Highlights
-
•
Medical staff experience mental health disturb during the COVID-19 pandemic.
-
•
Direct and indirect exposure to COVID-19 affects the mental health profoundly.
-
•
Psychological materials and resources provide some protection.
-
•
Interventions with appropriate level are urgent.
Abbreviations: COVID-19, novel coronavirus disease; SARS, severe acute respiratory syndrome; MERS, Middle East respiratory syndrome; PHQ-9, 9-item Patient Health Questionnaire; GAD-7, 7-item Generalized Anxiety Disorder; ISI, Insomnia Severity Index; IES-R, Impact of Event Scale-Revised; SEM, structural equation model; RMSEA, root mean square error of approximation; CFI, comparative fit index; TLI, Tucker-Lewis index
Keywords: 2019 novel coronavirus disease, Medical and nursing staff, Mental healthcare, Mental health, Exposure
Abstract
The severe 2019 outbreak of novel coronavirus disease (COVID-19), which was first reported in Wuhan, would be expected to impact the mental health of local medical and nursing staff and thus lead them to seek help. However, those outcomes have yet to be established using epidemiological data. To explore the mental health status of medical and nursing staff and the efficacy, or lack thereof, of critically connecting psychological needs to receiving psychological care, we conducted a quantitative study. This is the first paper on the mental health of medical and nursing staff in Wuhan. Notably, among 994 medical and nursing staff working in Wuhan, 36.9% had subthreshold mental health disturbances (mean PHQ-9: 2.4), 34.4% had mild disturbances (mean PHQ-9: 5.4), 22.4% had moderate disturbances (mean PHQ-9: 9.0), and 6.2% had severe disturbance (mean PHQ-9: 15.1) in the immediate wake of the viral epidemic. The noted burden fell particularly heavily on young women. Of all participants, 36.3% had accessed psychological materials (such as books on mental health), 50.4% had accessed psychological resources available through media (such as online push messages on mental health self-help coping methods), and 17.5% had participated in counseling or psychotherapy. Trends in levels of psychological distress and factors such as exposure to infected people and psychological assistance were identified. Although staff accessed limited mental healthcare services, distressed staff nonetheless saw these services as important resources to alleviate acute mental health disturbances and improve their physical health perceptions. These findings emphasize the importance of being prepared to support frontline workers through mental health interventions at times of widespread crisis.
1. Introduction
In November 2019, a novel coronavirus disease (COVID-19) was first reported and then became widespread within Wuhan, the capital city of Hubei Province of China (Chan et al., 2020). The disease rapidly spread throughout China and elsewhere, becoming a global health emergency (WHO, 2020). The mental health of medical and nursing staff has been greatly challenged during the immediate wake of the viral epidemic (Chong et al., 2004, Wu et al., 2009). In battling the sudden emergence of severe acute respiratory syndrome (SARS), psychological distress among medical staff appeared gradually: fear and anxiety appeared immediately and decreased in the early stages of the epidemic, but depression, psychophysiological symptoms and posttraumatic stress symptoms appeared later and lasted for a long time, leading to profound impacts (Chong et al., 2004, Wu et al., 2009). Being isolated, working in high-risk positions, and having contact with infected people are common causes of trauma (Wu et al., 2009, Maunder et al., 2003). These factors may have impacted medical and nursing staff in Wuhan, leading to mental health problems.
The experience of medical staff responding to SARS shows that the effects on medical staff members’ mental health have not only short-term but also long-term impacts and that the value of effective support and training is meaningful (Maunder et al., 2006). Efficient and comprehensive actions should be taken in a timely fashion to protect the mental health of medical staff. The Chinese government has made various efforts to reduce the pressure on medical and nursing staff in China, such as sending more medical and nursing staff to reduce work intensity, adopting strict infection control, providing personal protective equipment and offering practical guidance. Based on previous responses to Middle East respiratory syndrome (MERS), medical staff tend to believe that such measures help protect their mental health (Khalid et al., 2016). In addition, to reduce the psychological damage of COVID-19 among medical and nursing staff, mental health workers in Wuhan are also taking action by establishing psychological intervention teams and providing a range of psychological services, including providing psychological brochures, counseling and psychotherapy (Kang et al., 2020). At the same time, television news and online media are also disseminating information about coping strategies for psychological self-help. However, evidence-based mental health services are preferable, and it is necessary to assess the quality of mental health services (Aarons et al., 2012). Therefore, we explore the mental health status of medical and nursing staff in Wuhan, the efficacy of the psychological care accessed, and their psychological care needs.
2. Methods
2.1. Participant
We recruited doctors or nurses working in Wuhan to participate in this survey from January 29, 2020, to February 4, 2020.
