The population of cancer survivors in the United States reached 15.5 million in 2016, and is projected to total over 20 million by 2026 (Miller et al. 2016). As survival rates continue to increase and the number of cancer survivors grows (National Cancer Institute 2018), their long-term health-related quality of life (QOL), defined as perceived mental and physical health (Centers for Disease Control and Prevention 2018), is an increasing public health priority (De Moor et al. 2013). We especially need to study and address the needs of survivors who face health disparities, including rural cancer survivors (Andrykowski et al. 2014; Burris and Andrykowski 2010; Butow et al. 2012; Reid-Arndt and Cox 2010; Weaver et al. 2013a; Weaver et al. 2013b). Unfortunately, although more than 20% of cancer survivors reside in rural areas, less than 5% of cancer survivorship research focuses on this population (Harrop, Dean, and Paskett 2011; Weaver et al. 2013b). Limited but growing research indicates that rural cancer survivors experience a number of health disparities compared with their urban counterparts, including worse self-reported health (Weaver et al. 2013a; Weaver et al. 2013b), higher rates of health-related unemployment (Weaver et al. 2013a; Weaver et al. 2013b), higher risk of psychological distress (Weaver et al. 2013b), poorer mental health (Andrykowski et al. 2014; Burris and Andrykowski 2010), and poorer QOL (Reid-Arndt and Cox 2010).
Although multiple types of determinants of QOL exist (Klijs et al. 2017; Michael et al. 2002; Sapp et al. 2003; Schafer and Koltai 2015), extant literature on rural cancer survivors has largely focused on behavioral (e.g., smoking, physical inactivity) and social factors (e.g., hesitation in seeking social support) (Andrykowski et al. 2014; Weaver et al. 2013b). Much remains unknown about cancer-related stressors, including cancer-related debt, on rural survivors’ QOL. In the current study, cancer-related debt is defined here as debt, borrowed money, or bankruptcy due to cancer, its treatment, or the lasting effects of that treatment (Yabroff et al. 2012). Although a relationship between cancer-related debt and QOL has been established among cancer survivors overall (Hastert et al. 2019; Kale and Carroll 2016; Meneses et al. 2012), to our knowledge, no research has examined the role of cancer-related debt on QOL specifically among rural cancer survivors. There is also insufficient knowledge regarding the interactive effects between cancer-related debt and social determinants of QOL, including family/friend informal caregiver networks. Here, we define informal caregivers as individuals “who provide care that is typically uncompensated and usually at home, involves significant amounts of time and energy for months or years, and requires the performance of tasks that may be physically, emotionally, socially, or financially demanding” (Kent et al. 2016: 1987). Specifically, we focus on relatively intimate family/friend relationships that provide unpaid care during illness. The current study addresses these gaps in the literature by examining the moderating role of cancer survivors’ family/friend informal caregiver networks on the relationship between cancer-related debt and mental health-related quality of life (MHQOL) among rural cancer survivors.
BACKGROUND
Our first contribution to the literature is to examine the association between cancer-related debt and QOL among rural cancer survivors. Cancer-related financial hardship, including cancer-related debt, represents a major, modifiable, and increasingly studied stressor that negatively affects the QOL of cancer survivors (Ell et al. 2008; Fenn et al. 2014; Hastert et al. 2019; Kale and Carroll 2016; Meneses et al. 2012). Despite the growing body of work demonstrating a relationship between cancer-related financial hardship and cancer survivors’ QOL, relatively little work has assessed the extent or impact of this stressor for rural cancer survivors (McDougall et al. 2018; Palmer et al. 2013; Pisu et al. 2017; Zahnd et al. 2019). This is surprising, given rural populations often are more socioeconomically disadvantaged relative to urban populations in terms of individual and contextual factors, including individual and household income, job and wage growth, and, for some regions, poverty rate (Bishaw and Posey 2016; Cromartie 2017). Moreover, rural patients often face costly barriers to accessing healthcare, such as long travel distances for treatment (Charlton et al. 2015; Onega et al. 2008; Syed, Gerber, and Sharp 2013; Wishner and Solleveld 2016). The limited existing research suggests that rural survivors face greater cancer-related financial hardship and are more likely to forego medical and dental care due to cost, compared to their urban counterparts (McDougall et al. 2018; Palmer et al. 2013). Among rural breast cancer survivors, specifically, younger and lower-income survivors had greater out-of-pocket cost burden (Pisu et al. 2017). However, to date, there is limited evidence describing how cancer-related financial hardship among rural cancer survivors influences their current QOL. Our study advances this literature by examining how cancer-related debt, specifically, is associated with MHQOL among rural cancer survivors.
Our second contribution to the literature is to examine how rural cancer survivors’ family/friend informal caregiver networks may moderate the association between cancer-related debt and MHQOL. At large, social connectedness (e.g., social support, social networks, social capital) is considered protective for health (Callaghan and Morrissey 1993; Cornwell and Laumann 2015; Haines, Beggs, and Hurlbert 2011; Haynie et al. 2018; Kawachi, Subramanian, and Kim 2008; Rocco and Suhrcke 2012; Smith and Christakis 2008; Uchino 2006) and cancer survivorship (Kroenke et al. 2013; Lim and Zebrack 2006; Michael et al. 2002; Sapp et al. 2003). Specifically, social connectedness theoretically buffers the impact of various stressors and stress processes, including debt, on health (Cohen and Hoberman 1983; Cohen and McKay 1984; Cohen and Wills 1985).
Yet, how social connectedness mitigates or exacerbates the effects of cancer-related stressors may differ, depending on the type of support provided, relationship context, and interpersonal dynamics. We consider these factors in terms of family/friend informal caregivers. First, family/friend informal caregivers offer less specialized support focused on cancer than healthcare providers and more peripheral network members (e.g., new peer survivor acquaintances) (Arora et al. 2007; Kroenke 2018; Molina 2018; Molina et al. 2016). Thus, they may not necessarily provide the cancer-specific support necessary to buffer cancer-related debt and other stressors (e.g., knowledge of financial assistance programs). Second, family and friends provide cancer-related caregiving in the context of affectively close relationships, long-term relationships, and normative expectations of family responsibility for care (Jacobs et al. 2016; Keating et al. 2003; Litwin and Auslander 1990). The impact of cancer-related caregiving thus results from established long-term, central relationships (e.g., motive to give care), but also has implications for the future of those relationships (e.g., dissolution of friendship due to caregiver burden). Indeed, caregiver burden often puts strain on strong, established relationships (Adelman et al. 2014; Gaugler et al. 2005; Rha et al. 2015; Wagner et al. 2011), potentially exacerbating cancer-related stressors, like cancer-related debt, and resulting in long-term negative consequences on relationships. Third, while strong relationships between patient and family/friend caregivers theoretically offer the greatest support, they are also ripe for negative interpersonal dynamics that can affect patient health (Douglass 1997; Kiecolt-Glaser and Newton 2001), including conflict, mutual distress, communication issues, criticism, overprotective behaviors, and caregiver’s reluctance to care (Burridge, Winch, and Clavarino 2007; Martire et al. 2004). These factors are linked to the health of both patients and caregivers (Cooley and Moriarty 1997; Fletcher et al. 2012; Goldzweig et al. 2013; Kim et al. 2008, 2015; Li and Loke 2013; Litzelman and Yabroff 2015; Martire et al. 2004; Mehnert et al. 2018; Northouse et al. 2012; Sklenarova et al. 2015; Vellone et al. 2014).
How family/friend informal caregiver networks impact relationships between cancer-related debt and MHQOL may also be unique within rural communities. Rural norms of resiliency and autonomy may lead to greater preference for no or relatively few caregivers (e.g., to exercise self-reliance or avoid stigma) (Amato and Zuo 1992; Kirby et al. 2016; Myers and Gill 2004; Weaver, Roberto, and Blieszner 2017). Preferences may not be actualized however, due to spontaneous and chronic cancer survivorship needs (Cheng et al. 2014; Leach et al. 2017; Sterba et al. 2017). However, larger caregiver networks may not represent more quality care for rural survivors; instead, they may reflect more widely dispersed, inconsistent caregiving (Keating et al. 2003) and less intensive provision of care (Kayser, Watson, and Andrade 2007; Li, Mak, and Loke 2013; Maguire et al. 2018; Sterba et al. 2014; Yabroff and Kim 2009). This wide dispersion of caregiving may manifest in terms of more diversity in relationship types (e.g., not just primary spousal caregiver) and less daily engagement with caregivers overall. Furthermore, rural cancer patients’ more diverse social networks, including more non-spousal caregivers and friends, appears to be due to the necessity of geographic proximity, rather than relationship strength and patient preferences (Burns et al. 2015; Kirby et al. 2016). Thus, larger, more diverse family/friend informal caregiver networks may not necessarily reflect patients’ access and utilization of available social support, but rather limited collective resources (e.g., limited capacity to provide financial support, limited time to provide tangible support) (Mulia et al. 2008) and a need to have many individuals to help them during their cancer diagnosis (Perry and Pescosolido 2015). However, to date, there is limited evidence describing how social factors may moderate associations between cancer-related stressors and health outcomes among rural cancer survivors. Our study advances this literature by examining specifically how structural components of family/friend informal caregiver networks (size, spousal caregiver, % kin, communication frequency) moderate associations between cancer-related debt and MHQOL among rural cancer survivors.
Current Study
This study contributes to literature characterizing cancer-related debt and its effects among rural populations in the U.S. First, we examined the association between cancer-related debt and MHQOL among a population of rural cancer survivors. We hypothesized that rural survivors who reported cancer-related debt reported lower MHQOL than those who did not report cancer-related debt. Second, we tested whether the association between cancer-related debt and MHQOL differed by family/friend informal caregiver network factors, specifically caregiver network size, presence of spousal caregiver, percent of kin caregivers, and percent of caregivers with whom the survivor has daily communication. We hypothesized that cancer-related debt would be more strongly associated with MHQOL among survivors with larger family/friend informal caregiver networks, networks without spousal caregivers, networks with fewer family caregivers, and networks with less daily communication.
DATA AND METHODS
Data
The Illinois Rural Cancer Assessment (IRCA) study was a statewide cross-sectional assessment that examined mental and physical health among rural cancer survivors and caregivers. For the current study, we focused only on survivor participants. This study was approved by the University of Illinois at Chicago Institutional Review Board and University of Illinois Cancer Center Protocol Review Committee. All participants provided informed consent either verbally (for phone and mail survey participants) or online.
