The view of an air quality and ventilation expert
The rapid global rise of infected coronavirus cases after China dramatically impacts the daily life of everyone in every facet. Schools are closing, people are working from home, and stores are filling with panic shoppers. However, lessons learned the hard way in China have been disregarded in a majority of hard-hit countries globally, such as the enforcement of using facial masks.
Authorities of most developed countries make two primary suggestions to the general public: keeping social distance and washing hands. These are surely effective in defeating potential virus dispersion through direct contact and droplet transmission. Neither WHO nor US CDC encourage the usage of facial masks for the general public, rather only for those who are infected and who are in medical care environments. The reasoning can be fivefold.
First of all, most medical and public health professionals believe that direct body contact and secondary surface contact (such as via door handles) of virus sources are the main route for disease cross-infection. Although there is no direct evidence about airborne virus transmission, there is also no solid evidence that COVID-19 cannot disperse through air. Natural ventilation has been widely suggested and successfully implemented in handling various epidemic diseases historically. In principle, virus transmission through respiratory droplets produced when an infected person talks, eats, coughs, or sneezes should also be treated as airborne, whose flow trajectory is affected by local air conditions (e.g., velocity, temperature and humidity). Many cases in China have verified that body or surface contact may not be the main/only route for infection. One example in a local hospital in China had a patient in the 50s, who was hospitalized because of a bone fracture and was soon diagnosed with coronavirus disease exhibiting a constant fever. Both the patient and healthcare providers were wearing respiratory masks during the entire process, but without any other protective measures (not even with gloves). Some medical professionals wore regular medical masks (not surgical masks). Over 60 close-contact healthcare providers were immediately quarantined after the case was confirmed. Several runs of tests thereafter proved none of them were infected. However, the patient's wife was confirmed positive soon afterwards, as the patient did not consistently wear a mask at home. Dozens of such cases were observed in China, which highlights the critical role of masks in protecting person-to-person spread through “no-direct” contact.
Secondly, most medical and public health professionals believe that facial masks are more efficient in preventing virus spread from known sources, while less effective in protecting those in healthy conditions. Part of the reason is that because the virus is so small, it may not be protected by most facial masks (not respiratory or surgical masks). However, as broadly tested, virus cannot transmit and survive once it leaves the host, rather attaching to various carrying media such as droplets. These carrying media are in much larger size range e.g., 5–20 μm, which can be readily caught by regular masks. It is proven that droplets from the mouth in such sizes may not travel a long distance, mostly between 1 and 2 m (3–6 feet) during eating and talking, although it could reach 4–8 m (12–24 feet) with strong coughing and sneezing. This is the foundation for why a reasonable social distance should be maintained during any epidemic disease. Facial masks may not be necessary for such distanced conditions and are not needed for an outdoor environment with good ventilation and low population density. However, for a confined space with higher population density and less ventilation, facial masks are a lifesaver. Cases demonstrate that people in an elevator may get infected by an infected person within a few seconds without any direct contact. Grocery stores are another good example. Facial masks can effectively prevent person-to-person infection through droplet transmission. With the increasing number of no-symptom patients, wearing a facial mask becomes more crucial, even under the current recommendations of US CDC, as everyone could be a potential unknown virus source. Before these people could be fully identified and quarantined as done by China, encouraging the use of facial mask is the most effective approach to avoiding further outbreak of the disease.
Thirdly, medical professionals are concerned that improper use of facial masks may cause other unfavorable effects, such as causing potential breathing issues due to a long time of mask use, especially for younger and elder people. Indeed, facial masks for healthy or undetermined people should be constrained to conditions such as confined high-density spaces including public transportation (aircraft, bus, subway etc.) and public spaces (elevator, store, classroom etc.). The use of masks in these spaces typically will not last long enough to cause health problems. Another concern about using facial masks is that people may tend to touch faces more often with a mask than without a mask. General test reveals face-touching is a spontaneous human behavior which can hardly be controlled (an average test showed at least 1–2 touches within 3 minutes if not purposely controlled). Wearing facial masks will reduce the risk of directly touching the mouth and nose – the most critical parts on the face. The secondary infection because of direct contact with a potentially contaminated mask is another concern of medical professionals, which however can be mitigated by the “washing hand” recommendation conducted immediately after each wearing and removal of the mask. In addition, there is no evidence that people who wear masks would think they are safer than others and thus more neglectful than others; by contrast, people wearing masks are generally more cautious and mindful than peers.
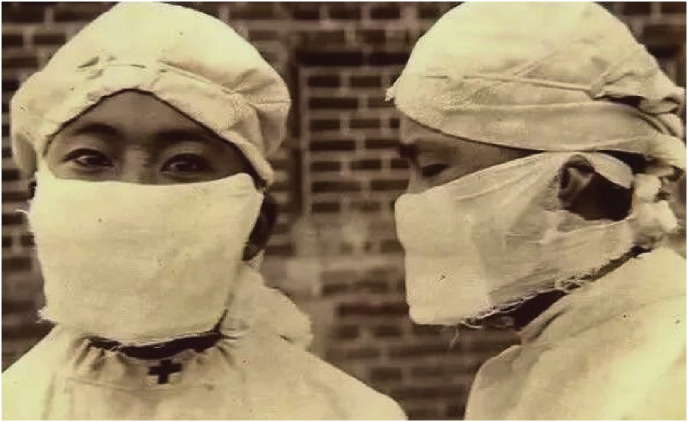
Fourthly, most countries are experiencing shortages of medical resources, including medical masks. Authorities worry that encouraging the use of masks will further worsen the situation, leaving doctors and nurses without adequate protection. China experienced this exact dilemma just a month ago but did not stop their enforcement of utilizing masks when people go out. Besides actively producing various medical supplies, home-made facial masks were promoted creatively and shared in the society. The role of facial masks in fighting the coronavirus is different from fighting PM2.5. Avoiding direct and large droplet impacts can be easily achieved by most homemade masks such as the early version developed by Dr. Liande Wu during the black death in Northeastern China in 1910 (Fig. 1 ). Methods for renewing and reusing facial masks were also presented and tested by various researchers depending on the types of masks such as water-boiling, microwave cleaning etc. Overall, it is not a reasonable and responsible practice to discourage the use of facial mask based on the resource availability.
Fig. 1.
One early version of medical mask developed by Dr. Liande Wu during the black death in Northeastern China in 1910.
Last but not least, encouraging the wide use of facial masks in critical spaces regardless of people's health conditions can provide significant social and psychological benefits. This will increase the public awareness of the severeness of COVID-19 and constantly remind people of the necessity of social distance. It will fully eliminate the biases towards those who are in infection and who are at risk; and will surely mitigate the growing hatred and violence towards those who are from the infection zones.
The COVID-19 occurs unexpected and likely may stay for a while. While there are many aspects of the epidemic that we do not know for sure, let's at least open our minds to try everything that might help, especially those proven measures learnt from the fresh lessons and experience.
Declaration of competing interest
The author declares that no potential conflicts of interest with respect to the research, authorship and/or publication of this article.