Abstract
Acute respiratory tract infections (ARTIs) are leading contributors to the global infectious disease burden, which is estimated to be 112,900,000 disability adjusted life years. Viruses contribute to the etiology of ARTIs in a big way compared with other microorganisms. Since the discovery of respiratory syncytial virus (RSV) 61 years ago, the virus has been recognized as a major cause of ARTI and hospitalization in children. The morbidity and mortality attributable to RSV infection appear to be higher in infants < 3 months and in those with known risk factors such as prematurity, chronic lung, and congenital heart diseases. Crowded living conditions, exposure to tobacco smoke, and industrial or other types of air pollution also increase the risk of RSV-associated ARTI. Many epidemiological studies have been conducted in developed countries to understand the seasonal patterns and risk factors associated with RSV infections. Dearth of information on RSV-associated morbidity and mortality in Asian and developing countries indicates the need for regional reviews to evaluate RSV-associated disease burden in these countries. Epidemiological studies including surveillance is the key to track the disease burden including risk factors, seasonality, morbidity, and mortality associated with RSV infection in these countries. These data will contribute to improve the clinical diagnosis and plan preventive strategies in resource-limited developing countries.
Keywords: acute respiratory tract infections, respiratory syncytial virus, epidemiology, children, Asia
Introduction
Acute respiratory tract infection (ARTI) is one of the major health issues in infants and children in the world causing morbidity and mortality with an estimated global disease burden of 112,900,000 disability adjusted life years. 1 Respiratory illness is the most common reason for consulting general practitioners and hospitalization in children and adults. 2 For example, in the United States, the incidence of lower respiratory tract infections (LRTIs) among children under 5 years of age is high contributing to 19% of hospitalizations in the general population of children. 3 In developed countries, ARTI rarely causes mortality but contributes to direct and indirect health costs; however, ARTI causes severe morbidity and mortality in developing countries. 4 In the latter, one-third of the deaths in children < 5 years of age are caused by respiratory illness, 5 6 which is 30 to 70 times higher than that reported in developed countries. 7 ARTI-associated morbidity is also high in developing countries due to malnutrition, low birth weight, passive smoking, absence of breastfeeding, low socioeconomic, and overcrowded living conditions. 8
Viruses contribute to a larger proportion of ARTI-associated morbidity and hospitalizations globally. Around 50 to 90% of the LRTI in young children are caused by respiratory syncytial virus (RSV), human metapneumovirus (hMPV), influenza viruses, human bocavirus (hBoV), parainfluenza viruses (PIVs), adenoviruses, rhinoviruses, human coronavirus (hCoV), and enteroviruses ( Table 1 ). 8 9 In 1956, RSV was isolated from chimpanzees with common cold-like illness 21 and this led to the identification of RSV as a causative agent of coryza in chimpanzees. 22 Subsequently, Chanock et al identified the same virus as the cause of LRTI in young infants. 23 The virus was later named as RSV reflecting its ability to form syncytia among infected cells. 24
Table 1. Prevalence of respiratory viruses causing LRTI in the world.
| Country | Age | Sample | Study period | Prevalence % | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RSV | hMPV | InfV | hBoV | PIV | RhiV | AV | hCoV | EntV | ||||
| Germany 10 | < 36 mo | 1,054 | 6 y | 34 | NA | 4.7 | NA | 7.7 | NA | NA | NA | NA |
| Ghana 11 | < 5 y | 128 | Jan 2008–Dec 2008 | 18 | NA | 1 | NA | 4 | NA | 13 | NA | NA |
| Spain 12 | < 1 y | 99 | Jan 2006–Jun 2006 | 35 | 25 | NA | NA | NA | 19 | NA | NA | NA |
| China 13 | Children | 34,885 | Jan 2001–Dec 2006 | 23.6 | NA | 2.0 (InfV A) |
NA | 4.3 (PIV-3) 0.6 (PIV-1) 0.1 (PIV-2) |
NA | 1.7 | NA | NA |
| Japan 14 | < 15 y | 921 | Apr 2000–Mar 2001 | 20.4 | NA | 11.9 (InfV A) |
NA | 3.8 | NA | 2.9 | NA | NA |
| France 15 | < 36 mo | 192 | Sep 2001–Jun 2002 | 30 | 4 | 6 | NA | NA | 21 | NA | NA | 9 |
| Thaiwan 16 | < 36 mo | 48 | Apr 2007–Dec 2007 | 41.7 | 27.1 | NA | 6.3 | NA | NA | NA | NA | 6.3 |
| Mexico 17 | < 15 y | 285 | NA | 85.6 | NA | 7.2 | NA | 2.4 | NA | NA | NA | NA |
| Korea 9 | 5 y | 515 | 2000–2005 | 23.7 | 4.7 | 4.7 (InfV A) 1.7 (InfV B) |
11.3 | 6.2 (PIV-3) 1.7 (PIV-1) |
5.8 | 6.8 | NA | NA |
| Egypt 18 | < 1 y | 450 | Nov 2006–Dec 2007 | 23.8 | 6.4 | NA | NA | 6.6 (PIV-1) 3.1 (PIV-2) 8.9 (PIV-3) |
NA | 18.4 | NA | NA |
| Malaysia 19 | < 24 mo | 5,691 | 1982–1997 | 84 | NA | 6 | NA | 8 | NA | 2 | NA | NA |
| Turkey 20 | ≤2 y | 147 | NA | 55.6 | 13 | 9.3 | NA | 27.8 | NA | 5.6 | NA | NA |
Abbreviations: AV, adenoviruses; EntV, enterovirus; hBoV, human bocavirus; hCoV, human coronavirus; hMPV, human metapneumovirus; InfV, influenza virus; LRTI, lower respiratory tract infection; NA, not available; PIV, parainfluenza virus; RhiV, rhinovirus; RSV, respiratory syncytial virus.
RSV is an enveloped virus with a nonsegmented negative sense RNA belonging to the genus Orthopneumovirus of the family Pneumoviridae. 25 The virus encodes for 10 genes and 11 proteins. 26 RSV has three surface glycoproteins: the fusion glycoprotein (F), attachment glycoprotein (G), and small hydrophobic (SH) proteins ( Fig. 1 ). G and F proteins are responsible for the initial phases of viral infection through attachment with the infecting cell. 26 The cell fusion is mediated by F, G, and SH proteins and the latter is believed to change membrane permeability. 27 Based on the structural features of the matrix protein (M) and ribonucleoprotein (RNP), there are three morphological forms (a, b, and c) of RSV particles ( Fig. 2 ). 28
Fig. 1.
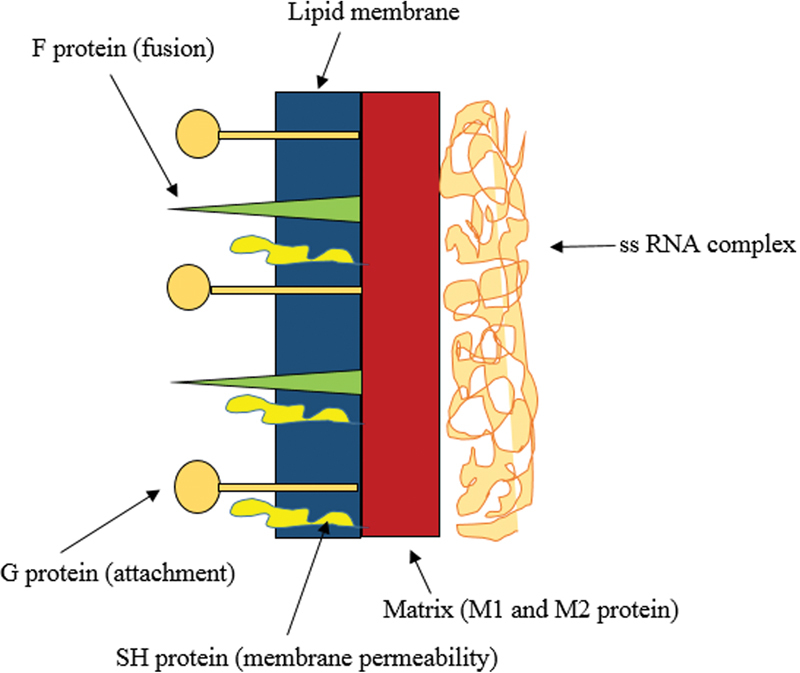
A schematic diagram showing the cross-sectional layers of RSV. The matrix comprises the M1 and M2 proteins and the viral capsid contains the F and G transmembrane proteins. RSV, respiratory syncytial virus.
