Summary
Background
In 2003 severe acute respiratory syndrome (SARS) affected 1755 people in Hong Kong, including 386 health care professionals, some of whom were infected during resuscitation attempts of affected patients. This study seeks to explore whether this epidemic has altered the willingness of Hong Kong medical students to perform basic life support and mouth-to-mouth ventilation during an out-of-hospital cardiac arrest.
Methods
A questionnaire was used to survey Year 4 medical students at the end of their undergraduate anaesthesia attachment, during which basic life support (BLS) skills were taught. The survey was conducted during July and August 2003, approximately two months after Hong Kong was removed from the World Health Organisation SARS Infected Areas list, and was designed to examine student confidence in BLS skills, their perceptions of the risks associated with performing BLS and their willingness to perform BLS in varying situations.
Results
The response rate was over 60% (35 from a possible 54). Students were positive regarding the adequacy of their BLS training. They were concerned about disease transmission during resuscitation but were less positive regarding whether the risks had increased due to SARS. In all situations they were significantly more likely to perform mouth-to-mouth ventilation for a family member compared with a stranger (p < 0.001) and to withhold mouth-to-mouth ventilation if either vomit or blood were present in the victim's mouth.
Conclusions
Hong Kong medical students feel able to perform BLS if required. They are concerned about the risk of disease transmission, including SARS, during resuscitation, but would be more likely to withhold mouth-to-mouth resuscitation in the presence of vomit or blood than due to a fear of contracting SARS.
Keywords: Basic life support (BLS), Infection, Safety
1. Introduction
Concern regarding the spread of communicable diseases is a well recognized cause of reluctance on the part of bystanders to perform basic life support (BLS) for a victim during an out-of-hospital cardiac arrest [1], [2], [3], [4], [5]. Many of the previous studies investigating this issue have indicated that respondees are more reluctant to perform mouth-to-mouth ventilation than chest compressions, and have highlighted rescuers’ fears regarding transmission of the human immunodeficiency virus (HIV) in particular as a reason for not performing BLS. These features appear to apply to both medically trained and lay rescuers. Other factors that have been found to affect rescuers’ attitudes to BLS include fear of litigation, aesthetic considerations and lack of confidence in BLS skills.
In late 2002, a previously unknown communicable disease with a high mortality rate emerged in China, spreading initially to neighbouring Asian countries and then globally by early 2003. As it caused severe breathing difficulties in affected patients it was named severe acute respiratory syndrome (SARS) and was later found to be caused by a coronavirus, the SARS-associated coronavirus (SARS-CoV), which spreads by close person-to-person contact and by droplet spread. In the 2003 SARS outbreak in Hong Kong, 1755 people contracted the disease, 386 of whom were healthcare workers or medical students (22%). In Hong Kong a total of 299 people died from SARS giving a mortality rate of 17% [6], [7]. Six healthcare workers died of SARS, and according to the coroner's report, two of them probably contracted the disease during the resuscitation attempt of a patient known to be suffering from SARS.
In the light of this and because SARS caused widespread fear and anxiety throughout both the Hong Kong medical and lay communities, we sought to explore whether the 2003 SARS outbreak in Hong Kong altered the willingness of our medical students to perform BLS and, in particular, mouth-to-mouth ventilation.
2. Materials and methods
Hong Kong University has a 5-year undergraduate medical curriculum which emphasises problem-based and self-directed learning. We used a questionnaire to survey those Year 4 medical students who completed their anaesthesiology attachment during July and August 2003 and had undergone clinical skills training in advanced life support at this time. This was approximately one third of the class. All questionnaires were therefore completed within two months following the removal of Hong Kong from the World Health Organisation's SARS Infected Areas list. All student participation was voluntary and the survey was approved by our institutional ethics committee.
The questionnaire was designed to examine three main areas: (1) student confidence in performing BLS skills; (2) student perceptions of risk associated with performing BLS; (3) student willingness to perform BLS in various situations. The first section of the questionnaire consisted of 25 statements to which the students were asked to select a response from a five-point Likert rating scale: 5, strongly agree; 4, agree; 3, neither agree nor disagree; 2, disagree; 1, strongly disagree. This was followed by four hypothetical out-of-hospital cardiac arrest situations involving (a) an adult stranger; (b) an elderly stranger; (c) a child who is a stranger; and (d) a family member, and the students were asked if they would definitely, probably, probably not, or definitely not, provide various resuscitation interventions during these situations. For each of the four patient types they were also asked if the SARS outbreak had made any difference to the likelihood that they would now perform mouth-to-mouth ventilation during resuscitation. The final section consisted of a list of eight possible reasons that might prevent the performance of mouth-to-mouth ventilation; fear of SARS; fear of HIV; fear of other infections; fear of being sued; fear of failure; fear of vomitus; mouth-to-mouth ventilation is unpleasant; mouth-to-mouth ventilation is not useful. The students were asked to indicate which, if any, of these reasons would stop them from performing mouth-to-mouth ventilation. Multiple responses were allowed.
