Abstract
Background: Access to specialized medical care is often limited in rural emergency departments (EDs). Specialist consultation through telemedicine services could help increase access in low-resource areas.
Introduction: The objective of this study was to better understand providers' perceptions of the anticipated impact of telemedicine in rural Midwestern EDs. The secondary objective was to understand differences in the perception of rural and academic providers in their views of the utility of telemedicine.
Materials and Methods: We conducted a survey of medical providers including physicians, physician assistants, and nurse practitioners at five rural Midwestern critical access hospitals and within six departments at a university medical center in the same region. The survey addressed opinions on telemedicine, including how often it would be used and the potential to improve patient care and reduce transfers.
Results: Specialties of high perceived utility to rural providers include psychiatry, cardiology, and neurology; whereas academic providers viewed services in psychiatry, pediatric critical care, and neurology to be of the most potential value. Academic and rural providers have differing opinions on the anticipated frequency of telemedicine use (p < 0.001) and prevention of inter-hospital transfers (p = 0.023). There were significant differences in perceived value by specialty.
Conclusion: There is a high demand for telemedicine consultation services in rural Midwestern hospitals, particularly in psychiatry, cardiology, and neurology. Overall, academic providers view telemedicine services as more valuable within their specialty than do rural providers. Further research should be done to investigate individualization of telehealth services based on regional needs and how disparate opinions predict telemedicine utilization.
Keywords: telemedicine, emergency service, hospital, hospitals, rural, rural health services
Introduction
Rural Americans comprise ∼20% of the U. S. population, often live in sparsely populated areas, and face a multitude of health care disparities.1 Residents of rural areas tend to face more comorbidities than their urban and suburban counterparts due to a variety of socioeconomic and geographic factors, with high levels of chronic disease burden and higher mortality.2,3 Lack of access to local medical providers and facilities is cited as one of the core reasons leading to health care underutilization and poor health outcomes in this population.4,5 Subspecialty medical care is becoming increasingly sparse within rural communities, resulting in a lack of available consultants for rural providers and discontinuity of care for patients with specialized medical needs.6,7
One proposed solution to help minimize these gaps in rural health care access is through telemedicine services, which involves the use of audio/visual technologies to allow providers to engage in video consultations, exchange images, and monitor patients from a remote location.8,9 Implementation of telemedicine services helps facilitate communication between providers and can allow for more access to general and subspecialized care for rural patients.10 The use of telemedicine has been established in many specialties and has shown benefit in areas such as emergency medicine, psychiatry, neurology, intensive care medicine, and pediatrics.8,11–15 The benefits of telemedicine use within these specialties include decreased mortality, decreased hospital length of stay, higher adherence to recommended care, cost-effectiveness, and high patient and provider satisfaction.15–20
One area in which telemedicine services could enhance care is within rural emergency departments (EDs). In many low-population-density states, such as those in the Midwest, patients may live hours away from the nearest tertiary medical center and associated specialty services. With a wide variety of presenting illness, frequently understaffed EDs, finite resources, and limited access to specialty consultations, telemedicine has been proposed to aid in delivering more advanced medical care to these areas.21,22 Reports have shown that EDs utilizing telemedicine services are often able to reduce patient transfers and associated costs while expediting necessary ones, allow for more frequent local treatment of specialized conditions, and provide high-quality care.8,21,23–26
In 2016, 48% of EDs in the United States received telemedicine services in some capacity,27 with one report demonstrating that telemedicine consultation is requested for ∼3.5% of ED visits within telemedicine-capable hospitals. Two recent studies described that telemedicine consults are most frequently requested for cardiovascular and cerebrovascular disease, mental health illness, trauma-related illness, and pediatrics, but consultation is only applied in a minority of ED encounters in telemedicine-capable facilities, usually within the context of a pilot study.27–29 Despite numerous reported benefits and apparent perceived utility, significant barriers to use exist.
The objective of our study is to better understand the role of telehealth in a rural state by determining which specialty consult services would be of the most perceived benefit to rural ED providers. A secondary aim of this study seeks to determine how opinions regarding the utility of telemedicine compare between academic and rural providers, as telemedicine services are largely developed by tertiary practices.
Materials and Methods
Study Design and Setting
This study was a cross-sectional survey of health care providers at critical access hospitals and an academic medical center in a single, rural Midwestern state between January and October 2018. Sites were selected that were within 200 miles of the regional academic medical center. The study was determined not to be human subjects' research by the local institutional review board, and the study is reported according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement for cross-sectional studies.30
Participants
Health care providers, including physicians, advanced practice providers (APPs; i.e., physician assistants and nurse practitioners), and podiatrists at six critical access hospitals, were eligible to participate. Participants were categorized into three groups for survey purposes: physicians (MD/DO), APPs physician assistant/advanced registered nurse practitioner (PA/ARNP), and Other (includes those who did not indicate their clinical role). Providers were recruited from all specialties at critical access hospitals. Participants were identified at critical access hospitals by contacting the medical staff coordinator at each location to arrange survey distribution at staff meetings. In two instances, in-person survey distribution could not be accommodated, and surveys were sent to the medical staff coordinator by e-mail who then distributed the survey in person to interested participants. Surveys were then returned by e-mail. Faculty and resident physicians at the academic medical center were eligible to participate. Participants at the academic medical center were identified by contacting a faculty member within the department to coordinate in-person survey distribution. In two instances, in-person distribution could not be accommodated, and surveys were distributed and returned by e-mail.