Fig. 2.
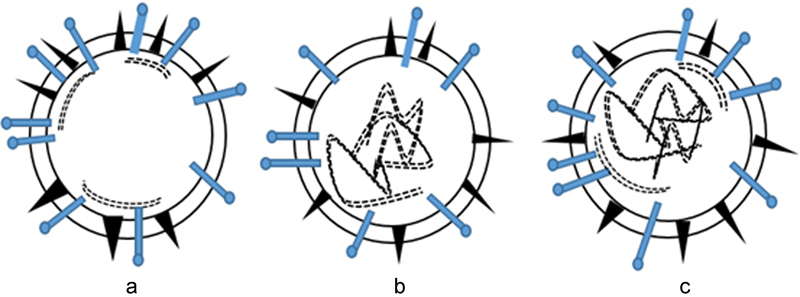
Three types ( a – c ) of spherical RSV particles have been described according to the major structural features of the M protein and RNP: ( a ) Presence of a characteristic layer beneath the membrane with extensive patches of M; ( b ) A large region within the capsid is filled with nucleic material with less contact points and 3 to 4 of RNP are dispersed throughout; ( c ) Nucleic material densely packed within the capsid membrane containing large number of RNP. 28 M, matrix; RNP, ribonucleoprotein; RSV, respiratory syncytial virus.
Transmission of RSV occurs mainly via the nose through infected aerosols. RSV remains infectious on many environmental surfaces suggesting that transmission can occur through contact with hands or inanimate surfaces contaminated with infected nasal secretions. 29 Most of the RSV-associated ARTI are community-acquired, but there have also been reports of hospital-acquired RSV infections. 8 30 The likelihood of hospital-acquired RSV infection increases with the duration of hospital stay and gaps in the infections control practices. 31 Based on a previous study, RSV detection in children at the time of admission was 39%, which increased to 62% during the hospital stay. 32
RSV alters host cells by initially infecting the epithelial lining of the respiratory airway and nasal passage. The virus influences the expression of genes controlling protein metabolism, inflammation, cell growth, proliferation, nucleic acid regulation, and synthesis. 33 RSV infection causes pneumonia through damaging the respiratory epithelium and broncho-ciliary apparatus; this results in the collection of fluid in bronchioles and alveoli causing obstruction and collapse of the affected area of the lung. Replication of RSV starts from nasopharynx primarily in the superficial layer of the respiratory epithelium and the virus then descends from the nasopharynx to lower respiratory tract via the respiratory epithelium or inhalation of secretions. 34
RSV-associated bronchiolitis is the most important cause of admission to the hospital during the first year of infancy. 8 Around 50 and 25% hospitalizations of infants are due to RSV-associated bronchiolitis and pneumonia. 34 RSV is responsible for precipitating recurrent wheezes and asthma in susceptible children. 35 Recurrent RSV infections also cause residual parenchymal or airway damage leading to minor abnormalities in lung function in the longer term. The mechanisms involved in RSV-associated recurrent wheeze and asthma are not clear, and whether RSV is directly responsible for asthma or infects children with preexisting broncho-obstructive disease remains unresolved. 36 Recent studies suggest that RSV causes asthma in some infants, but is also capable of attacking infants with a predisposition for wheezing. 36 37 Hospitalized infants aged < 1 year with RSV-associated bronchitis have a tendency to develop asthma and recurrent wheeze for a few years. 38 Here, we review the impact of RSV-associated ARTI on children in Asia including epidemiology, laboratory diagnosis, therapies, and future research priorities.
RSV-Associated Disease Burden
Since the discovery of RSV 61 years ago, the virus has been identified as a major cause of ARTI in infants and the single most common cause of childhood hospitalization. 39 During the past 31 years, RSV has been identified as the cause of severe LRTI in infants and children in developing countries. 39 RSV-associated morbidity and mortality appear to be high in infants < 3 months and children with known risk factors compared with other viral LRTI. Known risk factors for acquiring RSV-associated LRTI include prematurity, chronic lung disease, congenital heart disease, cystic fibrosis, bronchopulmonary dysplasia, down syndrome, compromised immunity, crowded living conditions, and exposure to tobacco or industrial smoke. 9 40 Moreover, RSV-associated ARTI appears to be common in boys than girls; 41 the reason for the male preponderance is believed to be due to immunomodulatory effects of the sex hormones during the early stages of life. 42 Severe RSV-associated respiratory disease has also been recognized as a significant health issue in adult populations, and epidemiological data suggest that the impact of RSV in adults is largely similar to nonpandemic influenza. ARTI due to RSV have been reported in the institutionalized elderly, the immunocompromised, and adults with cardiopulmonary diseases. 43
The Impact of RSV on Global Child Health
Globally, RSV is commonly associated with childhood ALRI and related hospital admissions, which results with a substantial burden to the health care systems and economy. Approximately 45% of the hospitalizations and deaths are caused by RSV-associated ARTI in infants < 6 months. In 2015, 33.1 million new episodes of RSV-associated ALRI occurred worldwide in children less than 5 years, with at least 3.2 million hospitalizations and 59,600 in-hospital deaths. 44 Moreover, RSV-associated ALRI caused 1.4 million hospitalizations with 27,300 in-hospital deaths in infants < 6 months. 44
Alaskan native infants have the highest rates of RSV hospitalizations in the world. 42 RSV-associated hospitalization rates for Alaskan native infants, in the rural Yukon–Kuskokwim Delta (YKD) region of Alaska were five times higher than that for the overall United States infant population. 45 From 1993 to 2004 is considered to be the period when the worst RSV outbreaks occurred in the YKD region, and RSV-associated hospitalization rates rose to 38 to 248 per 1,000 during that period. Infants from indigenous Canadian populations, Germany, the United States, New Zealand, and Europe also have high hospitalization rates with RSV-associated ARTI. 46
The Impact of RSV on Child Health in Asia
Based on studies conducted in Asia, the most common cause of LRTI in children is RSV ( Table 2 ). In Hong Kong, RSV-associated hospitalization has been described in children < 5 years. 64 In Japan, RSV-associated LRTI occurred in 31.4% of a sample of 535 children aged < 3 years. 47 In Lanzhou, China, RSV was detected in 40.71% of the children with ARTI. 50 In another study, RSV accounted for 25.0% of the LRTI cases in Harbin, China. 51 In Hong Kong, RSV has been detected in young infants with chronic lung disease, neurodevelopmental conditions, and congenital heart disease; these risk factors significantly increased the risk of RSV infection. 65
Table 2. Incidence and seasonality of RSV infection in Asian countries.
