Abstract
Objective
Both Internet-delivered cognitive behavioural therapy (ICBT) and Internet-delivered psychodynamic psychotherapy (IPDT) have shown promise in the treatment of social anxiety disorder (SAD). However, little is known about client preferences and what predicts treatment outcome. The objective of the present pilot study was to examine preference for ICBT versus IPDT in the treatment of SAD and whether participants' preference strength and therapeutic alliance predicted treatment response. Further, we also investigated the effect of the two treatments, including 6-months follow-up.
Method
Thirty-six participants were instructed to choose between either IPDT or ICBT based on a brief description. Both treatments were 10 weeks long. Liebowitz Social Anxiety Scale – Self Report was used as the primary outcome measure.
Results
IPDT (N = 23; 63.9%) was preferred more often than ICBT (N = 13; 36.1%), but the difference did not reach statistical significance (p = .10). Preference strength did not predict the treatment effect but therapeutic alliance did. The observed within-group effects for the treatment period were d = 0.40 [−0.21, 0.99] for the IPDT group and d = 0.53 [−0.29, 1.31] for the ICBT group. An intention-to-treat (ITT) analysis revealed no significant difference between the two treatments on any outcome measure at either post-treatment or at six months follow-up.
Conclusion
The present pilot study did not find a difference in preference for IPDT or ICBT in the treatment of SAD and both treatments resulted in small to moderate improvements in symptoms of SAD. Preference strength might not predict treatment effect, but this needs to be tested in larger studies.
Keywords: Social anxiety disorder, Psychodynamic psychotherapy, Cognitive behavioural therapy, Internet-delivered treatment, Preference matching
Highlights
-
•
No significant difference regarding preference for the two treatments were found.
-
•
Both treatments resulted in similar improvements in social anxiety symptoms.
-
•
Preference strength did not predict treatment effect but therapeutic alliance did.
-
•
The small sample size is a major limitation of the study.
1. Introduction
Social anxiety disorder (SAD) is one of the most common anxiety disorders, affecting between 5 and 15% of the adult population (Fehm et al., 2005; Kessler et al., 2005). It is characterized by excessive fear of being humiliated or embarrassed in social situations (American Psychiatric Association, 2013) and is often chronic and severely debilitating if untreated (Grant et al., 2005). Social anxiety disorder shows a high comorbidity with other diagnoses, such as depression, as well as other anxiety disorders (Goldstein-Piekarski et al., 2016; Langer and Rodebaugh, 2014).
Meta-analytic evidence supports the efficacy of several different treatment methods for treating SAD, with cognitive behavioural therapy (CBT) currently having the strongest research support (Cuijpers et al., 2013; Mayo-Wilson et al., 2014). There are also several trials on Internet-delivered CBT (ICBT) for SAD (Kampmann et al., 2016). Moreover, at least two randomized controlled trials (RCTs) have been published showing roughly equivalent outcomes for psychodynamic therapy (PDT) when compared to CBT (Bögels et al., 2014; Leichsenring et al., 2013). There is also a controlled trial on Internet-delivered PDT (IPDT) showing large treatment effects compared to a wait-list control, and the effects had increased at a two-year follow-up (Johansson et al., 2017). Thus, PDT could also be considered a promising treatment option for SAD that may also be possible to deliver via the Internet.
Even if there are different treatment options for SAD, there are many patients that do not obtain an optimal treatment effect despite receiving evidence-based treatment (Mayo-Wilson et al., 2014). In addition, several studies show that up to four out of five treated patients (60–80%) do not go into remission after treatment termination (Leichsenring et al., 2014; Liebowitz et al., 2005). With regards to Internet-based interventions, no consistent predictors of treatment response have yet emerged (Andersson et al., 2018), meaning that little is known about why a particular treatment works for one patient and not for another or which treatment would be most suitable for a particular patient. One exception was a patient-level analysis based on trials of ICBT for SAD (Tillfors et al., 2015) in which risk profiles based on cluster analysis showed that a cluster of individuals with high levels of social avoidance and depressive symptoms constituted a risk profile for poor treatment response. Another line of research has studied pre-treatment neuroimaging and machine learning with promising results (Månsson et al., 2015), although such predictors is thus far unlikely to be used in regular clinical practice. Moreover, the therapeutic alliance, which has shown a small but robust relationship to outcome in face-to-face psychotherapy studies (Horvath et al., 2011), has failed to consistently predict outcomes in Internet-delivered trials (Andersson et al., 2018). Still, a recent meta-analysis indicated that the association between early alliance and outcome in Internet interventions was about the same as in face-to-face studies (Probst et al., in press).
Notwithstanding the difficulties in finding robust predictors of outcomes mentioned above, one element that has been found to be associated with lower dropouts as well as better treatment effects in face-to-face psychotherapy is client treatment preferences (Swift et al., 2018). A recent meta-analysis based on 53 studies found that that considering treatment preferences increased the treatment effect with Cohen's d = 0.28 compared to providing a client with a non-preferred treatment. Being offered a preferred treatment also decreased the risk of dropout (odds ratio = 1.79; Swift et al., 2018). Interestingly, a study by Raue et al. (2009) found that preference strength was a better predictor than the preference matching itself. For example, in a study on behavioural activation and pharmacotherapy, Moradveisi et al. (2014) found that preference strength significantly predicted treatment adherence in the behavioural activation arm but not in the pharmacotherapy arm. In addition, not believing in your pharmacotherapy can reduce the effect by 50% (Faria et al., 2017). In a previous preference study on IPDT vs ICBT for depression from our group we found a small to moderate positive correlation between preference strength and treatment completion, that did not reach statistical significance (Johansson et al., 2013c). The same study also found a significant relationship between preference strength and long-term outcome in the CBT arm (Johansson et al., 2013c). One important factor related to the present study was that a significant number of participants chose ICBT over IPDT when given a choice (30 ICBT 68.2% vs 14 IPDT 31.8%).
Thus, in light of the above-mentioned previous research, the primary aim of the present study was to investigate preference for the psychodynamic and cognitive behavioural Internet-delivered treatments for SAD when participants could choose their treatment orientation. Our hypothesis was that participants would prefer ICBT over IPDT based on the study by Johansson et al. (2013c). A second aim of the study was to investigate whether preference strength at the beginning of the study was associated with treatment outcome or adherence, where we predicted that higher preference strength would be associated with better outcome and higher adherence, based on previous research summarized above. Thirdly, given the mixed finding regarding therapeutic alliance as a predictor in Internet-delivered interventions, we also investigated whether therapeutic alliance measured at week three predicted treatment outcome. Out hypothesis was that therapeutic alliance would be significantly related to treatment outcome. Finally, we also wanted to investigate the effectiveness of the two treatments, were we excepted both treatments to result in large within-group effects on social anxiety symptoms that would be maintained at 6-months follow-up.
2. Method
2.1. Design
The present study was part of a larger RCT – the SOFIA study – in which the effects of affect-focused IPDT for social phobia were evaluated (Johansson et al., 2017). The present study started when the treatment phase of the larger RCT study had been completed. The participants who had been allocated to the wait-list condition in the trial were given the opportunity to choose between IPDT or ICBT for SAD, a design known as preference matching. The choice was made following a brief description. Both treatments were 10 weeks long.
2.2. Recruitment
Participants were recruited through registration on the SOFIA project's website. The project had been advertised in newspapers and through social media during late 2013 and early 2014 (for details, see Johansson et al., 2017) and was approved by the regional ethics review board in Linköping, Sweden (reg. no. 2013/361–31).
