Abstract
Objective
The overall aim of this project was to assess compliance with evidence-based criteria regarding newborn resuscitation among healthcare workers in the maternity units in Maragua District Hospital (a busy district hospital in Kenya).
Introduction
Globally, a majority of deaths under five years are attributable to neonatal causes. Perinatal asphyxia accounts for a significant portion of these deaths, especially in developing countries. These deaths are largely preventable, and interventions geared towards assisting newborns to initiate their first breath within the first minute of life have markedly reduced mortality.
Methods
This implementation project was conducted in the maternity units of a busy district hospital. Evidence-based audit criteria were developed on the basis of an evidence summary developed by the Joanna Briggs Institute (JBI). Using the JBI Practical Application of Clinical Evidence System software (JBI PACES), a baseline audit was conducted including a sample size of 55 healthcare providers and 300 patient case notes followed by an identification of potential barriers and strategies to overcome them. A follow-up audit including a sample size of 55 healthcare providers was conducted by using the same audit criteria.
Results
Improvements in practice were demonstrated in all criteria. The baseline audit demonstrated that three of the five audit criteria were found to be less than 50%, indicating moderate compliance with current evidence with regards to newborn resuscitation. Following implementation of the strategies, which included a six-week education and demonstrative skills training, and updating of the protocols and equipment, there was a significant improvement in all the criteria audited, with the first four criteria achieving 100% compliance, and the fifth criteria achieving 90% compliance.
Conclusion
On completion of the project, the participants demonstrated an increase in knowledge and skills on newborn resuscitation, which led to a significant reduction in admission of newborns with birth asphyxia to the newborn unit.
Keywords: Newborn resuscitation, birth asphyxia, implementation project
Introduction
Globally, in 2013, it was estimated that 6.3 million children aged five years and younger died; 44% of these deaths were attributable to neonatal causes.1 Perinatal asphyxia accounts for a significant portion of these deaths, especially in developing countries.2 The majority of the babies born with perinatal asphyxia face long-term neurodevelopmental disability.3 Preventing and reducing newborn deaths is now a global focus, and to address this, an action plan to end preventable deaths was launched in 2014.4 It seeks to reduce neonatal mortality rates to less than 10 deaths per 1,000 live births in all countries by 2035.1,4 The Kenyan context mirrors the global trend – while there has been an overall reduction in childhood mortality trends, neonatal mortality has shown a much slower rate of decline with an estimated 22 deaths per 1000 live births.5 For Kenya, to achieve the aforementioned Every Newborn Action Plan goal, much needs to be done.4
Deaths due to perinatal asphyxia are largely preventable, and interventions geared towards assisting newborns to initiate their first breath within the first minute of life have markedly reduced mortality.6 Timely and correct resuscitation after birth saves many lives especially in developing countries where neonatal mortality remains unacceptably high.7 The majority of the newborns require simple resuscitation techniques, like warmth, proper positioning, and/or simple stimulation to initiate breathing,6 while up to 3-6% of newborns require bag-and-mask ventilation to help them breathe.7, 8 The importance of newborn resuscitation cannot be overstated. This is a proven highly effective intervention that can save many lives in developing countries.
In many developing countries, it has been noted that newborn resuscitation skills are available in theory but not in practice. Lack of functional equipment and poor preparation for resuscitation of a newborn baby have been cited as a barrier to achieving effective newborn resuscitation in Kenyan hospitals.9 Provision of effective newborn resuscitation is dependent on a skilled health provider, however, it has also been noted that some of these lacked the skills or used outdated practices. Other factors contribute towards this too: failure to recognize high risk deliveries and late referrals. The World health Organization (WHO) defines asphyxia as ‘the failure to initiate and sustain breathing at birth’,10)p.15) and based on this, they saw the need for clinical guidelines to address this gap that are suitable for resource-limited settings.10 The Kenya Paediatric Association (KPA) has adapted these guidelines and incorporated them into a five-day course, Emergency Triage Assessment and Treatment (ETAT), that equips health providers with the necessary skills for easy identification and management of childhood illness.11 This training has been incorporated into undergraduate training programs, and offered as a refresher course to health providers around the country.