| Country | Duration of the study | Age | Incidence % | Seasonality |
|---|---|---|---|---|
| Japan | Jul 1997–Jun 2000 54 | < 3 y 47 | 31.4 47 | Common in winter and a peak in Dec 47 |
| Nov 2001–Jul 2004 55 | Pediatric patients 48 | 37.1 48 | Winter–spring with a peak in Dec (2001–2003) and a peak in Nov (2003–2004) 48 | |
| China | 2010 49 | < 5 y 49 | 33.1 49 | Throughout the year, with a peak from Sep to Jan 49 |
| 2006–2009 50 | ≤ 14 y 50 | 40.71 50 | Fixed seasonal rhythm, with a peak from Nov to Apr 50 | |
| Jan 2008–Dec 2008 51 | 16 y 51 | 25.0 51 | Early spring to winter, with a peak from Jan to Apr 51 | |
| Hong Kong | Jan 2004–Dec 2004 52 | ≤3 y 52 | 11.6 52 | No winter seasonality 3 and peak in Mar and Sep 52 |
| Malaysia | 1982–2008 53 | ≤ 5 y 53 | 81.3 53 | Throughout the year with a seasonal peak from Sep to Dec 53 |
| Indonesia | Jan 1995–Jun 2009 43 | < 5 y 43 | 16 43 | Throughout the year 43 |
| Vietnam | 2009–2010 54 | < 2 y 54 | 48 54 | Peak during rainy season from May to Oct 54 |
| Philippines | 2012–2013 55 | Children 55 | 28.1 55 | Peak activity occurs in Jan 55 |
| Taiwan | Jan 2001–Dec 2005 56 | 2 y 56 | 60.7 56 | Showed a biennial pattern, with peaks in spring and fall 56 |
| Thailand | Sep 2003–Dec 2007 57 | All ages 57 | 8.9 57 | Detected most month of the year with a peak from Jun to Oct 57 |
| Nepal | Jul 2004–Jun 2007 58 | < 5 y 58 | 15.1 58 | Rainy season and winter season with a peak from Jul to Apr 58 |
| South India | NA | < 5 y 59 | 57 59 | Rainy season (Aug–Nov) 59 |
| Bangladesh | 1993–1996 60 | < 24 mo 60 | 81 60 | NA |
| 2009–2011 61 | Children 61 | 40/100 child y 61 | Throughout the year with a peak from Dec to Feb 61 | |
| Pakistan | 2011–2012 62 | Children 62 | 71.4 62 | Winter season with a peak from Dec to Jan 62 |
| Aug 2009–Jun 2012 63 | < 5 y 63 | 19 63 | Peak in Sep coinciding with the rainy season 63 |
Abbreviations: NA, not available; RSV, respiratory syncytial virus.
Information on the impact of RSV in childhood ARTI in South East Asian countries is scanty. In Malaysia, RSV is the most common respiratory virus identified in children ≤ 6 months, accounting for 81.3% of the LRTI cases. 53 Data from Lombok, Indonesia, suggest that 16% of LRTI deaths are caused by RSV. 66 In Vietnam, RSV, influenza A, and rhinoviruses contribute to pneumonia along with multiple viral and coinfections with bacteria. 67 In Bhaktapur, Nepal, RSV infections were detected in 15.1% of the study sample, 58 and in India RSV accounted for 57% of ARTI cases. 64 In Bangladesh, RSV has been identified as the predominant (81%) viral pathogen causing pneumonia in children in rural areas. 60 In urban areas of Bangladesh, the overall incidence of RSV-associated pneumonia is 40/100 child years. 61
In temperate regions of Asia RSV causes outbreaks mostly during the fall or winter; in tropical regions of Asia RSV outbreaks usually peak in hot or rainy seasons, but can occur at any time of the year with genotype shifting. 68 Based on the severe acute respiratory infection (SARI) surveillance in China, RSV has been mostly detected in infants year around with peaks from autumn to winter. 49 In contrast to these findings reported from the mainland China, 58 RSV seasonality has not been noted in winter in Hong Kong. 65 In Japan, cocirculation of different RSV genotypes has been observed every year with shifts in genotypes within a season. 48 In Nepal, the largest peaks of pneumonia occur during RSV peak seasons in rainy and winter periods from July to April. 58 69 In India, RSV outbreaks occur in the rainy season from August to November. 59
The Impact of RSV on Childhood ARTI in Sri Lanka
Childhood hospitalization due to RSV-associated ARTI is common in Sri Lanka. 70 RSV is recognized as the most common cause of viral ARTI among children in Sri Lanka, as in many other countries. RSV contributes to 90.6% of virus-associated ARTI based on the findings of a small-scale study of children admitted to Kegalle General Hospital with ARTI. 70 This study also described that RSV infections occurred predominantly from July to September. 70 A study based on Gampola and Anuradhapura Teaching Hospitals reported incidences of 31.3 and 28/100,000 person years, respectively, for RSV among infants with ARTI. In Anuradapura (which is located in the dry zone), RSV was detected throughout the year with a peak from May to July in both 2013 and 2014. In Gampola (located in the wet zone), RSV was again detected throughout the year, but peaked during December to January in 2013. 64 Larger studies are needed to fill the gap in understanding the local seasonality, disease burden, and severity of RSV-associated ARTI in Sri Lanka. 64
Epidemiology of RSV Infections
Data on the incidence and mortality of RSV-associated ARTI in Asian developing countries have not been published and thus the extent of this infection's contribution to mortality remains uncertain. According to the World Health Organization (WHO), almost three-fourths deaths in infants occur due to RSV-associated pneumonia in Southeast Asia and sub-Saharan Africa. 71 The Pneumonia Etiology Research for Child Health (PERCH) project evaluated the etiological agents causing severe pneumonia in children from seven developing counties including two in Asia, Bangladesh and Thailand. This study showed a significant association between hospitalization of children and RSV-associated pneumonia in Bangladesh. 72 Therefore, regional estimates of RSV-associated ARTI burden in Asian developing countries with local seasonal patterns, risk factors, and virus evolution would improve our understanding of RSV epidemiology in these countries.
Seasonality of RSV Infections
A few projects have been conducted in developed and developing countries to understand the seasonal patterns of RSV infection compared with other respiratory pathogens and to identify the risk factors for severe respiratory disease. 66 These projects have shown that RSV seasonality depends on the geographic location and altitude of a given country or a region. RSV-associated respiratory disease epidemics tend to occur in clusters during a particular season. Although the occurrence of RSV outbreaks varies among continents, the general pattern is that they start in coastal areas and spread to inland areas. 39 In countries experiencing tropical and semitropical climates and located far from the equator, RSV outbreaks occur in cool dry and cool wet seasons. In regions closer to the equator, RSV outbreaks occur throughout the year with periods of peak activity. 39 RSV outbreaks have been reported year around with a slight increase in the rainy seasons in equatorial islands like Singapore, Fiji, Taiwan, and Hawaii. 40 In countries north of the equator like India, outbreaks have been reported predominantly during the rainy season. 40 RSV peaks have been reported in the winter months in most of the European countries although the infections remain relatively consistent throughout the year. 40 Although there are predictions made on RSV seasonality patterns, the predictions are not reviewed systematically at a global level, in parallel with surveillance data for many other respiratory viruses like influenza in the last decade.
RSV diversity is influenced by the physiology of the host, host–virus interactions, social behavior of people, and transmissibility of the virus. The absence of a global picture of RSV seasonal patterns is a hindrance to planning public health strategies to combat RSV outbreaks. An extensive review of the literature, together with proper laboratory surveillance in different geographical areas, remains to be conducted on a global scale.
