Abstract
Background
Having a reliable source for health information is vital to build a strong foundation of knowledge, especially with the current revolution of the internet and social media, which raises many concerns regarding harmful effects on the health of the public. However, there are no studies on how the Saudi Arabian population seeks health information. Details about the most used and trusted sources of health information among the public will help health authorities and public awareness accounts on social media to effectively disseminate health information.
Objective
To investigate the types of sources accessed by the Saudi Arabian population while seeking health information, as well as their level of trust in the sources and to assess the impact of these sources on their perception of medical knowledge and health decision-making.
Methods
A cross-sectional study was conducted to meet the objectives. The study population included both men and women who were aged 16 years or more and visited primary care clinics at King Khalid University Hospital. Four hundred and thirteen participants were sampled using the simple random method, and a self-administered questionnaire was used to collect data. The data were analyzed using SPSS software (IBM Corp, Armonk, New York, USA).
Results
A total of 413 participants were included in this study, and of these, 99 (24.0%) were males and 206 (49.9%) had a bachelor’s degree. Doctors were chosen as the first source of information by 87.6% (283/323) of the participants, and they were completely trusted by most of the population (326/411, 79.3%). The second most commonly used source was pharmacists (112/194, 57.7%), and they were partially trusted by 41.4% (159/384) of the participants. Internet searches, social media, and traditional medicine were not prioritized by most of the participants as the first or second source of health information. The majority of the participants did not trust information obtained from social media, and WhatsApp was the most untrusted source. Almost half of the respondents (197/413, 47.7%) acknowledged that various sources of information can often help them understand their health problems. However, the majority disagreed on substituting a doctor’s prescription with information obtained from the internet or a friend or relative.
Conclusions
Although physicians were preferred and highly trusted, internet sources appeared to impact the medical knowledge of the population. The population still preferred to use internet search to obtain health information prior to a doctor’s visit.
Keywords: health information sources, health perception, medical information sources, satisfaction, social media, trust
Introduction
The current sources of health information are diverse, and they influence the perception of medical knowledge among the Saudi Arabian population. Having a reliable source of health information is critical for building a strong foundation of knowledge about health among the public, especially with the current revolution of the internet and social media. According to the latest statistics, more than 50% of the global population uses the internet. Moreover, more than 64% of the Saudi Arabian population uses the internet, and this number has been increasing every year [1]. Although social media, websites, and internet search engines are considered as easily accessible sources of medical information, these sources still contain ambiguities. There is increasing evidence that the instant exchange of news from random resources and the lack of verification and determination of the accuracy and credibility of the information being shared by nonprofessionals raise many concerns about the harmful effects on a person’s health [2].
Determining the frequency and characteristics of people who are likely to use the internet and social media to obtain their medical knowledge may guide both clinicians and the public. In addition, it is important from a public health perspective to appreciate the probable subsequent health outcomes. Moreover, the health information sought from different sources and trusted by the public could tremendously influence the quality of health care rendered, as it could affect their judgment of a physician’s medical opinion and, in turn, affect their health decision-making. Previous studies have found that the commonly used sources of health information are the internet [1,3,4], physicians [5], social media [6], radio and television [7], pharmacists [8], and parents [9]. It has been reported that more than half of the public widely use the internet to seek health information [1,10,11], and the majority are young adults [1]. In a study conducted in Qatar, it was found that about 37.8% of Qataris seek health information from family and friends and 31.2% rely on primary health care centers as a source of health information [1].
In Australia, the use of the internet as a source of health information by the university population (students and staff) is greater than the use by the low or middle socioeconomic population [12]. It has been reported that gender, age, and educational level play significant roles in predicting the source of medical information. However, irrespective of the source of consultation, women are generally more interested in seeking health information than men, and the majority of those who seek medical information from the internet are women [1]. In comparison with the different available sources of health information, health care providers have been reported to be the most trusted source among different adult populations in the United States [11]. The majority of those who trust health care providers as the source of their health information are female, young, and educated [11], and this is irrespective of their socioeconomic status [12].
