Universal health coverage means that every person everywhere should have affordable access to good quality essential health services. The governments of South Asian countries have embraced the goal of universal health coverage, which is the centrepiece of commitments to deliver the third health related sustainable development goal (SDG). Universal health coverage is linked to other SDGs related to poverty (SDG 1), education (SDG 4), gender (SDG 5), equality (SDG 10), and partnerships (SDG 17).1 Its association with SDG 11 focused on sustainable cities and communities, is comparatively overlooked.
An impediment to achieving universal health coverage is rapid urbanisation. A powerful engine of social and economic growth in the region, urbanisation also brings uneven development and hampers efforts to protect the health and access to healthcare of the urban poor and disadvantaged in South Asian cities. The complexities of scale, rapidity of change, and the diversity of urban dwellers upend typical approaches to financial protection and overwhelm the capacity of urban health systems.
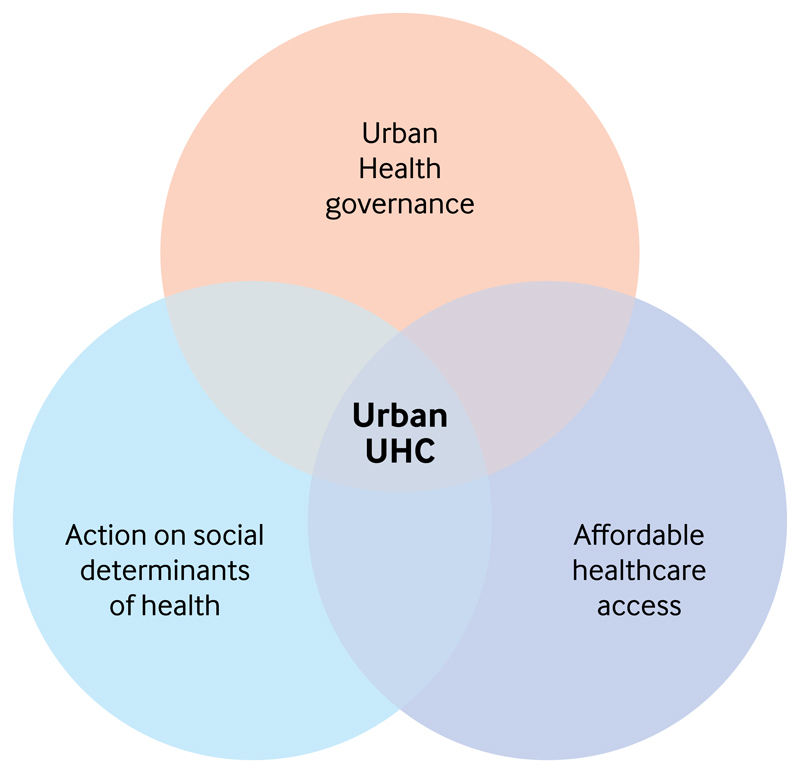
A review of grey and published literature strongly indicates that these urban complexities and the growing health disparities they produce require an urban sensitive approach to universal health coverage. We suggest a simple framework that identifies three areas of priority intervention that are necessary to achieving universal health coverage and greater health equity in South Asian cities (fig 1). We describe the realities of each of these areas and suggest priority actions based on this framework.
Fig 1.