Statistical analysis was performed using SPSS for Windows, Release 12.0.0 (SPSS Inc., USA). χ 2 was used for categorical data and the Mann–Whitney U and Wilcoxin signed rank tests for ordinal data. McNemar's test was used to compare proportions. For multi-variant analysis the Friedman test was used.
3. Results
A total of 35 questionnaires were completed and returned (65% of 54 distributed). Seventeen respondents were male (49%) and 18 were female (51%). All the students were between the ages of 20–29 years and none of them had ever performed either chest compressions or mouth-to-mouth ventilation in a real resuscitation situation before. Table 1 shows the students’ opinions regarding their performance of BLS. Nineteen students (54%) agreed or strongly agreed that they had received adequate training to enable them to perform BLS competently. However, only 34% of the students felt confident about performing BLS if required and the vast majority (94%) would like more practice before performing it in a real situation. Despite this, 57% of the students disagreed or strongly disagreed with the statement that medical students are not qualified to perform BLS during a real cardiac arrest situation. The students were asked if they found chest compressions and mouth-to-mouth ventilation easy skills to perform, but although 34% of the students felt that chest compressions are easy to perform whereas only 26% considered performing mouth-to-mouth ventilation to be easy, the differences in perception of the ease or difficulty of both skills were not significant (p = 0.16, S = 2.0). Student opinion as to whether mouth-to-mouth ventilation is an efficient way of delivering oxygen was neutral (Table 1). However, the majority of students (85%) disagreed or strongly disagreed that the option of performing only chest compressions was as effective as performing both chest compressions and mouth-to-mouth ventilation during a cardiorespiratory arrest. In addition, 48% of the students felt that it is morally wrong to withhold mouth-to-mouth ventilation if you are trained to do it.
Table 1.
Student opinions regarding the performance of BLS
| Percentage of students |
|||||
|---|---|---|---|---|---|
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | |
| I have received adequate training to enable me to perform BLS competently | 11 | 43 | 32 | 11 | 3 |
| I would feel confident in performing BLS should the need arise | 8 | 26 | 40 | 20 | 6 |
| I would like more practice at BLS before I have to perform it in a real situation | 57 | 37 | 3 | 3 | 0 |
| Medical students are not qualified to perform BLS in an out-of-hospital cardiac arrest | 3 | 17 | 23 | 46 | 11 |
| Chest compressions are easy to perform | 6 | 28 | 23 | 37 | 6 |
| Mouth-to-mouth ventilation is easy to perform | 6 | 20 | 23 | 43 | 8 |
| Mouth-to-mouth ventilation is an efficient way to provide oxygen for the patient | 0 | 31 | 31 | 38 | 0 |
| Performing chest compressions only is as effective as performing both chest compressions and mouth-to-mouth ventilation | 0 | 12 | 3 | 53 | 32 |
Twenty-seven students (13 male; 14 female) or 77%, were concerned regarding disease transmission to the rescuer during BLS (Table 2 ). Whereas previous studies have found HIV transmission to be the greatest perceived risk to the rescuer during BLS, 68% of our student responders either disagreed or strongly disagreed that HIV is a greater risk to the rescuer than SARS (Table 2). Performing mouth-to-mouth ventilation was thought to be a significantly more risky behaviour than performing chest compressions, as illustrated by the majority of students (68%) who considered the risk of transmission of infection to the rescuer from performing chest compressions to be low compared to only 26% who thought that the risk from performing mouth-to-mouth ventilation was low (p = 0.002; S = 9.3) (Table 2). Most students (71%) stated that the SARS outbreak had affected their opinion regarding the safety of mouth-to-mouth ventilation for the rescuer. However, when asked if the risk of disease transmission from mouth-to-mouth ventilation was higher after the SARS outbreak than it had been before, their responses were split fairly evenly between agreeing (52%) and disagreeing (40%), with very few neutral responses (8%) (Table 2). Nearly all of the students (100% and 80%, respectively) denied that the fear of SARS would prevent them from performing chest compressions in the situations of (a) resuscitating a family member or (b) resuscitating a stranger. However, although small, the differences in the student responses regarding willingness to perform chest compressions for family members and strangers were significant (p < 0.001; Z = −3.6) (Fig. 1a). Student opinion regarding the performance of mouth-to-mouth ventilation was much more divided. Whereas 100% of the student respondents indicated that the fear of SARS would not prevent them from performing mouth-to-mouth ventilation for a family member, only 54% stated this in regard to strangers while 37% claimed that it would prevent them from performing mouth-to-mouth ventilation in this situation (p < 0.001; Z = −4.3) (Fig. 1b). In addition, regarding the resuscitation of strangers only, the students claimed to be significantly more likely to withhold the performance of mouth-to-mouth ventilation due to a fear of SARS than they were to withhold chest compressions (p < 0.001; Z = −4.0).