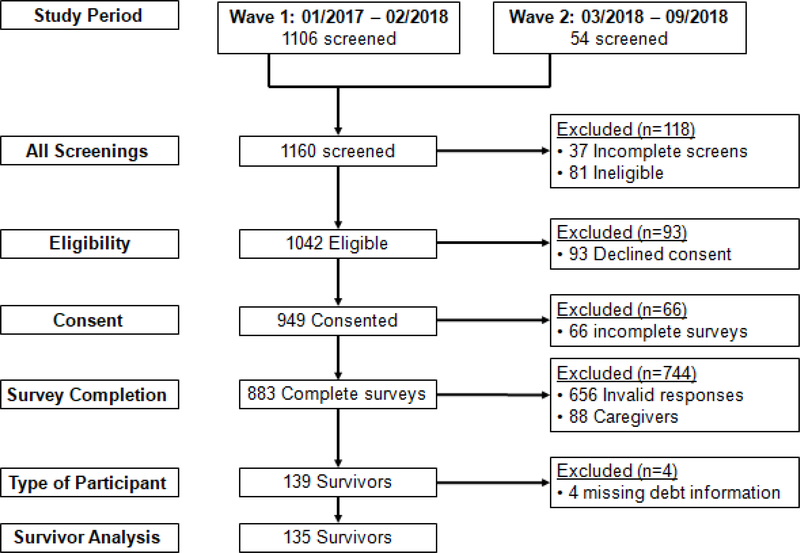
Participant recruitment occurred in two waves (Wave 1: January 2017 – February 2018 and Wave 2: March 2018 – September 2018). Wave 1 recruitment methods included physical flyers placed in clinical and community organizations that serve rural populations, including cancer centers, public health departments, clinics, and hospitals, churches, hair salons, support groups and at cancer-related events (e.g., Relay for Life); and electronic flyers distributed through websites, listservs, and social media. We focused Wave 2 recruitment efforts on outreach to rural African American adults in Illinois. We purchased a commercial list of landline and cellular phone numbers that used specific demographic targets and algorithms to identify African American adults from non-metropolitan counties in Illinois (2013 Rural Urban Continuum Code [RUCC] ≥4), as well as one metropolitan county (RUCC=3), due to its high proportion of African American adults and proximity to neighboring nonmetropolitan counties (United States Department of Agriculture 2016). Approximately 1–2 days prior to calling cellular phone numbers, research personnel sent text messages and an image of the recruitment flyer. Landline numbers only received a phone call from research personnel. The study team attempted to contact 3,214 phone numbers. The number of surveys completed of these attempted contacts was 20. For both waves, interested participants were able to visit a website or call research personnel, and interested Wave 2 participants could also respond to the recruitment text message with an attached website link. Of the final sample (n = 139), 119 survivors participated in Wave 1. See Figure 1 for an overview of IRCA study enrollment.
Figure 1:
Study Enrollment Flow Chat
After undergoing screening related to eligibility criteria (self-reported as 18 years or older, a cancer survivor, and a rural resident of the state of Illinois) and providing informed consent, participants in both waves completed the survey either online, by phone, or by mail. The survey took 60–90 minutes to complete. Participants received a $15 or $25 incentive. The incentive amount was increased midway through the study in order to encourage participation. All data were entered into a Qualtrics survey database by the participant or study staff, depending on mode of administration. Data were exported into IBM SPSS version 24 for analysis.
Measures
Covariates were measured with questions from the 2016 Behavioral Risk Factor Surveillance System (BRFSS) and the 2011 Medical Expenditure Panel Survey (MEPS) Experiences with Cancer Survivorship Supplement to obtain demographic and cancer-related information (Centers for Disease Control and Prevention 2016; Yabroff et al. 2012). Covariates included demographic characteristics (age, sex, race, marital status, education, employment, household income, household size, and rurality) and cancer-related characteristics (cancer site, number of cancers, time since last treatment, and treatment-related symptoms). We included treatment-related symptoms experienced during the past week to approximate disease severity and related complications, using an adjusted Physical Symptoms subscale of the Memorial Symptom Assessment Scale (Portenoy et al. 1994), which included the average of the following 8 symptoms: lack of appetite; lack of energy; pain; feeling drowsy; dry mouth; nausea; vomiting; and dizziness. Scoring incorporated the presence, frequency, and associated severity/distress of each symptom (0 = symptom not present; 0.8 = symptom present with no distress; 1.6 = symptom present and causes a little bit of distress; 2.4 = symptoms present and causes some distress; 3.2 = symptom present and causes quite a bit of distress; 4.0 = symptom present and causes much distress).
Cancer-related debt was measured using a single-item question modified from the 2011 MEPS: “Have you or has anyone in your family had to borrow money, go into debt, or file for bankruptcy because of your cancer, its treatment, or the lasting effects of that treatment?” Possible response categories were No or Yes. In the analyses and results, cancer-related debt is referred to as “debt”.
Mental Health-related Quality of Life (MHQOL) was measured using the Short Form-12 Health Survey (SF-12) Mental Component Summary Score (MCS-12). Scores range from 0 to 100, where 0 indicates the lowest level of health and 100 indicates the highest (Ware, Kosinski, and Keller 1996). The MCS-12 includes measures of general health, physical functioning, role functioning (physical), role functioning (emotional), bodily pain, vitality, mental health, and social functioning (Ware, Kosinski, and Keller 1996), providing a comprehensive assessment of mental health and well-being. All MCS-12 questions asked how respondents had been feeling in the past 4 weeks, except for three questions that asked how respondents were feeling “now”. The MCS-12 scale was created by generating indicator variables, adding population weights, summing all variables, and transforming the summary scale to norm-based scoring, as outlined by Ware, Kosinski and Keller (1996).
Family/friend informal caregiver network size and composition were assessed using items and procedures from Burt’s General Social Survey social network instrument (Burt 1984). Similar to other ego-network measurement tools, there was first a description of family/friend informal caregivers (“This section is about caregivers, meaning friends or family members who may have provided help with getting to the doctor, going to appointments with you, making decisions about treatment, or providing other types of care and support during or after cancer treatment.”). Subsequently, participants were asked, “Since the time you were first diagnosed with cancer, has any friend or family member provided care to you during or after your treatment?.” If participants answered yes, they were asked to enter names on a table that had 5 columns (“For each person, please fill in their name in the top row.”). We used the number of unique names provided to calculate caregiver network size. Limiting the number of identified names has been previously noted as useful for pilot field studies, such as this one, to minimize respondent burden (Schneider et al. 2013) and demonstrate feasibility of social network data collection (Burt 1984). Subsequently, participants were told, “We’d like to find out a little more about this person/these people. Please answer all of the questions for each person, individually. Every caregiver will have their own column.” They then provided each caregiver’s demographic information, current communication status, and their relationship to the participant (name interpreter questions). From these variables, we estimated the following four variables: family/friend informal caregiver network size (0–5); if one of the caregivers was a spouse (no/yes); percent of caregivers who were non-spousal relatives (0–100%); and percent of caregivers with whom survivors had current daily communication (0–100%).
Statistical Analysis
We first provided missingness and descriptive statistics for demographic, cancer-related, family/friend informal caregiver network factors and MHQOL, in Table 1, for the 135 participants who had data on cancer-related debt, network factors, and MHQOL. We conducted bivariable chi-square, Pearson’s exact tests, and regression analyses to examine differences between demographic, cancer-related, network, and MHQOL variables by debt status (Table 1).
Table 1.
Study sample characteristics (n = 135).
| Overall (n= 135) | Reported No Debt (n = 98) | Reported Any Debt (n = 37) | |||||
| DEMOGRAPHIC | Missing (%) | n | % | n | % | n | % |
| Age | 0% | ||||||
| ≤53 years old | 49 | 36% | 32 | 33% | 17 | 46% | |
| 54–64 years old | 48 | 36% | 34 | 35% | 14 | 38% | |
| 65–83 years old | 38 | 28% | 32 | 33% | 6 | 16% | |
| Sex | 0% | ||||||
| Male | 23 | 17% | 17 | 17% | 6 | 16% | |
| Female | 112 | 83% | 81 | 83% | 31 | 84% | |
| Race | 0% | ||||||
| Non-Latino White | 122 | 90% | 87 | 89% | 35 | 95% | |
| Other | 13 | 10% | 11 | 11% | 2 | 5% | |
| Marital Status | 0% | ||||||
| Married | 94 | 70% | 73 | 75% | 21 | 57% | |
| Not Married | 41 | 30% | 25 | 25% | 16 | 43% | |
| Education | 0% | ||||||
| <Bachelor’s Degree | 75 | 56% | 51 | 52% | 24 | 65% | |
| ≥Bachelor’s Degree | 60 | 44% | 47 | 48% | 13 | 35% | |
| Employment | 0% | ||||||
| Full-time employed | 63 | 47% | 50 | 51% | 13 | 35% | |
| Other | 72 | 53% | 48 | 49% | 24 | 65% | |
| Household income | 5% | ||||||
| <$35,000 | 36 | 27% | 23 | 23% | 13 | 35% | |
| $35,001–$50,000 | 27 | 20% | 17 | 17% | 10 | 27% | |
| ≥$50,001 | 65 | 48% | 53 | 54% | 12 | 32% | |
| Household size | 2% | ||||||
| 1–2 (including self) | 83 | 62% | 69 | 70% | 14 | 38% | |
| 3–6 | 49 | 36% | 28 | 29% | 21 | 57% | |
| RUCC | 0% | ||||||
| Metropolitan (1–3) | 52 | 38% | 41 | 42% | 11 | 30% | |
| Non-metropolitan (4–10) | 83 | 62% | 57 | 58% | 26 | 70% | |
| CANCER-RELATED | Missing (%) | n | % | n | % | n | % |
| Cancer sites | <1% | ||||||
| Breast cancer | 50 | 37% | 33 | 34% | 17 | 46% | |
| Gynecological | 10 | 7% | 8 | 8% | 2 | 5% | |
| Digestive | 11 | 8% | 8 | 8% | 3 | 8% | |
| Skin | 17 | 13% | 15 | 15% | 2 | 5% | |
| Lymphoma | 14 | 10% | 12 | 12% | 2 | 5% | |
| Other | 32 | 24% | 21 | 21% | 11 | 30% | |
| Number of cancers | 0% | ||||||
| One | 107 | 79% | 78 | 80% | 29 | 78% | |
| Multiple | 28 | 21% | 20 | 20% | 8 | 22% | |
| Treatment-related physical symptoms | 0% | ||||||
| None | 50 | 37% | 39 | 40% | 11 | 30% | |
| Any | 85 | 63% | 59 | 60% | 26 | 70% | |
| Time since last treatment | <1% | ||||||
| <1 year ago | 42 | 31% | 29 | 30% | 13 | 35% | |
| 1–4 years ago | 38 | 28% | 26 | 27% | 12 | 32% | |
| ≥5 years ago | 49 | 36% | 37 | 38% | 12 | 32% | |
| No treatment needed | 5 | 4% | 5 | 5% | 0 | 0% | |
| INFORMAL CAREGIVER NETWORK FACTORS | Missing (%) | n | % | n | % | n | % |
| Spousal informal caregiver | 0 | 69 | 51% | 53 | 54 | 16 | 43 |
| Number of family/friend informal caregivers | 0 | ||||||
| 0 | 36 | 27% | 29 | 30% | 7 | 19% | |
| 1 | 37 | 27% | 32 | 33% | 5 | 14% | |
| 2 | 20 | 15% | 13 | 13% | 7 | 19% | |
| 3 | 14 | 10% | 6 | 6% | 8 | 22% | |
| 4 | 12 | 9% | 10 | 10% | 2 | 5% | |
| 5 | 16 | 12% | 8 | 8% | 8 | 22% | |
| M | SD | M | SD | M | SD | ||
| % kin informal caregivers | 0 | 22% | 33% | 18% | 32% | 35% | 34% |
| % current daily communication | 0 | 53% | 42% | 51% | 44% | 56% | 37% |
| QOL | Missing (%) | M | SD | M | SD | M | SD |
| Mental health-related QOL | 0 | 49.32 | 10.25 | 50.74 | 9.45 | 45.56 | 11.45 |
Note: Variables age, education, household income, household size, RUCC, treatment-related physical symptoms, and number of caregivers are continuous but depicted categorically to facilitate interpretability. Categories for cancer sites and time since last treatment are provided to describe the sample. Debt = cancer-related debt, borrowed money, and/or bankruptcy. RUCC=Rural Urban Continuum Code
Next, we conducted bivariate regressions to examine the relationship of debt, network, demographic, and cancer-related factors with MHQOL (Table 2). Only one predictor was included per model in Table 2. Effect sizes and unstandardized coefficients with 95% confidence intervals are reported. These analyses identified covariates to include in subsequent moderation analyses.
