Key Points
Question
Is the burden of chronic liver disease–related hospitalization on the US health care system changing over time?
Findings
In this cross-sectional study of 1 016 743 adult hospitalizations related to chronic liver disease, the inpatient burden increased in association with an aging population with increasing comorbidities. While inpatient burden attributable to hepatitis C virus remained significant, the burden due to alcoholic cirrhosis and nonalcoholic fatty liver disease also increased.
Meaning
The increasing burden of hospitalizations related to chronic liver disease emphasizes this disease’s clinical and economic impact and the importance of optimizing outpatient management to prevent complications leading to the need for hospitalization.
This cross-sectional study assesses trends in the burden of chronic liver disease among hospitalized patients on the US health care system.
Abstract
Importance
One factor associated with the rapidly increasing clinical and economic burden of chronic liver disease (CLD) is inpatient health care utilization.
Objective
To understand trends in the hospitalization burden of CLD in the US.
Design, Setting, and Participants
This cross-sectional study of hospitalized adults in the US used data from the National Inpatient Sample from 2012 to 2016 on adult CLD-related hospitalizations. Data were analyzed from June to October 2019.
Main Outcomes and Measures
Hospitalizations identified using a comprehensive review of CLD-specific International Classification of Diseases, Ninth Revision, Clinical Modification and International Statistical Classification of Diseases, Tenth Revision, Clinical Modification codes. Survey-weighted annual trends in national estimates of CLD-related hospitalizations, in-hospital mortality, and hospitalization costs, stratified by demographic and clinical characteristics.
Results
This study included 1 016 743 CLD-related hospitalizations (mean [SD] patient age, 57.4 [14.4] years; 582 197 [57.3%] male; 633 082 [62.3%] white). From 2012 to 2016, the rate of CLD-related hospitalizations per 100 000 hospitalizations increased from 3056 (95% CI, 3042-3069) to 3757 (95% CI, 3742-3772), and total inpatient hospitalization costs increased from $14.9 billion (95% CI, $13.9 billion to $15.9 billion) to $18.8 billion (95% CI, $17.6 billion to $20.0 billion). Mean (SD) patient age increased (56.8 [14.2] years in 2012 to 57.8 [14.6] years in 2016) and, subsequently, the proportion with Medicare also increased (41.7% [95% CI, 41.1%-42.2%] to 43.6% [95% CI, 43.1%-44.1%]) (P for trend < .001 for both). The proportion of hospitalizations of patients with hepatitis C virus was similar throughout the period of study (31.6% [95% CI, 31.3%-31.9%]), and the proportion with alcoholic cirrhosis and nonalcoholic fatty liver disease showed increases. The mortality rate was higher among hospitalizations with alcoholic cirrhosis (11.9% [95% CI, 11.7%-12.0%]) compared with other etiologies. Presence of hepatocellular carcinoma was also associated with a high mortality rate (9.8% [95% CI, 9.5%-10.1%]). Cost burden increased across all etiologies, with a higher total cost burden among hospitalizations with alcoholic cirrhosis ($22.7 billion [95% CI, $22.1 billion to $23.2 billion]) or hepatitis C virus ($22.6 billion [95% CI, $22.1 billion to $23.2 billion]). Presence of cirrhosis, complications of cirrhosis, and comorbidities added to the CLD burden.
Conclusions and Relevance
Over the study period, the total estimated national hospitalization costs in patients with CLD reached $81.1 billion. The inpatient CLD burden in the US is likely increasing because of an aging CLD population with increases in concomitant comorbid conditions.
Introduction
The landscape of chronic liver disease (CLD) in the US is rapidly changing. This condition is currently the fourth leading cause of death among persons aged 45 to 64 years.1 With improvements in the management and treatment of viral hepatitis, the burden of liver disease is shifting toward alcoholic liver disease (ALD) and nonalcoholic fatty liver disease (NAFLD).2,3,4,5 A recent US population-based study focusing on cirrhosis-related mortality observed that increasing cirrhosis death rates in the US were largely driven by alcoholic cirrhosis, with the greatest increases seen among young adults aged 25 to 34 years.6
Inpatient hospitalization and care are a major contributor to health care resource utilization among patients with CLD.7,8,9,10 Few prior studies have used large-scale population-based data sets to evaluate time trends in the total CLD burden and among individual CLD etiologies,4,11,12 cirrhosis, and complications associated with cirrhosis.13 Asrani et al14,15 illustrated trends in the increasing burden of CLD using patient data from hospitalizations in a large and diverse metroplex. Another study4 used the National Health and Nutrition Examination Survey database to provide a more generalizable, comprehensive overview of CLD epidemiology in the US. While the inpatient burden remains unknown, these studies highlight the significant clinical impact of CLD. A more thorough understanding of trends in the hospitalization burden of CLD is an important first step in identifying potential areas of focus for public health initiatives and quality improvement programs to ameliorate CLD-related health care resource utilization in the US.
This study specifically aims to comprehensively evaluate the inpatient clinical and economic burden of CLD using a nationally representative sample of CLD-related hospitalizations and further analyze demographic and etiology-specific differences.
Methods
This study used deidentified data and was granted exempt status by the Alameda Health System institutional review board. We conducted analysis of these data from June 2019 to October 2019. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.16
Data Source
This study evaluated 2012 to 2016 data from the National Inpatient Sample (NIS).17 The NIS is the largest all-payer inpatient database of hospital discharges in the US and is maintained as part of the Healthcare Cost and Utilization Project by the Agency for Healthcare Research and Quality. The NIS contains deidentified information regarding each hospitalization, including patient demographic characteristics, admission status, discharge diagnoses, procedures, comorbid conditions, outcomes, and hospital charges. If race and ethnicity were provided in separate data elements, ethnicity took precedence over race in setting the Healthcare Cost and Utilization Project value for race. Participating hospitals are sampled based on characteristics such as size, location (rural vs urban), geographic region, ownership, and teaching status. Starting in 2012, the NIS modified its method of data acquisition to include a systematic sampling of 20% of discharges from all hospitals stratified by hospital, US Census division, ownership status, urban vs rural location, teaching status, and bed size, as well as patient diagnosis-related group and admission month.17 In 2015, data elements and data structure for the NIS were changed again.18 Trends based on diagnoses or procedures were affected because, starting October 2015, hospital administrative data in the US began using International Classification of Diseases, Tenth Revision, Clinical Modification/Procedure Coding System (ICD-10-CM/PCS). In the 2015 NIS, the first 9 months contain International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes and the last 3 months contain ICD-10-CM/PCS codes.19,20,21 The Elixhauser Comorbidity Index software indicators were not available beginning October 1, 2015, because the ICD-10-CM version of the software is still under development.18
Study Population and Variables
The sample included CLD-related hospitalizations of US adults (aged ≥18 years) between January 1, 2012, and December 31, 2016. We defined CLD using a comprehensive review of ICD-9-CM codes based on prior published algorithms14,15 from January 1, 2012, to September 30, 2015, and corresponding ICD-10-CM codes starting October 1, 2015 (eFigure and eTable 1 in the Supplement). To minimize ascertainment bias, we classified a hospitalization as CLD related if it was associated with (1) a primary discharge diagnosis of CLD or (2) a primary discharge diagnosis of another liver-related cause (eg, cirrhosis) in combination with a secondary diagnosis of CLD (eTable 1 in the Supplement).
Among CLD-related hospitalizations, we stratified hospitalizations by 4 main etiologies (alcoholic cirrhosis, hepatitis B virus [HBV] infection, hepatitis C virus [HCV] infection, and NAFLD), as these etiologies combined account for most of the burden of CLD among hospitalized patients in the US. Adult hospitalizations with alcoholic cirrhosis were identified by first isolating all hospitalizations with cirrhosis listed as a diagnosis (eTable 2 in the Supplement). From the cohort with cirrhosis, we excluded patients with autoimmune hepatitis, viral hepatitis, hemochromatosis, only NAFLD-specific codes (ICD-9: 571.5, 571.8-9; ICD-10: K75.81), primary biliary cholangitis, and primary sclerosing cholangitis listed as a diagnosis (eTable 2 in the Supplement). We then defined alcoholic cirrhosis as hospitalizations with ALD or alcohol use disorder in addition to cirrhosis22 (eTable 2 in the Supplement). Adult hospitalizations with NAFLD were identified by first using ICD codes for liver disease without mention of alcohol (ICD-9: 571.5, 571.8-9, 567.23, 572.2-4, 456.0-2x, 789.5x; ICD-10: I85.xx, K65.2, K72.1x, K72.9x, K74.0-2, K74.6x, K75.8x, K75.9, K76.0, K76.6-9, K77, R18.x) and then excluding patients with chronic liver disease with mention of alcohol or alcohol use disorder (eTable 2 in the Supplement), alcoholic cirrhosis, and other etiologies of acute or chronic liver disease8,11,23 (autoimmune hepatitis, Budd-Chiari syndrome, chronic passive congestion of liver, clonorchiasis, disorders of porphyrin and bilirubin metabolism, echinococcus of liver, fascioliasis, Gaucher disease, hemochromatosis, viral hepatitis, lysosomal acid lipase deficiency and other lipoid disorders, opisthorchiasis, other amyloidosis, other deficiencies of circulating enzymes, other disorders of the liver, primary biliary cholangitis, primary sclerosing cholangitis, syphilis of the liver, or Wilson disease) (eTable 2 in the Supplement). Patients with alcohol abuse listed as an Elixhauser comorbidity were included in the alcoholic cirrhosis cohort and excluded from the NAFLD cohort for data using ICD-9-CM codes.
