Italy's coronavirus disease 2019 (COVID-19) outbreak originated from Codogno, a small town in Southwest Lombardy, on February 21st, 2020. Codogno is 46 km from Pavia, home to one of the largest teaching hospitals (1300 beds) in the region, Fondazione IRCCS Policlinico San Matteo. The hospital has been involved in the management of the outbreak since its inception.
Before the COVID-19 outbreak the Division of Infectious Diseases (ID) was arranged in two floors located in a standalone four-storey building. The ground floor housed the ID outpatient clinic (seven rooms), a day-hospital, and an ultrasound service (eight rooms). The first and second floors were for inpatients (32 twin-bedded rooms with an adjacent buffer zone); at normal capacity each of the wards catered for 22 patients. Finally, the third floor, identical to the other two, housed the Division of Clinical Oncology.
On day 1 of the outbreak, the outpatient clinic and the wards were working as usual at their full capacity. As soon as news of the first severe acute respiratory syndrome coronavirus (SARS-CoV-2) cases reached the hospital, the outpatient clinic closed as a precaution to avoid unnecessary risks for the patients and staff should any COVID-19 case be transferred to the wards. On day 2 of the outbreak it was decided that the outpatient clinic would remain closed until further notice.
Between days 2 and 3 of the outbreak, ‘regular’ patients were discharged or transferred to other wards. On day 3, the ground floor was set up to allow ascertained or suspected cases to directly access the building to minimize the risk of contamination of the general emergency department. All the doors of the building were closed except one that only allowed access to four ultrasound rooms converted into observation rooms.
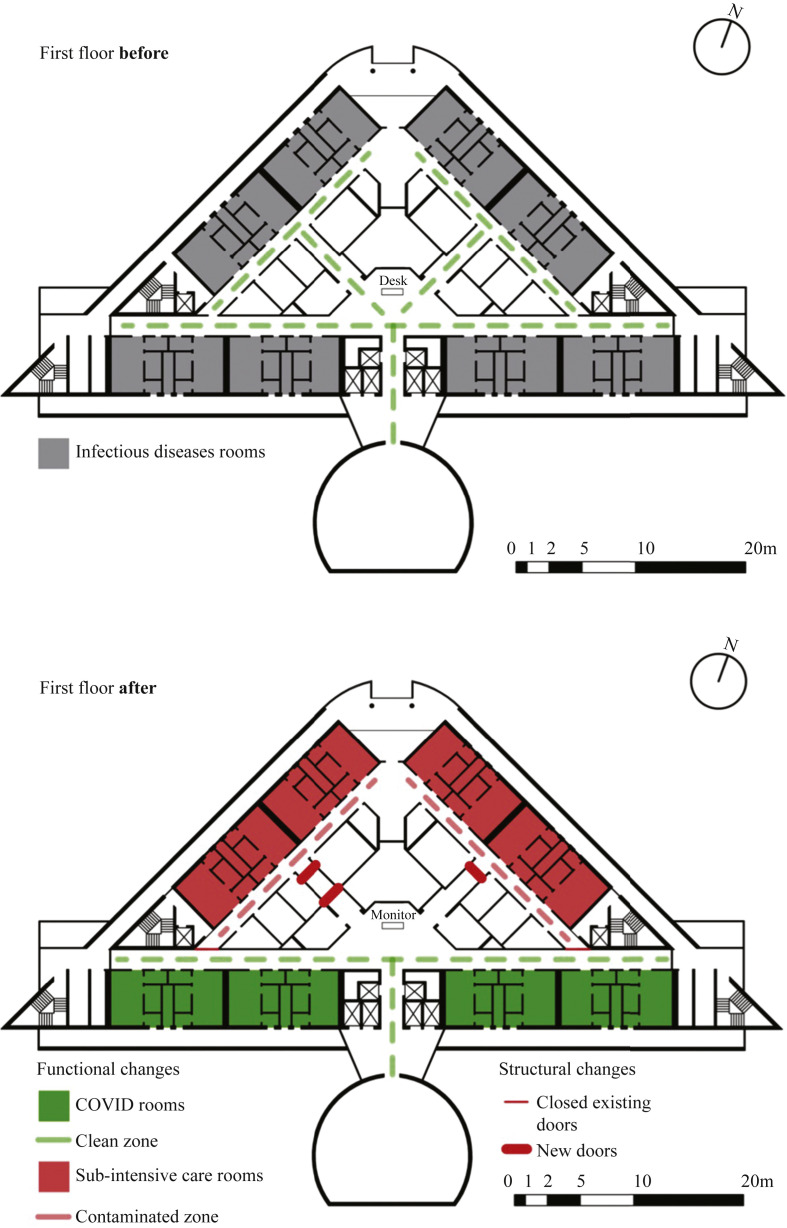
By day 5, all 44 beds in the ID ward were occupied by COVID-19 patients, most of whom required intensive-level care. On day 7 the number of critical patients increased to the point that a section of the first floor was transformed into a sub-intensive care ward. Four corridors were closed with fire doors, two of which were installed overnight. This excluded eight rooms (16 beds) from the other eight rooms of the first floor's ID ward, allowing for free circulation of intensive care specialists and nurses in a contaminated zone (Figure 1 ).