Our intention was to conduct a baseline audit on healthcare provider competencies in newborn resuscitation, and thereafter conduct training on the same. On completion of this audit, the feedback was shared with the relevant hospital teams at the hospital and county, and hopefully inform practice. This audit was conducted in Maragua District Hospital, a rural internship centre and level IV hospital in Murang’a County. It is located 89km from the capital, Nairobi. It is a busy hospital with pediatric and newborn units, and the estimated average deliveries per month are 350. The labour room has three cubicles where deliveries are conducted, and is in close proximity to the newborn unit. There are two functional resuscitaires, one each in the delivery room and maternity theater. The newborn unit has an average of 40 admissions in a month, and has been functional for slightly over a year and is supervised by one pediatrician. We cater to sick neonates from not only our maternity unit, but also nearby health centers and dispensaries which refer babies to us. The common causes of admissions are neonatal sepsis, perinatal asphyxia, prematurity and low birth weight, and related complications. In its first year of existence, we noted with concern an increase in admissions and deaths in neonates with severe perinatal asphyxia. This was of great concern because of its neurological implications on these children’s future and potential. Growing evidence conducted on the same has demonstrated a link between delay in delivery, poor or lack of proper newborn resuscitation and equipment, lack of attendance by a skilled health provider and severe perinatal asphyxia. The pediatrician and obstetrician work closely with a team of nurses, medical officers, clinical officers and interns. Currently, we conduct newborn resuscitation sessions, based on the WHO ETAT+ course, to the interns and the midwives on a regular basis. Together with the maternity team, we concentrate our efforts on making sure that every woman in labor is monitored and decisions on the delivery mode are acted on in good time. This is an ongoing process and while it has not been executed as planned – due to various reasons like staff shortages – we still continue to admit neonates with severe perinatal asphyxia and fresh still births. Recently, we acquired two resuscitaires, which we believe will help with resuscitation efforts. We seek to improve the outcome of every single delivery to ensure that every mother goes home with a live healthy infant. Secondly, being a relatively ‘new’ newborn unit, we hope to initiate best practice and build on the momentum going forward.
Best practice recommendations
The following best practice recommendations are derived from evidence-based international guidelines:12
Standardized formal neonatal resuscitation training (such as the Helping Babies Breathe program) for all health workers attending to births in order to decrease the variation in neonatal resuscitation practices.
Availability of functional equipment and supplies for basic newborn resuscitation in the maternity unit.
Availability of an evidence-based newborn resuscitation protocol in the maternity unit.
All newborns are assessed accurately and assigned an APGAR (Appearance, Pulse, Grimace, Activity and Respiration) score. If newborns do not breathe spontaneously after thorough drying and additional stimulation, then positive-pressure ventilation should be initiated within one minute.
Aims and objectives
The overall aim of this project was to assess compliance with evidence-based criteria regarding newborn resuscitation amongst health care providers in the labor ward and maternity theater in Maragua District Hospital in Kenya. These units are run by 35 nurses (who work on a rotational basis in the labor ward, maternity theater, and postnatal and newborn units), three clinical officer anesthetists, five permanent medical officers, and medical and clinical officer interns (who are attached to the units for a period of three months during their internship). Their work is overseen and supervised by a midwife in charge, the obstetrician and the pediatrician. Specifically, the aims were:
To identify and engage a multidisciplinary team to promote evidence-based practice in newborn health outcomes and assess compliance with best practice in newborn resuscitation using a baseline audit and an audit tool developed by JBI.
To reflect on the results from the baseline audit, and design and implement strategies to address areas of non-compliance with best practice in newborn resuscitation.
