Abstract
“Leaving no one behind” is at the heart of the agenda of the Sustainable Development Goals, requiring that health systems be vigilant to how interventions can be accessed equitably by all, including population subgroups that face exclusion. In the World Health Organization (WHO) South-East Asia Region, inequalities can be found across and within countries but there has been a growing commitment to examining and starting to tackle them. Over the past decade in particular, WHO has been developing an armamentarium of tools to enable analysis of health inequalities and action on health equity. Tools include the Health Equity Assessment Toolkit in built-in database and upload database editions, as well as the Innov8 tool for reorientation of national health programmes. Countries across the region have engaged meaningfully in the development and application of these tools, in many cases aligning them with, or including them as part of, ongoing efforts to examine inequities in population subgroups domestically. This paper reflects on these experiences in Bangladesh, India, Indonesia, Nepal, Sri Lanka and Thailand, where efforts have ranged from workshops to programme reorientation; the creation of assemblies and conferences; and collation of evidence through collaborative research, reviews/synthesis and conferences. This promising start must be maintained and expanded, with greater emphasis on building capacity for interpretation and use of evidence on inequalities in policy-making. This may be further enhanced by the use of innovative mixed methodologies and interdisciplinary approaches to refine and contextualize evidence, with a concomitant shift in attention, developing solutions to redress inequities and anchor health reform within communities. There are many lessons to be learnt in this region, as well as mounting political and popular will for change.
Keywords: equity, health equity assessment, health inequalities, South-East Asia
The case for looking at equity
Equity is at the heart of the agenda of the 2030 Sustainable Development Goals (SDGs), to “leave no one behind”, and encompassed in a number of goals and targets related to poverty, health, education, gender, equality and partnerships (SDGs 1, 3, 4, 5, 10 and 17).1–4 Progressive realization of the SDGs – especially universal health coverage, as part of the health goal (SDG 3) – requires that health systems be continuously vigilant towards intervention coverage and outcomes for the population overall, and also that they specifically look at whether the situation is improving for population subgroups.5
This is especially important in light of what has been known for a long time about the relationship between equity and health reform. Victora and colleagues postulated the “inverse equity hypothesis” many years ago, whereby health reform interventions that are not expressly designed with an equity orientation “will initially reach those of higher socioeconomic status and only later affect the poor. This results in an early increase in inequity ratios for coverage, morbidity, and mortality indicators, followed later by a reduction when the poor gain greater access to the interventions and the rich reach minimum achievable levels for morbidity and mortality, beyond which there are unlikely to be substantial further improvements.”6
As various interventions are rolled out in service of the goals of universal health coverage, therefore, the inverse equity hypothesis is something that countries must assess in relation to various socioeconomic groups, but possibly in relation to other population subgroups, identified by sex, age, education and place of residence.7 Further, given the SDG goal to “leave no one behind”, it is essential to go beyond the common dimensions of inequality and look specifically from a country and regional context. Some dimensions of inequality are more context specific, such as migrant status, race, ethnicity, caste, religion or other characteristics that can differentiate minority subgroups.