An urban sensitive universal health coverage framework, UHC, urban health coverage
Health disparities in South Asian cities
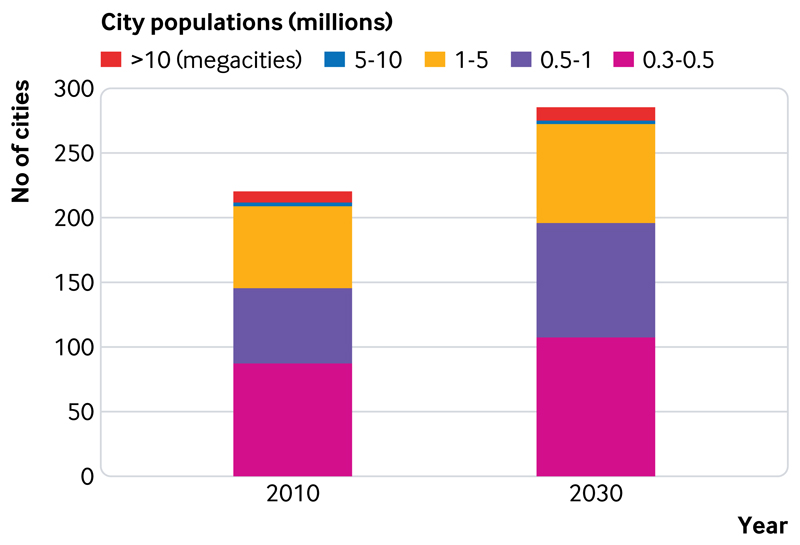
South Asia's urban population is projected to grow to 250 million by 2030.2 The agglomeration of people, innovation, and industry in cities is expected to increase the GDP by ≥7% a year. Greater prosperity is not confined to megacities of >10 million (fig 2), but also evident in the rapid proliferation of middle sized towns and cities.3
Fig 2.
Pattern of urbanisation in South Asia
The demographic pressures of rural, urban, intercity, and intercountry migration, extreme disparities of living conditions across social classes, hazardous transport and stressful traffic conditions, a changing climate, and erratic weather patterns create a wide range of challenges to health in South Asian cities. These include the threat of old and emerging infectious diseases; malnutrition, from underweight and stunting to overweight and obesity; maternal and child health; non-communicable diseases—a leading burden of disease; mental health disorders; and injuries related to road accidents, violence, and the workplace.4
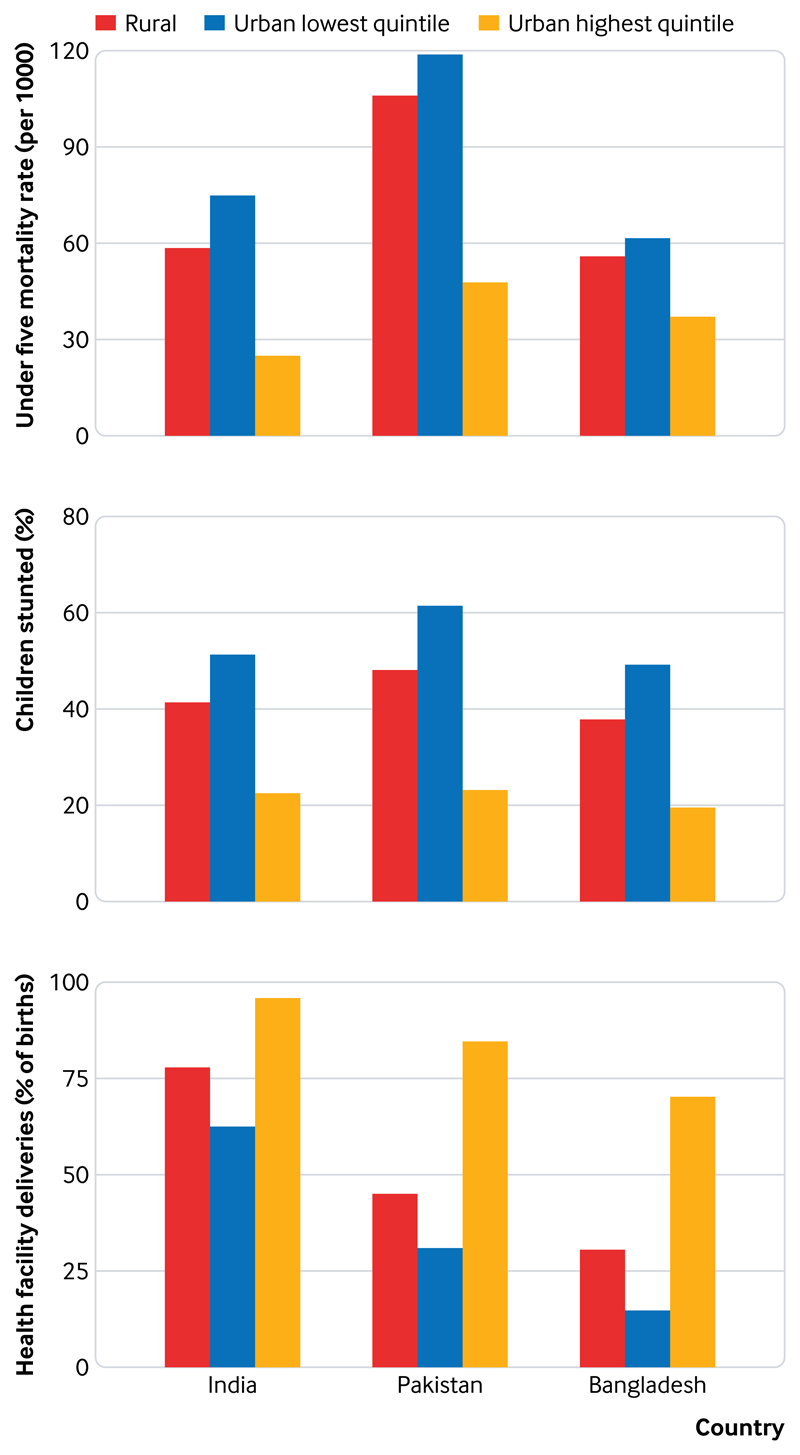
Within urban settings, among the most endangered by health risks and the least likely to have access to affordable health services are those living in informal settlements or slums, which are an entry point for migrants and home to about 130 million South Asians.2 The disparities in health outcomes between those in the highest and lowest socioeconomic quintiles are enormous, with rural dwellers outperforming the urban poorest on almost every indicator (fig 3).
Fig 3.
Urban quintile and rural comparisons for selected health indicators by country (based on Demographic and Health Survey Data: India 2015-16; Pakistan 2012-13; Bangladesh 2014)
Urban health governance
Perhaps the greatest challenge in realising universal health coverage in South Asia's cities is urban health governance. Typically complex and often contested, many urban health governance structures in the region echo a shared British colonial past.5 This legacy left responsibilities for primary healthcare delivery and services related to health, like water and