Abstract
Background
Stigma is a barrier for help-seeking, mental health service access, and contributes to the mental health treatment gap. Because the mental health treatment gap is greatest in low- and middle-income countries, it is vital to identify effective strategies to reduce stigma in these settings. To date, there has been a lack of synthesis of findings from interventions to reduce stigma related to mental disorders within India.
Method
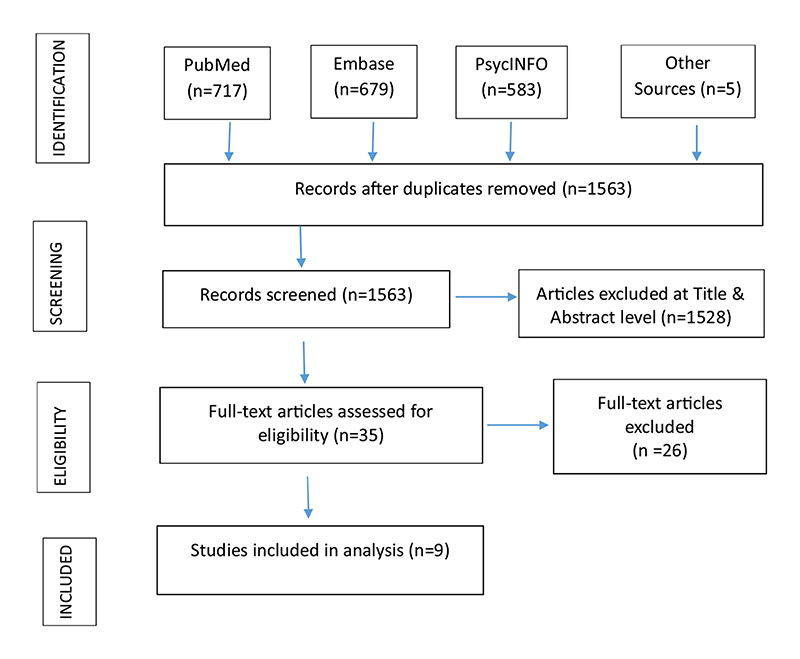
A systematic review was conducted to provide an overview of the characteristics and effectiveness of stigma reduction interventions studies in India. PubMed, Embase and PsycINFO databases were searched for literature published up to 30th June 2020.
Results
From a total of 1,984 articles identified, only 9 were eligible for final inclusion, published between 1990-2020. No study was found from North, North-East, Central or East India. Most stigma-reduction interventions were multi-level, that is, using a combination of intra-personal, inter-personal and community level strategies to target changes in outcomes of individuals, environments and community groups. Three studies focused on health and stigma-related changes at the organisational/institutional level. No interventions focused on the governmental/structural level. There were only two randomised controlled trials, and two studies focused on all three stigma components of knowledge, attitudes and behaviour. Most interventions were delivered to community members. None focused on mental health professionals as intervention delivery target.
Conclusion
There is a need for the development of comprehensive, culturally acceptable evidence-based interventions that act at multiple levels, and involve a mixture of various stigma reducing strategies with multiple target groups.
Keywords: Stigma, Culture, Mental disorders, Interventions, Review, India
1. Introduction
There is a large treatment gap for mental disorders in low- and middle-income countries (Semrau et al., 2015; Thornicroft et al., 2017), estimated to be about 95% within India (Sagar et al., 2017). Studies suggest barriers such as limited or absent mental health services, scar-city of trained mental health professionals, and stigma related to help-seeking for mental disorders contribute to this large treatment gap for mental disorders in India (Böge et al., 2018; Maulik, Devarapalli et al., 2017; Maulik, Kallakuri et al., 2017; Maulik et al., 2019; Shidhaye et al., 2016; Tewari et al., 2017).
Stigma can be understood as a problem of knowledge (ignorance), attitudes (prejudice) and behaviour (discrimination) (Thornicroft et al., 2007). Stigma associated with mental disorders is largely responsible for people with mental illness not receiving adequate mental health treatment and care (Tewari et al., 2017; Venkatesh et al., 2015). Stigma is a global phenomenon, but specific experiences of stigma and discrimination are local and greatly influenced by cultural factors (Gautam & Jain, 2010; Murthy, 2002; Stuart, 2016).
Patterns of help-seeking are influenced by local patient perspectives of common mental disorders (Sagar et al., 2017; Shankar et al., 2006), and the presentation of symptoms varies in different cultures (Gautam & Kapur, 1977). There seems to be a coexistence of high levels of perceived stigma and supernatural attributions of mental disorders in India (Thirthalli & Kumar 2012). Understanding local perspectives (cultural practices, beliefs and behaviours) can influence and help establish a culturally sensitive healthcare system for the community (Joel et al., 2006). There is a need to understand available culturally relevant interventions and their effectiveness in reducing stigma related to mental disorders in India. The aim of this paper was to conduct a systematic review to provide an overview of the characteristics and effectiveness of stigma-reduction interventions studies conducted in India.
2. Method
We conducted this narrative systematic review in accordance with Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines (Moher et al., 2009). We used the levels of stigma-reduction strategies and interventions outlined by Heijinders and Meij (2006), which differentiates between the following five levels: intrapersonal, interpersonal, organisational/institutional, community and governmental/structural level. Intra-personal level focuses on individual behaviour change by using strategies such as, treatment, counselling, psychotherapy, empowerment, group counselling, self-help, advocacy and support groups. The inter-personal level aims at modifying affected person’s environment which includes strategies like care and support, home care teams, and community-based rehabilitation. The organisational/institutional level targets the health and stigma related aspects of an organisation by using training programmes, (new) policies like patient centred and integrated approaches. The community level aims to inform the general public and specific community groups using approaches such as education, contact, advocacy, and protest. The governmental/structural level (legal and policy, rights-based approaches) aims to enforce the protection of rights of people affected with a stigmatising illness.