Table 2.
Bivariate linear and logistic regressions, with whole case analysis (n=125)
| MHQOL (Linear Regression) | Debt Status (Logistic Regression) | ||||||
|---|---|---|---|---|---|---|---|
| Cohen’s f | Unstd B | 95%CI | p-value | OR | 95%CI | p-value | |
| Debt | 0.23 | −5.21 | −9.26, −1.15 | 0.01 | -- | --- | --- |
| INFORMAL CAREGIVER NETWORK FACTORS | |||||||
| Family/friend informal caregiver network size (up to 5) | 0.03 | −0.23 | −1.30, 0.84 | 0.68 | 1.33 | 1.06, 1.66 | 0.02 |
| Spousal informal caregiver (REF: No) | 0.18 | 3.36 | −0.30, 7.01 | 0.07 | 0.56 | 0.25, 1.24 | 0.56 |
| % kin informal caregivers | 0.04 | −1.40 | −6.88, 4.09 | 0.62 | 3.97 | 1.29, 12.23 | 0.02 |
| % current daily communication | 0.10 | 2.60 | −1.81, 7.00 | 0.25 | 1.49 | 0.58, 3.86 | 0.41 |
| DEMOGRAPHIC | |||||||
| Age | 0.23 | 0.20 | 0.05, 0.35 | 0.009 | 0.96 | 0.92, 0.99 | 0.01 |
| Sex (REF: Male) | 0.14 | −3.39 | −8.22, 1.43 | 0.17 | 1.33 | 0.45, 3.95 | 0.60 |
| Race (REF: non-Latino White) | 0.10 | 4.07 | −2.17, 10.32 | 0.20 | 0.51 | 0.11, 2.44 | 0.40 |
| Marital Status (REF: Married) | 0.10 | −1.56 | −5.52, 2.40 | 0.43 | 2.08 | 0.92, 4.73 | 0.08 |
| Education | 0.10 | 0.99 | −0.50, 2.48 | 0.19 | 0.88 | 0.64, 1.20 | 0.42 |
| Employment (REF: Full-time employed) | 0.10 | 2.22 | −1.50, 5.93 | 0.24 | 0.45 | 0.19, 1.04 | 0.06 |
| Household income | 0.14 | 1.12 | −0.25, 2.50 | 0.11 | 0.78 | 0.58, 1.05 | 0.10 |
| Household size | 0.18 | −1.37 | −2.87, 0.13 | 0.07 | 1.64 | 1.18, 2.28 | 0.003 |
| RUCC | 0.06 | −0.34 | −1.29, 0.61 | 0.48 | 1.15 | 0.94, 1.41 | 0.19 |
| CANCER-RELATED | |||||||
| Cancer site (REF: Breast) | 0.14 | −2.74 | −6.55, 1.07 | 0.16 | 1.81 | 0.81, 4.03 | 0.15 |
| Number of cancers (REF: One) | 0.10 | −2.77 | −7.45, 1.91 | 0.24 | 0.87 | 0.31, 2.41 | 0.79 |
| Treatment-related physical symptoms | 0.27 | −3.81 | −6.29, −1.32 | 0.003 | 1.02 | 0.59, 1.76 | 0.94 |
| Time since last treatment (REF: <5 years ago) | 0.20 | −4.40 | −0.68, −8.11 | 0.02 | 0.56 | 0.24, 1.30 | 0.17 |
Note: Significant analyses in bold. Bivariate analyses include only the single predictor of interest noted above. Debt = cancer-related debt, borrowed money, and/or bankruptcy. RUCC=Rural Urban Continuum Code. Due to small sample sizes, bivariate analyses consider dichotomous variables (cancer site – breast, other; time since last treatment – <5 years, ≥5 years or no treatment needed).
For the moderation models, described in Table 3, we followed the moderation checklist provided by Frazier, Tix and Baron (2004). We checked for interactions between the predictor, debt, and each of the four family/friend informal caregiver networks factors; we then stratified by the signification interaction (Frazier, Tix, and Barron 2004). Due to the observational nature of our study, there were unequal sizes in groups. First, we conducted one multivariable linear regression wherein the outcome was MHQOL and the predictors were debt, all four network factors, and the demographic and cancer-related covariates (Model 1). Next, we conducted four multivariable linear regressions, wherein the outcome was MHQOL and predictors included covariates identified by Tables 1 and 2, main effects (debt, 4 network factors), and one interaction term (debt*network factors) (Models 2–5). A statistically significant interaction term indicated support for moderation. If significant, we depicted group-specific estimates for survivors with no debt and survivors with debt based on the moderating network characteristic. We also described patterns from supplemental analyses.
Table 3.
Main and interactive effects of cancer-related debt and family/friend informal caregiver network factors on quality of life, after adjusting for demographic and cancer-related variables, using complete case analysis (n = 125).
| Model # | MHQOL | ||||
|---|---|---|---|---|---|
| Main Effects | Cohen’s f | Unstd B | 95%CI | p-value | |
| 1 | Debt | 0.14 | −3.54 | −7.99, 0.91 | 0.12 |
| Family/friend informal caregiver network size | 0.01 | 0.10 | 1.26, 1.46 | 0.89 | |
| Spousal informal caregiver | 0.14 | 3.34 | −1.65, 8.32 | 0.19 | |
| % kin informal caregivers | 0.03 | 0.85 | −5.62, 7.31 | 0.80 | |
| % daily communication | 0.01 | 0.43 | −4.79, 5.64 | 0.87 | |
| Interactive Effects | |||||
| 2 | Debt * Family/friend informal caregiver network size | 0.04 | |||
| 3 | Debt * Spousal informal caregiver | 0.47 | |||
| 4 | Debt * % kin informal caregivers | 0.36 | |||
| 5 | Debt * % daily communication | 0.06 | |||
Notes. Significant analyses in bold. Debt = cancer-related debt, borrowed money, and/or bankruptcy. Adjusted for age, marital status, household size, treatment-related physical symptoms, and time since last treatment. Appendix 1 provides similar patterns when using multiple imputation and including all available covariates.
Finally, in Table 4, we conducted bivariable chi-square, Pearson’s exact tests, and regression analyses to examine differences between demographic, cancer-related, social, and MHQOL variables by network factors that emerged as moderators.
Table 4.
Demographic, cancer-related, and social network factors by number of family/friend informal caregivers (n = 125).
| 0 Caregivers (n = 35) | 1–2 Caregivers (n = 49) | 3–5 Caregivers (n = 41) | |||||
| DEMOGRAPHIC | n | % | n | % | N | % | p-value |
| Age | 0.04 | ||||||
| ≤53 years old | 15 | 43 | 13 | 27 | 19 | 46 | |
| 54–64 years old | 11 | 31 | 16 | 33 | 17 | 42 | |
| 65–83 years old | 9 | 26 | 20 | 41 | 5 | 12 | |
| Sex | 0.19 | ||||||
| Male | 6 | 17 | 12 | 25 | 4 | 10 | |
| Female | 29 | 83 | 37 | 76 | 37 | 90 | |
| Race | 0.16 | ||||||
| non-Latino White | 30 | 86 | 43 | 88 | 40 | 98 | |
| Other | 5 | 14 | 6 | 12 | 1 | 2 | |
| Marital Status | 0.26 | ||||||
| Married | 20 | 57 | 35 | 71 | 30 | 73 | |
| Not married | 15 | 43 | 14 | 29 | 11 | 27 | |
| Education | 0.52 | ||||||
| <Bachelor’s degree | 11 | 61 | 20 | 74 | 19 | 76 | |
| ≥Bachelor’s degree | 7 | 39 | 7 | 26 | 6 | 24 | |
| Employment | 0.20 | ||||||
| Full-time employed | 22 | 63 | 23 | 47 | 26 | 63 | |
| Other | 13 | 37 | 26 | 53 | 15 | 37 | |
| Household income | 0.61 | ||||||
| <$35,000 | 8 | 33 | 13 | 39 | 13 | 50 | |
| $35,001–$50,000 | 10 | 42 | 9 | 27 | 7 | 27 | |
| ≥$50,001 | 6 | 25 | 11 | 33 | 6 | 23 | |
| Household size | 0.06 | ||||||
| 1–2 (including self) | 22 | 63 | 36 | 74 | 20 | 49 | |
| 3–6 | 13 | 37 | 13 | 27 | 21 | 51 | |
| RUCC | 0.74 | ||||||
| Metropolitan (1–3) | 11 | 31 | 19 | 39 | 16 | 39 | |
| Non-metropolitan (4–10) | 24 | 69 | 30 | 61 | 25 | 61 | |
| CANCER-RELATED | |||||||
| Cancer sites | 0.05 | ||||||
| Breast cancer | 9 | 26 | 16 | 33 | 21 | 51 | |
| Gynecological | 5 | 14 | 2 | 4 | 2 | 5 | |
| Digestive | 1 | 3 | 6 | 12 | 4 | 10 | |
| Skin | 10 | 29 | 4 | 8 | 2 | 5 | |
| Lymphoma | 1 | 3 | 5 | 10 | 6 | 15 | |
| Other | 9 | 26 | 16 | 33 | 6 | 15 | |
| Number of cancers | 0.76 | ||||||
| One | 29 | 83 | 38 | 78 | 34 | 83 | |
| Multiple | 6 | 17 | 11 | 22 | 7 | 17 | |
| Treatment-related physical symptoms | 0.39 | ||||||
| None | 14 | 40 | 21 | 43 | 12 | 29 | |
| Any | 21 | 60 | 28 | 57 | 29 | 71 | |
| Time since last treatment | 0.06 | ||||||
| <1 year ago | 11 | 31 | 14 | 29 | 15 | 37 | |
| 1–4 years ago | 11 | 31 | 10 | 20 | 15 | 37 | |
| ≥5 years ago | 11 | 31 | 22 | 45 | 11 | 27 | |
| No treatment needed | 2 | 6 | 3 | 6 | 0 | 0 | |
| FAMILY/FRIEND INFORMAL CAREGIVERS | N | % | n | % | n | % | p-value |
| Spousal informal caregiver | -- | -- | 34 | 69 | 27 | 66 | 0.72 |
| M | SD | M | SD | M | SD | p-value | |
| % kin informal caregivers | -- | -- | 22% | 37% | 45% | 54% | 0.003 |
| % current daily communication | -- | -- | 87% | 27% | 54% | 28% | <0.0001 |
| QUALITY OF LIFE | M | SD | M | SD | M | SD | p-value |
| Mental health | 48.34 | 9.97 | 49.98 | 10.28 | 48.55 | 11.10 | 0.73 |
Note: Variables age, education, household income, household size, RUCC, and number of caregivers are continuous but depicted categorically to facilitate interpretability. Categories for cancer sites and time since last treatment are provided to describe the sample. Significant associations (p ≤.05) are marked in bold.
