Abstract
Mechanical ventilation practices in patients with acute respiratory distress syndrome (ARDS) have progressed with a growing understanding of the disease pathophysiology. Paramount to the care of affected patients is the delivery of lung-protective mechanical ventilation which prioritizes tidal volume and plateau pressure limitation. Lung protection can probably be further enhanced by scaling target tidal volumes to the specific respiratory mechanics of individual patients. The best procedure for selecting optimal positive end-expiratory pressure (PEEP) in ARDS remains uncertain; several relevant issues must be considered when selecting PEEP, particularly lung recruitability. Noninvasive ventilation must be used with caution in ARDS as excessively high respiratory drive can further exacerbate lung injury; newer modes of delivery offer promising approaches in hypoxemic respiratory failure. Airway pressure release ventilation offers an alternative approach to maximize lung recruitment and oxygenation, but clinical trials have not demonstrated a survival benefit of this mode over conventional ventilation strategies. Rescue therapy with high-frequency oscillatory ventilation is an important option in refractory hypoxemia. Despite a disappointing lack of benefit (and possible harm) in patients with moderate or severe ARDS, possibly due to lung hyperdistention and right ventricular dysfunction, high-frequency oscillation may improve outcome in patients with very severe hypoxemia.
Keywords: acute respiratory distress syndrome, mechanical ventilation, positive end-expiratory pressure, high-frequency oscillation, noninvasive ventilation, oxygen
Mechanical ventilation is the mainstay of therapy for acute respiratory distress syndrome (ARDS)—apart from mechanical ventilation, ARDS would likely not have been recognized. Recognizing the importance of avoiding lung injury and ensuring adequate gas exchange, optimal ventilator management in ARDS has been the subject of intensive research efforts for the last several decades, and will continue to be such for decades to come. This review provides a state-of-the-art summary of several aspects of mechanical ventilator management in ARDS. Given the widespread appreciation for the heterogeneity of this syndrome, possibilities for optimization through personalization are emphasized throughout.
Optimizing Tidal Volume
Lower tidal volumes ( V T ) attenuate biophysical lung injury by several mechanisms. Preventing frank overdistension (volutrauma/barotrauma), 1 2 3 decreasing tidal shear strain in regions of mechanical heterogeneity, 4 5 and reducing cyclic opening and collapse of small airways/alveoli (atelectrauma) 6 7 8 all reduce cellular and extracellular matrix injury. 9 10 11 Multicenter trials have demonstrated that targeting V T of 6 mL/kg predicted body weight (PBW), compared with 12 mL/kg PBW, expedites resolution of multiple organ failures, lessens systemic inflammation, and improves survival in patients with ARDS. 1 2 12 13
However, while 6 is superior to 12 mL/kg PBW, the ideal V T strategy in ARDS is unknown. Two mechanistic human studies have found lowering V T below 6 mL/kg PBW by means of extracorporeal life support as needed to maintain adequate gas exchange may attenuate systemic inflammation in select patients with severe ARDS and poor respiratory system compliance. 14 15 The recently published EOLIA trial aimed to address this question by randomizing patients with severe ARDS to conventional mechanical ventilation (CMV) or extracorporeal membrane oxygenation. 16 This trial was stopped early by the data safety monitoring board and failed to demonstrate a statistical difference in the primary outcome of mortality at 60 days. Reanalysis of the EOLIA trial suggested that this biological signal with ultra-low V T for very severe ARDS may translate to clinical benefit. 16 17 Readers are guided to the accompanying section on mechanical circulatory support for more details.
Existing data indicate that no arbitrary V T threshold, even if scaled to PBW, is universally protective for all patients. 18 19 20 Rather, an ideal V T strategy likely must incorporate two related patient-specific factors: mechanics and biology. 21
Several approaches have gained interest recently for adjusting V T according to mechanics. Perhaps most immediately clinically accessible is airway driving pressure, defined as plateau pressure minus positive end-expiratory pressure (PEEP). Airway driving pressure is equivalent mathematically to V T scaled to the individual patient's respiratory system compliance ( V T / C RS ) ( Fig. 1 ). It was highly correlated with mortality independent of V T in a secondary analysis of multiple ARDS randomized trials. 22 Airway driving pressure also appears highly correlated with V T scaled to lung compliance (transpulmonary driving pressure = V T / C L ). 23 Typical transpulmonary driving pressure is roughly 5 to 10 cm H 2 O with normal spontaneous breathing in healthy individuals, 24 25 indicating the usual amount of global stress experienced across the lung in health. However, transpulmonary driving pressure can be substantially higher in patients with ARDS due to changes in compliance of the injured lung. 21 26 Targeting healthy normal driving pressure during ARDS has intuitive appeal for this reason, but its role for enhancing lung protection remains to be tested directly in prospective clinical trials.
Fig. 1.
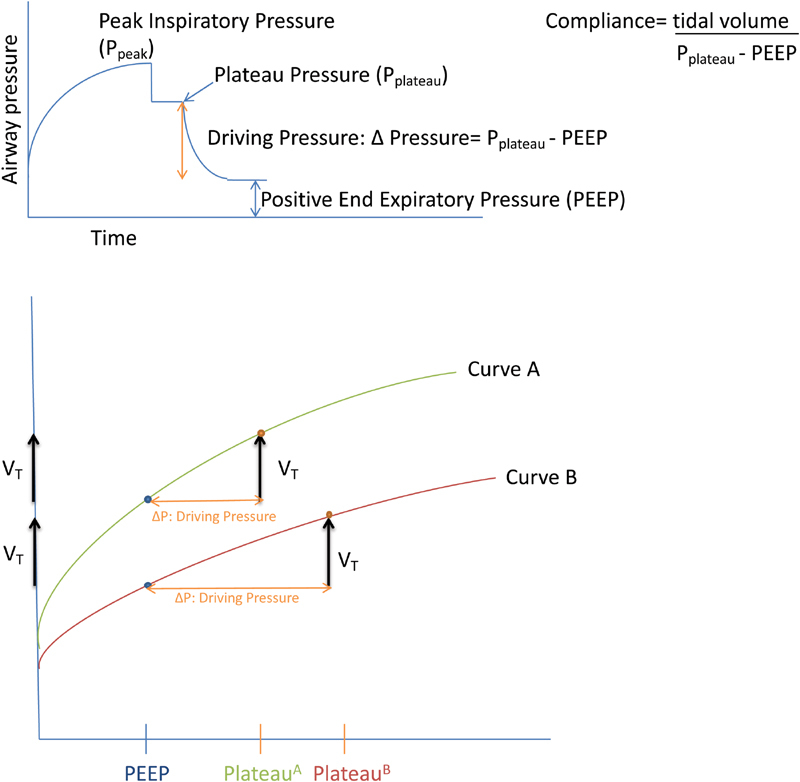
Driving pressure and compliance. Top panel: respiratory pressures generated during a volume-controlled ventilation breath with an end-inspiratory pause. After generation of the peak inspiratory pressure, a pause allows for static conditions and the measurement of plateau pressure. The difference between the plateau and end-expiratory pressure is the airway driving pressure. Respiratory system compliance is the tidal volume divided by the driving pressure. Bottom panel: the effect of compliance on driving pressure. On this pressure–volume graph, compared with curve B, curve A illustrates a patient with increased respiratory system compliance and as a result at a given tidal volume there is reduced driving pressure.
Volume-based strategies for individualizing V T to mechanics include scaling V T to either functional residual capacity (FRC) measured at end-expiration ( V T /FRC) or inspiratory capacity (IC) measured during a maximal insufflation maneuver ( V T /IC). FRC-based approaches use computed tomography imaging, nitrogen wash-out/wash-in, or helium dilution to measure end-expiratory lung volume, 26 27 28 after which V T might be set to equal a certain percentage of that volume. Of course, FRC may change rapidly with any adjustment in ventilator pressures or volumes and with the evolution of ARDS, requiring frequent reassessment. While important research tools, feasibility and availability of the techniques may limit broad clinical application. Measuring IC can be done at bedside with any modern ventilator able to report volume change in response to change in pressure, 23 but lung recruitment and hyperinflation may complicate measurement, and limited data exist on this approach. As with driving pressure, no threshold has been proposed nor strategy tested prospectively for scaling V T to these volume-based measures.
Indeed, it is likely that no universal threshold for lung protection exists regardless of how V T is scaled to patient-specific mechanics. Rather, the extent to which a given V T causes lung injury likely also depends on concomitant biological risk, including endothelial injury/activation, local/systemic inflammation, a primary alveolar epithelial insult, and heterogeneous distribution of injury patterns further confounding the ability to personalize lung protective ventilation. 29 30 31
Currently, no clinically available, well-validated metric to assess risk of biophysical injury is available. Lung injury prediction scores from clinical data have not identified risk of ARDS with sufficient accuracy for clinical use, 32 33 and similar is likely true of risk of biophysical injury in established ARDS. Both instances likely require incorporating molecular markers of lung injury to assess patient-specific risk. 34 Two potential plasma markers of promise are soluble receptor for advanced glycation end-products (sRAGE), a marker of alveolar epithelial injury, 35 36 37 38 and angiopoietin-2, a marker of vascular endothelial injury. 39 40 41 Whether these or other biomarkers, alone or in combination, identify risk of biophysical injury with sufficient reliability for clinical use remains to be tested.