The roles of family and friends, pharmacists, and local alternative medicine practitioners are rarely discussed. As such, additional research is needed to evaluate the use of the internet and social media as tools for medical decision-making. Familiarity with the most used and trusted sources of health information among the public will assist health authorities and public awareness accounts on the internet and social media in accurately and carefully disseminating health information among the public, who should be educated and advised about the most credible sources of health information.
It is important to mention that social media platforms in Saudi Arabia, specifically WhatsApp, are not only used as communication tools among family and friends. The easy broadcasting characteristics of WhatsApp allow the population to exchange numerous videos, news, and messages. As these broadcasts continue to circulate among the public, the source of the information can no longer be tracked and verified. Health information is one of the most commonly exchanged messages and are most frequently completely false. This is why we express our concerns in this paper, and we investigated the level of trust of information broadcasted through WhatsApp and assessed whether it affects a patient’s health-seeking behavior and medical decisions.
To our knowledge, there have been no studies on how the Saudi Arabian population seeks information regarding their health. Therefore, the purposes of this study were to (1) investigate the different sources that the Saudi Arabian population uses and trusts for medical information and (2) assess the impact of these sources on medical knowledge and the patient’s health decision-making. We hypothesized that more than half of the Saudi Arabian population uses the internet and social media to obtain medical information.
Methods
Study Setting and Population
We conducted an observational cross-sectional study to address our research objectives. The study was conducted in primary care clinics at King Khalid University Hospital (KKUH), which is a large 1000-bed tertiary-care hospital in the northern part of Riyadh, Saudi Arabia. KKUH provides primary, secondary, and tertiary care services to a large patient-catchment area and government-funded free preventive and curative services. A random selection was performed of all attending Saudi male and female patients aged 16 years or more, which is the cutoff age for patients attending the adult primary care clinics. There were no exclusion criteria other than age and nationality.
The required ethical approval was obtained from the institutional review board of King Saud University. Informed consent was obtained from the participants, and the confidentiality of the information and privacy of the participants were protected throughout the study.
Sample Size Estimation
According to a recent study from the neighboring gulf region, 71% of the Qatari population uses the internet to seek health-related information. With a 95% CI and precision of 5, the sample size in this study was estimated at 386, which was further increased to 425 considering a nonresponse rate of 10%.
Recruitment of Participants
Four hundred and thirteen participants were recruited using simple random sampling, which was conducted through a random number generator software.
Data Collection Tools
The data were collected using a self-administered questionnaire or an interview (in the case of illiterate participants). The questionnaire had three main parts. The first part assessed the demographic data of the participants, such as age, gender, area of residence, educational level, and current occupation. The second part assessed the different used and trusted sources of medical information. It contained two questions. The first question concerned the ranking of the most used source, and the second question concerned the extent of trust in the sources chosen in the first question. The third part of the questionnaire was designed to explore the impacts of those sources on the participant’s medical knowledge and their effects on health decision-making.
Tool Validation
The development of the questionnaire survey was based on a literature review, and some of the questions in the second part of the questionnaire were adapted from the Health Information National Trends Survey (HINTS). We used the information sources mentioned in the HINTS [13]. For the third part, we adopted most of the questions from the behavioral involvement subscale of the Assessment of Preferences for Self-Treatment and Information in Health Care survey [14]. A pilot study was conducted to assess the time needed to complete the questionnaire and the understandability of the included questions.
Statistical Analysis
The data were analyzed using IBM SPSS Statistics for Windows version 23.0 (IBM Corp, Armonk, New York, USA). The data are expressed using frequencies and percentages for categorical variables and means and SDs for continuous variables. The chi-square test was used for categorical variables. The association between the sociodemographic characteristics and the sources of health information was examined using logistic regression, and the results are expressed with ORs and 95% CIs. A two-sided P value of <0.05 was considered statistically significant.