This study was approved by the Clinical Research Ethics Committee of Renmin Hospital of Wuhan University (WDRY2020-K004). Data were collected through Wenjuanxing (www.wjx.cn) with an anonymous, self-rated questionnaire that was distributed to all workstations over the internet. All subjects provided informed consent electronically prior to registration. The informed consent page presented two options (yes/no). Only subjects who chose yes were taken to the questionnaire page, and subjects could quit the process at any time.
2.2. Questionnaire
The questionnaire consists of six parts: basic demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental healthcare services accessed, psychological needs, and self-perceived health status compared to that before the COVID-19 outbreak.
2.2.1. Demographic data
Basic demographic data include occupation (doctor or nurse), gender (male or female), age (years), marital status (unmarried, married or divorced), educational level (undergraduate or lower, postgraduate or higher), technical title (primary, intermediate, or senior), and department (divided into high-exposure departments and non-high-exposure departments according to the possibility of exposure to confirmed patients; high-exposure departments included the fever clinic, emergency department, general isolation ward, and intensive care unit).
2.2.2. Mental health assessment
We used four scales to assess the mental health status of medical and nursing staff. The 9-item Patient Health Questionnaire (PHQ-9), the 7-item Generalized Anxiety Disorder (GAD-7), the 7-item Insomnia Severity Index (ISI) and the 22-item Impact of Event Scale-Revised (IES-R) were used to evaluate depression, anxiety, insomnia and distress, respectively. The PHQ-9 is a self-report measure used to assess the severity of depression, with the total scores categorized as follows: minimal/no depression (0–4), mild depression (5–9), moderate depression (10–14), or severe depression (15–21) (Kocalevent et al., 2013). The GAD-7 is a self-rated scale to evaluate the severity of anxiety and has good reliability and validity. The total scores are categorized as follows: minimal/no anxiety (0–4), mild anxiety (5–9), moderate anxiety (10–14), or severe anxiety (15–21) (Löwe et al., 2008). The ISI is a measure of insomnia severity that has been shown to be valid and reliable. The total scores are categorized as follows: normal (0–7), subthreshold (8–14), moderate insomnia (15–21), or severe insomnia (22–28) (Morin et al., 2011). The IES-R is a self-report measure used to assess the response to a specific stressful life event and has extensive reliability and validity. The event used for this questionnaire was the occurrence of COVID-19. The total scores are categorized as follows: subclinical (0–8), mild distress (9–25), moderate distress (26–43), and severe distress (44–88) (Daniel and Weiss, 2007).
2.2.3. Exposure to COVID-19
Exposure to COVID-19 was determined with the following questions asked to medical and nursing staff: Have you been diagnosed with COVID-19? Do you manage patients diagnosed with COVID-19? Has your family been diagnosed with COVID-19? Have your friends been diagnosed? Have your neighbors (people living in the same community who may or may not know each other) been diagnosed? Then, participants were asked whether there was anyone living with them with suspected symptoms. The answer to each question was yes or no.
2.2.4. Accessed mental healthcare services
The following question was used to determine which psychological services the subject had accessed. Have you ever received the following services: psychological materials (leaflets, brochures and books provided by mental health workers and distributed to staff in the hospital), psychological resources available through media (psychological assistance methods and techniques provided by psychologists through online media or TV news or various online platforms) (Supplementary material), and counseling or psychotherapy (including individual or group therapy)?
2.2.5. Meeting psychological care needs
Three areas were assessed regarding the psychological services that participants hoped to receive in the future: what kind of mental health service content were participants most interested in (including knowledge of psychology, ways to alleviate their own psychological reactions, ways to help others alleviate their psychological reactions, or ways to seek help from psychologists or psychiatrists); what kind of resources were most anticipated (including psychological materials, psychological resources available through media, group psychotherapy, individual counseling and psychotherapy, uninterested or other); and who participants would prefer to receive care from (including psychologists or psychiatrists, family or relatives, friends or colleagues, do not need help, or other).
2.2.6. Self-perceived health status
Health status was determined by asking participants to compare their current health status to their health status before the outbreak of COVID-19: How do you perceive your current health status compared to your health status before the outbreak? (answer options included getting better, almost unchanged, worse, or much worse).
2.3. Statistical analysis
Data analysis was performed using IBM SPSS Statistics for Windows (Version 23.0) and Mplus (version 7.4). Descriptive analysis was used to describe the general data and currently accessed psychological services. For count data, frequencies and percentages were used. The k-means clustering method was used to cluster the PHQ-9, GAD-7, ISI, and IES-R scores (Ball, 1967). With the Euclidean square root distance as the measurement index, the patients were divided into 4 groups by the Ward method. According to this grouping, exposure to COVID-19 and the current state of mental healthcare services were compared. The chi-square test was used to compare the data for different categorical variables. A structural equation model (SEM) was constructed via Mplus to explore the relationship among the four components, namely, exposure, accessed mental healthcare services, mental health status (PHQ-9, GAD-7, ISI, and IES-R scores) and self-perceived health status compared to that before the COVID-19 outbreak. The estimation method used weighted least squares with mean and variance adjustment test statistics (Distefano and Morgan, 2014). We used a Monte Carlo method with 1000 guided resamplings to construct a confidence interval for the estimation effect (Bauer et al., 2006). In SEM, several criteria, such as root mean square error of approximation (RMSEA) values < 0.08 and comparative fit index (CFI) and Tucker-Lewis index (TLI) values >0.90, indicate acceptable models (Hu and Bentler, 1998). P values < 0.05 indicated that a difference was statistically significant.