Figure 1.
Layout of the first-floor Infectious Diseases ward before and after changes to accommodate the COVID-19 epidemic.
On day 9 the number of cases in Northern Italy exceeded 1000, several of whom required hospitalization. To this end, additional beds were requested, bringing the ward's total capacity to 64. Preference was given to ascertained cases for cohorting reasons. Negative cases were discharged or admitted to general medicine wards in the hospital.
However, the number of patients waiting for the result of the nasal swab grew so rapidly that it became impossible to cope with them. Consequently, on day 9, the ground floor was converted into an infectious diseases emergency area, where all patients with fever and respiratory symptoms were evaluated. Hallways connected to the central hall on the ground floor were closed, so that all available rooms could be circumscribed as a contaminated zone. Only a single corridor was spared to allow passage from the outside to the lifts connecting to the upper floors. The smaller outpatient offices were redesigned as separate waiting rooms for SARS-CoV-2-positive patients and for patients waiting for the swab results, an electrocardiogram room, and a radiology room with a dedicated portable X-ray machine. The larger ultrasound offices and the day hospital were transformed into a triage area and eight rooms with medical gas connections for acute care. The conversion of the ground floor into a small emergency area was accomplished in 24 h, being fully operational by the end of day 10.
Since the number of infections more than doubled during the day, the oncology ward on the third floor was relocated to another area of the hospital, so that an additional 15 SARS-CoV-2-positive patients could be transferred from the ground floor to the new ID ward during the night between day 11 and day 12. Additional beds, medical equipment, computers, stationery, and drugs were acquired, so that by day 14 the ward could care for a total of 30 patients.
In summary, in less than two weeks, the ID division managed to more than double its total capacity of regular beds from 44 to 94, create a sub-intensive ID ward, and create an ID emergency department with 16 beds for acute care.
All of this was accomplished thanks to the joint efforts of 16 ID specialists and 12 ID residents, additional intensive care, emergency care and internal medicine specialists, regular and additional nurses, the administrative and support staff, and the hospital direction that allowed these quick and brave changes to the structure with great foresight.
Conflict of interest statement
None declared.
Funding sources
None.
