Introduction
In December 2019, Wuhan, China, witnessed the outbreak of the novel coronavirus (SARS-CoV-2, Table 1), which would soon become an international public health emergency and world pandemic.1 In the United States, we are at a time where preparation for health care systems is critical. Given the rapidity with which SARS-CoV-2 is spreading, we can expect an increased burden of patients with cancer who have received a diagnosis of COVID-19 at oncology treatment clinics and a need to address this diagnosis. As of the date of this writing, the United States has witnessed an increase in confirmed cases, not far behind the large outbreaks of European countries.2,3
Table 1.
| Coronavirus fast facts | |
|---|---|
| Virus name | SARS-CoV-2 |
| Virus family | Coronaviridae |
| Virus type | (+)-ssRNA |
| Disease name | COVID-19 |
| Transmission method | Respiratory droplet |
| Viral incubation period | Median 5 (1-14) d |
| Duration of infectiousness | ~1 d postexposure to ~10 d after symptom resolution |
Since the outbreak in Wuhan, Chinese researchers have published on their experience with COVID-19 and have highlighted high-risk groups, including the elderly and patients with comorbidities, including cancer. In one of the largest series reported from Wuhan, elderly patients were at a higher risk for disease severity, with an 8.0% case fatality rate in those aged 70 to 79 years and 14.8% in those aged 80 years and older.4 The case fatality rate for patients with cancer in that cohort was notably higher than that among patients without cancer, at 5.6% versus 2.1% in the whole sample; however, it must be noted that this series is very small. How these numbers will evolve in the US population remains to be determined. Based on available data, the impact of patients both at risk for and positive for COVID-19 will be felt throughout oncology clinics. The burden this may place on radiation oncology clinics is of particular concern owing to the potential need for screening of patients for daily treatment, treatment interruptions, delays in restarting treatment, and a decreased workforce.
Patients with cancer are known to be at an increased risk for community-acquired respiratory viruses, such as influenza, because of their frequently observed immunocompromised state.5 The spread of SARS-CoV-2 is of particular concern in this vulnerable population, given the higher case fatality rate seen in Wuhan and the potentially increased severity of the disease course with COVID-19.4,6
Spread and Prevention of Exposure
Considering the Centers for Disease Control (CDC) data available on SARS-CoV-2, the virus appears to spread via respiratory droplets and contaminated surfaces and to require contact with the bodily fluids or secretions of an infected individual.7 Fortunately, modern health care facilities are usually prepared to deal with this route of spread owing to experience with other respiratory viruses, such as influenza. However, when dealing with a new pathogen for which limited information exists, predicting the efficacy of these measures is difficult. It is therefore imperative that patients with cancer be prevented from congregating in areas with potential SARS-CoV-2 carriers, which means controlling exposures in waiting rooms and treatment areas. Guidelines for prevention of other respiratory viral spread in the health care setting for patients with cancer should be followed,6,8 in addition to the continually updated recommendations from the CDC and World Health Organization.7,9 This includes screening of patients for symptoms upon entering a clinic and immediate isolation and contact precautions for patients suspected to be infected.10,11 Some clinics may opt to screen all patients upon immediate entry into the facility, or even before entering, to decrease exposure risks. For COVID-19, suspicion for infection would be high in patients with fever, cough, shortness of breath, and/or a history of recent travel to high-risk areas.7 It should be mentioned that guidelines and recommendations are likely subject to change over time as infectious disease and epidemiology experts learn more. As always, please be aware of the requirements of local and state health departments regarding reporting and regulations.
Radiation oncology clinics are uniquely taxed by an extra population of patients reporting to waiting rooms for daily radiation treatments. The large number of potential appointments and/or daily treatments, in addition to a pre-existing disease state, heightens the risk faced by radiation oncology patients. As noted in the SARS outbreak experience in radiation oncology clinics, we will continue to have a lag time even if new consultations are postponed, owing to patients currently on active treatment for weeks at a time.12 Cancelation of elective procedures will only limit the caseload by a fraction in our specialty, and we therefore must maintain efficient protocols of screening and triage to effectively lower risk to patients and staff.
Another consideration is that of shared treatment machines. Members of this patient group are treated on one of a few machines shared among many patients daily, depending on the center. It is therefore imperative that radiation oncology clinics review established infection control protocols and adapt as necessary to the unique considerations of SARS-CoV-2, in accordance with CDC recommendations. Screening by front desk staff upon check-in and triage with nursing and physicians is necessary to protect patients and to prevent possible exposures in both waiting rooms and treatment vaults. How to implement screening in the optimal fashion is a question that is evolving rapidly, and triaging patients remotely is vital.13 Remote screening has the potential to offset the load of individuals presenting to emergency rooms and clinics, avoiding possible exposures.13
Lastly, areas contaminated by a person under investigation or a patient with confirmed COVID-19 should ideally be decontaminated. Currently, the CDC recommends routine cleaning and disinfection procedures as appropriate for SARS-CoV-2 in the health care setting.14 Unique considerations in radiation oncology may include active breathing control devices, handles for arm positioning, and any attachments of the treatment couch that contact the patient. Attention should also be paid to the time of day patients with suspected COVID-19 are treated. High-risk patients should be treated at times that facilitate appropriate sterilization and minimize staff and patient exposure. Finally, efforts must be made to discard potentially contaminated personal protective equipment and/or garments before leaving the hospital so as not to carry viral particles outside.