Ideally, biomarker(s) might facilitate risk stratification for biophysical injury and allow the clinician to weigh risks/benefits of adjusting V T . Even if threshold mechanical and biological measures are established, lung protection is not the sole goal in titrating V T . Maintaining lower sub-physiologic V T requires escalating cointerventions that carry their own risks. Deeper sedation and/or neuromuscular blockade may be required to facilitate patient tolerance and suppress ventilatory drive, which in turn increase risk of delirium and disuse atrophy of the diaphragm and other skeletal muscle. 42 43 44 45 Extreme lowering of V T (e.g., 3 mL/kg PBW) may require extracorporeal life support to facilitate adequate gas exchange, which may heighten risk of hemorrhage, hematological, and neurological complications. 46
To truly individualize V T for patient-centered benefit will require (1) identifying who is at risk of biophysical injury, (2) developing an approach for titrating V T to risk, and (3) weighing clinically the tradeoff between further lung protection and escalating cointerventions required for lowering V T . Research in lung mechanics and biology is advancing toward that goal at an increasingly rapid pace, with clinical protocols ready for testing on the horizon.
Positive End-Expiratory Pressure and Lung Recruitment
Since the first description of ARDS by Ashbaugh and colleagues, PEEP has been integral to the management of hypoxemia in ARDS. 47 48 More recently, the use of higher PEEP has been studied as a possible strategy to avoid lung injury. While several strategies for optimizing PEEP have been tested, none have yet shown a mortality benefit and one strategy was even associated with harm in ARDS patients. Consequently, PEEP titration remains a controversial area of ventilator management and great care must be taken when applying PEEP at the bedside.
Physiological Basis for Titrating PEEP
Applied at the correct level, PEEP might mitigate the risk of ventilator-induced lung injury (VILI). By preventing end-expiratory collapse of alveoli and small airways during tidal ventilation, PEEP prevents the shear stresses resulting from cyclic opening and closing of alveolar units—“atelectrauma.” 49 50 PEEP effectively reduces intrapulmonary shunt and improves oxygenation by opening collapsed lung units to participate in gas exchange. 51 Increasing the number of aerated lung units participating in ventilation reduces the dynamic tidal strain and stress applied to the lung 52 53 ( Fig. 2 ). Finally, lung recruitment by PEEP results in more homogeneous inflation of the lung; this can significantly reduce mechanical stress resulting from local inhomogeneities in the lung, which act as stress multipliers. 4
Fig. 2.
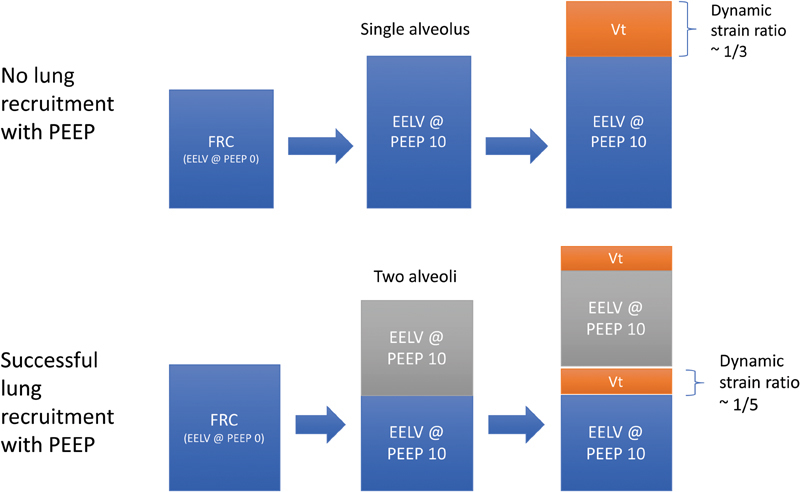
The effect of PEEP on dynamic strain depends on recruitability of the lungs. In the top panel, applying PEEP to the lung increases lung volume but because no additional alveoli are recruited, tidal ventilation is applied to the single alveolar unit and this unit experiences all of the dynamic strain. The amount of strain applied to the lung is determined by the ratio of tidal volume to end-expiratory lung volume ( V T /EELV) at a given PEEP and FRC. In this theoretical (and simplified) representation, dynamic strain is approximately one-third in the nonrecruitable lung. In the bottom panel, applying PEEP to the lung increases lung volume and recruits an additional previously collapsed alveolus to participate in tidal ventilation. The same tidal volume is now distributed between two alveolar units, hence decreasing the dynamic strain experienced by each individual unit. This is the mechanism by which lung recruitment from PEEP is thought to decrease dynamic stress and strain. EELV, end-expiratory lung volume; FRC, functional residual capacity; PEEP, positive end-expiratory pressure.
At the same time, PEEP has important cardiorespiratory interactions which can limit the aforementioned physiological benefit. Depending on the underlying left ventricular function PEEP may improve cardiac output by a relative reduction in afterload. 54 At higher levels of PEEP, however, the increased intrathoracic pressure can be deleterious by elevating right atrial pressure, decreasing the gradient for venous return, 55 56 and reducing left ventricular preload—ultimately reducing cardiac output. 56 57 PEEP may also influence right ventricular performance indirectly by increasing pulmonary vascular resistance. 58 This occurs as elevated pressures occlude the alveolar septal vasculature, 59 thereby increasing right ventricular afterload and reducing cardiac output. 58 59
From a pulmonary parenchymal perspective, PEEP may contribute to VILI by over-distending aerated lung units. Given that the ARDS lung is functionally a “baby lung,” 60 applied PEEP that fails to open collapsed alveoli will injuriously overinflate residual lung units propagating lung inflammation and injury, similar to the effects of excess tidal volume. Therefore, the benefit and harm of PEEP on the patient's overall physiological condition will depend on how much lung can be recruited and on hemodynamic conditions. 48
Recruitment Maneuvers and the Open Lung Approach
In view of concerns about the injurious effects of atelectasis and potential benefits of PEEP, the “open lung approach” gained favor. 61 Opening pressures in alveolar units often exceed 35 cm H 2 O (the accepted safe upper limit of plateau pressure) 62 while the PEEP required to maintain patency after opening is lower. Thus, various “recruitment” maneuvers for maximally inflating the lung to optimize lung recruitment have been studied. A recruitment maneuver is a sustained increase in airway pressure with the goal to open collapsed alveoli, after which sufficient PEEP is applied to keep the lungs open. 63 A sustained inflation is the most commonly employed maneuver: the ventilator is set to continuous positive airway pressure (CPAP) mode and pressures are increased to 30 to 40 cm H 2 O for 30 to 40 seconds. 63 An alternate approach is the “staircase” maneuver involving progressive increases in PEEP while maintaining a constant airway driving pressure until a maximum peak pressure of 50 to 60 cm H 2 O is achieved. 62 The physiological effects of recruitment maneuvers are transient and depend on the concomitant PEEP strategy. 64 The effects of a recruitment maneuver on lung injury are unclear, and hemodynamic instability (hypotension and/or bradycardia) can occur during maneuvers. The benefits of lung recruitment depend on lung recruitability, but these maneuvers can be used as a diagnostic test to assess for recruitability. 65
Clinical Evidence Guiding the Delivery of PEEP
In patients with ARDS, no clinical trial has definitively concluded whether a high or low PEEP strategy is associated with improved outcomes. The ALVEOLI, 66 LOVS, 67 EXPRESS, 68 and ART trials 69 provide the highest quality evidence to answer the high versus low PEEP question. The LOVS and ALVEOLI trials were both randomized controlled clinical trials that compared high to low PEEP/FiO 2 tables in the ventilation management of patients with ARDS. In both of these trials, the higher PEEP arms resulted in increased mean arterial oxygen tensions 66 67 but neither trial was able to demonstrate a mortality benefit of a particular strategy. The French EXPRESS trial, though designed with a plateau pressure limit of 28 to 30 cm H 2 O, also failed to show a mortality benefit. 68
The recently published ART trial was a multicenter randomized controlled trial (RCT) including just over 1,000 patients with moderate-to-severe ARDS randomized to a lower PEEP or higher PEEP arm with aggressive lung recruitment maneuvers. 69 Surprisingly, and different from previous trials, the 28-day mortality rate was significantly higher in the higher PEEP plus recruitment maneuver group compared with the control arm (55 vs. 49%, respectively). Several methodological criticisms were raised about this trial. 70 One major concern was that the duration and amplitude of the lung recruitment maneuver in the experimental arm were excessive, increasing the risk of respiratory acidosis and barotrauma. 70 Peak recruitment pressures of 60 cm H 2 O and a recruitment time process of 24 minutes without ensuring adequate volume resuscitation might have explained in part the three cardiac arrests and seven pneumothoraces documented during recruitment. 69 A high proportion of patient–ventilator asynchrony in the experimental arm raised further concerns for significant VILI during controlled ventilation. 70 71 Some of these issues may explain this trial's disappointing result. Of note, a recent pilot RCT which also involved recruitment maneuvers and a decremental PEEP trial identifying the PEEP level associated with the maximum dynamic compliance demonstrated that an open lung approach improved oxygenation and respiratory system mechanics without detrimental effects on 60-day mortality, ventilator-free days, or barotrauma 72 and set the stage for a larger trial. 69
It is important to note that none of the trials to date have explicitly considered lung recruitability as a criterion for enrolment or as a prespecified factor for stratifying analysis of the primary end-point. Given the foregoing physiological considerations, lung recruitability is likely a key determinant of benefit or harm from PEEP. 73 The importance of considering recruitability is supported by the observations that the oxygenation response to increased PEEP predicts mortality 74 and that the effect of PEEP on mortality appears to be mediated by its effect on driving pressure 22 (since both favorable oxygenation responses and mechanical responses will reflect lung recruitment).