3. Results
3.1. Demographic characteristics
In total, 994 participants, including 183 (18.4%) doctors and 811 (81.6%) nurses, completed the survey. A total of 31.1% worked in high-risk departments. The participants tended to be female (85.5%), be aged 25 to 40 years (63.4%), be married (56.9%), have an educational level of undergraduate or less (85%), and have a junior technical title (66.3%), as shown in Table 1 .
Table 1.
Demographic characteristics.
| Variables | Number | Percentage (%) | |
|---|---|---|---|
| Total | 994 | 100 | |
| Gender | |||
| Male | 144 | 14.5 | |
| Female | 850 | 85.5 | |
| Age | |||
| 18–25 | 214 | 21.5 | |
| ~30 | 339 | 34.1 | |
| ~40 | 291 | 29.3 | |
| ~50 | 114 | 11.5 | |
| >50 | 36 | 3.6 | |
| Marriage | |||
| Unmarried or divorce | 428 | 43.1 | |
| Married | 566 | 56.9 | |
| Education level | |||
| Undergraduate or less | 845 | 85.0 | |
| Postgraduate or more | 149 | 15.0 | |
| Technical title | |||
| Junior | 659 | 66.3 | |
| Intermediate | 278 | 28.0 | |
| Senior | 57 | 5.7 | |
| Occupation | |||
| Doctor | 183 | 18.4 | |
| Nurse | 811 | 81.6 | |
| Department | |||
| High risk | 309 | 31.1 | |
| Ordinary | 685 | 68.9 | |
3.2. Accessed mental healthcare services
Of all participants, 36.3% had received psychological materials, 50.4% had obtained psychological resources available through media, and 17.5% had participated in group psychological counseling, as shown in Table 2 .
Table 2.
Resources of mental healthcare services.
| Variables | Number | Percentage (%) | |
|---|---|---|---|
| Psychological materials | No | 633 | 63.7 |
| Yes | 361 | 36.3 | |
| Psychological resources available through media | No | 493 | 49.6 |
| Yes | 501 | 50.4 | |
| Counseling or psychotherapy | No | 820 | 82.5 |
| Yes | 174 | 17.5 |
3.3. Cluster analysis of mental health states
According to the PHQ-9, GAD-7, ISI, and IES-R scores, the 994 participants were divided into 4 groups. Thirty-six percent of the medical staff had subthreshold mental health disturbances (mean PHQ-9: 2.4, GAD-7: 1.5, ISI: 2.8, IES-R: 6.1), 34.4% had mild disturbances (mean PHQ-9: 5.4, GAD-7: 4.6, ISI: 6.0, IES-R: 22.9), 22.4% had moderate disturbances (mean PHQ-9: 9.0, GAD-7: 8.2, ISI: 10.4, IES-R: 39.9), and 6.2% had severe disturbances (mean PHQ-9: 15.1, GAD-7: 15.1, ISI: 15.6, IES-R: 60.0). There were significant differences in the PHQ-9, GAD-7, ISI, and IES-R scores among the four groups, as shown in Table 3 .
Table 3.
Cluster analysis grouping.
| Variables | 1 | 2 | 3 | 4 | P-value |
|---|---|---|---|---|---|
| Number/percentage (%) | 367 (36.9) | 342 (34.4) | 223 (22.4) | 62 (6.2) | |
| PHQ-9 M (SD) | 2.4 (3.0) | 5.4 (3.4) | 9.0 (3.9) | 15.1 (5.2) | <0.001 |
| GAD-7 M (SD) | 1.5 (2.4) | 4.6 (2.9) | 8.2 (3.6) | 15.1 (4.3) | <0.001 |
| ISI M (SD) | 2.8 (3.0) | 6.0 (4.0) | 10.4 (4.8) | 15.6 (5.2) | <0.001 |
| IES-R M (SD) | 6.1 (4.4) | 22.9 (4.8) | 39.9 (5.4) | 60.0 (9.8) | <0.001 |
3.4. Differences among clusters
In contrast, there were no significant differences in demographic data among the four groups, as shown in Table 4 .
Table 4.