sanitation, to cities and municipalities.6–9 Today, these authorities typically lack human, financial, and technical resources,10 even when provision of such services is constitutionally mandated.5, 11 Efforts to devolve power to city governments are motivated by the principle of subsidiarity. This brings decision making closer to the people by giving responsibility for key public services to locally elected officials. However, in practice, urban governance for health is distributed unevenly across national, regional, and municipal governments.5, 7 It spans public, private for-profit, and not-for-profit providers of various types,12, 13 and is characterised by internal politics at various levels,14–16 and almost systemic exclusion of vulnerable populations.17
South Asian cities are distinguished by a large private sector,13, 18 with the power to sustain existing profit and market share. The private sector is weakly regulated and largely unaccredited and ignored in national health information systems. Practices such as overcharging, inappropriate referral, substandard or unnecessary treatment, dual practice, bribes, and pharmaceutical industry influence are also widespread.19, 20
Compounding these challenges are insufficient allocations towards urban health reforms. This is due, in part, to the historical emphasis (much needed, of course) on rural primary healthcare systems.5, 16 The lack of investment, coordination, and oversight characterising health systems in South Asian cities has had the effect of urban health governance being “nobody's business.”
Access to healthcare
Healthcare in South Asian megacities is dense, diverse, and difficult to navigate. This is especially true for the urban poor, who lack the health literacy, time, and social and financial resources necessary for optimal care seeking.21 The challenges are well known—poor infrastructure, uncoordinated and fragmented health service delivery, suboptimal financing, insufficient coordination among multiple agencies, dynamic and heterogeneous population needs, and weak public primary care capacity.22 In addition, the epidemiological transition and the increasing prevalence of non-communicable diseases put additional stress on overburdened urban health systems.