Results
Characteristics of the Study Participants
Of 425 distributed questionnaires, 413 completed questionnaires were obtained (response rate of 88%). Twenty participants were illiterate and thus were interviewed. The majority of the respondents were female (314/413, 76.0%). The study sample was well distributed across all age groups, and most of the population was literate. The overall health status of the participants was good. However, 130 (31.6%) had chronic diseases, and 52 (40.0%) had diabetes, 44 (33.8%) had hypertension, and 34 (26.2%) had asthma. The demographic data are summarized in Table 1.
Table 1.
Characteristics of the study participants.
| Characteristic | Value, n (%) | |
| Gender |
|
|
|
|
Male | 99 (24.0) |
| Age (years) |
|
|
|
|
16-25 | 98 (24.0) |
|
|
26-35 | 138 (33.7) |
|
|
36-45 | 91 (22.2) |
|
|
46-55 | 64 (15.6) |
|
|
≥56 | 18 (4.4) |
| Residency (province) |
|
|
|
|
Central | 362 (87.7) |
|
|
Northern | 27 (6.5) |
|
|
Southern | 9 (2.2) |
|
|
Eastern | 6 (1.5) |
|
|
Western | 9 (2.2) |
| Educational level |
|
|
|
|
Elementary school | 16 (3.9) |
|
|
Intermediate school | 22 (5.3) |
|
|
High school | 86 (20.8) |
|
|
Diploma | 32 (7.7) |
|
|
Bachelor studies | 206 (49.9) |
|
|
Postgraduate studies | 31 (7.5) |
|
|
Illiterate | 20 (4.8) |
| Occupation |
|
|
|
|
Student | 64 (5.6) |
|
|
Government employee | 115 (28.0) |
|
|
Private sector employee | 55 (13.4) |
|
|
Retired | 21 (5.1) |
|
|
No occupation | 155 (37.8) |
| Field of occupation |
|
|
|
|
Education | 125 (45.6) |
|
|
Medical | 29 (10.6) |
|
|
Military | 9 (3.3) |
|
|
Business | 20 (3.7) |
|
|
Others | 91 (33.2) |
| Self-assessment of health status |
|
|
|
|
Very weak | 2 (0.5) |
|
|
Weak | 18 (4.4) |
|
|
Good | 253 (61.3) |
|
|
Excellent | 140 (33.9) |
| Reported history of chronic disease | 130 (31.6) | |
Different Sources and Choice of Preference for Health Information
Doctors were the most favored choice for the majority of the study population (283/323, 87.6%); however, a smaller fraction rated them as second (18/323, 5.6%), third (12/323, 3.7%), and fourth preferences (10/323, 3.1%). Pharmacists were rated as the second most favored choice after doctors by a little more than half of the population (112/194, 57.7%). Social media was least preferred as the first choice (2/105, 1.9%). Even doctors who are on social media were less preferred as the first choice (19/157, 12.1%) (Table 2).
Table 2.
Different sources used for health information.