Optimal PEEP Management
In the contemporary management of patients with ARDS, the optimal approach to titrating PEEP remains unclear. It is clear that no strategy should attempt to apply a “one-size-fits-all” approach and individual variation in lung recruitability must be considered. The biological phenotype of ARDS may also be a crucially important consideration. 75 A variety of strategies for titrating PEEP are under investigation such as oxygen response to PEEP, 74 computed tomography, 76 driving pressure, 22 pressure–volume loops, 77 stress index, 78 esophageal manometry, 79 and electrical impedance tomography. 80 After 20 years of investigation, PEEP remains a challenging and important area of clinical investigation.
Noninvasive Ventilation for ARDS
The role of noninvasive ventilation (NIV) in the management of ARDS is controversial and evolving. Although the benefits of NIV for acute exacerbations of chronic obstructive pulmonary disease 81 and cardiogenic pulmonary edema are substantial, 82 evidence supporting the use of NIV in ARDS is limited. The potential to avoid invasive mechanical ventilation in patients with ARDS is intriguing given the known complications linked to invasive mechanical ventilation, deep sedation, neuromuscular blockade, and immobility. 83 Despite the paucity of evidence, NIV in ARDS is commonly used as an initial supportive therapy for ARDS 84 85 and was formally recognized as a therapeutic approach in the Berlin Criteria 86 defining ARDS.
Physiological Considerations
NIV has specific physiological effects in acute lung injury. PEEP can recruit lung to improve oxygenation but improves work of breathing to only a minor degree. Applying additional inspiratory pressure support further reduces work of breathing and dyspnea. 87 Given the high respiratory drive of patients with ARDS, 88 the use of pressure support to unload the respiratory muscles can lead to excessive tidal volumes, which are associated with NIV failure 89 and may exacerbate lung injury. 90 The concern for excessive tidal volume and inability to support the high respiratory drive of patients with ARDS was confirmed in the LUNG SAFE study. 91 This prospective multicenter observational study demonstrated that 15.5% of patients with ARDS are managed with NIV as an initial approach. Interestingly, NIV was applied at similar rates across all ARDS severity categories. Patients managed with NIV had lower levels of PEEP and higher respiratory rates and tidal volumes in comparison to invasively mechanically ventilated patients, highlighting the challenge of controlling respiratory drive with a noninvasive approach. 91 Furthermore, the inspiratory pressures required to improve the work of breathing may worsen mask leaks, gastric distension, and patient tolerance. 87
Evidence Base
Notwithstanding the technical challenges of NIV titration in ARDS, there are data indicating some success with this approach. Antonelli and colleagues 84 investigated NIV as a first-line approach to patients with ARDS and found that endotracheal intubations were prevented 54% of the time. Correspondingly, avoiding endotracheal intubation was associated with less ventilator-associated pneumonia and decreased intensive care unit (ICU) mortality. A meta-analysis of randomized and observational studies which included 540 patients similarly indicated that NIV is successful in ARDS approximately 50% of the time. 92 However, the heterogeneity of the studies prevented interpretation on the effect of NIV on other outcomes such as mortality.
Thus, as clinicians grapple with applying these limited data for clinical care, there are a few points to consider. First, the success of NIV for ARDS varies based on severity of hypoxemia. 93 The rates of NIV failure double as severity of ARDS increases from mild to moderate or severe, increasing from 22.2 to 42.3 and 47.1%, respectively. 91 This has led some to recommend that NIV in ARDS be restricted to patients with mild–moderate severity, defined as P a O 2 /FiO 2 ≥150 mm Hg. 93 Second, NIV failure is associated with worse outcomes, 94 which may reflect a higher severity of illness or possibly suggest that delays in intubation can be deleterious. Therefore, risk factors associated with NIV failure such as lack of improvement of the P a O 2 /FiO 2 ratio and shock 84 95 should be considered to optimize patient selection. In parallel, close observation for early signs of failure is needed to prevent delays in endotracheal intubation. A new bedside tool, the HACOR score (heart rate, acidosis, consciousness, oxygenation, and respiratory rate) has been developed and validated to predict NIV failure in hypoxemic patients with high accuracy at 1 hour of NIV to prevent intubation delays. 96 Finally, although there are data indicating possible harm with NIV in ARDS, it is important to consider the clinical context. A randomized clinical trial comparing the efficacy of standard oxygen, high-flow nasal cannula (HFNC), and NIV in patients with hypoxemic respiratory failure suggested increased mortality in the NIV group. 97 However, patients in the NIV group received NIV only for 8 hours a day for 2 days. Given that the physiological effects of NIV dissipate quickly after discontinuation, it is unclear if the NIV protocol mediated these findings as opposed to NIV per se.
The capacity to apply prolonged NIV at higher pressures may mediate success. One small single-center clinical trial examined the effect of the NIV interface on its success in ARDS. 98 The authors postulated that the helmet, a transparent hood that encompasses the entire head of the patient and has a seal at the neck, would enhance titration of positive pressure and be better tolerated in comparison to the traditional facemask. Endotracheal intubation rates were reduced from 62% in the facemask group to 18% in the helmet group. In addition, 90-day mortality was reduced by 22% with helmet NIV. In a 1-year follow-up study, the authors also demonstrated that the avoidance of endotracheal intubation was associated with improved long-term neuromuscular and functional outcomes in ARDS survivors. 99 Early termination of the clinical trial may have exaggerated the magnitude of the findings and these data need to be replicated in larger multicenter trials prior to widespread adoption.
There are no definitive recommendations for or against the use of NIV for ARDS due to the paucity of high-level evidence. 100 Invasive mechanical ventilation remains the mainstay of supportive care for ARDS. However, NIV may obviate the need for endotracheal intubation in carefully selected and closely monitored patients. Clinicians must weigh the risk of complications with invasive mechanical ventilation against the potential harm of NIV due to delays in endotracheal intubation or exacerbation of lung injury. As the debate between controlled invasive mechanical ventilation versus spontaneous breathing in ARDS continues, more research is warranted to identify subgroups of patients who may benefit from NIV, understand the effect of NIV interface on the physiology and outcomes of lung injury, and compare NIV to other respiratory support devices such as HFNC.
Airway Pressure Release Ventilation
Airway pressure release ventilation (APRV) was originally described over 30 years ago by Stock et al as a mode of ventilation that maintained an elevated pressure for most of the respiratory cycle (inverse I:E ratio) with periods of “release” to a lower CPAP to facilitate elimination of CO 2 . 101 The mode is purely time-cycled, shifting between high-pressure and low-pressure settings at set time intervals while allowing unrestricted breathing by the patient at any time during ventilation. There are four settings that set APRV apart from other modes; high pressure ( P high ) and the length of time P high is maintained ( T high ), low pressure ( P low ) and the length of time P low is maintained ( T low ). However, the literature contains major differences in how these settings are used and in the ventilation strategies used as comparators in trials. 102 Older studies of APRV titrated P low to prevent alveolar collapse, whereas a more modern approach adjusts T low based on expiratory flow to maintain auto-PEEP to prevent alveolar collapse. Additionally, there are minor differences between studies of similar methods that may be important, such as the P low settings used, or how much expiratory flow is limited with T low 103 ( Table 1 ).
Table 1. Differences between studies of APRV.
| Study | P low | T low | Primary outcome | Considerations |
|---|---|---|---|---|
| Putensen et al 104 | P – V | Full exhalation | Cardiorespiratory function; better for APRV | Control group paralyzed for 72 h then switched to APRV for the rest of the time on the ventilator |
| Varpula et al 106 | P – V | 1 s | VFD; no difference | Used high V T |
| Maxwell et al 107 | 0 | Exp flow 75–25% | VD; no difference | First study to target 6 mL/kg, but not exclusively ARDS patients |
| Zhou et al 108 | 5 cm H 2 O | Exp flow > 50% | VFD; more for APRV | Sedation protocol differences; no spontaneous mode used in control group; unsuccessful extubation rate not explained |
| Lalgudi Ganesan et al 110 | 0 | Exp flow 75% | VFD; no difference | Higher mortality for APRV |
Abbreviations: APRV, airway pressure release ventilation; P low , pressure low; P – V , pressure–volume curve; T low , time low; VD, ventilator days; VFD, ventilator-free days.
Setting P low
The traditional method of APRV was to set a P low level and allow exhalation to that level prior to returning to P high . 101 In older studies, P low was set according to the lower inflection point of the pressure–volume curve and control groups had PEEP set by the same method. 104 105 106 One of the most widely cited studies using this method was a crossover study of trauma patients by Putensen et al that randomly assigned 30 patients to receive APRV or pressure-controlled ventilation. They reported lower inotropic support requirements, fewer ventilator days, and a shorter length of ICU stay in patients that were initially managed with APRV. 104 However, the control group was paralyzed for the first 72 hours then switched to APRV; it is possible that the observed benefit of APRV was attributable to the protocol design rather than the mode per se. Subsequently, Varpula et al published the first RCT of APRV in ARDS patients using a T high of 4 seconds and a T low set to 1 second. 106 Similar to the Putensen et al, P low values during APRV and PEEP in the control group were set according to the lower inflection point of the pressure–volume curve. They originally planned to enroll 80 patients but stopped early for futility after an interim analysis of the first 58 patients. They found no significant difference in the primary outcome of ventilator-free days (13.4 vs. 12.2 with APRV and synchronized intermittent mandatory ventilation [SIMV], respectively). Of note, tidal volumes were high in both groups (between 8 and 10 mL/kg).