In most South Asian cities, public sector service delivery is strong at the tertiary level but overcrowded as government hospitals serve city residents as well as patients from around the country.23 Research suggests that the public system has been unable to provide universal access to the required range of primary health services additional to maternal and child healthcare.5, 24 Referral across levels of care is neglected, which means that medical treatment is prioritised over prevention and wellness.24 Dubious practices are also common, such as the transfer of patients at high risk from private facilities to public sector hospitals.25 A notable exception is Sri Lanka, where high technical quality in inpatient and outpatient primary care has been observed in both public and private sectors.26, 27
At the same time, demand for care has increased, with the private sector filling the gap. This includes multiple levels of specialisation and different systems of medicine provision with a wide range of costs and quality, from boutique hospital chains to itinerant drug peddlers.13, 28, 29 It is not surprising that urban populations in South Asia are more likely to consult a private healthcare provider (table 1). Informal drug shops clustering in and around hospitals and informal settlements are the first point of care for many of the urban poor seeking longer hours of operation, credit, and unregulated access to medicine.5, 30
Table 1. Consultation with different healthcare providers (%) among urban populations in South Asia.
| Asia | Bangladesh (2010) | India (2015-16) | Pakistan (2014-15) |
|---|---|---|---|
| Private hospital or clinic (%) | 83 | 56 | 76 |
| Public sector facility (%) | 13 | 42 | 20 |
| Others (%) | 4 | 2 | 4 |
Source: Authors, using India's National Family Health Survey 4, India (2015-16); Pakistan's Social and Living Standards Measurement Survey (2014-15); and Household Income and Expenditure Survey, Bangladesh (2010).
Access inequities continue to grow as a result of high out-of-pocket expenditure on health. This is encouraged by provider practices of irrational prescribing and unnecessary care, and patient demand for investigations and treatments, such as injections and antibiotics, to hasten recovery.28 Consequently, spending on medicines and diagnostics accounts for around two thirds of national out-of-pocket expenditure across South Asia, largely due to urban spending.29, 31, 32 In the absence of social insurance, rational care seeking, and reduced costs of care, the rates of medical impoverishment are expected to increase.33 Already the risk of incurring catastrophic health expenditure and impoverishment due to out-of-pocket spending is substantial in South Asian countries (table 2). Urban specific data are lacking, but this risk is likely to be as great or even greater among poor urban households compared with the rural average.
Table 2. Financing indicators for South Asian countries in tracking universal health coverage34 .
| Bangladesh (2010) | India (2011) | Nepal (2010) | Pakistan (2010) | Sri Lanka (2009) | |
|---|---|---|---|---|---|
| SDG-UHC indicator 3.8.2, latest year: incidence of catastrophic expenditure (%)* | 13.57 | 17.33 | 27.41 | 1.03 | 2.89 |
| Incidence of impoverishment due to out-of-pocket health spending (%)† | 4.51 | 4.16 | 1.85 | 1.00 | 0.05 |
Note: Urban-specific data unavailable; data for Pakistan may need to be interpreted with caution.
At 10% of household total consumption or income.
Poverty line: at 2011 purchasing power parity $1.90 a day.
SDG, sustainable development goal; UHC, universal health coverage.