2.3. Assessment and selection
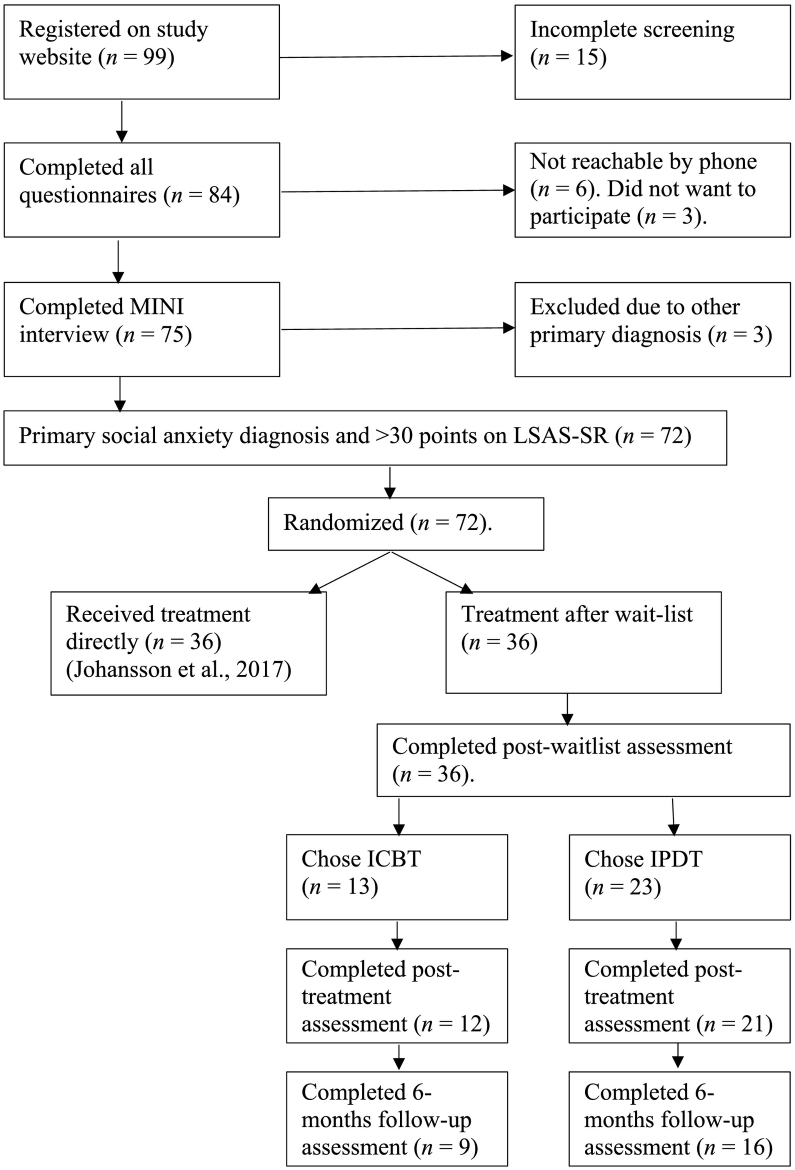
When the registration period for the project expired, a total of 99 people had reported their interest in participating in the study. A flowchart of the selection process is provided in Fig. 1. A total of 75 diagnostic interviews were conducted by master-level psychology students. To be included in the study, a participant had to meet the DSM-IV diagnostic criteria for social phobia. In addition, a participant had to be 18 years of age or above; attain a score on the LSAS-SR of ≥30 points; and be able to speak, write and read Swedish as well as have access to a computer with Internet connection. It was not possible to participate in the study if the participant was already undergoing any other psychological treatment. Concurrent medication was allowed if it had been taken as a stable dose for at least three months. Exclusion criteria included elevated suicide risk, serious psychiatric problems such as psychotic illness, another primary diagnosis requiring another form of treatment and ongoing substance abuse.
Fig. 1.
Flowchart of participants throughout the study.
In total, 73 participants met the inclusion criteria for the study and were randomized to either treatment or wait-list control (see Johansson et al., 2017). At the end of the trial period, telephone interviews were conducted with the wait-list participants (n = 36) who were invited to choose between either IPDT (n = 23; 63.9%) or ICBT (n = 13; 36.1%) based on a brief description (see below). Table 1 describes the demographics of the present study sample. The post-treatment assessment was conducted via the study platform and by telephone. See Fig. 1 below for an overview of the selection process.
Table 1.
Sociodemographic characteristics of participants at baseline.
| ICBT (n = 13) | IPDT (n = 23) | ||
|---|---|---|---|
| Age | Mean age, (SD) | 41.4 (12.0) | 43.8 (16.3) |
| Min-Max | 20–72 | 23–62 | |
| Gender | Woman | 8 (62%) | 17 (74%) |
| Man | 5 (38%) | 6 (26%) | |
| Marital status | Married or living with partner | 7 (54%) | 14 (61%) |
| Partner, not living together | 1 (8%) | 2 (9%) | |
| Divorced, widow, widower | 1 (8%) | 1 (4%) | |
| Single | 4 (31%) | 6 (26%) | |
| Occupation | Working | 8 (62%) | 18 (78%) |
| Unemployed | 0 (0%) | 3 (13%) | |
| Retired | 1 (8%) | 0 (0%) | |
| Parental leave | 0 (0%) | 1 (4%) | |
| Student | 4 (31%) | 1 (4%) | |
| Education level | Elementary school | 1 (8%) | 1 (4%) |
| High school/College | 5 (38%) | 0 (0%) | |
| University, < 3 years | 0 (0%) | 4 (17%) | |
| University, > 3 years | 5 (38%) | 14 (61%) | |
| Other | 2 (16%) | 4 (17%) | |
| Other psychotherapy | Ongoing | 2 (15%) | 0 (0%) |
| No, but previously | 7 (54%) | 16 (70%) | |
| No | 4 (31%) | 7 (30%) | |
| Medication | Ongoing | 5 (38%) | 4 (17%) |
| No, but previously | 3 (23%) | 7 (30%) | |
| No | 5 (38%) | 12 (52%) |
2.4. Procedure
2.4.1. Choice of treatment
The choice of treatment was made by having the participants read a text describing the two treatments; see Table 2. Both treatments were described in layman's terms. The descriptions did not explicitly state the name of the particular type of treatment. After the participants read the description, they were given the choice as to whether they wanted treatment ‘A' or treatment ‘B'. They were also asked to estimate their preference strength by answering the question ‘How important is this choice for you?’ on a scale of one to four, where one was ‘not at all important’, and four was ‘very important’. This constituted the study's preference strength measure.
Table 2.
Descriptions of the two treatments provided to participants.