Data Collected
Participants completed an anonymous, deidentified paper survey, administered and collected by a trained research assistant at the in-person visits. For the two critical access hospitals that could not accommodate in-person visits, surveys were sent electronically to the hospital contact and were printed on paper for providers to fill out on their own. Demographic information, including clinical role (e.g., nurse practitioner, physician) and specialty area, were self-reported by participants. All participants were asked about their perceptions of telemedicine among three domains: (1) impact on patient care, (2) frequency of telemedicine use, and (3) prevention of inter-hospital transfers. Responses were recorded by using a 10-cm visual analog scale, and data are reported in millimeters. Separate survey forms were provided to participants based on practice setting (Table 1). Providers at critical access hospitals were asked about their perceptions of telemedicine for patients presenting in a variety of specialty areas (Supplementary Table S1). Providers at the academic medical center were given a similar survey with a 10-cm visual analog scale and identical language to the rural hospital survey. However, questions on the academic survey pertained only to the specialty of the responding provider. No compensation or incentives were provided for survey completion, and participants were unaware of study hypotheses. Survey responses from the critical access hospitals and academic departments, except for neurology and psychiatry, were anonymous and protected. Within the academic departments of neurology and psychiatry, surveys were emailed from respondents directly back to the trained research assistant, and therefore were not anonymous. Surveys were printed without identifying features, measured manually, and entered into an electronic database by a trained research assistant.
Table 1.
Survey Questions with Response Categories
| SURVEY QUESTIONS | RESPONSE OPTIONS (VISUAL ANALOG SCALE) |
|---|---|
| Critical access hospital providers (for each specialty/patient type) | |
| Please indicate the degree to which the following telehealth services would improve patient care in your facility. If this is a service already offered at your facility, please indicate the degree to which you feel the service improves patient care. | Not at all likely (0 mm) ←→ Very likely (100 mm) |
| Please indicate how often you feel you would use the following telehealth services: | Never (0 mm) ←→ Always (100 mm) |
| Please indicate how many inter-hospital transfers you feel the following telehealth services would prevent: | No transfers (0 mm) ←→ All transfers (100 mm) |
| Academic medical center providers (for the provider's specialty only) | |
| Please indicate the degree to which telehealth services within your specialty would improve patient care. If this is a service already offered at your facility, please indicate the degree to which you feel the service improves patient care. | No improvement (0 mm) ←→ Complete improvement (100 mm) |
| If telehealth services within your specialty were offered at UIHC, how often do you feel you would be consulted for these services? | None of the qualifying patients (0 mm) ←→ All qualifying patients (100 mm) |
| Please indicate how many inter-hospital transfers you feel telehealth services within your specialty would prevent: | No transfers (0 mm) ←→ All transfers (100 mm) |
Data Analysis
Descriptive, univariate statistics were used to summarize the provider responses by frequency and median with interquartile range as appropriate. The Mann-Whitney U test and Kruskal-Wallis test were used to test the hypothesis that responses differed by provider type, provider specialty, and practice setting. Surveys with missing data were included in the final analysis only for questions with complete responses (i.e., missing data were excluded without imputation and complete case analysis was performed for each question). Analysis was conducted by using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Participant Characteristics
Of the 92 eligible participants approached for the study, 90 completed the survey (98% participation). Most participants were physicians (75.6%), and the most common specialty was family medicine (27.8%) with a similar number of overall participants in rural and academic settings (Table 2).
Table 2.
Participant Demographics
| N = 90 | % | COMMUNITY n = 44 | % | ACADEMIC n = 46 | % | |
|---|---|---|---|---|---|---|
| Type of provider | ||||||
| Advanced practice provider (PA or ARNP) | 19 | 21.1 | 18 | 40.9 | 1 | 2.2 |
| Physician (MD or DO) | 68 | 75.6 | 23 | 52.3 | 45 | 97.8 |
| Other or missing | 3 | 3.3 | 3 | 6.8 | 0 | 0 |
| Specialtya | ||||||
| Emergency medicine | 16 | 17.8 | 7 | 15.9 | 9 | 19.6 |
| Family medicine | 25 | 27.8 | 25 | 56.8 | 0 | 0 |
| Neurology | 10 | 11.1 | 0 | 0 | 10 | 21.7 |
| Neurosurgery | 5 | 5.6 | 0 | 0 | 5 | 10.9 |
| Orthopedics | 1 | 1.1 | 1 | 2.3 | 0 | 0 |
| Ophthalmology | 10 | 11.1 | 0 | 0 | 10 | 21.7 |
| Pediatric critical care | 9 | 10.0 | 0 | 0 | 9 | 19.6 |
| Podiatry | 1 | 1.1 | 1 | 2.3 | 0 | 0 |
| Psychiatry | 3 | 3.3 | 0 | 0 | 3 | 6.5 |
| Surgery | 1 | 1.1 | 1 | 2.3 | 0 | 0 |
| Obstetrics and gynecology | 3 | 3.3 | 3 | 6.8 | 0 | 0 |
| Hospitalist | 3 | 3.3 | 3 | 6.8 | 0 | 0 |
| None specified | 6 | 6.7 | 6 | 13.6 | 0 | 0 |
Totals more than survey sample, as some providers have greater than one specialty.
