Abstract
Aim
To compare the radiotherapy technique used in a randomised trial with VMAT and an in-house technique for prostate cancer.
Background
Techniques are evolving with volumetric modulated arc therapy (VMAT) commonly used. The CHHiP trial used a 3 PTV forward planned IMRT technique (FP_CH). Our centre has adopted a simpler two PTV technique with locally calculated margins.
Materials and methods
25 patients treated with FP_CH to 60 Gy in 20 fractions were re-planned with VMAT (VMAT_CH) and a two PTV protocol (VMAT_60/52 and VMAT_60/48). Target coverage, conformity index (CI), homogeneity index (HI), monitor units (MU) and dose to the rectum, bladder, hips and penile bulb were compared.
Results
PTV coverage was high for all techniques. VMAT_CH plans had better CI than FP_CH (p ≤ 0.05). VMAT_60/52/48 plans had better CI than VMAT_CH. FP_CH had better HI and fewer MU than VMAT (p ≤ 0.05). More favourable rectum doses were found for VMAT _CH than FP_CH (V48.6, V52.8, V57, p ≤ 0.05) with less difference for bladder (p ≥ 0.05). Comparing VMAT_CH to VMAT_60/52/48 showed little differences for the bladder and rectum but VMAT_CH had larger penile bulb doses (V40.8, V48.6, mean, D2,p ≤ 0.05). Femoral head doses (V40.8) were similarly low for all techniques (p = ≥ 0.05).
Conclusion
VMAT produced more conformal plans with smaller rectum doses compared to FP_CH albeit worse HI and more MU. VMAT_60/52 and VMAT_60/48 plans had similar rectal and bladder doses to VMAT_CH but better CI and penile bulb doses which may reduce toxicity.
Keywords: Prostate cancer, Intensity modulated radiotherapy, Dosimetric comparison, Hypofractionation, Planning technique
1. Background
Prostate cancer is the most common non cutaneous cancer in men accounting for approximately 26% of all new male cancers in the UK.1,2 Moderate hypofractionation has become a standard of care due to results published from trials like CHHiP (conventional or hypofractionated high dose intensity modulated radiotherapy for prostate cancer) which showed intensity modulated radiotherapy (IMRT) giving 60 Gy in 20 fractions was non-inferior to 74 Gy in 37 fractions.3 Given the low alpha beta ratio of prostate cancer commonly quoted as between 1.4 and 1.93, even more ultra hypofractionation schedules are used with promising results.4, 5, 6, 7 Until satisfactory longer follow up of 2–7 fraction treatment is published from randomised trials, many centres may continue to use 20 fractions.
When the CHHiP trial was introduced, inverse IMRT and volumetric modulated radiotherapy (VMAT) was not widely in use, so a complicated forward planned (FP_CH) 3 target multi-segment simultaneous integrated boost technique was predominantly used.8 With advances in technology, VMAT has emerged with promising dosimetric results showing improved conformity, fewer monitor units (MU), quicker treatments and superior organ at risk (OAR) sparing.9,10
As long term data emerged from CHHiP demonstrating non inferiority of 60 Gy in 20 fractions, it is of importance to compare VMAT with the FP_CH technique. Daily image guided radiotherapy (IGRT) has become a standard practice and institutions are gaining more information about the geometric uncertainties for their techniques. This allows for departmental specific planning target volume (PTV) margins to be used which are important. In our centre, we have adopted a less complicated 2 PTV technique delivering 60 Gy using locally derived PTV margins (5 mm around prostate and 10 mm around seminal vesicles (SV) at risk) based on daily soft tissue IGRT 11
Reducing PTV margins should be done with care to prevent clinical target volume (CTV) underdosing and lowering control 12 The CHHiP IGRT sub study used smaller margins for 3 PTVs (6 mm/3 mm) which, in turn, reduced rectal and bladder doses significantly and to a small non statistically significant degree 2 year bowel toxicity13 This study however did not have enough patients to demonstrate non-inferiority of reduced margins and as a result will unlikely change standard care for many institutions that use locally derived larger PTV margins. It is expected many other departments have similar PTV margins to ours, as 5 mm is commonly employed around the prostate and >7 mm for SV.14
2. Aim
To compare the FP_CH technique with VMAT and a less complex 2 PTV VMAT technique.
3. Materials and methods
3.1. Patients
25 patients treated with FP_CH within the CHHiP trial were re-planned with VMAT (VMAT_CH) and our institutions two PTV volume techniques (VMAT_60/52 and VMAT_60/48 (Table 1)).
Table 1.