Limiting Expiratory Flow
In more recent years, studies of APRV have used a different approach where T low is set short enough to limit expiratory flow deceleration. With this method, auto-PEEP rather than P low is used to prevent alveolar collapse. This approach has now been used in three randomized trials (two adult and one pediatric study), with minor differences between them related to setting P low and the allowable limit of expiratory flow. In an RCT by Maxwell et al, APRV was compared with low V T ventilation (using SIMV) in 63 trauma patients. 107 They set P low to 0 cm H 2 O with T low set to terminate exhalation when the expiratory flow fell between 75 and 25% of peak expiratory flow. The outcomes were similar in both groups despite worse baseline physiological scores (APACHE II) in the APRV group. Sedation requirements were similar, and the duration of ventilation was not significantly different.
Recently Zhou et al conducted an RCT comparing APRV to conventional low tidal volume ventilation using the ARDSNet trial protocol in 138 patients meeting criteria for ARDS. 108 This was the first RCT comparing APRV to low V T specifically in ARDS. They set P low to 5 cm H 2 O and set T low to prevent expiratory flow from falling below 50% of the peak expiratory flow. They reported a significant improvement in the primary outcome of ventilator-free days using APRV compared with low V T ventilation (19 vs. 2; p < 0.0001). In contrast to Maxwell et al, they included spontaneous breathing trials in the protocols of both groups. However, the results may be confounded by several cointerventions: sedatives were significantly reduced in APRV patients by protocol design and spontaneous modes were not used in the control arm (patient–ventilator interaction was not assessed or considered). Furthermore, it was a single-center study limiting generalizability, baseline characteristics were not well balanced between groups (more patients with comorbidities were enrolled in the control arm), and there was an abnormally high rate of unsuccessful extubations and tracheostomies in the low V T group. 103 109 Shortly after the Zhou et al publication, an RCT of pediatric ARDS patients comparing APRV with low V T was stopped early after 50% enrollment ( n = 52) when an interim analysis demonstrated higher mortality in the APRV group. 110
APRV with Shorter P high
Another method to use the APRV mode is often referred to as biphasic positive airway pressure. This method uses P high and P low pressures comparable to conventional ventilation with T high and T low ratios similar to conventional pressure control (1:1 or greater), in contrast to the typical inverse ratio in most APRV studies. 102 The mode simply allows the patient to breathe freely without the need to be synchronous (ventilator breaths are delivered based solely on time and not patient effort). The primary goal of this approach is to limit transpulmonary pressure swings by inducing dyssynchrony (rather than trying to avoid dyssynchrony). 111 This method was recently applied in the largest study to date using the APRV mode, but the results have not been published at the time of this writing [NCT01862016]. Nonetheless, it will address a different question as it deals more with the question of synchrony rather than alveolar recruitment and an open lung approach.
The ability to generate higher mean airway pressure at lower peak airway pressures is the reason why APRV has been discussed in the context of managing ARDS, similar to the story of high-frequency oscillatory ventilation (HFOV). 112 However, in recent years the use of HFOV has fallen out of favor in the management of ARDS due to lack of effect and even potential harm. 113 114 Other “open lung” approaches using recruitment maneuvers and setting PEEP according to respiratory system compliance have also seen troubling results demonstrating potential for harm. 69 A major concern with widespread adoption of APRV is that it has not been studied nearly as well as these other approaches, which have all produced disappointing and concerning results in recent trials. Clinicians should be cautious in assuming that an open lung approach using APRV would yield different results. Currently the data are insufficient to recommend its use outside of a clinical trial.
High Frequency Oscillatory Ventilation
HFOV is a unique mode of mechanical ventilation that utilizes nonconventional gas exchange mechanisms to deliver ventilation at very low tidal volumes and high frequencies. The rationale and clinical evidence are briefly reviewed here; interested readers are guided to a recently published comprehensive review of this topic. 115
Rationale for Use in ARDS
As described earlier, VILI is thought to result from excess tidal volume and pressure applied to the lung and the recurrent recruitment and collapse of lung units (atelectrauma). 116 HFOV is theoretically ideal for avoiding VILI because it delivers small (sub-dead space) V T while preventing atelectasis with a consistently elevated mean airway pressure (m P aw ). 117
Working Principles and Physiology
The oscillator circuit is relatively simple, with heated and humidified bias flow gas traversing a rapidly oscillating membrane. The set oscillatory frequency typically ranges from 3 to 15 Hz. This rapid oscillatory motion generates V T lower than anatomic dead space, generally in the range of 1 to 3 mL/kg PBW. During HFOV, oxygenation and ventilation are independently controlled, with the former determined by the fraction of inspired oxygen and m P aw , while the latter is influenced by the frequency, amplitude of oscillations, and inspiratory time. 118
During HFOV, ventilation (CO 2 clearance) is achieved despite the delivery of V T below physiological dead space through several theorized mechanisms. 119 120 121 122 123 124 Convective bulk flow is a major mechanism of gas exchange. Typically, bulk flow is most pronounced in the proximal gas exchange units. 121 Here, convection is possible due to the asymmetric velocity profiles of inspired and expired gasses creating opposing convection currents—a phenomenon where gas exchange is even more pronounced at airway bifurcations. 125 Other mechanisms of gas exchange during HFOV include pendelluft 126 and cardiac oscillations. 127 The movement of gas between lung units with differing time constants for inflation and deflation (pendelluft) promotes gas exchange 128 and cardiac contractions cause a percussive movement of gas molecules allowing gas exchange to occur. 129
Current Evidence Base
Several RCTs have compared HFOV to CMV. 74 113 114 130 131 132 Early trials in ARDS patients were underpowered to detect clinically relevant differences in mortality and demonstrated nonsignificant effects in opposing directions. 74 130 131 When employed intermittently as a strategy to mimic a recruitment maneuver, HFOV was associated with significant improvements in oxygenation, lung compliance, and mortality (risk ratio [RR]: 0.59; 95% confidence interval [CI]: 0.41–0.85). 132
Meta-analysis of these early trials found that the risks of complications such as barotrauma and hemodynamic instability were not different between HFOV and CMV, and suggested that mortality was significantly lower with HFOV. 133 One must cautiously interpret these findings given that many of these trials were published before the wide adoption of plateau pressure and tidal-volume-limited CMV.
The large multicenter RCTs OSCAR 114 and OSCILLATE 113 were designed to definitively elucidate the role of HFOV in early ARDS. In the OSCILLATE trial, HFOV was applied using recruitment maneuvers and relatively high m P aw and titrated according to the severity of hypoxemia. The CMV arm employed a low V T and a high PEEP strategy. 67 OSCILLATE was stopped early after enrolling just under half of a planned 1,200 patients because mortality was significantly higher in the HFOV group compared with CMV (47 vs. 35%; RR: 1.33; 95% CI: 1.09–1.64). Vasopressor use and net fluid balance were higher in the HFOV arm, suggesting that HFOV may have significantly impaired hemodynamics, possibly contributing to the worsened outcome.
The OSCAR trial included almost 800 patients with moderate–severe ARDS, with HFOV titrated similarly to OSCILLATE. In contrast, however, m P aw was generally lower in OSCAR and employed a lower PEEP strategy in the CMV arm. Mortality was no different between the trial arms (41.7% in HFOV vs. 41.1% in CMV; RR: 1.02; 95% CI: 0.86–1.20) and no significant difference in vasopressor requirements. A detailed comparison of these two trials is depicted in Table 2 .
Table 2. Characteristics of the landmark clinical trials of HFOV in adult patients with ARDS.
| Study | Patients ( N ) | HFOV | Conventional mechanical ventilation | ||||
|---|---|---|---|---|---|---|---|
| Frequency titration strategy | m P aw titration strategy | ∆ P titration strategy | Mode | Tidal volume | PEEP titration strategy | ||
| Ferguson et al 113 | 548 | 3–12 Hz, maximal to keep pH > 7.25 | m P aw –FiO 2 table | 90 | PCV | 6 mL/kg PBW (6.1 mL/kg) |
LOVS PEEP–FiO 2 table |
| Young et al 114 | 795 | Initially 10 Hz, titrated to keep pH > 7.25, minimum 5 Hz | 5 cm H 2 O above CMV | Cycle volume titrated to keep pH > 7.25—some maximum for each frequency | PCV | 6–8 mL/kg PBW (8.3 mL/kg) |
ARDSNet lower PEEP–FiO 2 table |
Abbreviations: ARDS, acute respiratory distress syndrome; ARDSNet, ARDSnet RCT of lower tidal volume ventilation; CMV, conventional mechanical ventilation, FiO 2 , fraction of inspired oxygen; HFOV, high-frequency oscillatory ventilation; LOVS, Lung Open Ventilation Study; m P aw , mean airway pressure; PBW, predicted body weight; PCV, pressure controlled ventilation; PEEP, positive end-expiratory pressure;
An individual patient meta-analysis was then performed on 1,552 patients across four trials of HFOV versus CMV, 134 demonstrating that HFOV was associated with worse outcomes in less severe ARDS, while possibly exerting a mortality benefit in very severe hypoxemia (P/F ratio ≤ 65 mm Hg). These findings suggest HFOV could have a limited role in very severe ARDS, reserved as a rescue strategy as reflected in current guidelines for ARDS management. 135
Risks of HFOV
Despite low V T as delivered with HFOV, experimental studies suggest that high respiratory rates can cause cellular injury by influencing the elastic and frictional properties of pulmonary epithelium, leading to increased local stress, edema formation, and fracture of liquid bridges in airspaces. 136 137 138 The use of high m P aw (and therefore high PEEP) during HFOV is thought to prevent atelectasis; however, it is possible that such elevated pressures may necessarily result in volutrauma. 139 Finally, there is emerging evidence that HFOV can place the lung above its natural resonance frequency where ventilation heterogeneity can significantly increase, potentially worsening ventilation–perfusion mismatch, exacerbating hypoxemia 140 and amplifying (to injurious levels) delivered V T . 141
HFOV must be carefully applied to avoid hemodynamic impairment. Through elevated m P aw , HFOV can have a profound impact on the right ventricle (RV) by increasing afterload and reducing preload. 142 143 Direct measurement of intracardiac pressures in animal studies 144 and echocardiography studies in humans (demonstrating progressive RV dysfunction with increasing m P aw ) corroborate these findings. 143 RV dysfunction, suggested by the significant increase in vasopressor use and fluid balance with HFOV in the OSCILLATE trial, may explain the increased mortality rate with HFOV observed in that study. 113
Despite consistently improving oxygenation, HFOV is associated with worse outcomes in unselected ARDS patients and currently recommended as rescue therapy only. Cardiopulmonary effects likely limit the effectiveness of this technique.