| Source of information | Respondents, n or n (%) | Ranking, n (%) | ||||||||||
| First | Second | Third | Fourth or more | |||||||||
| Total | Female | Total | Female | Total | Female | Total | Female | Total | Female | |||
| Doctor | 323 | 240 (74.3) | 283 (87.6) | 211 (87.9) | 18 (5.6) | 14 (5.8) | 12 (3.7) | 9 (3.8) | 10 (3.1) | 6 (2.5) | ||
| Pharmacist | 194 | 137 (70.6) | 13 (6.7) | 12 (8.8) | 112 (57.7) | 74 (54.0) | 31 (16.0) | 24 (17.5) | 38 (19.6) | 27 (19.7) | ||
| Traditional medicine practitioner | 78 | 50 (64.1) | 5 (6.4) | 2 (4.0) | 6 (7.7) | 5 (10.0) | 15 (19.2) | 9 (18.0) | 52 (66.7) | 34 (68.0) | ||
| Social media | 105 | 69 (65.7) | 2 (1.9) | 2 (2.9) | 11 (10.5) | 7 (10.1) | 17 (16.2) | 10 (14.5) | 75 (71.4) | 50 (72.5) | ||
| Doctors who are on social media | 157 | 122 (77.7) | 19 (12.1) | 16 (13.1) | 48 (30.6) | 38 (31.1) | 36 (22.9) | 29 (23.8) | 54 (34.3) | 39 (32.0) | ||
| Family and friends | 187 | 133 (71.1) | 14 (7.5) | 9 (6.8) | 26 (13.9) | 21 (15.8) | 46 (24.6) | 34 (25.6) | 101 (54.0) | 69 (51.9) | ||
| Internet search | 184 | 132 (71.7) | 28 (15.2) | 20 (15.2) | 41 (22.3) | 31 (23.5) | 45 (24.5) | 31 (23.5) | 70 (38.0) | 50 (37.9) | ||
| Articles | 95 | 64 (67.3) | 2 (2.1) | 1 (1.6) | 7 (7.4) | 4 (6.3) | 15 (15.8) | 11 (17.2) | 71 (74.7) | 48 (75.0) | ||
| Television and radio | 122 | 81 (66.3) | 5 (4.1) | 2 (2.5) | 14 (11.5) | 9 (11.1) | 19 (15.6) | 12 (14.8) | 84 (68.9) | 58 (71.6) | ||
| Courses and campaigns | 93 | 66 (70.9) | 13 (14.0) | 11 (16.7) | 19 (20.4) | 15 (22.7) | 61 (65.6) | 40 (60.6) | —a | —a | ||
aNone of the participants selected this source.
Level of Trust in Each Source of Health Information
The levels of trust in the sources of information are presented in Table 3. Doctors were the most trusted, and there was either complete trust (326/411, 79.3%) or partial trust (85/411, 20.6%), and no participant reported distrusting them. Pharmacists and traditional practitioners were partially trusted, with similar ratings; however, they were also distrusted by some participants. The majority of the participants did not trust the information obtained from social media. Gender differences were observed in the level of trust in social media, wherein more women showed distrust in social media than did men (P=.01) (Table 3).
Table 3.
The level of trust in each source of health information.
| Source of information | Number of respondents, n or n (%) | Level of trust, n (%) | ||||||||
| Completely trusted | Partially trusted | Not trusted | ||||||||
| Total | Female | Total | Female | Total | Female | Total | Female | |||
| Doctor | 411 | 312 (75.9) | 326 (79.3) | 244 (74.8) | 85 (20.6) | 68 (80.0) | —a | —a | ||
| Pharmacist | 384 | 287 (74.7) | 23 (6.0) | 1 (4.3) | 159 (41.4) | 89 (56.0) | 202 (52.6) | 197 (97.5) | ||
| Traditional medicine | 271 | 209 (66.6) | 9 (3.3) | 5 (55.6) | 115 (42.4) | 85 (74.0) | 147 (54.2) | 119 (81.0) | ||
| 331 | 233 (70.4) | 22 (6.6) | 3 (13.6) | 123 (37.1) | 69 (56.1) | 186 (56.1) | 161 (86.6) | |||
| Snapchat | 318 | 219 (68.9) | 22 (6.9) | 6 (27.3) | 127 (39.9) | 83 (65.4) | 169 (53.1) | 130 (77.0) | ||
| 273 | 205 (74.8) | 5 (1.8) | 3 (60.0) | 139 (50.9) | 104 (74.8) | 130 (47.6) | 98 (75.4) | |||
| Family and friends | 360 | 271 (75.3) | 27 (7.5) | 23 (85.2) | 265 (73.6) | 199 (75.1) | 68 (18.9) | 49 (72.1) | ||
| Internet search |
353 | 266 (75.4) | 28 (7.9) | 20 (71.4) | 249 (70.5) | 187 (75.1) | 76 (21.5) | 59 (77.6) | ||
| Television and radio | 314 | 234 (74.5) | 33 (10.5) | 22 (66.6) | 197 (62.7) | 147 (74.6) | 84 (26.8) | 65 (77.4) | ||
aNone of the participants selected this option.