Target volumes, PTV margins and doses.
| Protocol | Low risk (LR) | Moderate (MR)/intermediate risk (IR) | Dose (Gy) | Minimum isodoses coverage (Gy) | |
|---|---|---|---|---|---|
| CHHiP | PTV1 | Prostate and base of SV + 10 mm | Prostate + SV + 10 mm | 48 | 45.6 |
| CHHiP | PTV2 | Prostate + 10 mm/5 mm post | Prostate + 10 mm/5 mm | 57.6 | 54.6 |
| CHHiP | PTV3 | Prostate + 5 mm/0 mm post | Prostate + 5 mm/0 mm post | 60 | 57 |
| VMAT 60 52 | PTV60 | Prostate + 5 mm | 60 | 57 | |
| PTV52 | SV base + 10 mm | SV + 10 mm | 52 | 49.4 | |
| VMAT 60 48 | PTV60 | Prostate + 5 mm | 60 | 57 | |
| PTV48 | SV base + 10 mm | SV + 10 mm | 48 | 45.6 | |
Notes: PTV2 was created by adding a 5 mm margin to PTV3. Base of SV was proximal ∼2 cm. T3b patients outlining method excluded for this study.
3.2. Outlining
Outlining and planning was done as per Table 1 on 3 mm slice thickness CT scans. Rectum, bladder, femoral heads and penile bulb were outlined as per the CHHiP protocol. Contouring and growing of targets and optimising structures were done in Prosoma (MedCom, Darmstdt, Germany). No manual editing of volumes took place and the CHHiP PTV2 volumes did not include the base of SV. The SV base used in CHHiP plans was the same as that used in VMAT 60_52/48 plans.
3.3. Treatment planning
Dose objectives and constraints followed Table 1, Table 2. The FP_CH plans were prescribed to 100% point dose. These plans were field in field (anterior and laterals). VMAT plans were prescribed to the mean of the highest dose PTV. Plans were prescribed 60 Gy in 20 fractions.
Table 2.
Dose volume constraints used in CHHiP.
| Dose constraints |
||
|---|---|---|
| Dose (Gy) | Volume (%) | |
| Rectum | 24.6 | 80 |
| 32.4 | 70 | |
| 40.8 | 60 | |
| 48.6 | 50 | |
| 52.8 | 30 | |
| 57 | 15 | |
| 60 | 3 | |
| Bladder | 40.8 | 50 |
| 48.6 | 25 | |
| 60 | 5 | |
| Femoral heads | 40.8 | 50 |
| Penile bulb | 40.8 | 50 |
| 48.6 | 10 | |
FP_CH plans were created in Pinnacle ³ (Philips, Fitchburg, WI, USA) for a Siemens PRIMUS™ Linac (Siemens® Medical Solutions, Inc) using 1 cm MLCs, 15 MV and dynamic wedges. VMAT plans were planned in Pinnacle³ for an Elekta Synergy linear accelerator (Elekta Oncology Systems Ltd., Crawley, UK). VMAT maximum dose rate was 550 MU/min with MLC leaf width of 5 mm and a constrained leaf motion of 0.6 cm/deg. VMAT plans had a single arc from 181° to 179° at 6 MV and collimator angle of 5°. Maximum delivery time was set to 90 s with a gantry angle spacing of 4°. Final dose computation for all plans was on a grid voxel size of 3 × 3 × 3 mm using the adaptive convolve algorithm. VMAT plans were planned by one dosimetrist and FP_CH plans by various physics staff. PTV coverage was priority and not compromised for OAR. PTV dose homogeneity index (HI) and conformity index (CI) were calculated according to International Commission on Radiation Units and Measurements (ICRU) Report 83.15
| HI = D2% − D98%/D50% |
D2%, D98% and D50% is the dose (Gy) to 2%, 98% and 50% of PTV volume.
| CI = V95%/PTV volume (cc) |
V95% is the volume of PTV receiving 95 % of that PTV prescribed dose.
3.4. Statistics
Plan comparisons and statistical analysis were carried out in Statistical Package for Social Science (SPSS) version 24 software (SPSS, Chicago, IL, USA) using a one-way ANOVA with all pairwise comparisons tested using Bonferroni’s multiple comparisons test, with adjusted P-values ≤ 0.05 indicating statistical significance. As PTV2 was only relevant to FP_CH and VMAT_CH plans, a students two tailed t-test was used for this PTV.
4. Results
4.1. Comparison of FP_CH, VMAT_CH, VMAT_60/52 and VMAT_60/48
Table 3, Table 4 show high target coverage across all techniques albeit some variations in SV and OAR doses. CI was higher for VMAT plans than FP_CH and highest for VMAT_60/52 and VMAT_60/48 (p ≤ 0.05). MU was lower in FP_CH than all the VMAT techniques but had largest SV mean dose (p ≤ 0.05).
Table 3.