ARNP, advanced registered nurse practitioner; PA, physician assistant.
Perceptions of Telemedicine Among Critical Access Hospital Providers
Of the 44 critical access hospital provider surveys across all specialties/patient types, providers assigned an intermediate value to the impact of telemedicine on patient care (51 mm, interquartile range [IQR]: 20–76). Providers assigned a lower value to the perceived frequency of telemedicine use (28 mm, IQR: 9–57) and for the probability of preventing inter-hospital transfer (17 mm, IQR: 3–42). There were no observed differences in perception of telemedicine by the provider's specialty or the type of provider (Supplementary Tables S2 and S3) in any of the three domains.
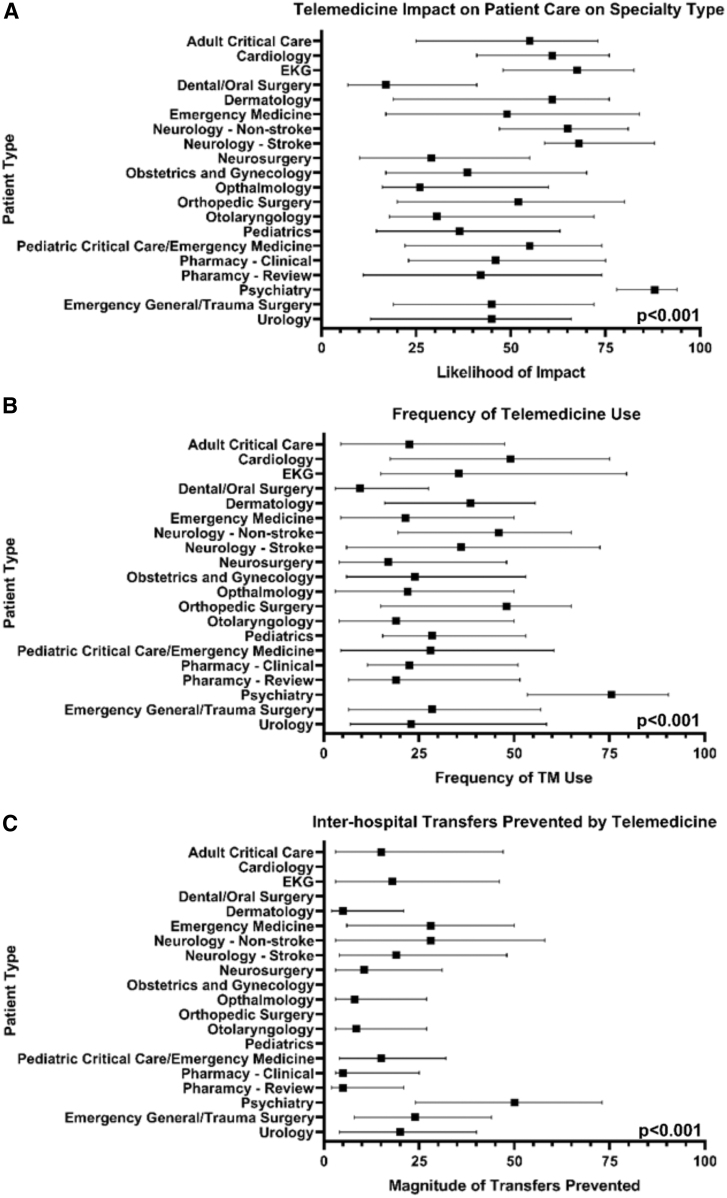
Perceptions of telemedicine varied by participant specialty (p < 0.001) for each of the three survey domains (i.e., impact on patient care, frequency of use, and prevention of inter-hospital transfer) (Fig. 1). Psychiatry patients were consistently perceived to be the most impacted by telemedicine (median 88 mm [IQR: 78–94]), to be likely to utilize telemedicine frequently (median 75 mm [IQR: 53–90]), and to prevent the most inter-hospital transfers (median 50 mm [24–73]). Neurosurgery and ophthalmology were areas where telemedicine was perceived as least likely to impact patient care. Further, neurosurgery was perceived to be the patient population with the least frequent use of telemedicine; dermatology, pharmacy (clinical support and remote review), and dentistry/oral surgery were considered patient areas with the least number of inter-facility transfers potentially preventable by telemedicine.