We additionally evaluated for the presence of hepatocellular carcinoma, cirrhosis, and cirrhosis-related complications, including ascites, esophageal varices, hepatic encephalopathy, and hepatorenal syndrome (eTable 1 and eTable 2 in the Supplement).
Outcome Measures
We estimated the number of CLD-related hospitalizations in each study year. We further described demographic (age, sex, race, and insurance), clinical (liver disease etiology; hepatocellular carcinoma; cirrhosis and concurrent presence of 0, 1, or ≥2 cirrhosis-related complications among patients with cirrhosis; and comorbidities), and hospital characteristics (region, bed size, location, and teaching status) of the sample in each study year. Among CLD-related hospitalizations, we examined year-specific in-hospital mortality and hospitalization costs, stratified by demographic and clinical characteristics.
Hospitalization charges as provided within the data set were inflation adjusted to and reported as 2016 US dollars using the Consumer Price Index maintained by the US Department of Labor.24 Hospitalization charges may be confounded by payer policies and other factors unrelated to resource utilization. Therefore, hospitalization costs were calculated for each hospitalization using hospital-specific cost to charge ratios developed by the Agency for Healthcare Research and Quality.25
Missing Data
Hospitalizations with missing data on age and/or sex were excluded. Hospitalizations with missing data on race (4.4%) were coded with a dummy variable to represent the missing data. In all, 0.2% of observations were missing data on insurance status, 0.07% of hospitalizations were missing data on in-hospital mortality, and 2.0% were missing data on costs. Because missingness for each variable with missing observations was 5% or less, and because the study was a cross-sectional analysis of trends, observations with missing data were excluded from the analysis of the respective variable.27,28
Statistical Analysis
Data were survey-weighted using individual discharge weights to obtain descriptive statistics and national estimates. We analyzed time trends in the rate of CLD-related hospitalizations, and among CLD-related hospitalizations, we analyzed trends in the prevalence of demographic and clinical characteristics. We further analyzed trends in in-hospital mortality, mean hospitalization costs, and total hospitalization costs; we performed subgroup analyses by demographic and clinical characteristics. Secular trends were assessed after regressing all outcomes on year, modeled as a continuous variable. We used logistic regression for demographic and clinical outcomes and in-hospital mortality and linear regression after log-transforming the outcome for mean hospitalization costs. We used Poisson regression with count variables to test for trend in the rate of CLD-related hospitalizations. Between-group comparisons used Pearson χ2 tests for binary and categorical variables.
A 2-tailed P < .05 was considered statistically significant. Statistical analyses were performed using Stata version 14.0 (StataCorp). We followed the research practices recommended when using NIS data.26
Results
Characteristics of the Study Cohort
Among 1 016 743 CLD-related hospitalizations from 2012 to 2016, the mean (SD) patient age was 57.4 (14.4) years; 582 197 (57.3%) were male; and 633 082 (62.3%) were white, 138 068 (13.6%) were African American, and 134 662 (13.2%) were Hispanic (Table 1). The largest proportion of hospitalizations were for patients aged 45 to 64 years (53.0% [95% CI, 52.8%-53.1%]). Medicare was the most common insurance type (42.7% [95% CI, 42.5%-42.9%]), followed by Medicaid or private insurance. The mean (SD) length of hospitalization was 6.3 (8.0) days. The most common liver disease etiology was HCV (31.6% [95% CI, 31.3%-31.9%]). Overall, 538 720 hospitalizations (95% CI, 53.0% [52.8%-53.2%]) had cirrhosis, and 25.7% (95% CI, 25.5%-25.8%) had cirrhosis with 1 cirrhosis-related complication present. Hypertension and diabetes were the most prevalent comorbidities (Table 1).
Table 1. Trends in the Clinical and Demographic Characteristics of the Study Cohort.
| Characteristic | Hospitalizations related to chronic liver disease, weighted % (95% CI) | P value for trend | |||||
|---|---|---|---|---|---|---|---|
| Total (n = 1 016 743) | 2012 (n = 187 690) | 2013 (n = 192 614) | 2014 (n = 201 069) | 2015 (n = 208 656) | 2016 (n = 226 714) | ||
| Chronic liver disease–related hospitalizations per 100 000, No. | 3372 | 3056 | 3214 | 3380 | 3459 | 3757 | <.001 |
| Age, mean (SD), y | 57.4 (14.4) | 56.8 (14.2) | 57.1 (14.3) | 57.3 (14.4) | 57.7 (14.5) | 57.8 (14.6) | <.001 |
| Age, y | |||||||
| <25 | 1.5 (1.5-1.6) | 1.6 (1.5-1.6) | 1.6 (1.6-1.7) | 1.6 (1.5-1.6) | 1.5 (1.5-1.6) | 1.5 (1.4-1.5) | .02 |
| 25-44 | 15.7 (15.6-15.8) | 15.6 (15.3-15.9) | 15.4 (15.1-15.7) | 15.6 (15.4-15.9) | 15.7 (15.4-16.0) | 16.1 (15.8-16.4) | .01 |
| 45-64 | 53.0 (52.8-53.1) | 55.5 (55.1-55.9) | 54.4 (54.0-54.8) | 53.4 (53.0-53.8) | 51.9 (51.5-52.2) | 50.3 (49.9-50.6) | <.001 |
| ≥65 | 29.8 (29.6-30.0) | 27.4 (26.9-27.9) | 28.6 (28.2-29.2) | 29.4 (28.9-29.9) | 30.9 (30.4-31.4) | 32.2 (31.7-32.6) | <.001 |
| Sex | |||||||
| Male | 57.3 (57.1-57.4) | 57.8 (57.5-58.1) | 57.5 (57.2-57.8) | 57.2 (56.9-57.7) | 56.9 (56.6-57.2) | 57.0 (56.7-57.3) | <.001 |
| Female | 42.7 (42.6-42.9) | 42.2 (41.9-42.5) | 42.5 (42.2-42.8) | 42.8 (42.5-43.1) | 43.1 (42.8-43.4) | 43.0 (42.7-43.3) | <.001 |
| Race | |||||||
| White | 62.3 (61.7-62.8) | 61.6 (60.2-63.0) | 62.1 (60.7-63.5) | 62.6 (61.2-64.0) | 62.4 (61.1-63.7) | 62.5 (61.2-63.8) | .35 |
| African American | 13.6 (13.3-13.9) | 14.1 (13.3-15.0) | 13.6 (12.8-14.4) | 13.4 (12.7-14.2) | 13.4 (12.7-14.2) | 13.5 (12.8-14.2) | .26 |
| Hispanic | 13.2 (12.9-13.6) | 13.0 (12.0-14.0) | 13.1 (12.2-14.2) | 13.0 (12.1-14.0) | 13.5 (12.5-14.4) | 13.6 (12.7-14.6) | .31 |
| Asian/Pacific Islander | 2.5 (2.4-2.6) | 2.3 (2.1-2.6) | 2.5 (2.2-2.8) | 2.5 (2.2-2.8) | 2.6 (2.4-2.9) | 2.6 (2.3-2.8) | .18 |
| Other | 4.1 (3.9-4.3) | 4.6 (3.9-5.3) | 3.8 (3.4-4.3) | 4.1 (3.7-4.5) | 3.8 (3.4-4.2) | 4.0 (3.6-4.5) | .26 |
| Missing | 4.4 (4.0-4.7) | 4.4 (3.7-5.4) | 4.9 (4.0-5.9) | 4.5 (3.6-5.5) | 4.3 (3.5-5.2) | 3.8 (3.1-4.8) | .17 |
| Insurance | |||||||
| Medicare | 42.7 (42.5-42.9) | 41.7 (41.1-42.2) | 42.3 (41.8-42.8) | 42.7 (42.2-43.3) | 43.1 (42.6-43.6) | 43.6 (43.1-44.1) | <.001 |
| Medicaid | 23.5 (23.2-23.8) | 21.6 (20.9-22.2) | 21.3 (20.7-22.0) | 24.5 (23.7-25.3) | 24.6 (23.9-25.4) | 24.9 (24.2-25.7) | <.001 |