Mean DVH and monitor unit parameters (mean ± SD) with p values for comparison.
| FP_CH | VMAT_CH | VMAT_60/52 | VMAT_60/48 | p value | |
|---|---|---|---|---|---|
| PTV1 or PTV52/48 | |||||
| V95 (%) | 99.7 ± 0.2 | 99.8 ± 0.1 | 99.6 ± 0.5 | 99.5 ± 0.7 | 0.145 |
| D98 (Gy) | 50.13 ± 1.9 | 47.7 ± 1.1 | 50.4 ± 0.5 | 46.7 ± 0.8 | 0.000 |
| D2 (Gy) | 60.8 ± 0.6 | 61.1 ± 0.4 | 61.0 ± 0.4 | 61.2 ± 0.4 | 0.032 |
| CI | 1.75 ± 0.11 | 1.48 ± 0.10 | 3.3 ± 1.5 | 3.8 ± 1.5 | 0.000 |
| HI | 0.18 ± 0.03 | 0.22 ± 0.02 | 0.19 ± 0.01 | 0.26 ± 0.02 | 0.000 |
| PTV2 | |||||
| V95 (%) | 99.7 ± 0.1 | 99.5 ± 0.4 | – | – | 0.041 |
| D98 (Gy) | 56.1 ± 0.5 | 55.8 ± 0.5 | – | – | 0.026 |
| D2 (Gy) | 60.9 ± 0.6 | 61.2 ± 0.4 | – | – | 0.084 |
| CI | 1.43 ± 0.1 | 1.13 ± 0.06 | – | – | 0.000 |
| HI | 0.08 ± 0.01 | 0.09 ± 0.01 | – | – | 0.005 |
| PTV3 or PTV60 | |||||
| V95 (%) | 99.9 ± 0.2 | 99.9 ± 0.2 | 99.7 ± 0.3 | 99.6 ± 0.3 | 0.000 |
| D98 (Gy) | 58.4 ± 0.3 | 58.7 ± 0.3 | 58.0 ± 0.3 | 58.0 ± 0.3 | 0.000 |
| D2 (Gy) | 60.9 ± 0.6 | 61.3 ± 0.4 | 61.6 ± 0.3 | 61.6 ± 0.3 | 0.000 |
| CI | 1.87 ± 0.22 | 1.55 ± 0.11 | 1.18 ± 0.05 | 1.17 ± 0.05 | 0.000 |
| HI | 0.04 ± 0.01 | 0.04 ± 0.01 | 0.05 ± 0.007 | 0.05 ± 0.009 | 0.000 |
| SV Mean (Gy) | 58.4 ± 1.1 | 56.7 ± 2.0 | 56.9 ± 1.2 | 56.1 ± 1.7 | 0.000 |
| MU | 393.2 ± 12.9 | 536.5 ± 28.1 | 578.7 ± 33.7 | 550.9 ± 27.5 | 0.000 |
| Rectum | |||||
| V24.6 (%) | 68.3 ± 10.7 | 61.2 ± 9.7 | 54.3 ± 10.7 | 53.7 ± 11.0 | 0.000 |
| V32.4 (%) | 48.8 ± 13.0 | 47.1 ± 9.8 | 41.6 ± 10.7 | 40.8 ± 11.0 | 0.027 |
| V40.8 (%) | 38.5 ± 11.8 | 33.1 ± 8.8 | 30.4 ± 9.5 | 29.2 ± 9.0 | 0.006 |
| V48.6 (%) | 28.3 ± 9.6 | 18.8 ± 6.7 | 19.9 ± 7.0 | 16.4 ± 6.3 | 0.000 |
| V52.8 (%) | 20.7 ± 7.9 | 12.6 ± 5.0 | 12.3 ± 5.1 | 11.3 ± 4.9 | 0.000 |
| V57 (%) | 9.7 ± 4.7 | 5.9 ± 2.8 | 6.4 ± 3.3 | 6.6 ± 3.4 | 0.001 |
| V60 (%) | 0.5 ± 1.0 | 0.1 ± 0.2 | 0.6 ± 0.6 | 0.7 ± 0.7 | 0.013 |
| Bladder | |||||
| V40.8 (%) | 25.5 ± 14.5 | 20.2 ± 9.5 | 14.9 ± 6.8 | 15.3 ± 7.4 | 0.001 |
| V48.6 (%) | 19.1 ± 10.6 | 15.0 ± 7.6 | 10.6 ± 5.0 | 10.4 ± 5.4 | 0.000 |
| V60 (%) | 2.3 ± 3.9 | 2.2 ± 1.7 | 1.9 ± 1.2 | 1.8 ± 1.1 | 0.812 |
| Right hip | |||||
| V40.8 (%) | 0.05 ± 0.2 | 0.004 ± 0.02 | 0.03 ± 0.16 | 0 ± 0 | 0.539 |
| Left hip | |||||
| V40.8 (%) | 0 ± 0 | 0.001 ± 0.006 | 0.006 ± 0.03 | 0.01 ± 0.06 | 0.568 |
| Penile bulb | |||||
| V40.8 (%) | 7.1 ± 15.5 | 18.7 ± 23.5 | 5.2 ± 12.5 | 5.4 ± 11.5 | 0.012 |
| V48.6 (%) | 3.5 ± 8.2 | 11.2 ± 15.9 | 2.5 ± 6.3 | 2.9 ± 6.9 | 0.008 |
| Mean (Gy) | 19.9 ± 10.5 | 23.2 ± 12.9 | 12.5 ± 9.9 | 12.6 ± 9.2 | 0.001 |
| D2 (Gy) | 34.9 ± 14.0 | 42.6 ± 14.6 | 25.5 ± 17.6 | 27.0 ± 18.0 | 0.001 |
Abbreviations: SV, seminal vesicles; MU, Monitor units; CI, Conformity index; HI, Homogeneity index; FP_CH, Forward planned CHHiP; VMAT_CH, Volumetric modulated radiotherapy CHHiP; Dx (Gy), dose to given volume (%); Vx (%), volume receiving percentage of that targets prescribed dose; compared with 1-way ANOVA test, p values ≤ 0.05 are highlighted.
