Abstract
There is good evidence that behavioural weight management interventions improve physical health, however the impact on mental health remains unclear. We evaluated the impact of behavioural weight management interventions on mental health-related outcomes in adults with overweight or obesity at intervention-end and 12-months from baseline. Eligible studies were randomised controlled trials (RCTs) or cluster-RCTs of adult behavioural weight loss interventions reporting affect, anxiety, binge-eating, body image, depression, emotional eating, quality of life, self-esteem, and stress. We searched seven databases from inception to 07/05/2019 and included 43 articles reporting 42 RCTs. Eighteen studies were deemed to be at high risk of bias. We conducted random-effects meta-analyses, stratified analyses, and meta-regression using Stata. Interventions generated greater improvements than comparators for depression, mental health-related quality of life, and self-efficacy at intervention-end and 12-months from baseline. There was no difference between groups for anxiety, overall quality of life, self-esteem, or stress at intervention-end. There was insufficient evidence to assess the impact on anxiety, binge-eating, body image, emotional eating, affect, life satisfaction, self-esteem, or stress at intervention-end and/or 12-months from baseline. While evidence suggests that interventions benefit some aspects of mental health, high-quality, transparently reported RCTs measuring a range of mental health outcomes over longer durations are required to strengthen the evidence base.
Keywords: Obesity, Mental health, Weight management, Interventions
1. Introduction
Overweight and obesity are associated with increased risk of conditions such as cardiovascular disease, type 2 diabetes, stroke, osteoarthritis and some cancers, as well as greater all-cause mortality.1–6 Additionally, obesity is related to an increased risk of poor mental health including mood disorders, anxiety, and psychiatric disorders.7,8 There is good evidence that behavioural weight management interventions can improve physical health in people with overweight and obesity.9,10 However, the evidence for their impact on mental health is less clear.
Some studies have reported mental health improvements with weight loss.11–15 However, qualitative evidence suggests that there is inadequate support for mental health and emotional wellbeing in weight management interventions16 Some studies also report concerns that a focus on dietary restriction may influence disordered eating and increase psychological distress.17–20 Greater understanding of the impact of weight management intervention on mental health is necessary to inform the development of interventions to support both mental and physical health concurrently, optimising care and minimising the risk of harm.
Previous systematic reviews have attempted to synthesise evidence for the impact of behavioural weight management interventions on various aspects of mental health, however, findings have been limited and conflicting.17,21–26 For example, Warkentin et al.23 concluded that weight loss may be associated with improved physical health but not mental health, Fabricatore et al.25 reported statistically significant reductions in depressive symptoms following behavioural weight loss interventions, and Lasikiewicz et al.24 concluded that weight management interventions are associated with improvements in multiple mental health outcomes including self-esteem, body image, quality of life and depressive symptoms.
Previous reviews have also highlighted the breadth of mental health outcomes that could be affected by attending a weight management intervention, however the majority of reviews have focused on a limited number of outcomes.17,21–26 It is important to generate a comprehensive understanding of the impact of weight management programmes on mental health as the benefits of improvements in one domain may be undermined by negative impacts on another. Previous reviews have also excluded participants with any concurrent physical or mental diagnosis to constrain the search or to exclude illnesses associated with unintentional weight changes (e.g. chronic obstructive pulmonary disease or cancer).17,27 Overweight and obesity is associated with increased risk of a wide range of comorbidities,28 therefore the exclusion of these participants limits the representativeness of findings.
The limitations of previous reviews and inconsistent findings make it difficult to draw clear, reliable conclusions on the impact of weight loss interventions on mental health. To our knowledge, there is no up-to-date, comprehensive review investigating the effect of weight management interventions on a broad range of mental health outcomes in a representative sample of adults with overweight or obesity, or investigating whether particular intervention or study characteristics are more supportive of mental health. Therefore, we aimed to:
Quantify the effect of behavioural weight management interventions on mental health in adults with overweight and obesity compared to inactive/minimal intervention or ‘usual care’ comparator groups.
Quantify whether particular study, intervention or participant characteristics influence the effect of interventions on mental health.
2. Methods
This review adheres to PRISMA reporting.29 Full details of the methods were reported in the published protocol.30
2.1. Eligibility criteria
Participants: Community-dwelling adults (≥ 18 years) with overweight or obesity (body mass index (BMI) ≥ 25 kg/m2) seeking intentional weight loss. To increase the generalisability of the findings, we included studies that included people with comorbidities but excluded papers that focused exclusively on populations with a physical or mental comorbidity (e.g. all participants had cancer), or pregnant women.
Interventions: Behavioural weight management interventions in community-based settings aiming to achieve weight loss through changes in diet and/or physical activity. Interventions treating eating disorders or involving surgical and/or pharmacological intervention were excluded.
Comparators: Inactive/minimal intervention (e.g. information leaflet) or usual care.
Outcomes: Affect/mood; anxiety; binge-eating; body image; depression; emotional eating; quality of life; self-esteem; stress. Outcomes reported at intervention-end and at 12-months from baseline were extracted, regardless of intervention duration. We chose these a priori defined outcomes as they were deemed to be the most relevant, were most frequently reported in previous relevant literature, represent the most prevalent mental health conditions, and provide the most comprehensive insight to date into mental health impacts of behavioural weight management interventions.
Study designs: Individual or cluster randomised controlled trials (RCTs). Non-English language publications were excluded.
2.2. Information sources and search
We searched seven databases (AMED, ASSIA, CINAHL, Cochrane database (CENTRAL), Embase, MEDLINE, and PsycINFO) from database inception to 7th May 2019. The search strategy was based on the concepts: (1) adults with overweight/obesity and (2) weight management interventions and (3) mental health outcomes and (4) study designs (Table S1). The search was restricted to English-language papers, with no other restrictions applied. To augment the results of the database search, we hand-searched the reference lists of included studies and previous relevant reviews.10,17,21–27,31–34
2.3. Study selection
Two-stage screening was completed in duplicate, with a third reviewer resolving discrepancies.30 We contacted study authors (n=2) to resolve any uncertainties about eligibility. Where studies were reported in more than one publication, all articles that met eligibility criteria were included and combined to make best use of the data available.
2.4. Data collection
Data extraction was completed by one investigator with full checking by one further investigator. Discrepancies were resolved through discussion, with use of a third investigator where necessary. We contacted study authors (n=26) to request missing data. If there was no response, authors were sent two email reminders. Authors were given a minimum of 2 months to respond. Authors of six studies did not respond, five responded that data was unavailable, and 15 responded with the data requested.
2.5. Risk of bias in individual studies
Risk of bias appraisal was completed by one investigator using the Cochrane ‘Risk of bias’ tool (RoB),35 with full checking by one further investigator. Discrepancies were resolved through discussion, with a third investigator providing consultation if required. Included studies were given an overall rating of ‘low’, ‘unclear’ or ‘high’ risk of bias dependent on the ratings for individual domains. Ratings given to ‘blinding of participants and personnel’ and ‘blinding of outcome assessment’ were excluded from overall assessment of risk of bias due to the behavioural nature of the interventions and self-reported assessment of outcomes.
2.6. Synthesis of results
Stata v.16 was used for all statistical analyses.36 Unstandardised mean differences between the intervention and comparator groups and 95% confidence intervals (CI) were calculated for continuous outcomes, and standardised mean differences (Hedges’ g) if different measurement tools were reported in the individual studies. Effect sizes for each outcome were combined across studies using random effects meta-analysis. When studies had multiple interventions meeting the inclusion criteria, each estimate of intervention versus comparator was included separately in the meta-analysis, and the comparator group was split between the different interventions to avoid the data in this group contributing more than once to the pooled result (i.e. unit-of-analysis error). When studies reported multiple measures for the same outcome, the measure deemed by the authorship team to be most valid and precise was prioritised and used. Meta-analyses examined effectiveness at intervention-end and 12-months from baseline, regardless of intervention duration. These timepoints were selected to assess the immediate effect and longer-term impact of interventions on mental health outcomes. The potential influence of intervention duration was assessed by subgroup meta-analyses.
For meta-analyses combining unstandardised mean differences, effect sizes based either on post-intervention or change from baseline results were combined in a single forest plot. Separate forest plots were produced for post-intervention and change from baseline when standardised mean differences were used in the meta-analyses.35
Heterogeneity was assessed using the I2 statistic and interpreted according to Cochrane recommendations.35 Contour-enhanced funnel plots of individual study effect sizes were produced for all outcomes to assess the risk of publication bias.
2.7. Additional analyses
Sensitivity analysis was conducted by removing studies judged to be high risk of bias from pooled estimates to investigate the potential impact on effect estimates. Potential study-level sources of observed heterogeneity between studies in the effect estimates were explored using random effects meta-regression and stratified analyses. Study-level characteristics considered were intervention type (education-only, physical activity-only, education and physical activity), intervention duration (in weeks), intervention delivery mode (face-to-face, online, resources, telephone, combination), comparator type (inactive, minimal, usual care), comparator intensity (minimal vs intervention-intensity), and demographic characteristics (e.g. gender, age).