Table 2 provides a selection of strategies to reduce infectious risk to patients and staff members in the clinic. Bass and Washington15 provide a more thorough array of the unique considerations in their book chapter dedicated to “Infection Control in Radiation Oncology Facilities.”
Table 2.
Example of COVID-19 radiation oncology clinic risk mitigation strategies
| Screening |
|
| |
| |
| Sanitation |
|
| |
| |
| |
| |
| |
| Containment |
|
| |
| Exposure |
|
| |
| |
| |
|
Abbreviation: CDC = Centers for Disease Control.
Impact of Treatment Interruptions
Radiation oncologists will also have to prepare for treatment interruptions caused by development of COVID-19 in patients with cancer. Patients who test positive for the novel coronavirus will, at a minimum, require a 14-day quarantine per CDC recommendations.16 At the other end of the spectrum, patients with cancer with immunosuppression may require hospitalization and isolation precautions, thus preventing the continuation of radiation treatments. Data from a report of the clinical characteristics of patients with COVID-19 showed that 6.1% of patients required intensive care or mechanical ventilation or died.17 Although it is yet unclear how the virus will behave in the United States, the situations in China and Italy suggest the burden on hospitals and intensive care units will be significant. Additionally, this study demonstrated that pneumonia and lymphocytopenia were prominent at 91.1% and 83.2%, respectively, which would affect decisions to delay treatments pending improvements in the patient’s clinical status and immune recovery.17 These treatment interruptions would be of utmost concern in tumors for which treatment package time significantly affects outcomes, such as head and neck and cervical tumors.18,19 This is also of concern in lung tumors and other thoracic tumors, both for tumor control and the lungs potentially lying in the path of treatment beams. Treatments would likely need to be paused while monitoring the course of COVID-19 in this setting. Treatment delays may also be due to strains on the health care system in the setting of a pandemic due to travel restrictions, availability of workforce, and/or lack of access to hospital care.20 If possible, travel restrictions for the general public should be tailored for patients with cancer, such as what is being done currently in Italy.21
Few data exist currently to guide radiation treatment decisions in the setting of a pandemic. However, we may borrow insight from the response of radiation oncology clinics during Hurricane Maria. As per Gay et al,22 mitigating the impact of a natural disaster on patients with cancer requires 4 components, or “PCOC”: prepare, communicate, operate, compensate. In preparing, consideration should be made for scenarios that may require delayed treatment starts or shorter fractionation regimens (ie, hypofractionation), given that COVID-19 poses a substantial immediate risk for elderly patients. Again, there is a paucity of data to guide these decisions, and priority should be given to higher risk tumors (eg, head and neck, cervix, lung), which are nicely referenced in the Hurricane Maria review. Overall, the immediate risk of COVID-19 will have to be weighed against the long-term risks associated with the specific cancer diagnosis.
Separately, patients receiving systemic agents including chemotherapy and/or targeted therapies will require input from multidisciplinary teams. Thus far, there are little data outside of 1 case report from China of a patient with EGFR T790M mutant advanced lung adenocarcinoma who was diagnosed with COVID-19, developed pneumonia, and then fully recovered.23 He was maintained on osimertinib during treatment for COVID-19, although radiation treatment was halted after the ninth fraction. Overall, systemic and radiation treatment adjustments will have to be discussed with input from the oncologic specialists and on an individual basis.
Upon recovery from COVID-19, patients will need to be cleared to return to the clinic. To ensure full recovery and no risk for asymptomatic transmission to other patients, a negative polymerase chain reaction test would ideally be required. Per current CDC recommendations on March 12, 2020, “Negative results of an FDA emergency use authorized molecular assay for COVID-19 from at least two consecutive sets of paired nasopharyngeal and throat swabs specimens collected ≥24 hours apart” are required before discontinuing home isolation.24 However, with a surge in demand for testing kits, the ability to do such testing remains unpredictable. If testing is simply not available, the return of recovered patients may be at the discretion of the treating physician, radiation oncologist, and infection control officials of the hospital.
