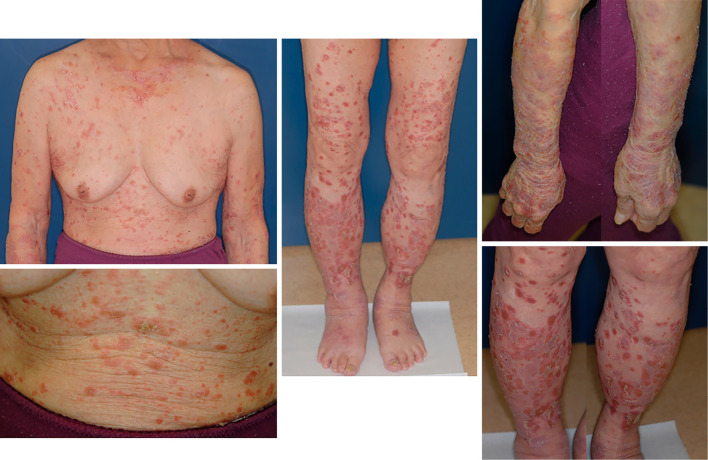
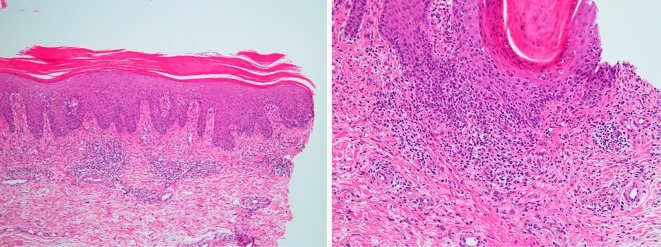
A 78-year-old woman was diagnosed with stage IV A left lower lobe adenocarcinoma by chest computed tomography. There was no history of psoriasis. Her tumor proportion score on PD-L1 was 55%, and she was given Pembrolizumab at 200 mg/body every 3 weeks. After three cycles of treatment, psoriasis-like rashes accompanied by itching rapidly appeared across her body (Picture 1). A skin biopsy indicated psoriasiform dermatitis (Picture 2). In the histopathological findings, the epidermis showed hyperkeratosis with the aggregation of neutrophils (Munro's microabscess) in the horny cell layer and thickening with regular elongation of rete ridges. She started administration of a topical application of steroid ointment, but her symptoms continued to worsen. Oral steroid tablets (prednisolone 1 mg/kg) were started in order to manage psoriasiform dermatitis as a grade 3 immune-related adverse event (irAE). After the treatment, her psoriasiform dermatitis gradually improved. We were able to gradually reduce the prednisolone without exacerbating the skin rash and finally maintained the dose at 2.5 mg per day (Picture 3). We were considering the re-administration of Pembrolizumab, but the patient refused the treatment due to concerns about the worsening of psoriasiform dermatitis. Fortunately, the cytoreductive effect of Pembrolizumab continued, even after the agent's cessation, and the patient's condition was able to be maintained without any special treatments. Various types of skin lesions are known to develop as irAEs following Pembrolizumab administration, but psoriasiform dermatitis has rarely been reported (1,2). Although steroids cannot be expected to be effective for treating systemic psoriasis in general, they should be considered for controlling psoriasiform dermatitis induced by immune checkpoint inhibitors.
Picture 1.
Picture 2.
Picture 3.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Bonigen J, Raynaud-Donzel C, Hureaux J, et al. Anti-PD1-induced psoriasis: a study of 21 patients. J Eur Acad Dermatol Venereol 31: e254-e257, 2017. [DOI] [PubMed] [Google Scholar]
- 2. De Bock M, Hulstaert E, Kruse V, Brochez L. Psoriasis vulgaris exacerbation during treatment with a PD-1 checkpoint inhibitor: case report and literature review. Case Rep Dermatol 10: 190-197, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]