Abstract
A 67-year old female with moderate chronic obstructive pulmonary disease (COPD) and generalized anxiety disorder presents with three episodes of severe hypercapnic respiratory failure over the previous three months without a clear precipitant that were treated with invasive and non-invasive ventilation. These episodes were labelled as acute exacerbations of COPD, however she lacked any typical features or triggers and responded faster than expected to treatment and she underwent extensive investigations to identify an alternative etiology. While admitted and under observation, she became extremely anxious, began to hyperventilate and went into hypercapnic respiratory failure, which was successfully aborted with sublingual lorazepam causing resolution of tachypnea. It became clear that the patient was suffering from panic attacks as the precipitant for her respiratory failure and she was successfully treated with psychiatric medication and breakthrough anxiolytics. Anxiety and panic disorders are more prevalent in patients with COPD than the general population and effective management is important as patient's with anxiety and COPD have worse clinical outcomes than with COPD alone. Additionally, panic attacks should be considered as an etiology for hypercapnic respiratory failure in patients with COPD and anxiety when the clinical presentation is atypical.
1. Introduction
Anxiety disorders are the most prevalent mental disorders in the general population and are even more common amongst patients with COPD with some studies estimating a prevalence of up to 50% [[1], [2], [3]]. Furthermore, the subset of patients with COPD that meet diagnostic criteria for panic disorder (PD), characterized by repeated and unexpected panic attacks, is up to 10-times that of age-adjusted controls [1,4]. According to the DSM-5, panic attacks are defined as an abrupt period of fear or discomfort accompanied by 4 or more of the following 13 symptoms [5];
-
1.
Palpitations, pounding heart or accelerated heart rate
-
2.
Sweating
-
3.
Trembling or shaking
-
4.
Shortness of breath or feeling of smothering
-
5.
Feelings of choking
-
6.
Chest pain or discomfort
-
7.
Nausea or abdominal distress
-
8.
Feeling dizzy, unsteady, lightheaded or faint
-
9.
Chills or heat sensations
-
10.
Paresthesias
-
11.
Derealization or depersonalization
-
12.
Fear of losing control or going crazy
-
13.
Fear of dying
Breathlessness and anxiety are linked by several mechanisms that are relevant to COPD; it has been demonstrated that the subjective feelings of dyspnea are able to induce panic, as well as elevated level carbon dioxide (CO2) in the blood is capable of triggering panic-inducing brainstem reflexes [6,7]. Eisner et al. demonstrate that increased severity of COPD, as measured by the COPD Severity Index and the BODE Index, correlates with an increased frequency of anxiety and as the disease progresses, anxiety may develop over time [8]. After adjusting for variables, Eisner et al. also demonstrates that once anxiety is established in a patient it has a negative impact on their health by measures of submaximal exercise performance, functional limitations and an increased frequency of COPD exacerbations requiring hospitalization [8].
1.1. Case presentation
A 67-year-old female with a diagnosis of chronic obstructive pulmonary disease (COPD) and generalized anxiety disorder (GAD) presents to the emergency department via emergency medical services (EMS) in a coma and is found to be in severe hypercapnic respiratory failure. 45-minutes prior to her presentation she had activated EMS with a chief complaint of chest tightness and dyspnea. This is her third episode of very similar presentations of hypercapnic respiratory failure in the last three months.
The patient's COPD was classified as moderate with a forced expiratory volume over 1-s (FEV1) of 61% of predicted and she was managed with 2L/min of home oxygen, inhaled tiotropium bromide and an inhaled combination of budesonide and formoterol. Her anxiety was managed with 60 mg of duloxetine.
In the early morning, the patient reported experiencing chest tightness and dyspnea and activated EMS. While on the phone with the dispatch officer, she was noted to sound frantic before ceasing communication with the operator. When paramedics arrived several minutes later, they found her unresponsive on the floor with a Glasgow coma scale (GCS) of 3, breathing shallowly but with a pulse. Her home oxygen was still attached running at a rate of 2L/min. Paramedics noted that after bag-valve ventilation on route to the hospital, her level of consciousness had slightly improved.