Summary
This review suggests that much progress remains to be made in optimizing mechanical ventilation. The astute clinician will carefully consider the patient's clinical features, physiological status, and response to ventilatory support to determine how to optimally ventilate the patient. The overarching goals of optimal ventilator management are to provide appropriate gas exchange while aiming to minimize dynamic stress and strain on the injured lung. This can be accomplished by minimizing tidal volume to the extent clinically permitted, increasing PEEP if improved mechanics and gas exchange suggest benefit, and implementing evidence-based strategies including neuromuscular blockade (discussed in the article by Syed et al on pp. 101–113) and prone positioning (discussed in the article by Gattinoni et al on pp. 94–100). The judicious use of NIV in appropriately selected candidates with mild/moderate ARDS may also be appropriate. HFOV and APRV may be considered as options for rescue therapy in deteriorating patients, although extracorporeal therapies (discussed in the article by Fan et al on pp. 114–128) may take on more importance in this context.
Footnotes
Conflict of Interest Dr. Beitler reports grants from National Heart, Lung, and Blood Institute, during the conduct of the study. Dr. Piraino reports personal fees from Drager, Philips, and Fisher & Paykel, outside the submitted work.
References
- 1.Brower R G, Matthay M A, Morris A, Schoenfeld D, Thompson B T, Wheeler A; Acute Respiratory Distress Syndrome Network.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome N Engl J Med 2000342181301–1308. [DOI] [PubMed] [Google Scholar]
- 2.Amato M B, Barbas C S, Medeiros D M et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(06):347–354. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 3.Dreyfuss D, Soler P, Basset G, Saumon G. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis. 1988;137(05):1159–1164. doi: 10.1164/ajrccm/137.5.1159. [DOI] [PubMed] [Google Scholar]
- 4.Cressoni M, Cadringher P, Chiurazzi C et al. Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2014;189(02):149–158. doi: 10.1164/rccm.201308-1567OC. [DOI] [PubMed] [Google Scholar]
- 5.Cressoni M, Chiumello D, Chiurazzi C et al. Lung inhomogeneities, inflation and [18F]2-fluoro-2-deoxy-D-glucose uptake rate in acute respiratory distress syndrome. Eur Respir J. 2016;47(01):233–242. doi: 10.1183/13993003.00885-2015. [DOI] [PubMed] [Google Scholar]
- 6.Ghadiali S, Huang Y. Role of airway recruitment and derecruitment in lung injury. Crit Rev Biomed Eng. 2011;39(04):297–317. doi: 10.1615/critrevbiomedeng.v39.i4.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muscedere J G, Mullen J B, Gan K, Slutsky A S. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med. 1994;149(05):1327–1334. doi: 10.1164/ajrccm.149.5.8173774. [DOI] [PubMed] [Google Scholar]
- 8.Taskar V, John J, Evander E, Robertson B, Jonson B. Surfactant dysfunction makes lungs vulnerable to repetitive collapse and reexpansion. Am J Respir Crit Care Med. 1997;155(01):313–320. doi: 10.1164/ajrccm.155.1.9001330. [DOI] [PubMed] [Google Scholar]
- 9.Gajic O, Lee J, Doerr C H, Berrios J C, Myers J L, Hubmayr R D. Ventilator-induced cell wounding and repair in the intact lung. Am J Respir Crit Care Med. 2003;167(08):1057–1063. doi: 10.1164/rccm.200208-889OC. [DOI] [PubMed] [Google Scholar]
- 10.Matthay M A, Bhattacharya S, Gaver D et al. Ventilator-induced lung injury: in vivo and in vitro mechanisms. Am J Physiol Lung Cell Mol Physiol. 2002;283(04):L678–L682. doi: 10.1152/ajplung.00154.2002. [DOI] [PubMed] [Google Scholar]
- 11.Pelosi P, Rocco P R. Effects of mechanical ventilation on the extracellular matrix. Intensive Care Med. 2008;34(04):631–639. doi: 10.1007/s00134-007-0964-9. [DOI] [PubMed] [Google Scholar]
- 12.Ranieri V M, Giunta F, Suter P M, Slutsky A S. Mechanical ventilation as a mediator of multisystem organ failure in acute respiratory distress syndrome. JAMA. 2000;284(01):43–44. doi: 10.1001/jama.284.1.43. [DOI] [PubMed] [Google Scholar]
- 13.Ranieri V M, Suter P M, Tortorella C et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1999;282(01):54–61. doi: 10.1001/jama.282.1.54. [DOI] [PubMed] [Google Scholar]
- 14.Bein T, Weber-Carstens S, Goldmann A et al. Lower tidal volume strategy (≈3 ml/kg) combined with extracorporeal CO2 removal versus ‘conventional’ protective ventilation (6 ml/kg) in severe ARDS: the prospective randomized Xtravent-study. Intensive Care Med. 2013;39(05):847–856. doi: 10.1007/s00134-012-2787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Terragni P P, Del Sorbo L, Mascia L et al. Tidal volume lower than 6 ml/kg enhances lung protection: role of extracorporeal carbon dioxide removal. Anesthesiology. 2009;111(04):826–835. doi: 10.1097/ALN.0b013e3181b764d2. [DOI] [PubMed] [Google Scholar]
- 16.Combes A, Hajage D, Capellier G et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 17.Goligher E C, Tomlinson G, Hajage D et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc bayesian analysis of a randomized clinical trial. JAMA. 2018;320(21):2251–2259. doi: 10.1001/jama.2018.14276. [DOI] [PubMed] [Google Scholar]
- 18.Deans K J, Minneci P C, Cui X, Banks S M, Natanson C, Eichacker P Q. Mechanical ventilation in ARDS: one size does not fit all. Crit Care Med. 2005;33(05):1141–1143. doi: 10.1097/01.ccm.0000162384.71993.a3. [DOI] [PubMed] [Google Scholar]
- 19.Frank J A, Gutierrez J A, Jones K D, Allen L, Dobbs L, Matthay M A. Low tidal volume reduces epithelial and endothelial injury in acid-injured rat lungs. Am J Respir Crit Care Med. 2002;165(02):242–249. doi: 10.1164/ajrccm.165.2.2108087. [DOI] [PubMed] [Google Scholar]
- 20.MacIntyre N R. Lung protective ventilator strategies: beyond scaling tidal volumes to ideal lung size. Crit Care Med. 2016;44(01):244–245. doi: 10.1097/CCM.0000000000001454. [DOI] [PubMed] [Google Scholar]
- 21.Beitler J R, Goligher E C, Schmidt M et al. Personalized medicine for ARDS: the 2035 research agenda. Intensive Care Med. 2016;42(05):756–767. doi: 10.1007/s00134-016-4331-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amato M B, Meade M O, Slutsky A S et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(08):747–755. doi: 10.1056/NEJMsa1410639. [DOI] [PubMed] [Google Scholar]
- 23.Beitler J R, Majumdar R, Hubmayr R D et al. Volume delivered during recruitment maneuver predicts lung stress in acute respiratory distress syndrome. Crit Care Med. 2016;44(01):91–99. doi: 10.1097/CCM.0000000000001355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cherniack R M, Farhi L E, Armstrong B W, Proctor D F. A comparison of esophageal and intrapleural pressure in man. J Appl Physiol. 1955;8(02):203–211. doi: 10.1152/jappl.1955.8.2.203. [DOI] [PubMed] [Google Scholar]
- 25.Mead J, Gaensler E A. Esophageal and pleural pressures in man, upright and supine. J Appl Physiol. 1959;14(01):81–83. doi: 10.1152/jappl.1959.14.1.81. [DOI] [PubMed] [Google Scholar]
- 26.Chiumello D, Carlesso E, Cadringher P et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008;178(04):346–355. doi: 10.1164/rccm.200710-1589OC. [DOI] [PubMed] [Google Scholar]
- 27.Chiumello D, Cressoni M, Chierichetti M et al. Nitrogen washout/washin, helium dilution and computed tomography in the assessment of end expiratory lung volume. Crit Care. 2008;12(06):R150. doi: 10.1186/cc7139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mattingley J S, Holets S R, Oeckler R A, Stroetz R W, Buck C F, Hubmayr R D. Sizing the lung of mechanically ventilated patients. Crit Care. 2011;15(01):R60. doi: 10.1186/cc10034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beitler J R, Schoenfeld D A, Thompson B T. Preventing ARDS: progress, promise, and pitfalls. Chest. 2014;146(04):1102–1113. doi: 10.1378/chest.14-0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Litell J M, Gong M N, Talmor D, Gajic O. Acute lung injury: prevention may be the best medicine. Respir Care. 2011;56(10):1546–1554. doi: 10.4187/respcare.01361. [DOI] [PubMed] [Google Scholar]
- 31.Terragni P P, Rosboch G, Tealdi A et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;175(02):160–166. doi: 10.1164/rccm.200607-915OC. [DOI] [PubMed] [Google Scholar]