In addition, the population distributions for the first choice of the source of health information and complete trust in the first choice are presented in Table 4.
Table 4.
Distributions of the population for the first choice and complete trust in the information.
|
|
First choice, n (%) | Complete trust, n (%) | ||||||
| Medicala | Mediab | Othersc | Medical | Media | Others | |||
| Age (years) |
|
|
|
|
|
|
||
|
|
16-25 | 73 (83.0) | 6 (7.0) | 8 (9.0) | 77 (93.0) | 0 (0.0) | 5 (6.0) | |
|
|
26-45 | 151 (75.0) | 38 (19.0) | 12 (6.0) | 179 (97.0) | 3 (2.0) | 3 (2.0) | |
|
|
≥46 | 67 (92.0) | 3 (4.0) | 3 (4.0) | 73 (95.0) | 1 (1.0) | 3 (4.0) | |
| Gender |
|
|
|
|
|
|
||
|
|
Male | 72 (78.0) | 10 (11.0) | 10 (11.0) | 82 (99.0) | 0 (0.0) | 1 (1.0) | |
|
|
Female | 221 (82.0) | 37 (14.0) | 13 (5.0) | 250 (95.0) | 4 (2.0) | 10 (4.0) | |
| Chronic diseases |
|
|
|
|
|
|
||
|
|
Present | 96 (83.0) | 18 (16.0) | 1 (1.0) | 110 (94.0) | 0 (0.0) | 7 (6.0) | |
|
|
Absent | 196 (79.0) | 29 (12.0) | 22 (9.0) | 222 (97.0) | 4 (2.0) | 4 (2.0) | |
| Occupation |
|
|
|
|
|
|
||
|
|
Employed | 49 (86.0) | 3 (5.0) | 5 (9.0) | 47 (96.0) | 0 (0.0) | 2 (4.0) | |
|
|
Retired | 115 (77.0) | 23 (15.0) | 12 (8.0) | 136 (96.0) | 3 (2.0) | 3 (2.0) | |
|
|
Unemployed | 17 (89.0) | 1 (5.0) | 1 (5.0) | 19 (96.0) | 0 (0.0) | 1 (5.0) | |
|
|
Student | 111 (82.0) | 20 (15.0) | 5 (4.0) | 128 (96.0) | 1 (1.0) | 4 (4.0) | |
| Education |
|
|
|
|
|
|
||
|
|
School | 92 (84.0) | 11 (10.0) | 6 (6.0) | 101 (97.0) | 1 (1.0) | 2 (2.0) | |
|
|
Higher education | 185 (78.0) | 35 (15.0) | 16 (7.0) | 215 (96.0) | 3 (1.0) | 7 (3.0) | |
|
|
Illiterate | 17 (89.0) | 1 (5.0) | 1 (5.0) | 17 (89.0) | 0 (0.0) | 2 (11.0) | |
aMedical includes doctors, pharmacists, and traditional medicine practitioners.
bMedia includes WhatsApp, Twitter, Snapchat, and the internet.
cOthers include family, friends, courses, campaigns, television, and radio.
Impacts of the Sources of Health Information on the Individual’s Health Perception and Clinical Decision-Making
Although around 86.0% (355/413) of the population reported using diverse sources for health information, 90.0% (371/413) preferred to seek help from doctors. Additionally, 68.0% (280/413) perceived to seek information from other sources only prior to a doctor’s visit. The majority disagreed on substituting a doctor’s prescription with information obtained from the internet or a friend or relative (Figure 1).
Figure 1.
