Background
In humans the renin-angiotensin system is the hormone system which regulates blood pressure and vascular resistances, as well as electrolytic balance; within this important system, the angiotensin-converting enzyme (ACE), present on the surface of vascular endothelial cells, in particular those of the lungs, is deputed to the conversion of angiotensin I to angiotensin II (AII), a potent vasoconstrictive peptide [1]. For this, both ACE and AII have been widely exploited as pharmacological targets in the treatment of hypertension, heart failure or diabetic nephropathy by means of ACE inhibitors and AII receptor antagonists, respectively [1]. In addition, homologous ACE2 receptors have been identified on the oral mucosa, in type-II pneumocytes, along the intestine and on the kidney and heart endothelia [1], [2]; these receptors have been found overexpressed in course of ACE inhibitors and AII receptor antagonists administration in murine models [3], [4].
Hypothesis
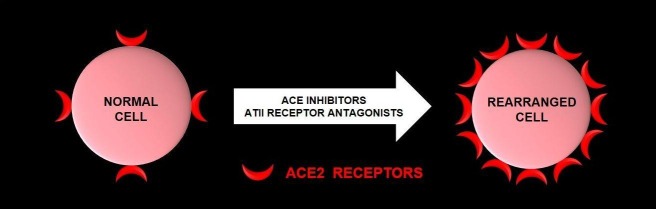
Surprisingly, the surface spike proteins of the ‘severe-acute-respiratory-syndrome-coronavirus-2′ (SARS-CoV-2), the etiological agent of the ongoing ‘coronavirus disease 2019’ (COVID-19), are able to bind the ACE2 receptors [2]. Therefore, a hypothesis arises: could a chronic therapeutic assumption of ACE inhibitors or AII receptor antagonists have induced several elderly and middle-aged patients to be more vulnerable to the virus by upregulating ACE2 receptors? If we translate the murine model to the human cells, the expected result would be that shown in the figure (Fig. 1 ). In our opinion, during the COVID-19 pandemic, it would be more prudent to replace these drugs, when possible, with calcium channel blockers, adrenergic receptor blockers, diuretics or vasodilators.
Fig. 1.
After a chronic assumption of ACE inhibitors and AII receptor antagonists a normal cell (on the left) could be hypothetically rearranged into one with higher expression of ACE2 receptors (on the right), so turning particularly receptive and vulnerable to SARS-CoV-2.
Sources of support in the form of grants
None.
Conflict of interest statement
No conflict of interest.
References
- 1.Boehm M., Nabel E.G. Angiotensin-converting enzyme 2–a new cardiac regulator. N Engl J Med. 2002;347(22):1795–1797. doi: 10.1056/NEJMcibr022472. [DOI] [PubMed] [Google Scholar]
- 2.Zhang H., Penninger J.M., Li Y., Zhong N. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang M.L., Li X., Meng Y., Xiao B. Upregulation of angiotensin-converting enzyme (ACE) 2 in hepatic fibrosis by ACE inhibitors. Clin Exp Pharmacol Physiol. 2010;37(1):1–6. doi: 10.1111/j.1440-1681.2009.05302.x. [DOI] [PubMed] [Google Scholar]
- 4.Ferrario C.M., Jessup J., Chappell M.C., Averill D.B. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111(20):2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]