3. Results
3.1. Study selection
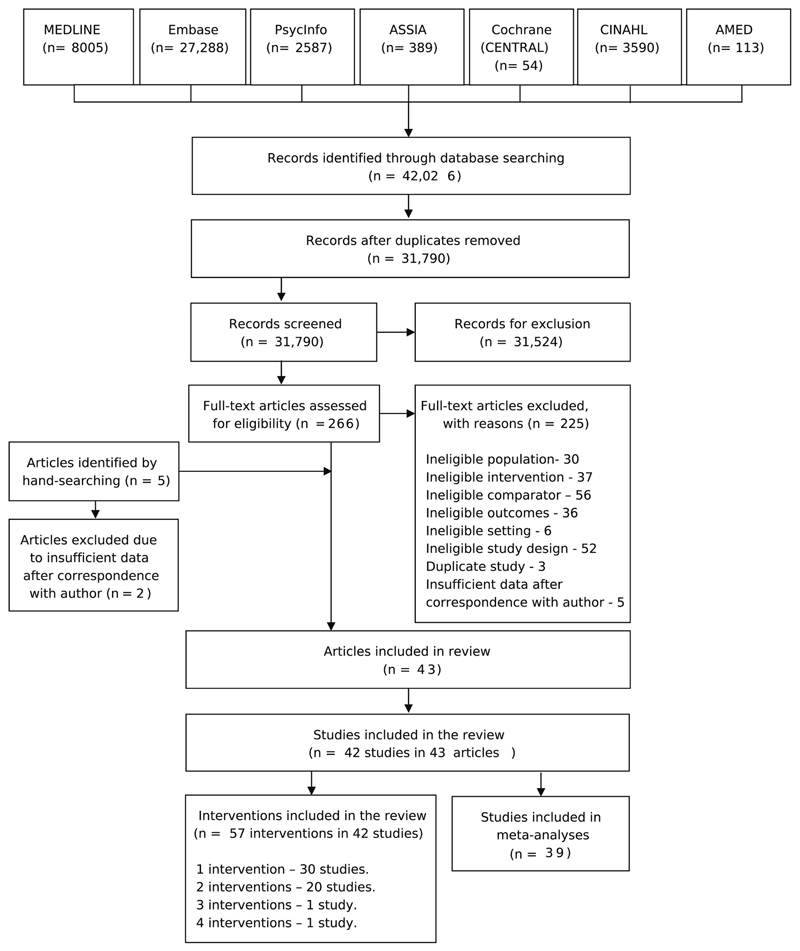
Following de-duplication, 31,390 articles were identified for title and abstract screening, with 265 articles eligible for full text screening. Five additional studies were identified through hand-searching. Forty-three articles, reporting on 42 studies, met eligibility criteria for inclusion in the review (Figure 1).37–79 Three studies were excluded from the meta-analyses as data were incomplete or unable to be pooled.45,52,67
Figure 1.
PRISMA Flow Diagram for the inclusion of studies.
3.2. Study characteristics
Table 1 provides an overview of included studies, and Table S2 presents detailed characteristics for each study. Briefly, studies included a total of 9,385 participants, with the sample size ranging from 2340 to 1,26937. Intervention were compared to no intervention, minimal intervention (e.g. leaflet), or usual care (ranging from minimal to delivery of an intervention). One study did not define what usual care entailed.71
Table 1.
Overview of characteristics of 42 trials, reported in 43 studies, included in the systematic review of behavioural weight management interventions
| Number of studies | Citations | |
|---|---|---|
| Study characteristics | ||
| Study design | ||
| RCTs | 43 (100%) | 37–79 |
| Year of publication | ||
| ≥2019 | 1 | 77 |
| 2017–2018 | 8 | 37, 48, 60, 61, 67, 70, 74, 76 |
| 2015–2016 | 11 | 38, 40, 41, 45, 47, 53, 58, 59, 62, 78, 79 |
| ≤2014 | 23 | 39, 42–44, 46, 49–52, 54–57, 63–66, 68, 69, 71–73, 75 |
| Overall risk of bias rating | ||
| Low risk of bias | 10 | 42, 46, 47, 52, 53, 56, 60, 61, 73, 77 |
| Unclear risk of bias | 15 | 30, 39–41, 44, 45, 48, 49, 64, 66, 67, 72, 76, 78, 79 |
| High risk of bias | 18 | 38, 43, 50, 51, 54, 55, 57–59, 62, 63, 65, 68–71, 74, 75 |
| Study location | ||
| United States | 15 | 38, 39, 41, 45, 46, 50–52, 59, 63, 64, 66, 71, 75, 79 |
| United Kingdom | 10 | 37, 40, 42, 44, 53, 57, 60, 69, 72, 73 |
| Australia | 8 | 48, 49, 54–56, 67, 72, 77 |
| Portugal | 2 | 68, 76 |
| Finland | 2 | 43, 58 |
| Germany | 2 | 72, 78 |
| Malaysia | 1 | 47 |
| Canada | 1 | 61 |
| Greece | 1 | 70 |
| India | 1 | 62 |
| New Zealand | 1 | 74 |
| Not reported | 1 | 65 |
| Participant characteristics | ||
| Sample size | ||
| ≤50 participants | 3 | 40, 44, 59 |
| 50–200 | 25 | 42, 43, 45, 48, 49, 51, 52, 54–58, 61, 62, 64, 66, 69–71, 74–79 |
| ≥200 | 15 | 37–39, 41, 46, 47, 50, 53, 60, 63, 65, 67, 68, 72, 73 |
| Mean age (years) | ||
| 18–30 | 2 | 41, 75 |
| 31–50 | 32 | 40, 42–45, 47, 49–58, 60–62, 66–74, 76–79 |
| 51–70 | 9 | 37–39, 46, 48, 59, 63–65 |
| Proportion female | ||
| 0% (all male) | 8 | 42, 54–56, 61, 62, 73, 79 |
| 50–99% | 27 | 37–39, 41, 43–45, 47–53, 57, 58, 60, 63, 65–67, 70–72, 74, 76, 77 |
| 100% (all female) | 8 | 40, 46, 59, 64, 68, 69, 75, 78 |
| Participant BMI (kg/m2) | ||
| 25–29.9 | 2 | 40, 41 |
| 30–34.9 | 23 | 37, 42, 43, 46–49, 51, 52, 54–56, 59, 64–68, 72, 75, 77–79 |
| 35–39.9 | 13 | 38, 39, 45, 53, 57, 58, 60, 61, 63, 69–71, 73 |
| ≥40 | 4 | 44, 50, 74, 76 |
| Not reported | 1 | 62 |
| Intervention characteristics | ||
| Intervention type | ||
| Education only | 33 | 37, 39, 41, 43, 45–55, 57–61, 63–72, 74, 77, 79 |
| Physical activity only | 4 | 40, 44, 46, 78 |
| Education and physical activity | 8 | 42, 46, 56, 57, 61, 62, 73, 75 |
| Delivery mode | ||
| Face to face | 23 | 37–40, 42, 44, 47, 49, 53, 57, 58, 60–62, 64, 68–70, 72, 73, 75, 78 |
| Online | 6 | 48, 51, 52, 59, 66, 77 |
| Resources | 4 | 48, 56, 65, 77 |
| Telephone | 2 | 39, 45 |
| Mixture of modes | 11 | 41, 43, 46, 50, 54–56, 63, 71, 74, 79 |
| Delivery format | ||
| Individuals only | 25 | 38, 39, 41, 43, 45, 48–52, 54–58, 60, 63, 65–67, 69–71, 76, 77, 79 |
| Groups only | 16 | 37, 39, 40, 42, 44, 47, 49, 53, 61, 62, 64, 68, 72, 73, 75, 78 |
| Groups and individuals | 4 | 46, 59, 63, 74 |
| Intervention duration | ||
| ≤2 months | 3 | 40, 49, 70 |
| >2–6 months | 25 | 37, 42, 44, 45, 47, 48, 51–57, 59–62, 64, 65, 69, 71, 73, 75, 77, 78 |
| >6–11 months | 4 | 50, 58, 66, 79 |
| >12–23 months | 9 | 37, 39, 43, 46, 61, 67, 68, 72, 74 |
| >24 months | 3 | 38, 41, 63 |
| Comparator characteristics | ||
| Type of control group | ||
| No intervention | 16 | 40, 43, 46, 51, 54–56, 61, 65, 66, 69, 73, 75, 77–79 |
| Minimal intervention | 14 | 37, 42, 47–49, 58, 59, 62–64, 67, 68, 70, 76 |
| Usual care | 13 | 38, 39, 41, 44, 45, 50, 52, 53, 57, 60, 71, 72, 74 |
| Outcome characteristics | ||
| Mental health outcomes reported at intervention-end | ||
| Anxiety | 6 | 37, 44, 46, 48, 57, 77 |
| Binge eating | 1 | 66 |
| Body image concerns | 2 | 66, 68 |
| Depression | 14 | 37, 38, 41, 44, 46, 48, 50, 57, 63, 64, 66, 70, 71, 77 |
| Emotional eating | 4 | 53, 58, 68, 72 |
| Negative affect | 4 | 42, 47, 61, 73 |
| Psychological distress | 1 | 74 |
| Quality of life (global) | 12 | 37, 39, 41, 48, 53, 57, 60, 61, 63, 69, 74, 77 |
| Quality of life (mental health-related) | 13 | 40, 42, 46, 47, 54–56, 63, 64, 67, 73, 74, 79 |
| Quality of life (obesity-related) | 4 | 51, 60, 72, 76 |
| Satisfaction with life | 2 | 37, 39 |
| Self-efficacy (general) | 2 | 49, 65 |
| Self-efficacy (diet-related) | 9 | 39, 43, 45, 47, 52, 59, 68, 75, 79 |
| Self-efficacy (exercise-related) | 7 | 39, 44, 54, 55, 68, 75, 79 |
| Self-esteem | 5 | 42, 57, 61, 73, 78 |
| Stress | 6 | 46, 48, 62, 70, 75, 78 |
| Mental health outcomes reported at 12 months from baseline | ||
| Anxiety | 0 | – |
| Body image concerns | 1 | 68 |
| Depression | 2 | 37, 46 |
| Emotional eating | 2 | 53, 68 |
| Negative affect | 1 | 73 |
| Psychological distress | 0 | – |
| Quality of life (global) | 5 | 37, 39, 53, 60, 74 |
| Quality of life (mental health-related) | 5 | 46, 67, 73, 74 |
| Quality of life (obesity-related) | 1 | 60 |
| Satisfaction with life | 1 | 39 |
| Self-efficacy (general) | 2 | 49, 65 |
| Self-efficacy (diet-related) | 3 | 39, 43, 68 |
| Self-efficacy (exercise-related) | 2 | 39, 68 |
| Self-esteem | 1 | 73 |
| Stress | 0 | – |
Note: Number of studies per characteristic may sum greater than 43 because of studies contributing multiple intervention arms.