RSV outbreaks have periodic emergence patterns and the reason for that is not clear. Even though geographic and climatic factors have a clear association with epidemics, the RSV epidemic pattern is also related to human behavior. 39 Due to similarities in risk factors, influenza and RSV epidemics often overlap. 73 In temperate areas, RSV and influenza activities both peak during the winter. However, there is greater diversity in the behavior of the two viruses in tropical countries, where RSV has been reported in 80% of areas, and influenza in 50% of areas, during the same outbreak. 74
Risk Factors
Repeated RSV infections are associated with increased prevalence of atopy in children and their families. 34 Some investigations were performed to explore whether there is a connection between RSV-associated bronchiolitis in infancy and subsequent development of allergic sensitization or clinical allergy. 75 These studies confirm the association between recurrent RSV infections and atopy in children. Conversely, children with atopy and recurrent RSV infections also had more siblings and smoking parents. 36 Children with recurrent RSV infections had cardiopulmonary conditions than those with influenza or bacterial infections. Thus, RSV infection in children is associated with asthma, atopy, and other forms of bronchial obstructive diseases. 76
Trials performed in the United States, the United Kingdom, Japan, Canada, and Denmark revealed the significance of crowded living conditions and exposure to tobacco smoke as risk factors for severe RSV disease. 40 Likewise, a study in Sri Lanka found that 31.3% of children with RSV-associated ARTI were from a household with at least one smoker. 64 Also, according to research conducted in Sri Lanka and Kenya, there is a close association between rural inhabitance and hospitalization due to RSV infection suggesting that rural inhabitance may also be a predisposing factor for RSV infection. 64 71 The time of birth has a significant association with RSV-induced bronchitis, 77 and moreover, birth during the winter virus peak season confers risk for childhood asthma. 78 Immunosuppression is another independent risk factor for RSV infection and the risk of mortality increases with the progression of infection from upper to lower respiratory tract. 77 Among adults, presence of a chronic pulmonary disease, physician-diagnosed congestive heart failure, and functional disability increase the risk of RSV-associated serious ARTI. 79 80 Moreover, hospitalization is a risk factor for severe RSV infection and mortality attributed to RSV-associated ARTI. 40
Virus Evolution
Virus evolution contributes to the emergence of new strains of RSV, while old RSV stains disappear under the selective pressures created by the new ones. 81 Pathogenicity and the fitness are strong in emerging RSV stains, which are widespread and cause recurrent infections and outbreaks. 82 The G and F proteins are considered as important antibody targets as changes occur in these areas to avoid the host immune responses. 83 RSV evolution is associated with accumulation of amino acid changes and antigenic variations in the G protein. 84 Even though the sequence variability of RSV is concentrated on the G gene, the rapid pace of infection underlines the contribution of the full genome to virus evolution. 83 According to the sequence variability in the F gene, mutations in the F protein are mostly deleterious, therefore, only a few sites in the F gene are under positive selection pressures. 85 RSV appears to undergo sequential evolution like influenza B, which has evolved through interactions between influenza A and C. It has been shown that multiple lineages of RSV originate from cocirculation of RSV subtypes. 81 RSV subtype B shows significantly faster rate of evolution than the subtype A, with a higher variation in the protein length, stop codon usage, and mechanisms for variation in the G gene. 46
The other explanation for the change of genotypes over time is the rapid distribution of new genotypes as they emerge around the world at the same time. 81 A study conducted in New Zealand on the evolution of the G gene sequence noted the circulation of RSV stains that were related to those circulating in nearby countries during the same period. This finding supports the emergence and spread of RSV stains between closer neighboring regions. 46 A combination of factors including virus persistence in defined areas and continuous reintroductions from different areas are believed to be responsible for RSV epidemics resulting from new subtypes. 86
Laboratory Diagnosis of RSV Infection
Respiratory viruses tend to circulate at the same time making it difficult to identify their individual contributions on the disease burden. 87 Moreover, the chances of detecting viruses in clinical specimens may be constrained by inadequate sample volume or quality, or by the laboratory techniques used. Isolation attempts often fail due to the lability of the virus. 88 However, the laboratory diagnosis should be sensitive and specific to identify viruses causing ARTI. 87 Thus, timely detection of RSV resulting from a rapid and an efficient assay is important. 89 Many laboratory tests are often limited to a single virus, rather than allowing detection of multiple respiratory viruses. Although widely used techniques like viral culture and antigen detection have greater sensitivity over direct antigen testing ( Fig. 3 ) from respiratory samples, their ability to detect only a single pathogen is a limitation. 90 Molecular techniques ( Fig. 3 ) are highly effective and have facilitated the identification of previously known and new viruses. 91 Moreover, molecular characterization of different respiratory viruses for epidemiological purposes has been performed using different types of conventional and advanced DNA sequencing methods ( Fig. 3 ).
Fig. 3.
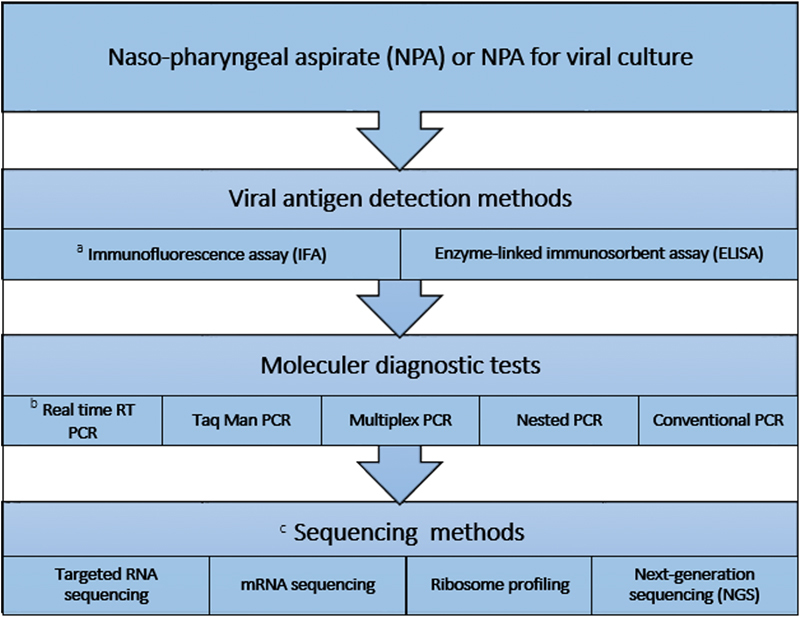
Laboratory diagnosis of RSV infection using NPA. When NPA is not available nasal swabs can be used but the chances of viral antigen or nucleic acid detection in the nasal swab is low when compared with that in the NPA. ( a ) Immunofluorescence assay has been used in many diagnostic laboratories to detect RSV antigen. ( b ) Real-time PCR has been used in well-equipped laboratories to detect RSV nucleic acid and is the gold standard test. However, other types of PCRs have also been used to detect RSV nucleic acid depending on the availability. ( c ) Sequencing is done to understand the local, regional, and global epidemiology of different RSV types. PCR, polymerase chain reaction; NPA, nasopharyngeal aspirate; RSV, respiratory syncytial virus.
