Abstract
Purpose
The current situation of coronavirus disease 2019 (COVID-19) is rapidly evolving. Radiation therapy facilities are places of concentrated patient interactions. Oncology patients with immunosuppression are at a higher risk for contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and easily developing severe postinfection events during the SARS-CoV-2 outbreaks. This review aimed to provide some guidance and be a reference to medical professionals in radiation oncology so that they may provide oncology patients with safe and high-quality care.
Methods and Materials
This paper discussed how radiation therapy departments or centers can most effectively respond to this public health emergency through summarizing the procedures and protocols implemented at hospitals in ShenZhen, China.
Results
The impact of the virus in radiation therapy facilities can be mitigated and managed with appropriate and timely implementation of infection control procedures and protocols.
Conclusions
In the face of acute infectious disease, it is critical to maintain strict infectious disease control procedures and to create a clear clinical workflow protocol to best protect medical staff and patients from the effect of acute infectious diseases.
Introduction
With the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the novel coronavirus responsible for coronavirus disease 2019 (COVID-19), a once-every-century event is being experienced in many countries that is leading to disruptions and uncertainty.1, 2, 3
Studies have suggested that COVID-19 can have high transmission rates, with the average infected person able to spread the disease to 2 or 3 other individuals.4 SARS-CoV-2 transmission is thought to occur mainly through respiratory droplets, which can also infect an individual through direct contact with mucous membranes such as ocular surfaces.5,6 Infection can also occur through fomite-mediated transmission through close unprotected contact.7 Close contact with SARS-CoV-2–infected individuals can expose people to high concentrations of aerosolized respiratory droplets that increase the risk of transmission.5,6,8,9 Fecal shedding has been demonstrated from some patients and its significance for COVID-19 is yet to be determined.7,10 COVID-19 is characterized by a long incubation period with most cases occurring approximately 4 to 5 days after exposure,11 and there is strong evidence that SARS-CoV-2 can be transmitted by individuals who are mildly ill or even asymptomatic.12,13 Sometimes, patients can have delayed onset of symptoms or have absence of typical symptoms including fever.14,15
Compared with other potentially susceptible populations, oncology patients with immunosuppression are at a higher risk of developing severe postinfection events during the SARS-CoV-2 outbreaks. Throughout the process of preparing for and receiving radiation therapy, exposure between inter- and intradepartmental medical professionals and patients may lead to a possibility of cross-infection. Therefore, developing infection prevention protocols and procedures specifically for managing radiation oncology patients is necessary to protect patients and staff. The capacity to ensure safe and orderly administration of radiation therapy to our patients during this pandemic is critical.
In this article, we discuss how radiation therapy departments or centers can most effectively respond to this public health emergency by discussing the procedures and protocols implemented at the Pingshan District People’s Hospital, Pingshan General Hospital of Southern Medical University, Shenzhen, Guangdong; the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital & Shenzhen Hospital, the Chinese Academy of Medical Sciences and Peking Union Medical College; and the First Affiliated Hospital of Shenzhen University, Health Science Center, Second People’s Hospital, Shenzhen, Guangdong.
Antipandemic Protocols and Operations
Establishment of a COVID-19 working group at the departmental level
A working group on the clinical procedures and workflow during the pandemic should be established and led by an individual at each radiation therapy facility. Within the working group, each team member should have a clear, assigned role and be familiar with the necessary protocols on infection prevention and control. At the previously mentioned hospitals, these working groups have created protocols covering hospital and ambulatory care workflow, facility infection prevention and control, emergency operations, protective material management, and radiation therapy procedures and equipment maintenance. There have also been personnel trainings on infection protection that have included information on basic prevention precautions, airborne infection isolation room specifications, epidemiologic and clinical characteristics of COVID-19 cases, and simulation exercises on various possible situations with assessments. All personnel must be trained and screened (Appendices E1 and E2) to work.16,17 All trainings should practice maintaining distance between individuals and limiting the number of individuals in 1 area, which can be accomplished via remote meetings and conference calls.