Contributor Information
the COVID-19 IRCCS San Matteo Pavia Task Force:
R. Bruno, M.U. Mondelli, E. Brunetti, A. Di Matteo, E. Seminari, L. Maiocchi, V. Zuccaro, L. Pagnucco, B. Mariani, S. Ludovisi, R.L.A. Parisi, P. Sacchi, S.F.A. Patruno, G. Michelone, R. Gulminetti, D. Zanaboni, S. Novati, R. Maserati, P. Orsolini, M. Vecchia, M. Sciarra, E. Asperges, M. Colaneri, A. Di Filippo, M. Sambo, S. Biscarini, M. Lupi, S. Roda, T.C. Pieri, I. Gallazzi, M. Sachs, P. Valsecchi, S. Perlini, C. Alfano, M. Bonzano, F. Briganti, G. Crescenzi, A.G. Falchi, R. Guarnone, B. Guglielmana, E. Maggi, I. Martino, P. Pettenazza, S. Pioli di Marco, F. Quaglia, A. Sabena, F. Salinaro, F. Speciale, I. Zunino, M. De Lorenzo, G. Secco, L. Dimitry, G. Cappa, I. Maisak, B. Chiodi, M. Sciarrini, B. Barcella, F. Resta, L. Moroni, G. Vezzoni, L. Scattaglia, E. Boscolo, C. Zattera, T.M. Fidel, C. Vincenzo, D. Vignaroli, M. Bazzini, G. Iotti, F. Mojoli, M. Belliato, L. Perotti, S. Mongodi, G. Tavazzi, G. Marseglia, A. Licari, I. Brambilla, B. Daniela, B. Antonella, C. Patrizia, C. Giulia, C. Giuditta, C. Marta, D. Rossana, F. Milena, M. Bianca, M. Roberta, M. Enza, P. Stefania, P. Maurizio, P. Elena, P. Antonio, R. Francesca, S. Antonella, Z. Maurizio, A. Guy, B. Laura, C. Ermanna, C. Giuliana, D. Luca, F. Gabriella, G. Gabriella, G. Alessia, L. Viviana, L. Claudia, M. Valentina, P. Simona, P. Marta, B. Alice, C. Giacomo, C. Irene, A. Corcione, R. di Martino, A. di Napoli, F. Alessandro, F. Guglielmo, F. Loretta, G. Federica, M. Alessandra, N. Federica, R. Giacomo, R. Beatrice, S.I. Maria, T. Monica, V.N. Edoardo, M. Calvi, M. Tizzoni, C. Nicora, A. Triarico, V. Petronella, C. Marena, A. Muzzi, and P. Lago
Appendix.
COVID-19 IRCCS San Matteo Pavia Task Force
ID Staff
R. Bruno, M.U. Mondelli, E. Brunetti, A. Di Matteo, E. Seminari, L. Maiocchi, V. Zuccaro, L. Pagnucco, B. Mariani, S. Ludovisi, R.L.A. Parisi, P. Sacchi, S.F.A. Patruno, G. Michelone, R. Gulminetti, D. Zanaboni, S. Novati, R. Maserati, P. Orsolini, M. Vecchia.
ID Residents
M. Sciarra, E. Asperges, M. Colaneri, A. Di Filippo, M. Sambo, S. Biscarini, M. Lupi, S. Roda, T.C. Pieri, I. Gallazzi, M. Sachs, P. Valsecchi.
Emergency Care Unit
ECU Staff: S. Perlini, C. Alfano, M. Bonzano, F. Briganti, G. Crescenzi, A.G. Falchi, R. Guarnone, B. Guglielmana, E. Maggi, I. Martino, P. Pettenazza, S. Pioli di Marco, F. Quaglia, A. Sabena, F. Salinaro, F. Speciale, I. Zunino.
ECU Residents: M. De Lorenzo, G. Secco, L. Dimitry, G. Cappa, I. Maisak, B. Chiodi, M. Sciarrini, B. Barcella, F. Resta, L. Moroni, G. Vezzoni, L. Scattaglia, E. Boscolo, C. Zattera, T.M. Fidel, C. Vincenzo, D. Vignaroli, M. Bazzini.
Intensive Care Unit
G. Iotti, F. Mojoli, M. Belliato, L. Perotti, S. Mongodi, G. Tavazzi.
Paediatric Unit
G. Marseglia, A. Licari, I. Brambilla.
Virology Staff
D. Barbarini, A. Bruno, P. Cambieri, G. Campanini, G. Comolli, M. Corbella, R. Daturi, M. Furione, B. Mariani, R. Maserati, V. Monzillo, S. Paolucci, M. Parea, E. Percivalle, A. Piralla, F. Rovida, A. Sarasini, M. Zavattoni, P. Marone.
Virology Technical staff
G. Adzasehoun, L. Bellotti, E. Cabano, G. Casali, L. Dossena, G. Frisco, G. Garbagnoli, A. Girello, V. Landini, C. Lucchelli, V. Maliardi, S. Pezzaia, M. Premoli.
Virology Residents
A. Bonetti, G. Caneva, I. Cassaniti, A. Corcione, R. Di Martino, A. Di Napoli, A. Ferrari, G. Ferrari, L. Fiorina, F. Giardina, A. Mercato, F. Novazzi, G. Ratano, B. Rossi, I.M. Sciabica, M. Tallarita, E. Vecchio Nepita.
Pharmacy Unit
M. Calvi, M. Tizzoni.
Hospital Leadership
C. Nicora, A. Triarico, V. Petronella, C. Marena, A. Muzzi, P. Lago.