| Private, including health maintenance organization | 22.4 (22.1-22.6) | 22.4 (21.8-23.0) | 22.0 (21.4-22.6) | 22.5 (21.9-23.2) | 22.7 (22.1-23.3) | 22.1 (21.6-22.7) | .86 |
| Self-pay | 7.1 (6.9-7.3) | 9.1 (8.6-9.5) | 8.8 (8.4-9.3) | 6.5 (6.1-6.9) | 5.8 (5.4-6.2) | 5.7 (5.3-6.1) | <.001 |
| No charge | 0.8 (0.7-0.8) | 0.8 (0.7-1.0) | 1.2 (1.0-1.4) | 0.7 (0.6-0.8) | 0.6 (0.5-0.8) | 0.6 (0.5-0.7) | <.001 |
| Other | 3.6 (3.5-3.8) | 4.5 (4.2-4.9) | 4.4 (4.0-4.7) | 3.1 (2.9-3.4) | 3.1 (2.9-3.4) | 3.1 (2.9-3.4) | <.001 |
| Hospital region | |||||||
| Northeast | 18.4 (17.8-18.9) | 19.3 (17.4-21.4) | 18.8 (16.8-20.9) | 18.6 (16.7-20.6) | 17.6 (15.9-19.6) | 17.7 (15.9-19.6) | .20 |
| Midwest | 19.2 (18.7-19.8) | 19.7 (17.9-21.7) | 19.8 (18.0-21.9) | 19.0 (17.2-20.9) | 18.8 (17.1-20.6) | 18.9 (17.2-20.8) | .42 |
| South | 39.7 (39.1-40.3) | 38.8 (36.3-41.3) | 39.3 (36.8-41.8) | 39.8 (37.4-42.3) | 40.1 (37.7-42.5) | 40.2 (37.9-42.6) | .40 |
| West | 22.7 (22.2-23.3) | 22.2 (20.3-24.2) | 22.1 (20.2-24.1) | 22.6 (20.7-24.7) | 23.5 (21.6-25.6) | 23.2 (21.3-25.2) | .33 |
| Hospital bed size | |||||||
| Small | 15.2 (14.8-15.6) | 12.5 (11.4-13.8) | 12.4 (11.3-13.6) | 17.1 (15.8-18.5) | 16.5 (15.2-17.8) | 17.1 (15.8-18.4) | <.001 |
| Medium | 27.6 (27.1-28.1) | 26.0 (24.1-27.9) | 25.9 (24.0-27.9) | 28.4 (26.4-30.4) | 29.1 (27.2-31.0) | 28.2 (26.3-30.1) | .03 |
| Large | 57.2 (56.6-57.8) | 61.5 (59.3-63.7) | 61.7 (59.4-63.9) | 54.6 (52.2-56.9) | 54.5 (52.2-56.8) | 54.7 (52.4-57.0) | <.001 |
| Hospital location and teaching status | |||||||
| Rural | 8.1 (7.9-8.4) | 9.3 (8.4-10.2) | 9.3 (8.5-10.3) | 7.7 (6.9-8.6) | 7.3 (6.6-8.0) | 7.2 (6.5-7.9) | <.001 |
| Urban, nonteaching | 29.3 (28.8-29.8) | 35.9 (33.8-38.0) | 35.3 (33.2-37.4) | 25.3 (23.5-27.1) | 25.9 (24.2-27.7) | 25.3 (23.6-27.1) | <.001 |
| Urban, teaching | 62.6 (62.1-63.2) | 54.9 (52.5-57.2) | 55.4 (53.0-57.8) | 67.0 (65.0-69.0) | 66.8 (64.8-68.7) | 67.5 (65.6-69.4) | <.001 |
| Length of stay, mean (SD), d | 6.3 (8.0) | 6.3 (8.2) | 6.2 (8.1) | 6.4 (8.3) | 6.0 (7.2) | 6.4 (8.2) | .77 |
| Alcoholic cirrhosis | 24.5 (24.3-24.7) | 19.4 (19.1-19.8) | 19.6 (19.2-19.9) | 19.6 (19.3-19.9) | 23.9 (23.6-24.2) | 37.7 (37.2-38.1) | <.001 |
| Hepatitis B virus | 4.4 (4.4-4.5) | 4.9 (4.7-5.1) | 4.8 (4.6-5.0) | 4.4 (4.2-4.6) | 4.1 (3.9-4.2) | 4.1 (3.9-4.3) | <.001 |
| Hepatitis C virus | 31.6 (31.3-31.9) | 35.2 (34.4-35.9) | 33.6 (32.9-34.3) | 31.9 (31.2-32.5) | 30.3 (29.7-30.9) | 27.9 (27.3-28.5) | <.001 |
| Nonalcoholic fatty liver disease | 19.8 (19.7-20.0) | 18.6 (18.2-19.0) | 19.9 (19.5-20.3) | 21.4 (21.0-21.8) | 21.4 (21.0-21.8) | 18.0 (17.6-18.4) | .67 |
| Hepatocellular carcinoma | 4.5 (4.4-4.6) | 4.7 (4.4-5.0) | 4.7 (4.5-5.0) | 4.5 (4.3-4.8) | 4.4 (4.2-4.6) | 4.0 (3.8-4.2) | <.001 |
| Cirrhosis | 53.0 (52.8-53.2) | 51.2 (50.6-51.7) | 51.8 (51.3-52.4) | 52.0 (51.5-52.5) | 53.0 (52.5-53.5) | 56.4 (55.9-56.8) | <.001 |
| Cirrhosis-related complications, No. | |||||||
| 0 | 14.7 (14.6-14.8) | 14.8 (14.5-15.0) | 14.8 (14.6-15.0) | 14.6 (14.4-14.9) | 14.8 (14.6-15.0) | 14.5 (14.2-14.7) | .08 |
| 1 | 25.7 (25.5-25.8) | 24.7 (24.4-25.1) | 25.0 (24.7-25.3) | 24.8 (24.5-25.1) | 25.4 (25.1-25.6) | 28.1 (27.8-28.3) | <.001 |
| ≥2 | 12.6 (12.5-12.8) | 11.6 (11.3-12.0) | 12.0 (11.7-12.4) | 12.6 (12.3-12.9) | 12.8 (12.5-13.2) | 13.8 (13.5-14.2) | <.001 |
| Coronary artery disease | 14.5 (14.4-14.6) | 13.5 (13.2-13.8) | 13.8 (13.5-14.1) | 13.9 (13.7-14.2) | 14.7 (14.5-15.0) | 16.0 (15.8-16.3) | <.001 |
| Congestive heart failure | 14.5 (14.4-14.6) | 12.9 (12.7-13.2) | 13.4 (13.2-13.7) | 14.3 (14.0-14.5) | 15.1 (14.8-15.3) | 16.4 (16.2-16.7) | <.001 |
| Chronic kidney disease | 20.7 (20.5-20.8) | 18.6 (18.3-19.0) | 19.4 (19.0-19.8) | 20.2 (19.8-20.6) | 21.3 (21.0-21.7) | 23.3 (22.9-23.6) | <.001 |
| Diabetes | 31.8 (31.6-31.9) | 30.6 (30.2-30.9) | 31.3 (30.9-31.6) | 31.7 (31.4-32.1) | 32.4 (32.0-32.7) | 32.6 (32.3-33.0) | <.001 |
| Dyslipidemia | 20.8 (20.6-21.0) | 18.0 (17.7-18.4) | 19.1 (18.7-19.5) | 20.6 (20.2-21.0) | 22.2 (21.8-22.6) | 23.5 (23.0-23.9) | <.001 |
| Hypertension | 46.5 (46.3-46.7) | 48.3 (47.9-48.8) | 49.6 (49.2-50.1) | 50.6 (50.1-51.1) | 48.7 (48.3-49.1) | 36.6 (36.3-36.9) | <.001 |
| Obesity | 14.2 (14.0-14.3) | 11.8 (11.5-12.1) | 12.9 (12.6-13.2) | 14.2 (13.9-14.5) | 15.3 (14.9-15.6) | 16.3 (15.9-16.6) | <.001 |
| Pneumonia | 14.2 (14.0-14.3) | 14.0 (13.7-14.2) | 14.2 (13.9-14.5) | 14.5 (14.2-14.7) | 14.0 (13.8-14.3) | 14.1 (13.9-14.3) | .76 |
| Stroke | 3.5 (3.4-3.5) | 3.3 (3.2-3.4) | 3.3 (3.2-3.4) | 3.5 (3.4-3.6) | 3.5 (3.4-3.6) | 3.6 (3.5-3.7) | <.001 |
Trends in CLD-Related Hospitalizations
The annual rate of CLD-related hospitalizations per 100 000 hospitalizations increased from 3056 (95% CI, 3042-3069) in 2012 to 3757 (95% CI, 3742-3772) in 2016 (P for trend < .001) (Table 1). The total number of CLD-related hospitalizations increased by 20.8% (187 690 in 2012 to 226 714 in 2016). When stratified by age, while the proportion of hospitalizations for patients aged 45 to 64 years decreased (55.5% [95% CI, 55.1%-55.9%] in 2012 to 50.3% [95% CI, 49.9%-50.6%] in 2016; P for trend < .001), the proportion for those aged 65 years or older showed a considerable increase (27.4% [95% CI, 26.9%-27.9%] in 2012 to 32.2% [95% CI, 31.7%-32.6%] in 2016; P for trend < .001). Mean (SD) age increased (56.8 [14.2] years in 2012 to 57.8 [14.6] years in 2016; P for trend < .001). There were also increases in the proportion of hospitalizations for patients enrolled in Medicare (41.7% [95% CI, 41.1%-42.2%] to 43.6% [95% CI, 43.1%-44.1%]; P for trend < .001). The proportion enrolled in Medicaid also increased, while the proportion of uninsured (ie, self-pay) hospitalizations decreased (Table 1). Among CLD etiologies, the proportion of hospitalizations with HBV and HCV decreased (Table 1), while the proportion with alcoholic cirrhosis increased (19.4% [95% CI, 19.1%-19.8%] in 2012 to 37.7% [95% CI, 37.2%-38.1%] in 2016) (P for trend < .001 for all). The proportion of hospitalizations with NAFLD increased from 18.6% (95% CI, 18.2%-19.0%) in 2012 to 21.4% (95% CI, 21.0%-21.8%) in 2015; however, it decreased to 18.0% (95% CI, 17.6%-18.4%) in 2016. The proportion of hospitalizations with cirrhosis and 1 or more concurrent complication showed substantial increases (Table 1). The comorbidity burden among CLD-related hospitalizations showed a significant increase for all comorbid conditions analyzed.