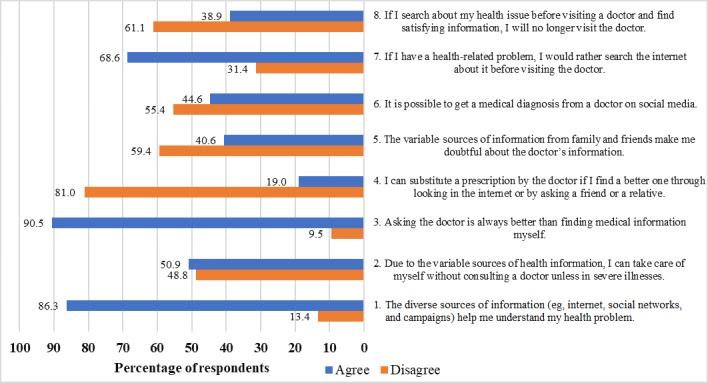
Impacts of sources of health information on an individual’s health perception and clinical decision-making.
Discussion
Principal Findings
This study aimed to investigate the different sources that the Saudi Arabian population uses and trusts for their health information and to assess the impact of these sources on an individual’s medical knowledge and health decision-making. The findings from this study revealed that doctors were the most commonly used source of health information, followed by internet search, whereas courses and campaigns were the least common sources. Doctors were the most trusted source, and unexpectedly, social media was the least trusted source. Although about half of the population admitted that various sources helped them understand their health problems, they prioritized doctor’s advice over other sources.
In this study, among the sources of information, we found that less than half of the Saudi Arabian population used the internet as a source of information. Similarly, more than half of the population did not use social media as one of the principal sources for health information. These findings did not support our study hypothesis. However, we found that more than half of the population (283/323, 87.6%) considered doctors as a primary source of information. Moreover, doctors were completely trusted for medical information by more than half of the population (326/411, 79.3%), which is similar to the findings in the study by Hesse et al, in which health care providers were the most trusted source among different populations [11].
However, 20.6% (85/411) of the population partially trusted their health care providers. This raises many concerns regarding the quality of medical care provided, as there might be an issue with the doctor-patient relationship. Many reasons could contribute to this diminished level of trust. For example, problems in communication between a doctor and patient could result in misunderstanding of the patient’s health issues, which could lead to patient dissatisfaction with the consultation. As a result, complete information will not be disclosed if the patient does not trust the doctor [15]. This affects the efficiency in patient management and consequently the trust in the doctor’s medical judgment.
Furthermore, more than half of the population stated that they will not substitute a doctor’s prescription with the information obtained from other sources. This finding is similar to that in the study by Diaz et al [10], confirming that other sources of information do not affect the certainty of the doctor’s information. In addition, it supports that initially seeking a doctor’s advice is prioritized over searching for other sources of information.
Pharmacists were considered as the second most commonly used source of information (112/194, 57.7%), although they were partially trusted by 41.4% (159/384) of the population. However, only a few respondents considered pharmacists as the first source of information (13/194, 6.7%). The fact that pharmacists follow doctors as a source of medical information is a good indicator of the population’s perception regarding the priorities for obtaining information from health care practitioners.
Despite the common use of traditional medicine by the Saudi Arabian population [16], our data revealed that traditional medicine practitioners were not trusted by the majority of the Saudi Arabian population. As a result, most of the population did not consider traditional medicine practitioners as a preferred source of information. These findings indicate that although individuals believe in traditional medicine, they do not obtain this kind of treatment from its practitioners. The reason for this is that a lot of traditional medicine practitioners in Saudi Arabia are not certified. Instead, most of them are owners of small shops of herbal remedies and practice this field of medicine as a hobby, and they lack a qualification and scientific background in this field.