Fig. 1.
Critical access hospital providers' perceptions of telemedicine by specialty/patient type.
Perceptions of Telemedicine Among Academic Medical Center Providers
The academic medical center providers (n = 46) provided responses only for their own specialties. Overall, academic medical providers responded that telemedicine would have improvement on patient care (median 67 mm [IQR: 45–77]), would be used with frequency (median 59 mm [IQR: 32–76]), and would prevent a modest amount of inter-hospital transfers (median 32 mm [IQR: 18–48]).
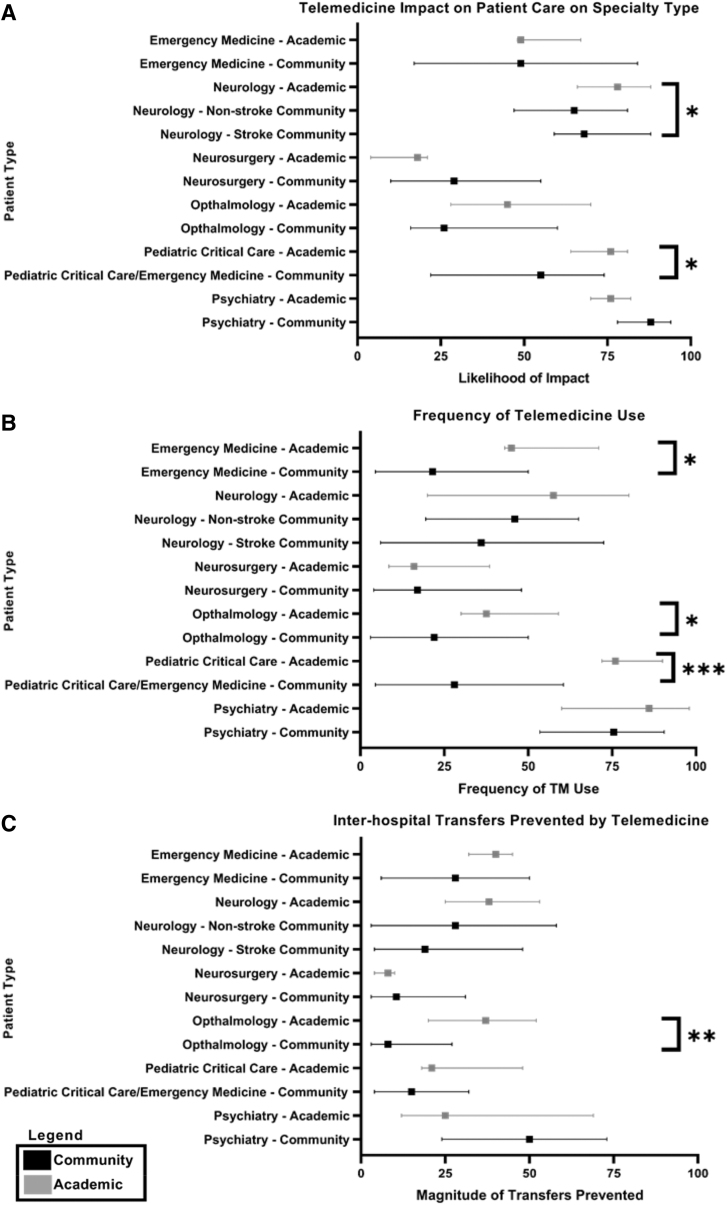
Perceptions of telemedicine varied by specialty for importance for patient care (p = 0.003) and the frequency of telemedicine use (p = 0.007) (Fig. 2). However, there were no differences by specialty on the role of telemedicine to prevent inter-hospital transfer (p = 0.102).
Fig. 2.
Comparison of academic and community providers' perceptions of telemedicine among academic medical center providers. *p < 0.05, **p < 0.01, ***p < 0.001.
Comparison of Telemedicine Perceptions Between Rural and Academic Providers
Overall, perceptions of the impact/importance of telemedicine for patient care was not different between rural and academic providers (p = 0.464) (Table 3). However, academic providers responded that they felt telemedicine would be used with more frequency than rural providers (59 vs. 32 mm, p < 0.001). Further, academic providers perceived the role of telemedicine in preventing inter-hospital transfer to be greater than rural providers perceived (32 vs. 21 mm, p = 0.023). There was also discordance in telemedicine perceptions between academic and rural providers in some specialties, especially pediatric critical care patients.
Table 3.