Comparison of demographic characteristics between different clusters.
| Cluster (n (Percentage (%))) | 1 | 2 | 3 | 4 | Total | P-value | |
|---|---|---|---|---|---|---|---|
| Age | 18–25 | 81 (22.1) | 74 (21.6) | 42 (18.8) | 17 (27.4) | 214 (21.5) | 0.101 |
| ~30 | 135 (36.8) | 123 (36.0) | 68 (30.5) | 13 (21.0) | 339 (34.1) | ||
| ~40 | 106 (28.9) | 96 (28.1) | 65 (29.1) | 24 (38.7) | 291 (29.3) | ||
| ~50 | 35 (9.5) | 35 (10.2) | 37 (16.6) | 7 (11.3) | 114 (11.5) | ||
| >50 | 10 (2.7) | 14 (4.1) | 11 (4.9) | 1 (1.6) | 36 (3.6) | ||
| Gender | Male | 62 (16.9) | 39 (11.4) | 31 (13.9) | 12 (19.4) | 144 (14.5) | 0.133 |
| Female | 305 (83.1) | 303 (88.6) | 192 (86.1) | 50 (80.6) | 850 (85.5) | ||
| Marriage | Unmarried and divorce | 161 (43.9) | 157 (45.9) | 81 (36.3) | 29 (46.8) | 428 (43.1) | 0.127 |
| Married | 206 (56.1) | 185 (54.1) | 142 (63.7) | 33 (53.2) | 566 (56.9) | ||
| Education level | Undergraduate or less | 306 (83.4) | 297 (86.8) | 186 (83.4) | 56 (90.3) | 845 (85.0) | 0.322 |
| Postgraduate or more | 61 (16.6) | 45 (13.2) | 37 (16.6) | 6 (9.7) | 149 (15.0) | ||
| Occupation | Doctor | 76 (20.7) | 56 (16.4) | 42 (18.8) | 9 (14.5) | 183 (18.4) | 0.409 |
| Nurse | 291 (79.3) | 286 (83.6) | 181 (81.2) | 53 (85.5) | 811 (81.6) | ||
| Department | High risk | 109 (29.7) | 98 (28.7) | 75 (33.6) | 27 (43.5) | 309 (31.1) | 0.092 |
| Ordinary | 258 (70.3) | 244 (71.3) | 148 (66.4) | 35 (56.5) | 685 (68.9) | ||
| Technical title | Junior | 252 (68.7) | 234 (68.4) | 137 (61.4) | 36 (58.1) | 659 (66.3) | 0.307 |
| Intermediate | 93 (25.3) | 89 (26.0) | 73 (32.7) | 23 (37.1) | 278 (28.0) | ||
| Senior | 22 (6.0) | 19 (5.6) | 13 (5.8) | 3 (4.8) | 57 (5.7) |
For medical and nursing staff, exposure to people around them who were infected varied among the different groups. The group with subthreshold mental health disturbances had contact with fewer people confirmed or suspected to be infected with the virus. Each group with a higher level of distress had a more extensive scope of exposure. There were also significant differences in mental healthcare services among the four groups; those with severe disturbances had accessed fewer psychological materials and psychological resources available through media. In addition, the perception of current health status compared to that before the outbreak of COVID-19 was also different among the groups, as shown in Table 5 .
Table 5.
Comparison of characteristics between different clusters.
| Cluster (n (Percentage (%))) | 1 | 2 | 3 | 4 | Total | P-value | |
|---|---|---|---|---|---|---|---|
| Risk factors for exposure | |||||||
| Patient infected | No | 210 (57.2) | 176 (51.5) | 92 (41.3) | 15 (24.2) | 493 (49.6) | <0.001 |
| Yes | 157 (42.8) | 166 (48.5) | 131 (58.7) | 47 (75.8) | 501 (50.4) | ||
| Own infection | No | 361 (98.4) | 340 (99.4) | 215 (96.4) | 59 (95.2) | 975 (98.1) | 0.023 |
| Yes | 6 (1.6) | 2 (0.6) | 8 (3.6) | 3 (4.8) | 19 (1.9) | ||
| Family infection | No | 359 (97.8) | 336 (98.2) | 208 (93.3) | 60 (96.8) | 963 (96.9) | 0.005 |
| Yes | 8 (2.2) | 6 (1.8) | 15 (6.7) | 2 (3.2) | 31 (3.1) | ||
| Colleague infection | No | 170 (46.3) | 149 (43.6) | 69 (30.9) | 18 (29.0) | 406 (40.8) | <0.001 |