To improve knowledge regarding best practice in newborn resuscitation amongst health providers in the newborn, postnatal and maternity units.
To undertake a follow-up audit, assess the extent and nature of increased compliance with evidence-based best practice, and identify areas and strategies to sustain and enhance care in delivery of newborn resuscitation to newborns in the maternity units at Maragua Distrrict hospital.
To improve outcomes regarding neonatal admissions and deaths due to asphyxia in Maragua District Hospital.
Methods
The implementation project was conducted in the labor ward and maternity theater in a busy district hospital. In this project, a retrospective baseline audit was conducted by reviewing patients’ medical charts from the month of May 2016 and administering questionnaires to the healthcare providers during the month of August 2016. The healthcare providers working in the relevant units (labor ward, maternity theater, postnatal and newborn units) were all eligible for the audit. A baseline and follow-up questionnaire (Appendix I) was administered to the healthcare providers in August and October 2016, respectively. This helped us understand their training competencies with regards to newborn resuscitation. The training and education was conducted over a six-week period from the last week of August 2016 (see Appendix VI for training materials). Data on different audit criteria was obtained from the patient case notes for both the baseline and follow-up audits.
Evidence-based audit criteria were developed based on an evidence summary developed by JBI.12
This evidence implementation project used the JBI PACES and Getting Research into Practice (GRiP) audit and feedback tool. The JBI PACES and GRiP framework for promoting evidence-based health care involves three phases of activity:
Establishing a team for the project and undertaking a baseline audit based on criteria informed by the evidence. The first phase of the project involved identifying relevant team participants for the project and engaging them. The project team consisted of the pediatrician, matron in charge of the nursing officers, and midwife in charge of nurses in the maternity unit, medical officer in paediatrics ward, and a data clerk. The paediatrician and the matron in charge oversaw the project audit and implementation, while the midwife in charge of the maternity unit worked together with the paediatrician to convene her staff for trainings. The data clerk was responsible for collecting the data in real time.
Reflecting on the results of the baseline audit and designing and implementing strategies to address non-compliance found in the baseline audit informed by the JBI GRiP framework.
Conducting a follow up audit to assess the outcomes of the interventions implemented to improve practice, and identify future practice issues to be addressed in subsequent audits.
Phase 1: Team establishment and baseline audit
Before commencing the project, the core team agreed on the trainers (paediatrician, medical officer and a midwife), and the members responsible for the data collection. Later on this comprised of a paediatrician from the Kenya Medical Research Institute, and a Nursing Officer from the Kenya Paediatric Association. They helped with formulation of data collection tools and ensuring the health care providers’ competencies were satisfactory. We held three meetings in total and education was provided to ensure the competencies were maintained, and also to minimize any errors that may occur during data entry. Using Joanna Briggs Institute Practical Application of Clinical Evidence System software (JBI PACES), a baseline audit of 55 healthcare providers was completed by the audit team. The 55 healthcare providers included 30 nursing officers, five medical officers, three clinical officer anesthetists, and four clinical officers from the reproductive health department, four medical officer interns and nine clinical officer interns. They were given a questionnaire with questions to help identify their training competencies on audit criteria 1 (refer to the audit criteria below). A baseline audit of functional equipment and supplies for basic newborn resuscitation in the labor ward and maternity theaters was done (refer to audit criteria 2 and 3). Additionally, a baseline audit on patients case notes was completed by the project team (refer to audit criteria 4 and 5).
The audit criteria for this project were based on an evidence summary developed by JBI.12 The evidence summary is based on a structured search of the literature and selected evidence-based healthcare databases.
Audit criteria
Healthcare providers attending to deliveries have received training and maintain competencies in relation to newborn resuscitation.
Availability of functional equipment and supplies for basic newborn resuscitation in the labor ward and maternity theater.
Availability of an evidence-based protocol in the labor ward and maternity theater.
All newborns are assessed accurately and assigned an APGAR score.