Debt = cancer-related debt, borrowed money, and/or bankruptcy. RUCC=Rural Urban Continuum Code.
Due to small sample sizes, bivariate analyses consider dichotomous variables (cancer site – breast, other; time since last treatment – <5 years, ≥5 years or no treatment needed).
RESULTS
Table 1 presents demographic and cancer-related sample characteristics. A majority of the sample were women (83%), 90% identified as non-Latino white, 70% were married, 44% had a Bachelor’s degree or above, 48% had an annual household income of $50,001 or above, and 62% lived in counties designated as non-metropolitan. Approximately 21% of our sample reported multiple cancers, 63% reported at least one treatment-related physical symptom, and 36% of our sample had completed treatment over 5 years before survey participation. Over a quarter of the sample (n=37) reported cancer-related debt. The average MHQOL score was 49.32 (SD = 10.25). With regard to missingness, four were missing data on one of our primary variables, seven were missing current annual household income, three were missing household size, one was missing cancer site, and one was missing time since the last cancer treatment. To address missingness, we used complete case analysis, given models with imputed and nonimputed data were comparable. For supplementary analyses with imputed data (Appendix 1), we used chained equations imputation (White, Royston, and Wood 2011) with 20 iterations, based on decisions concerning the fraction of missing information and a minimal tolerance for power falloff (Graham, Olchowski, and Gilreath 2007). Imputation models specified interactive terms of interest, in line with von Hippel’s recommendations (Von Hippel 2009), as well as covariates listed below.
Table 2 presents associations between debt and MHQOL with cancer-related debt status, network factors, demographic factors, and cancer-related factors. Participants reporting cancer-related debt, younger participants, participants reporting more treatment-related physical symptoms, and participants who more recently completed treatment reported worse MHQOL. Associations were mostly small in terms of magnitude, except for a moderate association between treatment-related physical symptoms and MHQOL. Participants with larger networks, participants with networks with more relatives, younger participants, and participants with larger household sizes had greater odds of reporting debt. Associations were relatively small in terms of magnitude, except for a moderate association between % kin caregivers and debt. Based on these analyses and previous literature regarding MHQOL, we included the following covariates in subsequent models: age, marital status, household size, treatment-related physical symptoms, and time since last treatment. We did not adjust for sex and race in primary analyses, due to small cell sizes. Appendix 1 provides supplement analyses with all covariates included, which should be treated cautiously.
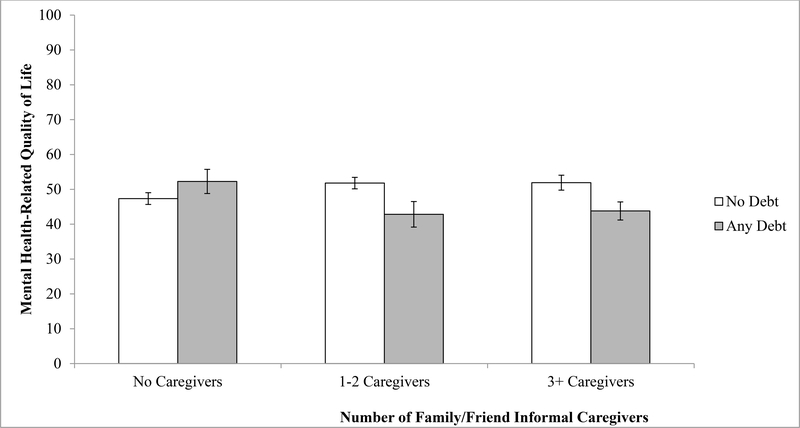
Table 3 presents findings from different multivariable regression models including debt and informal caregiver network factors (caregiver network size, spousal caregiver, percentage kin caregivers, percentage daily communication) on MHQOL, after adjusting for age, marital status, household size, treatment-related physical symptoms, and time since last treatment. There were no significant main effects when including cancer-related debt and all four network factors (Model 1). Multivariable regression models including interaction terms (Models 2–5) suggested a significant interaction between debt and family/friend informal caregiver network size. Figure 2 depicts group-specific estimates by caregiver network size and associated standard errors. Among participants with family/friend informal caregivers, participants with debt appeared to report slightly worse MHQOL than participants without any debt.
Figure 2.
Mean Differences and Associated Standard Errors in Mental Health-related Quality of Life between Survivors Reporting No Debt versus Any Debt Among Survivors with No Family/Friend Informal Caregivers, 1–2 Family/Friend Informal Caregivers, and 3+ Family/Friend Informal Caregivers (n= 125).
Given these findings, we conducted chi-square, Pearson’s exact tests, and regression analyses to examine differences between demographic, cancer-related, informal caregiver network, and MHQOL variables by caregiver network size (Table 4). Significant differences were observed in age and cancer site diagnoses across participants with no caregivers, 1–2 caregivers, and 3–5 caregivers. Patients with 3–5 caregivers appeared to be somewhat younger and more likely to have a breast cancer diagnosis. In comparison to participants with 1–2 caregivers, participants with 3–5 caregivers reported a greater proportion of caregivers who were relatives and a lower proportion of caregivers with whom they had daily communication.
DISCUSSION
This study contributes to a small but growing body of literature regarding cancer-related financial hardship among rural cancer survivors. Only four studies of which we are aware have addressed this topic (McDougall et al. 2018; Palmer et al. 2013; Pisu et al. 2017; Zahnd et al. 2019). No research, to our knowledge, has examined the relationship between cancer-related debt and MHQOL among rural cancer survivors. Further, no research has examined the interactive effects of diverse determinants of rural survivors’ MHQOL, including how cancer-related debt and family/friend informal caregiver networks interact.
In the current study, rural survivors who reported debt were younger, less likely to be married, lived in households with more individuals, and less likely to have a spousal caregiver. A study characterizing variation in financial hardship among rural survivors found younger breast cancer survivors had greater out-of-pocket cost burden, compared to older survivors (Pisu et al. 2017). Thus, it appears that younger rural survivors may be particularly vulnerable to cancer-related financial hardship.
When we examined the relationship between cancer-related debt and MHQOL among rural survivors, we found that debt had a significant depressive effect on MHQOL for survivors who had any family/friend informal caregivers, but not for survivors without family/friend informal caregivers (0 caregivers). Our findings suggest that larger family/friend informal caregiver networks exacerbate the negative effect of cancer-related debt on rural survivors’ MHQOL. These findings supplement what is already known about the role of social connectedness in cancer survivors’ health outcomes by focusing on established family and friend ties in the caregiving context. Our study findings can be interpreted in a number of ways.
First, our findings may implicate collective poverty and poor relationship quality. Within economically under-resourced networks, larger family/friend informal caregiver network size may not represent greater access to resources, as noted above (Mulia et al. 2008). As Kawachi and Berkman (2001) note, “social connections may paradoxically increase levels of mental illness symptoms among women with low resources, especially if such connections entail role strain associated with obligations to provide social support to others” (2001: 458). Simultaneously, our findings may suggest that survivors have to rely on more relationships that are poorer in quality, which is linked to worse health outcomes (Kroenke et al. 2012).
Second, our findings may reflect exposure to debt stigma. Stigma associated with financial hardship may be understood as the internalization of neoliberal ideologies and assumed personal responsibility for one’s debt (Sweet 2018). It may be particularly great in the context of marginalized populations in vulnerable social positions (Peacock, Bissell, and Owen 2013). Related research suggests that poor rural residents are more likely to perceive assistance, whether from government or society, as negative (Amato and Zuo 1992; Myers and Gill 2004); therefore, “accepting needed help can further feelings of inadequacy and failure” (Myers and Gill 2004: 236). Furthermore, poverty has a greater stigma in rural areas (Amato and Zuo 1992; Myers and Gill 2004; Rank and Hirschl 1988), and we may be observing a similar stigma regarding cancer-related debt among rural survivors. This may be particularly exacerbated in large networks, wherein there are many opportunities for “shame-inducing” social comparisons with caregivers and other members of their community (Peacock, Bissell, and Owen 2013). Thus, those with larger family/friend informal caregiver networks may perceive additional stigma and embarrassment related to cancer-related debt, rather than a positive buffering effect of financial strain on MHQOL.
Third, our findings may demonstrate greater patient need in relation to cancer, which may heighten the impact of financial stress and approximate negative interpersonal dynamics (e.g., greater conflict). This would align with research on other health conditions, wherein network activation, and subsequently network size, may be positively related to disease severity (Perry and Pescosolido 2015). While we have data on treatment-related physical symptoms and social network size, we did not have an adequate sample size to assess the interactive effects of network size, physical symptoms, and debt. Relatedly, it is possible that the objective and perceived impacts of debt may differ by cancer site. Within our sample, more survivors of skin and gynecological cancers reported having no caregivers than those with breast or digestive cancers or lymphoma. Skin cancer has historically been one of the least invasive and financially burdensome cancers to treat, though treatment costs are rising in recent years (Chen, Kempton, and Rao 2016; Rogers and Coldiron 2009).