2.1. Search Strategy
Three electronic databases - PubMed, Embase and PsycINFO - were searched to identify interventions published up to 30th June 2020. We searched papers with the terms “stigma”, “mental health”, “mental disorder” and “India” using Boolean operators (AND/OR), in either title or abstract. The terms “intervention”, “anti-stigma”, “trainings”, or “community programs” were deliberately not used, to reduce the chances of missing out on any model or program which may not have used the terms. An example is provided in Appendix A. Additional articles were obtained by searching primary papers listed in the references of the reviews and by hand searching.
2.2. Inclusion and Exclusion Criteria
Broad inclusion criteria were used as we expected to find limited research in the area of stigma-reduction interventions conducted in India. There were no restrictions on types of mental disorders or types of participants. The inclusion criteria for articles were: (1) published prior to initiation of search on June 30, 2020; (2) contained original research involving primary data collection; (3) examined stigma or stigma-related concepts as an outcome; (4) participants ≥ 18 years of age; (5) all types of stigma-related interventions in the field of mental health.
We excluded studies that were: (1) case studies, exploratory, descriptive or purely qualitative studies, and protocol papers, (2) systematic reviews, secondary data analysis and meta-analysis, (3) grey literature with unpublished and unindexed articles/documents or reports, (4) pharmacotherapy trials, and (5) papers published in languages other than English.
2.3. Study Selection
Endnote X9 (©Clarivate Analytics) was used to upload and organise articles for title and abstract review. The title, abstract review and subsequent full text article review of the studies were assessed independently by two investigators (AK and SK). After each stage, if at least one reviewer deemed the abstract relevant, the full text was reviewed. Discrepancies were discussed between AK and SK, and inclusion of an article was finally decided by mutual agreement.
2.4. Data Extraction and Synthesis
The two investigators (AK and SK) read each article in detail and extracted information as per inclusion and exclusion criteria. They independently extracted information from each article, discussed them in case of any discrepancy, and summarised details into categories. In case of any unresolved decision, the studies were discussed with PKM who acted as the adjudicator. The final information were grouped under author/year of publication, intervention level delivered, intervention strategies, component of stigma targeted, intervention target group, aims/purpose, study design, target sample and sample size, study setting and region, mental health condition/domain under study, intervention type and details, outcomes, key findings, and strengths and limitations. Given the paucity of literature and purpose of our review being descriptive, we included all studies which fulfilled our study criteria irrespective of quality.
3. Results
The database searches generated a total of 1984 records starting from inception till 30th June 2020. Nine studies were eligible for inclusion. The flowchart is depicted in Fig. 1.
Fig. 1. Flow diagram of study selection.
3.1. Brief summaries of the selected studies
Table 1 summarises the characteristics of the studies included in the review and Table 2 depicts the content summaries of the selected studies.
Table 1. Characteristics of included studies.
| Characteristic | N | |
|---|---|---|
| Publication date | 1990-2000 | 1 |
| 2001-2010 | 1 | |
| 2011-2015 | 4 | |
| 2016-2020 | 3 | |
| Regions of India* | South India | 7 |
| West India | 3 | |
| Central India | 0 | |
| North India | 0 | |
| North-East India | 0 | |
| East India | 0 | |
| Level at which intervention was delivered | Intra-personal, Inter-personal and Community | 6 |
| Organisational/Institutional | 3 | |
| Governmental/Structural | 0 | |
| Training Programmes | 3 | |
| Health promotion | 5 | |
| Self-help and support groups | 2 | |
| Community-based rehabilitation | 4 | |
| Home care teams | 1 | |
| Care and Support | 2 | |
| Intervention strategy used* | Counselling | 3 |
| Group Counselling | 1 | |
| Treatment | 5 | |
| Community education | 6 | |
| Community contact | 1 | |
| Cognitive Behaviour Therapy | 0 | |
| Community advocacy | 0 | |
| Legal and policy based | 0 | |
| Rights based approaches | 0 | |
| Component of stigma targeted | Knowledge | 2 |
| Attitudes | 1 | |
| Behaviour | 0 | |
| Internalised stigma and stigma fears | 1 | |
| Knowledge and attitudes | 3 | |
| Knowledge, attitudes and behaviour | 2 | |
| Intervention delivery target group | Community Members | 4 |
| Primary and Community Health Workers | 3 | |
| Patients with schizophrenia and caregivers | 1 | |
| Women living with HIV/AIDS | 1 | |
| Mental health professionals | 0 | |
| Non-mental health professionals working in secondary or tertiary settings | 0 | |
| Study Design | Randomised Control Trials (RCTs) | 2 |
| Pre-and-post, or Cross-sectional | 7 |
Some studies fall into more than 1 category.