Comparison of Telemedicine Perceptions Between CAH Providers and Academic Medical Center Providers by Patient Type
| IMPACT ON PATIENT CARE |
FREQUENCY OF TM USE |
PREVENTED INTER-HOSPITAL TRANSFERS |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| CAH MEDIAN (IQR) | ACADEMIC MEDIAN (IQR) | p-VALUE | CAH MEDIAN (IQR) | ACADEMIC MEDIAN (IQR) | p-VALUE | CAH MEDIAN (IQR) | ACADEMIC MEDIAN (IQR) | p-VALUE | |
| Overall | 61.0 (23.0–82.0) | 67.0 (45.0–77.0) | 0.464 | 32.0 (8.0–63.0) | 59.0 (32.0–76.0) | <0.001 | 59.0 (32.0–76.0) | 32.5 (18.0–48.0) | 0.023 |
| Patient type | |||||||||
| Emergency medicine | 49.0 (17.0–84.0) | 49.0 (48.0–67.0) | 0.820 | 21.5 (4.5–50.0) | 45.0 (43.0–71.0) | 0.039 | 28.0 (6.0–50.0) | 40.0 (32.0–45.0) | 0.448 |
| Neurology (stroke and nonstroke) | 65.5 (51.0–76.0) | 78.0 (66.0–88.0) | 0.045 | 37.0 (17.0–60.3) | 57.7 (20.0–80.0) | 0.247 | 25.5 (11.0–46.0) | 38.0 (25.0–53.0) | 0.197 |
| Neurosurgery | 29.0 (10.0–55.0) | 18.0 (4.0–21.0) | 0.319 | 17.0 (4.0–48.0) | 16.0 (8.5–38.5) | 0.911 | 10.5 (3.0–31.0) | 8.0 (4.0–10.0) | 0.743 |
| Ophthalmology | 26.0 (16.0–60.0) | 45.0 (28.0–70.0) | 0.285 | 22.0 (3.0–50.0) | 37.5 (30.0–59.0) | 0.048 | 8.0 (3.0–27.0) | 37.0 (20.0–52.0) | 0.007 |
| Pediatric critical care | 55.0 (22.0–74.0) | 76.0 (64.0–81.0) | 0.041 | 28.0 (4.5–60.5) | 76.0 (72.0–90.0) | <0.001 | 15.0 (4.0–32.0) | 21.0 (18.0–48.0) | 0.090 |
| Psychiatry | 88.0 (78.0–94.0) | 76.0 (70.0–82.0) | 0.161 | 75.5 (53.5–90.5) | 86.0 (60.0–98.0) | 0.384 | 50.0 (24.0–73.0) | 25.0 (12.0–69.0) | 0.436 |
In this table, CAH overall median (IQR) contains responses only for the six specialties provided by academic providers.
CAH, critical access hospital; IQR, interquartile range; TM, telemedicine.
Discussion
Telemedicine consultation can enhance patient care across multiple specialties, and this study highlights the need for targeted telemedicine consultation services within rural facilities. Our data suggest that perceived utility for telemedicine services is high among rural physicians, which is consistent with previous literature describing the positive perceptions of telemedicine and benefits to patient care.8,11,13 However, utilization of telemedicine services is variable within U. S. EDs.27,28 Interestingly, despite abundant literature on the impact and utility of telehealth solutions in rural hospitals, this is the first report of a rural provider-focused needs assessment to predict the use and impact of emergency telehealth services.
Our data suggest that the greatest value use case for telemedicine services among rural providers is within the fields of psychiatry, cardiology, and neurology. This finding is consistent with previous studies and is likely reflective of disease prevalence, resource availability, and time sensitivity of emergency conditions within these specialties.27,29,31–33 Importantly, these data are reflective of regional need, and these trends are likely to vary by geographic location, so user-directed needs assessments are a useful tool to predict the benefit of specific consultation services at a given facility. It is not a “one size fits all” scenario.
Similar to rural providers, academic providers also report high perceived utility for telemedicine services within rural hospitals, particularly within psychiatry, neurology, and pediatric critical care. Interestingly, academic providers tend to assign higher perceived value to telemedicine services within their specialty on average than do their rural counterparts, which raises the question: Why are telemedicine services valued more highly by academic providers? Could this differential between academic and rural providers explain lower than expected telemedicine utilization among rural hospitals?
First, we will address the disparity that exists between rural and academic providers, which we will refer to as “tertiary bias”—the tendency of providers to overvalue consultation services within their specialty. This study demonstrates that academic providers believe telemedicine services would be used with more frequency and prevent fewer inter-hospital transfers than do rural providers, implying that they feel optimal care within their specialty is delivered by specialists at a large, academic medical center. Academic physicians are often specialized and may practice among experts within the field—their knowledge and experience offered could certainly benefit patients outside their network through the reach of telemedicine. However, academic providers may underestimate rural provider capability and independence, or they may overestimate the need for specialized consultation in some rural areas. Prior reports demonstrate that rural providers only use telemedicine for particularly rare or difficult cases,34 and it has been shown in previous studies that telemedicine does not always improve or expedite care among some commonly encountered illnesses.35 Therefore, academic providers may overestimate their importance and use in many rural ED cases.