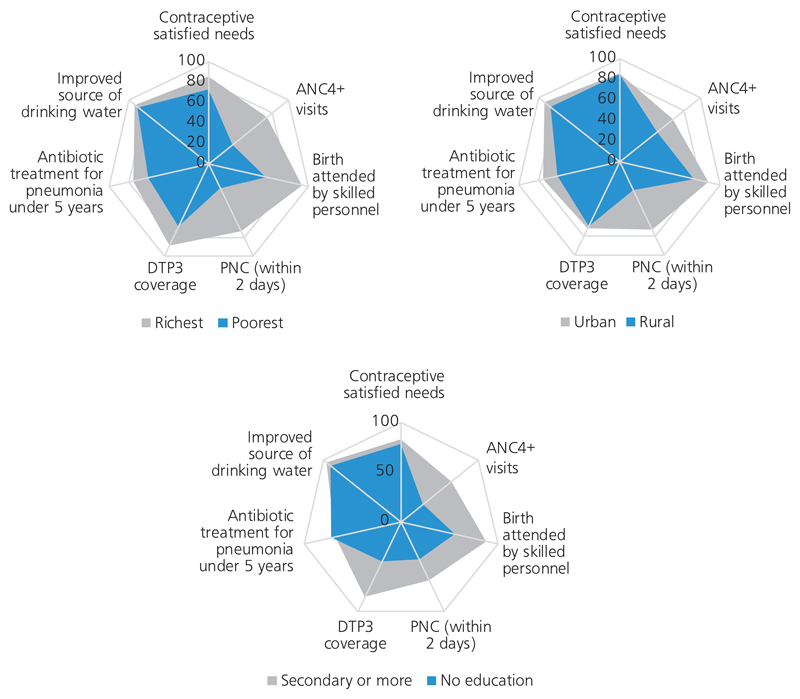
Health-related inequalities exist within all countries, as well as across countries at varying degrees. Fig. 1 illustrates seven areas of health service coverage in the World Health Organization (WHO) South-East Asia Region, comparing three dimensions of inequality: income group, place of residence (urban/rural) and level of education. Understanding these differences, and how they vary over time and among geographic areas when benchmarked against each other, is the first step in acting with an equity orientation.
Fig. 1. Inequalities in coverage of seven essential areas of health service coverage by income group, urban versus rural location and level of education, across the WHO South-East Asia Region.
ANC: four or more antenatal care visits; DTP3: diphtheria–tetanus–pertussis vaccination; PNC: postnatal care
Source: Monitoring progress on universal health coverage and the health-related Sustainable Development Goals in the South-East Asia Region: 2018 update. New Delhi: World Health Organization Regional Office for South-East Asia; 2018 (http://apps.who.int/iris/bitstream/handle/10665/274313/9789290226628-eng.pdf?sequence=6&isAllowed=y).8
Tools for equity analysis: contributions from WHO
While WHO has been supporting Member States with health inequality monitoring for many years, the use and development of various tools to support this and linked processes has been given greater emphasis over the past 5 years. Across WHO regions, capacity-building workshops have been held; a package of resources, including a handbook, a step-by-step manual and an e-learning module, has been created; and numerous tools to facilitate analysis and visualization of health inequalities have been released.9–13 Countries of the WHO South-East Asia Region have played a pivotal role in shaping the nature of capacity-building on health inequality monitoring and the tools that have been created for this purpose.12,14–17
A key milestone in this process has been development of the Health Equity Assessment Toolkit (HEAT), a free and open-source software package, updated in 2018, that displays disaggregated data and summary measures of inequality by six dimensions (economic status, education, place of residence and subnational region, as well as age and sex [where applicable]).12 HEAT draws from the WHO Health Equity Monitor database,18 which includes disaggregated health data based on re-analysis of over 330 demographic and health surveys, multiple indicator cluster surveys and reproductive health surveys carried out between 1991 and 2015, with as many as nine rounds of data for Bangladesh. In 2017, HEAT Plus was launched; this edition of the software allows bespoke data for any indicator (health or otherwise) to be uploaded into a simple template and used for analysis of disaggregated data and summary measures.11 HEAT Plus was developed based on extensive inputs from the WHO South-East Asia Region.14 Another long-standing effort has been the Innov8 package for review and reorientation of national health programmes aiming to “leave no one behind”.19 Innov8 involves an eight-step process where baseline data on a programme are gathered, its theory of change is understood, and then redesign of this theory is collaboratively developed using an equity-oriented, rights-based, gender-responsive approach, mindful of the social determinants of health and measures to monitor, evaluate and ensure sustained attention to leaving no one behind.19 The Innov8 approach has been used to increase equity orientation of policies in a number of countries globally.19–21
Experiences of countries in the WHO South-East Asia Region
There has been a series of capacity-building events in the region related to health equity, supported by WHO. Table 1 illustrates the capacity-building activities carried out using WHO tools in the region. While efforts are under way throughout the region, this paper focuses on a few illustrative country examples with which the authors have greater familiarity and indicates the lessons they offer.