Table 2. Content summary of the selected studies.
| S. No | Author(s) & Year of publication | Aims/Purpose | Study Design | Target Sample and sample size | Study Setting and Origin | Mental Health Condition / domains under study | Intervention Type and Details | Outcomes | Key Findings |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Chinnayya et al., 1990 |
|
Pre Post study/Before and after | 150 primary care paramedical health workers (multipurpose workers) who are working at the PHC and are involved in providing mental health care | Mental health unit of NIMHANS (psychiatric and neurological hospital), Bangalore, Karnataka in South India | Attitudes toward mental health care | Each month, a batch of 8 to 10 MPWs are deputed to undergo the training, which is of one week’s duration. The Training consists of lectures, case demonstrations, and role play. The training is facilitated by a manual of mental health developed in-house. | Significant changes in attitudes of paramedical health workers towards different mental health problems. | The results of the present study indicate that the mental health training of paramedical workers has been effective in bringing about a change of attitudes towards mental illness. Attitude change has been uniform for the different disorders. |
| 2. | Joel et al., 2006 | To test the effect of a biomedical intervention on explanatory models (EMs) of community health workers. | Cross-sectional intervention | 80 Community health workers from The Rural Unit for Health and Social Affairs (RUHSA). | RUHSA, a community health programme of the Christian Medical College Hospital, Vellore, South India. The programme operates in all 84 villages in the chosen district. | Chronic Psychosis | The community health workers were divided into two groups depending on the geographical location of their villages and peripheral health centres. Forty workers were taught about the biomedical aspects of schizophrenia. The training programme discussed local beliefs about mental illness, elicited by the SEMI interview. The health workers were encouraged to discuss their beliefs and their implications. The structured teaching programme, of 2 -h duration, then described the symptoms, causes, treatment and referral. The training was given in batches of 6-7 workers. The 40 workers of the control group were not educated during the study period. | Not mentioned. | A variety of indigenous beliefs, which contradicted the biomedical model, were elicited at the baseline evaluation. Seeking biomedical help at follow up was significantly related to receiving education about the biomedical aspects of chronic psychosis (OR 17.2; 95% CI: 18.75, 15.65; p < 0.001). This remained statistically significant (OR 9.7; 95% CI: 82.28, 1.14; p < 0.04) after using logistic regression to adjust for baseline variables |
| 3. | Armstrong et al., 2011 | To provide a mental health training intervention to community health workers and to evaluate the impact of this training on mental health literacy. | Pre test post test | 63 community health workers sourced through Gramina Abrudaya Seva Samstha (GASS), an NGO operating locally. The types of community health workers included Junior Health Assistants, Village Rehabilitation Workers, and ASHA workers. | Community setting in the rural district of Doddaballapur, Bangalore, South India. | Mental Health Literacy (MHL) is defined as ‘knowledge and beliefs about mental disorders which aid their recognition, management and prevention of mental illnesses. | The mental health training program is a four-day course that aims to increase recognition of mental disorders, enhance appropriate response and referral, support people with mental disorders and their families, and improve mental health promotion in communities. | Changes in the participants’ level of MHL, we adapted a MHL at three time points; i. e. baseline, completion of the training and three months follow up. | The training course improved participants’ ability to recognize a mental disorder in a vignette, and reduced participants’ faith in unhelpful and potentially harmful pharmacological interventions. There was evidence of a minor reduction in stigmatizing attitudes, and it was unclear if the training resulted in a change in participants’ faith in recovery following treatment. |
| 4. | Balaji et al., 2012 | To develop a lay health worker delivered community based intervention in three sites in India. | The intervention was designed into three phases with a structured format to suit the design of the RCT. | Participants suffering with schizophrenia and their primary caregivers from 30 families. | Goa, Satara, Kanchipuram in West and South India | Schizophrenia | The intervention comprised of five components (psychoeducation; adherence management; rehabilitation; referral to community agencies; and health promotion) which were delivered by trained lay health workers supervised by specialists. |
|
The intervention underwent a number of changes as a result of formative and pilot work. While all the components were acceptable and most were feasible, experiences of stigma and discrimination were inadequately addressed; some participants feared that delivery of care at home would lead to illness disclosure; some participants and providers did not understand how the intervention related to usual care; some families were unwilling to participate; and there were delivery problems, for example, in meeting the targeted number of sessions. Participants found delivery by health workers acceptable, and expected them to have knowledge about the subject matter. Some had expectations regarding their demographic and personal characteristics, for example, preferring only females or those who are understanding/friendly. |
| 5. | Mindlis et al., 2015 | To evaluate the impact that community interventions in mental health through a grassroots approach had on the knowledge and attitudes towards depression in a non-psychiatric population in rural Gujarat, India. | Cross sectional | 333 community member from 6 villages of Gujarat, Western India (intervention arm = 146 and control arm = 187 | The local study partner was the MINDS Foundation (www.mindsfoundation.org) located in Vadodara, Gujarat. Villages were selected for their accessibility from the SVU campus. | knowledge and attitudes towards depression | Series of interventions:
|
Significant changes in mean scores on knowledge and attitudes towards depression | The intervention villages showed higher levels of literacy regarding depression and lower levels of stigma, after adjusting for all other sociodemographic variables. |