A humanistic approach to patients should be employed, including treating patients with compassion and respect for their concerns, values, and preferences. The availability of psychological counseling services should be prioritized to individuals in need during the pandemic. Furthermore, patient education about COVID-19 should be emphasized. In the previously mentioned hospitals, educational campaigns have been employed that publicize the latest scientific knowledge about the prevention, diagnosis, and treatment of COVID-19. Medical personnel are provided training and encouraged to discuss information regarding the infection with patients. Providing factual information is paramount to reducing panic and promoting high quality care.
Appointment-based medical procedures and visits should be adopted to streamline the flow of patients to the hospital or radiation therapy facility. Working areas should be divided based on function to ensure a smooth workflow in the radiation therapy facility and to limit transmission. This is further described in the section on medical staff and patient flow management.
The “3 zones and 2 channels” management technique for medical staff and patient flow
At the previously mentioned hospitals, the “3 zones and 2 channels” management technique is used for facilitation of medical staff and patient flow through the hospital. There are 3 zones arranged to help facilitate treatment of patients: a “contaminated” area (red), a “semicontaminated” area (yellow), and a “clean” area (green). The personnel cross-infection is divided into 3 levels of risk. Level 1 indicates high-risk level for the “contaminated” zone, level 2 indicates medium-risk level for the “semicontaminated” zone, and level 3 indicates low-risk level for the “clean” zone. There are also 2 “channels.” One channel is areas that are only accessible by patients with suspected or confirmed infections, and the other channel is areas that are only accessible by routine patients and staff.
The contaminated zone at facilities is the area accessed by patients with SARS-CoV-2. The semicontaminated area at facilities is the area accessed by all patients and includes the entrance to the radiation therapy facility, the registration office/front desk, the waiting room, the patient examination rooms, the patient access elevator, and patient bathrooms. The “clean” area is a staff-only area that includes employee offices and other nonpatient work areas. For each zone, personnel should adhere to specific environment infection control protocols and strict routine disinfection of the workspace and equipment (Table 1). Individuals are prohibited from crossing between different zones and channels to reduce contamination and cross-infection. Keeping meticulous records of disinfection is necessary to also ensure a clean and safe environment.
Table 1.
Control level (zone) and disinfection policies
| Control level (zone) | Disinfection and sterilization | Machine, surface, and floor disinfection |
|---|---|---|
| Level 1: “contaminated” zone | Air sterilizer continuous operation/UV irradiation (1 hour each time, at least 2 times per day with 2 hours terminal disinfection) | 2000 mg/L chlorine disinfectant (with an action time of at least 30 minutes followed by cleaning with water after using disinfectant on metal instruments), 75% ethanol (use as directed in manufacturer instructions) |
| Level 2: “semicontaminated” zone | Disinfection according to the regulation of disinfection techniques in the health care setting as issued by the country before COVID-19 | Disinfection as according to the regulation of disinfection techniques in health care settings as issued by the country before COVID-19 |
| Level 3: “clean” zone |
Abbreviations: COVID-19 = coronavirus disease 2019; UV = ultraviolet.
Our experiences have shown that hand washing, respiratory hygiene including wearing masks, and keeping a safe distance between individuals can effectively mitigate transmission of SARS-CoV-2. Therefore, medical staff must strictly implement diligent hand hygiene before and after any contact with patients, before wearing protective equipment, and before and after removing protective equipment. Medical staff should wash hands after leaving a patient examination room, after contacting a potentially contaminated environment and articles, after exposure to any body fluids, before meals, and after using the restroom. Hand hygiene should be performed before touching hand-held electronics such as mobile phones, medical devices, or aids such as glasses.
Before their appointment in a health care facility, patients are screened at a screening checkpoint to determine whether they are exhibiting signs of a SARS-CoV-2 infection. Triage nurses are available to assess and help individuals at the main entrance outside of facilities and in the reception area of facilities. They may need to help answer patient questions about the virus, and issue up-to-date visiting notices (Fig 1). They must wear personal protective equipment including masks, caps, latex gloves, protective goggles or face shields, disposable waterproof isolation gowns, and shoe covers when they are escorting suspected or confirmed patients with SARS-CoV-2 to fever clinics, which are special infectious disease clinics that provide further evaluation and management.