Table 1. Timeline of capacity-building and development of tools for health inequality monitoring and programme reorientation in the WHO South-East Asia Region.
| Scope |
|||||
|---|---|---|---|---|---|
| Dates | Activity | Location/scope | National | Regional | Global |
| April 2013 | Health equity workshop | India | × | ||
| April 2014 | Health inequality monitoring workshop | India | × | ||
| November 2014 to 2017 | Development of Innov8 tool19 | Various | × | ||
| January to July 2015 | Development of HEAT12 (Beta) | WHO headquarters | × | ||
| June 2015 | HEAT12 launch | United States of America | × | ||
| September to November 2015 | Innov819 analysis | Nepal | × | ||
| June 2015 to March 2016 | Development of HEAT Plus11 (Beta) | Indonesia | × | × | |
| April 2016 | HEAT (Plus)11 workshop | Indonesia | × | ||
| June 2016 | Innov819 and AA-HA! programme22 to reach every adolescent | India | × | ||
| December 2016 | Innov819 launch | WHO headquarters | × | ||
| January 2017 | Health inequality monitoring workshop | Thailand | × | × | |
| February 2017 | HEAT12 and HEAT Plus11 workshop | India | × | ||
| July 2017 | HEAT Plus launch | WHO headquarters | × | ||
| August 2017 | HEAT Plus11 workshop | Bangladesh | × | ||
| December 2017 | HEAT Plus11 workshop | Sri Lanka (with a delegation from Myanmar) | × | × | |
| January 2018 – ongoing | Subnational application of HEAT Plus11 | India | × | ||
| September 2018 | HEAT Plus11 workshop | Nepal | × | ||
| October 2018 | Subnational application of HEAT Plus11 | Indonesia | × | ||
Bangladesh
The Government of Bangladesh has demonstrated its commitment to achieving universal health coverage by 2032.23 One of the three main objectives set is to improve equity. In 2017, WHO Bangladesh conducted a workshop on monitoring health inequalities. Prior efforts to look at health equity were already under way in the country, including a Health Equity Watch for which a bespoke survey was carried out in 2002.24 Following this, in 2006, the Bangladesh Health Watch (BHW) was launched to monitor health systems and equity-linked reform in the country. To date, BHW has produced analytical reports on health equity (2006); the health workforce (2007); governance of the health sector (2009); universal health coverage (2011); and urban health (2014). The most recent report in 2016 focuses on challenges raised by noncommunicable diseases for service provision at the primary health-care level; regulatory frameworks; and establishing a comprehensive and integrated surveillance system.25 Future steps in the country will seek to synergize these efforts and create momentum across government, academia and civil society for equity-oriented change in the country.