All newborns with birth asphyxia are correctly assessed and managed according to the WHO guidelines.
The project was registered as a quality improvement activity within the hospital, and therefore did not require ethical approval.
Table 1 below shows the evidence informed audit criteria used in the project (baseline and follow-up audit) together with a description of the sample and approach to measuring compliance with best practice for each audit criterion.
Table 1. Audit criteria and audit guide.
ETAT+: Emergency Triage Assessment and Treatment; TEO: tetracycline eye ointment; APGAR score: Appearance, Pulse,
| Audit criterion | Audit guide | Sample | Method used to measure % compliance with best practice |
|---|---|---|---|
| 1. Healthcare providers attending to deliveries have received training and maintain competencies in relation to newborn resuscitation | The auditor administered a questionnaire to find out if the healthcare providers had been trained in basic newborn resuscitation, using the national ETAT+ guidelines. Auditor marked as ‘Yes’ for trained and ‘No’ for no training | 55 healthcare providers | A questionnaire to healthcare providers (refer to Appendix I) Certification provided on completion |
| 2. Availability of functional equipment and supplies for basic newborn resuscitation in the labor ward and maternity theater | The auditor used a simple tool to check availability of equipment in the maternity theater and labor ward, and marked as ‘not available’, ‘partially available’ or ‘available’. | Warming device for room or resuscitaire Two warm dry towels Hand washing facilities or hand sanitizer Bag-valve mask Suction machine and catheters TEO available for eye prophylaxis Cord clamps Resuscitation starts within one minute of birth if needed Chlorhexidine available for cord care Baby placed skin to skin with mother | All supplies present in the resuscitation tray – ‘Yes’. Equipment partially or not available in the resuscitation tray – ‘No’. Refer to Appendix II |
| 3. Availability of evidence-based newborn resuscitation protocols in the labor ward and maternity theater | Audit team marked as: ‘Yes’ if available ‘No’ if unavailable or not updated |
A current evidence-based protocol | Presence of printed protocol in the 2 rooms (maternity theater and labor ward). Refer to Appendix V |
| 4. All newborns are assessed correctly and assigned an APGAR score | Audit team looked at the patient case notes and marked as: ‘Yes’ if APGAR score documented ‘No’ if empty | Baseline – conducted retrospectively on 300 case notes (from mothers) from May 2016 Follow-up – October 2016 |
Refer to Appendix III for audit tool |
| 5. All newborns with perinatal asphyxia are correctly assessed and managed according to the WHO guidelines | Audit team looked at the patient case notes and marked as: ‘Yes’ if APGAR score was documented and the resuscitation efforts documented. ‘No’ if resuscitation efforts not documented |
Baseline - 15 case notes of newborns in May 2016 Follow-up – October 2016 | Refer to Appendix IV for audit tool |
Grimace, Activity and Respiration; WHO: World Health Organization
Phase 2: Design and implementation of strategies to improve practice (GRiP) (level 2 heading)
The baseline audit results were assessed by the project team and the GRiP tool was used to identify the barriers and develop strategies to overcome the barriers. The results of GRiP are shown in Table 2.
Table 2. Getting Research into Practice matrix.
| Barrier | Strategy | Resources | Outcomes |
|---|---|---|---|
| Some of the healthcare providers were resistant to change e.g. For example, more experienced midwives insisting on outdated practices |
|
|
Surpassed expectations as the team embraced the skills taught and became familiar with best practice. |
| Lack of incentives Most health providers attend meetings and trainings if there is an incentive or motivation attached to it e.g. money, food or certification |
|
|
Increased attendance. |
| Poor collaboration among the maternity nurses, and between the maternity and paediatric units |
|
|
Staff collaboration improved. |
| Knowledge gaps amongst healthcare providers |
|
|
Staff became more familiar with current best practice in newborn resuscitation. Staff encouraged when they know their input is appreciated. |
Time constraints to provide education and training
|
|
|
Increased education and training. |
| Sustainability of the project The excitement of the project tends to wear down with the conclusion of a project | Identifying champions to ensure that best practice continues, even after the conclusion of this current audit cycle. | We intend to conduct a follow-up audit in 6 months’ time (April 2016) |
ETAT+: Emergency Triage Assessment and Treatment
All team members held discussions to identify potential barriers and came up with potential strategies to address these barriers.