On arrival to the emergency department the patient had a GCS of 8, was afebrile, heartrate of 110, blood pressure of 160/95, and was receiving bag-valve ventilations at a rate of 10/min. She had a significant wheeze and decreased breath sounds to the bases upon auscultation. Her jugular venous pressure was 2cm above the sternal angle and there was no peripheral edema. The remainder of her examination was unremarkable. Initial arterial blood gas (ABG) revealed an unmeasurable pH of <6.80, unmeasurable carbon dioxide (pCO2) of >150 mmHg, bicarbonate (HCO3) of 24 mmol/L and lactate of 5.2 mmol/L. High-sensitivity troponin was mildly elevated at 23 ng/L with a repeat value 2-h later trending downwards at 21 ng/L. Her complete blood count, creatinine, D-dimer, and liver function tests were within normal limits. The patient was initially treated as a severe acute exacerbation of COPD with the initiation of bilevel positive airway pressure (BiPAP), nebulized salbutamol and ipratropium bromide, high-dose prednisone and antibiotics.
The patient responded rapidly over the following 3-h with an improvement on her ABG with pH of 7.30 and pCO2 to 55 mmHg and an improvement in GCS to 15 at which point BiPAP was discontinued. The patient denied any toxic ingestions, substance use, or taking any additional medications such as narcotics. She also denied increasing the flowrate of her home oxygen greater than her normal 2L/min at any time. Both of her previous admissions began with a similar call to EMS for chest tightness and dyspnea and she was subsequently found unresponsive secondary to severe hypercapnic respiratory failure. The first of her two recent episodes required intubation and admission to the intensive care unit where she rapidly improved, was extubated hours later, and discharged from hospital three days afterwards. The second of these admissions was managed with BiPAP which caused rapid improvement and she was discharged two days later. These were both labelled as acute exacerbations of COPD; however, they were unusual in that the onset was rapid, she had negative infectious workups, she lacked any typical symptoms such as increased cough, dyspnea or sputum production, and she improved so rapidly with ventilation. Given the lack of convincing evidence for an acute exacerbation of COPD, the patient underwent extensive workup for an alternative etiology for her hypercapnic respiratory failure.
After a return to clinical baseline, a repeat ABG on her home dose of 2L/min of oxygen revealed a pH 7.38, CO2 39 mmHg and HCO3 24 mmol/L, demonstrating that this patient was not a CO2 retainer. Given a negative D-dimer and complete clinical resolution without anticoagulation, a pulmonary embolism was sufficiently ruled out. Computed tomography (CT) of her chest and neck were normal and did not demonstrate a structural etiology such as tracheomalacia or a mass lesion that could be contributing to an acute obstructive process. A CT head revealed age-related changes, but no lesions or causes of central apnea. A 48-h Holter monitor failed to identify any cardiac arrythmias. Upon further history, the patient described a remote history of childhood epilepsy, so neurology was involved who performed an electroencephalogram (EEG) and magnetic resonance imaging (MRI) of her brain to investigate for a possible seizure disorder, which returned unremarkable. Direct laryngoscopy was performed by otolaryngology to investigate possible vocal cord dysfunction, which appeared normal. A speech language pathology assessment and barium swallow revealed no concern with her swallowing.
On the third day of hospital admission, the patient woke up in the early morning and felt similar symptoms of chest tightness and dyspnea and was found to be in respiratory distress with a rapid and shallow respiratory rate of 50/min and had developed an expiratory wheeze on examination but did not have stridor. The patient was tachycardic, tremulous, diaphoretic and reported feeling extremely anxious and stated that she felt she was going to die. Stat ABG revealed pH 7.12, CO2 79 mmHg and HCO3 25 mmol/L. Given her symptoms of extreme anxiety she was given 1 mg of sublingual lorazepam which immediately corrected her hyperventilation and aborted her episode with normalization of her blood gas. After repeat investigations returned unremarkable, it became clear that the patient was suffering from panic attacks causing her to hyperventilate and breath-stack which, in combination with her underlying obstructive lung disease, culminated in acute hypercapnic respiratory failure.
The patient later revealed that she had stopped taking her duloxetine 4 months ago as she didn't believe it was helpful for her anxiety. Psychiatry was involved and the patient was restarted on her duloxetine, initiated on bupropion and prescribed sublingual lorazepam as a breakthrough anxiolytic to take on a p.r.n. basis should she develop further episodes. The patient was discharged from hospital with outpatient follow-up for her COPD and anxiety disorder and has had no further episodes requiring hospitalization as of 8-months.