| Treatment A (Internet-delivered Cognitive Behavioural Therapy) | Treatment B (Internet-delivered psychodynamic therapy) |
|---|---|
| This treatment assumes that social phobia should be understood as a phobia for certain social situations and the reactions that these situations cause. Previous negative experiences from social situations mean that you associate these with unpleasant experiences that you prefer to avoid. This avoidance in the short term causes the anxiety to decrease, but in the longer term the avoidance causes the social anxiety to worsen. The central focus of treatment is to gradually and at one's own pace approach anxiety-laden situations in order to respond to them in new, alternative ways. For example, it may be about staying in the situation and trying to accept the discomfort, confronting and getting used to the emotions that arise or to investigate and challenge the negative thoughts associated with the situation. Some examples of such situations may be small talk with colleagues at work, asking a question during a workplace meeting or giving a short presentation. Many people with social phobia suffer through social situations and it can therefore be difficult to understand why the feelings do not change over time. According to this treatment, it is because different parts of the situation are avoided by, for example, looking down into the ground or thinking of something completely different. Such “safety behaviors” make the situation easier to deal with at the moment but the problems remain in the long term. The avoidance and the negative thoughts together lead to an increased self-focus, which becomes a vicious circle where the symptoms worsen. The treatment begins with an in-depth presentation of the diagnosis and treatment arrangement. Then you begin to map thoughts and interpretations before moving on to look at different types of thought traps. You then begin to systematically challenge negative thoughts through different types of thought and behavior experiments. After working with the thoughts, in small steps you begin to expose yourself to the difficult situations, through so-called exposure. Then you put the reasoning about thoughts, feelings and behavior together into a whole where you practice to break the vicious self-focusing circle and continue to do exposure. In the last stage, one exercises various social skills such as setting boundaries and active listening. |
This treatment assumes that social phobia should be understood as a phobia for certain emotional reactions. Experiences we have had in relation to our caregivers and other important people at an early age have taught us to avoid certain types of feelings, such as anger, sadness, joy or interest - and it is this avoidance that causes social anxiety. The central focus of the treatment is to learn to approach one's feelings gradually and in the long term to stay with them and to welcome them, despite the fact that they are often unpleasant. The treatment is based on the premise that closer contact with our emotions lead us to feel more secure and content with ourselves. Sometimes the emotions can be difficult to understand or accept, and then they can lead to internal conflicts that cause discomforting reactions. These reactions to the emotions sometimes lead to anxiety and other symptoms, and during treatment you will look more closely at these reactions. At the heart of treatment's understanding of emotions is that they are associated with important people in our lives, and by developing a deeper understanding of these connections, it becomes easier to approach the emotions. Since people with social phobia are often very self-critical and feel a lot of shame, the treatment also focuses on treating oneself more kindly and with greater compassion. The treatment is divided into four steps. The first step is to become aware of feelings and to begin to be consciously present with them without changing them or fleeing from them. The second step is to deal with the anxiety that arises as we approach our emotions, and you will learn different tools to do so. The third step is a deepening of step one as one tries to delve even deeper into the emotions in all their complexity. The fourth step is to listen to one's feelings and then share them with others. Here you will learn different tools for communicating with others in a conscious and present way. |
2.4.2. Treatment and therapists
Each treatment consisted of nine chapters of text with associated homework assignments in accordance with the guided self-help model (Andersson, 2016). All contact between the participants and the therapists took place via a secure Internet platform, where double authentication was required to log in. In addition to providing the treatment material, this platform fulfilled the function of a secure mail service where therapists could provide feedback on participants' homework assignment on a weekly basis. It also enabled the weekly measurements to take place in a secure manner. In the current study, the therapists were given the general guideline of spending 15 min per patient per week.
The ICBT treatment was a version of the SOFIE treatment (for details see Furmark et al., 2013). The ICBT treatment is based on a model of SAD by Clark and Wells (1995) as well as Heimberg's model for SAD (Heimberg and Becker, 2002). The SOFIE ICBT treatment has been tested in several controlled trials (Andersson et al., 2014), including effectiveness studies (e.g. El Alaoui et al., 2015).
The psychodynamic IPDT treatment was a Swedish translation and adaption of the self-help book Living Like You Mean It (Frederick, 2009), originally translated for a transdiagnostic trial on mixed anxiety and depression (Johansson et al., 2013a). The book broadly follows the original manual for affect-focused treatment (McCullough et al., 2003). The treatment also included homework assignments at the end of each chapter to enhance participants' ability to learn and generalize the material (Johansson et al., 2013b; Johansson et al., 2017). A more detailed description of the treatment can be found in Johansson et al. (2017).
Regarding the content and purpose of therapist feedback, the focus in both treatments was to make sure that the participants completed each week's homework assignment, give encouragement and validation, as well as provide additional clarifications when needed. The role of the therapist and the therapist feedback could thus be considered more similar than different across the two treatments (Johansson et al., 2013b).
The study had seven therapists, four in the IPDT arm and three in the ICBT arm. All were master's degree-level psychology students. The four students in the IPDT arm had previous experience of working with psychodynamic therapy and the three students in the ICBT arm had previous experience of working with CBT. None of the therapists had had previous experience of guided self-help via the Internet. The therapists did not receive any systematic preparation for the study but were primarily encouraged to study the treatment manuals on their own. All therapists received supervision on four occasions with clinicians with extensive experience of the two respective treatments. The therapists did not receive any monetary compensation for their participation in the study.
2.5. Measures
Throughout the course of the study, a total of nine measurement instruments were administered. Participants were required to fill out the Liebowitz Social Anxiety Scale – Self Report (LSAS-SR), which was the primary outcome measure, on a weekly basis. The post-baseline/pre-treatment, post-treatment and follow-up assessments also included the Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder Screener (GAD-7), Inventory of Interpersonal Problems (IIP-64) and Clinical Global Impression (CGI). In addition, the Working Alliance Inventory (WAI-S) was administered on three occasions – pre-treatment, three weeks after treatment start and post-treatment.
2.5.1. Primary outcome measure
To measure symptoms of social anxiety, the LSAS-SR self-assessment instrument was used (Baker et al., 2002). It consists of 24 items where, based on the previous week, the participant is asked to estimate the degree of perceived fear and avoidance in situations involving either social interaction or achievement (Baker et al., 2002). LSAS-SR has shown good psychometric properties, with a test-retest reliability of r = 0.83, an internal consistency of α = 0.79 or higher and satisfactory change sensitivity (Baker et al., 2002). Similar psychometric properties have also been shown when administered over the Internet (Hedman et al., 2010).
2.5.2. Secondary outcome measures
To detect and assess depression severity, the self-assessment instrument PHQ-9 was used. The instrument consists of nine statements based on DSM-IV depression criteria (Kroenke et al., 2001). PHQ-9 exhibits a test-retest reliability of r = 0.84 and an internal consistency of Cronbach's α = 0.86–0.89 (Kroenke et al., 2001). PHQ-9 exhibits good sensitivity and specificity for detecting and assessing the severity of depression and is a well-validated instrument (Kroenke et al., 2010; Titov et al., 2011).
As a secondary anxiety measure, the GAD-7 (Spitzer et al., 2006) was used. The GAD-7 is a self-assessment instrument consisting of a total of eight questions based on the diagnostic criteria for generalized anxiety disorder according to DSM-IV (Spitzer et al., 2006). The test shows an internal consistency of Cronbach's α = 0.92 and a test-retest reliability of r = 0.83 (Spitzer et al., 2006). Furthermore, the instrument has been shown to have good properties for measuring treatment effects during ongoing treatment (Dear et al., 2011).
The WAI-S is an instrument intended to measure working alliance through 12 items divided into three sub-scales of task, goals and bond (Horvath and Greenberg, 1989; Tracey and Kokotovic, 1989). In the present study, a version of the form specifically adapted for guided Internet-based treatment was used (Bergman Nordgren et al., 2013). A minor linguistic adjustment of this instrument was made for the current study. WAI-S exhibits an internal consistency for sub-scales and a total score of Cronbach's α between 0.95 and 0.91 (Busseri and Tyler, 2003). WAI-S correlates highly with the longer original version regarding psychometric and predictive properties, and the two are thus interchangeable (Busseri and Tyler, 2003).
The M.I.N.I. is a brief, structured diagnostic interview for psychiatric diagnoses in accordance with DSM-IV and ICD-10 (Lecrubier et al., 1997). The instrument can be used by non-specialized interviewers after practice and administered over a short period of time and can therefore be seen as a good alternative to other diagnostic instruments such as SCID-P and CIDI, which have longer administration times (Lecrubier et al., 1997; Sheehan et al., 1997). The instrument exhibits an inter-rater reliability with kappa values between 0.88 and 1.0 and A test-retest reliability of 0.75 (Lecrubier et al., 1997; Sheehan et al., 1997).
The CGI is an instrument used to assess the extent to which improvement has occurred (Guy, 1976). The instrument comprises three sub-scales; severity of illness, global impression and efficacy index. In the present study, only global impression was used, which is intended to measure the degree to which the participant has improved or deteriorated since the start of the study. This is stated on a seven-degree scale from −3 (very much deteriorated) to +3 (very much improved). In the present study, the CGI was administered through a telephone interview in conjunction with the pre- and post-treatment assessments, by master-level psychology students that were not blind to treatment allocation.