Phase 3: Follow-up audit post implementation of change strategy (level 2 heading)
The follow-up audit was conducted by the project team members following the GRiP phase. The data was collected by using the same audit criteria as in the baseline audit. The follow-up data collection started in October 2016.
Results
Phase 1: Baseline audit
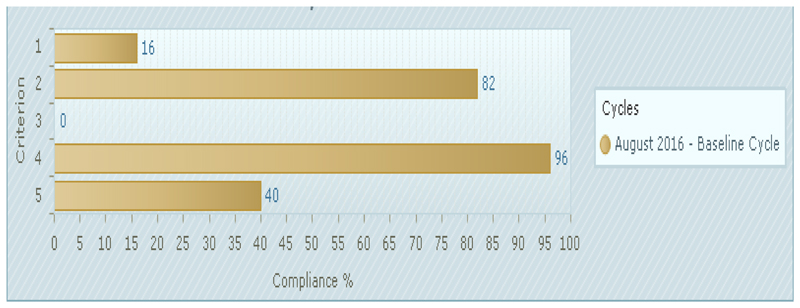
The baseline audit was conducted in August 2016, and the results from the baseline audit are as shown in Figure 1.
Figure 1. Baseline compliance with best practice for audit criteria (%).
- Healthcare workers attending to deliveries have received training and maintain competencies in relation to newborn resuscitation (55 of 55 samples taken)
- Availability of functional equipment and supplies for basic newborn resuscitation in the maternity theater and labor ward (11 of 11 samples taken)
- Availability of an evidence-based newborn resuscitation protocol in the maternity theater and labor ward (1 of 1 samples taken)
- All newborns are assessed accurately and assigned an APGAR score (300 of 300 samples taken)
- All newborns with birth asphyxia are managed according to the WHO guidelines (15 of 15 samples taken)
As can be seen from Figure 1, three of the five audit criteria scored less than 50%, indicating poor compliance with current evidence. The compliance for criterion 1 (healthcare workers attending to deliveries have received training and maintain competencies in relation to newborn resuscitation) was 16% (with nine out of 55 healthcare providers having prior education on basic newborn resuscitation from ETAT training or other newborn care courses). Most of these healthcare providers received this education more than three years ago. Of the 55 healthcare providers assessed, a majority (54.5%) were nurses. The compliance for criterion 2 (availability of functional equipment and supplies for basic newborn resuscitation in the maternity theater and labor ward) was 82% for both the labor ward and maternity theater. While most of the equipment was available, we faced challenges such as: incorrect size of masks, the equipment not easily accessible during resuscitation, and unavailability of chlorhexidine for cord care. Criterion 3 was the worst performing, with zero compliance: the newborn protocols in both the maternity theater and labor ward were not updated. Criteria 4 (all newborns are assessed accurately and assigned an APGAR score) and 5 (all newborns with birth asphyxia are managed according to the WHO guidelines) reported compliance of 96% and 40%, respectively. While these results were encouraging, it is worth noting that documentation seems to be major problem (since even in some cases time of delivery was missing in the case notes of newborns), due to reasons cited, such as increased workload, task shifting or, at times, expecting someone else to do the task. The staff agreed that results from the last two audit criteria might not be reflecting the true picture on the ground.