| 6 | Nimgaonkar and Menon (2015) | To identify and manage psychiatric disorders rapidly, comprehensively and sustainably, with an emphasis on task-shifting and community participation. | Cross sectional, mixed methods, Pre-post design | 2759 families comprising of village leaders, other members of the community, medical psychiatric social worker, health animators and health volunteers at a public space in total 184 villages of Tamilnadu as part of ASHWINI program | The study was conducted in the Gudalur and Pandalur Taluks of the Nilgiris District located within the Nilgiri mountain ranges in the state of Tamil Nadu, in South India. The ASHWINI program serves five tribal peoples residing in 184 villages, comprising 2759 families | knowledge and attitudes toward mental illness. Acceptance of mental illnesses within the community. | Health workers were trained to provide community education and to identify and refer individuals with psychiatric problems to a community hospital. A combination of education, supportive counseling and pharmacotherapy provided by doctors, health animators and village health workers formed the key components of the treatment that was offered to participants. | Changes in the healthcare delivery as well services utilization; Change in knowledge and attitudes towards mental illness | Treated patients experienced significant improvement in daily function (p = 0.01). Mean treatment adherence scores remained stable at the beginning and end of treatment, overall. The proportion of selfreferrals increased from 27% to 57% over three years. Surveys conducted before and after program initiation also suggested improved knowledge, attitudes and acceptance of mental illness by the community. |
| 7. | Shidhaye et al., 2017 | To assess whether implementation of VISHRAM intervention was associated with an increase in the proportion of people with depression who sought treatment (contact coverage). | Cross-sectional, Before and after intervention | 1457 and 1887 adult community members from voter list of 30 villages surveyed at baseline and 18 months respectively. | 30 villages in the Amravati district in Vidarbha, central India. | Depression and mental health literacy | Vishram was a collaborative care model which was delivered by community health workers, village based lay counselors, primary health care physicians and visiting psychiatrists. Awareness about mental disorders was carried out by lay health workers in the community. They referred individuals identified with depression to health counselors and provided first aid. Health counselors offered Health Activity Program (HAP). Those who dint respond to HAP were offered help at health facilities. | The primary outcome was change in contact coverage with VISHRAM, defined as the difference in the proportion of individuals with depression (PHQ-9 score >9) who sought treatment for symptoms of depression between the baseline and the 18-month survey population. Secondary outcomes were whether the distribution of coverage was equitable, the type of services sought, and mental health literacy. | The contact coverage for current depression was six-times higher in the 18month survey population (27·2%, 95% CI 21·4–331·7) than in the baseline survey population (4·3%, 1·5-7·1). Contact coverage was equitably distributed across sex, education, income, religion, and caste. Most providers consulted for care were general physicians. They observed significant improvements in a range of mental health literacy indicators, for example, conceptualisation of depression as a mental health problem and the intention to seek care for depression. |
| 8. | Garfin et al. 2019 | To explore predictors of improved QOL over time in Women Living with HIV/AIDS (WLH/A) in India | RCT with a factorial design | 600 WLH/A in Andhra Pradesh, in Southern India enrolled in a larger nurse-led- Asha-support randomized control trial (RCT). | one Community Health Center and 1-2 Primary Care Centers (PHCs) in rural Andhra Pradesh near one of four high-HIV- prevalence sites. | Depression and stigma amongst WLH/A | 4 group based modules: keeping healthy, caregiving, staying upbeat, and healthy eating for self and family. A minimum of six group sessions (three modules with two sessions each) were delivered by experts in a large room at the research site. | Analyses examined whether psychosocial variables measured at baseline could help classify subgroups of WLH/A enrolled in an Asha- supported intervention and whether subgroup membership predicted QOL at baseline, change over time, and at 6-month followup. | At follow-up, the sample as a whole exhibited lower depression (M = 0.05, SD = 0.32), internalized stigma, (M = 0.004, SD = 0.03), and stigma fears (M = 0.01, SD = 0.13) and improved social support (M = 4.96, SD = 0.09) compared to baseline (for paired t tests comparing baseline to followup scores all p-values < .001). |
| 9. | Maulik et al., 2019 | To report changes in stigma perceptions over three time points in the rural | Pre test and post test study design followed by a post communities where the antistigma campaign was conducted. | 1417 Community member ≥18 years old intervention evaluation at end of 3Months | Community setting, in two villages of west Godavari district of Andhra Pradesh, South India. This was part of the larger study named Smart Mental Health. | Stigma perceptions in seeking mental health care | A multimediabased anti-stigma campaign was conducted over a 3-month period in the West Godavari district of Andhra Pradesh, India. Following that, the primary carebased mental health service was delivered for 1 year. The antistigma campaign was evaluated in two villages and data were captured at three time points over a 24-month period before and after delivery of the campaign and after completion of the health services delivery intervention. Standardised tools captured data on knowledge, attitude and behaviour towards mental health as well as perceptions related to help seeking for mental illnesses | Significant changes in mean scores of each item of KAB and BACE-TS across three time points. | Most knowledge, attitude and behaviour scores improved over the three time points. Overall mean scores on stigma perceptions related to help seeking improved by – 0.375 (minimum/maximum of – 2.7/2.4, s.d. 0.519, P < 0.001) during this time. |
3.1.1. Organisational/Institutional level of intervention
Chinnayya et al. (1990) and Armstrong et al. (2011) focused on training and educating primary and community health workers in the health facility and community respectively for effective identification and management of mental disorders. Both studies evaluated training or educational sessions that were provided using different strategies, like lectures, case demonstrations, and vignettes. The studies found that the intervention strategies were effective in increasing mental health literacy and changing attitudes towards patients with mental disorders. They had some limitations. They did not have a control group, findings could not be generalized to other geographic locations or cultures and the pre-post differences of level of interactions of health workers with the patients were not clearly captured.