Table 2.
Student perceptions regarding the risks to the rescuer from performing BLS
| Percentage of students |
|||||
|---|---|---|---|---|---|
| Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree | |
| I am concerned about disease transmission to the rescuer during BLS | 11 | 66 | 17 | 6 | 0 |
| The risk from performing chest compressions is low | 17 | 51 | 12 | 14 | 6 |
| The risk from performing mouth-to-mouth ventilation is low | 0 | 26 | 14 | 40 | 20 |
| The risk of infection transmission during mouth-to-mouth ventilation is greater now than it was before the SARS epidemic | 9 | 43 | 8 | 34 | 6 |
| The SARS epidemic has had no effect on my opinion regarding the safety of mouth-to-mouth ventilation | 3 | 23 | 3 | 54 | 17 |
| HIV is a greater risk to the rescuer than SARS during BLS | 0 | 3 | 29 | 37 | 31 |
Fig. 1.
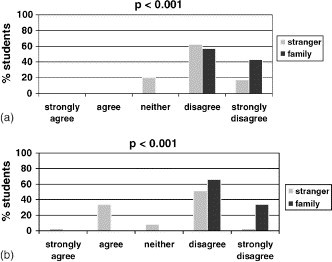
Student responses to the question: (a) the fear of contracting SARS would stop me from performing chest compressions for a stranger/family member; (b) the fear of contracting SARS would stop me from performing mouth-to-mouth ventilation for a stranger/family member.
However, the effect of the fear of SARS in causing student reluctance to perform mouth-to-mouth ventilation is less than the effect of the presence of either vomit or blood in the victim's mouth. Fig. 2a compares these effects on student willingness to perform mouth-to-mouth ventilation for strangers, and shows that both the presence of vomit and the presence of blood in the victim's mouth have a significantly greater effect than the fear of SARS (vomit versus SARS: p < 0.001, Z = −3.2; blood versus SARS: p < 0.001, Z = −3.6), although there is no significant difference in the effect of the presence of vomit compared with the presence of blood (p = 0.9, Z = −0.1). Similar results were obtained when these three factors were compared regarding the resuscitation of family members (Fig. 2b).
Fig. 2.
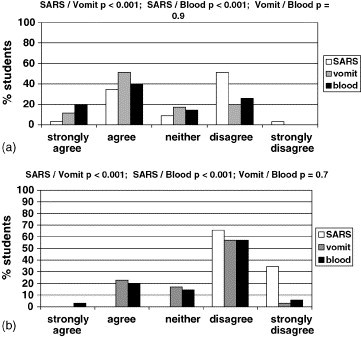
Student responses to the question: (a) regarding strangers: (1) the fear of SARS; (2) the presence of vomit; (3) the presence of blood in the victim's mouth would stop me from performing mouth-to-mouth ventilation; (b) regarding family members: (1) the fear of SARS; (2) the presence of vomit; (3) the presence of blood in the victims mouth would stop me from performing mouth-to-mouth ventilation.