Phase 2: Strategies for Getting Research into Practice (GRiP)
The main barriers identified were resistance to change, lack of incentives, poor collaboration and knowledge gaps amongst the healthcare providers, time constraints to provide education and training, and sustainability of the project. Some of the strategies that were employed to address these barriers were: identifying dedicated healthcare providers to champion this cause, provision of snacks and certificates during the training to boost attendance, holding continuous medical education and demonstrative skills stations, enhancing teamwork through joint meetings, and appreciating and reinforcing positive change. All this was possible with resources provided for by the hospital administration and certification by KPA. The main barriers, strategies, resources and outcomes are presented in Table 2.
Phase 3: Follow-up audit
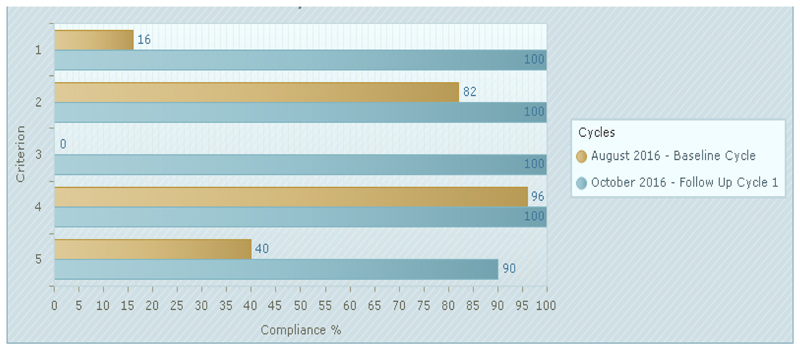
The rates of compliance with best practice for the audit criteria in the baseline and follow-up audits are shown in Figure 2. Compared to the baseline, there was significant improvement in all criteria audited in the follow-up audit. All criteria, except for one, achieved 100% compliance. The most improved was criterion 3, with 100% improvement, and 1, with 84% improvement. Based on the results of mean knowledge scores for the newborn resuscitation (pre-test and post-test) for healthcare providers in the Maragua District Hospital, overall knowledge increased significantly following the intervention. Also worth noting was that, for criterion 5 (all newborns with birth asphyxia are managed according to the WHO guidelines), the mortality rate among the newborns who were resuscitated in the pre-intervention period was 50%, while there was no death that occurred in the group of newborns who were resuscitated in the period after the intervention. The baseline and follow-up audit results are compared in Table 3.
Figure 2. Compliance with best practice audit criteria in follow-up audit compared to baseline audit (%).
- Healthcare workers attending to deliveries received training and maintain competencies in relation to newborn resuscitation. (55 of 55 samples taken)
- Availability of functional equipment and supplies for basic newborn resuscitation in the maternity theater and labor wards. (11 of 11 samples taken)
- Availability of an evidence-based resuscitation protocol in the maternity theater and labor ward. (1 of 1 samples taken)
- All newborns are assessed accurately and assigned an APGAR score. (300 of 300 samples taken)
- All newborns with birth asphyxia are managed according to the WHO guidelines. (10 of 10 samples taken)
Table 3. Baseline and post audit results.
| Baseline audit | Follow up audit | |||||||
|---|---|---|---|---|---|---|---|---|
| Audit criteria | Y | N | N/A | %Y | Y | N | N/A | %Y |
| 1. Healthcare workers attending to deliveries have received training and maintain competencies in relation to newborn resuscitation | 9 | 46 | 0 | 16% | 55 | 0 | 0 | 100% |
| 2. Availability of functional equipment and supplies for basic newborn resuscitation in the labor ward and maternity theater | 9 | 2 | 0 | 82% | 11 | 0 | 0 | 100% |
| 3. Availability of an evidence-based newborn resuscitation protocol in the labor ward and maternity theater | 0 | 2 | 0 | 0% | 2 | 0 | 0 | 100% |
| 4. All newborns are assessed accurately and assigned an APGAR score | 287 | 13 | 0 | 96% | 300 | 0 | 0 | 100% |
| 5. All newborns with perinatal asphyxia are correctly assessed and managed according to the WHO guidelines | 6 | 9 | 0 | 40% | 9 | 1 | 0 | 90% |
Y: Yes; N: No; N/A: not applicable; APGAR score: Appearance, Pulse, Grimace, Activity, Respirations; WHO: World Health Organization
Discussion
In this implementation project, we looked at current practice in relation to basic newborn resuscitation in a hospital setting with limited resources. This was accomplished by administering a questionnaire to all healthcare providers involved in newborn care in the relevant departments, reviewing structures and documentation using an audit, intervention and post-implementation audit cycle based on evidence-based practice. Baseline data was gathered, and thereafter, barriers, actions and resources were identified using the JBI PACES and GRiP tools.