Abbreviation: BMI, body mass index; RCT, randomized controlled trial.
Overall, the majority of interventions were education-based (n=33),37,39,51–55,57–61,41,63–72,43,74,77,79,45–50 delivered face-to-face (n=23), 37,38,58,60–62,64,68–70,72,73,39,75,78,40,42,44,47,49,53,57 and provided to individuals only (n=25).38,39,54–58,60,63,65–67,41,69–71,76,77,79,43,45,48–52
Twenty-nine studies37,42,54–62,64,44,65,66,69,71,73,75,77–79,45,47,48,50–53 provided interventions lasting between 2 to 11 months, whilst 12 studies provided interventions lasting greater than 12 months.37,38,72,74,39,41,43,46,61,63,67,68 Three studies were less than 2 months in duration.40,49,70 Studies contributing to the analysis of intervention effects at 12 months from baseline were between 1 week and 12 months in duration; ten interventions were less than 6 months in duration,37,49,53,60,65,73 and eight interventions were 12 months in duration.37,39,43,46,68,74
Seven outcomes were positively scaled, defined as measured on a numeric scale where a positive effect size represented a desired impact of the intervention (all measures of quality of life, self-efficacy, and self-esteem). Seven outcomes were negatively scaled, defined as measured on a numeric scale where higher values represented higher levels of the trait, and hence a negative effect size represented a desired impact of the intervention (anxiety, body image concerns, depression, emotional eating, negative affect, psychological distress, and stress). One outcome (obesity-related quality of life was assessed on a variety of scales with higher values representing different concepts in different scales; hence these were analysed separately.
3.3. Risk of bias
Forty-two percent of studies received an overall rating of high risk of bias,38,43,63,65,68–71,74,75,50,51,54,55,57–59,62 35% received an unclear risk of bias rating,30,39,67,72,76,78,79,40,41,44,45,48,49,64,66 and 23% received a low risk of bias rating42,46,47,52,53,56,60,61,73,77 (Table 1). Table S3 reports the domain ratings for all included studies and Figure S1 presents the summary of risk of bias domain ratings across studies.
3.4. Intervention effects on mental health
3.4.1. Anxiety
There was no evidence of a difference between intervention and comparator for anxiety at intervention-end [Post intervention: SMD -0.02 (95% CI -0.25, 0.21; n=11; I2=61%); change from baseline: SMD - 0.22 (95% CI -0.72, 0.29; n=2; I2=0%)] (Figure 2). After excluding studies deemed to be at high risk of bias (n=2)57 there was still no evidence of a difference between groups at intervention-end (Figure S42–43). No studies reported anxiety at 12-months from baseline.
Figure 2.
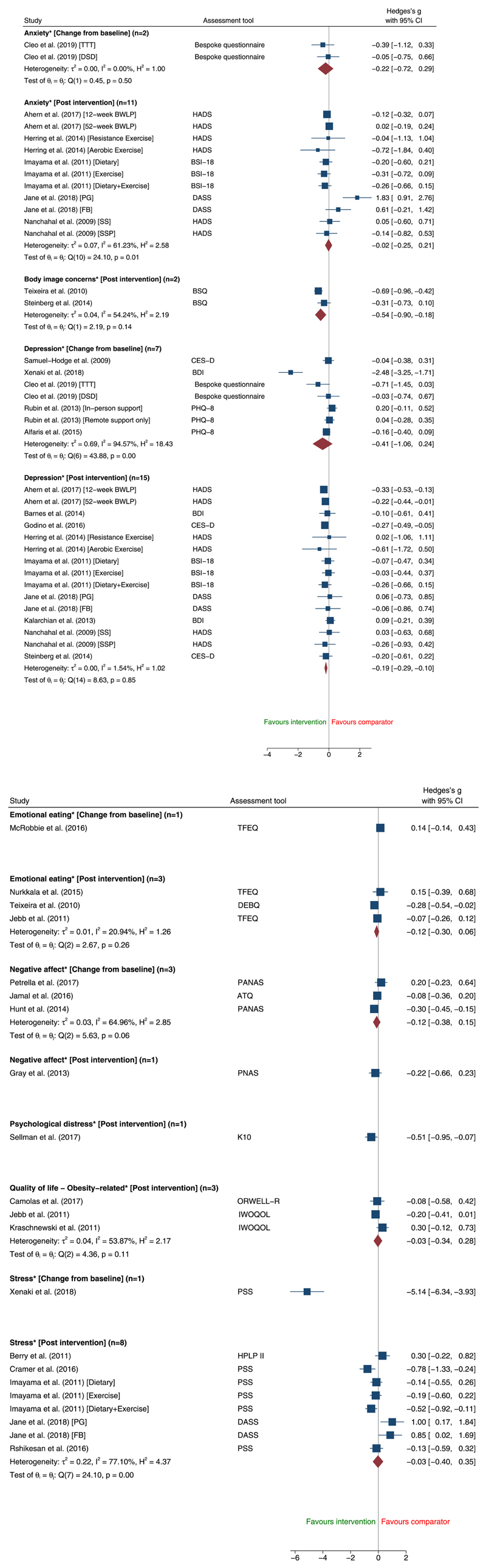
Changes in negatively scaled mental health outcomes at intervention-end comparing adult behavioural weight management interventions with inactive, minimal or usual care comparator using random-effects pairwise meta-analysis. [Abbreviations: TTT: Ten Top Tips; DSD: Do Something Different; BWLP: Behavioural Weight Loss Programme; PG: Pamphlet Group; FB: Facebook Group; SS: Structured Support; SSP: Structured Support and Physical Activity; HADS: Hospital Anxiety and Depression Scale: BSI: Brief Symptom Inventory; DASS: Depression Anxiety Stress Scales; BSQ: Body Shape Questionnaire; CES-D: Center for Epidemiologic Studies Depression Scale; BDI: Beck Depression Inventory: PHQ: Patient Health Questionnaire; TFEQ: Three Factor Eating Questionnaire; DEBQ: Dutch Eating Behaviour Questionnaire; PANAS/PNAS: Positive and Negative Affect Schedule; ATQ: Automatic Thoughts Questionnaire; ORWELL-R: Obesity Related Wellbeing Questionnaire; IWOQOL: Impact of Weight on Quality of. Life; PSS: Perceived Stress Scale; HPLP II: Health Promoting Lifestyle Profile.]
Meta-regression identified that the substantial heterogeneity at intervention-end was explained by one study48 where the intervention consisted solely of provision of resources (Table S4). After removing this study, there was a suggestion of an effect in favour of the intervention [SMD -0.10 (95% CI -0.22, 0.02; n=10; I2=0%)] (Figure S49).
3.4.2. Binge-eating
Only one study66 reported results for binge-eating at intervention-end, so this could not be included in the meta-analysis, despite being a pre-specified outcome. This study found no evidence of a difference between intervention and control in the likelihood of reporting any binge eating [odds ratio 3.9 (95% CI 0.9, 10.0), p=0.079]. No studies reported binge-eating at 12 months from baseline, so no meta-analysis was possible.