Social determinants of health equity
Health in South Asian cities is powerfully determined by urbanisation and other determinants of health, which intersect and amplify inequities in health outcomes.35–38 These are most visible in vast informal settlements where conditions of overcrowding, inadequate sanitation, poor access to clean water, poverty, malnutrition, and proximity to open drains, riverbanks, and dumping sites increase vulnerability to infectious diseases such as diarrhoea, respiratory illness, and tuberculosis.5, 39, 40 Urban density and lifestyles also contribute to rising rates of cardiovascular disease, diabetes, asthma, and cancers and their risk factors.5, 29, 41 The harmful health effects of toxic air pollution related to vehicular and industrial emissions, burning, dust, and construction are ubiquitous in the megacities of South Asia.42, 43 The depletion and disruption of natural environmental systems, including the water supply, coupled with the destabilising effects of climate change, are a further challenge to South Asia's cities, with population densities among the highest in the world.44
Crime and violence are simmering determinants of urban health, affecting the mental health and security of all urban dwellers, but with disproportionate effects on women: a recent poll ranked Karachi, Delhi, and Dhaka among the 10 most dangerous megacities for women in the world.45–47
The health effects of rapid, unplanned urbanisation are also apparent in high rates of pedestrian and occupational injuries and deaths, especially among the poorest.45
Towards an urban sensitive approach to universal health coverage
To attain universal health coverage in South Asian countries, the specific challenges of urban settings must be taken into account. However, current frameworks provide inadequate guidance. Galea et al offer a research model that recognises the many influences on the health of urban populations. However, it fails to capture the interactions that produce inequities in health that must be dealt with when designing interventions.48 The framework of the World Health Organization Commission on CO the Social Determinants of Health (CSDH) illustrates how structural and intermediate factors interact, leading to health inequities. It does not state which of these influences is more or less important in urban settings.49 The CSDH knowledge networks have used health assessment to both monitor and act on urban health inequities. The results are promising, albeit in cities outside South Asia.50, 51 Frameworks guiding efforts towards universal healthcare focus on service coverage and its financing, with priority given to financial protection of the poor and disadvantaged. They acknowledge that governance and social determinants are important, but their particular significance in achieving urban universal health coverage is not emphasised.34
The framework we present applies our understanding of universal health coverage to the scale and complexities of South Asian urban cities. It shows how the features and activities of urban governance, health service delivery, and sectors influencing health must coalesce to provide universal health coverage in view of the growing demand for services and increasing inequities arising from rapid, unplanned urbanisation.
The first domain is urban health governance, and the need to strengthen regulation of a large and diverse healthcare landscape, and to ensure that all sectors consider health effects. To ensure a more equitable distribution of power and resources, forms of governance are required that engage and empower urban citizens, especially the most disadvantaged, and promote accountability of all stakeholders.
A second dimension is affordable healthcare access. This requires attention to subgroups at particular risk of poor health and medical impoverishment. In addition to a solid foundation of quality primary healthcare with effective referral, we must consider financing and social protection, public-private partnerships that enable universal health coverage and also reduce any barriers to receiving services among vulnerable populations.
The third dimension incorporates actions that tackle the social determinants of health equity. These include intersectoral actions in housing, food, transportation, air quality, water, and sanitation, and other determinants that affect population subgroups differentially and prevent attainment of universal urban health reform.
This framework is intended to catalyse cross-city as well as regional learning and reflection to develop urban sensitive interventions as part of universal health coverage reform in the region as a whole.
Key Messages.
South Asia's cities exemplify the perils of rapid unplanned urbanisation and its adverse health effects
Urban governance for health must emphasise the stewardship and regulation of urban services, greater municipal agency, and citizen engagement
Strengthened access to healthcare requires a solid foundation of urban primary care with effective referral, public-private partnerships that enable universal health coverage, and a focus on vulnerable populations
Sustained health improvement depends on coordinated actions that tackle the social, environmental, and other structural determinants of health inequities
Footnotes
Contributors and sources: AMA developed the outline for the paper, with valued input from all authors. AMA, DN, SS, BBA, and SR contributed sections to the paper, drawing on research from their respective countries and their previous research in the area. AMA and DN consolidated drafts and coordinated further revisions. All authors reviewed and approved the final manuscript. DN was supported by a grant on urban health research from the Indian Council for Social Science Research and is a Wellcome Trust/DBT India Alliance Intermediate Investigator in Public Health.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1.World Health Organization. Health in 2015: from Millennium Development Goals to Sustainable Development Goals. World Health Organization; 2015. [Google Scholar]
- 2.Ellis P, Roberts M. Leveraging urbanisation in South Asia: managing spatial transformation for prosperity and livability. World Bank Group; 2016. https://openknowledge.worldbank.org/bitstream/handle/10986/22549/2015_0903%20SOUTH%20ASIA%20REPORT%20OVERVIEW.pdf?sequence=11. [Google Scholar]
- 3.United Nations Department of Economic and Social Affairs. Revision of world urbanization prospects. 2018 https://www.un.org/development/desa/publications/2018-revision-of-world-urbanization-prospects.html.