Finally, the IIP-64 is designed to measure the severity of interpersonal problems (Horowitz et al., 1988). The instrument consists of 64 statements that measure eight domains of interpersonal problems, including domineering, vindictive, cold, socially avoidant, non-assertive, exploitable, overly nurturant and intrusive (Weinryb et al., 1996). Regarding psychometric properties, the scale has shown an internal consistency between Cronbach's α = 0.67 and 0.84 and a test-retest reliability between 0.80 and 0.90 (Horowitz et al., 1988; Weinryb et al., 1996).
2.6. Data analytic approach
All descriptive statistics were calculated using SPSS version 24. For the analysis of the main treatment effect, a piecewise latent growth curve model was used. This type of model was used to model the baseline period, when the participants were waiting for treatment, and the treatment period as two distinct phases but in the same model (Hesser, 2015). In addition, the latent growth curve model allows for the modelling of individual differences in rate of change as well as initial symptom levels while also taking into account the non-independence of observations in repeated measures over time, making this approach well-suited to the analysis of longitudinal data (Hesser, 2015; Wang and Wang, 2012). The Wald test was used to test for the significance of the individual random and fixed effects variables as well as the covariation of the random effects. All calculations were carried out using Mplus version 8.1 (Muthén and Muthén, 2017).
For the secondary outcome measures, as well as to test for any difference in the primary outcome measure at follow-up, regression for continuous outcome variables was estimated using maximum likelihood. Similar to an ANCOVA analysis, the pre-treatment value of the respective outcome measure was used as a predictor in the analysis to control for any pre-treatment differences (Muthén et al., 2016).
The analyses made use of all available data through the use of full information maximum likelihood estimation, thereby making them full intention-to-treat analyses. Hence, the analyses rested on the assumption of Missing at Random (MAR), which means that the probability of missing data could be dependent on any observed variable but not on the would-be value of the missing data point (Schafer and Graham, 2002).
For the latent growth model, Cohen's d between-group effect sizes were calculated by dividing the estimated differences in change scores between the two groups with the square root of the sum of the residual plus the estimate of the random intercept at pre-treatment (Feingold, 2009). For the regression model used for the secondary outcome measures as well as to test for post-treatment to follow-up differences, between-group effect sizes were calculated based on model-estimated means and variances divided with the standard deviation at pre-treatment. Within-group effect sizes were estimated based on differences in observed means and pooled standard deviations between pre- and post-treatment as well as post-treatment and follow-up.
Finally, treatment remission was defined as a raw score below or equal to 30 on the LSAS-SR, in accordance with previous research (Doyle and Pollack, 2002; Leichsenring et al., 2013).
3. Results
3.1. Treatment preference
Twenty-three of the participants chose IPDT (63.9%), and 13 chose ICBT (36.1%). A one-sample chi-squared test revealed that difference was not statistically significant, χ2 (1) = 2.79, p = .10, Cramer's V = 0.28, a small effect size.
3.2. Attrition and adherence
Thirty-three of the 36 participants (92%) completed the post-treatment assessment, with one missing from the ICBT group and two from the IPDT group. For the follow-up assessment, data were obtained from 25 participants (69%), with four participants missing in the ICBT group and seven in the IPDT group. In total, data were missing from 93 of the 864 unique measurement occasions (11%).
Regarding treatment adherence, a module was considered to be completed if the participant had done the module's corresponding homework assignments and sent answers about the exercises to his or her therapist. In the IPDT group, the participants had completed on average 80% of the modules when the treatment ended after 10 weeks, while the participants in the ICBT group had completed 59% of the modules. An independent t-test showed that this difference was not statistically significant, t(34) = 1.82, p = .08. In the IPDT group, 15 of the 23 participants (65.2%) completed all nine modules, while 3 of the 13 participants (23.1%) completed all modules in the ICBT group. Two of the participants did not complete any of the modules, one from each group. A chi-squared (χ2) test showed that there was a significant difference between the proportion of participants who completed all modules in the different groups, χ2 (1) = 5.90, p = .02. Thus, participants in the IPDT group completed the treatment to a greater extent than those in the ICBT group, thereby obtaining a larger treatment dose. However, treatment adherence was not related to change on the LSAS-SR, r = −0.103, p = .57.
3.3. Analysis of treatment effects
Observed means, standard deviations and Ns as well as within-group effect sizes for all primary and secondary outcome measures can be found in Table 3.
Table 3.
Means, standard deviations, Ns and within-group effect sizes for continuous primary and secondary outcome measures throughout the study.
| Measure | ICBT |
IPDT |
Cohen's D Within-group effect size [95% CI] |
||||
|---|---|---|---|---|---|---|---|
| M (SD) | N | M (SD) | N | Period | ICBT | IPDT | |
| LSAS-SR | |||||||
| Pre-baseline | 62.46 (15.46) | 13 | 63.70 (17.95) | 23 | – | – | – |
| Pre-treatment | 62.69 (26.28) | 13 | 50.74 (21.45) | 23 | Pre-baseline to pre-treatment | −0.1 [−0.78, 0.76] | 0.66 [0.05, 1.24] |
| Post-treatment | 50.25 (19.99) | 12 | 42.14 (21.64) | 21 | Pre-treatment to post-treatment | 0.53 [−0.29, 1.31] | 0.40 [−0.21, 0.99] |
| Follow-up | 44.22 (25.46) | 9 | 34.0 (20.19) | 16 | Post-treatment to follow-up | 0.27 [−0.61, 1.13] | 0.39 [−0.28, 1.03] |
| PHQ-9 | |||||||
| Pre-treatment | 9.08 (7.29) | 13 | 8.52 (6.18) | 23 | – | – | – |
| Post-treatment | 4.25 (4.62) | 12 | 4.19 (4.50) | 21 | Pre-treatment to post-treatment | 0.78 [−0.05, 1.57] | 0.80 [0.17, 1.39] |
| Follow-up | 4.44 (1.67) | 9 | 4.69 (3.57) | 16 | Post-treatment to follow-up | −0.05 [−0.91, 0.81] | −0.12 [−0.77, 0.53] |
| GAD-7 | |||||||
| Pre-treatment | 7.54 (6.09) | 13 | 6.70 (5.30) | 23 | – | – | – |
| Post-treatment | 5.50 (4.83) | 12 | 4.05 (4.84) | 21 | Pre-treatment to post-treatment | 0.37 [−0.43, 1.15] | 0.52 [−0.09, 1.11] |
| Follow-up | 5.44 (3.68) | 9 | 4.06 (4.80) | 16 | Post-treatment to follow-up | 0.01 [−0.85, 0.88] | 0.00 [−0.65, 0.65] |
| IIP-64 | |||||||
| Pre-treatment | 44.69 (19.04) | 13 | 42.91 (18.34) | 23 | – | – | – |
| Post-treatment | 36.17 (14.29) | 12 | 39.76 (18.78) | 21 | Pre-treatment to post-treatment | 0.50 [−0.31, 1.28] | 0.17 [−0.43, 0.76] |
| Follow-up | 80.22 (29.63) | 9 | 72.56 (39.92) | 16 | Post-treatment to follow-up | −1.99 [−2.95, −0.87] | −1.10 [−1.77, −0.38] |
3.3.1. Main outcome measures
The results from the random effects repeated measures piecewise growth model revealed significant individual variability in initial symptom level (intercept) as well as rate of change (slope) during both the baseline period and the treatment period for the LSAS-SR. There was a significant covariance between the random intercept and the random slope for the treatment period, −11.5 95% CI [−22.69, −0.32], z = −2.02, p = .04, showing that participants with higher symptoms on the LSAS-SR at the beginning of the study improved faster during the treatment period.