Treatment Options for RSV
Ribavirin is the only licensed antiviral treatment for RSV infections and has shown promising results in placebo-controlled studies with administration at the beginning of the illness to children who are more prone to get life-threatening complications. 76 However, the drug is less used clinically, at least in part because of a lack of confidence in its efficacy. 92 Factors such as the inconvenience of administration and toxicity also compromise its therapeutic potential in severe RSV infections. 93
Palivizumab (Synagis) is a drug approved for use in selected risk groups, such as infants with chronic lung disease, congenital heart disease, and history of prematurity. 94 It is a monoclonal antibody (mAb) that targets one of the proteins in RSV subtypes A and B. 95 However, palivizumab is only around 40% effective in reducing RSV-associated hospitalization rates in premature infants and high risk children. 96 While this prophylactic treatment may be effective in reducing RSV-associated morbidity in infants, high cost and inconvenience of administration have limited it use. 97
An effective vaccine against RSV has not been available yet, and clinical experience of both inactivated and attenuated test vaccines have not shown great promise. In one trial, RSV-infected children were administrated an inactivated vaccine named “lot 100” and following the vaccination, vaccinees developed severe respiratory disease. Infants aged under 23 months showed a higher incidence of pneumonia (60%) in the vaccinated group compared with the placebo group that had only an 8% incidence of pneumonia. The vaccine was reported to induce the production of a neutralizing antibody against F and G proteins but the reason for the increased respiratory disease in the vaccinated children was not clear. 34
An RSV live-attenuated vaccine (LAV) with enhanced immunogenicity was tested in cotton rats and this vaccine exhibited thermal stability, efficacy, and immunogenicity. This genetically modified vaccine candidate merits consideration as the next-generation RSV vaccine design for humans. 98 Many other experimental vaccines are being tested on animal models and inactivated vaccines have shown superiority over attenuated vaccines in eliciting humoral and cell-mediated immunity. Recombinant vaccines with the expression of F, G, and N genes are currently under investigation. The common obstacles in the progress of developing a RSV vaccine are the young age group that needs to be protected and the fact that individuals experience continued reinfections with RSV even in the presence of humoral immunity. 34
Future RSV Research Priorities
Poor growth of RSV in vitro, lack of suitable animal models, and instability of RSV in test environments have limited RSV research. More research is needed to address different aspects of RSV structure, function, and infection. The genome structure of the negative strand RNA, three-dimensional structure of the virus, and virion structure should also be evaluated to identify immunogenic proteins as vaccine candidates.
Due to limited therapeutic options to treat RSV-associated respiratory disease, the development of effective novel therapies must be high priority too. Currently, the effect of administering RSV neutralizing antibodies is being studied. These studies have also progressed to evaluating the effectiveness of combination therapy with these antibodies and antivirals like ribavirin. 99 Combinations of intravenous palivizumab and ribavirin have also been studied in high-risk RSV disease in children; such combination therapy has been reported to be effective, and associated with reduced mortality rates. 100 The combination of two mAbs (130–6D and 131–2G), which are reactive to the central conserved region (CCR) of RSV G protein, has also shown promising results in reducing the pulmonary inflammation caused by RSV compared with the effect of these antibodies alone in reducing the inflammation. 99 Finally, mucolytic agents such as recombinant human deoxyribonuclease (rhDNase) have shown promising results based on the improvements shown on chest X-rays, 78 but more work is needed to evaluate the effectiveness of these drugs.
As the immune responses elicited by viruses are specific despite their structural and pathogenic similarities, work is needed to identify the fundamental aspects of the immune response in RSV infections. For instance, very little information is available on the mechanisms of mucin (MUC) expression in human epithelial cells during an RSV infection and its contribution to immune response. As MUC is recognized as an important component of the immune response, further research on this would bring a better understanding on the role of MUC in rendering protection in RSV infections. Moreover, research on the immune response in primary, secondary, homotypic, and heterotypic RSV infections would help to design immunoprophylactic strategies. Conversely, identifying the role of the respiratory microbiome in severe RSV infections will help to understand the impact of microbiome in disease severity as well as in protection.
The evolution of RSV around the globe is not fully understood, and thus sequence analysis of the stains will provide knowledge about the ancestry of the RSV and its evolution. Studies should also be performed to gather information on seasonality patterns and transmission dynamics according to regional differences in RSV seasonality data with climatic and population data. 82 Better understanding of the epidemiology of ARTI in developing countries would provide options for preventive measures in a timely manner as use of respiratory precautions and health education can be undertaken in different target populations.
Conclusion
Respiratory syncytial virus has a worldwide distribution and it contributes to significant morbidity and mortality in infants compared with other respiratory pathogens. Regional seasonality of RSV infections is pronounced. In equatorial countries, RSV is seen year-round, but there is an association with the rainy season in tropical and semitropical countries north of the equator, and with the dry season south of the equator. Changes in temperature and humidity correspond with the spread of the disease. Many host and environmental risk factors contribute to RSV-associated ARTI and hospitalizations including prematurity, overcrowded living conditions, passive exposure to tobacco smoke, and bronchopulmonary dysplasia/chronic lung disease. Detecting RSV-associated ARTI in resource-limited countries will contribute to minimizing irrational antibiotic use. Research is needed to develop effective vaccines and antiviral agents to tackle the increasing RSV-associated ARTI burden.
Footnotes
Conflict of Interest None declared.
References
- 1.Murray C J, Lopez A D.Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study Lancet 1997349(9063):1436–1442. [DOI] [PubMed] [Google Scholar]
- 2.Creer D D, Dilworth J P, Gillespie S H et al. Aetiological role of viral and bacterial infections in acute adult lower respiratory tract infection (LRTI) in primary care. Thorax. 2006;61(01):75–79. doi: 10.1136/thx.2004.027441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peck A J, Holman R C, Curns A T et al. Lower respiratory tract infections among American Indian and Alaska Native children and the general population of U.S. Children. Pediatr Infect Dis J. 2005;24(04):342–351. doi: 10.1097/01.inf.0000157250.95880.91. [DOI] [PubMed] [Google Scholar]