Limitations
Limitations of the current study include its cross-sectional design; low response rates; limited racial and gender representation of cancer survivors in rural Illinois; focus on family/friend informal caregivers; and measurement issues. Our cross-sectional design inhibited our capacity to assess causal relationships. Due to low response rates, our sample was small and included predominantly non-Latina white women, despite our efforts to obtain a more diverse sample. The failure to recruit minority participants was in part due to limited resources to conduct comprehensive statewide recruitment by trusted community partners. Simultaneously, it should be noted that the rural population in Illinois is relatively less racially/ethnically diverse than other rural communities throughout the United States (91% non-Latino white in 2010) (Housing Assistance Council 2012). Relatedly, Wave 2 involved commercial phone lists; yet, previous research has suggested that recruitment from trusted sources may be more effective in recruiting minority populations than random digit dialing and other “cold call” efforts (Yancey, Ortega, and Kumanyika 2006).
Our findings were also likely affected by having a sample of mostly women. Our study may specifically reflect rural women’s unique challenges with employment (Smith 2011) and simultaneous pressure to be the primary source of family income as rural men’s jobs wane (Smith and Tickamyer 2011), women cancer patients’ worse mental health relative to their male counterparts (Linden et al. 2012), and rural women’s elevated risk for mental health problems (Myers and Gill 2004). With regard to networks and cancer outcomes, it should be noted that a significant proportion of the literature on the networks of cancer survivors has focused on women cancer survivors (Kroenke 2018). Limited existing literature suggests that network and support effects on mental health may be stronger among women (Hann et al. 2002), potentially due to the different types of support that are given to them relative to men (Wareham, Fowler, and Pike 2007). Altogether, our findings regarding cancer-related debt, informal caregiver networks, and MHQOL may not be generalizable or relationships may be weaker for men survivors.
Our study may also have been affected by the types of measures we used. The use of self-reported measures of debt and disease severity may contribute to response bias and limit the interpretation of findings. Unfortunately, we were not able to incorporate robust self-report or objective measures of disease severity (i.e., duration of treatment, cancer stage) in analyses, although we did include time since treatment and treatment-related physical symptoms as proxy covariates. Future work would benefit from using cancer tumor registry data (Centers for Disease Control and Prevention 2019), which includes information on stage of disease at treatment as well as time from treatment. Further, our instruments to characterize survivors’ caregiver networks were limited in terms of the number of alters that participants could identify and due to the wording, which offered a somewhat broad definition of support and caregiving. Future studies should consider a more inclusive name generator, wherein the survivor is prompted to provide all possible names, to calculate a robust measure of family/friend informal caregiver network size. This will also be helpful for contextualizing research on rural survivors’ networks relative to research that leverages other measures of caregiver network size (Ashida et al. 2009; Payne, Palmer Kelly, and Pawlik 2019; Sapp et al. 2003). While measures of social network size are different and challenging to compare, we note that relatively few individuals in this study reported the maximum number of alters (5). The wording of name generators can affect which alters are identified and the overall composition of participants’ networks (Bailey and Marsden 1999; Marsden 2003; Straits 2000). Wording is thus particularly important, given the composition of missing data/missed alter opportunities has important implications for bias in social network research, although networks regarding peer influence may be relatively stable in the face of such missing data (Smith, Moody, and Morgan 2017). Future studies are warranted that leverage multiple name generators to address these potential effects, especially in terms of highlighting specialized types of support (e.g., nurses, healthcare workers) and caregiving (e.g., paid versus informal).
Our findings may have been different if we had included formal caregivers, healthcare workers, and/or more peripheral but cancer-specific ties (e.g., peer survivors) in our analysis. While distress may also be experienced in the patient-formal caregiver relationship (Goldzweig et al. 2015), given the temporary nature of such relationships and specialized cancer-specific support they provide, it’s possible that their presence would have buffered the effect of cancer-related debt on MHQOL for survivors. Furthermore, measurement including more broad social networks may have demonstrated more buffering effects, based on the past literature (Beasley et al. 2010; Berkman 1995; Chou et al. 2012; Cornwell and Laumann 2015; Frank, Davis, and Elgar 2014; Haynie et al. 2018; Huang and Hsu 2013; Klijs et al. 2017; Kroenke et al. 2006; Michael et al. 2002; Sapp et al. 2003; Schafer and Koltai 2015). While we provide interesting data regarding a specific type of network (i.e., family/friend informal caregivers), it is pivotal for future studies to replicate our findings by capturing data on survivors’ broader, more diverse networks. Further, our study did not characterize the type, amount, and benefit of support that caregivers provided. Characterizing the type of support is needed in future studies, as there is variation in how different types of support are associated with health (Cohen and Wills 1985; Tajvar, Grundy, and Fletcher 2018). We also did not measure closeness, or the strength of the relationships between survivors and their caregivers, which may be particularly relevant for MHQOL (Kossakowski et al. 2016; Perry and Pescosolido 2015). Future studies are warranted that address these gaps for substantive theoretical and practical implications regarding networks, financial factors, and health. Objective measures of debt and psychosocial stress are also needed to confirm study findings.
Despite the aforementioned limitations, our study is an important contribution to the growing body of literature regarding cancer-related financial hardship among rural cancer survivors (McDougall et al. 2018; Palmer et al. 2013; Pisu et al. 2017; Zahnd et al. 2019). To our knowledge, the present study is the first to examine the relationship between cancer-related debt and MHQOL among rural cancer survivors, and to assess how family/friend informal caregiver networks moderate this relationship.
Implications for Future Research and Conclusion
Future research on cancer-related financial hardship should recruit larger, more diverse samples in order to more fully assess the impact of this stressor on underserved rural survivors. Such work is pivotal, given these suggestive findings may have important implications but cannot be confirmed without larger, more representative samples. Indeed, our use of validated survey tools from the 2011 MEPS Experiences with Cancer Survivorship Supplement, BRFSS, the General Social Survey social network instrument, and the Short Form-12 Health Survey allows comparison with research on other cancer survivor populations. Further, future work should also investigate the nature of ties between survivors and their caregivers in more depth, including using strategies discussed above to measure network size, to incorporate different segments of patients’ networks, to quantify type, amount, and benefits of support given, and to incorporate closeness and centrality measures. The topic of potential stigma related to cancer-related financial strain among rural populations also requires further inquiry. Finally, researchers should direct efforts toward understanding how cancer-related financial hardship can best be ameliorated for rural survivors. We support recent calls for increased investment in research in rural areas in order to more fully understand the impact of cancer for America’s rural residents (Blake et al. 2017; Ghazarian, Martin, and Lam 2018; Meilleur et al. 2013; Paskett 2015).
This study makes a key contribution to a growing body of literature on cancer-related debt and its impact on rural cancer survivors. The current study advances this small but emergent body of literature by establishing a negative association between debt and MHQOL among rural survivors with larger family/friend informal caregiver networks.
Supplementary Material
Footnotes
Conflict of Interest/Financial Disclosure Statement: The authors declare that there are no conflicts of interest and no financial disclosures to report.
REFERENCES
- Adelman Ronald D., Tmanova Lyubov L., Delgado Diana, Dion Sarah, and Lachs Mark S. 2014. “Caregiver Burden: A Clinical Review.” JAMA 311(10):1052–60. [DOI] [PubMed] [Google Scholar]
- Amato Paul R. and Zuo Jiping. 1992. “Rural Poverty, Urban Poverty, and Psychological Well-Being.” The Sociological Quarterly 33(2):229–40. [Google Scholar]
- Andrykowski MA, Steffens RF, Bush HM, and Tucker TC 2014. “Disparities in Mental Health Outcomes among Lung Cancer Survivors Associated with Ruralness of Residence.” Psycho-Oncology 23(4):428–36. [DOI] [PubMed] [Google Scholar]
- Arora Neeraj K., Rutten Lila J. Finney, Gustafson David H., Moser Richard, and Hawkins Robert P. 2007. “Perceived Helpfulness and Impact of Social Support Provided by Family, Friends, and Health Care Providers to Women Newly Diagnosed with Breast Cancer.” Psycho‐Oncology 16(5):474–86. [DOI] [PubMed] [Google Scholar]
- Ashida Sato, Palmquist Aunchalee E. L., Basen-Engquist Karen, Singletary S. Eva, and Koehly Laura M. 2009. “Changes in Female Support Network Systems and Adaptation After Breast Cancer Diagnosis: Differences Between Older and Younger Patients.” The Gerontologist 49(4):549–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey Stefanie and Marsden Peter V. 1999. “Interpretation and Interview Context: Examining the General Social Survey Name Generator Using Cognitive Methods.” Social Networks 21(3):287–309. [Google Scholar]
- Beasley Jeannette M., Newcomb Polly A., Trentham-dietz Amy, Hampton John M., Ceballos Rachel M., Titus-ernstoff Linda, Egan Kathleen M., and Holmes Michelle D. 2010. “Social Networks and Survival after Breast Cancer Diagnosis.” Journal of Cancer Survivorship 4(4):372–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman Lisa F. 1995. “The Role of Social Relations in Health Promotion.” Psychosomatic Medicine 57(3):245–54. [DOI] [PubMed] [Google Scholar]
- Bishaw Alemayehu and Posey Kirby G. 2016. A Comparison of Rural and Urban America: Household Income and Poverty. United States Census Bureau; Washington D.C. [Google Scholar]
- Blake Kelly D., Moss Jennifer L., Gaysynsky Anna, Srinivasan Shobha, and Croyle Robert T. 2017. “Making the Case for Investment in Rural Cancer Control: An Analysis of Rural Cancer Incidence, Mortality, and Funding Trends.” Cancer Epidemiology Biomarkers & Prevention 26(7):992 LP–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns Catherine M., Eleonora Dal Grande Jennifer Tieman, Abernethy Amy P., and Currow David C. 2015. “Who Provides Care for People Dying of Cancer? A Comparison of a Rural and Metropolitan Cohort in a S Outh A Ustralian Bereaved Population Study.” Australian Journal of Rural Health 23(1):24–31. [DOI] [PubMed] [Google Scholar]
- Burridge Letitia, Winch Sarah, and Clavarino Alexandra. 2007. “Reluctance to Care: A Systematic Review and Development of a Conceptual Framework.” Cancer Nursing 30(2):E9–E19. [DOI] [PubMed] [Google Scholar]
- Burris Jessica L. and Andrykowski Michael. 2010. “Disparities in Mental Health between Rural and Nonrural Cancer Survivors: A Preliminary Study.” Psycho-Oncology 19(6):637–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt Ronald S. 1984. “Network Items and the General Social Survey.” Social Networks 6(4):293–339. [Google Scholar]
- Butow Phyllis N., Phillips Fiona, Schweder Janine, White Kate, Underhill Craig, and Goldstein David. 2012. “Psychosocial Well-Being and Supportive Care Needs of Cancer Patients Living in Urban and Rural/Regional Areas: A Systematic Review.” Supportive Care in Cancer 20(1):1–22. [DOI] [PubMed] [Google Scholar]
- Callaghan Patrick and Morrissey Jean. 1993. “Social Support and Health: A Review.” Journal of Advanced Nursing 18(2):203–10. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2016. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. [Google Scholar]
- Centers for Disease Control and Prevention. 2019. “National Program of Cancer Registries (NPCR).” Retrieved October 25, 2019 (https://www.cdc.gov/cancer/npcr/index.htm).