When considering the four different patient types, the students were significantly more likely to perform both skills for family members compared to any of the other groups (p ≤ 0.001; χ 2 = 13.6–25.7), but there were no significant differences in the responses comparing each group of strangers to each other (Fig. 3 ). Performing no basic life support at all was not a popular option for the majority (80–86%) of our students regardless of the type of patient they were resuscitating. The SARS outbreak has, for the majority (89%), made no difference to the student likelihood of performing mouth-to-mouth ventilation for family members (Fig. 4 ). The responses for each of the stranger groups were similar to each other with no significant difference between any of the groups and were mainly split between the SARS outbreak having made (a) no difference to the likelihood that the students would perform mouth-to-mouth ventilation (46–54%) and (b) a decrease in the likelihood that the students would perform mouth-to-mouth ventilation (29–37%) for these patient types (Fig. 4). A constant 17% of students claimed that they would now be more likely to perform mouth-to-mouth ventilation for each of the stranger groups than they would have been before the SARS outbreak.
Fig. 3.
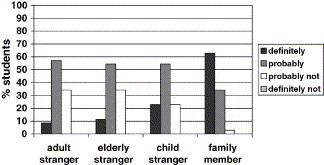
Student responses to the statement: I would perform chest compressions and mouth-to-mouth ventilation during an out-of-hospital cardiac arrest resuscitation. Family member/adult stranger; p < 0.001, χ2 = 25.7. Family member/elderly stranger; p < 0.001, χ2 = 23.3. Family member/child stranger; p = 0.001, χ2 = 13.6. Adult stranger/elderly stranger; p = 0.92, χ2 = 0.17. Adult stranger/child stranger; p = 0.21, χ2 = 3.19. Elderly stranger/child stranger; p = 0.34, χ2 = 2.13.
Fig. 4.
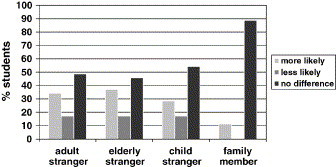
Student responses to the question: before the SARS outbreak I would have been more or less likely than I am now to perform mouth-to-mouth ventilation. Family member/adult stranger; p < 0.001, χ2 = 14.1. Family member/elderly stranger; p < 0.001, χ2 = 15.6. Family member/child stranger; p = 0.003, χ2 = 11.4. Adult stranger/elderly stranger; p = 0.97, χ2 0.07. Adult stranger/child stranger; p = 0.86, χ2 = 0.29. Elderly stranger/child stranger; p = 0.72, χ2 = 0.64.
In the final section of the questionnaire, the two most common reasons indicated by the students that would prevent performance of mouth-to-mouth ventilation were fear of SARS (74%) and fear of vomitus (66%). Only 6% of students felt that they would not perform mouth-to-mouth ventilation because it is not useful. There was a significant male:female divide. Male students were significantly more concerned regarding HIV than female students (p = 0.03, χ 2 = 4.9) who in turn were more concerned with the fear of failure (p = 0.01, χ 2 = 6.7) and the unpleasant nature of mouth-to-mouth ventilation (p < 0.01, χ 2 = 7.1) (Fig. 5 ).
Fig. 5.
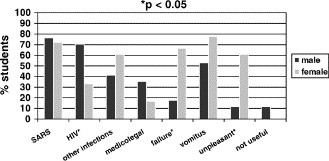
Students’ reasons for not performing mouth-to-mouth ventilation—a comparison of the sexes.