| Yes | 197 (53.7) | 193 (56.4) | 154 (69.1) | 44 (71.0) | 588 (59.2) | ||
| Friend infection | No | 305 (83.1) | 280 (81.9) | 174 (78.0) | 32 (51.6) | 791 (79.6) | <0.001 |
| Yes | 62 (16.9) | 62 (18.1) | 49 (22.0) | 30 (48.4) | 203 (20.4) | ||
| Neighbor infection | No | 295 (80.4) | 273 (79.8) | 157 (70.4) | 36 (58.1) | 761 (76.6) | <0.001 |
| Yes | 72 (19.6) | 69 (20.2) | 66 (29.6) | 26 (41.9) | 233 (23.4) | ||
| Co-residents with suspected symptoms | Yes | 48 (13.1) | 69 (20.2) | 63 (28.3) | 19 (30.6) | 199 (20.0) | <0.001 |
| No | 319 (86.9) | 273 (79.8) | 160 (71.7) | 43 (69.4) | 795 (80.0) | ||
| Self-perceived health status compared to before COVID-19 outbreak | |||||||
| Self-perceived health status | Better | 32 (8.7) | 7 (2.0) | 5 (2.2) | 1 (1.6) | 45 (4.5) | <0.001 |
| Almost unchanged | 296 (80.7) | 240 (70.2) | 99 (44.4) | 16 (25.8) | 651 (65.5) | ||
| Worse | 38 (10.4) | 94 (27.5) | 99 (44.4) | 28 (45.2) | 259 (26.1) | ||
| Much worse | 1 (0.3) | 1 (0.3) | 20 (9.0) | 17 (27.4) | 39 (3.9) | ||
| Resources of mental healthcare services | |||||||
| Psychological materials | No | 215 (58.6) | 216 (63.2) | 151 (67.7) | 51 (82.3) | 633 (63.7) | 0.002 |
| Yes | 152 (41.4) | 126 (36.8) | 72 (32.3) | 11 (17.7) | 361 (36.3) | ||
| Psychological publicity of the media | No | 168 (45.8) | 161 (47.1) | 125 (56.1) | 39 (62.9) | 493 (49.6) | 0.011 |
| Yes | 199 (54.2) | 181 (52.9) | 98 (43.9) | 23 (37.1) | 501 (50.4) | ||
| Counseling or psychotherapy | No | 301 (82.0) | 276 (80.7) | 194 (87.0) | 49 (79.0) | 820 (82.5) | 0.216 |
| Yes | 66 (18.0) | 66 (19.3) | 29 (13.0) | 13 (21.0) | 174 (17.5) | ||
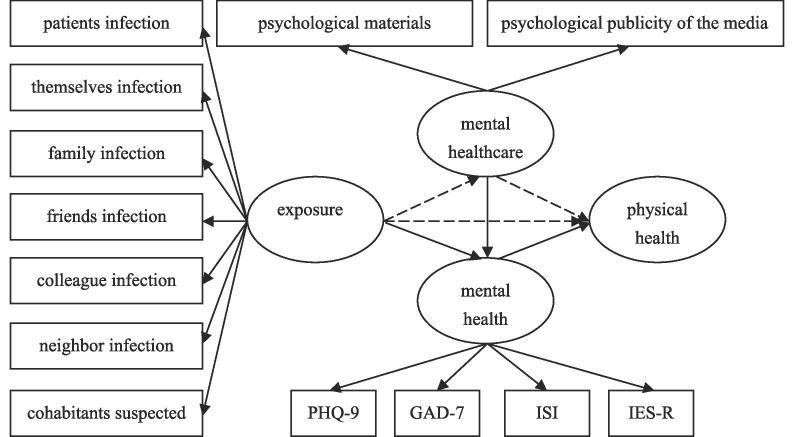
3.5. Role of mental healthcare services accessed
We established an SEM of the associations between the four areas. First, exposure as a risk factor for mental health, including the confirmed diagnosis of patients, the participants’ themselves, family, friends, colleagues, neighbors, and coresidents with suspected symptoms, was analyzed in the previous step. Second, the mental healthcare services accessed consisted of psychological materials and psychological resources available through media. Third, mental health consisted of the PHQ-9, GAD-7, ISI, and IES-R scores. The fourth area was the subjective feelings of the staff regarding whether their physical conditions were worse than before the epidemic. The chi-square test of model fit yielded a value of 129.1, with degrees of freedom = 72, P-value = 0.000, RMSEA = 0.028, CFI = 0.978, and TLI = 0.973, indicating a good fit. The results showed that the risk factors of exposure affected mental health and that mental health affected subjective physical health perceptions. Mental healthcare services only partially mediated the relationship between exposure risks and mental health. Mental healthcare services regulated the relationship between the risk of exposure and subjective physical health perceptions by affecting mental health. The results are shown in Fig. 1 and Table 6 .
Fig. 1.
In this model, the solid line represents a significant relationship between the two, while the dotted line represents the relationship is not significant.
Table 6.