India
In India, an important stream of work on health equity began with a Health Equity Watch workshop held in collaboration with the WHO country office in Delhi in 2013, followed by regional capacity-building on monitoring health inequality. Following this, extensive case-study documentation of research and action on health equity and the social determinants of health was carried out, culminating in a series of publications,26–29 and the eventual formation, in 2018, of Health Equity Network India (HENI).30 Key findings from these publications include the greater emphasis on socioeconomic inequality in current Indian research; the overall disconnect between research and policy-making; and the fact that many models of concerted action on social determinants of health do exist, but are not identified as such, not evaluated and not considered at scale. Various studies with hard-to-reach populations are under way. A programme of work to carry out health inequality monitoring at the district and subdistrict level in the state of Kerala, as part of monitoring comprehensive primary health-care reforms, was also initiated early in 2018.31 At the national level, the newly launched India Strategy for Women’s Adolescents’ and Children’s Health places emphasis on disaggregated data and has a separate set of recommendations on ensuring inclusion.32
Indonesia
In Indonesia, there was enthusiastic adoption of health inequality monitoring, culminating in the creation of a State of health inequality report in 2017,33 followed by a special issue of the journal Global Heath Action showcasing the various analyses undertaken as part of this exercise.14–17,34 In addition to HEAT Plus,11 the Innov8 tool19 was also used for analysis and reorientation of the country’s action plans for neonatal and maternal health and the National Action Plan on School Aged Children and Adolescent Health 2017–2019,35 to “leave no one behind”.11,21 Processes have revealed key geographic areas of the country that require additional attention, as well as emerging areas of emphasis (water and sanitation, adolescent smoking) where inequalities exist.15,17 Finally, a conversation around health inequalities has allowed more granular analysis of the Public Health and Development Index in the state, which was designed for programmatic priority-setting and can now be looked at in light of not just average index scores, but also inequalities in the score across regions.16 Currently, the government is looking at how to develop subnational analyses using the HEAT Plus toolkit and various other data sources that are relevant for more local decision-making.
Nepal
Through the Nepal Health Sector Strategy, the Government of Nepal has made a commitment to universal health coverage ensuring health for all.36 As Nepal is transitioning towards federalism, it provides an opportunity to restructure and centre the health systems around the principles of universal health coverage. In response to this, the WHO Nepal country office conducted a two-day workshop in 2018 to build local government staff capacity on health inequality monitoring and equity analysis, using HEAT Plus.11 This built on a pilot study in 2015 of Nepal’s adolescent sexual and reproductive health programme using the WHO Innov8 tool,19 which allowed identification of target subpopulations of adolescents who were either being missed by the national programme, or received suboptimal benefit from the programme.20 These recommendations were incorporated in the revised Adolescent Development and Health Strategy in 2017.37 Similarly, in 2016, the government established the Nepal Non-communicable Disease and Injuries Poverty Commission, which, in its 2018 report, identified 23 potential cost-effective interventions to be introduced and/or incrementally intensified by 2030, with an emphasis on the poor.38
Sri Lanka
In Sri Lanka, there was interest around the upload database edition of the toolkit – HEAT Plus11 – and the possibility of using this for facility-based data that exist in the country. At the capacity-building event hosted by this Member State in December 2017, the health department was able to assemble a broad range of stakeholders, including individuals from the statistics, excise and police departments, demonstrating emerging demand for consideration of health equity across sectors. At the workshop, emphasis was placed on gains made in reducing wealth-related inequalities in satisfaction with modern methods of family planning between 2007 and 2016, while also noting growing inequalities across districts. For other indicators, like stunting among children aged under 5 years, district-level inequalities were highlighted and emphasis placed on regions of the country where tea estates dominated: it appeared that these communities needed greater emphasis in service coverage. Beyond family planning and child health, participants also discussed intimate partner violence, where it was observed that the poorest quintile was more likely than all other wealth groups to report violence in 2016. At this stage, it is unclear whether this is related to instrumentation (comprehension of the question), or operationalization of the indicator (which referred to never experiencing violence from an intimate partner), or truly reflects a phenomenon of concern. Whatever the case, it is clearly a key area for further study and policy action.
Thailand
Thailand has served as a frame of reference for many others seeking to bring greater equity considerations into routine programming, particularly in relation to universal health coverage. For example, the country’s model of national health assemblies represents a key framework within which public engagement with decision-making and priority-setting in health can take place.39 Academics from this country have served as trainers for regional workshops on health inequality monitoring. Further, the Prince Mahidol conference for various years has been related to equity – in the context of neglected diseases, underserved populations, transformative learning, the legacy of comprehensive primary health care, political economy/health-in-all/whole-of-society approaches, and more.40 The 2017 conference also featured training on health inequality monitoring. Thailand also uses several data sources to monitor three dimensions of universal health coverage: population coverage, service coverage and financial risk protection.41 There are many lessons for process and country stewardship here, not just for Thailand, but also for the region.