Table 4.
Post hoc multiple comparisons (p values) of FP_CH, VMAT_CH, VMAT_60/52 and VMAT_60/48.
| FP_CH vs VMAT_CH | FP_CH vs VMAT_60/52 | FP_CH vs VMAT_60/48 | VMAT_CH vs VMAT_60/52 | VMAT_CHvs VMAT_60/48 | VMAT_60/52 vs VMAT_60/48 | |
|---|---|---|---|---|---|---|
| PTV1 or PTV52/48 | ||||||
| V95 (%) | 1.000 | 1.000 | 0.641 | 0.682 | 0.281 | 1.000 |
| D98 (Gy) | 0.000 | 1.000 | 0.000 | 0.000 | 0.029 | 0.000 |
| D2 (Gy) | 0.421 | 1.000 | 0.023 | 1.000 | 1.000 | 0.504 |
| CI | 1.000 | 0.000 | 0.000 | 0.000 | 0.000 | 1.000 |
| HI | 0.000 | 0.782 | 0.000 | 0.000 | 0.000 | 0.000 |
| PTV2* | ||||||
| V95 (%) | 0.021 | N/A | N/A | N/A | N/A | N/A |
| D98 (Gy) | 0.031 | N/A | N/A | N/A | N/A | N/A |
| D2 (Gy) | 0.095 | N/A | N/A | N/A | N/A | N/A |
| CI | 0.000 | N/A | N/A | N/A | N/A | N/A |
| HI | 0.006 | N/A | N/A | N/A | N/A | N/A |
| PTV3 or PTV60 | ||||||
| V95 (%) | 1.000 | 0.002 | 0.000 | 0.001 | 0.000 | 1.000 |
| D98 (Gy) | 0.005 | 0.000 | 0.000 | 0.000 | 0.000 | 1.000 |
| D2 (Gy) | 0.083 | 0.000 | 0.000 | 0.137 | 0.073 | 1.000 |
| CI | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 1.000 |
| HI | 1.000 | 0.000 | 0.000 | 0.000 | 0.000 | 1.000 |
| SV Mean (Gy) | 0.001 | 0.013 | 0.000 | 1.000 | 1.000 | 0.524 |
| MU | 0.000 | 0.000 | 0.000 | 0.000 | 0.353 | 0.002 |
| Rectum | ||||||
| V24.6 (%) | 0.109 | 0.000 | 0.000 | 0.140 | 0.091 | 1.000 |
| V32.4 (%) | 1.000 | 0.150 | 0.077 | 0.492 | 0.279 | 1.000 |
| V40.8 (%) | 0.349 | 0.026 | 0.007 | 1.000 | 0.950 | 1.000 |
| V48.6 (%) | 0.000 | 0.001 | 0.000 | 1.000 | 1.000 | 0.574 |
| V52.8 (%) | 0.000 | 0.000 | 0.000 | 1.000 | 1.000 | 1.000 |
| V57 (%) | 0.003 | 0.011 | 0.021 | 1.000 | 1.000 | 1.000 |
| V60 (%) | 0.261 | 1.000 | 1.000 | 0.051 | 0.015 | 1.000 |
| Bladder | ||||||
| V40.8 (%) | 0.362 | 0.002 | 0.003 | 0.406 | 0.525 | 1.000 |
| V48.6 (%) | 0.322 | 0.001 | 0.000 | 0.247 | 0.199 | 1.000 |
| V60 (%) | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Right hip | ||||||
| V40.8 (%) | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Left hip | ||||||
| V40.8 (%) | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| Penile bulb | ||||||
| V40.8 (%) | 0.085 | 1.000 | 1.000 | 0.028 | 0.030 | 1.000 |
| V48.6 (%) | 0.048 | 1.000 | 1.000 | 0.017 | 0.027 | 1.000 |
| Mean (Gy) | 1.000 | 0.103 | 0.108 | 0.004 | 0.004 | 1.000 |
| D2 (Gy) | 0.558 | 0.255 | 0.523 | 0.002 | 0.005 | 1.000 |
Abbreviations: SV, seminal vesicles; MU, Monitor units; CI, Conformity index; HI, Homogeneity index; FP_CH, Forward planned CHHiP; VMAT_CH, Volumetric modulated radiotherapy CHHiP; Dx (Gy), dose to given volume (%); Vx (%), volume receiving percentage of that targets prescribed dose; *, paired t-test used for PTV2 only, p values ≤ 0.05 are highlighted.