Social media was not the most used or trusted source of health information by the majority of the participants. However, in the United States, more than half of the population uses social media to obtain health information [17]. Furthermore, we found that among the different social media applications, WhatsApp was the most untrusted source. These findings seem to be a good indicator of the population’s awareness that unreliable sources should not be used to obtain health information. Similarly, a large percentage of the population did not rely on doctors who are on social media to obtain diagnoses of their conditions, and instead, they used this source to acquire general health information. This finding reflects the population’s awareness of the dangers of a social media diagnosis without a medical consultation, as social media diagnosis can involve many inaccuracies despite the good intentions of the doctors. It emphasizes that doctors who are on social media need to deliver accurate and up-to-date material to avoid potentially harmful effects among their audience.
The majority of the participants did not prioritize internet searching, and more than half partially trusted this source. It is known that internet searches for medical information have well-recognized drawbacks regarding the quality and accuracy of information, as mentioned in the study by Benigeri and Pluye [18]. Surprisingly, courses and campaigns were the least used sources of information, and they were not used at all as the first source of information by the study participants. This reflects a weakness in the role of community awareness of health problems.
Strengths and Limitations
To our knowledge, this is the first study to discuss the use and trust of the Saudi Arabian population regarding different sources of medical information. The strength of this study is that the sample size was relatively large. However, a few limitations exist. The study population included many female individuals (314/413, 76%) and individuals living in the central province (362/413, 87.7%), which may not be a good reflection of the whole Saudi Arabian population. More diverse patient groups with a larger sample size may be needed to generalize the results. In addition, the data were self-reported, which might involve recall bias. Lastly, we did not investigate the types of information searched for in every source, such as sensitive topics, serious conditions, and educational information, which may change the information source preference.
Conclusion and Recommendations
This study is the first in Saudi Arabia to investigate the different sources of medical information that are used and trusted by the Saudi Arabian population. We found that doctors were the most used and trusted source, courses and campaigns were the least used sources, and social media, specifically WhatsApp, was the least trusted source. This draws attention to the need to develop well-structured courses and campaigns that meet the needs of the population in an easily understandable way. It also sheds light on the requirement to increase the quality of information provided in the nonmedical field. In addition, further research is needed to understand why a large number of participants only partially trusted their doctors.
Acknowledgments
The authors are grateful to the Deanship of Scientific Research, King Saud University, Riyadh, Kingdom of Saudi Arabia for funding through the Vice Deanship of Scientific Research Chairs. The authors would like to thank Enago (www.enago.com) for English language review.
Abbreviations
- HINTS
Health Information National Trends Survey
- KKUH
King Khalid University Hospital
Footnotes
Conflicts of Interest: None declared.
References
- 1.Choudhury S, Arora T, Alebbi S, Ahmed L, Aden A, Omar O, Taheri S. How Do Qataris Source Health Information? PLoS One. 2016;11(11):e0166250. doi: 10.1371/journal.pone.0166250. http://dx.plos.org/10.1371/journal.pone.0166250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rice R. Influences, usage, and outcomes of Internet health information searching: multivariate results from the Pew surveys. Int J Med Inform. 2006 Jan;75(1):8–28. doi: 10.1016/j.ijmedinf.2005.07.032. [DOI] [PubMed] [Google Scholar]
