Abstract
Pressure-regulated volume control (PRVC) is a mode of ventilation in which the ventilator attempts to achieve set tidal volume at lowest possible airway pressure. This mode of ventilation is being commonly used as the initial mode of ventilation in many intensive care units. We describe two cases where this adaptive mode of ventilation became maladaptive leading to patient-ventilator dyssynchrony.
1. Introduction
The two most common modes in the world are volume control (VC) and pressure control (PC). VC is flow controlled, and a guaranteed tidal volume and minute ventilation ensured, but in scenarios where flow desired is less than flow delivered, patient-ventilator asynchrony ensues. PC has a set inspiratory pressure: the neural desire of flow can be synchronized to delivered flow given the flow variability. These traditional modes have a set-point targeting scheme, in other words: what the clinician sets, the ventilator will deliver [1]. Ventilator modes are becoming increasingly sophisticated, and settings are previously requiring input and adjustment by the clinician are now becoming automated. Pressure Regulated Volume Control (PRVC) is an example of an Adaptive targeting scheme, in the sense that there is the adaptive targeting of inspiratory pressure with the aim of delivering the desired minute ventilation/tidal volume [2]. In an Adaptive targeting scheme, the ventilator uses a feedback method on a breath-to-breath basis, to continuously adjust the pressure delivered to achieve the tidal volume target. PRVC theoretically provides the benefits of variable flow from PC along with the guaranteed minute ventilation of VC [3]. Given the constant feedback and adaptive targeting, there is often an assumption that PRVC is a set it and forget it type of mode, but asynchronies can ensue. We provide two cases where the Adaptive mode became maladaptive.
2. Case 1
A 42-year-old woman with a history of intravenous drug abuse and reactive airway disease was transferred to our hospital after a cardiac arrest. She had been found down in the field and was given naloxone by emergency medical services (EMS), but on the route to the outside facility's emergency department, she became bradycardic and subsequently lost pulses. She underwent advanced cardiopulmonary life support (ACLS) and achieved return of spontaneous circulation after an unknown period of downtime. She was then intubated and transferred to our hospital for further care.
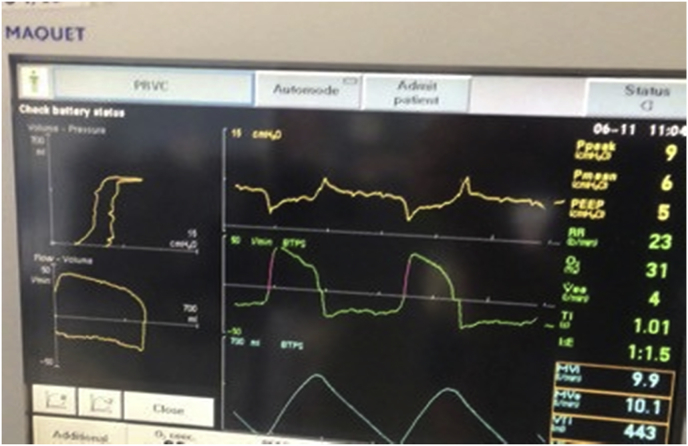
At our hospital, the patient was placed on the ventilator, using PRVC with a set tidal volume of 350 cc (6 cc/kg of ideal body weight (IBW)) and a rate of 15 breaths per minute. The patient was overbreathing at a rate of 22 breaths per minute and was trying to pull tidal volumes of more than 700 cc (>12 cc/kg of IBW) (Fig. 1). As a result, the Adaptive targeting scheme of PRVC lowered the delivered pressure to reach the lower tidal volume set.
Fig. 1.
The pressures on the pressure-time curve were minimal due to the larger tidal volumes that patient was pulling.
We investigated the cause of her high minute ventilation. The arterial blood gas obtained on the above settings showed a pH of 7.08, pCO2 of 54 mmHg, PaO2 of 193 mmHg, with an HCO3 of 15 mmol/L. The mixed metabolic and respiratory acidosis primarily drove the patient's high respiratory drive. The patient was diaphoretic with sternocleidomastoid contraction and intercostal retractions noted, eventually changed to PC of 15 mmHg over PEEP with noted improved patient comfort and synchrony.