3.4.3. Body image concerns
The combined effect estimate favoured the intervention over comparator for body image concerns at intervention-end [SMD -0.54 (95% CI -0.90, -0.18; n=2; I2= 54%)], but there was moderate heterogeneity (Figure 2). Only one study reported body image concerns at 12-months from baseline [SMD -0.69 (-0.96, -0.42)],68 so no meta-analysis was possible.
3.4.4. Depression
There was some evidence of an effect in favour of interventions for depression at intervention-end [Post intervention: SMD -0.19 (95% CI -0.29, -0.10; n=15; I2=2%); Change from baseline: SMD -0.41 (95% CI -1.06, 0.24; n=7; I2=1%)] (Figure 2) and at 12-months from baseline [Post intervention: SMD -0.19 (95% CI -0.34, -0.04; n=5; I2=0%)] (Figure S41).
After removal of interventions from studies deemed to be high risk of bias (n=8)38,50,57,63,70,71 an effect remained in favour of the intervention at the end of the intervention [Post intervention: SMD -0.23 (95% CI -0.34, -0.13; n=11; I2=0%); Change from baseline: SMD -0.17 (95% CI -0.51, 0.18; n=3; I2=19%)] (Figure S42–43).
3.4.5. Emotional eating
There was no evidence of a difference between intervention and comparator for emotional eating [Post intervention: SMD -0.12 (95% CI -0.30, 0.06; n=3; I2=21%)] (Figure 2). Only one study reported change from baseline results for emotional eating at intervention-end53 [SMD 0.14 (95% CI -0.14, 0.43)] or at 12-months from baseline, [Post intervention: SMD -0.28 (95%CI -0.54, -0.02); Mean change SMD 0.14 (95% CI -0.13, 0.41)]71 so no meta-analysis was possible.
3.4.6. Negative affect
At intervention-end, there was no evidence of a difference between intervention and comparator for negative affect [Change from baseline: SMD -0.12 (95% CI -0.38, 0.15; n=3; I2=65%)] (Figure 2). Only one study reported post-intervention results for negative affect at the end of the intervention [SMD - 0.22 (95% CI -0.66, 0.23)],42 and one study reported results at 12-months from baseline [SMD -0.21 (95% CI -0.36, -0.06)],73 so no meta-analysis was possible.
3.4.7. Psychological distress
Only one study reported results for psychological distress at intervention-end [SMD -0.51 (95% CI - 0.95, -0.07)],74 and no studies reported psychological distress data at 12-months from baseline, so no meta-analysis was possible for this outcome.
3.4.8. Quality of life (Global)
There was no evidence of a difference between intervention and comparator for global quality of life at intervention-end [Post intervention: SMD -0.06 (95% CI -0.51, 0.40; n=11; I2=94%); Change from baseline: SMD 0.19 (95% CI -0.03, 0.40; n=8; I2=60%)] (Figure 3) or at 12-months from baseline [Post intervention: SMD 0.12 (95% CI -0.04, 0.28; n=4; I2=0%); Change from baseline: SMD 0.00 (95% CI -0.16, 0.16; n=3; I2=0%)] (Figure S41). After excluding studies deemed to be at high risk of bias (n=7)57,63,69,74, there was still no evidence of a difference between intervention and comparator for global quality of life at intervention-end (Figure S44–45).
Figure 3.
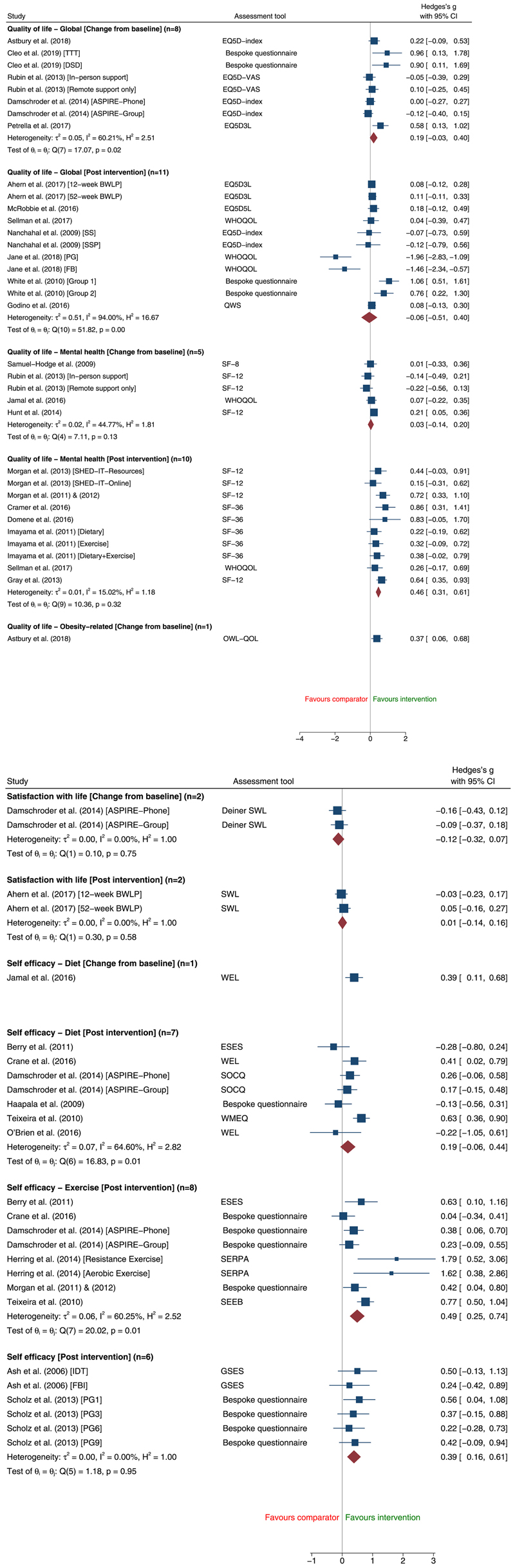
Changes in posivitely scaled mental health outcomes at intervention-end comparing adult behavioural weight management interventions with inactive, minimal or usual care comparator using random-effects pairwise meta-analysis. [Abbreviations: TTT: Ten Top Tips; DSD: Do Something Different; BWLP: Behavioural Weight Loss Programme; PG: Pamphlet Group; FB: Facebook Group; SS: Structured Support; SSP: Structured Support and Physical Activity; SHED-IT: Self-Help, Exercise, and Diet using Information Technology; IDT: Individualised dietetic treatment; FBI: Fat Boosters Incorporated; WHOQOL: World Health Organization Quality of Life; QWS: Quality of Well-being Scale; SF: Short Form; OWL-QOL: Obesity and Weight-Loss Quality of Life; SWL: Satisfaction with Life; WEL: Weight Efficacy Lifestyle Questionnaire; ESES: Exercise Self-Efficacy Scale; SOCQ: Stages of Change questionnaire; WMEQ: Weight Management Efficacy Questionnaire; SERPA: Self-Efficacy for Regulating Physical Activity; SEEB: Self-Efficacy for Exercise Behaviours; GSES: General Self-Efficacy Scale.]
Meta-regression identified that the substantial heterogeneity at intervention-end was explained by three interventions48,69 where 90-100% of intervention participants were women, or where the intervention consisted solely of provision of resources (Table S5). After excluding of the identified sources of heterogeneity, there was some evidence of an effect in favour of the intervention [SMD 0.06 (95% CI -0.06, 0.18; n=7; I2=0%)] (Figure S50).
3.4.9. Quality of life (Mental health-related)
Interventions were associated with improvements in mental health-related quality of life at intervention-end [Post intervention: SMD 0.46 (95% CI 0.31, 0.61; n=10; I2=15%); Change from baseline: SMD 0.03 (95% CI -0.14, 0.20; n=5; I2=45%)] (Figure 3) and at 12-months from baseline [Post intervention: SMD 0.29 (95% CI 0.09, 0.50; n=4; I2=0%)] (Figure S41). After excluding studies deemed to be at high risk of bias (n=4)54,55,63,74, there was evidence of an effect in favour of the intervention for mental health-related quality of life at intervention-end [Post intervention: SMD 0.45 (95% CI 0.28, 0.61; n=8; I2=14%); Change from baseline: SMD 0.15 (95% CI 0.03, 0.28; n=3; I2=0%)] (Figure S44–45).
Only one study reported change from baseline results for mental health-related quality of life at 12-months from baseline [SMD 0.04 (95% CI -0.11, 0.19)],73 so meta-analysis was not possible.
3.4.10. Quality of life (Obesity-related)
Only one study60 measured obesity-related quality of life with a positively scaled measure at intervention-end [SMD 0.37 (95% CI 0.06, 0.68)] and at 12-months from baseline [SMD 0.16 (95% CI -0.12, 0.44)], so meta-analysis could not be conducted.