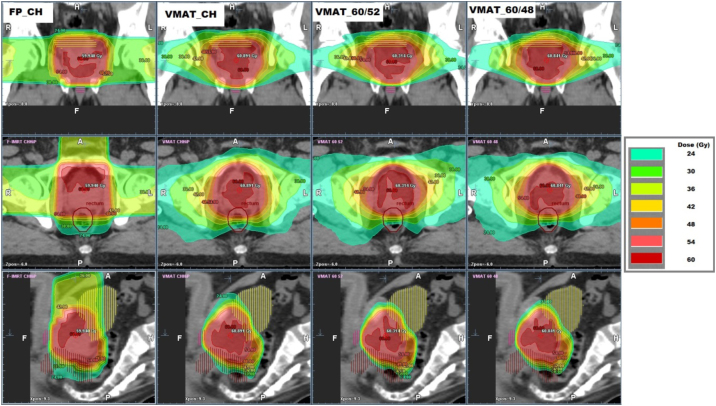
FP_CH showed the highest rectal and bladder doses followed by VMAT_CH, VMAT_60/52 and VMAT_60/48 (Fig. 1, Fig. 2). FP_CH had many statistically significant (SS) higher rectal doses compared to VMAT_CH. Only rectal V60 was SS different between VMAT_60/52/48 and VMAT_CH. Table 4 shows the bladder V40.8 and V48.6 were SS higher for FP_CH than VMAT_60/52 and VMAT_60/48 but no SS differences were seen when comparing VMAT only techniques with each other (p ≥ 0.05). Penile bulb doses were smaller in FP_CH than VMAT_CH and decreased significantly in the VMAT_60_52/48 techniques (p ≤ 0.05) (Fig. 3, Table 3, Table 4). Femoral head doses (V40.8) were low for all techniques and of no significance. Fig. 4 illustrates a typical dose distribution for all techniques which shows the superior doses of VMAT plans than FP_CH.
Fig. 1.
Mean rectum doses for all techniques.
Fig. 2.
Mean bladder doses for all techniques.
Fig. 3.
Mean penile bulb doses for all techniques.
Fig. 4.
Dose distributions for the 4 techniques.
4.2. Discussion
This study compares various different IMRT techniques with different margins, volumes and doses showing acceptable target coverage albeit with variable doses to OAR and SV. For PTV3/60 CI was the best for VMAT_60/52/48 than VMAT_CH/FP_CH. This appeared to be most likely down to having a three PTV protocol in CHHiP compared to two. The distance between PTV3 to PTV2 was 5 mm in CHHiP and the PTV2 required a minimum 54.6 Gy isodose to cover meaning that the 57 Gy had to become slightly less conformal on PTV3. This 54.6 Gy coverage aim was not an issue in the 2 target techniques and, therefore, could place the 57 Gy isodose more tightly around the PTV60 (distance from 57 Gy to 54.6 Gy isodose was ∼2 mm). Table 3, Table 4 show superior CI for VMAT_60/52 and VMAT_60/48. The improved CI for VMAT over IMRT has been previously highlighted in numerous studies and allow further potential to spare OARs and dose escalate more safely.16,17
Inclusion of SV and to what dose remains controversial with some excluding portions depending on invasion risk and others excluding them altogether.4,9 FP_CH plans showed significantly higher mean doses to SV than the VMAT plans by a max of 2.3 Gy but no SS differences were seen among VMAT plans only. This is most likely better conformity in all directions in the VMAT plans. The proximal 1 cm of SV has been noted to be at most risk of invasion in pathological studies and the effect of increased incidental doses to CTV is something to note as unintentional failures may arise with increased conformity.18 This concept has been shown for nodes in higher risk prostate patients.19,20 Additionally, the VMAT_60/52 and VMAT_60/48 techniques which do not have a PTV2 target like CHHiP may lead to tighter isodoses around the prostate. A more simple 2 target approach appears to be the direction of travel as shown in more current trials like PACE B and PIVOTALboost.6,21
VMAT_CH plans had mostly lower rectal doses than FP_CH (V48.6, V52.8, V57). Similar planning work was found by Boylan et al. comparing IMRT and VMAT in CHHiP plans.9 Moreover, in the CHHiP trial comparing an inverse solution to the F-IMRT, they found significant results for the rectum, but not V60 due to small volumes at this dose.22 Encouragingly our VMAT_60/52/48 plans were less than the FP_CH plans and also had little differences with VMAT_CH. Rectum V60 in VMAT_CH was marginally smaller by 0.7 % (Table 3) due to its smaller posterior PTV margin. This is unlikely to be of any clinical significance for toxicity and the VMAT_60/52 technique uses a more appropriate 5 mm posterior margin. This allows consideration for the larger uncertainties of anterior-posterior prostate motion which is well documented.23