- Centers for Disease Control and Prevention and U.S. Department of Health & Human Services. 2018. “Health-Related Quality of Life (HRQOL).” Retrieved December 18, 2018 (https://www.cdc.gov/hrqol/index.htm).
- Charlton Mary, Schlichting Jennifer, Chioreso Catherine, Ward Marcia, and Vikas Praveen. 2015. “Challenges of Rural Cancer Care in the United States.” Oncology 29(9):633–40. [PubMed] [Google Scholar]
- Chen Jenny T., Kempton Steven J., and Rao Venkat K. 2016. “The Economics of Skin Cancer: An Analysis of Medicare Payment Data.” Plastic and Reconstructive Surgery – Global Open 4(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng KKF, Darshini Devi Rajasegeran, Wong WH, and Koh C 2014. “Perceived Symptoms and the Supportive Care Needs of Breast Cancer Survivors Six Months to Five Years Post-Treatment Period.” European Journal of Oncology Nursing 18(1):3–9. [DOI] [PubMed] [Google Scholar]
- Chou Ann F., Stewart Susan L., Wild Robert C., and Bloom Joan R. 2012. “Social Support and Survival in Young Women with Breast Carcinoma.” Psycho-Oncology 21(2):125–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen Sheldon and Hoberman Harry M. 1983. “Positive Events and Social Supports as Buffers of Life Change Stress1.” Journal of Applied Social Psychology 13(2):99–125. [Google Scholar]
- Cohen Sheldon and McKay Garth. 1984. “Social Support, Stress and the Buffering Hypothesis: A Theoretical Analysis.” Handbook of Psychology and Health 4:253–67. [Google Scholar]
- Cohen Sheldon and Wills Thomas A. 1985. “Stress, Social Support, and the Buffering Hypothesis.” Psychological Bulletin 98(2):310. [PubMed] [Google Scholar]
- Cooley Mary E. and Moriarty Helene J. 1997. “An Analysis of Empirical Studies Examining the Impact of the Cancer Diagnosis and Treatment of an Adult on Family Functioning.” Journal of Family Nursing 3(4):318–47. [Google Scholar]
- Cornwell Benjamin and Laumann Edward O. 2015. “The Health Benefits of Network Growth: New Evidence from a National Survey of Older Adults.” Social Science and Medicine 125:94–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cromartie John. 2017. Rural America at a Glance, 2017 Edition. United States Department of Agriculture Economic Research Service; Washington D.C. [Google Scholar]
- Douglass LG 1997. “Reciprocal Support in the Context of Cancer: Perspectives of the Patient and Spouse.” Oncology Nursing Forum 24(9):1529–1536. [PubMed] [Google Scholar]
- Ell Kathleen, Xie Bin, Wells Anjanette, Frances Nedjat-Haiem Pey Jiuan Lee, and Vourlekis Betsy. 2008. “Economic Stress among Low-Income Women with Cancer: Effects on Quality of Life.” Cancer 112(3):616–25. [DOI] [PubMed] [Google Scholar]
- Fenn Kathleen M., Evans Suzanne B., Ruth McCorkle Michael P. DiGiovanna, Pusztai Lajos, Sanft Tara, Hofstatter Erin W., Killelea Brigid K., Knobf M. Tish, Lannin Donald R., Abu-Khalaf Maysa, Horowitz Nina R., and Chagpar Anees B. 2014. “Impact of Financial Burden of Cancer on Survivors’ Quality of Life.” Journal of Oncology Practice 10(5):332–38. [DOI] [PubMed] [Google Scholar]
- Fletcher Barbara Swore, Miaskowski Christine, Given Barbara, and Schumacher Karen. 2012. “The Cancer Family Caregiving Experience: An Updated and Expanded Conceptual Model.” European Journal of Oncology Nursing 16(4):387–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank Christine, Davis Christopher G., and Elgar Frank J. 2014. “Financial Strain, Social Capital, and Perceived Health during Economic Recession: A Longitudinal Survey in Rural Canada.” Anxiety, Stress, & Coping 27(4):422–38. [DOI] [PubMed] [Google Scholar]
- Frazier Patricia A., Tix Andrew P., and Barron Kenneth E. 2004. “Testing Moderator and Mediator Effects in Counseling Psychology Research.” Journal of Counseling Psychology 51(1):115. [Google Scholar]
- Gaugler Joseph E., Hanna Nader, Linder Jeanette, Given Charles W., Tolbert Valerie, Kataria Ritesh, and Regine William F. 2005. “Cancer Caregiving and Subjective Stress: A Multi-Site, Multi-Dimensional Analysis.” Psycho-Oncology 14(9):771–85. [DOI] [PubMed] [Google Scholar]
- Ghazarian Armen A., Martin Damali N., and Lam Tram K. 2018. “Opportunities and Challenges in Rural Cancer Research: An Epidemiologic Perspective.” Cancer Epidemiology Biomarkers & Prevention 27(11):1245 LP–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldzweig G, Merims S, Ganon R, Peretz T, Altman A, and Baider L 2013. “Informal Caregiving to Older Cancer Patients: Preliminary Research Outcomes and Implications.” Annals of Oncology 24(10):2635–40. [DOI] [PubMed] [Google Scholar]
- Goldzweig G, Rottenberg Yakir, Peretz Tamar, and Baider Lea. 2015. “Silent Partners to Cancer Patients: Formal Caregivers and Oncologists.” Journal of Cancer Education 30(4):704–10. [DOI] [PubMed] [Google Scholar]
- Graham John W., Olchowski Allison E., and Gilreath Tamika D. 2007. “How Many Imputations Are Really Needed? Some Practical Clarifications of Multiple Imputation Theory.” Prevention Science 8(3):206–13. [DOI] [PubMed] [Google Scholar]
- Haines Valerie A., Beggs John J., and Hurlbert Jeanne S. 2011. “Neighborhood Disadvantage, Network Social Capital, and Depressive Symptoms.” Journal of Health and Social Behavior 52(1):58–73. [DOI] [PubMed] [Google Scholar]
- Hann Danette, Baker Frank, Denniston Maxine, Gesme Dean, Reding Douglas, Flynn Tom, Kennedy John, and Kieltyka R. Ly. 2002. “The Influence of Social Support on Depressive Symptoms in Cancer Patients: Age and Gender Differences.” Journal of Psychosomatic Research 52(5):279–83. [DOI] [PubMed] [Google Scholar]
- Harrop J. Phil, Dean Julie A., and Paskett Electra D. 2011. “Cancer Survivorship Research: A Review of the Literature and Summary of Current NCI-Designated Cancer Center Projects.” Cancer Epidemiology Biomarkers and Prevention 20(10):2042–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastert Theresa A., Kyko Jaclyn M., Reed Amanda R., Harper Felicity W. K., Beebe-Dimmer Jennifer L., Baird Tara E., and Schwartz Ann G. 2019. “Financial Hardship and Quality of Life among African American and White Cancer Survivors: The Role of Limiting Care Due to Cost.” Cancer Epidemiology Biomarkers & Prevention doi: 10.1158/1055-9965.EPI-18-1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynie Dana L., Whichard Corey, Kreager Derek A., Schaefer David R., and Wakefield Sara. 2018. “Social Networks and Health in a Prison Unit.” Journal of Health and Social Behavior 59(3):318–34. [DOI] [PubMed] [Google Scholar]
- Housing Assistance Council. 2012. Race & Ethnicity in Rural America. Washington D.C. [Google Scholar]
- Huang Chiung-Yu and Hsu Mei-Chi. 2013. “Social Support as a Moderator between Depressive Symptoms and Quality of Life Outcomes of Breast Cancer Survivors.” European Journal of Oncology Nursing 17(6):767–74. [DOI] [PubMed] [Google Scholar]
- Jacobs Marianne T., Broese van Groenou Marjolein I., Aartsen Marja J., and Deeg Dorly J. H. 2016. “Diversity in Older Adults’ Care Networks: The Added Value of Individual Beliefs and Social Network Proximity.” The Journals of Gerontology: Series B 73(2):326–36. [DOI] [PubMed] [Google Scholar]
- Kale Hrishikesh P. and Carroll Norman V. 2016. “Self-Reported Financial Burden of Cancer Care and Its Effect on Physical and Mental Health-Related Quality of Life among US Cancer Survivors.” Cancer 122(8):1283–89. [DOI] [PubMed] [Google Scholar]
- Kawachi Ichiro and Berkman Lisa F. 2001. “Social Ties and Mental Health.” Journal of Urban Health 78(3):458–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi Ichiro, Venkata Subramanian Sankaran, and Kim Daniel. 2008. “Social Capital and Health” Pp. 1–26 in Social capital and health. Springer. [Google Scholar]
- Kayser Karen, Watson Lisa E., and Andrade Joel T. 2007. “Cancer as a” We-Disease”: Examining the Process of Coping from a Relational Perspective.” Families, Systems, & Health 25(4):404. [Google Scholar]
- Keating Norah, Otfinowski Pamela, Wenger Clare, Fast Janet, And Derksen Linda. 2003. “Understanding the Caring Capacity of Informal Networks of Frail Seniors: A Case for Care Networks.” Ageing and Society 23(1):115–27. [Google Scholar]
- Kent Erin E., Rowland Julia H., Northouse Laurel, Litzelman Kristin, Chou Wen Ying Sylvia, Shelburne Nonniekaye, Timura Catherine, O’Mara Ann, and Huss Karen. 2016. “Caring for Caregivers and Patients: Research and Clinical Priorities for Informal Cancer Caregiving.” Cancer 122(13):1987–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser Janice K. and Newton Tamara L. 2001. “Marriage and Health: His and Hers.” Psychological Bulletin 127(4):472. [DOI] [PubMed] [Google Scholar]
- Kim Youngmee, Carver Charles S., Shaffer Kelly M., Gansler Ted, and Cannady Rachel S. 2015. “Cancer Caregiving Predicts Physical Impairments: Roles of Earlier Caregiving Stress and Being a Spousal Caregiver.” Cancer 121(2):302–10. [DOI] [PubMed] [Google Scholar]
- Kim Youngmee, Kashy Deborah A., Wellisch David K., Spillers Rachel L., Kwei Kaw Chiew, and Smith Tenbroeck G. 2008. “Quality of Life of Couples Dealing with Cancer: Dyadic and Individual Adjustment among Breast and Prostate Cancer Survivors and Their Spousal Caregivers.” Annals of Behavioral Medicine 35(2):230. [DOI] [PubMed] [Google Scholar]
- Kirby Sue, Barlow Veronica, Saurman Emily, Lyle David, Passey Megan, and Currow David. 2016. “Are Rural and Remote Patients, Families and Caregivers Needs in Life‐limiting Illness Different from Those of Urban Dwellers? A Narrative Synthesis of the Evidence.” Australian Journal of Rural Health 24(5):289–99. [DOI] [PubMed] [Google Scholar]