Moving the equity agenda forward
Rising inequities across the world have become a defining challenge of our time. They are putting sustainable development at risk, stirring social unrest, undermining social progress, threatening economic and political stability, and undercutting human rights.4 While evidence shows that income inequality between countries has been falling in recent decades, income inequality within countries (across income levels) has been rising, reaching unprecedented levels in the post-World War II period. A significant majority of households in developing countries – more than 75% of the population – are living today in societies where income is more unequally distributed than it was in the 1990s.42,43 Hence, in South-East Asia, improving capacity for equity analysis for health, by income and other intersecting stratifiers, is timely and needed as reforms are undertaken towards universal health coverage.
As these country experiences have revealed, there is great need, moving forward, to carry out more finely grained analyses of equity as an integral part of universal health coverage-relevant policy implementation and decision-making at national and subnational levels. Here, there is great value in indicator-based quantitative monitoring, as well as qualitative forms of monitoring, such as social audits, community-based monitoring and mixed methods barrier assessments. The use of qualitative evidence of strong quality can also help to move beyond discussions around magnitudes of inequalities to mechanisms, contexts, structures and strictures that allow inequities to both proliferate and perpetuate. In the WHO South-East Asia Region, there is growing recognition of this and demand for interdisciplinary approaches to understand and act on health inequities.
This being the case, as one member of the Health Equity Network India put it, “pathways to health inequities are different from pathways to health equity”. This is an important notion, not just in conceptual, but also in practical terms. Health inequality monitoring is but a first step in determining the root causes of inequalities that can point towards, but are inadequate to fully determine, how equity may be promoted. Sustained and community-led research and programmatic activity on promoting health equity is an essential step in moving forward and must include the development and testing of approaches and processes that foster distribution of resources according to need and are accountable to outcomes at the population level. Equity must remain centre-stage – not just rhetorically, but de facto – in the emerging agenda of universal health coverage, anchored in the legacy of Alma-Ata44 and the continuing movement towards health for all. There are many lessons to be learnt in this region, as well as mounting political and popular will for change.
Acknowledgements
We are grateful to Ms Benedicte Briot for her tireless, on-the-ground support of this process and review of this piece, Dr Neena Raina for her vision and guidance, and delegations and experts from across the region who gave shape and direction to this work. There should be no suggestion that the WHO endorses any specific organization, products or services. This notice should be preserved along with the article’s original URL. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the views, decisions or policies of their institutions.
Source of support
This work was supported by the Wellcome Trust/DBT India Alliance Fellowship (grant number IA/CPHI/16/1/502653) awarded to Dr Devaki Nambiar.
Footnotes
Conflict of interest: None declared.
Authorship: DN created an outline of the paper, RR and DN contributed to the drafting, TSK and ARH provided critical inputs to the manuscript. All authors approved the final version of the manuscript.