In-Hospital Mortality Among CLD-Related Hospitalizations
Among CLD-related hospitalizations, the crude in-hospital mortality rate remained stable from 7.4% (95% CI, 7.2%-7.6%) in 2012 to 7.3% (95% CI, 7.1%-7.4%) in 2016 (P for trend = .33) (Table 2), while the overall adjusted in-hospital mortality rate showed a decrease (odds ratio, 0.96; 95% CI, 0.95-0.96; P for trend < .001) (eTable 3 in the Supplement). The proportion of in-hospital deaths increased with increasing age (Table 2). Despite lower proportions of Asian/Pacific Islander individuals among the total cohort, those with Asian/Pacific Islander or African American background had higher rates of in-hospital death compared with individuals of other races (Table 2). Rates of in-hospital mortality were higher among CLD-related hospitalizations with Medicare compared with other insurance types (Table 2). Among etiologies, hospitalizations with HBV and HCV had relatively low in-hospital mortality rates and showed small increases (Table 2), while hospitalizations with alcoholic cirrhosis had the highest in-hospital mortality rate and showed the greatest increase (11.1% [95% CI, 10.7%-11.5%] in 2012 to 13.4% [95% CI, 13.1%-13.7%] in 2016, P for trend < .001). The overall rate of alcoholic cirrhosis was 11.9% (95% CI, 11.7%-12.0%). The in-hospital mortality rate among hospitalizations of patients with cirrhosis increased significantly, and an increasing number of concurrent cirrhosis-related complications was associated with increasing in-hospital mortality rates (Table 2). For example, the in-hospital mortality rate among patients with 2 or more cirrhosis-related complications was considerably higher than the rate among patients who had cirrhosis but no cirrhosis-related complications (13.1% [95% CI, 12.9%-13.3%] vs 4.8% [95% CI, 4.7%-4.9%]; P < .001). Presence of hepatocellular carcinoma was also associated with a high mortality rate (9.8% [95% CI, 9.5%-10.1%]).
Table 2. Trends in In-Hospital Mortality.
| Characteristic | Proportion with in-hospital mortality, weighted % (95% CI) | P value for trend | |||||
|---|---|---|---|---|---|---|---|
| Total | 2012 | 2013 | 2014 | 2015 | 2016 | ||
| Overall | 7.4 (7.4-7.5) | 7.4 (7.2-7.6) | 7.5 (7.3-7.6) | 7.6 (7.4-7.8) | 7.4 (7.3-7.6) | 7.3 (7.1-7.4) | .33 |
| Age, y | |||||||
| <25 | 2.6 (2.3-2.8) | 2.7 (2.1-3.3) | 2.2 (1.8-2.8) | 2.5 (2.0-3.1) | 2.6 (2.1-3.3) | 2.8 (2.3-3.4) | .43 |
| 25-44 | 3.7 (3.5-4.0) | 3.6 (3.4-3.9) | 3.9 (3.6-4.1) | 3.8 (3.6-4.1) | 3.5 (3.3-3.8) | 3.7 (3.5-4.0) | .77 |
| 45-64 | 6.5 (6.4-6.5) | 6.4 (6.2-6.6) | 6.5 (6.3-6.7) | 6.5 (6.4-6.7) | 6.5 (6.3-6.7) | 6.4 (6.2-6.6) | .62 |
| ≥65 | 11.4 (11.3-11.5) | 11.7 (11.4-12.0) | 11.6 (11.3-11.9) | 11.9 (11.6-12.2) | 11.3 (11.0-11.6) | 10.7 (10.5-11.0) | <.001 |
| Sex | |||||||
| Male | 7.4 (7.4-7.5) | 7.4 (7.2-7.6) | 7.5 (7.3-7.7) | 7.6 (7.4-7.8) | 7.4 (7.2-7.6) | 7.3 (7.1-7.5) | .39 |
| Female | 7.4 (7.3-7.5) | 7.4 (7.2-7.6) | 7.5 (7.3-7.7) | 7.6 (7.4-7.8) | 7.5 (7.3-7.7) | 7.3 (7.1-7.5) | .47 |
| Race | |||||||
| White | 7.5 (7.4-7.6) | 7.5 (7.3-7.7) | 7.5 (7.3-7.7) | 7.7 (7.5-7.9) | 7.5 (7.3-7.7) | 7.3 (7.1-7.5) | .23 |
| African American | 7.7 (7.5-7.8) | 7.4 (7.0-7.8) | 7.5 (7.2-7.9) | 7.8 (7.4-8.2) | 8.0 (7.6-8.4) | 7.7 (7.4-8.0) | .09 |
| Hispanic | 6.3 (6.1-6.4) | 6.4 (6.1-6.8) | 6.5 (6.2-6.9) | 6.4 (6.1-6.8) | 6.0 (5.7-6.4) | 6.0 (5.7-6.3) | .02 |
| Asian/Pacific Islander | 8.8 (8.4-9.2) | 8.7 (7.8-9.6) | 9.3 (8.4-10.2) | 9.0 (8.2-9.9) | 8.7 (7.9-9.5) | 8.3 (7.6-9.1) | .25 |
| Insurance | |||||||
| Medicare | 9.1 (9.0-9.2) | 9.1 (8.8-9.3) | 9.2 (8.9-9.4) | 9.4 (9.1-9.6) | 9.1 (8.9-9.4) | 8.8 (8.6-9.0) | .12 |
| Medicaid | 5.5 (5.4-5.6) | 5.5 (5.3-5.8) | 5.8 (5.5-6.1) | 5.6 (5.3-5.8) | 5.3 (5.0-5.5) | 5.4 (5.2-5.6) | .05 |
| Private, including health maintenance organization | 6.8 (6.7-6.9) | 6.9 (6.6-7.2) | 6.6 (6.4-6.9) | 6.8 (6.5-7.1) | 6.9 (6.6-7.1) | 6.7 (6.4-7.0) | .77 |
| Self-pay | 6.0 (5.8-6.2) | 5.9 (5.5-6.3) | 6.0 (5.6-6.5) | 6.4 (5.9-6.9) | 5.9 (5.5-6.4) | 5.6 (5.2-6.1) | .46 |
| Alcoholic cirrhosis | 11.9 (11.7-12.0) | 11.1 (10.7-11.5) | 10.7 (10.3-11.0) | 10.7 (10.4-11.1) | 11.8 (11.4-12.1) | 13.4 (13.1-13.7) | <.001 |
| Hepatitis B virus | 4.4 (4.2-4.6) | 4.3 (3.8-4.7) | 4.2 (3.8-4.7) | 4.5 (4.1-5.0) | 4.4 (4.0-4.9) | 4.4 (4.0-4.9) | .43 |
| Hepatitis C virus | 4.1 (4.1-4.2) | 3.9 (3.7-4.1) | 4.2 (4.0-4.4) | 4.2 (4.0-4.4) | 4.3 (4.2-4.5) | 4.0 (3.8-4.1) | .44 |
| Nonalcoholic fatty liver disease | 4.1 (4.0-4.3) | 4.8 (4.5-5.0) | 4.6 (4.4-4.9) | 4.7 (4.5-4.9) | 4.0 (3.8-4.2) | 2.7 (2.5-2.9) | <.001 |
| Hepatocellular carcinoma | 9.8 (9.5-10.1) | 9.7 (9.0-10.4) | 9.4 (8.6-10.1) | 9.9 (9.2-10.6) | 10.1 (9.4-10.8) | 9.8 (9.2-10.5) | .37 |
| Cirrhosis | 9.1 (9.0-9.2) | 8.3 (8.1-8.5) | 8.1 (7.9-8.4) | 8.3 (8.1-8.5) | 9.0 (8.8-9.2) | 11.2 (10.9-11.4) | <.001 |
| Cirrhosis-related complications | |||||||
| 0 | 4.8 (4.7-4.9) | 5.0 (4.7-5.3) | 5.3 (5.0-5.5) | 5.2 (4.9-5.5) | 4.6 (4.4-4.9) | 4.1 (3.9-4.3) | <.001 |
| 1 | 9.6 (9.4-9.7) | 8.0 (7.7-8.2) | 7.6 (7.3-7.9) | 7.9 (7.6-8.1) | 9.6 (9.3-9.8) | 13.6 (13.2-13.9) | <.001 |
| ≥2 | 13.1 (12.9-13.3) | 13.2 (12.7-13.7) | 12.8 (12.3-13.3) | 12.8 (12.3-13.3) | 12.9 (12.5-13.4) | 13.7 (13.2-14.1) | .09 |
| Coronary artery disease | 9.4 (9.2-9.6) | 9.2 (8.8-9.6) | 9.4 (9.0-9.8) | 9.7 (9.3-10.1) | 9.2 (8.9-9.6) | 9.4 (9.1-9.8) | .71 |
| Congestive heart failure | 12.8 (12.6-13.0) | 12.8 (12.4-13.3) | 13.5 (13.0-13.9) | 13.3 (12.8-13.7) | 12.7 (12.3-13.1) | 12.1 (11.8-12.5) | <.001 |
| Chronic kidney disease | 10.2 (10.1-10.4) | 10.3 (10.0-10.7) | 10.5 (10.2-10.9) | 10.5 (10.2-10.9) | 10.3 (10.0-10.6) | 9.7 (9.5-10.0) | .002 |
| Diabetes | 6.6 (6.5-6.7) | 6.6 (6.4-6.8) | 6.6 (6.3-6.8) | 6.6 (6.4-6.9) | 6.6 (6.4-6.8) | 6.5 (6.3-6.7) | .31 |
| Dyslipidemia | 6.5 (6.3-6.6) | 6.3 (6.0-6.5) | 6.3 (6.0-6.6) | 6.7 (6.4-7.0) | 6.5 (6.2-6.7) | 6.5 (6.3-6.8) | .10 |