3. Case 2
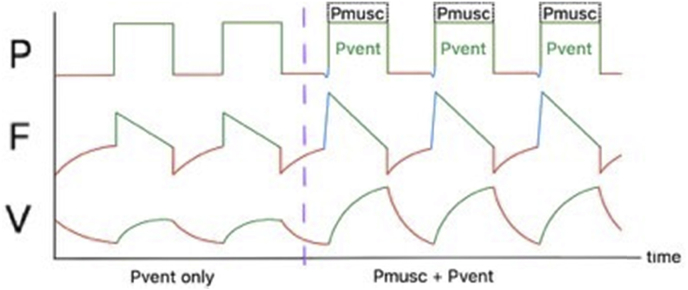
A 49-year-old man with no past medical history presented to our hospital with an intra-parenchymal hemorrhagic stroke. He was intubated for airway protection and was placed on the ventilator using PRVC with a set tidal volume of 400 cc (6 cc/kg of IBW). The patient was noted to be taking higher than set tidal volumes and his pressure-time curve on the ventilator showed negative inspiratory deflections, indicating a high respiratory drive and significant inspiratory efforts (Fig. 2). As the patient was on PRVC, the Adaptive targeting scheme detected the higher tidal volumes and subsequently decreased the inspiratory pressure, auto-peep was also noted, which also contributed to the poor patient-ventilator interactions. We switched to pressure control which improved patient synchrony. The cause for a high respiratory drive was unclear, metabolic, pain and anxiety did not appear to cause; we hypothesized a central etiology in the setting of possible anoxic brain injury.
Fig. 2.
Negative pressure-time curve related to patient inspiratory efforts leading to high tidal volumes and auto-peep (seen on flow-time and flow-volume curves).
4. Discussion
PRVC is a form of an adaptive pressure controlled ventilation in which tidal volume is used as a feed back control to continuously adjust the pressure limit. This adaptive mode of ventilation targets the lowest inspiratory pressures to achieve the set tidal volume. Adaptive targeting scheme in PRVC is a great asset in our ventilator toolbox. In most cases, PRVC can deliver the desired tidal volume at the lowest pressures, using the Adaptive targeting scheme as a feedback method. The beauty of the adaptive mode is that when there is a change in respiratory mechanics in the form of resistance or compliance, the pressure will adjust to deliver the desired tidal volume. However, there have been many occasions in our ICU when we have noticed that the Adaptive targeting scheme becomes maladaptive and can lead to harm in our patients.
One potential dyssynchrony for PRVC is the clinical scenario where an increased desire of flow occurs (pain, anxiety, acidosis, etc.), and the targeting scheme will continue to reduce the inspiratory pressure to minimal levels, theoretically significantly increasing work of breathing [4,5]. We can better understand the physiology of this asynchrony through the lens of the equation of motion [6]. The total pressure applied to the respiratory system is equal to the pressure needed to overcome Elastic (E) and Resistive(R) components. The Elastic and resistive pressures are proportional to the Volume(V) and Flow (V*) respectively. The total pressure can be divided into the pressure applied by the ventilator (Pvent) and by the patient (Pmusc).
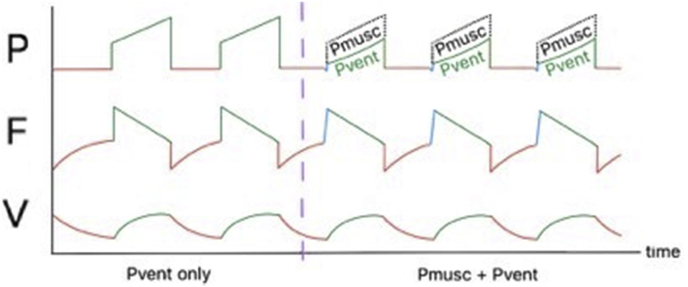
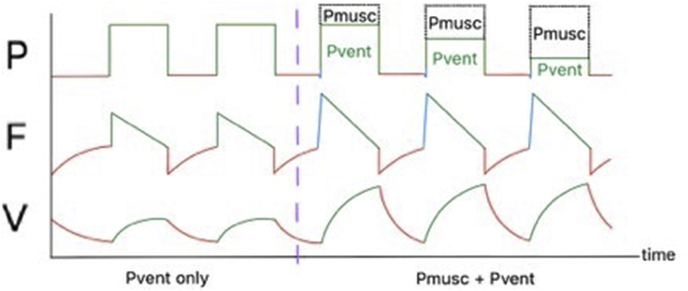
In our ventilator illustrations (Fig. 3, Fig. 4, Fig. 5) we demonstrate PC, VC, PRVC in a patient that is initially passive where Pvent is applying all the pressure, but as the patient becomes active, Pmusc will also contribute to the overall pressure applied. In Fig. 5, the tidal volume is higher than set by the clinician. Therefore the Pvent component will be reduced, but to maintain the desired flow, the Pmusc component will continue to increase.