For the baseline period when the participants were waiting for treatment, a latent growth model showed that the ICBT group did not improve significantly on the LSAS-SR during this period, 0.07 95% CI [−0.6, 0.8], z = 0.22, p = .82. The IPDT group improved on average 0.7 points more per week as compared to the ICBT group, −0.70 95% CI [−1.49, 0.08], z = −1.75, p = .08, however this difference was not statistically significant. The between-group effect was calculated to Cohen's d = 0.34 95% CI [−0.05, 0.72], a small effect size in favour of the IPDT group.
For the treatment period, a latent growth model showed that the ICBT group improved on average 1.19 points per week during this period on the LSAS-SR, −1.19 95% CI [−2.04, −0.34], z = −2.76, p = .006, and that the IPDT group did not differ significantly from the ICBT group, 0.46 95% CI [−0.61, 1.53], z = −0.84, p = .40, thus indicating that the two treatment groups did not differ significantly in their rate of change during this period. The between-group effect was Cohen's d = 0.22 95% CI [−0.30, 0.74], which is a small effect size, in favour of the ICBT group.
At follow-up, a regression model revealed that no significant difference existed between the two groups, b = −0.1, p = .54. The between-group effect size was calculated to Cohen's d = 0.18 95% CI [−0.41, 0.77], again a small effect size, but at this point in favour of the IPDT group.
3.3.2. Secondary outcome measures
For the PHQ-9, a regression model showed that there was no significant difference between the two groups at either post-treatment, b = −0.02, p = .85, or at follow-up, b = −0.07, p = .66. The between-group effect at post-treatment was calculated to Cohen's d = 0.04 95% CI [−0.34, 0.41], in favour of the IPDT group, and Cohen's d = 0.06 95% CI [−0.22, 0.35] at follow-up, in favour of the ICBT group.
For the GAD-7, a regression model showed that there were no significant differences between the two groups at either post-treatment, b = −0.13, p = .41, or at follow-up, b = −0.13, p = .51. The between-group effect at post-treatment was Cohen's d = 0.24 95% CI [−0.34, 0.81] and Cohen's d = 0.20 95% CI [−0.37, 0.78] at follow-up, both in favour of the IPDT group.
For the IIP-64, a regression model showed that there were no significant differences between the two groups at either post-treatment, b = 0.06, p = .56, or at follow-up, b = −0.17, p = .15. The between-group effect at post-treatment was Cohen's d = 0.12 95% CI [−0.27, 0.51], in favour of the ICBT group, and Cohen's d = 0.70 95% CI [−0.26, 1.66] at follow-up, in favour of the IPDT group.
Finally, with regards to the CGI—I, due to the small sample size we decided to reduce the number of categories from seven (−3, −2, −1, 0, 1, 2, 3) to two (deteriorated/not improved, improved). Eleven of the 13 (85%) participants in the ICBT group had improved following treatment compared to 17 of the 23 (74%) participants in the IPDT group. A chi-squared test corrected with Fisher's exact test due to the small sample size showed that this difference was not significant, χ2 (1) = 0.55, p = .68.
3.4. Predictor analysis
3.4.1. Preference strength
The mean preference strength was 2.77 (SD = 0.60) for the participants in the ICBT group and 3.09 (SD = 0.73) for the participants in the IPDT group. An independent t-test revealed that the preference strength did not differ significantly between the two groups, t(34) = 1.33, p = .19. Adding preference strength as a predictor of the change rate during the treatment period in the piecewise growth model revealed that preference strength did not significantly predict treatment effectiveness, z = −0.56, p = .57, and was thus removed from the final piecewise growth model. With regards to treatment adherence, preference strength did not correlate significantly with number of completed modules, r = 0.18, p = .30. Finally, we found that preference strength and treatment completion was not significantly correlated, r = 0.28, p = .09.
3.4.2. Working alliance
An unconditional latent growth curve model of participant working alliance during the treatment period revealed a significant effect of time, 0.74 95% CI [0.22, 1.27], z = 2.77, p = .006, meaning that the participants' working alliance improved 0.74 points on average per week. The treatment group did not significantly predict change in working alliance, 0.48 95% CI [−0.59, 1.54], z = 0.88, p = .38; however, there was a significant covariance between the random intercept and the random slope, −7.29 95% CI [−13.90, −0.68], z = −2.74, p = .006, showing that participants who started lower on the WAI had a steeper increase during the treatment period. Adding working alliance measured at week three as a predictor of the change rate during the treatment period in the piecewise growth model revealed a significant relationship between the two, −0.05 95% CI [−0.072, −0.018], z = −3.22, p = .001, indicating that a higher working alliance at week three was related to having a faster decline in symptoms during the treatment period.
3.5. Remission and adverse events
Following the baseline period, four participants had recovered to a level of LSAS-SR below or equal to 30 raw points, three in the IPDT group (13%) and one in the ICBT group (8%). After treatment, no additional participant in the ICBT group had recovered (8%), while in the IPDT group seven of the participants had recovered (30%). A chi-squared test corrected with Fisher's exact test showed that the difference between the groups after treatment was not statistically significant, χ2 (1) = 2.90, p = .21, with the odds ratio (OR) = 5.25, 95% CI [0.57–48.58].
At follow-up, two of the ICBT participants and eight of the IPDT participants had recovered (15% and 35%, respectively). A chi-squared test corrected with Fisher's exact test showed that this difference was not significant, χ2 (1) = 1.57, p = .27, OR = 2.93, 95% CI [0.52–16.61].
With regards to adverse events (cf., Rozental et al., 2018), one (4%) of the participants in the IPDT group was classified as having significant deterioration according to the CGI. In addition, two of the participants in the ICBT group reported that they did not recognize themselves in the CBT description of social phobia.
4. Discussion
To our knowledge, this pilot study is the first study to examine preference for IPDT versus ICBT in the treatment of SAD. First, we found that IPDT was descriptively preferred more often than ICBT, which is different from a similar previous preference study on depression (Johansson et al., 2013c). However, the difference did not reach statistical significance in this sample. Secondly, contrary to our hypothesis, we did not find preference strength to significantly predict either treatment outcome or adherence. We did however, find a significant association between alliance ratings at week three and treatment outcome. The study also showed that both treatments had small to moderate effects on social anxiety, depression, generalized anxiety and interpersonal problems at post-treatment and that effects were maintained or improved at six months follow-up. With regards to remission, 35% of participants in the IPDT group had remitted at follow-up compared to 15% in the ICBT group. The differences between the treatments were small and non-significant which is in line with the overall research literature on outcomes of bona-fide therapies. Still, given that the participants were not randomized to treatment, and it is likely that the preference matching introduced systematic differences between the two groups, it is not possible to draw inferences regarding any differences between the two treatments. Also, the study was not powered to detect between-group differences. Furthermore, we found that participants in the IPDT group completed treatment modules to a significantly greater extent than those in the ICBT group, thereby receiving a larger treatment dose, although this proved unrelated to outcome.
The observed within-group effect sizes for the treatment period (ICBT d = 0.53; IPDT d = 0.40) were lower than what has been observed in most Internet-based studies on SAD (Andersson et al., 2012a; Carlbring et al., 2007; Johansson et al., 2017; Tillfors et al., 2011). A similar phenomenon was observed in the IPDT study of depression, where the RCT study showed an effect size that was twice as high as in the subsequent treatment of the control group by preference matching (Johansson et al., 2013c). The results also need to be interpreted in light of the fact that the participants in the IPDT group had a small, non-significant, improvement on social anxiety symptoms compared to the participants in the ICBT group during the baseline period while waiting for treatment. This finding is in line with previous research demonstrating a small decrease in symptoms for wait-list control groups in randomized controlled trials for social anxiety disorder (Steinert et al., 2017). However, it is unclear why this applied only to participants who subsequently choose IPDT. In addition, natural recovery and regression towards the mean cannot be excluded as explanations.