| Hypertension | 6.6 (6.5-6.7) | 6.8 (6.6-7.0) | 6.8 (6.6-7.0) | 7.0 (6.8-7.2) | 6.7 (6.6-6.9) | 5.6 (5.4-5.8) | <.001 |
| Obesity | 6.2 (6.0-6.3) | 6.3 (5.9-6.6) | 6.1 (5.7-6.4) | 6.3 (6.0-6.7) | 6.2 (5.9-6.5) | 6.0 (5.8-6.3) | .46 |
| Pneumonia | 15.2 (15.0-15.4) | 15.1 (14.6-15.6) | 15.3 (14.8-15.8) | 15.7 (15.2-16.2) | 15.2 (14.7-15.6) | 14.8 (14.4-15.3) | .33 |
| Stroke | 14.2 (13.8-14.6) | 13.4 (12.6-14.3) | 13.6 (12.7-14.5) | 14.8 (13.9-15.7) | 14.4 (13.6-15.3) | 14.5 (13.7-15.2) | .04 |
Hospitalization Costs Among CLD-Related Hospitalizations
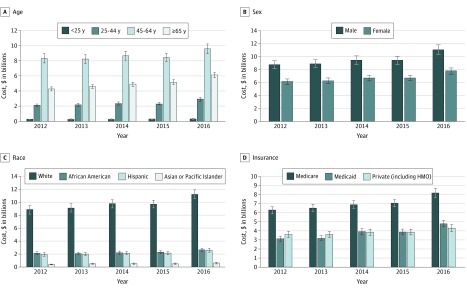
The mean cost per CLD-related hospitalization was $16 271 (95% CI, $16 069-$16 473), while the total national estimated cost for CLD-related hospitalizations over the study period was $81.1 billion (95% CI, $79.4 billion to $82.7 billion). The adjusted mean cost per CLD-related hospitalization increased by 0.62% (95% CI, 0.07%-1.18%; P for trend = .03) over the study period (eTable 3 in the Supplement). From 2012 to 2016, mean hospitalization costs increased from $15 611 (95% CI, $13 870-$17 353) to $17 478 (95% CI, $15 653-$19 304) (P for trend < .001), and total hospitalization costs increased from $14.9 billion (95% CI, $13.9 billion to $15.9 billion) in 2012 to $18.8 billion (95% CI, $17.6 billion to $20.0 billion) in 2016 (Table 3). While mean and total hospitalization costs increased for all age groups (Table 3 and Figure 1A), total costs were highest among hospitalized patients aged 45 to 64 years (Figure 1A). Mean hospitalization costs increased significantly among men and women; however, men had a higher total cost burden ($47.6 billion [95% CI, $46.5 billion to $48.6 billion] vs $33.5 billion [95% CI, $32.8 billion to $34.2 billion]) (Figure 1B). While African American individuals had the most significant increase in mean hospitalization costs, mean costs were highest among Asian/Pacific Islander individuals (Table 3), and white patients had the highest total economic burden ($48.5 billion [95% CI, $47.5 billion to $49.6 billion]) (Figure 1C).
Table 3. Trends in Mean Hospitalization Costs.
| Characteristic | Costs, weighted mean (95% CI), 2016 US dollars | P value for trend | ||||
|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | ||
| Total costs (95% CI), 2016 US dollars, billions | 14.9 (13.9-15.9) | 15.2 (14.2-16.2) | 16.1 (15.0-17.1) | 16.1 (15.1-17.1) | 18.8 (17.6-20.0) | |
| Overall | 16 168 (15 667-16 670) | 16 094 (15 618-16 571) | 16 332 (15 821-16 843) | 15 763 (15 324-16 203) | 16 919 (16 417-17 422) | <.001 |
| Age, y | ||||||
| <25 | 15 611 (13 870-17 353) | 15 731 (14 043-17 420) | 16 958 (15 234-18 681) | 16 823 (15 434-18 212) | 17 478 (15 653-19 304) | <.001 |
| 25-44 | 14 607 (13 969-15 245) | 14 766 (14 136-15 397) | 15 098 (14 482-15 714) | 14 239 (13 702-14 777) | 16 038 (15 371-16 704) | <.001 |
| 45-64 | 16 211 (15 656-16 765) | 16 009 (15 501-16 516) | 16 389 (15 822-16 955) | 15 842 (15 365-16 319) | 17 071 (16 500-17 642) | <.001 |
| ≥65 | 17 013 (16 543-17 483) | 16 996 (16 509-17 483) | 16 855 (16 398-17 313) | 16 361 (15 944-16 779) | 17 100 (16 674-17 527) | .01 |
| Sex | ||||||
| Male | 16 424 (15 883-16 966) | 16 458 (15 938-16 979) | 16 738 (16 184-17 291) | 16 180 (15 710-16 650) | 17 426 (16 870-17 982) | <.001 |
| Female | 15 818 (15 335-16 302) | 15 601 (15 140-16 062) | 15 789 (15 299-16 278) | 15 212 (14 785-15 639) | 16 247 (15 780-16 713) | <.001 |
| Race | ||||||
| White | 15 540 (15 031-16 050) | 15 475 (14 998-15 952) | 15 710 (15 214-16 205) | 15 079 (14 672-15 487) | 15 994 (15 531-16 457) | <.001 |
| African American | 16 615 (16 046-17 185) | 16 494 (15 905-17 083) | 16 923 (16 340-17 510) | 16 873 (16 311-17 435) | 18 036 (17 370-18 703) | <.001 |
| Hispanic | 16 391 (15 275-17 507) | 16 516 (15 387-17 646) | 16 848 (15 848-17 849) | 15 773 (14 899-16 647) | 17 434 (16 427-18 442) | <.001 |
| Asian/Pacific Islander | 21 278 (19 163-23 392) | 22 312 (20 711-23 913) | 22 383 (20 374-24 391) | 20 262 (18 984-21 540) | 22 302 (20 516-24 088) | .01 |
| Insurance | ||||||
| Medicare | 16 435 (15 953-16 916) | 16 384 (15 912-16 856) | 16 391 (15 911-16 870) | 15 976 (15 562-16 391) | 16 945 (16 504-17 387) | <.001 |
| Medicaid | 15 660 (15 052-16 268) | 15 748 (15 215-16 281) | 16 215 (15 673-16 757) | 15 335 (14 868-15 803) | 17 229 (16 631-17 826) | <.001 |
| Private, including health maintenance organization | 17 832 (16 982-18 681) | 17 558 (16 760-18 355) | 17 615 (16 758-18 473) | 16 934 (16 202-17 667) | 17 726 (16 919-18 533) | |
| Self-pay | 12 728 (12 250-13 207) | 12 690 (12 215-13 165) | 12 944 (12 487-13 400) | 12 277 (11 821-12 732) | 13 160 (12 442-13 878) | |
| Alcoholic cirrhosis | 17 787 (17 140-18 434) | 17 615 (16 963-18 266) | 17 677 (16 977-18 376) | 17 453 (16 877-18 028) | 20 282 (19 560-21 004) | <.001 |
| Hepatitis B virus | 15 203 (14 429-15 977) | 15 454 (14 659-16 248) | 16 029 (15 112-16 947) | 15 533 (14 749-16 318) | 16 970 (16 069-17 871) | <.001 |
| Hepatitis C virus | 13 991 (13 502-14 479) | 14 164 (13 669-14 659) | 14 290 (13 810-14 770) | 14 197 (13 758-14 636) | 15 085 (14 602-15 568) | <.001 |
| Nonalcoholic fatty liver disease | 13 566 (13 119-14 013) | 13 346 (12 924-13 769) | 13 456 (13 021-13 891) | 13 203 (12 847-13 560) | 13 769 (13 387-14 151) | <.001 |
| Hepatocellular carcinoma | 18 512 (17 162-19 863) | 18 111 (16 528-19 694) | 17 861 (16 579-19 143) | 18 049 (16 718-19 380) | 18 952 (17 563-20 341) | .14 |
| Cirrhosis | 16 285 (15 663-16 908) | 16 190 (15 573-16 806) | 16 309 (15 641-16 976) | 16 298 (15 726-16 870) | 19 185 (18 485-19 885) | <.001 |
| Cirrhosis-related complications | ||||||
| 0 | 13 313 (12 868-13 759) | 13 402 (12 950-13 855) | 13 390 (12 950-13 829) | 13 165 (12 803-13 528) | 13 616 (13 246-13 985) | <.001 |