Direct and indirect effects in SEM.
| Direct or indirect effects pathway | Estimate | standard error | P-value | 95% confidence interval |
|---|---|---|---|---|
| Exposure → mental health | 5.347 | 1.130 | <0.001 | 3.831, 8.184 |
| Mental healthcare → mental health | −0.868 | 0.272 | 0.001 | −1.385, −0.289 |
| Exposure → mental healthcare | −0.320 | 0.170 | 0.059 | −0.734, −0.040 |
| Mental health → physical health | 0.131 | 0.016 | <0.001 | 0.098, 0.159 |
| Exposure → physical health | 0.120 | 0.248 | 0.628 | −0.340, 0.675 |
| Mental healthcare → physical health | −0.008 | 0.059 | 0.887 | −0.115, 0.105 |
| Exposure → mental healthcare → mental health | 0.278 | 0.133 | 0.036 | 0.016, 0.565 |
| Exposure → mental healthcare → physical health | 0.003 | 0.022 | 0.903 | −0.043, 0.047 |
| Exposure → mental health → physical health | 0.698 | 0.167 | <0.001 | 0.475, 1.103 |
| Exposure → mental healthcare → mental health → physical health | 0.036 | 0.018 | 0.040 | 0.002, 0.072 |
| Mental healthcare → mental health → physical health | −0.113 | 0.037 | 0.002 | −0.184, −0.038 |
3.6. Psychological care needs of medical and nursing staff
In terms of the content of interest, namely, psychological care, medical and nursing staff with subthreshold disturbances most wanted to obtain skills to help alleviate others’ psychological distress, whereas other medical and nursing staff most wanted to obtain self-help skills. Medical and nursing staff with higher levels of mental health problems were more interested in skills for self-rescue and showed more urgent desires to seek help from psychotherapists and psychiatrists. Medical and nursing staff differed in terms of how they wanted to obtain services based on their levels of mental health problems. Medical and nursing staff with subthreshold and mild disturbances preferred to obtain such services from media sources, while staff with heavier burdens wanted to seek services directly from professionals. Apart from medical and nursing staff with subthreshold disturbances who did not think they needed help from others, the other workers saw a greater need to obtain help from professionals than from close family and friends. The results are shown in Table 7 .
Table 7.
Mental Healthcare Services among Medical Staff.
| Cluster (n (Percentage (%))) | 1 | 2 | 3 | 4 | Total | P-value | |
|---|---|---|---|---|---|---|---|
| Content of interest | |||||||
| Knowledge of psychology | No | 181 (49.3) | 169 (49.4) | 133 (59.6) | 42 (67.7) | 525 (52.8) | 0.004 |
| Yes | 186 (50.7) | 173 (50.6) | 90 (40.4) | 20 (32.3) | 469 (47.2) | ||
| Skills for self-rescue | No | 149 (40.6) | 91 (26.6) | 38 (17.0) | 10 (16.1) | 288 (29.0) | <0.001 |
| Yes | 218 (59.4) | 251 (73.4) | 185 (83.0) | 52 (83.9) | 706 (71.0) | ||
| Skills for help others alleviate psychological distress | No | 131 (35.7) | 117 (34.2) | 100 (44.8) | 33 (53.2) | 381 (38.3) | 0.004 |
| Yes | 236 (64.3) | 225 (65.8) | 123 (55.2) | 29 (46.8) | 613 (61.7) | ||
| Seek help from psychologists or psychiatrists | No | 272 (74.1) | 227 (66.4) | 133 (59.6) | 31 (50.0) | 663 (66.7) | <0.001 |
| Yes | 95 (25.9) | 115 (33.6) | 90 (40.4) | 31 (50.0) | 331 (33.3) | ||
| Resources | |||||||
| Psychological materials | 88 (24.0) | 63 (18.4) | 28 (12.6) | 6 (9.7) | 185 (18.6) | <0.001 | |
| Psychological resources available through media | 96 (26.2) | 86 (25.1) | 53 (23.8) | 7 (11.3) | 242 (24.3) | ||
| Group psychotherapy | 52 (14.2) | 56 (16.4) | 47 (21.1) | 15 (24.2) | 170 (17.1) | ||
| Individual counseling and psychotherapy | 39 (10.6) | 67 (19.6) | 57 (25.6) | 27 (43.5) | 190 (19.1) | ||
| Uninterested | 79 (21.5) | 64 (18.7) | 34 (15.2) | 6 (9.7) | 183 (18.4) | ||
| Others | 13 (3.5) | 6 (1.8) | 4 (1.8) | 1 (1.6) | 24 (2.4) | ||
| Prefer to receive care from | |||||||
| Psychologists or psychiatrists | 117 (31.9) | 139 (40.6) | 103 (46.2) | 41 (66.1) | 400 (40.2) | <0.001 | |
| Family or relatives | 52 (14.2) | 53 (15.5) | 28 (12.6) | 6 (9.7) | 139 (14.0) | ||
| Friends or colleagues | 37 (10.1) | 57 (16.7) | 40 (17.9) | 12 (19.4) | 146 (14.7) | ||
| Do not need help | 154 (42.0) | 89 (26.0) | 49 (22.0) | 2 (3.2) | 294 (29.6) | ||
| Others | 7 (1.9) | 4 (1.2) | 3 (1.3) | 1 (1.6) | 15 (1.5) | ||
4. Discussion
This is the first mental health investigation in the wake of the coronavirus epidemic in Wuhan, China that aims, in part, to explore the demand for mental healthcare services in this context. When cities are struck by deadly, large-scale disasters of various types, the characteristics of mental health problems that arise can differ across different periods (Shioyama et al., 2000). We therefore chose to survey a set of people (health care providers) in the discrete window of time soon after the initiation of a chaotic event (the outbreak of coronavirus infections). To conduct a comprehensive analysis, we used multiple different scales to evaluate the mental health of medical staff.