Figure 1.
Triage nurse with personal protective equipment including medical mask, cap, medical grade gloves, and protective goggles in the main entrance of a facility.
Consultant physicians or medical staff from other departments also have specific procedures to limit infection risk. Upon finishing their clinical duties in a different department, the medical providers must change out of their masks and clean and disinfect frequently touched items including personal medical aids, electronic devices, pens, and other hand-held items with a 75% alcohol disinfectant solution or wet disinfectant wipes. Then, they wash their hands and return to the department only after changing into clean work clothes at designated facility changing rooms. Reusable protective goggles are collected and brought to the facility’s disinfection and sterilization division for disinfection before the next use.
Common area procedures and meeting procedures
In all common areas, a distance of at least 1 meter between seats is encouraged. For dining, limit the number of individuals that are simultaneously dining and encourage distance between individuals. If conditions permit, only 1 person should be seated per dining table. If possible, the dining area should be set up in a clean area that is separate from the work area with staff eating in different clothes than their work clothes.
Facilities are recommended to avoid holding large conferences and to work in limited numbers at a time to reduce exposure to multiple people. Events that must be held should be properly planned to reduce the number of participants and to reduce the duration of time that individuals may be exposed to potential infection. If it is necessary to meet, a large group meeting can be divided into smaller group meetings in which individuals should also wear appropriate protective equipment. It is recommended to have virtual meetings using video, audio, and text to share information remotely.
Diagnosis of COVID-19
Understanding the clinical presentation of patients with suspected and confirmed infection is vital in protecting both the medical staff and uninfected patients. Physicians should proactively educate themselves on the clinical presentation and the prevention strategies for COVID-19. The diagnosis for COVID-19 combines these epidemiologic history and clinical manifestations8:
-
A.
Epidemiologic history: See COVID-19 Screening Questionnaire (Appendix E1)
-
B.Clinical manifestations
-
a.Fever or respiratory symptoms
-
b.Characteristic COVID-19 imaging features on chest computed tomography
-
c.Normal or decreased total number of white blood cell count in the early stage of disease onset and normal or decreased lymphocyte count
-
a.
If patients meet any 1 criterion from A and meet any 2 criteria of B, or do not meet any criteria from A and meet 3 criteria from B, then they begin the facility’s emergency procedures. A confirmed case is diagnosed if 1 of the following criteria is met1,8,15:
-
•
Results of reverse transcriptase–polymerase chain reaction of the new coronavirus nucleic acid detection test are positive
-
•
Gene sequencing is highly homologous with known new coronaviruses
-
•
Sera of the new coronavirus-specific immunoglobulin M antibodies and immunoglobulin G antibodies are positive. Note: immunoglobulin G antibodies can change from negative to positive or increase 4 times or more during the recovery phase than during the acute phase.
Clinical procedures for patients receiving radiation therapy
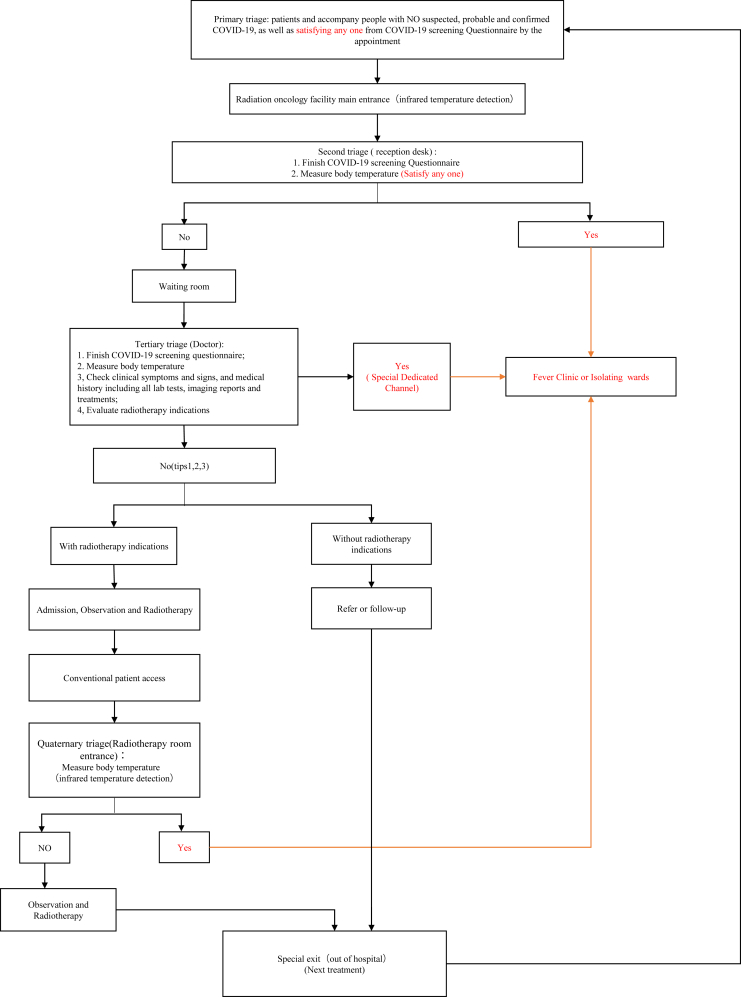