- 4.World Health Organization. The WHO Centre for Health Development and United Nations Human Settlements Programme. UNHabitat, Kobe; 2010. Hidden cities: unmasking and overcoming health inequities in urban settings. http://www.who.int.proxy1.library.jhu.edu/kobe_centre/publications/hiddencities_media/who_un_habitat_hidden_cities_web.pdf. [Google Scholar]
- 5.Technical Resource Group - National Urban Health Mission. Making the Urban Health Mission work for the urban poor: report of the technical resource group Urban Health Mission National Health Mission. Ministry of Health and Family Welfare; 2014. [Google Scholar]
- 6.Sarker AE. The political economy of decentralized governance: an assessment of rural local government reforms in Bangladesh. Int J Public Adm. 2006;29:1285–309. doi: 10.1080/01900690600928128. [DOI] [Google Scholar]
- 7.Ganesan P, Nambiar D, Sundararaman T. Who's in charge of social determinants of health? Understanding the office of the municipal health officer in urban areas. In: Nambiar D, Muralidharan A, editors. The social determinants of health in India: concepts, processes, indicators. Springer; 2017. pp. 103–15. [DOI] [Google Scholar]
- 8.Lahariya C. Mohalla clinics of Delhi, India: could these become platform to strengthen primary healthcare? J Family Med Prim Care. 2017;6:1–10. doi: 10.4103/jfmpc.jfmpc_29_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zaidi S. Sindh health sector strategy 2012–2020. The Aga Khan University; 2012. https://ecommons.aku.edu/cgi/viewcontent.cgi?article=1215&context= pakistan_fhs_mc_chs_chs. [Google Scholar]
- 10.Sharma J, Osrin D, Patil B, et al. Newborn healthcare in urban India. J Perinatol. 2016;36(s3):S24–31. doi: 10.1038/jp.2016.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazhar MA, Shaikh BT. Constitutional reforms in Pakistan: turning around the picture of health sector in Punjab Province. J Ayub Med Coll Abbottabad. 2016;28:386–91. [PubMed] [Google Scholar]
- 12.Sengupta A, Nundy S. The private health sector in India. BMJ. 2005;331:1157–8. doi: 10.1136/bmj.331.7526.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sengupta A, Mukhopadhyay I, Weerasinghe MC, Karki A. The rise of private medicine in South Asia. BMJ. 2017;357:j1482. doi: 10.1136/bmj.j1482. [DOI] [PubMed] [Google Scholar]
- 14.Ravi A. AAP's 1000 Mohalla clinics still a long way off. Sunday Guard Live. 2017 Jan 14; https://www.sundayguardianlive.com/news/8024-aap-s-1000-mohalla-clinics-still-long-way. [Google Scholar]
- 15.Khurshid al. SHC orders Jinnah Hospital, its subsidiaries to be under central govt. The News. 2016 Jul 5; https://www.thenews.com.pk/print/133059-SHC-orders-Jinnah-Hospital-its-subsidiaries-to-be-under-central-govt. [Google Scholar]
- 16.Shafique S, Bhattacharyya DS, Anwar I, Adams A. Right to health and social justice in Bangladesh: ethical dilemmas and obligations of state and non-state actors to ensure health for urban poor. BMC Med Ethics. 2018;19(Suppl 1):46. doi: 10.1186/s12910-018-0285-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nambiar D, Mander H. Inverse care and the role of the state: the health of the urban poor. Bull World Health Organ. 2017;95:152–3. doi: 10.2471/BLT.16.179325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Afsana K, Wahid SS. Health care for poor people in the urban slums of Bangladesh. Lancet. 2013;382:2049–51. doi: 10.1016/S0140-6736(13)62295-3. [DOI] [PubMed] [Google Scholar]