This project was successful in improving awareness, knowledge and skills on basic newborn resuscitation to health care providers. Most of these healthcare providers received this education more than three years ago, and whilst others still practiced outdated practices. We successfully trained all the healthcare providers attending to deliveries in basic newborn resuscitation. This was achieved over a six-week period with minimal resources. The standard ETAT course is a five-day course that involves significant resources and currently may not be feasible. This audit therefore demonstrated that one can still transfer knowledge and skills to a larger audience without necessarily using considerable resources. The healthcare providers are also motivated and more confident striving to ensure that every mother goes home with a healthy baby. Additionally, this project has boosted team work amongst the healthcare providers. The reason why we trained all the nurses, even in the newborn and postnatal units, was due to the fact that they are rotated across different departments. They also work closely together and can be called upon any time to assist in the event of staffing shortages. This is a basic skill integral in any nursing officer’s career. Additionally, for the other healthcare providers – clinical officer anesthetists, medical officers and clinical officers in reproductive health – this skill remains a major part of their training. The project has improved the quality of equipment in our facility as the audit was able to highlight the availability or absence of some of this equipment. For example, before the audit, the bag-valve-mask devices were in short supply or ill-fitting; however, following the audit, we now have the correct sizes. Prior to the audit, the resuscitation equipment was not easily accessible during resuscitation. Following the audit, this was corrected – the resuscitation tray with the right equipment is checked before each shift by a nursing officer and is within reach in both the labor ward and maternity theater. The protocols for newborns in both the maternity theater and labor ward were updated. Although it may be too soon to know the impact this audit has on the newborns’ lives, we have already seen a reduction in newborn admissions and deaths of newborns with birth asphyxia.
The main limitation of the project was time constraints. Most of our staff work on a shift basis, and some were on leave during this audit. We had to develop innovative ways to capture all the staff in this training. This was achieved by providing the training during their work hours (when they were less busy), or during changeover shifts. We had to ensure that none of our exercises interfered with the daily routine of the hospital services. Another limitation of this project, due to the limited time period of this project, was the inability to conduct an observation to ensure that the APGAR score assigned to a newborn was indeed the correct one. Due to the limited time period of this project, a future audit to explore this limitation would be worthwhile to inform practice. In connection to this, although most newborns were assigned an APGAR score, there were some instances where the auditor noted that these were not available. During the general feedback sessions, the staff in the maternity units noted that all newborns were in fact assigned an APGAR score, and the omissions were probably due to the increased workload. We hope to share the audit findings with the relevant departments to ensure that staffing challenges are adequately addressed.
Future directions for promoting best practice include: conducting a follow-up audit after six months, and providing training to all newly joined medical staff on basic newborn resuscitation and any others who were on leave when this audit was carried out. We were able to share our results in other meetings, for example, at the annual Kenya Paediatric Association in April 2017, so as to disseminate this information and hopefully, encourage clinicians in similar settings to follow our example. Since we receive referrals from the dispensaries and nearby health centers, we plan to train this basic skill to all healthcare providers in these hospitals and health centers who attend to deliveries. We are also looking forward to carrying out other implementation projects in the near future, but on different topics in relation to other conditions affecting children under five years.