A variety of indigenous beliefs were elicited at baseline evaluation in the study conducted by Joel et al. (2006). This study found that local cultural beliefs were common among the general population and community health workers, especially in non-western cultures. Seeking biomedical help at follow-up was significantly related to receiving education about the biomedical aspects of chronic psychosis. The experimental group consisted of community health workers who received education only. A statistically significant difference in explanatory models of psychosis were found in intervention arm compared to the control arm. Long-term retention of learnt information and practice were not evaluated.
3.1.2. Multi-level interventions
The Community Care for People with Schizophrenia in India (COPSI) trial (Balaji et al., 2012) had different intervention components including psychoeducation, adherence management, rehabilitation, referral to the community agencies and health promotion which were implemented in three stages of the intervention. The study collected data on mental health service delivery. The stigma related intervention was adapted to the local context and modified based on formative research. This study captured data on different aspects of stigma and discrimination in relation to socio-demographic determinants, such as, gender, personality, and knowledge of subject matter among community health workers.
Mindlis et al. (2015) evaluated mental health knowledge and attitudes within the general community. Using multiple stakeholders as implementers, the interventions included creating awareness on mental health in the community, providing free and easy access to care for mental illnesses, training of community health workers, and providing life skill support to better mental health. Using multiple stakeholders, the intervention arm showed higher levels of literacy regarding depression and lower levels of stigma than control arm. However, longitudinal data was absent to measure change in knowledge and attitude towards depression. The results were not generalizable.
Two studies - Association for Health and Welfare in the Nilgiris (ASHWINI) (Nimgaonkar and Menon, 2015) and Systematic Medical Appraisal Referral and Treatment (SMART) Mental Health Project (Maulik, Devarapalli et al., 2017; Maulik, Kallakuri et al., 2017; Maulik et al., 2019; Maulik et al., 2020), focussed on multifaceted interventions and emphasized on task sharing and community participation. Though both the studies were part of larger programmes, they had components that concentrated on improving knowledge and attitudes toward mental health, and reducing stigma perceptions related to help-seeking. The latter study observed improved changes with respect to knowledge, attitudes and behaviours towards mental disorders, thereby increasing the service utilisation and help-seeking. These two studies were implemented in tribal and rural settings and provided a local context to the interventions as well. Maulik et al. (2019) also provided longitudinal follow-up data on the impact of the intervention over a 2-year period and showed a positive trend on both knowledge, attitude and behaviours and stigma perceptions related to help-seeking. Additionally, qualitative evaluation of the intervention indicated acceptability and feasibility of implementing the intervention in the rural and tribal settings of India (Maulik, Devarapalli et al., 2017; Maulik, Kallakuri et al., 2017). Though both the studies had shown improvement in the knowledge, and attitudes related to mental health within the community, more robust results are required on clinical effectiveness and cost-effectiveness. One limitation was that neither study had a control group, hence the results should be interpreted with caution.
Shidhaye et al. (2017) reported the findings of the community-based study called the Vidarbha Stress and Health Program (VISHRAM), which addressed the mental health risk factors in a rural community. The three-step intervention helped to identify and treat people suffering from mental illnesses. The primary and community health workers and the psychiatrists sensitized the community, provided counselling and managed cases that needed psychiatric care. The study showed significant improvements in mental health literacy about depression and seeking care.
Garfin et al. (2019) explored Quality of Life (QOL) among women living with Human Immuno-deficiency Virus (HIV) using an educational component delivered by community health workers. The modules included increasing coping skills, knowledge and acceptance of HIV and depression, and staying healthy. The study was effective in reducing depression, internalised stigma and stigma related fears towards HIV and depression, and improved social support at follow-up phase. The researchers opined that interventions combining education with primary health worker support are beneficial.
3.2. Primary vs. secondary stigma reduction focus
We categorized interventions as those that were explicitly designed to reduce stigma versus those that had a stigma-reduction component within another primary objective. Five studies had stigma-reduction as a secondary component with a different primary focus (Garfin et al., 2019; Joel et al. 2006; Maulik et al., 2019; Nimgaonkar and Menon, 2015; Shidhaye et al., 2017). The types of primary focus in the other four studies were: attitude changes towards mental health care (Chinnayya et al., 1990); mental health literacy (knowledge and beliefs) about mental disorders (Armstrong et al., 2011); addressing myths about mental disorders, coping strategies to address negative reactions and self-disclosure (Balaji et al., 2012); and knowledge and attitudes towards depression (Mindlis et al., 2015).
4. Discussion
The review provides an overview of the characteristics and effectiveness of stigma-reduction interventions undertaken in India. Majority of the studies focused on community education, health promotion and treatment in combination with other strategies aimed at individual behaviour change, individual’s environment and the community. Research suggests that stand-alone educational programs can only help to suppress rather than reject stereotypes and could be ineffective and short-lived in reducing stigma (Corrigan et al., 2000; Penn & Corrigan, 2002). Only one study attempted to use social contact as a part of the intervention (Maulik, Devarapalli et al., 2017; Maulik, Kallakuri et al., 2017; Maulik et al., 2019), even though literature suggests social contact as the most effective strategy to reduce stigma related to mental health (Corrigan et al., 2012; Thornicroft et al., 2016). No study focused on governmental or policy level strategies. This could be an important direction for future research and worth exploring using policy reviews.
Multi-country studies such as Emerging Mental Health Systems in Low and Middle Income Countries (EMERALD) (Semrau et al., 2015) and Programme for Improving Mental Health Care-PRIME (Mendenhall et al., 2014) have indicated barriers, such as the lack of a monitoring system, discrimination, systemic and sociocultural challenges, in providing acceptable and successful mental health care and services in low-resource countries such as India. Collaborations with other global researchers can help identify tools can be adapted for future use in India.