There was no evidence of a difference between intervention and comparator for negatively scaled obesity-related quality of life at intervention-end [Post intervention: SMD 0.03 (95% CI -0.34, 0.28; n=3; I2= 54%)] (Figure 2). After excluding studies deemed to be at high risk of bias (n=1)51, there was some evidence of an effect in favour of the intervention for negatively scaled obesity-related quality of life at intervention-end [Post intervention: SMD -0.18 (95% CI -0.38, 0.01; n=2; I2= 0%)] (Figure S42–43). No studies reported negatively scaled obesity-related quality of life at 12-months from baseline, so meta-analysis was not possible.
3.4.11. Satisfaction with life
There was no evidence of a difference between intervention and comparator in satisfaction with life at intervention-end [Post intervention: SMD 0.01 (95% CI -0.14, 0.16; n=2; I2=0%); Change from baseline: SMD -0.12 (95% CI -0.32, 0.07; n=2; I2=0%)] (Figure 3). Effect estimates favoured the comparator for satisfaction with life at 12-months from baseline [Change from baseline: SMD -0.12 (95% CI -0.37, -0.18; n=2; I2=0%)] (Figure S41). No studies measuring satisfaction with life were deemed to be at high risk of bias.
3.4.12. Self-efficacy (General)
Effect estimates favoured intervention groups for general self-efficacy at intervention-end [Post intervention: SMD 0.39 (95% CI 0.16, 0.61; n=6; I2=0%)] (Figure 3) and at 12-months from baseline [Post intervention: SMD 0.35 (95% CI 0.13, 0.57; n=6; I2=0%)] (Figure S41).
After excluding studies deemed to be at high risk of bias (n=4)65, there was some evidence of an effect in favour of the intervention for general self-efficacy at intervention-end [Post intervention: SMD 0.37 (95% CI -0.08, 0.83; n=2; I2=0%)] (Figure S44–45).
3.4.13. Self-efficacy (Diet-related)
There was some evidence of an effect in favour of interventions for diet-related self-efficacy at intervention-end [Post intervention: SMD 0.19 (95% CI -0.06, 0.44; n=7; I2=65%)] (Figure 3) and at 12-months from baseline [Post intervention: SMD 0.26 (95% CI -0.04, 0.56; n=4; I2=71%)] (Figure S41), but there was substantial heterogeneity. Findings were unchanged following exclusion of studies deemed to be at high risk of bias (n=5)43,59,68,75,79 (Figure S44–45). There were insufficient studies to conduct meta-regression to identify sources of heterogeneity.
Only one study reported change from baseline results for diet-related self-efficacy at intervention-end [SMD 0.39 (95% CI 0.11, 0.68)],47 so meta-analysis was not possible.
3.4.14. Self-efficacy (Exercise-related)
Effect estimates favoured the interventions for exercise-related self-efficacy at intervention-end [Post intervention: SMD 0.49 (95% CI 0.25, 0.74; n=8; I2=60%)] (Figure 3) and at 12-months from baseline [Post intervention: SMD 0.47 (95% CI 0.15, 0.79; n=3; I2=71%)], but there was substantial heterogeneity. Findings were unchanged after exclusion of studies deemed to be at high risk of bias (n=4).54,55,68,75,79 There were insufficient studies to conduct meta-regression to identify sources of heterogeneity.
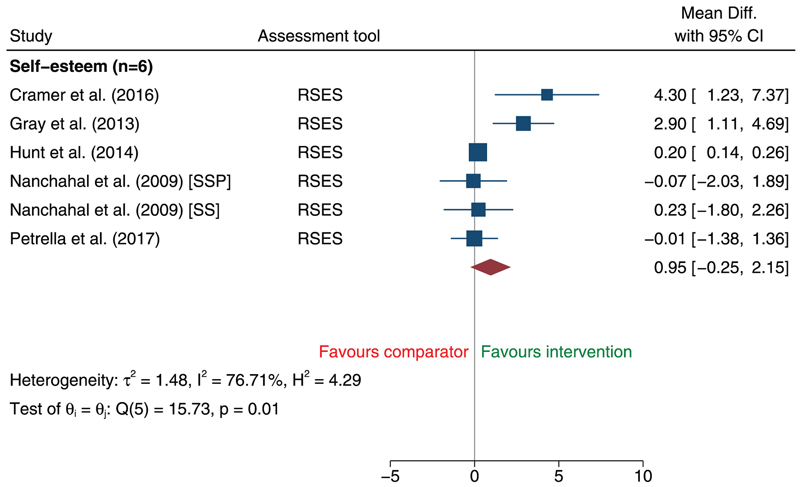
3.4.15. Self-esteem
There was no evidence of a difference between intervention and comparator groups for self-esteem at intervention-end [MD 0.95 (95% CI -0.25, 2.15; n=6; I2=77%)] (Figure 4). Findings were unchanged following exclusion of studies deemed to be at high risk of bias (n=2)57 (Figure S46). There were insufficient studies to conduct meta-regression to identify sources of heterogeneity. Only one study reported data for self-esteem at 12-months from baseline [SMD 0.57 (95% CI 0.41, 0.72)],73 so meta-analysis was not possible.
Figure 4.
Changes in [positively scaled] self-esteem at intervention-end comparing adult behavioural weight management interventions with inactive, minimal or usual care comparator using random-effects pairwise meta-analysis. [Abbreviations: SS: Structured Support; SSP: Structured Support and Physical Activity; RSES: Rosenberg self-esteem scale.]
3.4.16. Stress
There was no evidence of a difference between intervention and comparator for stress at intervention-end [Post intervention: SMD -0.03 (95% CI -0.40, 0.35; n=8; I2=77%)] (Figure 2). Findings were unchanged following exclusion of studies deemed to be at high risk of bias (n=3) (Figure S42–43). Only one study reported change from baseline results for stress at intervention-end [SMD -5.14 (95% CI - 6.34, -3.93)],70 and no studies reported stress at 12-months from baseline, so meta-analysis was not possible.
3.5. Additional analyses
Figure S51–S85 present the findings from stratified random-effects meta-analyses investigating the differential effects of pre-specified study, intervention and participant characteristics on pooled estimates for anxiety (post-intervention), depression (post-intervention), global quality of life (post-intervention/change from baseline), mental health-related quality of life (post-intervention), and exercise self-efficacy (post-intervention). There was no clear and consistent evidence that any of these characteristics explained heterogeneity in effect sizes. The remaining outcomes at intervention-end, and all outcomes at 12-month follow-up, did not have sufficient variability in any pre-specified characteristics to enable stratified analyses.
Contour-enhanced funnel plots of individual study effect sizes show high risk of publication bias across all outcomes (Figure S3–40).
4. Discussion
This comprehensive systematic review and meta-analysis found evidence suggesting that behavioural weight loss interventions result in greater improvements for a number of mental health outcomes compared to a minimal/inactive comparison group. At the end of the intervention, there was evidence to suggest greater improvements for depression, mental health-related quality of life, body image concerns, self-efficacy, exercise self-efficacy, and diet self-efficacy. At 12-months from baseline, evidence suggests improvements to depression, mental health-related quality of life, satisfaction with life, general self-efficacy, and exercise self-efficacy. Notably, this review found no evidence to suggest that interventions negatively impacted mental health relative to comparator groups. However, there was insufficient evidence to assess the impact on a large number of mental health domains at intervention-end (including binge-eating and psychological distress) and 12-month follow up (including anxiety, binge-eating, body image concerns, emotional eating, negative affect, psychological distress, obesity-related quality of life, self-esteem, and stress). Furthermore, findings should be interpreted with caution given the risk of bias of many studies and the possibility of publication bias.
Improvements in depression in favour of the behavioural interventions aligned with the findings of Fabricatore et al.25 and Peckmezian et al.17 A previous review by Baillot et al.22 found no evidence of an effect on depression following an exercise-only intervention, which is consistent with the stratified analysis in this review. Previous reviews assessing the impact of behavioural interventions on mental health-related quality of life found no effect for exercise-only behavioural interventions,22 and improvements in mental health-related quality of life for male-only interventions.33 We found evidence to suggest improvements in mental health-related quality of life at intervention-end and at 12-months from baseline. Stratified analysis suggested that exercise-only interventions are beneficial for mental health-related quality of life, contrasting with the findings of Balliot et al.22 Contrasting with previous evidence,22,27 we found evidence of improvements in body image following a behavioural weight loss intervention. This may be due to key differences in study participants (i.e. ≥25 kg/m2 vs. ≥30 kg/m2), study designs (e.g. inclusion of non-RCTs), or interventions studied (e.g. behavioural intervention vs. cognitive behaviour interventions). Consistent with previous reviews,22,27 we found no evidence of an effect of interventions on anxiety. However, there was significant heterogeneity for this outcome and after removal of a single study48 identified as the source of heterogeneity, the behavioural interventions were associated with a reduction in anxiety. This highlights the potential influence of study-, intervention- or participant characteristics on anxiety; insights into the differential effects of these characteristics is limited, however, due to the low number of heterogeneous studies.