- 4.Gröndahl B, Puppe W, Hoppe A, Kühne I, Weigl J A, Schmitt H J. Rapid identification of nine microorganisms causing acute respiratory tract infections by single-tube multiplex reverse transcription-PCR: feasibility study. J Clin Microbiol. 1999;37(01):1–7. doi: 10.1128/jcm.37.1.1-7.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forgie I M, Campbell H, Lloyd-Evans N et al. Etiology of acute lower respiratory tract infections in children in a rural community in The Gambia. Pediatr Infect Dis J. 1992;11(06):466–473. doi: 10.1097/00006454-199206000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Technical Advisory Group on ARI. A program for controlling ARI in children: memorandum from a WHO meeting. Bull World Health Organ. 1984;64:47–58. [PMC free article] [PubMed] [Google Scholar]
- 7.Roca A, Loscertales M P, Quintó Let al. Genetic variability among group A and B respiratory syncytial viruses in Mozambique: identification of a new cluster of group B isolates J Gen Virol 200182(Pt 1):103–111. [DOI] [PubMed] [Google Scholar]
- 8.Bezerra P G, Britto M CO, Correia J B et al. Viral and atypical bacterial detection in acute respiratory infection in children under five years. PLoS One. 2011;6(04):e18928. doi: 10.1371/journal.pone.0018928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi E H, Lee H J, Kim S J et al. The association of newly identified respiratory viruses with lower respiratory tract infections in Korean children, 2000-2005. Clin Infect Dis. 2006;43(05):585–592. doi: 10.1086/506350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wasem S, Weichert S, Walther S et al. Lower respiratory tract disease in children: constant pathogens - constant management?! Klin Padiatr. 2008;220(05):291–295. doi: 10.1055/s-2007-990301. [DOI] [PubMed] [Google Scholar]
- 11.Kwofie T B, Anane Y A, Nkrumah B, Annan A, Nguah S B, Owusu M. Respiratory viruses in children hospitalized for acute lower respiratory tract infection in Ghana. Virol J. 2012;9:78. doi: 10.1186/1743-422X-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Camps M, Ricart S, Dimova V et al. Prevalence of human metapneumovirus among hospitalized children younger than 1 year in Catalonia, Spain. J Med Virol. 2008;80(08):1452–1460. doi: 10.1002/jmv.21209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang L F, Wang T L, Tang H F, Chen Z M. Viral pathogens of acute lower respiratory tract infection in China. Indian Pediatr. 2008;45(12):971–975. [PubMed] [Google Scholar]
- 14.Numazaki K, Chiba S, Umetsu M et al. Etiological agents of lower respiratory tract infections in Japanese children. In Vivo. 2004;18(01):67–71. [PubMed] [Google Scholar]
- 15.Jacques J, Bouscambert-Duchamp M, Moret H et al. Association of respiratory picornaviruses with acute bronchiolitis in French infants. J Clin Virol. 2006;35(04):463–466. doi: 10.1016/j.jcv.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 16.Sung C C, Chi H, Chiu N C et al. Viral etiology of acute lower respiratory tract infections in hospitalized young children in Northern Taiwan. J Microbiol Immunol Infect. 2011;44(03):184–190. doi: 10.1016/j.jmii.2011.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noyola D E, Rodríguez-Moreno G, Sánchez-Alvarado J, Martínez-Wagner R, Ochoa-Zavala J R. Viral etiology of lower respiratory tract infections in hospitalized children in Mexico. Pediatr Infect Dis J. 2004;23(02):118–123. doi: 10.1097/01.inf.0000110269.46528.a5. [DOI] [PubMed] [Google Scholar]
- 18.Shafik C F, Mohareb E W, Yassin A S et al. Viral etiologies of lower respiratory tract infections among Egyptian children under five years of age. BMC Infect Dis. 2012;12:350. doi: 10.1186/1471-2334-12-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan P W, Goh A Y, Chua K B, Kharullah N S, Hooi P S. Viral aetiology of lower respiratory tract infection in young Malaysian children. J Paediatr Child Health. 1999;35(03):287–290. doi: 10.1046/j.1440-1754.1999.00359.x. [DOI] [PubMed] [Google Scholar]
- 20.Hatipoğlu N, Somer A, Badur S et al. Viral etiology in hospitalized children with acute lower respiratory tract infection. Turk J Pediatr. 2011;53(05):508–516. [PubMed] [Google Scholar]
- 21.Wright P F, Wright M D. Progress in the prevention and treatment of RSV infection. N Engl J Med. 2014;371(08):776–777. doi: 10.1056/NEJMe1407467. [DOI] [PubMed] [Google Scholar]
- 22.Blount R E, Jr, Morris J A, Savage R E. Recovery of cytopathogenic agent from chimpanzees with coryza. Proc Soc Exp Biol Med. 1956;92(03):544–549. doi: 10.3181/00379727-92-22538. [DOI] [PubMed] [Google Scholar]
- 23.Schickli J H, Dubovsky F, Tang R S. Challenges in developing a pediatric RSV vaccine. Hum Vaccin. 2009;5(09):582–591. doi: 10.4161/hv.9131. [DOI] [PubMed] [Google Scholar]
- 24.Chanock R M, Kim H W, Vargosko A J et al. Respiratory syncytial virus. I. Virus recovery and other observations during 1960 outbreak of bronchiolitis, pneumonia, and minor respiratory diseases in children. JAMA. 1961;176:647–653. [PubMed] [Google Scholar]
- 25.Vandini S, Biagi C, Lanari M. Respiratory syncytial virus: the influence of serotype and genotype variability on clinical course of infection. Int J Mol Sci. 2017;18(08):1717. doi: 10.3390/ijms18081717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eshaghi A, Duvvuri V R, Lai R et al. Genetic variability of human respiratory syncytial virus A strains circulating in Ontario: a novel genotype with a 72 nucleotide G gene duplication. PLoS One. 2012;7(03):e32807. doi: 10.1371/journal.pone.0032807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fuentes S, Tran K C, Luthra P, Teng M N, He B. Function of the respiratory syncytial virus small hydrophobic protein. J Virol. 2007;81(15):8361–8366. doi: 10.1128/JVI.02717-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kiss G, Holl J M, Williams G M et al. Structural analysis of respiratory syncytial virus reveals the position of M2-1 between the matrix protein and the ribonucleoprotein complex. J Virol. 2014;88(13):7602–7617. doi: 10.1128/JVI.00256-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall C B.Respiratory syncytial virus: its transmission in the hospital environment Yale J Biol Med 198255(3–4):219–223. [PMC free article] [PubMed] [Google Scholar]
- 30.French C E, McKenzie B C, Coope C et al. Risk of nosocomial respiratory syncytial virus infection and effectiveness of control measures to prevent transmission events: a systematic review. Influenza Other Respir Viruses. 2016;10(04):268–290. doi: 10.1111/irv.12379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hall C B, Hall C B. Nosocomial respiratory syncytial virus infections: the “Cold War” has not ended. Clin Infect Dis. 2000;31(02):590–596. doi: 10.1086/313960. [DOI] [PubMed] [Google Scholar]
- 32.Avendaño L F, Larrañaga C, Palomino M A et al. Community- and hospital-acquired respiratory syncytial virus infections in Chile. Pediatr Infect Dis J. 1991;10(08):564–568. doi: 10.1097/00006454-199108000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Zhao D, Peng D, Li L, Zhang Q, Zhang C. Inhibition of G1P3 expression found in the differential display study on respiratory syncytial virus infection. Virol J. 2008;5:114. doi: 10.1186/1743-422X-5-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heilman C A. Respiratory syncytial and parainfluenza viruses. J Infect Dis. 1990;161(03):402–406. doi: 10.1093/infdis/161.3.402. [DOI] [PubMed] [Google Scholar]
- 35.Erdman D D, Weinberg G A, Edwards K M et al. GeneScan reverse transcription-PCR assay for detection of six common respiratory viruses in young children hospitalized with acute respiratory illness. J Clin Microbiol. 2003;41(09):4298–4303. doi: 10.1128/JCM.41.9.4298-4303.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pullan C R, Hey E N.Wheezing, asthma, and pulmonary dysfunction 10 years after infection with respiratory syncytial virus in infancy Br Med J (Clin Res Ed) 1982284(6330):1665–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu P, Hartert T V. Evidence for a causal relationship between respiratory syncytial virus infection and asthma. Expert Rev Anti Infect Ther. 2011;9(09):731–745. doi: 10.1586/eri.11.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Henderson J, Hilliard T N, Sherriff A, Stalker D, Al Shammari N, Thomas H M. Hospitalization for RSV bronchiolitis before 12 months of age and subsequent asthma, atopy and wheeze: a longitudinal birth cohort study. Pediatr Allergy Immunol. 2005;16(05):386–392. doi: 10.1111/j.1399-3038.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 39.Stensballe L G, Devasundaram J K, Simoes E A.Respiratory syncytial virus epidemics: the ups and downs of a seasonal virus Pediatr Infect Dis J 200322(2, Suppl):S21–S32. [DOI] [PubMed] [Google Scholar]