The review indicates that research about stigma is absent from large parts of India, except Southern and Western parts. Understanding stigma in diverse regions in India is important to understand the prevalence and nature of stigma across the country. Most of the interventions included in this review did not discuss specific terminologies related to stigma and discrimination. However, Balaji et al. (2012) mentioned that people with schizophrenia and their caregivers used labels and terms to describe their diagnosis as ‘nerve problem’ and attributed it to stress, childhood, trauma, personality and supernatural phenomena. Joel et al. (2006) found that the majority of the community health workers attributed black magic or evil spirits as the cause for mental disorders and sought treatment from traditional healers or faith healers instead of seeking medical help. Over two thirds of community members from another study also reported that black magic was the major cause for mental illness (Nimgaonkar and Menon, 2015).
An exploratory study found that around one third of the patients with severe mental illness visiting a tertiary care centre in North India, had faced stigmatizing labels such as paagal (mad), aalsi (lazy), sust (lethargic), darpok (coward), while seeking treatment, and due to that stopped or wanted to stop their treatment (Grover et al., 2020). Others reported stigma and embarrassment associated with mental disorders across all social strata, and this was a reason for under-reporting of psychological symptoms and poor help-seeking (Sagar et al., 2017; Venkatesh et al., 2015). There is a need to increase awareness about mental health-related stigma and discrimination amongst community members, people with mental disorders, their caregivers and families, and even among health workers.
Mental health service delivery is affected by help-seeking, the treatment gap and by the types of stigma prevalent in society. Levels of mental health literacy is not only poor amongst the community members, but even amongst the health care professionals working in tertiary care hospitals (Ransing et al., 2020). Mental health literacy has been part of the community-based interventions carried out in some studies (Maulik, Devarapalli et al., 2017; Maulik, Kallakuri et al., 2017, 2019; Mindlis et al., 2015; Shidhaye et al., 2017), which contributed to improved uptake of mental health services. Most interventions included in this review were delivered to community members only. Research suggests that single intervention level and single target group (intervention delivered to) approaches are not enough to reduce stigma and discrimination significantly (Heijnders and Van Der Meij, 2006). Knowledge, attitudes and behaviours of mental health professionals, policy makers, clinical patients and other health care professionals were not evaluated or targeted as a part of the intervention in any of these studies.
There is a need to involve different types of stakeholders such as patients and their caregivers, community members, community and primary health workers, mental health professionals, non-mental health professionals working in secondary or tertiary settings, and policy makers, in developing, designing and implementing culturally relevant, sustainable, stigma reduction programmes or interventions. Only two studies (Nimgoankar et al., 2015; Maulik, Devarapalli et al., 2017; Maulik, Kallakuri et al., 2017, 2019) included tribal communities, but interventions relevant to other vulnerable and marginalized populations are absent.
The scope of this review was limited as it focused on original research with primary data on stigma interventions related to reducing mental health-related stigma. Some relevant studies might have been missed because of the exclusion of grey literature, qualitative studies and unindexed journals. Only studies in English language were included. While there is a chance that this may lead to publication bias due to non-inclusion of vernacular languages, medical scientific literature in India is predominantly in English.
The review has several strengths in that it provides the first synthesised overview of interventions to reduce mental health-related stigma in India specifically. This review’s broad search strategy allowed any program or intervention with stigma and mental health as outcomes to be included. The review was conducted according to PRISMA guidelines and involved two independent researchers who extracted the data, thus reducing chances of bias.
The review highlights areas for future stigma research. First, more research is needed in other regions of India apart from Western and Southern India. Second, research should focus on people with substance use disorders and their caregivers. Third, longitudinal studies and interventions targeting multilevel systems are needed. Fourth, the relationship between stigma interventions, socio-economic factors, treatment adherence and help-seeking should be explored more carefully using robust study designs including randomized controlled trials. Fifth, stigma reduction strategies apart from community sensitization and educational trainings need to be explored. Sixth, culturally validated tools should be used and new tools for local settings should be developed.
5. Conclusions
Stigma is a barrier for mental health service delivery and help-seeking, and it contributes to the treatment gap. This review captures extant research on interventions to reduce stigma related to mental health, and it provides information that can guide future research. Development of comprehensive, contextually adapted interventions involving multiple levels such as intrapersonal, interpersonal, community, organisational and governmental levels is needed. Interventions targeting different population groups and spread across the country are required.
Supplementary Material
Acknowledgements
The authors would like to thank Dr. Soumyadeep Bhaumik for his assistance in constructing the search strategy.
Funding Source Declaration
The Indigo Partnership research programme is a part of the Indigo Network; a collaboration of research colleagues in over 30 countries worldwide committed to developing knowledge about mental-illness-related stigma and discrimination, both in terms of their origins and their eradication. It is coordinated by the Centre for Global Mental Health, Institute of Psychiatry, Psychology and Neuroscience at King’s College London. This work was supported by the Medical Research Council (grant number MR/R023697/1).