| 1 | 15 303 (14 775-15 831) | 15 170 (14 652-15 689) | 15 169 (14 673-15 666) | 15 747 (15 280-16 213) | 20 041 (19 415-20 667) | <.001 |
| ≥2 | 22 185 (20 858-23 512) | 21 759 (20 530-22 988) | 21 958 (20 418-23 498) | 21 027 (19 821-22 233) | 23 279 (21 718-24 841) | .20 |
| Coronary artery disease | 17 096 (16 531-17 660) | 16 699 (16 150-17 249) | 17 297 (16 714-17 880) | 16 627 (16 195-17 059) | 17 712 (17 194-18 230) | <.001 |
| Congestive heart failure | 23 012 (22 073-23 951) | 21 906 (21 118-22 695) | 22 530 (21 704-23 356) | 21 292 (20 600-21 984) | 22 489 (21 715-23 263) | .20 |
| Chronic kidney disease | 19 803 (18 940-20 667) | 19 228 (18 526-19 929) | 19 517 (18 742-20 291) | 18 562 (17 960-19 164) | 20 049 (19 274-20 823) | .01 |
| Diabetes | 15 800 (15 321-16 279) | 15 464 (15 028-15 900) | 15 553 (15 093-16 014) | 15 373 (14 958-15 788) | 16 213 (15 769-16 657) | <.001 |
| Dyslipidemia | 15 094 (14 636-15 553) | 14 994 (14 614-15 374) | 15 373 (14 949-15 797) | 14 962 (14 618-15 306) | 15 787 (15 386-16 186) | <.001 |
| Hypertension | 15 930 (15 448-16 413) | 15 529 (15 107-15 951) | 15 843 (15 394-16 292) | 15 209 (14 839-15 579) | 14 913 (14 527-15 299) | .56 |
| Obesity | 17 692 (17 096-18 287) | 17 318 (16 750-17 887) | 17 471 (16 909-18 032) | 17 200 (16 685-17 714) | 18 162 (17 591-18 734) | .01 |
| Pneumonia | 27 959 (26 718-29 200) | 27 066 (25 973-28 160) | 27 815 (26 694-28 936) | 25 710 (24 768-26 653) | 28 360 (27 217-29 503) | .17 |
| Stroke | 25 569 (24 115-27 024) | 24 944 (23 507-26 381) | 25 885 (24 499-27 272) | 24 571 (23 348-25 794) | 28 509 (26 978-30 039) | <.001 |
Figure 1. Trends in Total Hospitalization Costs Stratified by Demographic Characteristics.
Costs are shown in 2016 US dollars. Error bars represent 95% CIs; HMO, health maintenance organization.
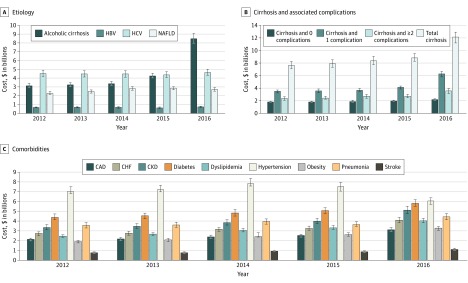
Compared with other insurance types, hospitalizations of patients with private insurance had higher mean costs (Table 3), hospitalizations of those enrolled in Medicare had a higher total burden (Figure 1D), and mean costs for hospitalizations of patients enrolled in Medicaid experienced the greatest increase ($15 660 [95% CI, $15 052-$16 268] in 2012 to $17 229 [95% CI, $16 631-$17 826] in 2016; P for trend < .001). Cost burden increased across all etiologies, with a higher total cost burden among hospitalizations with alcoholic cirrhosis ($22.7 billion [95% CI, $22.1 billion to $23.2 billion]) or hepatitis C virus ($22.6 billion [95% CI, $22.1 billion to $23.2 billion]) (Table 3 and Figure 2A). Mean costs per hospitalization were higher among patients with alcoholic cirrhosis and HBV compared with the other etiologies. Hospitalizations for patients with HCV had the highest total costs from 2012 to 2015, and those with alcoholic cirrhosis had the highest total costs in 2016 (Figure 2A). Hospitalization costs increased among patients with cirrhosis, with a higher burden among patients with concurrent cirrhosis-related complications (Table 3 and Figure 2B). While CLD-related hospitalizations with concurrent congestive heart failure, pneumonia, or stroke had relatively higher mean costs, hospitalizations with concurrent diabetes and hypertension had a higher total cost burden compared with other comorbidities (Figure 2C).
Figure 2. Trends in Total Hospitalization Costs Stratified by Clinical Characteristics.
Costs are shown in 2016 US dollars. CAD indicates coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; HBV, hepatitis B virus; HCV, hepatitis C virus; NAFLD, nonalcoholic fatty liver disease; and error bars, 95% CIs.
Discussion
Among a large, nationally representative sample of hospitalized US adults from 2012 to 2016, there was a 20.8% increase in the number of CLD-related hospitalizations, resulting in a 26.2% increase in the total estimated hospitalization costs. In 2016, CLD-related hospitalizations alone accounted for $18.8 billion of the economic burden.
The observed increases in the clinical and economic burden of CLD among hospitalized adults in the US is a major public health concern. Improvements in the management of viral hepatitis, specifically the introduction of direct-acting antivirals for HCV treatment,29 have led to significantly reduced morbidity and mortality associated with HBV and HCV.30,31,32,33,34,35,36 However, existing studies4,11 highlight the growing epidemic of NAFLD in the US. Studies2,5,6 have also shown the rising prevalence of ALD and increasing disease severity among patients with ALD, with consistent trends across different nationally representative databases. In this study, while the proportion of patients with alcoholic cirrhosis and NAFLD showed an increasing trend, the highest mortality burden was among hospitalizations with alcoholic cirrhosis, and the major cost burden was distributed between hospitalizations of patients with alcoholic cirrhosis and HCV. Even with decreasing HCV-associated morbidity and mortality, the high HCV cost burden may be due to aging patients with HCV cirrhosis and continued suboptimal access to HCV treatment.37,38
These epidemiological trends likely reflect the lack of early diagnosis, of ALD and NAFLD in particular, and the paucity of effective therapies to treat and prevent disease progression. The findings of the current study raise concern regarding the vast burden of CLD on the US health care system, and the impending wave of patients with ALD and NAFLD will further stress the health care system unless precautionary actions are taken. There is an urgent need for greater awareness among patients and clinicians about the consequences of unhealthy alcohol use, the need for consistent screening for alcohol use disorder, and timely implementation of prevention and intervention strategies aimed specifically at addressing alcohol use disorders.