Our study has revealed the limits in the availability of mental healthcare services provided by psychologists and psychiatrists and thus the limits in access points for psychological care for distressed individuals, including less personalized sources of support such as publication-style psychological materials and psychological resources available from media. These latter methods can nonetheless contribute positively to alleviating mental health problems and physical discomfort caused by risk factors such as the exposure of close contacts to COVID-19. Such exposure is known to be mentally injurious in epidemic settings: when the SARS epidemic hit, not only did the direct exposure of the work environment affect the mental health of medical staff, but the infection of friends or close relatives generated psychological trauma (Wu et al., 2009).
We found that subthreshold and mild mental health disturbances accounted for a large proportion of disturbances. People with such levels of disturbances may be more likely than those with more severe disturbances to take action and be motivated to learn the necessary skills and to adapt in productive ways to respond to diverse challenges. These skills have been shown in previous retrospective studies to be protective for later mental health (Maunder et al., 2006). In addition, we note that people with subthreshold and mild mental health disturbances want to find ways to better help others, which is beneficial for health care teams. In terms of physiology, positive coping has been seen to increase immune function when victimized subjects report high mental demands, leading to a better state of response (Sakami et al., 2004). However, there are negative consequences of stimulation caused by pressure, as acute psychological stress is known to activate the sympathetic adrenal medulla system and hypothalamus-pituitary adrenal axis, and this two-component stress response impacts physical and mental health and has disease consequences (Turner et al., 2020). In summary, continuous mental healthcare services are necessary even for subthreshold and mild psychological reactions during this epidemic to attenuate the possibility of escalating complications.
Multiple features were found for the group of untreated clinical personnel who had serious psychological problems. First, compared to less severely affected groups, they had accessed fewer printed psychological advice materials (e.g., office brochures) and had accessed less psychological guidance publicized through digital media. Second, they were more likely to desire personalized, one-on-one counseling as a therapy option. One might speculate a cause-and-effect relationship wherein more frequent exposure of the other groups to the noted materials in some way protected them from reaching the most severely impacted category, but our cross-sectional results are, by nature, correlational. This study limitation does not detract, however, from the importance of widely implementing prevention and monitoring strategies; mildly to moderately impacted personnel expressed interest in having access to psychological guidance materials, which provides evidence of the importance of prevention strategies.
The number of people suffering from mental health impacts after a major event is often greater than the number of people who are physically injured, and mental health effects may last longer. Nonetheless, mental health attracts far fewer personnel for planning and resources (Allsopp et al., 2019). Thus, the Lancet Global Mental Health Commission’s observation that the use of nonprofessionals and digital technologies can provide a range of mental health interventions may indicate an opportunity (Patel et al., 2018). Our data are consistent with a model in which psychological advice and guidance in print resources and disseminated in the media can provide a level of protection for medical and nursing staff, improving mental health by reducing the stress impacts caused by high risk of infection. Clearly, there is a role, nonetheless, for therapist-driven sessions, as previous research showed that a convenient group course intervention for doctors reduced depersonalization, improved views on the meaning of work, and achieved sustained results (West et al., 2014). We anticipate similar benefit for COVID-19 staff in Wuhan based on our findings contained herein.
Interestingly, previous studies on medical staff and other infectious agents have repeatedly emphasized that mental health impacts are related to department and occupation (Hawryluck et al., 2004, Wu et al., 2009). Health care workers with professional knowledge about differences in the relative exposure patterns and transmission of different infectious diseases could gain some degree of comfort and control over their situations (Chowell et al., 2015). For example, over the decades, although hepatitis viruses and HIV have often caused lethal infections, radiologists, pathologists and nurses knew that their risk of exposure was low as long as they exercised caution in their contact with bodily fluids. The situation has been different in Wuhan due to the pernicious characteristics of COVID-19. Many infected individuals exhibit minimal or no symptoms while contagious, for example, early in the course of infection (Bai et al., 2020). These individuals may thus visit a variety of different hospital departments in an infectious but asymptomatic state, unknowingly spreading the disease directly through aerosolized droplets or indirectly through skin contact with handled surfaces. These features of the infectivity of coronavirus involve a substantial risk of exposure for medical workers, regardless of their hospital department, job title or building location; thus, any worker – whether doctor or nurse, specialist or generalist – is at substantial risk. The resultant stress due to concerns about infection risk thus indiscriminately affects large numbers of personnel.