- Klijs Bart, Mendes de Leon Carlos F., Kibele Eva U. B., and Smidt Nynke. 2017. “Do Social Relations Buffer the Effect of Neighborhood Deprivation on Health-Related Quality of Life? Results from the LifeLines Cohort Study.” Health & Place 44:43–51. [DOI] [PubMed] [Google Scholar]
- Kossakowski Jolanda J., Epskamp Sacha, Kieffer Jacobien M., van Borkulo Claudia D., Rhemtulla Mijke, and Borsboom Denny. 2016. “The Application of a Network Approach to Health-Related Quality of Life (HRQoL): Introducing a New Method for Assessing HRQoL in Healthy Adults and Cancer Patients.” Quality of Life Research 25(4):781–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke Candyce H. 2018. “A Conceptual Model of Social Networks and Mechanisms of Cancer Mortality, and Potential Strategies to Improve Survival.” Translational Behavioral Medicine 8(4):629–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke Candyce H., Kubzansky Laura D., Schernhammer Eva S., Holmes Michelle D., and Kawachi Ichiro. 2006. “Social Networks, Social Support, and Survival after Breast Cancer Diagnosis.” Journal of Clinical Oncology 24(7):1105–11. [DOI] [PubMed] [Google Scholar]
- Kroenke Candyce H., Kwan Marilyn L., Neugut Alfred I., Ergas Isaac J., Wright Jaime D., Caan Bette J., Hershman Dawn, and Kushi Lawrence H. 2013. “Social Networks, Social Support Mechanisms, and Quality of Life after Breast Cancer Diagnosis.” Breast Cancer Research and Treatment 139(2):515–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke Candyce H., Michael Yvonne, Tindle Hilary, Gage Elizabeth, Chlebowski Rowan, Garcia Lorena, Messina Catherine, Manson Joann E., and Caan Bette J. 2012. “Social Networks, Social Support and Burden in Relationships, and Mortality after Breast Cancer Diagnosis.” Breast Cancer Research and Treatment 133(1):375–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach Corinne R., Troeschel Alyssa N., Wiatrek Dawn, Stanton Annette L., Diefenbach Michael, Stein Kevin D., Sharpe Katherine, and Portier Kenneth. 2017. “Preparedness and Cancer-Related Symptom Management among Cancer Survivors in the First Year Post-Treatment.” Annals of Behavioral Medicine 51(4):587–98. [DOI] [PubMed] [Google Scholar]
- Li QP, Mak YW, and Loke AY 2013. “Spouses’ Experience of Caregiving for Cancer Patients: A Literature Review.” International Nursing Review 60(2):178–87. [DOI] [PubMed] [Google Scholar]
- Li Qiuping and Loke Alice Yuen. 2013. “A Spectrum of Hidden Morbidities among Spousal Caregivers for Patients with Cancer, and Differences between the Genders: A Review of the Literature.” European Journal of Oncology Nursing 17(5):578–87. [DOI] [PubMed] [Google Scholar]
- Lim Jung-won and Zebrack Brad. 2006. “Social Networks and Quality of Life for Long-Term Survivors of Leukemia and Lymphoma.” Supportive Care in Cancer 14(2):185–92. [DOI] [PubMed] [Google Scholar]
- Linden Wolfgang, Vodermaier Andrea, MacKenzie Regina, and Greig Duncan. 2012. “Anxiety and Depression after Cancer Diagnosis: Prevalence Rates by Cancer Type, Gender, and Age.” Journal of Affective Disorders 141(2–3):343–51. [DOI] [PubMed] [Google Scholar]
- Litwin Howard and Auslander Gail K. 1990. “Evaluating Informal Support.” Evaluation Review 14(1):42–56. [Google Scholar]
- Litzelman Kristin and Yabroff K. Robin. 2015. “How Are Spousal Depressed Mood, Distress, and Quality of Life Associated with Risk of Depressed Mood in Cancer Survivors? Longitudinal Findings from a National Sample.” Cancer Epidemiology and Prevention Biomarkers 24(6):969–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguire R, Hanly P, Hyland P, and Sharp L 2018. “Understanding Burden in Caregivers of Colorectal Cancer Survivors: What Role Do Patient and Caregiver Factors Play?” European Journal of Cancer Care 27(1):e12527. [DOI] [PubMed] [Google Scholar]
- Marsden Peter V. 2003. “Interviewer Effects in Measuring Network Size Using a Single Name Generator.” Social Networks 25(1):1–16. [Google Scholar]
- Martire Lynn M., Lustig Amy P., Schulz Richard, Miller Gregory E., and Helgeson Vicki S. 2004. “Is It Beneficial to Involve a Family Member? A Meta-Analysis of Psychosocial Interventions for Chronic Illness.” Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association 23(6):599–611. [DOI] [PubMed] [Google Scholar]
- McDougall Jean A., Banegas Matthew P., Wiggins Charles L., Chiu Vi K., Rajput Ashwani, and Kinney Anita Y. 2018. “Rural Disparities in Treatment-Related Financial Hardship and Adherence to Surveillance Colonoscopy in Diverse Colorectal Cancer Survivors.” Cancer Epidemiology Biomarkers & Prevention 27(11): 1275–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehnert A, Hartung TJ, Friedrich M, Vehling S, Brähler E, Härter M, Keller M, Schulz H, Wegscheider K, Weis J, Koch U, and Faller H 2018. “One in Two Cancer Patients Is Significantly Distressed: Prevalence and Indicators of Distress.” Psycho-Oncology 27(1):75–82. [DOI] [PubMed] [Google Scholar]
- Meilleur Ashley, Subramanian SV, Plascak Jesse J., Fisher James L., Paskett Electra D, and Lamont Elizabeth B. 2013. “Rural Residence and Cancer Outcomes in the United States: Issues and Challenges.” Cancer Epidemiology Biomarkers & Prevention 22(10):1657–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meneses K, Azuero A, Hassey L, McNees P, and Pisu M 2012. “Does Economic Burden Influence Quality of Life in Breast Cancer Survivors?” Gynecol Oncol 124(3):437–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael Yvonne L., Berkman Lisa F., Colditz Graham A., Holmes Michelle D., and Kawachi Ichiro. 2002. “Social Networks and Health-Related Quality of Life in Breast Cancer Survivors: A Prospective Study.” Journal of Psychosomatic Research 52(5):285–93. [DOI] [PubMed] [Google Scholar]
- Miller Kimberly D., Siegel Rebecca L., Chun Chieh Lin Angela B. Mariotto, Kramer Joan L., Rowland Julia H., Stein Kevin D., Alteri Rick, and Jemal Ahmedin. 2016. “Cancer Treatment and Survivorship Statistics, 2016.” CA: A Cancer Journal for Clinicians 66(4):271–89. [DOI] [PubMed] [Google Scholar]
- Molina Yamilé. 2018. “A Conceptual Model of Social Networks and Mechanisms of Cancer Mortality, and Potential Strategies to Improve Survival: An Invited Commentary.” Translational Behavioral Medicine 8(4):643–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina Yamilé, Scherman Ashley, Tara Hayes Constant Bridgette Hempstead, Jacci Thompson-Dodd Shayla Richardson, Shauna Rae Weatherby Kerryn W. Reding, and Ceballos Rachel M. 2016. “Medical Advocacy among African-American Women Diagnosed with Breast Cancer: From Recipient to Resource.” Supportive Care in Cancer 24(7):3077–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moor De, Janet S, Mariotto Angela B., Parry Carla, Alfano Catherine M., Padgett Lynne, Kent Erin E., Forsythe Laura, Scoppa Steve, Hachey Mark, and Rowland Julia H. 2013. “Cancer Survivors in the United States: Prevalence across the Survivorship Trajectory and Implications for Care.” Cancer Epidemiology Biomarkers and Prevention 22(4):561–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia Nina, Schmidt Laura, Bond Jason, Jacobs Laurie, and Korcha Rachael. 2008. “Stress, Social Support and Problem Drinking among Women in Poverty.” Addiction 103(8):1283–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers Jane E. and Gill Carman S. 2004. “Poor, Rural and Female: Under-Studied, Under-Counseled, More At Risk.” Journal of Mental Health Counseling 26:225–42. [Google Scholar]
- National Cancer Institute. 2018. “Cancer Stat Facts: Cancer of Any Site.” Surveillance, Epidemiology, and End Results Program. Retrieved January 19, 2018 (https://seer.cancer.gov/statfacts/html/all.html). [Google Scholar]
- Northouse Laurel L., Katapodi Maria C., Schafenacker Ann M., and Weiss Denise. 2012. “The Impact of Caregiving on the Psychological Well-Being of Family Caregivers and Cancer Patients.” Seminars in Oncology Nursing 28(4):236–45. [DOI] [PubMed] [Google Scholar]
- Onega Tracy, Duell Eric J., Shi Xun, Wang Dongmei, Demidenko Eugene, and Goodman David. 2008. “Geographic Access to Cancer Care in the U.S.” Cancer 112(4):909–18. [DOI] [PubMed] [Google Scholar]
- Palmer Nynikka R. A., Geiger Ann M., Lingyi Lu, Douglas Case L, and Weaver Kathryn E. 2013. “Impact of Rural Residence on Forgoing Healthcare after Cancer Because of Cost.” Cancer Epidemiology Biomarkers and Prevention 22(10):1668–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paskett Electra D. 2015. “Breast Cancer Among Special Populations: Disparities in Care Across the Cancer Control Continuum BT - Improving Outcomes for Breast Cancer Survivors: Perspectives on Research Challenges and Opportunities.” Pp. 39–52 in, edited by Ganz PA Cham: Springer International Publishing. [DOI] [PubMed] [Google Scholar]
- Payne Nicolette, Palmer Kelly Elizabeth, and Pawlik Timothy M. 2019. “Assessing Structure and Characteristics of Social Networks among Cancer Survivors: Impact on General Health.” Supportive Care in Cancer. 27(8):3045–3051. [DOI] [PubMed] [Google Scholar]
- Peacock Marian, Bissell Paul, and Owen Jenny. 2013. “Shaming Encounters: Reflections on Contemporary Understandings of Social Inequality and Health.” Sociology 48(2):387–402. [Google Scholar]