2. Discussion
Patients with COPD who present in acute respiratory failure are at high-risk for poor clinical outcomes including death. Hypercapnic respiratory failure in these patients is often caused by an exacerbation of their obstructive lung disease, most often from an infection, environmental allergens or pollution, pulmonary embolism or non-compliance with medications [9]. Clinical presentation generally occurs over hours to days and typically includes at least one of increased cough frequency or severity, increased sputum production or change in character, and an increase in dyspnea [9]. Patients who present in respiratory failure that develops acutely over a matter of minutes, like our patient, is unusual and should prompt consideration for an alternative diagnosis.
I report the case of a thoroughly investigated 67-year old female with a diagnosis of moderate COPD and anxiety that presented with multiple episodes of acute, severe hypercapnic respiratory failure secondary to panic attacks. Although the diagnosis of vocal cord dysfunction is difficult to definitively exclude as this too would respond to benzodiazepines, given her normal direct laryngoscopy, lack of stridor during her observed episode, and clinical information that supports an alternative diagnosis (ie. stopping duloxetine), I feel this diagnosis is less likely. To my knowledge, this is the first case in the literature that has demonstrated recurrent episodes of severe hypercapnic respiratory failure that was a direct consequence of panic attacks in a patient with anxiety and COPD.
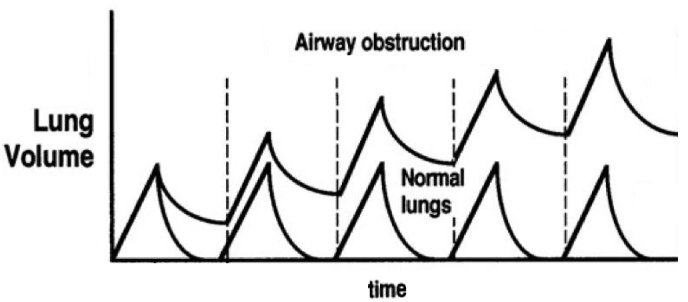
Panic attacks can be often associated with tachypnea and, although normally physically harmless, when combined with obstructive lung disease this has the potential to cause significant deterioration due to the phenomenon of breath-stacking. As these patient's breathe at a rapid rate, they fill their lungs with gas that they are unable to effectively exhale due to obstruction, which can physiologically culminate in acute hypercapnic respiratory failure (Fig. 1). Additionally, hypercapnia has been demonstrated as an inducible trigger of panic attacks due to activation of specific brainstem reflexes [7]. This may lead to a vicious cycle when an obstructive lung process is present as hyperventilation due to panic may cause gas trapping in the lungs, further increasing the patient's CO2 levels, and thus further exacerbating their symptoms of panic.
Fig. 1.
A graph demonstrating the phenomenon of breath stacking in respect to lung volume over time. The patient does not have enough time to exhale, with each breath leading to a larger and larger lung volume.
According to a study by McGarvey, sudden/unexpected death is responsible for 16% of patients with COPD and, given the high prevalence of anxiety and panic disorder amongst this population, it is possible that acute hypercapnic respiratory failure secondary to panic attacks may be a contributor to a subset of this [10].
Despite the high burden of anxiety in patients with COPD, it is often underrecognized and undermanaged by clinicians [8,11]. Effective management of anxiety within these patients is important as patients with established anxiety and COPD have been demonstrated to have worse clinical outcomes than with COPD alone [8]. Screening for anxiety is critically important and tools such as the validated Anxiety Inventory for Respiratory Disease developed by Willgoss et al. can be utilized to help identify these patients [11]. In addition to pharmacologic therapy, non-pharmacological interventions for management of anxiety such as cognitive behavioural therapy and exercise therapy have recently been demonstrated to be clinically effective [12,13].
The true etiology of our patient's respiratory failure was not suspected until her third episode and, given the severity of her blood gases, her presentations would almost certainly have been fatal without medical intervention. Increased awareness of panic attacks having the ability to cause hypercapnic respiratory failure is important to minimize delays in diagnosis as this case illustrates that the clinical presentation can be severe and is potentially avoidable with effective management of anxiety.