4. Discussion
The majority of students who participated in this study were concerned about disease transmission to the rescuer during BLS, and considered the performance of mouth-to-mouth ventilation to constitute a significantly greater risk to the rescuer than the performance of chest compressions. Many previous studies have investigated the willingness of bystanders and healthcare workers to perform mouth-to-mouth ventilation in various scenarios involving both family members and strangers [1], [2], [3], [4], [5] and the majority of these have highlighted the fear of HIV transmission as a major reason for rescuer reluctance to perform mouth-to-mouth ventilation [1], [2], [3]. Our students were also concerned regarding the transmission of HIV with, interestingly, the males being significantly more concerned than the female students. Although the reasons as to why this should be were beyond the scope of our study, it is possible that this reflects the fact that, in Hong Kong, HIV predominantly affects adult heterosexual males [8]. However, the majority of students felt that the SARS infection was an even greater risk to the rescuer than HIV. This may be true. Both, the American Heart Association and the Resuscitation Council (UK) state that, although in theory HIV transmission can occur during mouth-to-mouth ventilation, the risk is minimal [9], [10]. With current levels of knowledge it is difficult to state accurately the risk of transmission of SARS-CoV virus during mouth-to-mouth ventilation, but since it is known to be transmitted by contaminated droplets, this seems a plausible route. In the early stages of the SARS outbreak in Hong Kong, there was a widely reported resuscitation attempt of a known SARS patient, which resulted in two members of the resuscitation team fatally contracting SARS despite wearing the full recommended personal protective equipment and using a bag-valve-mask for ventilation. Following this several Hong Kong hospitals, including our own, put together guidelines for safer resuscitation which recommended the use of viral filters on the expiratory limb of the breathing system used. In the case of bag-valve-mask systems the filter was attached to the valve using a PEEP connector. We did not include questions in our survey regarding the use of such viral filters, or the use of barrier masks, to protect the rescuer during mouth-to-mouth ventilation, but the use of such devices may help to decrease rescuer reluctance to ventilate cardiac arrest patients. Hew, Brenner and Kaufman, investigating the reluctance of paramedics and emergency medical technicians to perform mouth-to-mouth resuscitation, found that the availability of barrier masks increased the likelihood of mouth-to-mouth ventilation performance dramatically [3]. Further study is required to elucidate whether or not barrier masks and viral filters actually do protect the rescuer from SARS-CoV infection during mouth-to-mouth and bag-valve-mask ventilation. In theory, both the barrier masks and the viral filters are effective at removing both viral and bacterial particles from the gas filtering through them and should, therefore, prevent environmental contamination by the viral particles present in the droplets from the patient's respiratory tract. However, filtration of all contaminants will only occur if a perfect seal between the mask and the patient's face is maintained at all times. Safe disposal of a contaminated barrier mask is also important as the SARS-CoV virus can survive on surfaces for several hours [11]. At present it is not known whether or not there is a ‘safe’ level of environmental contamination less than which the risk of SARS transmission is negligible. Given the high mortality rate of this infection, however, it seems sensible to aim for zero contamination.
Many (71%) of our students asserted that the SARS outbreak had affected their opinion regarding the safety of mouth-to-mouth ventilation for the rescuer. While the majority (89%) indicated that SARS has made no difference to the likelihood of them performing mouth-to-mouth ventilation for a family member, 11% claimed that they would have been more likely to do this for a family member before the SARS outbreak had occurred. Regarding the three groups of strangers (adult, elderly and child) 29–37% claimed that they would have been more likely to do mouth-to-mouth ventilation before the SARS outbreak, but surprisingly 17% stated that they would be more likely to do it afterwards. This may be because SARS has heightened awareness of the need for mouth-to-mouth ventilation, or perhaps they did not understand the question. Interestingly and in contrast to previous studies, our students did not greatly differentiate between children and adults regarding their willingness to provide mouth-to-mouth ventilation [12]. This may be because in Hong Kong children have a very low prevalence of HIV infection [8], which was the primary concern for rescuers previously, whereas it is perceived that anyone, including children, can suffer from SARS. In reality, children were only rarely infected during the 2003 SARS outbreak [13].
The chest compression only option for BLS is mentioned to the students during their teaching regarding resuscitation, but it has not before now been greatly emphasized. Provision of prompt BLS, including mouth-to-mouth ventilation, has been shown to be beneficial in improving survival following an out-of-hospital cardiac arrest [14], [15], [16], and our teaching has closely followed the guidelines of the European Resuscitation Council (ERC) in which both chest compressions and mouth-to-mouth ventilation constitute an important aspect of the chain of survival [10]. This may explain why very few (6%) students indicated that they would withhold mouth-to-mouth ventilation because they felt it was ‘not useful’. Recent evidence concerning bystander BLS for out-of-hospital cardiac arrests has, however, questioned the need for mouth-to-mouth ventilation. Van Hoeyweghen et al. [17] found that long term survival following ‘good quality’ bystander chest compressions without mouth-to-mouth ventilation was almost identical to the outcome obtained when both were performed. These findings are consistent with laboratory investigations involving swine models of resuscitation [18]. Several studies have suggested that simplifying the recommendations for bystander resuscitation to the performance of chest compressions alone may encourage bystanders to perform BLS more often [2], [11].