When faced with major public health emergencies from infectious diseases, infection prevention and control should begin with the initial patient appointment. Clinic and treatment areas should streamline flow through the clinic and limit traffic, including the number of patient escorts. If there is a patient who requires assistance, the patient can be accompanied by another person. The requirements for the escort are the same as the requirements for the patients receiving radiation treatment. Only patients and escorts who are not suspected to have a SARS-CoV-2 infection can enter the radiation facility. Figure 2 displays a flow chart of suggested radiation oncology facility processing.
Figure 2.
Suggested radiation oncology facility processing map.
In the Pingshan District People’s Hospital, the appointment registration area has various signs that provide visual guidance to patients and voice instructions through different electronic channels to issue up-to-date visiting notices to patients. Before their appointment, patients are screened at a screening checkpoint to determine whether they are exhibiting signs of a SARS-CoV-2 infection. For example, initially all individuals undergo infrared temperature detection before entering the radiation oncology facility (Fig 2). This type of temperature measurement uses a portable infrared thermometer to measure the temperature of the patient's head from a distance.18
All medical staff receive training regarding the appropriate protocols and procedures to follow if patients have suspected or confirmed COVID-19 or if they have fever. Physicians are trained to understand and recognize the clinical features of COVID-19. If patients are suspected or confirmed to have COVID-19 or if they have a fever, then their current radiation therapy treatment is on hold and the emergency procedure is enacted. The emergency procedure is outlined in the next section. For patients who have confirmed COVID-19, the evaluation and treatment of their acute infection takes precedence.
For prescreened patients who do not have suspected or confirmed COVID-19, they can continue to undergo their radiation treatments and follow-up appointments as scheduled. These appointments can continue as scheduled owing to the strict implementation of the previously mentioned protocols and procedures to mitigate infection risk.
Emergency procedures
Patients with suspected COVID-19 or fever begin the emergency procedures and their current radiation therapy treatment plan is suspended.
In “contaminated” zones, these standard prevention and control measures are implemented for suspected and confirmed patients with COVID-19 or fever:
-
1.
Personal protection measures are employed, including personal protection equipment, to protect against the spread of droplets and aerosols. Individuals in contact with the patient should wear appropriate personal protective equipment, including masks, caps, latex gloves, protective goggles or face shields, disposable waterproof isolation gowns, and shoe covers.
-
2.
When encountering a suspected patient with COVID-19 or with fever, the reporting physician or medical staff immediately alerts the supervising physician as well as contacting medical professionals from the fever clinic who provide further evaluation and treatment. A patient handoff process is completed with the fever clinic professionals.
-
3.
Medical staff who are directly exposed during work are also placed in infection isolation rooms immediately and medically observed.
-
4.
If the hospital or clinic is unable to appropriately manage a suspected or confirmed patient with COVID-19, then exposures need to be immediately reported to hospitals that are prepared for external transfers. After the emergency procedure is followed, the patients are then transferred to a designated treatment hospital.8
-
5.