Regarding the predictor analysis, we found a small to moderate positive correlation of r = 0.28 between preference strength and completion of all treatment modules. The result was not statistically significant, however this could be due to lack of power. This finding is in line with the study by Johansson et al. (2013c), where they also found a non-significant correlation of similar strength between preference strength and completion of all treatment modules. This might indicate that both studies were underpowered to detect this relationship. No relationship was found between preferences strength and either adherence or improvement in social anxiety symptoms. Thus, the present study largely failed to confirm previous findings of a significant relationship between preference strength and treatment adherence and outcome (Moradveisi et al., 2014; Raue et al., 2009). With regards to the effect of the preference matching itself, this was not possible to examine with the present study design given that every participant got the treatment of their choice. However, a recent study by Leuzinger-Bohleber et al. (2019) found no difference in outcome between preferential and randomized allocation to CBT and long-term psychoanalytic therapy. Furthermore, we also found that alliance ratings at week three by participants predicted better treatment response regarding social anxiety symptoms. As stated earlier, while some previous research on Internet-based treatment has failed to show a consistent relationship (Andersson et al., 2018), the most recent meta-analysis found a similar effect as in face-to-face trials (Probst et al., in press), in line with the findings of the present study.
Concerning treatment adherence, participants in the present study completed on average 5.3 modules (59% of the modules) in the ICBT group, while the average participant in the IPDT group completed 7.2 modules (80%). These findings are in line with previous studies on the SOFIE manual, where participants had completed between 2.9 (32%) and 7.5 (83%) modules by the end of treatment (Andersson et al., 2006; Boettcher et al., 2014a; Carlbring et al., 2006; Tillfors et al., 2011). This is also in line with the other studies conducted on IPDT where participants completed between 5.9 (74%) to 7.73 (86%) of the modules (Andersson et al., 2012b; Johansson et al., 2013a; Johansson et al., 2012; Johansson et al., 2013c). The 65% treatment completion rate for the IPDT group is also very similar to the 69% completion rate found in the Johansson et al. (2017) study.
It is worth mentioning that both treatment groups showed a deterioration on the IIP-64 at the six-month follow-up relative to post-treatment. To our knowledge, this has not been reported in previous research on Internet-based treatments, where transient side effects have been observed for individual participants but not at the group level (Boettcher et al., 2014b). Given the often longstanding nature of anxiety disorders, the recurrence of symtoms and also interpersonal problems that may occur as a consequence of getting better cannot be excluded as explanations for this finding. Regardless, possible deterioration and/or the negative effects of treatments on secondary outcomes such as interpersonal functioning should be followed up more rigorously in future studies on the negative effects of Internet-based treatments (Rozental et al., 2014).
With regards to the limitations of the present study, one is that the description of the two treatments were very brief, where a longer description or even access to the treatment material would have made it easier for the participants to make a better-informed decision. Related to this, it is also possible that some participants could have interpreted the question on the importance of the choice of treatment in some way other than what was intended. For instance, participants could have rated the choice as important since it made them eligible to start treatment, rather than the choice itself being important. A second limitation concerns the fact that no diagnostic interviews were conducted at the post-treatment assessment, which means that there is no way of knowing the extent to which the participants meet diagnostic criteria for SAD after the treatment. A third limitation concerns the small sample size, with an observed power of 19% for the difference between the two treatments on the LSAS-SR at post-treatment. The same problem with power also applied for the predictor analysis. Overall, the low power increases the risk type II error (i.e. concluding that there is no effect when there in reality is one) in respect to all outcomes. With regards to the risk of type I error when testing multiple outcomes, we overall considered this to be a minor issue given the exploratory nature of the present study and since we had specified a primary outcome, however this explanation cannot be completely ruled out in regards to the significant findings in the present study. A fourth limitation concerns the non-randomized design which makes it impossible to draw any inferences regarding the differential effect of the two treatments. A fifth limitation concerns the fact that the master-level psychology students who rated CGI at post-treatment were aware of treatment allocation which might have biased this assessment in some way. Finally, another limitation concerns the fact that competence and fidelity to the treatment manual on part of the therapists were not systematically investigated.
With regards to the strengths of the present study, it deserves mentioning that this is the first study to our knowledge that examines the preference for IPDT and ICBT in the treatment of SAD.
Regarding clinical implications of the present study, it seems like both IPDT and ICBT could be acceptable treatment options for patients with SAD. However, the strength of the preference does not in itself seem to predict how well a person will respond to that particular treatment, although it might be related to treatment completion. Also, the therapeutic alliance seems to be an important predictor of outcome in internet-based treatment of SAD and thus might be important to attend to.
5. Conclusion
The present study did not find a difference in preference for IPDT or ICBT in the treatment of SAD. The study also does not lend support to preference strength as a predictor of symptom reduction; however, there is some indication that it might be useful in predicting treatment module completion. Furthermore, treatment alliance measured at week three predicted treatment outcome. Moreover, both treatments had small to moderate effects on social anxiety depression, generalized anxiety and interpersonal problems, with the caveat that the study design itself does not preclude systematic pre-treatment differences between the two groups. Also, due to the low sample size, all of the above-mentioned conclusions must be regarded as highly tentative and in need of further replication.
Declaration of competing interest
The Internet intervention under study is not commercially available and the authors hold no financial interest or other conflict of interest.
Acknowledgements
We thank our co-workers in the original trial. This study was sponsored in part with a professor's grant to the last author from Linköping University. We also want to thank the following individuals who helped with the interviews and acted as therapists in the study: Stefan Deak, Linnea Klintberg, Sophia Bongiorno, Jacob Bryntesson, Tove Ringmar, Lisa Ekelund, Eva Berglund, Glenn Kristoffersson, Katarina Ernborg, Sofie Lind, Matilda Bergman and Amanda Hultling.