- 32.Gajic O, Dabbagh O, Park P K et al. Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2011;183(04):462–470. doi: 10.1164/rccm.201004-0549OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Levitt J E, Bedi H, Calfee C S, Gould M K, Matthay M A. Identification of early acute lung injury at initial evaluation in an acute care setting prior to the onset of respiratory failure. Chest. 2009;135(04):936–943. doi: 10.1378/chest.08-2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jabaudon M, Berthelin P, Pranal T et al. Receptor for advanced glycation end-products and ARDS prediction: a multicentre observational study. Sci Rep. 2018;8(01):2603. doi: 10.1038/s41598-018-20994-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jabaudon M, Blondonnet R, Pereira B et al. Plasma sRAGE is independently associated with increased mortality in ARDS: a meta-analysis of individual patient data. Intensive Care Med. 2018;44(09):1388–1399. doi: 10.1007/s00134-018-5327-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jabaudon M, Blondonnet R, Roszyk L et al. Soluble receptor for advanced glycation end-products predicts impaired alveolar fluid clearance in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2015;192(02):191–199. doi: 10.1164/rccm.201501-0020OC. [DOI] [PubMed] [Google Scholar]
- 37.Jabaudon M, Futier E, Roszyk L et al. Soluble form of the receptor for advanced glycation end products is a marker of acute lung injury but not of severe sepsis in critically ill patients. Crit Care Med. 2011;39(03):480–488. doi: 10.1097/CCM.0b013e318206b3ca. [DOI] [PubMed] [Google Scholar]
- 38.Uchida T, Shirasawa M, Ware L B et al. Receptor for advanced glycation end-products is a marker of type I cell injury in acute lung injury. Am J Respir Crit Care Med. 2006;173(09):1008–1015. doi: 10.1164/rccm.200509-1477OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agrawal A, Matthay M A, Kangelaris K N et al. Plasma angiopoietin-2 predicts the onset of acute lung injury in critically ill patients. Am J Respir Crit Care Med. 2013;187(07):736–742. doi: 10.1164/rccm.201208-1460OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Calfee C S, Gallagher D, Abbott J, Thompson B T, Matthay M A; NHLBI ARDS Network.Plasma angiopoietin-2 in clinical acute lung injury: prognostic and pathogenetic significance Crit Care Med 201240061731–1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van der Heijden M, Pickkers P, van Nieuw Amerongen G P et al. Circulating angiopoietin-2 levels in the course of septic shock: relation with fluid balance, pulmonary dysfunction and mortality. Intensive Care Med. 2009;35(09):1567–1574. doi: 10.1007/s00134-009-1560-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ely E W, Shintani A, Truman B et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 43.Girard T D, Jackson J C, Pandharipande P P et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38(07):1513–1520. doi: 10.1097/CCM.0b013e3181e47be1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goligher E C, Fan E, Herridge M S et al. Evolution of diaphragm thickness during mechanical ventilation: impact of inspiratory effort. Am J Respir Crit Care Med. 2015;192(09):1080–1088. doi: 10.1164/rccm.201503-0620OC. [DOI] [PubMed] [Google Scholar]
- 45.Schweickert W D, Pohlman M C, Pohlman A Set al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial Lancet 2009373(9678):1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brodie D, Bacchetta M. Extracorporeal membrane oxygenation for ARDS in adults. N Engl J Med. 2011;365(20):1905–1914. doi: 10.1056/NEJMct1103720. [DOI] [PubMed] [Google Scholar]
- 47.Ashbaugh D G, Bigelow D B, Petty T L, Levine B E.Acute respiratory distress in adults Lancet 19672(7511):319–323. [DOI] [PubMed] [Google Scholar]
- 48.Sahetya S K, Goligher E C, Brower R G. Fifty years of research in ARDS. Setting positive end-expiratory pressure in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(11):1429–1438. doi: 10.1164/rccm.201610-2035CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Caironi P, Cressoni M, Chiumello D et al. Lung opening and closing during ventilation of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2010;181(06):578–586. doi: 10.1164/rccm.200905-0787OC. [DOI] [PubMed] [Google Scholar]
- 50.Ghadiali S N, Gaver D P.Biomechanics of liquid-epithelium interactions in pulmonary airways Respir Physiol Neurobiol 2008163(1–3):232–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mélot C. Contribution of multiple inert gas elimination technique to pulmonary medicine. 5. Ventilation-perfusion relationships in acute respiratory failure. Thorax. 1994;49(12):1251–1258. doi: 10.1136/thx.49.12.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Di Marco F, Devaquet J, Lyazidi A et al. Positive end-expiratory pressure-induced functional recruitment in patients with acute respiratory distress syndrome. Crit Care Med. 2010;38(01):127–132. doi: 10.1097/CCM.0b013e3181b4a7e7. [DOI] [PubMed] [Google Scholar]
- 53.Protti A, Andreis D T, Monti M et al. Lung stress and strain during mechanical ventilation: any difference between statics and dynamics? Crit Care Med. 2013;41(04):1046–1055. doi: 10.1097/CCM.0b013e31827417a6. [DOI] [PubMed] [Google Scholar]
- 54.Suter P M, Fairley B, Isenberg M D. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975;292(06):284–289. doi: 10.1056/NEJM197502062920604. [DOI] [PubMed] [Google Scholar]
- 55.Dhainaut J F, Devaux J Y, Monsallier J F, Brunet F, Villemant D, Huyghebaert M F. Mechanisms of decreased left ventricular preload during continuous positive pressure ventilation in ARDS. Chest. 1986;90(01):74–80. doi: 10.1378/chest.90.1.74. [DOI] [PubMed] [Google Scholar]
- 56.Cournand A, Motley H L, Werko L, Richards D W., Jr Physiological studies of the effects of intermittent positive pressure breathing on cardiac output in man. Am J Physiol. 1948;152(01):162–174. doi: 10.1152/ajplegacy.1947.152.1.162. [DOI] [PubMed] [Google Scholar]
- 57.Barach A L, Eckman M, Ginsburg E et al. Studies on positive pressure respiration; general aspects and types of pressure breathing; effects on respiration and circulation at sea level. J Aviat Med. 1946;17:290–32. [PubMed] [Google Scholar]
- 58.Mekontso Dessap A, Boissier F, Charron C et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med. 2016;42(05):862–870. doi: 10.1007/s00134-015-4141-2. [DOI] [PubMed] [Google Scholar]
- 59.Jardin F, Delorme G, Hardy A, Auvert B, Beauchet A, Bourdarias J P. Reevaluation of hemodynamic consequences of positive pressure ventilation: emphasis on cyclic right ventricular afterloading by mechanical lung inflation. Anesthesiology. 1990;72(06):966–970. doi: 10.1097/00000542-199006000-00003. [DOI] [PubMed] [Google Scholar]
- 60.Gattinoni L, Pesenti A. The concept of “baby lung”. Intensive Care Med. 2005;31(06):776–784. doi: 10.1007/s00134-005-2627-z. [DOI] [PubMed] [Google Scholar]
- 61.Lachmann B. Open up the lung and keep the lung open. Intensive Care Med. 1992;18(06):319–321. doi: 10.1007/BF01694358. [DOI] [PubMed] [Google Scholar]
- 62.Borges J B, Okamoto V N, Matos G F et al. Reversibility of lung collapse and hypoxemia in early acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;174(03):268–278. doi: 10.1164/rccm.200506-976OC. [DOI] [PubMed] [Google Scholar]
- 63.Hess D R, Bigatello L M.Lung recruitment: the role of recruitment maneuvers Respir Care 20024703308–317., discussion 317–318 [PubMed] [Google Scholar]
- 64.Lim S C, Adams A B, Simonson D A et al. Intercomparison of recruitment maneuver efficacy in three models of acute lung injury. Crit Care Med. 2004;32(12):2371–2377. doi: 10.1097/01.ccm.0000147445.73344.3a. [DOI] [PubMed] [Google Scholar]
- 65.Gattinoni L, Caironi P, Cressoni M et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354(17):1775–1786. doi: 10.1056/NEJMoa052052. [DOI] [PubMed] [Google Scholar]
- 66.Brower R G, Lanken P N, MacIntyre N et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(04):327–336. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 67.Meade M O, Cook D J, Guyatt G H et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(06):637–645. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 68.Mercat A, Richard J-CM, Vielle B et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(06):646–655. doi: 10.1001/jama.299.6.646. [DOI] [PubMed] [Google Scholar]
- 69.Cavalcanti A B, Suzumura E A, Laranjeira L N et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318(14):1335–1345. doi: 10.1001/jama.2017.14171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Villar J, Suárez-Sipmann F, Kacmarek R M. Should the ART trial change our practice? J Thorac Dis. 2017;9(12):4871–4877. doi: 10.21037/jtd.2017.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yoshida T, Nakahashi S, Nakamura M AM et al. Volume-controlled ventilation does not prevent injurious inflation during spontaneous effort. Am J Respir Crit Care Med. 2017;196(05):590–601. doi: 10.1164/rccm.201610-1972OC. [DOI] [PubMed] [Google Scholar]