- 19.Gadre A, Shukla A. Dissenting diagnosis. Random House; 2016. [Google Scholar]
- 20.Jain A, Nundy S, Abbasi K. Corruption: medicine's dirty open secret. BMJ. 2014;348:g4184. doi: 10.1136/bmj.g4184. [DOI] [PubMed] [Google Scholar]
- 21.Aleemi AR, Khaliqui H, Faisal A. Challenges and patterns of seeking primary health care in slums of Karachi: a disaster lurking in urban shadows. Asia Pac J Public Health. 2018;30:479–90. doi: 10.1177/1010539518772132. [DOI] [PubMed] [Google Scholar]
- 22.Lahariya C, Bhagwat S, Saksena P, Samuel R. Strengthening urban health for advancing universal health coverage in India. J Health Manag. 2016;18:361–6. doi: 10.1177/0972063416663534. [DOI] [Google Scholar]
- 23.van Weel C, Kassai R, Qidwai W, et al. Primary healthcare policy implementation in South Asia. BMJ Glob Health. 2016;1:e000057. doi: 10.1136/bmjgh-2016-000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sundararaman T, Muraleedharan VR. Falling sick, paying the price. Econ Polit Wkly. 2015;50:16–20. [Google Scholar]
- 25.Adams AM, Ahmed R, Shuvo TA, et al. The private healthcare sector in Bangladesh: a qualitative assessment of motivations, strategies and opportunities for engagement around national public health goals. Icddr,b; 2015. [Google Scholar]
- 26.Rannan-Eliya RP, Wijemanne N, Liyanage IK, et al. Quality of inpatient care in public and private hospitals in Sri Lanka. Health Policy Plan. 2015;30(Suppl 1):i46–58. doi: 10.1093/heapol/czu062. [DOI] [PubMed] [Google Scholar]
- 27.Rannan-Eliya RP, Wijemanne N, Liyanage IK, et al. The quality of outpatient primary care in public and private sectors in Sri Lanka--how well do patient perceptions match reality and what are the implications? Health Policy Plan. 2015;30(Suppl 1):i59–74. doi: 10.1093/heapol/czu115. [DOI] [PubMed] [Google Scholar]
- 28.Das N, Khan AN, Badini ZA, Baloch H, Parkash J. Prescribing practices of consultants at Karachi, Pakistan. J Pak Med Assoc. 2001;51:74–7. [PubMed] [Google Scholar]
- 29.Bangladesh Bureau of Statistics. Report of the Household Income & Expenditure Survey 2010. 2011 http://catalog.ihsn.org/index.php/catalog/2257/download/36931.
- 30.Adams AM, Islam R, Ahmed T. Who serves the urban poor? A geospatial and descriptive analysis of health services in slum settlements in Dhaka, Bangladesh. Health Policy Plan. 2015;30(Suppl 1):i32–45. doi: 10.1093/heapol/czu094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhojani U, Thriveni B, Devadasan R, et al. Out-of-pocket healthcare payments on chronic conditions impoverish urban poor in Bangalore, India. BMC PublicHealth. 2012;12:990. doi: 10.1186/1471-2458-12-990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pakistan Bureau of Statistics, Government of Pakistan. Pakistan National Health Accounts 201314. 2016 http://www.pbs.gov.pk/sites/default/files/NHA%20report%202013-14….pdf.