In terms of environmental infection control, the area that the patient is transferred from is disinfected as according to the level 1 risk category.16,17 The facility should be strictly disinfected with all personnel wearing appropriate personal protective equipment.
Conclusions
Radiation therapy facilities are places of concentrated patient interactions. In the face of acute infectious disease, it is critical to maintain strict infectious disease control procedures and to create a clear clinical workflow protocol to best protect medical staff and patients from the effect of acute infectious diseases. The current situation of COVID-19 is rapidly evolving, but the effect of the virus in radiation therapy facilities can be mitigated and managed with appropriate and timely implementation of infection control procedures and protocols. We hope the present article can provide guidance and be a reference to medical professionals in radiation oncology so that they may provide oncology patients with safe and high-quality care.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: none.
Supplementary material for this article can be found at https://doi.org/10.1016/j.adro.2020.03.008.
Contributor Information
Wei Chen, Email: 1530831809@qq.com.
Guoping Sun, Email: sunguoping163@163.com.
Jun Xia, Email: xiajun@email.szu.edu.cn.
Supplementary materials
References
- 1.Sharfstein JM, Becker SJ, Mello MM. Diagnostic testing for the novel coronavirus [epub ahead of print]. JAMA. 2020. https://doi.org/10.1001/jama.2020.3864. [DOI] [PubMed]
- 2.Yang Y, Peng F, Wang R, et al. The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China [epub ahead of print]. J Autoimmun.https://doi.org/10.1016/j.jaut.2020.102434. [DOI] [PMC free article] [PubMed]
- 3.Yao X, Ye F, Zhang M, et al. In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [epub ahead of print]. Clin Infect Dis.https://doi.org/10.1093/cid/ciaa237. [DOI] [PMC free article] [PubMed]
- 4.Gates B. Responding to Covid-19 — A once-in-a-century pandemic? [epub ahead of print] N Engl J Med.https://doi.org/10.1056/NEJMp2003762. [DOI] [PubMed]
- 5.Lu C, Liu X, Jia Z. 2019-nCoV transmission through the ocular surface must not be ignored [epub ahead of print]. Lancet.https://doi.org/10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed]
- 6.Clinical updates in women's health care summary: Liver disease: Reproductive Considerations. Obstet Gynecol. 2017;129:236. doi: 10.1097/AOG.0000000000001858. [DOI] [PubMed] [Google Scholar]
- 7.Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-2019) https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf?sfvrsn=fce87f4e_2 February 16-24, 2020. Available at: Accessed March 3, 2020.
- 8.National Health Commission of the People’s Republic of China home page. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf Available at: Accessed March 3, 2020. [DOI] [PMC free article] [PubMed]
- 9.Ong SWX, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA.https://doi.org/10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed]
- 10.Xu Y, Li X, Zhu B, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding [epub ahead of print]. Nat Med. https://doi.org/10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed]
- 11.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China [epub ahead of print]. N Eng J Med.https://doi.org/10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed]
- 12.Hoehl S, Rabenau H, Berger A, et al. Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, China [epub ahead of print]. N Engl J Med.https://doi.org/10.1056/NEJMc2001899. [DOI] [PMC free article] [PubMed]
- 13.Rothe C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany [e-pub ahead of print]. N Engl J Med.https://doi.org/10.1056/ NEJMc2001468. [DOI] [PMC free article] [PubMed]
- 14.Chen N., Zhou M., Dong X. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;15:395. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med.https://doi.org/10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed]
- 16.World Health Organization Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected: Interim guidance. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 January 25, 2020. Available at: Accessed March 19, 2020.
- 17.World Health Organization Infection prevention and control during health care for probable or confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection: Interim guidance, updated October 2019. WHO/MERS/IPC/15.1 Rev. 1https://apps.who.int/iris/handle/10665/174652 Available at:
- 18.Zhang H-W, Yu J, Xu H.-J, et al. Coronavirus international public health emergencies: Implications for radiology management [epub ahead of print]. Acad Radiol.https://doi.org/10.1016/j.acra.2020.02.003. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.