To our knowledge, this is the first review to apply stratification techniques to investigate if effect estimates were influenced by study, participant or intervention characteristics. However, few outcomes had a sufficient number of contributing studies and variability in characteristics to permit these analyses to be conducted, and there were no clear and consistent findings. Suitably powered, high-quality trials are required to explore the differential effects of study, participant or intervention characteristics.
Many studies included in this review were deemed to be at high or unclear risk of bias. Common underlying reasons included selective reporting, allocation concealment, and incomplete data. Although sensitivity analyses showed minimal impact of high risk of bias studies on pooled estimates, these recurring weaknesses should be addressed to strengthen the evidence base. Incomplete data, selective reporting and biased publication increases the risk of review findings inheriting bias, consequently impacting the interpretation of findings and patient healthcare. In efforts to overcome this, study authors were contacted for missing data. Future studies should consistently adopt standards for trial reporting, such as the CONSORT recommendations,80 to improve study validity and credibility.81
Substantial heterogeneity was present for many outcomes in this review, hypothesised to be due to diversity in intervention types, populations under study, and measurement tools. Whilst there was no evidence of a difference between intervention and comparator for anxiety or global quality of life (with substantial heterogeneity present), pooled estimates suggested evidence of an effect in favour of the interventions for both outcomes when adjusted for heterogeneity. This suggests that substantial heterogeneity may impact the magnitude and/or direction of effect estimates. Identifying and adjusting for heterogeneity is challenging when research lacks the necessary detail of information, further highlighting the need for adherence to trial reporting recommendations.80
Despite previous reviews highlighting a need for more research,17,21–25,27,33 there remains a lack of high-quality behavioural weight loss intervention studies measuring and reporting mental health outcomes. Systematic reviews of effectiveness of behavioural weight loss intervention identified 58 RCTs82 in 2014 and 89 RCTs10 in 2018, whilst we identified only 42 trials that measured and reported mental health. It is essential to build a robust evidence base to comprehensively understand the impact of current interventions on mental health, and to identify how services may better support participants in the future. Future RCTs should investigate the impact of behavioural weight loss interventions on a broad variety of mental health outcomes, assessed repeatedly over longer durations, and compared to inactive comparison groups.
It is also important to note that we assessed the average effect of interventions on mental health. While evidence suggests that on average mental health outcomes improve following a behavioural intervention, it is likely that this is not the case for all participants. Future research should investigate whether the effect of interventions on mental health is different in different subgroups of participants and should seek to identify whether we can predict who might be at risk of adverse mental health effects.
4.1. Strengths and limitations
To our knowledge, this is the most up-to-date, comprehensive review investigating the effect of weight management interventions on a broad range of mental health outcomes in a representative sample of adults with overweight or obesity. Additionally, this review is the first to investigate whether particular intervention or study characteristics are more supportive of mental health. The methodological approach of this systematic review was rigorous and comprehensive. This review was strengthened by exclusively including RCTs, assessing a broad variety of mental health outcomes, and including adults that were representative of the general population with obesity. This review is further strengthened by comparing behavioural weight management interventions to inactive comparator groups or usual care, allowing the review to assess if providing an intervention is more supportive of mental health than not intervening. The impact on mental health was at assessed the end of the intervention to understand the immediate effects, and additionally at 12-months from baseline to explore the sustained effects. Finally, this review aligns with key recommendations for open science and reproducibility of meta-analyses.83 In particular, the review protocol was pre-registered and published, data and methods are comprehensively reported, PRISMA reporting guidelines adhered to,29 a librarian was consulted in the search strategy development and the authorship team included a statistician.
The review findings were limited by the scarcity of eligible evidence, and the high risk of bias in many included studies. Intervention trials rarely report mental health outcomes in title and abstracts; consequently, the screening process may not have identified all eligible studies. However, investigators conducted extensive hand-searching of reviews assessing other outcomes and study reference lists to maximise the inclusion of eligible studies. Review findings were further limited by poor reporting within studies which made it difficult to conduct stratified analyses and meta-regression for many outcomes.
Despite the comprehensive and inclusive eligibility criteria, the findings of this review are limited to the populations studied in the individual trials. Included studies had a high proportion of female participants and were conducted in middle-high or high-income countries; this is common for weight management interventions.84,85 Consequently, how interventions affect the mental health of male participants or adults with obesity in low-middle or low-income countries remains unclear, as does the impact of other characteristics not represented in the review.
5. Conclusion
This comprehensive and inclusive systematic review suggests that behavioural weight loss interventions result in improvements in a number of mental health outcomes, including body image concerns, depression, mental health-related quality of life, self-efficacy, exercise self-efficacy, and diet self-efficacy. This review found no evidence to suggest that interventions negatively impacted mental health, however there was insufficient evidence to assess the impact on a large number of mental health outcomes at intervention-end and beyond. The review contributes to a growing field of research and makes recommendations to strengthen future intervention studies. Specifically, future RCTs should ensure inclusion of a broad range of mental health outcomes, transparent reporting of findings, repeated measures over longer durations, and comparison with a suitable inactive comparator group. Larger, high-quality studies are required to provide sufficient statistical power to assess differential effects in participant subgroups and to investigate the influential components of interventions.
Supplementary Material
Acknowledgements
The authors would like to thank the University of Cambridge School of Clinical Medicine librarian, Eleanor Barker, for assistance in developing the search strategy, and the patient and public involvement (PPI) representatives who contributed to the development of this research.
Funding
RAJ, ERL, JMB, ALA, SJG and SJS are supported by the Medical Research Council (MRC) (Grant MC_UU_12015/4). The University of Cambridge has received salary support in respect of SJG from the National Health Service in the East of England through the Clinical Academic Reserve. EMFvS is supported by the Medical Research Council (MRC) (Grant MC_UU_12015/7). AOW is supported by the São Paulo Research Foundation (FAPESP) with a PhD scholarship and Research Internship Abroad (Grants 2019/24124-7 and 2018/19183-1). EH is supported by the Australian National Health and Medical Research Council (APP1156909).
Abbreviations
- RCT
Randomised controlled trials
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analysis
- BMI
Body Mass Index
- CI
Confidence interval
- SMD
Standardised mean difference
- MD
Mean difference
- CONSORT
Consolidated Standards of Reporting Trials.
Footnotes
PROSPERO registration number: CRD42019131659
Conflicts of interest: AA and SJG are the chief investigators on two publicly funded (MRC, NIHR) trials where the intervention is provided by WW (formerly Weight Watchers) at no cost outside the submitted work. RAJ, ERL, JMB, MP, AOW, EH, EMFS, and SJS have no conflicts of interest.