- 40.Simoes E A, Carbonell-Estrany X.Impact of severe disease caused by respiratory syncytial virus in children living in developed countries Pediatr Infect Dis J 200322(2, Suppl)S13–S18., discussion S18–S20 [DOI] [PubMed] [Google Scholar]
- 41.Weber M W, Mulholland E K, Greenwood B M. Respiratory syncytial virus infection in tropical and developing countries. Trop Med Int Health. 1998;3(04):268–280. doi: 10.1046/j.1365-3156.1998.00213.x. [DOI] [PubMed] [Google Scholar]
- 42.Nagayama Y, Tsubaki T, Nakayama S et al. Gender analysis in acute bronchiolitis due to respiratory syncytial virus. Pediatr Allergy Immunol. 2006;17(01):29–36. doi: 10.1111/j.1399-3038.2005.00339.x. [DOI] [PubMed] [Google Scholar]
- 43.Falsey A R, Walsh E E. Respiratory syncytial virus infection in adults. Clin Microbiol Rev. 2000;13(03):371–384. doi: 10.1128/cmr.13.3.371-384.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shi T, McAllister D AL, O'Brien K Let al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study Lancet 2017390(10098):946–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Borse R H, Singleton R J, Bruden D T, Fry A M, Hennessy T W, Meltzer M I. The economics of strategies to reduce respiratory syncytial virus hospitalizations in Alaska. J Pediatric Infect Dis Soc. 2014;3(03):201–212. doi: 10.1093/jpids/pit072. [DOI] [PubMed] [Google Scholar]
- 46.Matheson J W, Rich F J, Cohet C et al. Distinct patterns of evolution between respiratory syncytial virus subgroups A and B from New Zealand isolates collected over thirty-seven years. J Med Virol. 2006;78(10):1354–1364. doi: 10.1002/jmv.20702. [DOI] [PubMed] [Google Scholar]
- 47.Law B J, Carbonell-Estrany X, Simoes E AF. An update on RSV epidemiology: a developed country perspective. J Res Med. 2002;96:2–7. [PubMed] [Google Scholar]
- 48.Sato M, Saito R, Sakai T et al. Molecular epidemiology of respiratory syncytial virus infections among children with acute respiratory symptoms in a community over three seasons. J Clin Microbiol. 2005;43(01):36–40. doi: 10.1128/JCM.43.1.36-40.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huo X, Fang B, Liu L et al. Clinical and epidemiologic characteristics of respiratory syncytial virus infection among children aged <5 years, Jingzhou City, China, 2011. J Infect Dis. 2013;208(03) 03:S184–S188. doi: 10.1093/infdis/jit518. [DOI] [PubMed] [Google Scholar]
- 50.Jin Y, Zhang R F, Xie Z P et al. Newly identified respiratory viruses associated with acute lower respiratory tract infections in children in Lanzou, China, from 2006 to 2009. Clin Microbiol Infect. 2012;18(01):74–80. doi: 10.1111/j.1469-0691.2011.03541.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang H Y, Li Z M, Zhang G L, Diao T T, Cao C X, Sun H Q. Respiratory viruses in hospitalized children with acute lower respiratory tract infections in Harbin, China. Jpn J Infect Dis. 2009;62(06):458–460. [PubMed] [Google Scholar]
- 52.Chan D CW, Chiu W K, Ip P LS. Respiratory syncytial virus and influenza infections among children ≤3 years of age with acute respiratory infections in a regional hospital in Hong Kong. HK J Paediatr. 2007;12:15–21. [Google Scholar]
- 53.Khor C S, Sam I C, Hooi P S, Quek K F, Chan Y F. Epidemiology and seasonality of respiratory viral infections in hospitalized children in Kuala Lumpur, Malaysia: a retrospective study of 27 years. BMC Pediatr. 2012;12(32):32. doi: 10.1186/1471-2431-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Do L AH, Bryant J E, Tran A T et al. Respiratory syncytial virus and other viral infections among children under two years old in southern Vietnam 2009–2010: clinical characteristics and disease severity. PLoS One. 2016;11(08):e0160606. doi: 10.1371/journal.pone.0160606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Malasao R, Okamoto M, Chaimongkol N et al. Molecular characterization of human respiratory syncytial virus in the Philippines, 2012–2013. PLoS One. 2015;10(11):e0142192. doi: 10.1371/journal.pone.0142192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee J T, Chang L Y, Wang L C et al. Epidemiology of respiratory syncytial virus infection in northern Taiwan, 2001-2005 -- seasonality, clinical characteristics, and disease burden. J Microbiol Immunol Infect. 2007;40(04):293–301. [PubMed] [Google Scholar]
- 57.Fry A M, Chittaganpitch M, Baggett H C et al. The burden of hospitalized lower respiratory tract infection due to respiratory syncytial virus in rural Thailand. PLoS One. 2010;5(11):e15098. doi: 10.1371/journal.pone.0015098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mathisen M, Strand T A, Sharma B N et al. RNA viruses in community-acquired childhood pneumonia in semi-urban Nepal; a cross-sectional study. BMC Med. 2009;7:35. doi: 10.1186/1741-7015-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cherian T, Simoes E A, Steinhoff M C et al. Bronchiolitis in tropical south India. Am J Dis Child. 1990;144(09):1026–1030. doi: 10.1001/archpedi.1990.02150330086028. [DOI] [PubMed] [Google Scholar]
- 60.Hasan K, Jolly P, Marquis G et al. Viral etiology of pneumonia in a cohort of newborns till 24 months of age in rural Mirzapur, Bangladesh. Scand J Infect Dis. 2006;38(08):690–695. doi: 10.1080/00365540600606473. [DOI] [PubMed] [Google Scholar]
- 61.Homaira N, Luby S P, Petri W A et al. Incidence of respiratory virus-associated pneumonia in urban poor young children of Dhaka, Bangladesh, 2009-2011. PLoS One. 2012;7(02):e32056. doi: 10.1371/journal.pone.0032056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bashir U, Alam M M, Sadia H, Zaidi S SZ, Kazi B M. Molecular characterization of circulating respiratory syncytial virus (RSV) genotypes in Gilgit Baltistan Province of Pakistan during 2011-2012 winter season. PLoS One. 2013;8(09):e74018. doi: 10.1371/journal.pone.0074018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ali A, Yousafzai M T, Waris R et al. RSV associated hospitalizations in children in Karachi, Pakistan: implications for vaccine prevention strategies. J Med Virol. 2017;89(07):1151–1157. doi: 10.1002/jmv.24768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Muthulingam A, Noordeen F, Morel A. Viral etiology in hospitalized children with acute respiratory tract infection in the Kegalle area of Sri Lanka. J Pediatr Infect Dis. 2014;9(04):167–170. [Google Scholar]
- 65.Hon K L, Leung T F, Cheng W Y et al. Respiratory syncytial virus morbidity, premorbid factors, seasonality, and implications for prophylaxis. J Crit Care. 2012;27(05):464–468. doi: 10.1016/j.jcrc.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 66.Nair H, Nokes D J, Gessner B Det al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis Lancet 2010375(9725):1545–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yoshida L M, Suzuki M, Thiem V Det al. Population based cohort study for pediatric infectious diseases research in Vietnam Trop Med Health 201442(2, Suppl):47–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Al-Toum R, Bdour S, Ayyash H. Epidemiology and clinical characteristics of respiratory syncytial virus infections in Jordan. J Trop Pediatr. 2006;52(04):282–287. doi: 10.1093/tropej/fml002. [DOI] [PubMed] [Google Scholar]