The median absolute reductions in rectal volume receiving a certain dose were larger in the study by Naismith et al. than the means in this one and they showed that acute bowel toxicity was worse in the FP_CH group than the inverse planned group (acute RTOG grade ≥2 was 52 % versus 21 %).21 The CHHiP trial used mostly five field step and shoot five IMRT for its inverse group and comparing this to VMAT may be of interest. A study Rosenthal et al. compared VMAT with step and shoot IMRT and found VMAT to be equivalent or better for sparing OAR.24 Other work has replicated this finding with VMAT preferred.20,25,26
The bladder doses were significantly higher for the FP_CH compared with VMAT_60/52/48 for V40.8 and V48.6 but there were no statistical differences at V60 for all techniques. The doses assessed were also less for VMAT_CH compared to FP_CH but were not significant. This is in contrast to the CHHiP forward versus inverse planning work which showed statistically higher V100 % in inverse plans, predominantly the step and shoot technique.21 In their work despite inverse plans showing lower bladder doses (equivalent to the V40.8 and V48.6 in this study) as well as similar acute and 2 year RTOG grade ≥ 2 toxicity between FP_CH and inverse, the inverse group appeared to have slightly higher grade ≥ 1 and late bladder toxicity. This may indicate the higher importance of reducing high doses to the bladder to minimise toxicity. Work has shown that the main predictor of bladder toxicity is likely related to high doses to the bladder base/neck.27 There were no statistically significant differences between techniques for bladder doses among VMAT plans. There was, however, a trend seen for lower bladder doses to V48.6 and V40.8 for the VMAT_60/52/48 plans compared with VMAT_CH. This appears to be explained by exclusion of PTV2 and having the lower dose PTV52/48 grown only around the CTV SV.
Penile bulb doses were significantly lower in the VMAT_60/52/48 techniques compared to both FP_CH and VMAT_CH. Although not within the CHHiP dose constraints, the mean dose and D2 were collected retrospectively as these have been most associated with erectile function.28,29 As the penile bulb is positioned mostly inferior to the PTV, dose gradients and scatter are important factors affecting its dose. The use of a penile bulb dose objective during optimisation may be more needed for VMAT_CH plans in attempt to lower doses. The dose will unlikely be as low in the CHHiP plans due to minimum isodose coverage constraints applied to PTV2 and PTV1 which extend inferior also. The significant reduction of penile bulb dose by VMAT_60/52 and VMAT_60/48 techniques compared to VMAT_CH plans is supported by a recent UK radiotherapy treatment planning study. From a total of 48 departments that submitted localised prostate plans based on their centres’ practice, the VMAT_60/52 technique scored the lowest penile bulb doses (V40.8 and V48.6).30 This finding is significant given the large heterogeneity between departments including differences in target volume growing, techniques, planners and local procedures. The study reported that 47% of departments adhered to the CHHiP protocol with 76% using VMAT 6 MV.
The IGRT sub study of CHHiP had randomized groups to IGRT or without. Two of the groups had either standard or reduced margins which found more favourable side effects in the reduced margin group. The margins used were 3 mm (0 mm post) around the prostate and 6 mm around PTV1 and PTV2 (3 mm post).13 These margins may reduce OAR doses to lower that of the two PTV technique used in the current study, however long term control is less clear for those smaller margins. Our PTV margins of 5 mm and 10 mm around the prostate and SV may therefore be more applicable to the wider community.