In this study, presence of cirrhosis and cirrhosis-related complications resulted in a higher mortality rate and cost burden on the health care system. Tapper et al39 applied a quality improvement intervention on an inpatient liver unit that resulted in a 40% reduction in 30-day readmissions among patients with cirrhosis, which was likely driven by a decrease in readmissions for hepatic encephalopathy. Kanwal et al40 demonstrated that while early clinic follow-up following hospital discharge led to an increase in readmissions, this ultimately translated into reduced overall mortality. Similarly, other studies have proposed quality improvement tools and shown that prevention and early management of cirrhosis are cost-effective.41,42,43,44,45,46 However, owing to the lack of nationally representative data to guide the optimal allocation of resources and preventive efforts, there is a lag in the application and use of these evidence-based protocols by clinicians.
With advancements in medical care, there is a shift in the burden toward an older population. This is reflected in the current study, which observed increases in the mean age of hospitalized patients with CLD and found that 42.7% of hospitalizations were for patients enrolled in Medicare. This is particularly concerning given that older populations have higher risk of comorbidities. A recent study by Younossi et al4 showed that increases in the prevalence of NAFLD were associated with increasing rates of obesity and type 2 diabetes.47,48,49 This study demonstrated similar observations showing concurrent increases in the comorbidity burden, albeit among a hospitalized cohort. As with prior studies, the presence of these comorbidities was associated with worse prognosis among this CLD cohort.6,50,51
The proportion of CLD-related hospitalizations for patients enrolled in Medicare increased significantly over the study period, and hospitalizations for those with Medicare experienced the highest in-hospital mortality rate as well as the greatest total economic burden. Asrani et al14 found a similar trend among hospitalizations covered by Medicare (increase from 31.8% to 41.5%). These observations, along with the results of the current study, draw attention to the imminent surge in the burden of older patients with CLD and call attention to the need for greater research aimed at preventive care and novel quality-driven health care delivery so that we may adequately address the future needs of patients with CLD in a cost-effective and cost-efficient manner.
Limitations
As with many studies using large claims databases, these findings should be interpreted within the context of certain limitations.52 The NIS records data per hospitalization, and not per individual patient, without linkage or follow-up data. Owing to the cross-sectional nature of the database, longitudinal analysis is not possible, and no causal inferences can be drawn. Thus, there may be repeat hospitalizations of patients with CLD among this study cohort. Nevertheless, given that the main objective of this study was to characterize the overall clinical and economic burden of CLD hospitalizations in the US, these results still provide critical data to address this important public health concern. This study focused specifically on alcoholic cirrhosis to minimize error in the estimates given the limitations inherent in the use of ICD-9-CM coding-based algorithms to identify and isolate ALD as a whole. However, because this study focused specifically on alcoholic cirrhosis, it may not capture the true burden of ALD (eg, the burden among patients with alcoholic hepatitis who may be hospitalized but do not have cirrhosis). A considerable proportion of hospitalizations did not have an identifiable underlying etiology. Hospitalizations in this category related to CLD may be attributable to other chronic diseases (eg, cholestatic liver diseases). The changes in coding and data structure of the NIS in 2015 may have resulted in misclassification bias,21 and the P value for trend for some characteristics may not be as informative owing to these changes. Chronic liver disease with mention of alcohol is more thoroughly defined in ICD-10-CM (K70.xx) compared with the ICD-9-CM; however, NAFLD ICD codes still lack specificity in both coding systems. This change may have contributed to the apparent increased burden of alcoholic cirrhosis and decreased burden of NAFLD in 2016. The loss of Elixhauser comorbidity software within the NIS for the fourth quarter of 2015 and for 2016 may have led to underestimation of the burden of certain comorbidities (eg, hypertension). We tried to circumvent these limitations through a comprehensive review of ICD codes to ensure that our definitions using ICD-10-CM codes are congruent with the ICD-9-CM codes previously used.
Conclusions
While this study is unable to account for outpatient outcomes, including mortality following hospitalization and long-term costs associated with chronic care, inpatient burden is a common and relevant metric used to estimate the health care burden for chronic conditions. Similar to other chronic diseases, a large proportion of CLD-related health care burden is reflected in inpatient mortality and resource utilization. In addition, severe decompensation often leads to hospitalization, which has been linked to early mortality among patients with other chronic conditions.46,53,54,55 Thus, despite inherent limitations and potential underestimation of the true burden of CLD, this study provides a comprehensive view of trends in CLD-related inpatient resource utilization in the US as a stepping stone to guide health care policy and more efficient allocation of resources to address the looming burden of an aging CLD population with higher morbidity and mortality.
eFigure. Flow Diagram for the Identification of CLD-Related Hospitalizations and Categorization Into the Etiologies of Interest for Trends Analysis
eTable 1. List of ICD Codes Used in CLD Definition
eTable 2. List of ICD Codes Used for Other Definitions
eTable 3. Regression Models for Trends in In-Hospital Mortality and Mean Hospitalization Costs Among CLD-Related Hospitalizations
References
- 1.Asrani SK, Larson JJ, Yawn B, Therneau TM, Kim WR. Underestimation of liver-related mortality in the United States. Gastroenterology. 2013;145(2):-. doi: 10.1053/j.gastro.2013.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong T, Dang K, Ladhani S, Singal AK, Wong RJ. Prevalence of alcoholic fatty liver disease among adults in the United States, 2001-2016. JAMA. 2019;321(17):1723-1725. doi: 10.1001/jama.2019.2276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313(22):2263-2273. doi: 10.1001/jama.2015.5370 [DOI] [PubMed] [Google Scholar]
- 4.Younossi ZM, Stepanova M, Younossi Y, et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut. 2020;69(3):564-568. doi: 10.1136/gutjnl-2019-318813 [DOI] [PubMed] [Google Scholar]
- 5.Dang K, Hirode G, Singal A, Sundaram V, Wong RJ. Alcoholic liver disease epidemiology in the United States: a retrospective analysis of three United States databases. Am J Gastroenterol. 2019. doi: 10.14309/ajg.000000000000038 [DOI] [PubMed] [Google Scholar]
- 6.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ. 2018;362:k2817. doi: 10.1136/bmj.k2817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen AL, Park H, Nguyen P, Sheen E, Kim YA, Nguyen MH. Rising inpatient encounters and economic burden for patients with nonalcoholic fatty liver disease in the USA. Dig Dis Sci. 2019;64(3):698-707. doi: 10.1007/s10620-018-5326-7 [DOI] [PubMed] [Google Scholar]
- 8.Allen AM, Van Houten HK, Sangaralingham LR, Talwalkar JA, McCoy RG. Healthcare cost and utilization in nonalcoholic fatty liver disease: real-world data from a large U.S. claims database. Hepatology. 2018;68(6):2230-2238. doi: 10.1002/hep.30094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen MH, Burak Ozbay A, Liou I, et al. Healthcare resource utilization and costs by disease severity in an insured national sample of US patients with chronic hepatitis B. J Hepatol. 2019;70(1):24-32. doi: 10.1016/j.jhep.2018.09.021 [DOI] [PubMed] [Google Scholar]
- 10.Younossi ZM, Zheng L, Stepanova M, Venkatesan C, Mishra A. Clinical outcomes and resource utilisation in Medicare patients with chronic liver disease: a historical cohort study. BMJ Open. 2014;4(5):e004318. doi: 10.1136/bmjopen-2013-004318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirode G, Vittinghoff E, Wong RJ. Increasing clinical and economic burden of nonalcoholic fatty liver disease among hospitalized adults in the United States. J Clin Gastroenterol. 2019;53(10):765-771. doi: 10.1097/MCG.0000000000001229 [DOI] [PubMed] [Google Scholar]
- 12.Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9(6):524-530.e1. doi: 10.1016/j.cgh.2011.03.020 [DOI] [PubMed] [Google Scholar]
- 13.Hirode G, Vittinghoff E, Wong RJ. Increasing burden of hepatic encephalopathy among hospitalized adults: an analysis of the 2010-2014 National Inpatient Sample. Dig Dis Sci. 2019;64(6):1448-1457. doi: 10.1007/s10620-019-05576-9 [DOI] [PubMed] [Google Scholar]