- 69.Mathisen M, Strand T A, Sharma B N et al. Clinical presentation and severity of viral community-acquired pneumonia in young Nepalese children. Pediatr Infect Dis J. 2010;29(01):e1–e6. doi: 10.1097/INF.0b013e3181c2a1b9. [DOI] [PubMed] [Google Scholar]
- 70.Jayaweera J AAS, Noordeen F, Morel A J et al. Viral burden in acute respiratory tract infections in hospitalized children in the wet and dry zones of Sri Lanka. Int J Infect Dis. 2016;45(01):463. doi: 10.1371/journal.pone.0259443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hammitt L L, Kazungu S, Morpeth S C et al. A preliminary study of pneumonia etiology among hospitalized children in Kenya. Clin Infect Dis. 2012;54(02) 02:S190–S199. doi: 10.1093/cid/cir1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86(05):408–416. doi: 10.2471/BLT.07.048769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thompson W WT, Shay D K, Weintraub E et al. Mortality associated with Influenza and RSV in the United States. JAMA. 2003;289(02):179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 74.Bloom-Feshbach K, Alonso W J, Charu V et al. Latitudinal variations in seasonal activity of influenza and respiratory syncytial virus (RSV): a global comparative review. PLoS One. 2013;8(02):e54445. doi: 10.1371/journal.pone.0054445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sigurs N, Bjarnason R, Sigurbergsson F, Kjellman B. Respiratory syncytial virus bronchiolitis in infancy is an important risk factor for asthma and allergy at age 7. Am J Respir Crit Care Med. 2000;161(05):1501–1507. doi: 10.1164/ajrccm.161.5.9906076. [DOI] [PubMed] [Google Scholar]
- 76.Dowell S F, Anderson L J, Gary H E, Jr et al. Respiratory syncytial virus is an important cause of community-acquired lower respiratory infection among hospitalized adults. J Infect Dis. 1996;174(03):456–462. doi: 10.1093/infdis/174.3.456. [DOI] [PubMed] [Google Scholar]
- 77.Stewart K D, Nguyen V, Nguyen S. RSV infection in the immunocompromised host. US Pharm. 2013;38:8–10. [Google Scholar]
- 78.Wu P, Dupont W D, Griffin M R et al. Evidence of a causal role of winter virus infection during infancy in early childhood asthma. Am J Respir Crit Care Med. 2008;178(11):1123–1129. doi: 10.1164/rccm.200804-579OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Walsh E E, Peterson D R, Falsey A R. Risk factors for severe respiratory syncytial virus infection in elderly persons. J Infect Dis. 2004;189(02):233–238. doi: 10.1086/380907. [DOI] [PubMed] [Google Scholar]
- 80.Falsey A R, Hennessey P A, Formica M A, Cox C, Walsh E E. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352(17):1749–1759. doi: 10.1056/NEJMoa043951. [DOI] [PubMed] [Google Scholar]
- 81.Cane P A, Pringle C R. Evolution of subgroup A respiratory syncytial virus: evidence for progressive accumulation of amino acid changes in the attachment protein. J Virol. 1995;69(05):2918–2925. doi: 10.1128/jvi.69.5.2918-2925.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Heminway B R, Yu Y, Tanaka Y et al. Analysis of respiratory syncytial virus F, G, and SH proteins in cell fusion. Virology. 1994;200(02):801–805. doi: 10.1006/viro.1994.1245. [DOI] [PubMed] [Google Scholar]
- 83.Agoti C N, Otieno J R, Munywoki P K et al. Local evolutionary patterns of human respiratory syncytial virus derived from whole-genome sequencing. J Virol. 2015;89(07):3444–3454. doi: 10.1128/JVI.03391-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Venter M, Madhi S A, Tiemessen C T, Schoub B D.Genetic diversity and molecular epidemiology of respiratory syncytial virus over four consecutive seasons in South Africa: identification of new subgroup A and B genotypes J Gen Virol 200182(Pt 9):2117–2124. [DOI] [PubMed] [Google Scholar]
- 85.Gaunt E R, Jansen R R, Poovorawan Y, Templeton K E, Toms G L, Simmonds P. Molecular epidemiology and evolution of human respiratory syncytial virus and human metapneumovirus. PLoS One. 2011;6(03):e17427. doi: 10.1371/journal.pone.0017427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zou L, Yi L, Wu J et al. Evolution and transmission of respiratory syncytial group a (RSV-A) viruses in Guangdong, China 2008–2015. Front Microbiol. 2016;7:1263. doi: 10.3389/fmicb.2016.01263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Coiras M T, Aguilar J C, García M L, Casas I, Pérez-Breña P. Simultaneous detection of fourteen respiratory viruses in clinical specimens by two multiplex reverse transcription nested-PCR assays. J Med Virol. 2004;72(03):484–495. doi: 10.1002/jmv.20008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vilcek S, Elvander M, Ballagi-Pordány A, Belák S. Development of nested PCR assays for detection of bovine respiratory syncytial virus in clinical samples. J Clin Microbiol. 1994;32(09):2225–2231. doi: 10.1128/jcm.32.9.2225-2231.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hu A, Colella M, Tam J S, Rappaport R, Cheng S M. Simultaneous detection, subgrouping, and quantitation of respiratory syncytial virus A and B by real-time PCR. J Clin Microbiol. 2003;41(01):149–154. doi: 10.1128/JCM.41.1.149-154.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Osiowy C. Direct detection of respiratory syncytial virus, parainfluenza virus, and adenovirus in clinical respiratory specimens by a multiplex reverse transcription-PCR assay. J Clin Microbiol. 1998;36(11):3149–3154. doi: 10.1128/jcm.36.11.3149-3154.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ali S A, Gern J E, Hartert T V et al. Real-world comparison of two molecular methods for detection of respiratory viruses. Virol J. 2011;8:332. doi: 10.1186/1743-422X-8-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rodriguez W J, Hall C B, Welliver R et al. Efficacy and safety of aerosolized ribavirin in young children hospitalized with influenza: a double-blind, multicenter, placebo-controlled trial. J Pediatr. 1994;125(01):129–135. doi: 10.1016/s0022-3476(94)70139-3. [DOI] [PubMed] [Google Scholar]
- 93.American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. J Pediatr. 2006;118(04):1774–1793. doi: 10.1542/peds.2006-2223. [DOI] [PubMed] [Google Scholar]
- 94.Turner T L, Kopp B T, Paul G, Landgrave L C, Hayes D, Jr, Thompson R. Respiratory syncytial virus: current and emerging treatment options. Clinicoecon Outcomes Res. 2014;6:217–225. doi: 10.2147/CEOR.S60710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hu J, Robinson J L. Treatment of respiratory syncytial virus with palivizumab: a systematic review. World J Pediatr. 2010;6(04):296–300. doi: 10.1007/s12519-010-0230-z. [DOI] [PubMed] [Google Scholar]
- 96.Homaira N, Rawlinson W, Snelling T L, Jaffe A. Effectiveness of Palivizumab in preventing RSV hospitalization in high risk children: a real-world perspective. Int J Pediatr. 2014;2014:571609. doi: 10.1155/2014/571609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.American Academy of Pediatrics Committee on Infectious Diseases and Bronchiolitis Guidelines Committee. Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. J Pediatr. 2014;134:415–420. doi: 10.1542/peds.2014-1665. [DOI] [PubMed] [Google Scholar]
- 98.Stobart C C, Rostad C A, Ke Zet al. A live RSV vaccine with engineered thermostability is immunogenic in cotton rats despite high attenuation Nat Commun 20167(13916):13916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Caidi H, Harcourt J L, Tripp R A, Anderson L J, Haynes L M. Combination therapy using monoclonal antibodies against respiratory syncytial virus (RSV) G glycoprotein protects from RSV disease in BALB/c mice. PLoS One. 2012;7(12):e51485. doi: 10.1371/journal.pone.0051485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chávez-Bueno S, Mejías A, Merryman R A, Ahmad N, Jafri H S, Ramilo O. Intravenous palivizumab and ribavirin combination for respiratory syncytial virus disease in high-risk pediatric patients. Pediatr Infect Dis J. 2007;26(12):1089–1093. doi: 10.1097/INF.0b013e3181343b7e. [DOI] [PubMed] [Google Scholar]