References
- 1.Fang X, Wei J, He X, et al. Quantitative association between body mass index and the risk of cancer: A global Meta-analysis of prospective cohort studies. Int J Cancer. 2018;143(7):1595–1603. doi: 10.1002/ijc.31553. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation. Obesity and overweight [Google Scholar]
- 3.National Institute for Health and Care Excellence. Obesity: Identification, Assessment and Management. Clinical Guideline [CG189] 2014 https://www.nice.org.uk/guidance/cg189/ [PubMed]
- 4.Flegal K, Kit B, Orpana H, Graubard B. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laxy M, Holle R, Döring A, Peters A, Hunger M. The longitudinal association between weight change and health-related quality of life: The KORA S4/F4 cohort study. Int J Public Health. 2014;59(2):279–288. doi: 10.1007/s00038-013-0506-x. [DOI] [PubMed] [Google Scholar]
- 6.Williams EP, Mesidor M, Winters K, Dubbert PM, Wyatt SB. Overweight and obesity: Prevalence, consequences, and causes of a growing public health problem. Curr Obes Rep. 2015;4:363–370. doi: 10.1007/s13679-015-0169-4. [DOI] [PubMed] [Google Scholar]
- 7.Rajan TM, Menon V. Psychiatric disorders and obesity: A review of association studies. J Postgrad Med. 2017;63(3):182–190. doi: 10.4103/jpgm.JPGM_712_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Avila C, Holloway AC, Hahn MK, et al. An overview of links between obesity and mental health. Curr Obes Rep. 2015;4(3):303–310. doi: 10.1007/s13679-015-0164-9. [DOI] [PubMed] [Google Scholar]
- 9.Ma C, Avenell A, Bolland M, et al. Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta-analysis. BMJ. 2017;359 doi: 10.1136/bmj.j4849. j4849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults updated evidence report and systematic review for the US preventive services task force. JAMA - J Am Med Assoc. 2018;320(11):1172–1191. doi: 10.1001/jama.2018.7777. [DOI] [PubMed] [Google Scholar]
- 11.Alhalel N, Schueller SM, O’Brien MJ. Association of changes in mental health with weight loss during intensive lifestyle intervention: does the timing matter? Obes Sci Pract. 2018;4(2):153–158. doi: 10.1002/osp4.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webber KH, Casey EM, Mayes L, Katsumata Y, Mellin L. A comparison of a behavioral weight loss program to a stress management program: A pilot randomized controlled trial. Nutrition. 2016;32(7-8):904–909. doi: 10.1016/j.nut.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fuller NR, Burns J, Sainsbury A, et al. Examining the association between depression and obesity during a weight management programme. Clin Obes. 2017;7(6):354–359. doi: 10.1111/cob.12208. [DOI] [PubMed] [Google Scholar]
- 14.Janney CA, Greenberg JM, Moin T, et al. Does mental health influence weight loss in adults with prediabetes? Findings from the VA Diabetes Prevention Program. Gen Hosp Psychiatry. 2018;53:32–37. doi: 10.1016/j.genhosppsych.2018.04.001. July-August 2018. [DOI] [PubMed] [Google Scholar]
- 15.Young MD, Morgan PJ. Effect of a gender-tailored ehealth weight loss program on the depressive symptoms of overweight and obese men: pre-post study. J Med Internet Res. 2018;20(1):1–7. doi: 10.2196/mental.8920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rand K, Vallis M, Aston M, et al. “It is not the diet; it is the mental part we need help with.” A multilevel analysis of psychological, emotional, and social well-being in obesity. Int J Qual Stud Health Well-being. 2017;12(1) doi: 10.1080/17482631.2017.1306421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peckmezian T, Hay P. A systematic review and narrative synthesis of interventions for uncomplicated obesity: weight loss, well-being and impact on eating disorder. J Eat Disord. 2017;5(15):212–213. doi: 10.1016/j.enfcli.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walls HL, Peeters A, Proietto J, McNeil JJ. Public health campaigns and obesity - A critique. BMC Public Health. 2011;11:1–7. doi: 10.1186/1471-2458-11-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pearl RL. Weight bias and stigma: public health implications and structural solutions. Soc Issues Policy Rev. 2018;12(1):146–182. doi: 10.1111/sipr.12043. [DOI] [Google Scholar]
- 20.Lazzeretti L. Assessment of psychological predictors of weight loss: How and what for? World J Psychiatry. 2015;5(1):56. doi: 10.5498/wjp.v5.i1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Booth AO, Wang X, Turner AI, Nowson CA, Torres SJ. Diet-induced weight loss has no effect on psychological stress in overweight and obese adults: A meta-analysis of randomized controlled trials. Nutrients. 2018;10(5) doi: 10.3390/nu10050613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baillot A, Saunders S, Brunet J, Romain AJ, Trottier A, Bernard P. A systematic review and meta-analysis of the effect of exercise on psychosocial outcomes in adults with obesity: A call for more research. Ment Health Phys Act. 2018;14:1–10. doi: 10.1016/j.mhpa.2017.12.004. [DOI] [Google Scholar]
- 23.Warkentin LM, Das D, Majumdar SR, Johnson JA, Padwal RS. The effect of weight loss on health-related quality of life: Systematic review and meta-analysis of randomized trials. Obes Rev. 2014;15(3):169–182. doi: 10.1111/obr.12113. [DOI] [PubMed] [Google Scholar]
- 24.Lasikiewicz N, Myrissa K, Hoyland A, Lawton CL. Psychological benefits of weight loss following behavioural and/or dietary weight loss interventions. A systematic research review. Appetite. 2014;72:123–137. doi: 10.1016/j.appet.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 25.Fabricatore A, Wadden T, Higginbotham A, et al. Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obes. 2011;35(11):1363–1376. doi: 10.1038/ijo.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blaine BE, Rodman J, Newman JM. Weight loss treatment and psychological well-being: A review and meta-analysis. J Health Psychol. 2007;12(1):66–82. doi: 10.1177/1359105307071741. [DOI] [PubMed] [Google Scholar]
- 27.Jacob A, Moullec G, Lavoie KL, et al. Impact of cognitive-behavioral interventions on weight loss and psychological outcomes: A meta-analysis. Heal Psychol. 2018;37(5):417–432. doi: 10.1037/hea0000576. [DOI] [PubMed] [Google Scholar]
- 28.Fruh SM. Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract. 2017;29:S3–S14. doi: 10.1002/2327-6924.12510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones RA, Lawlor ER, Griffin SJ, Van Sluijs EMF, Ahern AL. Impact of adult weight management interventions on mental health: a systematic review and meta-analysis protocol. BMJ Open. 2020;10(1):1–6. doi: 10.1136/bmjopen-2019-031857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hartmann-Boyce J, Johns DJ, Jebb SA, Summerbell C, Aveyard P. Behavioural weight management programmes for adults assessed by trials conducted in everyday contexts: Systematic review and meta-analysis. Obes Rev. 2014;15(11):920–932. doi: 10.1111/obr.12220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tronieri JS, Wadden TA, Chao AM, Tsai AG. Primary care interventions for obesity: review of the evidence. Curr Obes Rep. 2019;8(2):128–136. doi: 10.1007/s13679-019-00341-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Drew RJ, Morgan PJ, Pollock ER, Young MD. Impact of male-only lifestyle interventions on men’s mental health: A systematic review and meta-analysis. Obes Rev. 2020:1–16. doi: 10.1111/obr.13014. November 2019. [DOI] [PubMed] [Google Scholar]
- 34.Hartmann-Boyce J, Johns DJ, Jebb SA, et al. Effect of behavioural techniques and delivery mode on effectiveness of weight management: Systematic review, meta-analysis and meta-regression. Obes Rev. 2014;15(7):598–609. doi: 10.1111/obr.12165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Higgins J, Thomas J, Chandler J, et al., editors. The Cochrane Public Health Group. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0. The Cochrane Collaboration; 2019. Updated July 2019 www.training.cochrane.org/handbook. [Google Scholar]
- 36.StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC; 2019. [Google Scholar]
- 37.Ahern AL, Wheeler GM, Aveyard P, et al. Extended and standard duration weight-loss programme referrals for adults in primary care (WRAP): a randomised controlled trial. Lancet. 2017;389:2214–2225. doi: 10.1016/s0140-6736(17)30647-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alfaris N, Wadden TA, Sarwer DB, et al. Effects of a 2-year behavioral weight loss intervention on sleep and mood in obese individuals treated in primary care practice. Obesity. 2015;23(3):558–564. doi: 10.1002/oby.20996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Damschroder LJ, Lutes LD, Kirsh S, et al. Small-changes obesity treatment among veterans: 12-month outcomes. Am J Prev Med. 2014;47(5):541–553. doi: 10.1016/j.amepre.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 40.Domene PA, Moir HJ, Pummell E, Knox A, Easton C. The health-enhancing efficacy of Zumba® fitness: An 8-week randomised controlled study. J Sports Sci. 2016;34(15):1396–1404. doi: 10.1080/02640414.2015.1112022. [DOI] [PubMed] [Google Scholar]
- 41.Godino JG, Merchant G, Norman GJ, Donohue MC, Marshall SJ, et al. Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): a 2-year parallel group randomized controlled trial. Lancet Diabetes Endocrinol. 2016;4(9):747–755. doi: 10.1016/S2213-8587(16)30105-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gray CM, Hunt K, Mutrie N, Anderson AS, Treweek S, Wyke S. Weight management for overweight and obese men delivered through professional football clubs: A pilot randomized trial. Int J Behav Nutr Phys Act. 2013;10(121):1–17. doi: 10.1186/1479-5868-10-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: A 1-year effectiveness study. Public Health Nutr. 2009;12(12):2382–2391. doi: 10.1017/S1368980009005230. [DOI] [PubMed] [Google Scholar]
- 44.Herring LY, Wagstaff C, Scott A. The efficacy of 12 weeks supervised exercise in obesity management. Clin Obes. 2014;4:220–227. doi: 10.1111/cob.12063. [DOI] [PubMed] [Google Scholar]