AK is partly covered out of INDIGO partnership programme while AK, SK and PKM are all partly supported by the NHMRC/GACD funded SMART Mental Health Project (APP1143911). This project was supported by INDIGO Partnership programme (MR/R023697/1) awarded to GT on which he is the principal investigator. GT is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration South London at King’s College London NHS Foundation Trust, and by the NIHR Asset Global Health Unit award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. GT also receives support from the National Institute of Mental Health of the National Institutes of Health under award number R01MH100470 (Cobalt study). GT is supported by the UK Medical Research Council in relation to the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards. BAK is supported by the US National Institute of Mental Health (grants K01MH104310 and R21MH111280). PCG is supported by the UK Medical Research Council in relation the Indigo Partnership (MR/R023697/1) award.
Footnotes
Contributors
AK did the literature search, article screening, data extraction, wrote the first draft and edited the manuscript. SK did the article screening, data extraction, and edited the final manuscript. PKM provided overall direction and critical analysis for the manuscript. BK, EH, PCG and GT conceived the initial focus of the review and the relevant key words for the search strategy and then provided critical inputs into the draft of the manuscript. All listed authors provided critical comments to the manuscript, edited and have approved the final manuscript.
Declaration of Competing Interest
The authors report no declarations of interest.
Contributor Information
Sudha Kallakuri, Email: skallakuri1@georgeinstitute.org.in.
Brandon A. Kohrt, Email: bkohrt@email.gwu.edu.
Eva Heim, Email: e.heim@ psychologie.uzh.ch.
Petra C. Gronholm, Email: petra.gronholm@kcl.ac.uk.
Graham Thornicroft, Email: graham.thornicroft@kcl.ac.uk.
Pallab K. Maulik, Email: pmaulik@georgeinstitute.org.in.
References
- Armstrong G, Kermode M, Raja S, Suja S, Chandra P, Jorm AF. A mental health training program for community health workers in India: impact on knowledge and attitudes. International journal of mental health systems. 2011;5(1):17. doi: 10.1186/1752-4458-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balaji M, Chatterjee S, Koschorke M, Rangaswamy T, Chavan A, Dabholkar H, Dakshin L, Kumar P, John S, Thornicroft G, Patel V. The development of a lay health worker delivered collaborative community based intervention for people with schizophrenia in India. BMC health services research. 2012;12(1):42. doi: 10.1186/1472-6963-12-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böge K, Zieger A, Mungee A, Tandon A, Fuchs LM, Schomerus G, Ta TMT, Dettling M, Bajbouj M, Angermeyer M, Hahn E. Perceived stigmatization and discrimination of people with mental illness: a survey-based study of the general population in five metropolitan cities in India. Indian journal of psychiatry. 2018;60(1):24. doi: 10.4103/psychiatry.IndianJPsychiatry_406_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinnayya HP, Chandrashekar CR, Moily S, Puttamma Raghuram A, Subramanya KR, Shanmugham V, Udaykumar GS. Training primary care health workers in mental health care: Evaluation of attitudes towards mental illness before and after training. International journal of social psychiatry. 1990;36(4):300–307. doi: 10.1177/002076409003600408. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatric services. 2012;63(10):963–973. doi: 10.1176/appi.ps.201100529. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, River LP, Lundin RK, Wasowski KU, Campion J, Mathisen J, Goldstein H, Bergman M, Gagnon C, Kubiak MA. Stigmatizing attributions about mental illness. Journal of Community Psychology. 2000;28(1):91–102. [Google Scholar]
- Garfin DR, Shin SS, Ekstrand ML, Yadav K, Carpenter CL, Sinha S, Nyamathi AM. Depression, social support, and stigma as predictors of quality of life over time: results from an Asha-based HIV/AIDS intervention in India. AIDS care. 2019;31(5):563–571. doi: 10.1080/09540121.2018.1563281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautam S, Jain N. Indian culture and psychiatry. Indian journal of psychiatry. 2010;52(1):S309. doi: 10.4103/0019-5545.69259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautam SS, Kapur RL. Psychiatric patients with somatic complaints. Indian Journal of Psychiatry. 1977;19(4):75. [Google Scholar]
- Grover S, Shouan A, Sahoo S. Labels used for persons with severe mental illness and their stigma experience in North India. Asian Journal of Psychiatry. 2020;48 doi: 10.1016/j.ajp.2019.101909. 101909. [DOI] [PubMed] [Google Scholar]
- Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma�reduction strategies and interventions. Psychology, health & medicine. 2006;11(3):353–363. doi: 10.1080/13548500600595327. [DOI] [PubMed] [Google Scholar]
- Joel D, Sathyaseelan M, Jayakaran R, Vijayakumar C, Muthurathnam S, Jacob KS. A biomedical educational intervention to change explanatory models of psychosis among community health workers in South India. Indian journal of psychiatry. 2006;48(3):138. doi: 10.4103/0019-5545.31575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulik PK, Devarapalli S, Kallakuri S, Tewari A, Chilappagari S, Koschorke M, Thornicroft G. Evaluation of an anti-stigma campaign related to common mental disorders in rural India: a mixed methods approach. Psychological medicine. 2017;47(3):565–575. doi: 10.1017/S0033291716002804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulik PK, Kallakuri S, Devarapalli S, Vadlamani VK, Jha V, Patel A. Increasing use of mental health services in remote areas using mobile technology: a pre-post evaluation of the SMART Mental Health project in rural India. Journal of global health. 