent type 2 diabetes: participant-level evaluation of CDC’s national diabetes prevention program. Diabetes Care. 2017;40(10):1331–1341. doi: 10.2337/dc16-2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunbar J, Jayawardena A, Johnson G, et al. Scaling up diabetes prevention in Victoria, Australia: Policy development, implementation and evaluation. Diabetes Care. 2014;37(4):934–42. doi: 10.2337/dc12-2647. [DOI] [PubMed] [Google Scholar]
- 9.Saaristo T, Moilanen L, Korpi-Hyövälti E, et al. Lifestyle intervention for prevention of type 2 diabetes in primary health care: one-year follow-up of the Finnish National Diabetes Prevention Program (FIN-D2D) Diabetes Care. 2010;33(10):2146–2151. doi: 10.2337/dc10-0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barron E, Clark R, Hewing’s R, et al. Progress of the Healthier You: NHS Diabetes Prevention Programme: referrals, uptake and participant characteristics. Diabet Med. 2018;35(4):513–518. doi: 10.1111/dme.13562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas C, Sadler S, Breeze, et al. Assessing the potential return on investment of the proposed UK NHS diabetes prevention programme in different population subgroups: an economic evaluation. BMJ Open. 2017;7:e014953. doi: 10.1136/bmjopen-2016-014953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute for Health and Clinical Excellence. Type 2 diabetes: prevention in people at high risk. [Accessed 18th May 2019];2012 Available from: https://www.nice.org.uk/guidance/ph38/
- 13.UK Government. Childhood Obesity: a plan for action. [Accessed 18th May 2019];2016 Available from: www.gov.uk/government/publications/childhood-obesity-a-plan-for-action.
- 14.UK Government. Childhood Obesity: a plan for action, chapter 2. [Accessed 18th May 2019];2018 Available from: https://www.gov.uk/government/publications/childhood-obesity-a-plan-for-action-chapter-2.
- 15.Public Health England. The Eatwell guide. [Accessed 23rd September 2019];2018 Available from: https://www.gov.uk/government/publications/the-eatwell-guide.
- 16.Department of Health and Social Care. Physical Activity Guidelines. [Accessed 23rd September 2019];2019 Available from: https://www.gov.uk/government/collections/physical-activity-guidelines.
- 17.Public Health England. NHS Health Check Best Practice Guidance. [Accessed 18th May 2019];2017 Available from: https://www.healthcheck.nhs.uk/commissioners-and-providers/national-guidance/
- 18.NHS England and NHS Improvement. Diabetes Prevention Programme Information Governance and Data Flows Framework 2016. [Accessed 23rd September 2019]; Available at: https://www.england.nhs.uk/wp-content/uploads/2019/09/diabetes-prevention-programme-information-governance-and-data-flows-framework.pdf.
- 19.Department for Communities and Local Government. The English indices of deprivation 2015. [Accessed 23rd September 2019]; Available from: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015.
- 20.WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 21.Hirst JA, McLellan JH, Price CP, et al. Performance of point-of-care HbA1c test devices: implications for use in clinical practice – a systematic review and meta-analysis. Clin Chem Lab Med. 2017;55(2):167–180. doi: 10.1515/cclm-2016-0303. [DOI] [PubMed] [Google Scholar]
- 22.Greenberg L, Stampfer MJ, Schwarzfuchs D, et al. Adherence and success in long-term weight loss diets: the dietary intervention randomized controlled trial (DIRECT) J Am Coll Nutr. 2019;28(2):159–68. doi: 10.1080/07315724.2009.10719767. [DOI] [PubMed] [Google Scholar]
- 23.National Diabetes Audit and Diabetes Prevention Programme (NDA-DPP) pilot study. [Accessed May 2019];2017 Available at: https://digital.nhs.uk/data-and-information/clinical-audits-and-registries/national-diabetes-audit-and-diabetes-prevention-programme-nda-dpp-pilot-study.
- 24.Aveyard P, Lewis A, Tearne S, et al. Screening and brief intervention for obesity in primary care: a parallel, two-arm, randomised trial. Lancet. 2016;388(10059):2492–2500. doi: 10.1016/S0140-6736(16)31893-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Graham J, Tudor K, Jebb SA, et al. The equity impact of brief opportunistic interventions to promote weight loss in primary care: secondary analysis of the BWeL randomised trial. BMC Med. 2019;7(1):51. doi: 10.1186/s12916-019-1284-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NOMIS Official labour market statistics. Ethnic group by sex and age. [Accessed May 2019]; Available from: www.nomisweb.co.uk/census/2011/lc2101ew.
- 27.Joiner KL, Nam S, Whittemore R. Lifestyle interventions based on the diabetes prevention programme delivered via eHealth: A systematic review and meta-analysis. Prev Med. 2017;100:194–207. doi: 10.1016/j.ypmed.2017.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray E, Daff K, Lavida A, et al. Evaluation of the Digital Diabetes Prevention Programme Pilot: Uncontrolled Mixed Methods Study Protocol. BMJ Open. 2019;9(5):e025903. doi: 10.1136/bmjopen-2018-025903. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.