Since telemedicine research and program design are heavily focused on the opinions of academic clinicians, this incongruity poses a potential issue. If design of telemedicine service bundles is heavily influenced by the academic perspective, they may be designed with excessive or redundant services that rural providers find unnecessary. Although limited data exist on long-term viability of telemedicine pilot programs, one study demonstrated that only about 25% of one pilot program cohort were sustainable in the long term and cites low demand as a main barrier to sustainability.36 Increasing demand involves developing an understanding of rural provider needs and tailoring services accordingly. Our data show that academic physicians may not inherently understand the needs of rural facilities but can better appreciate them through prepilot needs assessments. Telemedicine programs should be developed with the customer in mind to ensure that services most perceived as valuable are offered to the receiving facilities. Tertiary bias likely leads to delivery of inessential consultation services and therefore plays a role in variable telemedicine utilization. However, rural providers still have a positive perception of telemedicine despite differential opinion, so tertiary bias is unlikely to be the sole explanation for inconsistent use. So, what other factors might be involved in telemedicine utilization? Past studies have suggested that low perceived value of telemedicine services can lower utilization rates.34 Since our current data contrarily suggest a very high perceived value among rural providers, a more appropriate supposition may instead be that rural providers have low perceived use despite high perceived value. Factors affecting perceived use likely include appropriateness of the service, cost, and an understanding of system capabilities, and if these features are not optimized, facilities may decide not to purchase a service despite obvious utility.
The first element to be considered regarding perceived use is appropriateness of the service, which, as described earlier, should address the needs of each individual facility. Another element in determining feasibility of telemedicine use is cost. Small hospitals may not have the independent funding to support implementation of expensive telemedicine programs, and reimbursement varies by state.37–39 Although reimbursement rates are beginning to increase, they are still lower for telemedicine services than for in-person visits, making wide adoption of telemedicine practice difficult.40 Some payment models are beginning to incentivize telemedicine use,38 which, if widely adopted, could help increase utilization and decrease financial barriers encountered by small hospitals, but that is not yet common practice. Cost of telemedicine bundles is likely driven up by inclusion of redundant services, which is influenced by tertiary bias. Therefore, universal use of needs assessments may also help reduce cost by identifying nonessential services and decreasing expenditures in these areas. Telemedicine distributors that understand the individual needs of their customers will be able to provide services of both high perceived value and high perceived use, leading to increased utilization of telemedicine services in rural facilities.
One additional factor that may contribute to low perceived use within rural hospitals is simply an incomplete understanding of telemedicine capabilities. One data point that highlights this involves the perceived value of pediatric critical care. Academic providers assign higher perceived value to pediatric critical care services than do rural providers despite recent literature stating that community providers feel ill-equipped to deal with the majority of pediatric emergencies.41 Studies have shown pediatric emergency telemedicine to be an effective tool in assisting with triage and care, and expediting transfer to capable facilities,42,43 so it is surprising that rural providers did not assign a very high value to this service. This finding may reflect a limited understanding of the telemedicine system capabilities, and efforts should be made to provide adequate education on the potential use of each specialty service as part of the marketing agenda.
One potential limitation in this survey is that data were collected from a predominantly rural geographic region of which all participating hospitals were within a 200-mile radius, and therefore findings may not be generalizable to other populations. In addition, sample sizes for academic provider specialties were small, which could have concealed potentially significant findings within certain specialties. Although specialty specific opinions may not be generalizable, our objective was to identify general differences in rural and academic opinion, so this limitation is unlikely to influence the overarching findings of this study. In addition, although most surveys were administered in person, surveys were administered electronically at two rural hospitals and within one academic specialty, which eliminated potential for in-person questions and clarification. Since e-mail respondents made up only a small fraction of the total participants, any effect that this had on provider response would also be unlikely to affect overall conclusions. Lastly, our survey tool did not assess participant baseline understanding of telemedicine services.
Both rural and academic providers indicate a high perceived utility for telemedicine consultation services within rural hospitals despite variable utilization. On average, academic providers seem to value telemedicine services within their specialty more highly than their rural counterparts. Academic providers do not inherently understand the needs of rural facilities, and tertiary bias may lead to excessive standardization and inclusion of unnecessary services during telemedicine program design, which could indirectly drive cost and decrease perceived use among rural providers. Routine use of needs assessments before telemedicine pilot programs would shift focus to meet the needs of rural provides, which may help minimize tertiary bias, decrease cost, and possibly increase utilization among rural hospitals. Overall, increasing access to telemedicine services through user-directed needs assessments can help increase access to specialized care and reduce health care disparities among rural populations.