The most striking finding of our survey was that, although the majority of students surveyed did consider SARS to be a risk to the rescuer during mouth-to-mouth ventilation, it appears they would actually be significantly more likely to withhold mouth-to-mouth ventilation during resuscitation of both strangers and family members if either blood or vomit were present in the victim's mouth rather than due to a fear of SARS. Our questionnaire did not investigate this further by asking why this should be, but possibilities include the aesthetically unpleasant nature of performing mouth-to-mouth ventilation under these circumstances and a perceived increase in risk of transmission of infection from direct contact with the victim's blood and bodily secretions. Although none of our students had actually performed mouth-to-mouth ventilation in a real situation they were aware that it can be an unpleasant task, and 37% indicated that this ‘unpleasantness’ would be a reason for them to withhold it. Other reasons given for withholding mouth-to-mouth ventilation included a ‘fear of failure’, with 43% of the students citing this as a factor. Other studies have also found a lack of confidence in ability to perform the required skills to be a significant cause of bystander reluctance to perform BLS and mouth-to-mouth ventilation [4], [5], [12], although this motive diminished with increased training and previous use of BLS skills. Interestingly our study showed a male:female divergence regarding the unpleasant nature of mouth-to-mouth ventilation and the fear of failure of mouth-to-mouth resuscitation, with the females significantly more likely to cite these as concerns.
Our study has a number of limitations. We had a response rate of 65% which is comparable to similar questionnaire surveys. However, our actual number of respondents was low (35 out of a possible 54 students) making it less valid to draw generalisations from our data. Medical students were chosen for the investigation because, having witnessed the impact of the SARS outbreak from inside the hospital system, they were well aware of the risks the SARS infection posed. In addition, they had also been trained in the knowledge and skills required to perform resuscitation and, as a group, tend to be motivated to put their medical skills into practice. None of our student responders had ever actually performed any BLS manoeuvres in a real cardiac arrest situation, so all were answering from a similar level of zero past practical experience. However, their answers are therefore hypothetical, and as such may not accurately represent what they would do in a real situation. It is also possible that their expressed opinions may have been influenced by the attitudes of their trainers and that their answers may not reflect that of the general population of Hong Kong. This may be important as it is the general population who would be expected to perform the majority of the bystander BLS that occurs outside hospital. The actual rates of bystander BLS in Hong Kong are low (15.6% of arrests) [19], and citizen preparedness and knowledge regarding resuscitation have been estimated as very poor [20]. It would be interesting to perform a similar survey to ours among the general population to see if SARS has had any impact on the already low level of bystander BLS that is currently performed. Ideally such surveys should be conducted before and after the arrival of SARS onto the clinical stage, to determine whether or not its impact has truly changed willingness to perform BLS. Obviously this is not feasible, and although it could be useful to conduct a similar study in a region that has remained relatively unaffected by SARS and compare the responses to ours, the populations would be different. Nevertheless, despite these limitations we believe that our study has produced interesting data regarding a subject that may need to be reassessed in the light of newly emerging infections (e.g. SARS, avian flu)—namely the true rather than perceived risks that performing BLS poses to the rescuer.
In conclusion, our students generally agreed that they had received an adequate level of BLS training to enable them to perform it competently if required. However, it appears that this training does not directly translate into confidence regarding one's skills, as a smaller percentage of students claimed such confidence despite agreeing that their training had been adequate, and almost all the students would have appreciated further BLS practice before having to do it for real. Perhaps this is something that needs to be addressed in undergraduate medical curricula. Hong Kong medical students are concerned about the risk of transmission of disease, including SARS, during resuscitation, but would be more likely to withhold mouth-to-mouth ventilation owing to the presence of vomit or blood in the victim's mouth, than due to a fear of contracting SARS. The actual risk of transmission of SARS-CoV virus during resuscitation is unknown, but it can occur. The first step in resuscitation is to ensure the safety of the rescuer [10]. Further work is, therefore, required to elucidate the risks that newly emerging infectious diseases, such as SARS, pose to rescuers during resuscitation attempts, and the efficacy of protective equipment, such as barrier masks and viral filters in preventing the transmission of such infections.
Conflict of interest statement
There is no conflict of interest related to this study.
Footnotes
A Spanish translated version of the summary of this article appears as Appendix at 10.1016/j.resuscitation.2005.05.014.