References
- 1.Health in 2015: from Millennium Development Goals to Sustainable Development Goals. Geneva: World Health Organization; 2015. [accessed 7 January 2019]. http://apps.who.int/iris/bitstream/handle/10665/200009/eng.pdf;jsessionid=F45741B9900E9690B7C68DF74F918E8C?.sequence=1. [Google Scholar]
- 2.Transforming our world: the 2030 Agenda for Sustainable Development. New York: United Nations; 2015. [accessed 7 January 2019]. A/RES/70/1; https://sustainabledevelopment.un.org/content/documents/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf. [Google Scholar]
- 3.Hosseinpoor AR, Bergen N, Magar V. Monitoring inequality: an emerging priority for health post-2015. Bull World Health Organ. 2015;93:5915–91A. doi: 10.2471/BLT.15.162081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Report of the High-Level Committee on Programmes at its thirty-second session. New York: United Nations; 2016. [accessed 7 January 2019]. Equality and non-discrimination at the heart of sustainable development: a shared United Nations Framework for Action. CEB/2016/6/Add.1; https://www.unsceb.org/CEBPublicFiles/CEB_2016_6%20_Add.1%20%28inequalities%20framework%29.pdf. [Google Scholar]
- 5.Hosseinpoor AR, Bergen N, Koller T, Prasad A, Schlotheuber A, Valentine N, et al. Equity-oriented monitoring in the context of universal health coverage. PLoS Med. 2014;11:e1001727. doi: 10.1371/journal.pmed.1001727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Victora CG, Vaughan JP, Barros FC, Silva AC, Tomasi E. Explaining trends in inequities: evidence from Brazilian child health studies. Lancet. 2000;356:1093–8. doi: 10.1016/S0140-6736(00)02741-0. [DOI] [PubMed] [Google Scholar]
- 7.Evans T, Brown H. Road traffic crashes: operationalizing equity in the context of health sector reform. Inj Control Saf Promot. 2003;10:11–12. doi: 10.1076/icsp.10.1.11.14117. [DOI] [PubMed] [Google Scholar]
- 8.Monitoring progress on universal health coverage and the health-related Sustainable Development Goals in the South-East Asia Region: 2018 update. New Delhi: World Health Organization Regional Office for South-East Asia; 2018. [accessed 7 January 2019]. http://apps.who.int/iris/bitstream/handle/10665/274313/9789290226628-eng.pdf?sequence=6&isAllowed=y. [Google Scholar]
- 9.Handbook on health inequality monitoring with a special focus on low- and middle-income countries. Geneva: World Health Organization; 2013. [accessed 7 January 2019]. http://apps.who.int/iris/bitstream/handle/10665/85345/9789241548632_eng.pdf?sequence=1. [Google Scholar]
- 10.Hosseinpoor AR, Bergen N, Schlotheuber A, Grove J. Measuring health inequalities in the context of sustainable development goals. Bull World Health Organ. 2018;96:654–9. doi: 10.2471/BLT.18.210401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hosseinpoor AR, Schlotheuber A, Nambiar D, Ross Z. Health Equity Assessment Toolkit Plus (HEAT Plus): software for exploring and comparing health inequalities using uploaded datasets. Glob Health Action. 2018;11(Suppl. 1) doi: 10.1080/16549716.2018.1440783. 1440783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hosseinpoor AR, Nambiar D, Schlotheuber A, Reidpath D, Ross Z. Health Equity Assessment Toolkit (HEAT): software for exploring and comparing health inequalities in countries. BMC Med Res Methodol. 2016;16:141. doi: 10.1186/s12874-016-0229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hosseinpoor AR, Bergen N, Schlotheuber A. Promoting health equity: WHO health inequality monitoring at global and national levels. Glob Health Action. 2015;8 doi: 10.3402/gha.v8.29034. 29034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosseinpoor AR, Nambiar D, Tawilah J, Schlotheuber A, Briot B, Bateman M, et al. Capacity building for health inequality monitoring in Indonesia: enhancing the equity orientation of country health information system. Glob Health Action. 2018;11(Suppl. 1) doi: 10.1080/16549716.2017.1419739. 1419739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afifah T, Nuryetty MT, Cahyorini, Musadad DA, Schlotheuber A, Bergen N, et al. Subnational regional inequality in access to improved drinking water and sanitation in Indonesia: results from the 2015 Indonesian National Socioeconomic Survey (SUSENAS) Glob Health Action. 2018;11(Suppl. 1) doi: 10.1080/16549716.2018.1496972. 