There is a need to better recognize mental health needs as an important component of mobilizing a large-scale therapeutic response to sudden city-scale crisis scenarios. A large rapid response team in crisis situations should include mental healthcare workers. Local medical and nursing staff at the epicenter of a crisis are pivotal to the overall response, and care for these caregivers – whether through face-to-face counseling or comparable support through digital platforms such as cell phone interfaces – is essential in efforts to extend their immediate efficiency and to better protect their mental health in the long term.
Our research also has some limitations. First, compared with face-to-face interviews, self-reporting has certain limitations. Second, the study is cross-sectional and does not track the efficacy of psychological services. Due to changes in posttraumatic mental health, dynamic observation is necessary. A randomized prospective study could better determine correlation and causation. Third, a larger sample size is needed to verify the results.
In summary, the results demonstrate that a strikingly large portion of health care providers in virus-plagued Wuhan are suffering from mental health disturbances. They would benefit from greater availability of personalized mental health care from psychotherapists and psychiatrists, wherein different mental health groups could focus on providing specialized mental healthcare services. Among the steps needed to better prepare for future infectious disease outbreaks would be a greater investment in the mental health tools in society’s medical arsenal to protect and care for future medical and nursing staff who find themselves unexpectedly on the dangerous front lines of disease response.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
This work was supported by grants from the National Key R&D Program of China (grant numbers: 2018YFC1314600) and the National Natural Science Foundation of China (grant numbers: 81771472).
Author contribution
Participated in research design: ZL, CM, GW, KZ, SH, BXY, ZC, HB, MC.
Performed acquisition, analysis, and interpretation of data: ZL, CM, LK, SM, BXY, ZC, HB, MC, JY, YW, RL, LY.
Wrote and contributed to the writing of the manuscript: ZL, CM, LK and SM.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbi.2020.03.028.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Aarons G.A. The organizational social context of mental health services and clinician attitudes toward evidence-based practice: a United States national study. Implement. Sci. IS. 2012;7:56. doi: 10.1186/1748-5908-7-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allsopp K. Responding to mental health needs after terror attacks. BMJ. 2019;366 doi: 10.1136/bmj.l4828. [DOI] [PubMed] [Google Scholar]
- Bai Y. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball G.H. A clustering technique for summarizing multivariate data. Behav. Sci. 1967 doi: 10.1002/bs.3830120210. [DOI] [PubMed] [Google Scholar]
- Bauer D.J., Preacher K.J., Gil K.M. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychol. Methods. 2006;11:142–163. doi: 10.1037/1082-989X.11.2.142. [DOI] [PubMed] [Google Scholar]
- Chan J.F.-W. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong M.Y. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiat. J. Mental Sci. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- Chowell G. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210. doi: 10.1186/s12916-015-0450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel S., Weiss, Ph.D., 2007. The Impact of Event Scale: Revised. Guilford Press, New York, pp. 399–411.
- Distefano C., Morgan G.B. A comparison of diagonal weighted least squares robust estimation techniques for ordinal data. Struct. Equ. Model. A Multidisc. J. 2014;21:425–438. doi: 10.1080/10705511.2014.915373. [DOI] [Google Scholar]
- Hawryluck L. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Diseas. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L.T., Bentler P.M. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol. Methods. 1998;3:424–453. doi: 10.1037//1082-989X.3.4.424. [DOI] [Google Scholar]
- Kang L. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiat. 2020;7 doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalid I. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin. Med. Res. 2016;14:7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocalevent R.D. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen. Hospital Psychiat. 2013;35:551–555. doi: 10.1016/j.genhosppsych.2013.04.006. [DOI] [PubMed] [Google Scholar]
- Löwe B. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med. Care. 2008;46:266–274. doi: 10.1097/mlr.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Maunder R. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Can. Med. Assoc. J. 2003;168:1245–1251. doi: 10.1001/jama.289.18.2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Diseas. 2006;12:1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin C.M. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392:1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- Sakami S. Positive coping up- and down-regulates in vitro cytokine productions from T cells dependent on stress levels. Psychother. Psychosom. 2004;73:243–251. doi: 10.1159/000077743. [DOI] [PubMed] [Google Scholar]
- Shioyama A. The mental health of school children after the Great Hanshin-Awaji Earthquake: II. Longitudinal analysis. Seishin Shinkeigaku Zasshi. 2000;102(5):481–497. [PubMed] [Google Scholar]
- Turner A.I. Psychological stress reactivity and future health and disease outcomes: a systematic review of prospective evidence. Psychoneuroendocrinology. 2020;114 doi: 10.1016/j.psyneuen.2020.104599. [DOI] [PubMed] [Google Scholar]
- West C.P. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Inter. Med. 2014;174:527–533. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]
- WHO, 2020. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (assessed Feb 15, 2020).
- Wu P. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Canadian journal of psychiatry. Revue canadienne de psychiatrie. 2009;54:302–311. doi: 10.1192/bjp.194.5.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.