- 33.Mullen P, Nair D, Nigam J, Seth K. Discussion paper on urban health advantages and penalties in India. Overview and case studies. World Bank Group; 2016. [Google Scholar]
- 34.World Health Organization, International Bank for Reconstruction and Development/The World Bank. Tracking universal health coverage: 2017 global monitoring report. WHO; 2017. http://apps.who.int/iris/bitstream/handle/10665/259817/9789241513555-eng.pdf;jsessionid=6B2D1FA2AACCAB438E87A3B84F774C75?sequence=1. [Google Scholar]
- 35.World Health Organization. Our cities, our health, our future: acting on social determinants for health equity in urban settings. WHO Centre for Health Development; 2008. http://www.who.int/social_determinants/resources/knus_final_report_052008.pdf. [Google Scholar]
- 36.Nambiar D, Muralidharan A, editors. The social determinants of health in India: concepts, processes, indicators. Springer; 2017. [DOI] [Google Scholar]
- 37.Nishtar S, Ralston J. Can human resources for health in the context of noncommunicable disease control be a lever for health system changes? Bull World Health Organ. 2013;91:895–6. doi: 10.2471/BLT.13.118711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kumar S, Kumar S, Gupta B. Urban health: needs urgent attention. Indian J Public Health. 2018;62:214–7. doi: 10.4103/ijph.IJPH_90_18. [DOI] [PubMed] [Google Scholar]
- 39.Govindraj R, Dhushyanth R, Secci F, Choudhury S, Frere J. Health and nutrition in urban Bangladesh: social determinants and health sector governance Directions in development—human development. World Bank Group; 2018. https://openknowledge.worldbank.org/handle/10986/29091. [Google Scholar]
- 40.Pradhan NA, Ali TS, Hasnani FB, Bhamani SS, Karmaliani R. Measuring socio-economic status of an urban squatter settlement in Pakistan using WAMI Index. J Pak Med Assoc. 2018;68:709–14. [PubMed] [Google Scholar]
- 41.BRAC James P Grant School of Public Health, BRAC University and Japan International Cooperation Agency. Baseline survey of strengthening health systems through organizing communities (SHASTO) BRAC University; 2018. [Google Scholar]
- 42.Amann M, Purohit P, Bhanarkar AD, et al. Managing future air quality in megacities: a case study for Delhi. Atmos Environ. 2017;161:99–111. doi: 10.1016/j.atmosenv.2017.04.041. [DOI] [Google Scholar]
- 43.Gurjar BR, Jain A, Sharma A, et al. Human health risks in megacities due to air pollution. Atmos Environ. 2010;44:4606–13. doi: 10.1016/j.atmosenv.2010.08.011. [DOI] [Google Scholar]
- 44.Wendell Cox Consultancy. Demographia: world urban areas 14th annual edition: 201804. 2018 http://www.demographia.com/db-worldua.pdf.
- 45.Nambiar D, Razzak J, Afsana K, et al. Mental illness and injuries: emerging health challenges of urbanisation in South Asia. BMJ. 2017;357:j1126. doi: 10.1136/bmj.j1126. [DOI] [PubMed] [Google Scholar]
- 46.Thomson Reuters Foundation. Most dangerous cities for women. 2017 http://poll2017.trust.org/
- 47.Hussain N, Shelley L. Karachi: organized crime in a key megacity. Connect Q J. 2016;15:5–15. https://it4sec.org/system/files/15.3.01_karachi.pdf. [Google Scholar]
- 48.Galea S, Freudenberg N, Vlahov D. Cities and the health of the public. Vanderbilt University Press; 2006. A framework for the study of urban health; pp. 3–18. https://jhu.pure.elsevier.com/en/publications/a-framework-for-the-study-of-urban-health-3. [Google Scholar]
- 49.World Health Organization Commission on the Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. WHO; 2008. http://www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf. [Google Scholar]
- 50.Prasad A. The Urban Health Equity Assessment and Response Tool (HEART)—a decade of development and implementation. J Urban Health. 2018;95:609–609. doi: 10.1007/s11524-018-0317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sohn EK, Stein LJ, Wolpoff A, et al. Avenues of influence: the relationship between health impact assessment and determinants of health and health equity. J Urban Health. 2018;95:754–64. doi: 10.1007/s11524-018-0263-5. [DOI] [PMC free article] [PubMed] [Google Scholar]