- 72.Kacmarek R M, Villar J, Sulemanji D et al. Open lung approach for the acute respiratory distress syndrome: a pilot, randomized controlled trial. Crit Care Med. 2016;44(01):32–42. doi: 10.1097/CCM.0000000000001383. [DOI] [PubMed] [Google Scholar]
- 73.Goligher E C, Kavanagh B P, Rubenfeld G D, Ferguson N D. Physiologic responsiveness should guide entry into randomized controlled trials. Am J Respir Crit Care Med. 2015;192(12):1416–1419. doi: 10.1164/rccm.201410-1832CP. [DOI] [PubMed] [Google Scholar]
- 74.Goligher E C, Kavanagh B P, Rubenfeld G D et al. Oxygenation response to positive end-expiratory pressure predicts mortality in acute respiratory distress syndrome. A secondary analysis of the LOVS and ExPress trials. Am J Respir Crit Care Med. 2014;190(01):70–76. doi: 10.1164/rccm.201404-0688OC. [DOI] [PubMed] [Google Scholar]
- 75.Calfee C S, Delucchi K L, Sinha P et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med. 2018;6(09):691–698. doi: 10.1016/S2213-2600(18)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chiumello D, Marino A, Brioni M et al. Lung recruitment assessed by respiratory mechanics and computed tomography in patients with acute respiratory distress syndrome. What is the relationship? Am J Respir Crit Care Med. 2016;193(11):1254–1263. doi: 10.1164/rccm.201507-1413OC. [DOI] [PubMed] [Google Scholar]
- 77.Decailliot F, Demoule A, Maggiore S M, Jonson B, Duvaldestin P, Brochard L. Pressure-volume curves with and without muscle paralysis in acute respiratory distress syndrome. Intensive Care Med. 2006;32(09):1322–1328. doi: 10.1007/s00134-006-0265-8. [DOI] [PubMed] [Google Scholar]
- 78.Grasso S, Terragni P, Mascia L et al. Airway pressure-time curve profile (stress index) detects tidal recruitment/hyperinflation in experimental acute lung injury. Crit Care Med. 2004;32(04):1018–1027. doi: 10.1097/01.ccm.0000120059.94009.ad. [DOI] [PubMed] [Google Scholar]
- 79.Talmor D, Sarge T, Malhotra A et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med. 2008;359(20):2095–2104. doi: 10.1056/NEJMoa0708638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Costa E L, Borges J B, Melo A et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35(06):1132–1137. doi: 10.1007/s00134-009-1447-y. [DOI] [PubMed] [Google Scholar]
- 81.Brochard L, Mancebo J, Wysocki M et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1995;333(13):817–822. doi: 10.1056/NEJM199509283331301. [DOI] [PubMed] [Google Scholar]
- 82.Masip J, Roque M, Sánchez B, Fernández R, Subirana M, Expósito J A. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA. 2005;294(24):3124–3130. doi: 10.1001/jama.294.24.3124. [DOI] [PubMed] [Google Scholar]
- 83.Herridge M S, Tansey C M, Matté A et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 84.Antonelli M, Conti G, Esquinas A et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med. 2007;35(01):18–25. doi: 10.1097/01.CCM.0000251821.44259.F3. [DOI] [PubMed] [Google Scholar]
- 85.Walkey A J, Wiener R S. Use of noninvasive ventilation in patients with acute respiratory failure, 2000–2009: a population-based study. Ann Am Thorac Soc. 2013;10(01):10–17. doi: 10.1513/AnnalsATS.201206-034OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ranieri V M, Rubenfeld G D, Thompson B T et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 87.L'Her E, Deye N, Lellouche F et al. Physiologic effects of noninvasive ventilation during acute lung injury. Am J Respir Crit Care Med. 2005;172(09):1112–1118. doi: 10.1164/rccm.200402-226OC. [DOI] [PubMed] [Google Scholar]
- 88.Kallet R H, Hemphill J C, III, Dicker R A et al. The spontaneous breathing pattern and work of breathing of patients with acute respiratory distress syndrome and acute lung injury. Respir Care. 2007;52(08):989–995. [PubMed] [Google Scholar]
- 89.Carteaux G, Millán-Guilarte T, De Prost N et al. Failure of noninvasive ventilation for de novo acute hypoxemic respiratory failure: role of tidal volume. Crit Care Med. 2016;44(02):282–290. doi: 10.1097/CCM.0000000000001379. [DOI] [PubMed] [Google Scholar]
- 90.Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195(04):438–442. doi: 10.1164/rccm.201605-1081CP. [DOI] [PubMed] [Google Scholar]
- 91.Bellani G, Laffey J G, Pham T et al. Noninvasive ventilation of patients with acute respiratory distress syndrome. Insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195(01):67–77. doi: 10.1164/rccm.201606-1306OC. [DOI] [PubMed] [Google Scholar]
- 92.Agarwal R, Aggarwal A N, Gupta D. Role of noninvasive ventilation in acute lung injury/acute respiratory distress syndrome: a proportion meta-analysis. Respir Care. 2010;55(12):1653–1660. [PubMed] [Google Scholar]
- 93.Thille A W, Contou D, Fragnoli C, Córdoba-Izquierdo A, Boissier F, Brun-Buisson C. Non-invasive ventilation for acute hypoxemic respiratory failure: intubation rate and risk factors. Crit Care. 2013;17(06):R269. doi: 10.1186/cc13103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rana S, Jenad H, Gay P C, Buck C F, Hubmayr R D, Gajic O. Failure of non-invasive ventilation in patients with acute lung injury: observational cohort study. Crit Care. 2006;10(03):R79. doi: 10.1186/cc4923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Antonelli M, Conti G, Moro M L et al. Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study. Intensive Care Med. 2001;27(11):1718–1728. doi: 10.1007/s00134-001-1114-4. [DOI] [PubMed] [Google Scholar]
- 96.Duan J, Han X, Bai L, Zhou L, Huang S. Assessment of heart rate, acidosis, consciousness, oxygenation, and respiratory rate to predict noninvasive ventilation failure in hypoxemic patients. Intensive Care Med. 2017;43(02):192–199. doi: 10.1007/s00134-016-4601-3. [DOI] [PubMed] [Google Scholar]
- 97.Frat J P, Thille A W, Mercat A et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 98.Patel B K, Wolfe K S, Pohlman A S, Hall J B, Kress J P. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2016;315(22):2435–2441. doi: 10.1001/jama.2016.6338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Patel B K, Wolfe K S, MacKenzie E L et al. One-year outcomes in patients with acute respiratory distress syndrome enrolled in a randomized clinical trial of helmet versus facemask noninvasive ventilation. Crit Care Med. 2018;46(07):1078–1084. doi: 10.1097/CCM.0000000000003124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rochwerg B, Brochard L, Elliott M W et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(02):50. doi: 10.1183/13993003.02426-2016. [DOI] [PubMed] [Google Scholar]
- 101.Stock M C, Downs J B, Frolicher D A. Airway pressure release ventilation. Crit Care Med. 1987;15(05):462–466. doi: 10.1097/00003246-198705000-00002. [DOI] [PubMed] [Google Scholar]
- 102.Rose L, Hawkins M. Airway pressure release ventilation and biphasic positive airway pressure: a systematic review of definitional criteria. Intensive Care Med. 2008;34(10):1766–1773. doi: 10.1007/s00134-008-1216-3. [DOI] [PubMed] [Google Scholar]
- 103.Piraino T, Fan E. Airway pressure release ventilation in patients with acute respiratory distress syndrome: not yet, we still need more data! J Thorac Dis. 2018;10(02):670–673. doi: 10.21037/jtd.2017.11.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Putensen C, Zech S, Wrigge H et al. Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med. 2001;164(01):43–49. doi: 10.1164/ajrccm.164.1.2001078. [DOI] [PubMed] [Google Scholar]
- 105.Varpula T, Jousela I, Niemi R, Takkunen O, Pettilä V. Combined effects of prone positioning and airway pressure release ventilation on gas exchange in patients with acute lung injury. Acta Anaesthesiol Scand. 2003;47(05):516–524. doi: 10.1034/j.1399-6576.2003.00109.x. [DOI] [PubMed] [Google Scholar]
- 106.Varpula T, Valta P, Niemi R, Takkunen O, Hynynen M, Pettilä V V. Airway pressure release ventilation as a primary ventilatory mode in acute respiratory distress syndrome. Acta Anaesthesiol Scand. 2004;48(06):722–731. doi: 10.1111/j.0001-5172.2004.00411.x. [DOI] [PubMed] [Google Scholar]
- 107.Maxwell R A, Green J M, Waldrop Jet al. A randomized prospective trial of airway pressure release ventilation and low tidal volume ventilation in adult trauma patients with acute respiratory failure J Trauma 20106903501–510., discussion 511 [DOI] [PubMed] [Google Scholar]