Screening for In-Person Visits
In trying to prevent community spread to nonaffected patients with cancer, some clinics may consider alternatives to in-person triage and visits for sick patients as mentioned by the CDC guidance for outpatient facilities.11 This may entail training of front desk staff to screen patients via telephone before scheduling new appointments. For radiation oncology clinics, this may also require rescheduling of nonessential follow-up visits or diverting these visits to telemedicine if available.13 Because a large proportion of our patients are elderly, discretion is needed to protect this vulnerable group from exposure. Visits past the 5-year mark for patients with no evidence of disease or concerning symptoms should be considered for rescheduling if all clinical, laboratory, and imaging data suggest low risk for recurrence. This would ideally be at the discretion of the treating physician with appropriate clinically specific concern. However, in the context of elevated community-spread risk of a new pathogen with a considerable fatality rate among the elderly, it seems prudent to re-evaluate the timing of follow-up visits for patients who are clinical without evidence of disease with long disease-free intervals.
Impact of a Decreased Workforce
We will have to prepare for a shortage of health care workers in radiation oncology clinics in the near term as well. In the Wuhan outbreak, as reported by Wu and McGoogan,4 63% of health care workers became infected, and 14.8% of cases in health care personnel were severe or critical. Although it is too early to predict how this will affect the US workforce, the number is suggestive of a great potential for a shortage of providers. Additionally, some clinicians will remain home to serve as caregivers for others who are ill. Just as patients are at risk for possible quarantine or hospitalization, so are health care workers, and we will need to adapt accordingly. This may mean other measures in addition to the strict travel restrictions being implemented by many institutions, such as identification of back-up staff or consideration for staff teams who can rotate to retain a team at all times.12 Furthermore, thought may be put into essential and nonessential staff as the outbreak grows, as was done during the SARS experience in Canada.25 Consideration of remote work for nonessential members should be reviewed. As an example, some institutions may ask some members of the dosimetry and/or physics teams to work remotely to decrease unnecessary risk of viral transmission. This should also include a strict policy on remaining home when ill or potentially ill to avoid unnecessary exposures to both patients and staff. Data from Wuhan are unavailable regarding oncology staff management during the outbreak. The situation in Italy is evolving rapidly but may serve as a useful model in the coming weeks.
Management of the COVID-19–Positive Patient
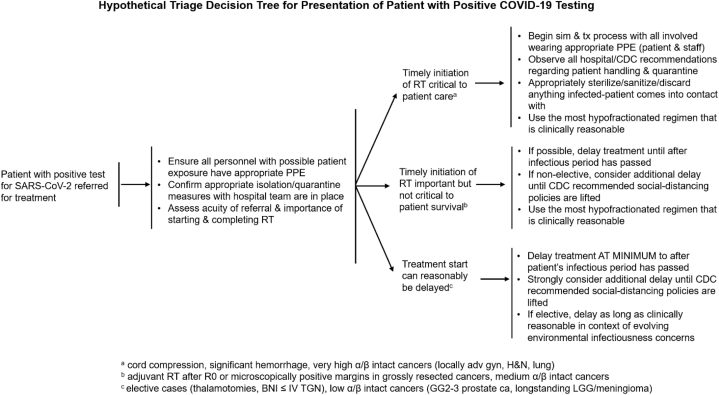
The inevitable presentation of a COVID-19–positive patient to a radiation oncology clinic promises to pose significant challenges to the staff, administration, and physician who are charged with not only that patient’s care and well-being, but also the care and well-being of other patients (and staff) in the department. Figure 1 is a diagram depicting a hypothetical triage decision tree for a patient presenting to a radiation oncology clinic with a recent positive test for the COVID-19 virus, informed by attention to the CDC outpatient guidelines and the Bass and Washington radiation facility infection control textbook chapter.11,15
Figure 1.
A hypothetical decision tree for the triage of a patient with COVID-19 referred for radiation therapy. Example triage decision tree for patient who presents to a radiation oncology clinics with a positive COVID-19 test.
The American Society of Radiation Oncology (ASTRO) recommends encouraging staff who interface with a high volume of patients, such as therapists, to wear non-N95 masks, if available. Droplet precautions are essential for any patient with positive or suspected COVID-19.26 The clinical landscape with respect to the management of patients with COVID-19 continues to evolve at a galloping pace, and professional societies, including ASTRO, continue to work to develop useful and evidence-based guidelines for the management and care of patients as that landscape changes. We encourage clinicians to look to these updated guidelines as they are released for the most up-to-date and informed management information.
Conclusions
Overall, it is important to remember that radiation oncology clinics have always functioned as an interdisciplinary team of support staff, nurses, therapists, dosimetrists, physicists, and physicians, all aiming to help patients with cancer. Heading into the fight with COVID-19, that team nature and vision to protect patients with cancer remain critical. As the World Health Organization reminds us during this time: “Be safe, be smart, be kind.”