Supplementary Material
Acknowledgments
The authors would like to thank the following departments and institutions for their support and participation in this study: UIHC Departments of Emergency Medicine, Pediatric Critical Care, Psychiatry, Neurology, Neurosurgery, and Ophthalmology; Waverly Health Center; Winneshiek Medical Center; Virginia Gay Medical Center; Henry County Health Center; Keokuk County Health Center; and Van Buren County Hospitals and Clinics. The authors would also like to thank Brett Faine, PharmD, and Paul Van Heukelom, MD for their assistance with the development of this survey and Kelli Wallace, MS and Kari Harland, PhD, MPH for their technical assistance in preparing the article for publication.
Disclosure Statement
S.E.R.O., M.B.S., and A.A. have no competing financial interests to disclose. Dr. N.M.M. is supported by grant K08 HS025753 from the Agency for Healthcare Research and Quality (AHRQ). The findings and conclusions are those of the author(s), who are responsible for its content, and do not necessarily represent the views of the AHRQ.
Funding Information
No funding was received for this article.
Supplementary Material
References
- 1. United States Census Bureau. American Community Survey: 2011. –2015. 2016 Available at https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t (last accessed September26, 2019)
- 2. Eberhardt MS, Pamuk ER. The importance of place of residence: Examining health in rural and nonrural areas. Am J Public Health 2004;94:1682–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health 2004;94:1675–1678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Merwin E, Snyder A, Katz E. Differential access to quality rural healthcare: Professional and policy challenges. Fam Community Health 2006;29:186–194 [DOI] [PubMed] [Google Scholar]
- 5. Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res 2016;79:169–176 [DOI] [PubMed] [Google Scholar]
- 6. Sanders JL, Raja AS, Hasegawa K, et al. Decline in consultant availability in Massachusetts Emergency Departments: 2005 to 2014. Ann Emerg Med 2016;68:461–466 [DOI] [PubMed] [Google Scholar]
- 7. Levey LM, Curry JP, Levey S. Rural-urban differences in access to Iowa child health services. J Rural Health 1988;4:59–72 [DOI] [PubMed] [Google Scholar]
- 8. Mueller KJ, Potter AJ, MacKinney AC, Ward MM. Lessons from tele-emergency: Improving care quality and health outcomes by expanding support for rural care systems. Health Aff (Millwood) 2014;33:228–234 [DOI] [PubMed] [Google Scholar]
- 9. Breen G-M, Matusitz J. An evolutionary examination of telemedicine: A health and computer-mediated communication perspective. Soc Work Public Health 2010;25:59–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gagnon MP, Duplantie J, Fortin JP, Landry R. Implementing telehealth to support medical practice in rural/remote regions: What are the conditions for success? Implement Sci 2006;1:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hailey D, Ohinmaa A, Roine R. Study quality and evidence of benefit in recent assessments of telemedicine. J Telemed Telecare 2004;10:318–324 [DOI] [PubMed] [Google Scholar]
- 12. Narasimhan M, Druss BG, Hockenberry JM, et al. Impact of a telepsychiatry program at emergency departments statewide on the quality, utilization, and costs of mental health services. Psychiatr Serv 2015;66:1167–1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Roine R, Ohinmaa A, Hailey D. Assessing telemedicine: A systematic review of the literature. CMAJ 2001;165:765–771 [PMC free article] [PubMed] [Google Scholar]
- 14. Schwamm LH, Holloway RG, Amarenco P, et al. A review of the evidence for the use of telemedicine within stroke systems of care: A scientific statement from the American Heart Association/American Stroke Association. Stroke 2009;40:2616–2634 [DOI] [PubMed] [Google Scholar]
- 15. Lilly CM, Cody S, Zhao H, et al. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA 2011;305:2175–2183 [DOI] [PubMed] [Google Scholar]
- 16. Armaignac DL, Saxena A, Rubens M, et al. Impact of telemedicine on mortality, length of stay, and cost among patients in progressive care units: Experience from a large healthcare system. Crit Care Med 2018;46:728–735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Marcin JP, Nesbitt TS, Kallas HJ, et al. Use of telemedicine to provide pediatric critical care inpatient consultations to underserved rural Northern California. J Pediatr 2004;144:375–380 [DOI] [PubMed] [Google Scholar]
- 18. Kumar S, Tay-Kearney ML, Chaves F, et al. Remote ophthalmology services: Cost comparison of telemedicine and alternative service delivery options. J Telemed Telecare 2006;12:19–22 [DOI] [PubMed] [Google Scholar]
- 19. Callahan EJ, Hilty DM, Nesbitt TS. Patient satisfaction with telemedicine consultation in primary care: Comparison of ratings of medical and mental health applications. Telemed J E Health 1998;4:363–369 [DOI] [PubMed] [Google Scholar]