- 45.Huber JM, Shapiro JS, Wieland ML, et al. Telecoaching plus a portion control plate for weight care management: A randomized trial. Trials. 2015;16(323):1–9. doi: 10.1186/s13063-015-0880-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Imayama I, Alfano CM, Kong A, et al. Dietary weight loss and exercise interventions effects on quality of life in overweight/obese postmenopausal women: A randomized controlled trial. Int J Behav Nutr Phys Act. 2011;8(1):118. doi: 10.1186/1479-5868-8-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jamal SN, Moy FM, Mohamed MNA, Mukhtar F. Effectiveness of a group support lifestyle modification (GSLiM) programme among obese adults in workplace: A randomised controlled trial. PLoS One. 2016;11(8):1–22. doi: 10.1371/journal.pone.0160343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jane M, Foster J, Hagger M, Ho S, Kane R, Pal S. Psychological effects of belonging to a Facebook weight management group in overweight and obese adults: Results of a randomised controlled trial. Heal Soc Care Community. 2018;26:714–724. doi: 10.1111/hsc.12584. [DOI] [PubMed] [Google Scholar]
- 49.Ash S, Reeves M, Bauer J, et al. A randomised control trial comparing lifestyle groups, individual counselling and written information in the management of weight and health outcomes over 12 months. Int J Obes. 2006;30(10):1557–1564. doi: 10.1038/sj.ijo.0803263. [DOI] [PubMed] [Google Scholar]
- 50.Kalarchian MA, Marcus MD, Courcoulas AP, Cheng Y, Levine MD. Preoperative lifestyle intervention in bariatric surgery: Initial results from a randomized, controlled trial. Obesity. 2013;21(2):254–260. doi: 10.1002/oby.20069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kraschnewski JL, Stuckey HL, Rovniak LS, et al. Efficacy of a weight-loss website based on positive deviance: A randomized trial. Am J Prev Med. 2011;41(6):610–614. doi: 10.1016/j.amepre.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Laing BY, Mangione CM, Tseng CH, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients. Ann Intern Med. 2014;161:S5–S12. doi: 10.7326/M13-3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McRobbie H, Hajek P, Peerbux S, et al. Tackling obesity in areas of high social deprivation: Clinical effectiveness and cost-effectiveness of a task-based weight management group programme – A randomised controlled trial and economic evaluation. Health Technol Assess (Rockv) 2016;20(79) doi: 10.3310/hta20790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morgan PJ, Collins CE, Plotnikoff RC, et al. Efficacy of a workplace-based weight loss program for overweight male shift workers: The Workplace POWER (Preventing Obesity Without Eating like a Rabbit) randomized controlled trial. Prev Med (Baltim) 2011;52:317–325. doi: 10.1016/j.ypmed.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 55.Morgan PJ, Collins CE, Plotnikoff RC, et al. The impact of a workplace-based weight loss program on work-related outcomes in overweight male shift workers. J Occup Environ Med. 2012;54(2):122–127. doi: 10.1097/JOM.0b013e31824329ab. [DOI] [PubMed] [Google Scholar]
- 56.Morgan PJ, Callister R, Collins CE, et al. The SHED-IT community trial: A randomized controlled trial of internet- and paper-based weight loss programs tailored for overweight and obese men. Ann Behav Med. 2013;45(2):139–152. doi: 10.1007/s12160-012-9424-z. [DOI] [PubMed] [Google Scholar]
- 57.Nanchahal K, Townsend J, Letley L, Haslam D, Wellings K, Haines A. Weight-management interventions in primary care: A pilot randomised controlled trial. Br J Gen Pract. 2009:e157–166. doi: 10.3399/bjgp09X420617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nurkkala M, Kaikkonen K, Vanhala ML, Karhunen L, Keränen AM, Korpelainen R. Lifestyle intervention has a beneficial effect on eating behavior and long-term weight loss in obese adults. Eat Behav. 2015;18:179–185. doi: 10.1016/j.eatbeh.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 59.O’Brien T, Jenkins C, Amella E, Mueller M, Moore M, Hathaway D. An internet-assisted weight loss intervention for older overweight and obese rural women: a feasibility study. CIN - Comput Informatics Nurs. 2016;34(11):513–519. doi: 10.1097/CIN.0000000000000275. [DOI] [PubMed] [Google Scholar]
- 60.Astbury NM, Aveyard P, Nickless A, et al. Doctor referral of overweight people to low energy total diet replacement treatment (DROPLET): pragmatic randomised controlled trial. BMJ. 2018;362:1–10. doi: 10.1136/bmj.k3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Petrella RJ, Gill DP, Zou G, et al. Hockey fans in training: a pilot pragmatic randomized controlled trial. Med Sci Sports Exerc. 2017;49(12):2506–2516. doi: 10.1249/MSS.0000000000001380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rshikesan PB, Subramanya P, Nidhi R. Yoga practice for reducing the male obesity and weight related psychological difficulties - A randomized controlled trial. J Clin Diagnostic Res. 2016;10(11):22–28. doi: 10.7860/JCDR/2016/22720.8940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rubin RR, Peyrot M, Wang NY, et al. Patient-reported outcomes in the practice-based opportunities for weight reduction (POWER) trial. Qual Life Res. 2013;22(9):2389–2398. doi: 10.1007/s11136-013-0363-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Samuel-Hodge CD, Johnston LF, Gizlice Z, et al. Randomized trial of a behavioral weight loss intervention for low-income women: The weight wise program. Obesity. 2009;17(10):1891–1899. doi: 10.1038/oby.2009.128. [DOI] [PubMed] [Google Scholar]
- 65.Scholz U, Ochsner S, Luszczynska A. Comparing different boosters of planning interventions on changes in fat consumption in overweight and obese individuals: a randomised controlled trial. Int J Psychol. 2013;48(4):604–615. doi: 10.1080/00207594.2012.661061. [DOI] [PubMed] [Google Scholar]
- 66.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. Daily self-weighing and adverse psychological outcomes: A randomized controlled trial. Am J Prev Med. 2014;46(1):24–29. doi: 10.1016/j.amepre.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tapsell LC, Lonergan M, Batterham MJ, et al. Effect of interdisciplinary care on weight loss: A randomised controlled trial. BMJ Open. 2017;7:1–12. doi: 10.1136/bmjopen-2016-014533. e014533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Teixeira PJ, Silva MN, Coutinho SR, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity. 2010;18(4):725–735. doi: 10.1038/oby.2009.281. [DOI] [PubMed] [Google Scholar]
- 69.White C, Drummond S, De Looy A. Comparing advice to decrease both dietary fat and sucrose, or dietary fat only, on weight loss, weight maintenance and perceived quality of life. Int J Food Sci Nutr. 2010;61(3):282–294. doi: 10.3109/09637480903397355. [DOI] [PubMed] [Google Scholar]
- 70.Xenaki N, Bacopoulou F, Kokkinos A, Nicolaides NC, Chrousos GP, Darviri C. Impact of a stress management program on weight loss, mental health and lifestyle in adults with obesity: a randomized controlled trial. J Mol Biochem. 2018;7:78–84. [PMC free article] [PubMed] [Google Scholar]
- 71.Barnes RD, White MA, Martino S, Grilo CM. A randomized controlled trial comparing scalable weight loss treatments in primary care. Obesity. 2014;22(12):2508–2516. doi: 10.1002/oby.20889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jebb SA, Ahern AL, Olson AD, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: A randomised controlled trial. Lancet. 2011;378(9801):1485–1492. doi: 10.1016/S0140-6736(11)61344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hunt K, Wyke S, Gray CM, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): A pragmatic randomised controlled trial. Lancet. 2014;383(9924):1211–1221. doi: 10.1016/S0140-6736(13)62420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sellman D, Schroder R, Deering D, Elmslie J, Foulds J, Frampton C. Psychosocial enhancement of the Green Prescription for obesity recovery: a randomised controlled trial. N Z Med J. 2017;130(1450):44–54. [PubMed] [Google Scholar]
- 75.Berry D, Colindres M, Sanchez-Lugo L, Sanchez M, Neal M, Smith-Miller C. Adapting, feasibility testing, and pilot testing a weight management intervention for recently immigrated Spanish-speaking women and their 2- to 4-year-old children. Hisp Heal Care Int. 2011;9(4):186–193. doi: 10.1891/1540-4153.9.4.186. [DOI] [Google Scholar]
- 76.Camolas J, Santos O, Moreira P, do Carmo I. INDIVIDUO: Results from a patient-centered lifestyle intervention for obesity surgery candidates. Obes Res Clin Pract. 2017;11:475–488. doi: 10.1016/j.orcp.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 77.Cleo G, Glasziou P, Beller E, Isenring E, Thomas R. Habit-based interventions for weight loss maintenance in adults with overweight and obesity: a randomized controlled trial. Int J Obes. 2019;43(2):374–383. doi: 10.1038/s41366-018-0067-4. [DOI] [PubMed] [Google Scholar]
- 78.Cramer H, Thoms MS, Anheyer D, Lauche R, Dobos G. Yoga in women with abdominal obesity - a randomized controlled trial. Dtsch Arztebl Int. 2016;113:645–652. doi: 10.3238/arztebl.2016.0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Crane MM, Ward DS, Lutes LD, Bowling JM, Tate DF. Theoretical and behavioral mediators of a weight loss intervention for men. Ann Behav Med. 2016;50:460–470. doi: 10.1007/s12160-016-9774-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kane RL, Wang J, Garrard J. Reporting in randomized clinical trials improved after adoption of the CONSORT statement. J Clin Epidemiol. 2007;60(3):241–249. doi: 10.1016/j.jclinepi.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 82.Williams RL, Wood LG, Collins CE, Callister R. Effectiveness of weight loss interventions - is there a difference between men and women: A systematic review. Obes Rev. 2015;16(2):171–186. doi: 10.1111/obr.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lakens D, Hilgard J, Staaks J. On the reproducibility of meta-analyses: Six practical recommendations. BMC Psychol. 2016;4(1):1–10. doi: 10.1186/s40359-016-0126-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity. 2012;20(6):1234–1239. doi: 10.1038/oby.2011.140. [DOI] [PubMed] [Google Scholar]
- 85.Ford ND, Patel SA, Narayan KMV. Obesity in low- and middle-income countries: burden, drivers, and emerging challenges. Annu Rev Public Health. 2017;38(1):145–164. doi: 10.1146/annurev-publhealth-031816-044604. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.