References
- American Psychiatric Association . 5th ed. American Psychiatric Association; Washington, D.C: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Andersson G. Internet-delivered psychological treatments. Annu. Rev. Clin. Psychol. 2016;12:157–179. doi: 10.1146/annurev-clinpsy-021815-093006. [DOI] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Holmström A., Sparthan E., Furmark T., Nilsson-Ihrfelt E., Buhrman M., Ekselius L. Internet-based self-help with therapist feedback and in-vivo group exposure for social phobia: a randomized controlled trial. J. Consult. Clin. Psychol. 2006;74:677–686. doi: 10.1037/0022-006X.74.4.677. [DOI] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Furmark T., on behalf of the SOFIE Research Group Therapist experience and knowledge acquisition in Internet-delivered CBT for social anxiety disorder: a randomized controlled trial. PLoS One. 2012;7(5) doi: 10.1371/journal.pone.0037411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Paxling B., Roch-Norlund P., Östman G., Norgren A., Almlöv J., Georén L., Breitholtz E., Dahlin M., Cuijpers P., Carlbring P., Silverberg F. Internet-based psychodynamic vs. cognitive behavioural guided self-help for generalized anxiety disorder: a randomised controlled trial. Psychother. Psychosom. 2012;81:344–355. doi: 10.1159/000339371. [DOI] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Furmark T. Internet-delivered treatments for social anxiety disorder. In: Weeks J., editor. Handbook of Social Anxiety Disorder. Wiley-Blackwell; New York: 2014. pp. 569–587. [Google Scholar]
- Andersson G., Titov N., Dear B.F., Rozental A., Carlbring P. Internet-delivered psychological treatments: from innovation to implementation. World Psychiatry. 2018;18:20–28. doi: 10.1002/wps.20610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker S.L., Heinrichs N., Kim H.J., Hofmann S.G. The Liebowitz Social Anxiety Scale as a self-report instrument: a preliminary psychometric analysis. Behav. Res. Ther. 2002;40:701–715. doi: 10.1016/s0005-7967(01)00060-2. [DOI] [PubMed] [Google Scholar]
- Bergman Nordgren L., Carlbring P., Linna E., Andersson G. Role of the working alliance on treatment outcome in tailored internet-based cognitive behavioural therapy for anxiety disorders: randomized controlled pilot trial. JMIR Research Protocols. 2013;2:e4. doi: 10.2196/resprot.2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boettcher J., Hasselrot J., Sund E., Andersson G., Carlbring P. Combining attention training with Internet-based cognitive-behavioural self-help for social anxiety: a randomized controlled trial. Cogn. Behav. Ther. 2014;43:34–48. doi: 10.1080/16506073.2013.809141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boettcher J., Rozental A., Andersson G., Carlbring P. Side effects in internet-based interventions for social anxiety disorder. Internet Interv. 2014;1:3–11. [Google Scholar]
- Bögels S.M., Wijts P., Oort F.J., Sallaerts S.J. Psychodynamic psychotherapy versus cognitive behavior therapy for social anxiety disorder: an efficacy and partial effectiveness trial. Depression and Anxiety. 2014;31:363–373. doi: 10.1002/da.22246. [DOI] [PubMed] [Google Scholar]
- Busseri M.A., Tyler J.D. Interchangeability of the Working Alliance Inventory and Working Alliance Inventory, short form. Psychol. Assess. 2003;15:193–197. doi: 10.1037/1040-3590.15.2.193. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Furmark T., Steczkó J., Ekselius L., Andersson G. An open study of Internet-based bibliotherapy with minimal therapist contact via e-mail for social phobia. Clin. Psychol. 2006;10:30–38. [Google Scholar]
- Carlbring P., Gunnarsdóttir M., Hedensjö L., Andersson G., Ekselius L., Furmark T. Treatment of social phobia: randomized trial of internet delivered cognitive behaviour therapy and telephone support. Br. J. Psychiatry. 2007;190:123–128. doi: 10.1192/bjp.bp.105.020107. [DOI] [PubMed] [Google Scholar]
- Clark D.M., Wells A. A cognitive model of social phobia. In: Heimberg R.G., Liebowitz M.R., Hope D.A., Schneier F.R., editors. Social Phobia: Diagnosis, Assessment, and Treatment. Guilford Press; New York, NY, US: 1995. pp. 69–93. [Google Scholar]
- Cuijpers, P., Sijbrandij, M., Koole, S. L., Andersson, G., Beekman, A. T., & Reynolds III, C. F. (2013). The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry, 12, 137–148. doi: 10.1002/wps.20038. [DOI] [PMC free article] [PubMed]
- Dear B.F., Titov N., Sunderland M., McMillan D., Anderson T., Lorian C., Robinson E. Psychometric comparison of the generalized anxiety disorder scale-7 and the Penn State Worry Questionnaire for measuring response during treatment of generalised anxiety disorder. Cogn. Behav. Ther. 2011;40:216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- Doyle A.C., Pollack M.H. Establishment of remission criteria for anxiety disorders. J. Clin. Psychiatry. 2002;64(Suppl 15):40–45. [PubMed] [Google Scholar]
- El Alaoui S., Hedman E., Kaldo V., Hesser H., Kraepelien M., Andersson E., Rück C., Andersson G., Ljótsson B., Lindefors N. Effectiveness of internet-based cognitive behavior therapy for social anxiety disorder in clinical psychiatry. J. Consult. Clin. Psychol. 2015;83:902–914. doi: 10.1037/a0039198. [DOI] [PubMed] [Google Scholar]
- Faria V., Gingnell M., Hoppe J.M., Hjorth O., Alaie I., Frick A., Hultberg S., Wahlstedt K., Engman J., Månsson K.N.T., Carlbring P., Andersson G., Reis M., Larsson E.-M., Fredrikson M., Furmark T. Do you believe it? Verbal suggestions influence the clinical and neural effects of escitalopram in social anxiety disorder: a randomized trial. EBioMedicine. 2017;24(Supplement C):179–188. doi: 10.1016/j.ebiom.2017.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehm L., Pelissolo A., Furmark T., Wittchen H.U. Size and burden of social phobia in Europe. Eur. Neuropsychopharmacol. 2005;15:453–462. doi: 10.1016/j.euroneuro.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol. Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frederick R.J. John Wiley & Sons; 2009. Living Like You Mean It: Use the Wisdom and Power of Your Emotions to Get the Life You Really Want. [Google Scholar]
- Furmark T., Holmström A., Sparthan E., Carlbring P., Andersson G. 2 ed. Liber; Stockholm: 2013. Social fobi - Effektiv hjälp med kognitiv beteendeterapi [Social Phobia - Effective Help Via CBT] [Google Scholar]
- Goldstein-Piekarski A.N., Williams L.M., Humphreys K. A trans-diagnostic review of anxiety disorder comorbidity and the impact of multiple exclusion criteria on studying clinical outcomes in anxiety disorders. Transl. Psychiatry. 2016;6:e847. doi: 10.1038/tp.2016.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B.F., Stinson F.S., Hasin D.S., Dawson D.A., Chou S.P., Ruan W.J., Huang B. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the National Epidemiologic Survey on alcohol and related conditions. J. Clin. Psychiatry. 2005;66:1205–1215. doi: 10.4088/jcp.v66n1001. [DOI] [PubMed] [Google Scholar]
- Guy W. US Department of Health and Human Services; Rockville: 1976. Clinical Global Impressions. [Google Scholar]
- Hedman E., Ljótsson B., Rück C., Furmark T., Carlbring P., Lindefors N., Andersson G. Internet administration of self-report measures commonly used in research on social anxiety disorder: a psychometric evaluation. Comput. Hum. Behav. 2010;26:736–740. [Google Scholar]
- Heimberg R.G., Becker R.E. Guilford Press; 2002. Cognitive-behavioral Group Therapy for Social Phobia: Basic Mechanisms and Clinical Strategies. [Google Scholar]
- Hesser H. Modeling individual differences in randomized experiments using growth models: recommendations for design, statistical analysis and reporting of results of internet interventions. Internet Interv. 2015;2:110–120. [Google Scholar]
- Horowitz L.M., Rosenberg S.E., Baer B.A., Ureno G., Villasenor V.S. Inventory of interpersonal problems: psychometric properties and clinical applications. J. Consult. Clin. Psychol. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Horvath A.O., Greenberg L.S. The development and validation of the Working Alliance Inventory. J. Couns. Psychol. 1989;36:223–233. [Google Scholar]