- 20. Moya M, Valdez J, Yonas H, Alverson DC. The impact of a telehealth web-based solution on neurosurgery triage and consultation. Telemed J E Health 2010;16:945–949 [DOI] [PubMed] [Google Scholar]
- 21. Stingley S, Schultz H. Helmsley trust support for telehealth improves access to care in rural and frontier areas. Health Aff (Millwood) 2014;33:336–341 [DOI] [PubMed] [Google Scholar]
- 22. Williams JM, Ehrlich PF, Prescott JE. Emergency medical care in rural America. Ann Emerg Med 2001;38:323–327 [DOI] [PubMed] [Google Scholar]
- 23. Brennan JA, Kealy JA, Gerardi LH, et al. Telemedicine in the emergency department: A randomized controlled trial. J Telemed Telecare 1999;5:18–22 [DOI] [PubMed] [Google Scholar]
- 24. Stamford P, Bickford T, Hsiao H, Mattern W. The significance of telemedicine in a rural emergency department. IEEE Eng Med Biol Mag 1999;18:45–52 [DOI] [PubMed] [Google Scholar]
- 25. Mohr NM, Young T, Harland KK, et al. Emergency department telemedicine shortens rural time-to-provider and emergency department transfer times. Telemed J E Health 2018;;24:582–593 [DOI] [PubMed] [Google Scholar]
- 26. Natafgi N, Shane DM, Ullrich F, et al. Using tele-emergency to avoid patient transfers in rural emergency departments: An assessment of costs and benefits. J Telemed Telecare 2018;24:193–201 [DOI] [PubMed] [Google Scholar]
- 27. Zachrison KS, Boggs KM, E MH, et al. A national survey of telemedicine use by US emergency departments. J Telemed Telecare 2018. [Epub ahead of print]; DOI: 10.1177/1357633X18816112 [DOI] [PubMed]
- 28. Ward MM, Ullrich F, MacKinney AC, et al. Tele-emergency utilization: In what clinical situations is tele-emergency activated? J Telemed Telecare 2016;22:25–31 [DOI] [PubMed] [Google Scholar]
- 29. Ward MM, Jaana M, Natafgi N. Systematic review of telemedicine applications in emergency rooms. Int J Med Inform 2015;84:601–616 [DOI] [PubMed] [Google Scholar]
- 30. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int J Surg 2014;12:1495–1499 [DOI] [PubMed] [Google Scholar]
- 31. Baratloo A, Rahimpour L, Abushouk AI, et al. Effects of telestroke on thrombolysis times and outcomes: A meta-analysis. Prehosp Emerg Care 2018;22:472–484 [DOI] [PubMed] [Google Scholar]
- 32. Escobar-Curbelo L, Franco-Moreno AI. Application of telemedicine for the control of patients with acute and chronic heart diseases. Telemed J E Health 2019;25:1033.–1039. [DOI] [PubMed] [Google Scholar]
- 33. Emergency department visits by patients with mental health disorders—North Carolina, 2008–2010. MMWR Morb Mortal Wkly Rep 2013;62:469–472 [PMC free article] [PubMed]
- 34. Asiedu GB, Fang JL, Harris AM, et al. Health care professionals' perspectives on teleneonatology through the lens of normalization process theory. Health Sci Rep 2019;2:e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mohr NM, Young T, Harland KK, et al. Telemedicine is associated with faster diagnostic imaging in stroke patients: A cohort study. Telemed J E Health 2019;25:93–100 [DOI] [PubMed] [Google Scholar]
- 36. Wade V, Eliott J, Karnon J, Elshaug AG. A qualitative study of sustainability and vulnerability in Australian telehealth services. Stud Health Technol Inform 2010;161:190–201 [PubMed] [Google Scholar]
- 37. Aamodt IT, Lycholip E, Celutkiene J, et al. Health care professionals' perceptions of home telemonitoring in heart failure care: Cross-sectional survey. J Med Internet Res 2019;21:e10362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Driessen J, Castle NG, Handler SM. Perceived benefits, barriers, and drivers of telemedicine from the perspective of skilled nursing facility administrative staff stakeholders. J Appl Gerontol 2018;37:110–120 [DOI] [PubMed] [Google Scholar]
- 39. State Telehealth Laws and Reimbursement Policies: Public Health Institute, The Center for Connected Health Policy, 2018. Available at https://www.cchpca.org/telehealth-policy/current-state-laws-and-reimbursement-policies# (last accessed September26, 2019)
- 40. Wilson FA, Rampa S, Trout KE, Stimpson JP. Reimbursements for telehealth services are likely to be lower than non-telehealth services in the United States. J Telemed Telecare 2017;23:497–500 [DOI] [PubMed] [Google Scholar]
- 41. Query LA, Olson KR, Meyer MT, Drendel AL. Minding the gap: A qualitative study of provider experience to optimize care for critically Ill children in general emergency departments. Acad Emerg Med 2018;26:803–813 [DOI] [PubMed] [Google Scholar]
- 42. Brova M, Boggs KM, Zachrison KS, et al. Pediatric telemedicine use in united states emergency departments. Acad Emerg Med 2018;25:1427–1432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Heath B, Salerno R, Hopkins A, et al. Pediatric critical care telemedicine in rural underserved emergency departments. Pediatr Crit Care Med 2009;10:588–591 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.