2.1. Take-home points
-
•
Anxiety is more prevalent in patients with COPD than in the general population and a large subset of this population meets the diagnostic criteria for panic disorder
-
•
Screening for and management of anxiety in these patients is important as patients with COPD and anxiety have worse clinical outcomes than with COPD alone
-
•
Hypercapnic respiratory failure that develops acutely is unusual for an acute exacerbation of COPD and should prompt consideration for an alternate diagnosis
-
•
Panic attacks should be considered as an etiology for hypercapnic respiratory failure in patients with COPD and anxiety when the clinical presentation is atypical
Funding
There is no funding associated with this case report.
Author's contributions
CO was directly in the diagnosis and patient care. CO prepared the manuscript.
Declaration of competing interest
I have no financial or non-financial competing interests related to this case report.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2020.101044.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Willgoss T.G., Yohannes A.M. Anxiety disorders in patients with COPD: a systematic review. Respir. Care. 2013;58(5):858–866. doi: 10.4187/respcare.01862. [DOI] [PubMed] [Google Scholar]
- 2.Di Marco F., Verga M., Reggente M., Maria Casanova F., Santus P., Blasi F. Anxiety and depression in COPD patients: The roles of gender and disease severity. Respir. Med. 2006;100(10):1767–1774. doi: 10.1016/j.rmed.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 3.Mikkelsen R.L., Middelboe T., Pisinger C., Stage K.B. Anxiety and depression in patients with chronic obstructive pulmonary disease (COPD). A review. Nord. J. Psychiatr. 2004;58(1):65–70. doi: 10.1080/08039480310000824. [DOI] [PubMed] [Google Scholar]
- 4.Livermore N., Sharpe L., McKenzie D. Panic attacks and panic disorder in chronic obstructive pulmonary disease: a cognitive behavioral perspective. Respir. Med. 2010;104(9):1246–1253. doi: 10.1016/j.rmed.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 5.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. fifth ed. 2013. Washington D.C. [Google Scholar]
- 6.Klein D.F. False suffocation alarms, spontaneous panics, and related conditions: an integrative hypothesis. Arch. Gen. Psychiatr. 1993;50(4):306–317. doi: 10.1001/archpsyc.1993.01820160076009. [DOI] [PubMed] [Google Scholar]
- 7.Goossens L., Leibold N., Peeters R., Esquivel G., Knuts I., Backes W. Brainstem response to hypercapnia: a symptom provocation study into the pathophysiology of panic disorder. J. Psychopharmacol. 2014;28(5):449–456. doi: 10.1177/0269881114527363. [DOI] [PubMed] [Google Scholar]
- 8.Eisner M.D., Blanc P.D., Yelin E.H., Katz P.P., Sanchez G., Iribarren C. Influence of anxiety on health outcomes in COPD. Thorax. 2010;65(3):229–234. doi: 10.1136/thx.2009.126201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ko F.W., Chan K.P., Hui D.S., Goddard J.R., Shaw J.G., Reid D.W. Acute exacerbation of COPD. Respirology. 2016;21(7):1152–1165. doi: 10.1111/resp.12780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McGarvey L.P., John M., Anderson J.A., Zvarich M., Wise R.A. Ascertainment of cause-specific mortality in COPD: operations of the TORCH clinical endpoint committee. Thorax. 2007;62(5):411–415. doi: 10.1136/thx.2006.072348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Willgoss T.G., Goldbart J., Fatoye F., Yohannes A.M. The development and validation of the anxiety inventory for respiratory disease. Chest. 2013;144(5):1587–1596. doi: 10.1378/chest.13-0168. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 12.Heslop-Marshall K., Baker C., Carrick-Sen D., Newton J., Echevarria C., Stenton C. Randomised controlled trial of cognitive behavioural therapy in COPD. ERJ Open Res. 2018;4(4) doi: 10.1183/23120541.00094-2018. [Internet] 00094–2018. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tselebis A., Pachi A., Ilias I., Kosmas E., Bratis D., Moussas G. Strategies to improve anxiety and depression in patients with COPD: a mental health perspective. Neuropsychiatric Dis. Treat. 2016;12:297–328. doi: 10.2147/NDT.S79354. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.