This single institution study was limited by the influence of the planner on the optimisation of the plans. Plans may be further optimised by individual changing of the dose objectives dependent on treatment plan strategy. Despite this, PTV target coverage was kept as a priority and a single planner avoided any effects of inter-planner variability for the VMAT plans. The FP_CH plans were planned using 1 cm MLC compared to VMAT plans with 5 mm leaf width. It is known that finer MLC can improve CI and lower OAR doses further.31 The FP_CH technique in this work represents real plans delivered to patients within the CHHiP trial and, therefore, its comparison with more current VMAT solutions quantifies the evolution of the techniques and dosimetry.
5. Conclusion
All techniques gave acceptable target coverage albeit different doses to OAR and SV. The FP_CH plans tended to give less favourable CI and dose to the rectum and bladder than VMAT and our in-house two PTV techniques. FP_CH had less MU, better HI and penile bulb doses than VMAT. Rectum and bladder differences between VMAT_CH and VMAT_60/52/48 were relatively small but significant reductions were seen for the penile bulb favouring the two PTV technique. These dosimetric differences will allow a more informed decision about using different margins, volumes and doses in moderately hypofractionated radiotherapy for localised prostate cancer.
Conflicts of interest
None declared.
Financial disclosure
None declared.
References
- 1.Barrett A., Dobbs J., Morris S., Roques T. 4th ed. Hodder Arnold; London: 2009. Practical radiotherapy planning; p. 332. [Google Scholar]
- 2.Cancer Research UK. Prostate cancer statistics, https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer [Accessed online September 2019].
- 3.Dearnaley D., Syndikus I., Mossop H. Conventional versus hypofractionated high-dose intensity modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority phase 3 CHHiP trial. Lancet Oncol. 2016;17:1047–1060. doi: 10.1016/S1470-2045(16)30102-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Widmark A., Gunnlaugsson A., Beckman L. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial. Lancet. 2019;394(10196):385–395. doi: 10.1016/S0140-6736(19)31131-6. [DOI] [PubMed] [Google Scholar]
- 5.Jackson W.C., Silva J., Hartman H.E. Stereotactic body radiation therapy for localized prostate cancer: a systematic review and meta analysis of over 6,000 patients treated on prospective studies. Int J Radiat Oncol Biol Phys. 2019;104(4):778–789. doi: 10.1016/j.ijrobp.2019.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brand D.H., Tree A.C., Oster P. Intensity-modulated fractionated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): acute toxicity findings from an international, randomised, open-label, phase 3, non-inferiority trial. Lancet Oncol. 2019;19:S1470–2045. doi: 10.1016/S1470-2045(19)30569-8. 30569-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alayed Y., Cheung P., Chu W. Two StereoTactic ablative radiotherapy treatments for localized prostate cancer (2STAR): results from a prospective clinical trial. Radiother Oncol. 2019;135:86–90. doi: 10.1016/j.radonc.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 8.South C.P., Khoo V.S., Naismith O., Norman A., Dearnaley D.P. A comparison of treatment planning techniques used in two randomised UK external beam radiotherapy trials for localised prostate cancer. Clin Oncol (R Coll Radiol) 2008;20(1):15–21. doi: 10.1016/j.clon.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 9.Boylan C.J., Golby C., Rowbottom C.G. A VMAT planning solution for prostate patients using a commercial treatment planning system. Phys Med Biol. 2010;55:N395–N404. doi: 10.1088/0031-9155/55/14/N01. [DOI] [PubMed] [Google Scholar]
- 10.Ren W., Sun C., Lu N. Dosimetric comparison of intensity-modulated radiotherapy and volumetric-modulated arc radiotherapy in patients with prostate cancer: a meta-analysis. J Appl Clin Med Phys. 2016;17(6):254–262. doi: 10.1120/jacmp.v17i6.6464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas S.J., Ashburner M., Tudor G.S. Intra-fraction motion of the prostate during treatment with helical tomotherapy. Radiother Oncol. 2013;109(3):482–486. doi: 10.1016/j.radonc.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 12.Engels B., Soete G., Verellen D., Storme G. Conformal arc radiotherapy for prostate cancer: Increased biochemical failure in patients with distended rectum on the planning computed tomogram despite image guidance by implanted markers. Int J Radiat Oncol Biol Phys. 2009;74(2):388–391. doi: 10.1016/j.ijrobp.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Murray J., Griffin C., Gulliford S. A randomised assessment of image guided radiotherapy within a phase 3 trial of conventional or hypofractionated high dose intensity modulated radiotherapy for prostate cancer. Radiother Oncol. 2019 doi: 10.1016/j.radonc.2019.10.017. In Press, Corrected Proof. Available online 22 November 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yartsev S., Bauman G. Target margins in radiotherapy of prostate cancer. Br J Radiol. 2016;89(1067) doi: 10.1259/bjr.20160312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ICRU International Commission on Radiation Units and Measurements. prescribing, recording, and reporting photon-beam intensity modulated radiation therapy (IMRT). ICRU Report 83. J ICRU. 2010;10(1):1–106. [Google Scholar]