1496972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suparmi, Kusumawardani N, Nambiar D, Trihono, Hosseinpoor AR. Subnational regional inequality in the public health development index inIndonesia. Glob Health Action. 2018;11(Suppl. 1) doi: 10.1080/16549716.2018.1500133. 1500133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kusumawardani N, Tarigan I, Suparmi, Schlotheuber A. Socioeconomic, demographic and geographic correlates of cigarette smoking among Indonesian adolescents: results from the 2013 Indonesian Basic Health Research (RISKESDAS) survey. Glob Health Action. 2018;11(Suppl. 1) doi: 10.1080/16549716.2018.1467605. 1467605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hosseinpoor AR, Bergen N, Schlotheuber A, Victora C, Boerma T, Barros AJ. Data resource profile: WHO Health Equity Monitor (HEM) Int J Epidemiol. 2016;45:14041–405e. doi: 10.1093/ije/dyw176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Innov8 approach for reviewing national programmes to leave no one behind. Geneva: World Health Organization; 2016. [accessed 7 January 2019]. http://apps.who.int/iris/bitstream/handle/10665/250442/9789241511391-eng.pdf?ua=1. [Google Scholar]
- 20.Adolescent sexual and reproductive health programme to address equity, social determinants, gender and human rights in Nepal. New Delhi: World Health Organization Regional Office for South-East Asia; 2017. [accessed 7 January 2019]. http://www.searo.who.int/nepal/documents/review_of_the_national_asrh_programme.pdf?ua=1. [Google Scholar]
- 21.Koller TS, Saint V, Floranita R, Koemara Sakti GM, Pambudi I, Hermawan L, et al. Applying the Innov8 approach for reviewing national health programmes to leave no one behind: lessons learnt from Indonesia. Glob Health Action. 2018;11(Suppl. 1) doi: 10.1080/6549716.2018.1423744. 1423744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. [accessed 7 January 2019];Global Accelerated Action for the Health or Adolescents (AA-HA!): guidance to support country implementation. https://www.who.int/maternal_child_adolescent/topics/adolescence/framework-accelerated-action/en/
- 23.Expanding social protection for health: towards universal coverage – Health Care Financing Strategy 2012–2032. Dhaka: Ministry ofHealth and Family Welfare, Government of the People’s Republic of Bangladesh; 2012. [accessed 7 January 2019]. http://socialprotection.gov.bd/wp-content/uploads/2017/03/HCF-Strategy-Bd-2012-2032.pdf. [Google Scholar]
- 24.Ahmed SM, Bhuiya A, Rana AKMM, Hadi A, Mahmud S, Salam A, et al. Monitoring the status of health equity in Bangladesh: The BHEW Survey 2002. Dhaka: Bangladesh Health Equity Watch; 2003. [accessed 7 January 2019]. http://research.brac.net/new/event/survey2002. [Google Scholar]
- 25.Ahmed SM. Non communicable diseases in Bangladesh: current scenario and future directions. Dhaka: Bangladesh Health Watch; 2017. [accessed 7 January 2019]. Bangladesh Health Watch Report 2016. https://www.brac.net/images/news/2017/bhw_report2016_final.pdf. [Google Scholar]
- 26.Nambiar D, Muralidharan A, editors. The social determinants of health in India: concepts, processes, indicators. Singapore: Springer Singapore; 2017. [Google Scholar]
- 27.Bhan N, Rao KD, Kachwaha S. Health inequalities research in India: a review of trends and themes in the literature since the 1990s. Int J Equity Health. 2016;15(1):166. doi: 10.1186/s12939-016-0457-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prasad P, Jesani A, editors. Equity and access: health care studies in India. New Delhi: Oxford University Press India; 2018. [Google Scholar]
- 29.Ravindran TKS, Gaitonde R, editors. Health inequities in India: a synthesis of recent evidence. Singapore: Springer Singapore; 2017. [Google Scholar]
- 30.Ravindran TKS, Seshadri T. A health equity research agenda for India: results of a consultative exercise. Health Res Policy Syst. 2018;16(Suppl. 1):94. doi: 10.1186/s12961-018-0367-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The George Institute for Global Health India. Assessing equity of universal health coverage in India: from data to decision-making usingmixed methods. [accessed 7 January 2019]; https://www.georgeinstitute.org.in/projects/assessingequity-of-universal-health-coverage-in-india-from-data-to-decisionmaking-using.