- 14.Asrani SK, Kouznetsova M, Ogola G, et al. Increasing health care burden of chronic liver disease compared with other chronic diseases, 2004-2013. Gastroenterology. 2018;155(3):719-729.e4. doi: 10.1053/j.gastro.2018.05.032 [DOI] [PubMed] [Google Scholar]
- 15.Asrani SK, Hall L, Hagan M, et al. Trends in chronic liver disease-related hospitalizations: a population-based study. Am J Gastroenterol. 2019;114(1):98-106. doi: 10.1038/s41395-018-0365-4 [DOI] [PubMed] [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344-349. doi: 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 17.Houchens R, Ross D, Elixhauser A, Jiang J. Nationwide Inpatient Sample Redesign: Final Report US Agency for Healthcare Research and Quality; 2014. Accessed June 10, 2019. https://www.hcup-us.ahrq.gov/db/nation/nis/nisrelatedreports.jsp
- 18.Barrett M. 2015 Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample: Change in Structure and Data Elements Caused by Transition to ICD-10-CM/PCS US Agency for Healthcare Research and Quality; 2017. Accessed October 16, 2019. https://www.hcup-us.ahrq.gov/datainnovations/icd10_resources.jsp
- 19.Healthcare Cost and Utilization Project Introduction to the HCUP National Inpatient Sample (NIS) 2016. Healthcare Cost and Utilization Project; 2018. [DOI] [PubMed] [Google Scholar]
- 20.Barrett M, Bailey M. 2016 Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample: Change in Structure Due to ICD-10-CM/PCS US Agency for Healthcare Research and Quality; 2018. Accessed October 16, 2019. https://www.hcup-us.ahrq.gov/datainnovations/icd10_resources.jsp
- 21.Gibson T, Casto A, Young J, Karnell L, Coenen N. Impact of ICD-10-CM/PCS on Research Using Administrative Databases. HCUP Methods Series Report# 2016-02 US Agency for Healthcare Research and Quality; 2016. Accessed October 16, 2019. https://www.hcup-us.ahrq.gov/reports/methods/methods.jsp
- 22.Beste LA, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001-2013. Gastroenterology. 2015;149(6):1471-1482.e5. doi: 10.1053/j.gastro.2015.07.056 [DOI] [PubMed] [Google Scholar]
- 23.Allen AM, Therneau TM, Larson JJ, Coward A, Somers VK, Kamath PS. Nonalcoholic fatty liver disease incidence and impact on metabolic burden and death: a 20 year-community study. Hepatology. 2018;67(5):1726-1736. doi: 10.1002/hep.29546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bureau of Labor Statistics CPI Inflation Calculator. Accessed September 29, 2019. https://data.bls.gov/cgi-bin/cpicalc.pl
- 25.Healthcare Cost and Utilization Project (HCUP) Cost-to-Charge Ratio Files: User Guide for National Inpatient Sample (NIS) CCRs US Agency for Healthcare Research and Quality; 2018. Accessed September 28, 2019. https://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp
- 26.Khera R, Angraal S, Couch T, et al. Adherence to methodological standards in research using the National Inpatient Sample. JAMA. 2017;318(20):2011-2018. doi: 10.1001/jama.2017.17653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8(1):3-15. doi: 10.1177/096228029900800102 [DOI] [PubMed] [Google Scholar]
- 28.Bennett DA. How can I deal with missing data in my study? Aust N Z J Public Health. 2001;25(5):464-469. doi: 10.1111/j.1467-842X.2001.tb00294.x [DOI] [PubMed] [Google Scholar]
- 29.Moon AM, Green PK, Berry K, Ioannou GN. Transformation of hepatitis C antiviral treatment in a national healthcare system following the introduction of direct antiviral agents. Aliment Pharmacol Ther. 2017;45(9):1201-1212. doi: 10.1111/apt.14021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151-171. doi: 10.1016/j.jhep.2018.09.014 [DOI] [PubMed] [Google Scholar]
- 31.Marcellin P, Kutala BK. Liver diseases: a major, neglected global public health problem requiring urgent actions and large-scale screening. Liver Int. 2018;38(suppl 1):2-6. doi: 10.1111/liv.13682 [DOI] [PubMed] [Google Scholar]
- 32.Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2015 annual data report: liver. Am J Transplant. 2017;17(suppl 1):174-251. doi: 10.1111/ajt.14126 [DOI] [PubMed] [Google Scholar]
- 33.Hernaez R, Solà E, Moreau R, Ginès P. Acute-on-chronic liver failure: an update. Gut. 2017;66(3):541-553. doi: 10.1136/gutjnl-2016-312670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology. 2017;152(5):1090-1099.e1. doi: 10.1053/j.gastro.2017.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim D, Li AA, Gadiparthi C, et al. Changing trends in etiology-based annual mortality from chronic liver disease, from 2007 through 2016. Gastroenterology. 2018;155(4):1154-1163.e3. doi: 10.1053/j.gastro.2018.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Serag HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016;14(2):301-308.e1, 2. doi: 10.1016/j.cgh.2015.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davis GL, Alter MJ, El-Serag H, Poynard T, Jennings LW. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology. 2010;138(2):513-521, 521.e1-521.e6. doi: 10.1053/j.gastro.2009.09.067 [DOI] [PubMed] [Google Scholar]
- 38.Ward JW, Mermin JH. Simple, effective, but out of reach? public health implications of HCV drugs. N Engl J Med. 2015;373(27):2678-2680. doi: 10.1056/NEJMe1513245 [DOI] [PubMed] [Google Scholar]
- 39.Tapper EB, Finkelstein D, Mittleman MA, Piatkowski G, Chang M, Lai M. A quality improvement initiative reduces 30-day rate of readmission for patients with cirrhosis. Clin Gastroenterol Hepatol. 2016;14(5):753-759. doi: 10.1016/j.cgh.2015.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kanwal F, Asch SM, Kramer JR, Cao Y, Asrani S, El-Serag HB. Early outpatient follow-up and 30-day outcomes in patients hospitalized with cirrhosis. Hepatology. 2016;64(2):569-581. doi: 10.1002/hep.28558 [DOI] [PubMed] [Google Scholar]
- 41.Kanwal F, Tapper EB, Ho C, et al. Development of quality measures in cirrhosis by the Practice Metrics Committee of the American Association for the Study of Liver Diseases. Hepatology. 2019;69(4):1787-1797. doi: 10.1002/hep.30489 [DOI] [PubMed] [Google Scholar]
- 42.Kanwal F, Kramer J, Asch SM, et al. An explicit quality indicator set for measurement of quality of care in patients with cirrhosis. Clin Gastroenterol Hepatol. 2010;8(8):709-717. doi: 10.1016/j.cgh.2010.03.028 [DOI] [PubMed] [Google Scholar]
- 43.Tapper EB, Catana AM, Sethi N, et al. Direct costs of care for hepatocellular carcinoma in patients with hepatitis C cirrhosis. Cancer. 2016;122(6):852-858. doi: 10.1002/cncr.29855 [DOI] [PubMed] [Google Scholar]
- 44.Rein DB, Smith BD, Wittenborn JS, et al. The cost-effectiveness of birth-cohort screening for hepatitis C antibody in U.S. primary care settings. Ann Intern Med. 2012;156(4):263-270. doi: 10.7326/0003-4819-156-4-201202210-00378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tapper EB, Sengupta N, Hunink MG, Afdhal NH, Lai M. Cost-effective evaluation of nonalcoholic fatty liver disease with NAFLD fibrosis score and vibration controlled transient elastography. Am J Gastroenterol. 2015;110(9):1298-1304. doi: 10.1038/ajg.2015.241 [DOI] [PubMed] [Google Scholar]
- 46.Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107(2):247-252. doi: 10.1038/ajg.2011.314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organization Overweight and obesity. Accessed July 26, 2019. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- 48.Centers for Disease Control and Prevention Adult overweight and obesity. Accessed July 26, 2019. https://www.cdc.gov/obesity/data/adult.html
- 49.Centers for Disease Control and Prevention National diabetes statistics report. Accessed July 26, 2019. https://www.cdc.gov/diabetes/data/statistics/statistics-report.html
- 50.Kim WR, Lake JR, Smith JM, et al. Liver. Am J Transplant. 2016;16(suppl 2):69-98. doi: 10.1111/ajt.13668 [DOI] [PubMed] [Google Scholar]
- 51.Liu TL, Trogdon J, Weinberger M, Fried B, Barritt AS IV. Diabetes is associated with clinical decompensation events in patients with cirrhosis. Dig Dis Sci. 2016;61(11):3335-3345. doi: 10.1007/s10620-016-4261-8 [DOI] [PubMed] [Google Scholar]
- 52.Haut ER, Pronovost PJ, Schneider EB. Limitations of administrative databases. JAMA. 2012;307(24):2589. doi: 10.1001/jama.2012.6626 [DOI] [PubMed] [Google Scholar]
- 53.Chen J, Normand S-LT, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. 2011;306(15):1669-1678. doi: 10.1001/jama.2011.1474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ratib S, Fleming KM, Crooks CJ, Aithal GP, West J. 1 and 5 year survival estimates for people with cirrhosis of the liver in England, 1998-2009: a large population study. J Hepatol. 2014;60(2):282-289. doi: 10.1016/j.jhep.2013.09.027 [DOI] [PubMed] [Google Scholar]
- 55.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291(11):1358-1367. doi: 10.1001/jama.291.11.1358 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Flow Diagram for the Identification of CLD-Related Hospitalizations and Categorization Into the Etiologies of Interest for Trends Analysis
eTable 1. List of ICD Codes Used in CLD Definition
eTable 2. List of ICD Codes Used for Other Definitions
eTable 3. Regression Models for Trends in In-Hospital Mortality and Mean Hospitalization Costs Among CLD-Related Hospitalizations