- Perry Brea L. and Pescosolido Bernice A. 2015. “Social Network Activation: The Role of Health Discussion Partners in Recovery from Mental Illness.” Social Science & Medicine 125:116–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisu Maria, Azuero Andres, Benz Rachel, McNees Patrick, and Meneses Karen. 2017. “Out-of-Pocket Costs and Burden among Rural Breast Cancer Survivors.” Cancer Medicine 6(3):572–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portenoy Russell K., Thaler Howard T., Kornblith Alice B., Lepore J. McCarthy, Friedlander-Klar H, Kiyasu E, Sobel K, Coyle N, Kemeny N, and Norton L 1994. “The Memorial Symptom Assessment Scale: An Instrument for the Evaluation of Symptom Prevalence, Characteristics and Distress.” European Journal of Cancer 30(9):1326–36. [DOI] [PubMed] [Google Scholar]
- Rank Mark R. and Hirschl Thomas A. 1988. “A Rural-Urban Comparison of Welfare Exits: The Importance of Population Density.” Rural Sociology 53(2):190. [Google Scholar]
- Reid-Arndt Stephanie A. and Cox Cathy R. 2010. “Does Rurality Affect Quality of Life Following Treatment for Breast Cancer?” Journal of Rural Health 26(4):402–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rha Sun Young, Park Yeonhee, Su Kyung Song Chung Eun Lee, and Lee Jiyeon. 2015. “Caregiving Burden and the Quality of Life of Family Caregivers of Cancer Patients: The Relationship and Correlates.” European Journal of Oncology Nursing 19(4):376–82. [DOI] [PubMed] [Google Scholar]
- Rocco Lorenzo and Suhrcke Marc. 2012. Is Social Capital Good for Health?: A European Perspective. WHO Regional Office for Europe; Copenhagen, Denmark. [Google Scholar]
- Rogers Howard W. and Coldiron Brett M. 2009. “A Relative Value Unit-Based Cost Comparison of Treatment Modalities for Nonmelanoma Skin Cancer: Effect of the Loss of the Mohs Multiple Surgery Reduction Exemption.” Journal of the American Academy of Dermatology 61(1):96–103. [DOI] [PubMed] [Google Scholar]
- Sapp Amy L., Amy Trentham-Dietz Polly A. Newcomb, Hampton John M., Moinpour Carol M., and Remington Patrick L. 2003. “Social Networks and Quality of Life among Female Long-Term Colorectal Cancer Survivors.” Cancer 98(8):1749–58. [DOI] [PubMed] [Google Scholar]
- Schafer Markus H. and Koltai Jonathan. 2015. “Cancer Diagnosis and Mental Health among Older White Adults: Moderating Role for Social Networks?” Society and Mental Health 5(3):182–202. [Google Scholar]
- Schneider John A., Cornwell Benjamin, Ostrow David, Michaels Stuart, Schumm Phil, Laumann Edward O., and Friedman Samuel. 2013. “Network Mixing and Network Influences Most Linked to HIV Infection and Risk Behavior in the HIV Epidemic among Black Men Who Have Sex with Men.” American Journal of Public Health 103(1):e28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sklenarova Halina, Arne Krümpelmann Markus W. Haun, Hans Christoph Friederich Johannes Huber, Thomas Michael, Winkler Eva C., Herzog Wolfgang, and Hartmann Mechthild. 2015. “When Do We Need to Care about the Caregiver? Supportive Care Needs, Anxiety, and Depression among Informal Caregivers of Patients with Cancer and Cancer Survivors.” Cancer 121(9):1513–19. [DOI] [PubMed] [Google Scholar]
- Smith Jeffrey A., Moody James, and Morgan Jonathan. 2017. “Network Sampling Coverage II: The Effect of Non-Random Missing Data on Network Measurement.” Social Networks 48:78–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Kirsten P. and Christakis Nicholas A. 2008. “Social Networks and Health.” Annu. Rev. Sociol 34:405–29. [Google Scholar]
- Smith Kristin E. 2011. “Changing Roles: Women and Work in Rural America” Pp. 60–81 in Economic Restructuring and Family Well-Being in Rural America, edited by Smith KE and Tickamyer AR University Park: The Pennsylvania State University Press. [Google Scholar]
- Smith Kristin E. and Tickamyer Ann R. 2011. Economic Restructuring and Family Well-Being in Rural America. University Park: The Pennsylvania State University Press. [Google Scholar]
- Sterba KR, Zapka J, LaPelle N, Garris TK, Buchanan A, Scallion M, and Day T 2017. “Development of a Survivorship Needs Assessment Planning Tool for Head and Neck Cancer Survivors and Their Caregivers: A Preliminary Study.” Journal of Cancer Survivorship 11(6):822–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterba Katherine Regan, Burris Jessica L., Heiney Sue P., Megan Baker Ruppel Marvella E. Ford, and Zapka Jane. 2014. “‘We Both Just Trusted and Leaned on the Lord’: A Qualitative Study of Religiousness and Spirituality among African American Breast Cancer Survivors and Their Caregivers.” Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation 23(7):1909–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straits Bruce C. 2000. “Ego’s Important Discussants or Significant People: An Experiment in Varying the Wording of Personal Network Name Generators.” Social Networks 22(2):123–40. [Google Scholar]
- Sweet Elizabeth. 2018. “‘Like You Failed at Life’: Debt, Health and Neoliberal Subjectivity.” Social Science & Medicine 212:86–93. [DOI] [PubMed] [Google Scholar]
- Syed Samina T., Gerber Ben S., and Sharp Lisa K. 2013. “Traveling towards Disease: Transportation Barriers to Health Care Access.” Journal of Community Health 38(5):976–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tajvar Maryam, Grundy Emily, and Fletcher Astrid. 2018. “Social Support and Mental Health Status of Older People: A Population-Based Study in Iran-Tehran.” Aging & Mental Health 22(3):344–53. [DOI] [PubMed] [Google Scholar]
- Uchino Bert N. 2006. “Social Support and Health: A Review of Physiological Processes Potentially Underlying Links to Disease Outcomes.” Journal of Behavioral Medicine 29(4):377–87. [DOI] [PubMed] [Google Scholar]
- United States Department of Agriculture. 2016. “Rural-Urban Commuting Area Codes.” Retrieved November 18, 2018 (https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/).
- Vellone Ercole, Chung Misook L., Cocchieri Antonello, Rocco Gennaro, Alvaro Rosaria, and Riegel Barbara. 2014. “Effects of Self-Care on Quality of Life in Adults with Heart Failure and Their Spousal Caregivers: Testing Dyadic Dynamics Using the Actor–Partner Interdependence Model.” Journal of Family Nursing 20(1):120–41. [DOI] [PubMed] [Google Scholar]
- Hippel Von, Paul T 2009. “8. How to Impute Interactions, Squares, and Other Transformed Variables.” Sociological Methodology 39(1):265–91. [Google Scholar]
- Wagner Christina D., Tanmoy Das Lala, Bigatti Silvia M., and Storniolo Anna Maria. 2011. “Characterizing Burden, Caregiving Benefits, and Psychological Distress of Husbands of Breast Cancer Patients During Treatment and Beyond.” Cancer Nursing 34(4). [DOI] [PubMed] [Google Scholar]
- Ware John E., Kosinski Mark, And Keller Susan D. 1996. “A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity.” Medical Care 34(3). [DOI] [PubMed] [Google Scholar]
- Wareham Stacey, Fowler Ken, and Pike Andrea. 2007. “Determinants of Depression Severity and Duration in Canadian Adults: The Moderating Effects of Gender and Social Support.” Journal of Applied Social Psychology 37(12):2951–79. [Google Scholar]
- Weaver Kathryn E., Palmer N, Lu L, Case D, and Geiger AM 2013a. “Rural-Urban Differences in Health Behaviors and Implications for Health Status among US Cancer Survivors.” Cancer Causes Control 24(8):1481–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver Kathryn E., Geiger Ann M., Lu Lingyi, and Douglas Case L 2013b. “Rural-Urban Disparities in Health Status among US Cancer Survivors.” Cancer 119(5):1050–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver Raven H., Roberto Karen A., and Blieszner Rosemary. 2017. “Older Adults in Rural Appalachia: Preference and Expectations for Future Care.” The International Journal of Aging and Human Development 86(4):364–81. [DOI] [PubMed] [Google Scholar]
- White Ian R., Royston Patrick, and Wood Angela M. 2011. “Multiple Imputation Using Chained Equations: Issues and Guidance for Practice.” Statistics in Medicine 30(4):377–99. [DOI] [PubMed] [Google Scholar]
- Wishner Jane and Solleveld Patricia. 2016. A Look at Rural Hospital Closures and Implications for Access to Care: Three Case Studies. Kaiser Family Foundation. [Google Scholar]
- Yabroff K. Robin, Dowling Emily, Rodriguez Juan, Ekwueme Donatus U., Meissner Helen, Soni Anita, Lerro Catherine, Willis Gordon, Forsythe Laura P., and Borowski Laurel. 2012. “The Medical Expenditure Panel Survey (MEPS) Experiences with Cancer Survivorship Supplement.” Journal of Cancer Survivorship 6(4):407–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yabroff K. Robin and Kim Youngmee. 2009. “Time Costs Associated with Informal Caregiving for Cancer Survivors.” Cancer 115(S18):4362–73. [DOI] [PubMed] [Google Scholar]
- Yancey Antronette K., Ortega Alexander N., and Kumanyika Shiriki K. 2006. “Effective Recruitment And Retention Of Minority Research Participants.” Annual Review of Public Health 27(1):1–28. [DOI] [PubMed] [Google Scholar]
- Zahnd Whitney E., Davis Melinda M., Rotter Jason S., Vanderpool Robin C., Perry Cynthia K., Shannon Jackilen, Ko Linda K., Wheeler Stephanie B., Odahowski Cassie L., and Farris Paige E. 2019. “Rural-Urban Differences in Financial Burden among Cancer Survivors: An Analysis of a Nationally Representative Survey.” Supportive Care in Cancer 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.