Fig. 3.
Pressure Control in a passive and active patient.
Fig. 4.
Volume Control in a passive and active patient.
Fig. 5.
PRVC in a passive and active patient.
We describe two cases where patients exhibited a high respiratory drive and were placed on PRVC as an initial mode. In both cases flow demanded by the patient was higher than the set tidal volume. In our cases, the total pressure delivered above PEEP was consistently below five mmHg. During a high respiratory drive state, the Pvent will be reduced on a breath to breath basis, if the patient continues to get high tidal volumes, pmusc will significantly increase. A high and variable respiratory drive leads to variable levels of pvent, this can cause a cycle where the patient becomes increasingly dyssynchronous with the ventilator. Patient-ventilator dyssynchrony is an essential but often unrecognized issue; it is associated with poor patient outcomes, such as patient discomfort and prolonged mechanical ventilation [7,8].
5. Conclusion
PRVC is “typically” a set it and forgets it type of mode, which can be dangerous. We do not believe that PRVC should be the initial mode upon initiation of mechanical ventilation, as respiratory drive can be variable which can lead to assynchrony. In high respiratory drive states the adaptive targeting scheme in PRVC can lead to decreased Pvent and subsequent increased Pmusc, contributing to an overall increase in work of breathing. We recommend that PRVC should be set in patients who have stable respiratory drives.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2019.03.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Chatburn R.L., Mireles-Cabodevila E. Closed-loop control of mechanical ventilation: description and classification of targeting schemes. Respir. Care. 2011;56(1):85–102. doi: 10.4187/respcare.00967. [DOI] [PubMed] [Google Scholar]
- 2.Branson R.D., Chatburn R.L. Controversies in the critical care setting. Should adaptive pressure control modes be utilized for virtually all patients receiving mechanical ventilation? Respir. Care. 2007;52(4):478–485. discussion 485-478. [PubMed] [Google Scholar]
- 3.Guldager H., Nielsen S.L., Carl P., Soerensen M.B. A comparison of volume control and pressure-regulated volume control ventilation in acute respiratory failure. Crit. Care (Lond. Engl.) 1997;1(2):75–77. doi: 10.1186/cc107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jaber S., Delay J.M., Matecki S., Sebbane M., Eledjam J.J., Brochard L. Volume-guaranteed pressure-support ventilation facing acute changes in ventilatory demand. Intensive Care Med. 2005;31(9):1181–1188. doi: 10.1007/s00134-005-2726-x. [DOI] [PubMed] [Google Scholar]
- 5.Kallet R.H., Campbell A.R., Dicker R.A., Katz J.A., Mackersie R.C. Work of breathing during lung-protective ventilation in patients with acute lung injury and acute respiratory distress syndrome: a comparison between volume and pressure-regulated breathing modes. Respir. Care. 2005;50(12):1623–1631. [PubMed] [Google Scholar]
- 6.Marini J.J., Crooke P.S., 3rd A general mathematical model for respiratory dynamics relevant to the clinical setting. Am. Rev. Respir. Dis. 1993;147(1):14–24. doi: 10.1164/ajrccm/147.1.14. [DOI] [PubMed] [Google Scholar]
- 7.Mellott K.G., Grap M.J., Munro C.L. Patient-ventilator asynchrony in critically ill adults: frequency and types. Heart Lung : J. Crit. Care. 2014;43(3):231–243. doi: 10.1016/j.hrtlng.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thille A.W., Rodriguez P., Cabello B., Lellouche F., Brochard L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32(10):1515–1522. doi: 10.1007/s00134-006-0301-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.