- 16.Cakir A., Akgun Z., Fayda M., Agaoglu F. Comparison of three dimensional conformal radiation therapy, intensity modulated radiation therapy and volumetric modulated arc therapy for low radiation exposure of normal tissue in patients with prostate cancer. Asian Pac J Cancer Prev. 2015;16(8):3365–3370. doi: 10.7314/apjcp.2015.16.8.3365. [DOI] [PubMed] [Google Scholar]
- 17.Elith C.A., Cao F., Dempsey S.E., Findlay N., Warren-Forward H.A. Retrospective planning analysis comparing volumetric-modulated arc therapy (VMAT) to intensity-modulated radiation therapy (IMRT) for radiotherapy treatment of prostate Cancer. J Med Imaging Radiat Sci. 2013;44(2):79–86. doi: 10.1016/j.jmir.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Kestin L., Goldstein N., Vicini F. Treatment of prostate cancer with radiotherapy: should the entire seminal vesicles be included in the clinical target volume? Int J Radiat Oncol Biol Phys. 2002;54(3):686–697. doi: 10.1016/s0360-3016(02)03011-0. [DOI] [PubMed] [Google Scholar]
- 19.Witte M.G., Heemsbergen W.D., Bohoslavsky R. Relating dose outside the prostate with freedom from failure in the Dutch trial 68 Gy vs. 78 Gy. Int J Radiat Oncol Biol Phys. 2010;77(1):131–138. doi: 10.1016/j.ijrobp.2009.04.040. [DOI] [PubMed] [Google Scholar]
- 20.Heemsbergen W.D., Al-Mamgani A., Witte M.G. Radiotherapy with rectangular fields is associated with fewer clinical failures than conformal fields in the high-risk prostate cancer subgroup: results from a randomized trial. Radiother Oncol. 2013;107(2):134–139. doi: 10.1016/j.radonc.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 21.PIVOTALboost trial (ISRCTN80146950, CRUK/16/018). http://www.isrctn.com/ISRCTN80146950 [Accessed online October 2019].
- 22.Naismith O.F., Griffin C., Syndikus I. Forward- and inverse-planned intensity-modulated radiotherapy in the CHHiP Trial: a comparison of dosimetry and normal tissue toxicity. Clin Oncol. 2019;31(9):600–610. doi: 10.1016/j.clon.2019.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gleeson I. Calculation of planning margins for different verification techniques in radical prostate radiotherapy. J Radiother Pract. 2014;13:149–158. [Google Scholar]
- 24.Rosenthal S.A., Wu C., Mangat J.K. Comparison of volumetric arc therapy (VMAT) vs. fixed field intensity modulated radiation therapy (IMRT) techniques for the treatment of localized prostate cancer. Int J Radiat Oncol Biol Phys. 2010;78(3):S755. [Google Scholar]
- 25.Lalya I., Zaghba N., Andaloussi-Saghir K. Volumetric modulated arc therapy versus intensity modulated radiation therapy in the treatment of prostate Cancer: a systematic literature review. Int J Radiol Radiat Oncol. 2016;2(1):015–020. [Google Scholar]
- 26.Teoh M., Clark C.H., Wood K., Whitaker S., Nisbet A. Volumetric modulated arc therapy: a review of current literature and clinical use in practice. Br J Radiol. 2011;84(1007):967–996. doi: 10.1259/bjr/22373346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghadjar P., Zelefsky M.J., Spratt D.E. The impact of dose to the bladder trigone on long-term urinary function after high-dose intensity-modulated radiation therapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2014;88(2):339–344. doi: 10.1016/j.ijrobp.2013.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray J., Dean J., Mossop H. Effect of dose to the penile bulb on erectile potency (EP) in prostate image-guided radiotherapy (IGRT) Clin Oncol. 2017;29:e84–e89. [Google Scholar]
- 29.Rasmusson E., Gunnlaugsson A., Wieslnder E. Erectile dysfunction and absorbed dose to penile base structures in a randomized trial comparing ultrahypofractionated and conventionally fractionated radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2019;105(1):S133–S134. doi: 10.1016/j.ijrobp.2020.01.022. [DOI] [PubMed] [Google Scholar]
- 30.UK Planning Study 2019: Prostate (60Gy). https://proknowsystems.com/planning/studies [Accessed online October 2019].
- 31.Orlandini L.C., Betti M., Fulcheri C., Coppola M., Cionini L. Dosimetric impact of different multileaf collimators on prostate intensity modulated treatment planning. Rep Pract Oncol Radiother. 2015;20(5):358–364. doi: 10.1016/j.rpor.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]