- 3.Beck F, Richard J, Nguyen-Thanh V, Montagni I, Parizot IR, Renahy E. Use of the internet as a health information resource among French young adults: results from a nationally representative survey. J Med Internet Res. 2014 May 13;16(5):e128. doi: 10.2196/jmir.2934. https://www.jmir.org/2014/5/e128/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simou E. Health information sources: trust and satisfaction. IJH. 2015 Oct 25;2(1):38. doi: 10.5430/ijh.v2n1p38. [DOI] [Google Scholar]
- 5.Clarke M, Moore J, Steege L, Koopman R, Belden J, Canfield S, Meadows SE, Elliott SG, Kim MS. Health information needs, sources, and barriers of primary care patients to achieve patient-centered care: A literature review. Health Informatics J. 2016 Dec;22(4):992–1016. doi: 10.1177/1460458215602939. [DOI] [PubMed] [Google Scholar]
- 6.Laranjo L, Arguel A, Neves A, Gallagher A, Kaplan R, Mortimer N, Mendes GA, Lau AY. The influence of social networking sites on health behavior change: a systematic review and meta-analysis. J Am Med Inform Assoc. 2015 Jan;22(1):243–56. doi: 10.1136/amiajnl-2014-002841. http://europepmc.org/abstract/MED/25005606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alishahi-Tabriz A, Sohrabi M, Kiapour N, Faramarzi N. Addressing the changing sources of health information in Iran. Int J Prev Med. 2013 Jan;4(1):33–41. http://europepmc.org/abstract/MED/23412519. [PMC free article] [PubMed] [Google Scholar]
- 8.Tsai M, Chou Y, Lin S, Lin S. Factors associated with adolescents' perspectives on health needs and preference for health information sources in Taiwan. Arch Dis Child. 2013 Jan;98(1):9–15. doi: 10.1136/archdischild-2012-301629. [DOI] [PubMed] [Google Scholar]
- 9.Baheiraei A, Khoori E, Foroushani A, Ahmadi F, Ybarra M. What sources do adolescents turn to for information about their health concerns? Int J Adolesc Med Health. 2014;26(1):61–8. doi: 10.1515/ijamh-2012-0112. [DOI] [PubMed] [Google Scholar]
- 10.Diaz J, Griffith R, Ng J, Reinert S, Friedmann P, Moulton A. Patients' use of the Internet for medical information. J Gen Intern Med. 2002 Mar;17(3):180–5. doi: 10.1046/j.1525-1497.2002.10603.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0884-8734&date=2002&volume=17&issue=3&spage=180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hesse B, Nelson D, Kreps G, Croyle R, Arora N, Rimer B, Viswanath K. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Intern Med. 2005;165(22):2618–24. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- 12.Dart J, Gallois C, Yellowlees P. Community health information sources--a survey in three disparate communities. Aust Health Rev. 2008 Feb;32(1):186–96. doi: 10.1071/ah080186. [DOI] [PubMed] [Google Scholar]
- 13.Rutten L, Squiers L, Hesse B. Cancer-related information seeking: hints from the 2003 Health Information National Trends Survey (HINTS) J Health Commun. 2006;11 Suppl 1:147–56. doi: 10.1080/10810730600637574. [DOI] [PubMed] [Google Scholar]
- 14.Krantz D, Baum A, Wideman MV. Assessment of preferences for self-treatment and information in health care. Journal of Personality and Social Psychology. 1980;39(5):977–990. doi: 10.1037/0022-3514.39.5.977. [DOI] [PubMed] [Google Scholar]
- 15.Dorr Goold S, Lipkin M. The doctor-patient relationship: challenges, opportunities, and strategies. J Gen Intern Med. 1999 Jan;14 Suppl 1:S26–33. doi: 10.1046/j.1525-1497.1999.00267.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0884-8734&date=1999&volume=14&issue=&spage=S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.K Suleiman A. Attitudes and Beliefs of Consumers of Herbal Medicines in Riyadh, Saudi Arabia. J Community Med Health Educ. 2013;4(2):269. doi: 10.4172/2161-0711.1000269. [DOI] [Google Scholar]
- 17.Fox S. Pew Research Center. Washington, DC: Pew Internet & American Life Project; [2019-04-16]. The Social Life of Health Information, 2011 https://www.pewinternet.org/wp-content/uploads/sites/9/media/Files/Reports/2011/PIP_Social_Life_of_ Health_Info.pdf. [Google Scholar]
- 18.Benigeri M, Pluye P. Shortcomings of health information on the Internet. Health Promot Int. 2003 Dec;18(4):381–6. doi: 10.1093/heapro/dag409. [DOI] [PubMed] [Google Scholar]