Appendix A. Supplementary data
References
- 1.Brenner B.E., Kauffman J. Reluctance of internists and medical nurses to perform mouth-to-mouth resuscitation. Arch Intern Med. 1993;153:1763–1769. [PubMed] [Google Scholar]
- 2.Locke C.J., Berg R.A., Sanders A.B. Bystander cardiopulmonary resuscitation: concerns about mouth-to-mouth contact. Arch Inter Med. 1995;155:938–943. doi: 10.1001/archinte.155.9.938. [DOI] [PubMed] [Google Scholar]
- 3.Hew P., Brenner B.E., Kauffman J. Reluctance of paramedics and emergency medical technicians to perform mouth-to-mouth resuscitation. J Emerg Med. 1997;15:279–284. doi: 10.1016/s0736-4679(97)00006-1. [DOI] [PubMed] [Google Scholar]
- 4.Jelinek G.A., Gennat H., Celenza T., O’Brien D., Jacobs I., Lynch D. Community attitudes towards performing cardiopulmonary resuscitation in Western Australia. Resuscitation. 2001;51:239–246. doi: 10.1016/s0300-9572(01)00411-7. [DOI] [PubMed] [Google Scholar]
- 5.Johnston T.C., Clark M.J., Dingle G.A., FitzGerald G. Factors influencing Queenslander's willingness to perform bystander cardiopulmonary resuscitation. Resuscitation. 2003;56:67–75. doi: 10.1016/s0300-9572(02)00277-0. [DOI] [PubMed] [Google Scholar]
- 6.Government of the Hong Kong Special Administration Region: Official Statistics; 19 January 2004.
- 7.Government of the Hong Kong Special Administration Region: Health, Welfare and Food Bureau. SARS Bull; 23 June 2003.
- 8.Government of Hong Kong Special Administration Region. HIV Surveillance Report—2003 update. http://www.info.gov.hk/aids/archives/backissuestd/aids03.pdf
- 9.Emergency Cardiac Care Committee. Guidelines for cardiopulmonary resuscitation and emergency cardiac care; adult basic life support. Part II. JAMA 1992;268:2184–98. [PubMed]
- 10.Advanced life support course provider manual. 4th ed. London: Resuscitation Council (UK) & European Resuscitation Council; 2000.
- 11.Duan S.M., Zhao X.S., Wen R.F. Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed Environ Sci. 2003;16:246–255. [PubMed] [Google Scholar]
- 12.Shibata K., Taniguchi T., Yoshida M., Yamamoto K. Obstacles to bystander cardiopulmonary resuscitation in Japan. Resuscitation. 2000;44:187–193. doi: 10.1016/s0300-9572(00)00143-x. [DOI] [PubMed] [Google Scholar]
- 13.Department of Communicable Disease Surveillance and Response. Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). WHO/CDS/CSR/GAR/2003.11. Geneva; WHO:2003
- 14.Copley D.P., Mantle J.A., Rodgers W.J., Russell R.O., Jr., Rackley C.E. Improved outcome for pre-hospital cardiopulmonary collapse with resuscitation by bystanders. Circulation. 1977;56:901–905. doi: 10.1161/01.cir.56.6.901. [DOI] [PubMed] [Google Scholar]
- 15.Cummins R.O., Eisenberg M.S. Pre-hospital cardiopulmonary resuscitation: is it effective? JAMA. 1985;253:2408–2412. [PubMed] [Google Scholar]
- 16.Herlitz J., Bang A., Gunnarsson J. Factors associated with survival to hospital discharge among patients hospitalized alive after out of hospital cardiac arrest: change in outcome over 20 years in the community of Goteborg, Sweden. Heart. 2003;89:25–30. doi: 10.1136/heart.89.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Hoeyweghen R.J., Bossaert L.L., Mullie A. Quality and efficacy of bystander CPR. Resuscitation. 1993;26:47–52. doi: 10.1016/0300-9572(93)90162-j. [DOI] [PubMed] [Google Scholar]
- 18.Berg R.A., Kern K.B., Hilwig M.D. Assisted ventilation does not improve outcome in a porcine model of single-rescuer bystander cardiopulmonary resuscitation. Circulation. 1997;95:1635–1641. doi: 10.1161/01.cir.95.6.1635. [DOI] [PubMed] [Google Scholar]
- 19.Fan K.L., Leung L.P. Prognosis of patients with ventricular fibrillation in out-of-hospital cardiac arrest in Hong Kong: a prospective study. Hong Kong Med J. 2002;8:318–321. [PubMed] [Google Scholar]
- 20.Cheung B.M., Ho C., Kou K.O. Knowledge of cardiopulmonary resuscitation among the public in Hong Kong: a telephone questionnaire survey. Hong Kong Med J. 2003;9:323–328. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