The results of project were shared with different stakeholders at the hospital; however, we plan to hold a county meeting to share the same.
Conclusion
In conclusion, the aims and objectives of the project were realized. At the end of the project, all staff in the maternity units, with the exception of those on leave, received training on basic newborn resuscitation. There was also a significant reduction in admission of newborns with birth asphyxia to the newborn unit. Additionally, we were able to update the units with evidence-based newborn resuscitation protocols, and other equipment pertinent to newborn resuscitation. This project has demonstrated that ongoing education on basic newborn resuscitation can create awareness and prevent admissions and deaths of newborns with birth asphyxia. The project was successful in increasing knowledge in this area and providing future directions for sustaining evidence-based practice change. Future plans and ideas are in place and have been discussed. Further audits will need to be carried out in order to maintain the practice change and ensure that new practices are supported and maintained.
Supplementary Material
Acknowledgements
The author would like to thank the JBI Clinical Fellowship Program for the training and invaluable support provided throughout the entire course. A special thank you to the Joanna Briggs Foundation for their sponsorship of my clinical fellowship.
Footnotes
Conflict of Interest
There is no conflict of interest in this project.
References
- 1.Levels and trends in child mortality – report 2013. Estimates Developed by the UN Inter- agency Group for Child Mortality Estimation. New York: UNICEF; 2013. [Google Scholar]
- 2.Lawn JE, Cousens S, Zupan J. Neonatal Survival Steering 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 3.Shibuya K, Murray C. Birth Asphyxia. In: Murray C, Lopez A, editors. The Global Burden of Disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press; 1996. pp. 429–453. [Google Scholar]
- 4.Every newborn: an action plan to end preventable deaths [Internet] Geneva: World Health Organization; 2014. [cited 2014 Mar 30]. [internet]. Available from: http://www.everynewborn.org. [Google Scholar]
- 5.Kenya National Bureau of Statistics, Ministry of Health/Kenya. National AIDS Control Council/Kenya, Kenya Medical Research Institute, and National Council for Population and Development/Kenya. [cited 2014 Mar 30];Kenya Demographic Health Survey. 2014 [internet]. Available from: https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf. [Google Scholar]
- 6.Lee AC, Cousens S, Wall SN, Niermeyer S, Darmstadt GL, Carlo WA, et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: a systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Pub Health. 2011;11((Suppl. 3)) doi: 10.1186/1471-2458-11-S3-S12. S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375(9730) doi: 10.1016/S0140-6736(10)60549-1. 1969e87. [DOI] [PubMed] [Google Scholar]
- 8.Gülmezoglu AM, Lawrie TA. Impact of training on emergency resuscitation skills: Impact on Millennium Development Goals (MDGs) 4 and 5 Original Research Article. Best Pract Res Clin Obstet Gynaecol. 2015;29(8):1119–1125. doi: 10.1016/j.bpobgyn.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 9.English M, Ntoburi S, Wagai J, Mbindyo P, Opiyo N, Ayieko P, et al. An intervention to improve paediatric and newborn care in Kenyan district hospitals: understanding the context. Implement Sci. 2009;4:42. doi: 10.1186/1748-5908-4-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Guidelines on Basic Newborn Resuscitation. WHO Press; 2012. [PubMed] [Google Scholar]
- 11.World Health Organization. Updated guideline: Paediatric emergency triage, assessment and treatment. [cited 2014 Mar 30];Care of critically ill children. 2016 [internet]. Available from: http://apps.who.int/iris/bitstream/handle/10665/204463/9789241510219_eng.pdf;jsessionid=EAA53566E0B626ABE0576D6790E17323?sequence=1. [PubMed] [Google Scholar]
- 12.McArthur A. Evidence summary. Neonatal Resuscitation: Perinatal asphyxia. Joanna Briggs EBP Database, JBI@Ovid. 2016 JBI15818. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.