- 32.I-WACH: India strategy for women’s, adolescents’ and children’s health. New Delhi: Ministry of Health and Family Welfare, Government of India; 2018. [Google Scholar]
- 33.State of health inequality: Indonesia. Interactive visualization of health data. Geneva: World Health Organization; 2017. [accessed 7 January 2019]. http://apps.who.int/iris/bitstream/handle/10665/259685/9789241513340-eng.pdf;jsessionid=E990CD7115A1C44AEE25E6DFC647C712?sequence=1. [Google Scholar]
- 34.Hosseinpoor AR, Nambiar D, Suparmi, Kusumawardani N. Data source mapping: an essential step for health inequality monitoring. Glob HealthAction. 2018;11(Suppl. 1) doi: 10.1080/16549716.2018.1456743. 1456743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. Leaving no adolescent behind in health and development in Indonesia. [accessed 7 January 2019]; https://www.who.int/life-course/partners/innov8/indonesia-adolescents/en/index1.html.
- 36.Nepal Health Sector Strategy 2015–2020. Kathmandu: Government of Nepal Ministry of Health and Population; 2015. [accessed 7 January 2019]. http://nhsp.org.np/wp-content/uploads/2016/08/NHSS-English-Book-final-4-21-2016.pdf. [Google Scholar]
- 37.National Adolescent Development and Health Strategy Nepal 2018 [in Nepali] Kathmandu: Ministry of Health and Population, Government of Nepal; 2019. [Google Scholar]
- 38.An equity initiative to address noncommunicable diseases and injuries. National report – 2018. Kathmandu: The Nepal NCDI Poverty Commission; 2018. [accessed 7 January 2019]. https://static1.squarespace.com/static/55d4de6de4b011a1673a40a6/t/5abe85111ae6cfa98183e7a9/1522435346791/Nepal+NCDI+Poverty+Commission+National+Report+2018.pdf. [PubMed] [Google Scholar]
- 39.Rasanathan K, Posayanonda T, Birmingham M, Tangcharoensathien V. Innovation and participation for healthy public policy: the first National Health Assembly in Thailand. Health Expect. 2012;15:87–96. doi: 10.1111/j.1369-7625.2010.00656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.PMAC. Prince Mahidol Award Conference; [accessed 7 January 2019]. http://www.pmaconference.mahidol.ac.th/index.php?option=com_content&view=article&id=548&Itemid=194. [Google Scholar]
- 41.Witthayapipopsakul W, Kulthanmanusorn A, Vongmongkol V, Viriyathorn S, Wanwong Y, Tangcharoensathien V. Achieving the targets for universal health coverage: how is Thailand monitoring progress? WHO South-East Asia J Public Health. 2019;8(1):10–17. doi: 10.4103/2224-3151.255343. [DOI] [PubMed] [Google Scholar]
- 42.Poverty reduction. Humanity divided: confronting inequality in developing countries. New York: United Nations Development Programme; [accessed 7 January 2019]. https://www.undp.org/content/dam/undp/library/Poverty%20Reduction/Inclusive%20development/Humanity%20Divided/HumanityDivided_Full-Report.pdf. [Google Scholar]
- 43.Global trends: challenges and opportunities in the implementation of the sustainable development goals. New York: United Nations Development Programme, United Nations Research Institute for Social Development; 2017. [accessed 7 January 2019]. http://www.undp.org/content/undp/en/home/librarypage/sustainable-development-goals/global-trends--challenges-and-opportunities-in-the-implementatio.html. [Google Scholar]
- 44.Declaration of Alma-Ata. International Conference on Primary Health Care; 6–12 September 1978; Alma-Ata: USSR; [accessed 7 January 2019]. https://www.who.int/publications/almaata_declaration_en.pdf?ua=1. [Google Scholar]