2017;(1):7. doi: 10.7189/jogh.07.010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulik PK, Devarapalli S, Kallakuri S, Tripathi AP, Koschorke M, Thornicroft G. Longitudinal assessment of an anti-stigma campaign related to common mental disorders in rural India. The British Journal of Psychiatry. 2019;214(2):90–95. doi: 10.1192/bjp.2018.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulik PK, Devarapalli S, Kallakuri S, Bhattacharya A, Peiris D, Patel A. The systematic medical appraisal referral and treatment mental health project: Quasi-experimental study to evaluate a technology-enabled mental health services delivery model implemented in rural India. Journal of medical Internet research. 2020;22(2) doi: 10.2196/15553. 15553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendenhall E, De Silva MJ, Hanlon C, Petersen I, Shidhaye R, Jordans M, Luitel N, Ssebunnya J, Fekadu A, Patel V, Tomlinson M. Acceptability and feasibility of using non-specialist health workers to deliver mental health care: stakeholder perceptions from the PRIME district sites in Ethiopia, India, Nepal, South Africa, and Uganda. Social science & medicine. 2014;118:33–42. doi: 10.1016/j.socscimed.2014.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindlis I, Schuetz-Mueller J, Shah S, Appasani R, Coleman A, Katz CL. Impact of community interventions on the social representation of depression in Rural Gujarat. Psychiatric Quarterly. 2015;86(3):419–433. doi: 10.1007/s11126-015-9342-x. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement Open Med. 2009;3(3):123–130. [PMC free article] [PubMed] [Google Scholar]
- Murthy RS. Stigma is universal but experiences are local. World psychiatry. 2002;1(1):28. [PMC free article] [PubMed] [Google Scholar]
- Nimgaonkar AU, Menon SD. A task shifting mental health program for an impoverished rural Indian community. Asian journal of psychiatry. 2015;16:41–47. doi: 10.1016/j.ajp.2015.05.044. [DOI] [PubMed] [Google Scholar]
- Penn DL, Corrigan PW. The effects of stereotype suppression on psychiatric stigma. Schizophrenia research. 2002;55(3):269–276. doi: 10.1016/s0920-9964(01)00207-9. [DOI] [PubMed] [Google Scholar]
- Ransing R, Kukreti P, Deshpande S, Godake S, Neelam N, Raghuveer P, Mahadevaiah M, Kataria D, Patil S, Puri M, Padma K. Perinatal depression–knowledge gap among service providers and service utilizers in India. Asian journal of psychiatry. 2020;47:1018–1022. doi: 10.1016/j.ajp.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagar R, Pattanayak RD, Chandrasekaran R, Chaudhury PK, Deswal BS, Singh RL, Malhotra S, Nizamie SH, Panchal BN, Sudhakar TP, Trivedi JK. Twelve-month prevalence and treatment gap for common mental disorders: Findings from a large-scale epidemiological survey in India. Indian journal of psychiatry. 2017;59(1):46. doi: 10.4103/psychiatry.IndianJPsychiatry_333_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semrau M, Evans-Lacko S, Alem A, Ayuso-Mateos JL, Chisholm D, Gureje O, Hanlon C, Jordans M, Kigozi F, Lempp H, Lund C. Strengthening mental health systems in low-and middle-income countries: the Emerald programme. BMC medicine. 2015;13(1):79. doi: 10.1186/s12916-015-0309-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar BR, Saravanan B, Jacob KS. Explanatory models of common mental disorders among traditional healers and their patients in rural south India. International Journal of Social Psychiatry. 2006;52(3):221–233. doi: 10.1177/0020764006067215. [DOI] [PubMed] [Google Scholar]
- Shidhaye R, Murhar V, Gangale S, Aldridge L, Shastri R, Parikh R, Shrivastava R, Damle S, Raja T, Nadkarni A, Patel V. The effect of VISHRAM, a grassroots community-based mental health programme, on the treatment gap for depression in rural communities in India: a population-based study. The Lancet Psychiatry. 2017;4(2):128–135. doi: 10.1016/S2215-0366(16)30424-2. [DOI] [PubMed] [Google Scholar]
- Shidhaye R, Shrivastava S, Murhar V, Samudre S, Ahuja S, Ramaswamy R, Patel V. Development and piloting of a plan for integrating mental health in primary care in Sehore district, Madhya Pradesh. India The British Journal of Psychiatry. 2016;208(s56):13–20. doi: 10.1192/bjp.bp.114.153700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart H. Reducing the stigma of mental illness. Global Mental Health. 2016:3. doi: 10.1017/gmh.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tewari A, Kallakuri S, Devarapalli S, Jha V, Patel A, Maulik PK. Process evaluation of the systematic medical appraisal, referral and treatment (SMART) mental health project in rural India. BMC psychiatry. 2017;17(1):385. doi: 10.1186/s12888-017-1525-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirthalli J, Kumar CN. Stigma and disability in schizophrenia: Developing countries’ perspective. International Review of Psychiatry. 2012;24(5):423–440. doi: 10.3109/09540261.2012.703644. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: ignorance, prejudice or discrimination? The British Journal of Psychiatry. 2007;190(3):192–193. doi: 10.1192/bjp.bp.106.025791. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, Koschorke M, Shidhaye R, O’Reilly C, Henderson C. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet. 2016;387(10023):1123–1132. doi: 10.1016/S0140-6736(15)00298-6. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Andrade L, Borges G, Bruffaerts R. Undertreatment of people with major depressive disorder in 21 countries. The British Journal of Psychiatry. 2017;210(2):119–124. doi: 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesh BT, Andrews T, Mayya SS, Singh MM, Parsekar SS. Perception of stigma toward mental illness in South India. Journal of family medicine and primary care. 2015;4(3):449–453. doi: 10.4103/2249-4863.161352. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.