- Horvath A.O., Del Re A.C., Fluckiger C., Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48:9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- Johansson R., Ekbladh S., Hebert A., Lindström M., Möller S., Petitt E., Poysti S., Holmqvist-Larsson M., Rousseau A., Carlbring P., Cuijpers P., Andersson G. Psychodynamic guided self-help for adult depression through the Internet: a randomised controlled trial. PLoS One. 2012;7:e38021. doi: 10.1371/journal.pone.0038021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson R., Björklund M., Hornborg C., Karlsson S., Hesser H., Ljótsson B., Rousseau A., Frederick R.J., Andersson G. Affect-focused psychodynamic psychotherapy for depression and anxiety through the Internet: a randomized controlled trial. PeerJ. 2013;1:e102. doi: 10.7717/peerj.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson R., Frederick R.J., Andersson G. Using the Internet to provide psychodynamic psychotherapy. Psychodynamic Psychiatry. 2013;41:385–412. doi: 10.1521/pdps.2013.41.4.513. [DOI] [PubMed] [Google Scholar]
- Johansson R., Nyblom A., Carlbring P., Cuijpers P., Andersson G. Choosing between Internet-based psychodynamic versus cognitive behavioral therapy for depression: a pilot preference study. BMC Psychiatry. 2013;13:268. doi: 10.1186/1471-244X-13-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson R., Hesslow T., Ljotsson B., Jansson A., Jonsson L., Fardig S., Karlsson J., Hesser H., Frederick R.J., Lilliengren P., Carlbring P., Andersson G. Internet-based affect-focused psychodynamic therapy for social anxiety disorder: a randomized controlled trial with 2-year follow-up. Psychotherapy. 2017;54:351–360. doi: 10.1037/pst0000147. [DOI] [PubMed] [Google Scholar]
- Kampmann I.L., Emmelkamp P.M., Morina N. Meta-analysis of technology-assisted interventions for social anxiety disorder. Journal of Anxiety Disorders. 2016;42:71–84. doi: 10.1016/j.janxdis.2016.06.007. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. (doi:jgi01114) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Lowe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen. Hosp. Psychiatry. 2010;32:345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Langer J.K., Rodebaugh T.L. Comorbidity of social anxiety disorder and depression. In: Richards C.S., O’Hara M.W., editors. The Oxford Handbook of Depression and Comorbidity. Oxford University Press; New York, NY: 2014. pp. 111–128. [Google Scholar]
- Lecrubier Y., Sheehan D.V., Weiller E., Amorim P., Bonora I., Harnett Sheehan K., Janavs J., Dunbar G.C. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. European Psychiatry. 1997;12:224–231. [Google Scholar]
- Leichsenring F., Salzer S., Beutel M.E., Herpertz S., Hiller W., Hoyer J., Huesing J., Joraschky P., Nolting B., Poehlmann K., Ritter V., Stangier U., Strauss B., Stuhldreher N., Tefikow S., Teismann T., Willutzki U., Wiltink J., Leibing E. Psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder: a multicenter randomized controlled trial. Am. J. Psychiatr. 2013;170:759–767. doi: 10.1176/appi.ajp.2013.12081125. [DOI] [PubMed] [Google Scholar]
- Leichsenring F., Salzer S., Beutel M.E., Herpertz S., Hiller W., Hoyer J., Huesing J., Joraschky P., Nolting B., Poehlmann K., Ritter V., Stangier U., Strauss B., Tefikow S., Teismann T., Willutzki U., Wiltink J., Leibing E. Long-term outcome of psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder. Am. J. Psychiatr. 2014;171:1074–1082. doi: 10.1176/appi.ajp.2014.13111514. [DOI] [PubMed] [Google Scholar]
- Leuzinger-Bohleber, M., Hautzinger, M., Fiedler, G., Keller, W., Bahrke, U., Kallenbach, L., … Beutel, M. E. (2019). Outcome of psychoanalytic and therapy with chronically depressed patients: a controlled trial with preferential and randomized allocation. Can. J. Psychiatry, 64, 47–58. 10.1177/0706743718780340. [DOI] [PMC free article] [PubMed]
- Liebowitz M.R., Mangano R.M., Bradwejn J., Asnis G. A randomized controlled trial of venlafaxine extended release in generalized social anxiety disorder. J. Clin. Psychiatry. 2005;66:238–247. doi: 10.4088/jcp.v66n0213. [DOI] [PubMed] [Google Scholar]
- Månsson K.N.T., Frick A., Boraxbekk C.-J., Marquand A.F., Williams S.C.R., Carlbring P., Andersson G., Furmark T. Predicting long-term outcome of Internet-delivered cognitive behavior therapy for social anxiety disorder using fMRI and support vector machine learning. Transl. Psychiatry. 2015;5:e530. doi: 10.1038/tp.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo-Wilson E., Dias S., Mavranezouli I., Kew K., Clark D.M., Ades A.E., Pilling S. Psychological and pharmacological interventions for social anxiety disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2014;1:368–376. doi: 10.1016/S2215-0366(14)70329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough L., Kuhn N., Andrews S., Kaplan A., Wolf J., Hurley C.L. xvi. Guilford Press; New York, NY, US: 2003. Treating Affect Phobia: A Manual for Short-Term Dynamic Psychotherapy. [Google Scholar]
- Moradveisi L., Huibers M., Renner F., Arntz A. The influence of patients’ preference/attitude towards psychotherapy and antidepressant medication on the treatment of major depressive disorder. J. Behav. Ther. Exp. Psychiatry. 2014;45:170–177. doi: 10.1016/j.jbtep.2013.10.003. [DOI] [PubMed] [Google Scholar]
- Muthén L.K., Muthén B.O. 8th edition. Muthén & Muthén; Los Angeles, CA: 2017. Mplus User’s Guide. [Google Scholar]
- Muthén B.O., Muthén L.K., Asparouhov T. Muthén & Muthén; Los Angeles, CA: 2016. Regression and Mediation Analysis Using Mplus. [Google Scholar]
- Probst G.H., Berger T., Flückiger C. The alliance-outcome relation in internet-based interventions for psychological disorders: a correlational meta-analysis. Verhaltenstherapie. 2020 (In press) [Google Scholar]
- Raue P.J., Schulberg H.C., Heo M., Klimstra S., Bruce M.L. Patients’ depression treatment preferences and initiation, adherence, and outcome: a randomized primary care study. Psychiatr. Serv. 2009;60:337–343. doi: 10.1176/appi.ps.60.3.337. (doi:10176/ps.2009.60.3.337) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozental A., Andersson G., Boettcher J., Ebert D., Cuijpers P., Knaevelsrud C., Ljótsson B., Kaldo V., Titov N., Carlbring P. Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interv. 2014;1:12–19. [Google Scholar]
- Rozental A., Castonguay L., Dimidjian S., Lambert M., Shafran R., Andersson G., Carlbring P. Negative effects in psychotherapy: commentary and recommendations for future research and clinical practice. BJPsych Open. 2018;4:307–312. doi: 10.1192/bjo.2018.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer J.L., Graham J.W. Missing data: our view of the state of the art. Psychol. Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Sheehan D., Lecrubier Y., Harnett Sheehan K., Janavs J., Weiller E., Keskiner A., Dunbar G. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12:232–241. [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Steinert C., Stadter K., Stark R., Leichsenring F. The effects of waiting for treatment: a meta-analysis of waitlist control groups in randomized controlled trials for social anxiety disorder. Clinical Psychology and Psychotherapy. 2017;24:649–660. doi: 10.1002/cpp.2032. [DOI] [PubMed] [Google Scholar]
- Swift J.K., Callahan J.L., Cooper M., Parkin S.R. The impact of accommodating client preference in psychotherapy: a meta-analysis. J. Clin. Psychol. 2018;74:1924–1937. doi: 10.1002/jclp.22680. [DOI] [PubMed] [Google Scholar]
- Tillfors M., Andersson G., Ekselius L., Furmark T., Lewenhaupt S., Karlsson A., Carlbring P. A randomized trial of Internet delivered treatment for social anxiety disorder in high school students. Cogn. Behav. Ther. 2011;40:147–157. doi: 10.1080/16506073.2011.555486. [DOI] [PubMed] [Google Scholar]
- Tillfors M., Furmark T., Carlbring P., Andersson G. Risk profiles for poor treatment response to internet-delivered CBT in people with social anxiety disorder. Journal of Anxiety Disorders. 2015;33:103–109. doi: 10.1016/j.janxdis.2015.05.007. [DOI] [PubMed] [Google Scholar]
- Titov N., Dear B.F., McMillan D., Anderson T., Zou J., Sunderland M. Psychometric comparison of the PHQ-9 and BDI-II for measuring response during treatment of depression. Cogn. Behav. Ther. 2011;40:126–136. doi: 10.1080/16506073.2010.550059. [DOI] [PubMed] [Google Scholar]
- Tracey T.J., Kokotovic A.M. Factor structure of the Working Alliance Inventory. Psychol. Assess. 1989;1:207–210. [Google Scholar]
- Wang J., Wang X. Wiley; Chichester, West Sussex: 2012. Structural Equation Modeling: Applications Using Mplus. [Google Scholar]
- Weinryb R.M., Gustavsson J.P., Hellström C., Andersson E., Broberg A., Gunnar R. Interpersonal problems and personality characteristics: psychometric studies of the Swedish version of the IIP. Personal. Individ. Differ. 1996;20:13–23. [Google Scholar]