- 108.Zhou Y, Jin X, Lv Y et al. Early application of airway pressure release ventilation may reduce the duration of mechanical ventilation in acute respiratory distress syndrome. Intensive Care Med. 2017;43(11):1648–1659. doi: 10.1007/s00134-017-4912-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mireles-Cabodevila E, Dugar S, Chatburn R L. APRV for ARDS: the complexities of a mode and how it affects even the best trials. J Thorac Dis. 2018;10 09:S1058–S1063. doi: 10.21037/jtd.2018.03.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lalgudi Ganesan S, Jayashree M, Chandra Singhi S, Bansal A. Airway pressure release ventilation in pediatric acute respiratory distress syndrome. A randomized controlled trial. Am J Respir Crit Care Med. 2018;198(09):1199–1207. doi: 10.1164/rccm.201705-0989OC. [DOI] [PubMed] [Google Scholar]
- 111.Rittayamai N, Beloncle F, Goligher E C et al. Effect of inspiratory synchronization during pressure-controlled ventilation on lung distension and inspiratory effort. Ann Intensive Care. 2017;7(01):100. doi: 10.1186/s13613-017-0324-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Stawicki S P, Goyal M, Sarani B. High-frequency oscillatory ventilation (HFOV) and airway pressure release ventilation (APRV): a practical guide. J Intensive Care Med. 2009;24(04):215–229. doi: 10.1177/0885066609335728. [DOI] [PubMed] [Google Scholar]
- 113.Ferguson N D, Cook D J, Guyatt G H et al. High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med. 2013;368(09):795–805. doi: 10.1056/NEJMoa1215554. [DOI] [PubMed] [Google Scholar]
- 114.Young D, Lamb S E, Shah S et al. High-frequency oscillation for acute respiratory distress syndrome. N Engl J Med. 2013;368(09):806–813. doi: 10.1056/NEJMoa1215716. [DOI] [PubMed] [Google Scholar]
- 115.Sklar M C, Fan E, Goligher E C. High-frequency oscillatory ventilation in adults with ARDS: past, present, and future. Chest. 2017;152(06):1306–1317. doi: 10.1016/j.chest.2017.06.025. [DOI] [PubMed] [Google Scholar]
- 116.Slutsky A S, Ranieri V M. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–2136. doi: 10.1056/NEJMra1208707. [DOI] [PubMed] [Google Scholar]
- 117.Ferguson N, Slutsky A. Last word on point:counterpoint: high-frequency ventilation is/is not the optimal physiological approach to ventilate ARDS patients. J Appl Physiol (1985) 2008;104(04):1240. doi: 10.1152/japplphysiol.00199.2008. [DOI] [PubMed] [Google Scholar]
- 118.Slutsky A S, Kamm R D, Rossing T H et al. Effects of frequency, tidal volume, and lung volume on CO2 elimination in dogs by high frequency (2-30 Hz), low tidal volume ventilation. J Clin Invest. 1981;68(06):1475–1484. doi: 10.1172/JCI110400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Drazen J M, Kamm R D, Slutsky A S. High-frequency ventilation. Physiol Rev. 1984;64(02):505–543. doi: 10.1152/physrev.1984.64.2.505. [DOI] [PubMed] [Google Scholar]
- 120.Khoo M C, Slutsky A S, Drazen J M, Solway J, Gavriely N, Kamm R D. Gas mixing during high-frequency ventilation: an improved model. J Appl Physiol. 1984;57(02):493–506. doi: 10.1152/jappl.1984.57.2.493. [DOI] [PubMed] [Google Scholar]
- 121.Pillow J J.High-frequency oscillatory ventilation: mechanisms of gas exchange and lung mechanics Crit Care Med 200533(3, Suppl):S135–S141. [DOI] [PubMed] [Google Scholar]
- 122.Rossing T H, Slutsky A S, Lehr J L, Drinker P A, Kamm R, Drazen J M. Tidal volume and frequency dependence of carbon dioxide elimination by high-frequency ventilation. N Engl J Med. 1981;305(23):1375–1379. doi: 10.1056/NEJM198112033052303. [DOI] [PubMed] [Google Scholar]
- 123.Slutsky A S, Drazen F M, Ingram R H, Jret al. Effective pulmonary ventilation with small-volume oscillations at high frequency Science 1980209(4456):609–671. [DOI] [PubMed] [Google Scholar]
- 124.Slutsky A S, Drazen J M. Ventilation with small tidal volumes. N Engl J Med. 2002;347(09):630–631. doi: 10.1056/NEJMp020082. [DOI] [PubMed] [Google Scholar]
- 125.Scherer P W, Haselton F R. Convective exchange in oscillatory flow through bronchial-tree models. J Appl Physiol. 1982;53(04):1023–1033. doi: 10.1152/jappl.1982.53.4.1023. [DOI] [PubMed] [Google Scholar]
- 126.Greenblatt E E, Butler J P, Venegas J G, Winkler T. Pendelluft in the bronchial tree. J Appl Physiol (1985) 2014;117(09):979–988. doi: 10.1152/japplphysiol.00466.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Slutsky A S. Gas mixing by cardiogenic oscillations: a theoretical quantitative analysis. J Appl Physiol. 1981;51(05):1287–1293. doi: 10.1152/jappl.1981.51.5.1287. [DOI] [PubMed] [Google Scholar]
- 128.Ultman J S, Shaw R G, Fabiano D C, Cooke K A. Pendelluft and mixing in a single bifurcation lung model during high-frequency oscillation. J Appl Physiol (1985) 1988;65(01):146–155. doi: 10.1152/jappl.1988.65.1.146. [DOI] [PubMed] [Google Scholar]
- 129.Cybulsky I J, Abel J G, Menon A S, Salerno T A, Lichtenstein S V, Slutsky A S. Contribution of cardiogenic oscillations to gas exchange in constant-flow ventilation. J Appl Physiol (1985) 1987;63(02):564–570. doi: 10.1152/jappl.1987.63.2.564. [DOI] [PubMed] [Google Scholar]
- 130.Bollen C W, van Well G TJ, Sherry T et al. High frequency oscillatory ventilation compared with conventional mechanical ventilation in adult respiratory distress syndrome: a randomized controlled trial [ISRCTN24242669] Crit Care. 2005;9(04):R430–R439. doi: 10.1186/cc3737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Derdak S, Mehta S, Stewart T E et al. High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. Am J Respir Crit Care Med. 2002;166(06):801–808. doi: 10.1164/rccm.2108052. [DOI] [PubMed] [Google Scholar]
- 132.Mentzelopoulos S D, Malachias S, Zintzaras E et al. Intermittent recruitment with high-frequency oscillation/tracheal gas insufflation in acute respiratory distress syndrome. Eur Respir J. 2012;39(03):635–647. doi: 10.1183/09031936.00158810. [DOI] [PubMed] [Google Scholar]
- 133.Sud S, Sud M, Friedrich J O et al. High frequency oscillation in patients with acute lung injury and acute respiratory distress syndrome (ARDS): systematic review and meta-analysis. BMJ. 2010;340:c2327. doi: 10.1136/bmj.c2327. [DOI] [PubMed] [Google Scholar]
- 134.Meade M O, Young D, Hanna S et al. Severity of hypoxemia and effect of high-frequency oscillatory ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;196(06):727–733. doi: 10.1164/rccm.201609-1938OC. [DOI] [PubMed] [Google Scholar]
- 135.Fan E, Del Sorbo L, Goligher E C et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(09):1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 136.Fabry B, Maksym G N, Butler J P, Glogauer M, Navajas D, Fredberg J J. Scaling the microrheology of living cells. Phys Rev Lett. 2001;87(14):148102. doi: 10.1103/PhysRevLett.87.148102. [DOI] [PubMed] [Google Scholar]
- 137.Huh D, Fujioka H, Tung Y-C et al. Acoustically detectable cellular-level lung injury induced by fluid mechanical stresses in microfluidic airway systems. Proc Natl Acad Sci U S A. 2007;104(48):18886–18891. doi: 10.1073/pnas.0610868104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hussein O, Walters B, Stroetz R, Valencia P, McCall D, Hubmayr R D. Biophysical determinants of alveolar epithelial plasma membrane wounding associated with mechanical ventilation. Am J Physiol Lung Cell Mol Physiol. 2013;305(07):L478–L484. doi: 10.1152/ajplung.00437.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Cressoni M, Chiumello D, Algieri I et al. Opening pressures and atelectrauma in acute respiratory distress syndrome. Intensive Care Med. 2017;43(05):603–611. doi: 10.1007/s00134-017-4754-8. [DOI] [PubMed] [Google Scholar]
- 140.Tabuchi A, Nickles H T, Kim M et al. Acute lung injury causes asynchronous alveolar ventilation that can be corrected by individual sighs. Am J Respir Crit Care Med. 2016;193(04):396–406. doi: 10.1164/rccm.201505-0901OC. [DOI] [PubMed] [Google Scholar]
- 141.Brusasco V, Beck K C, Crawford M, Rehder K. Resonant amplification of delivered volume during high-frequency ventilation. J Appl Physiol (1985) 1986;60(03):885–892. doi: 10.1152/jappl.1986.60.3.885. [DOI] [PubMed] [Google Scholar]
- 142.David M, von Bardeleben R S, Weiler N et al. Cardiac function and haemodynamics during transition to high-frequency oscillatory ventilation. Eur J Anaesthesiol. 2004;21(12):944–952. doi: 10.1017/s0265021504000328. [DOI] [PubMed] [Google Scholar]
- 143.Guervilly C, Forel J-M, Hraiech S et al. Right ventricular function during high-frequency oscillatory ventilation in adults with acute respiratory distress syndrome. Crit Care Med. 2012;40(05):1539–1545. doi: 10.1097/CCM.0b013e3182451b4a. [DOI] [PubMed] [Google Scholar]
- 144.Smailys A, Mitchell J R, Doig C J, Tyberg J V, Belenkie I. High-frequency oscillatory ventilation versus conventional ventilation: hemodynamic effects on lung and heart. Physiol Rep. 2014;2(03):e00259. doi: 10.1002/phy2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]