Updated information on the coronavirus from ASTRO can be found at www.astro.org/coronavirus and from the American Society of Clinical Oncology at www.asco.org/asco-coronavirus-information.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: Dr Knoll reports consulting fees from Bristol Myers Squibb outside of the submitted work. Dr Ohri reports consulting fees from Merck and AstraZeneca outside of the submitted work. Dr Thomas reports honoraria from Varian Medical Systems outside of the submitted work. Dr Rivera reports no disclosures. Dr Miller is editor-in-chief of Advances in Radiation Oncology.
References
- 1.Coronavirus disease (COVID-19) outbreak. World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at:
- 2.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gardner N. Mapping 2019-nCoV. https://www.arcgis.com/apps/opsdashboard/ Available at:
- 4.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 5.Thom K.A., Kleinberg M., Roghmann M.C. Infection prevention in the cancer center. Clin Infect Dis. 2013;57:579–585. doi: 10.1093/cid/cit290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention What healthcare personnel should know about caring for patients with confirmed or possible COVID-19 infection. https://www.cdc.gov/coronavirus/2019-ncov/hcp/caring-for-patients.html Available at:
- 8.Ariza-Heredia E.J., Chemaly R.F. Update on infection control practices in cancer hospitals. CA Cancer J Clin. 2018;68:340–355. doi: 10.3322/caac.21462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf Available at:
- 10.Sehulster L., Chinn R.Y., CDC, HICPAC Guidelines for environmental infection control in health-care facilities. Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC) MMWR Recomm Rep. 2003;52:1–42. [PubMed] [Google Scholar]
- 11.Basic infection control and prevention plan for outpatient oncology settings. Atlanta, Georgia: Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention. https://www.cdc.gov/hai/pdfs/guidelines/basic-infection-control-prevention-plan-2011.pdf Available at:
- 12.Mukherjee R.K., Back M.F., Lu J.J., Shakespeare T.P., Wynne C.J. Hiding in the bunker: Challenges for a radiation oncology department operating in the Severe Acute Respiratory Syndrome outbreak. Australas Radiol. 2003;47:143–145. doi: 10.1046/j.0004-8461.2003.01165.x. [DOI] [PubMed] [Google Scholar]
- 13.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention Interim guidance for healthcare facilities: Preparing for community transmission of COVID-19 in the United States. https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/guidance-hcf.html Available at:
- 15.Bass L.H., Washington C.M.S. Principles and Practice of Radiation Therapy. Mosby; St. Louis, MO: 2015. Infection control in radiation oncology facilities; pp. 178–218. [Google Scholar]
- 16.Centers for Disease Control and Prevention Interim guidance for implementing home care of people not requiring hospitalization for 2019 novel coronavirus (2019-nCoV) https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-home-care.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fguidance-home-care.html Available at:
- 17.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goel A.N., Frangos M.I., Raghavan G. The impact of treatment package time on survival in surgically managed head and neck cancer in the United States. Oral Oncol. 2019;88:39–48. doi: 10.1016/j.oraloncology.2018.11.021. [DOI] [PubMed] [Google Scholar]
- 19.Song S., Rudra S., Hasselle M.D. The effect of treatment time in locally advanced cervical cancer in the era of concurrent chemoradiotherapy. Cancer. 2013;119:325–331. doi: 10.1002/cncr.27652. [DOI] [PubMed] [Google Scholar]
- 20.Wang H., Zhang L. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020 doi: 10.1016/S1470-2045(20)30149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.What to expect: Oncology’s response to coronavirus in Italy. https://cancerletter.com/articles/20200311_1/ Available at:
- 22.Gay H.A., Santiago R., Gil B. Lessons learned from Hurricane Maria in Puerto Rico: Practical measures to mitigate the impact of a catastrophic natural disaster on radiation oncology patients. Pract Radiat Oncol. 2019;9:305–321. doi: 10.1016/j.prro.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 23.Zhang H., Huang Y., Xie C. The treatment and outcome of a lung cancer patient infected with SARS-CoV-2. J Thorac Oncol. 2020 doi: 10.1016/j.jtho.2020.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention Interim guidance for discontinuation of in-home isolation for patients with COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html Available at:
- 25.Stewart J., Savage P., Johnson J.C., Saunders C. Telling the story of SARS: Compassionate oncology care in the face of a futuristic health crisis. Can Oncol Nurs J. 2005;15:175–183. doi: 10.5737/1181912x153175178. [DOI] [PubMed] [Google Scholar]
- 26.COVID-10 FAQs. https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/COVID-19-FAQs Available at:
- 27.Lauer S.A., Grantz K.H., Bi Q. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Woelfel R., Corman V.M., Guggemos W. Clinical presentation and virological assessment of hospitalized cases of coronavirus disease 2019 in a travel-associated transmission cluster. medRxiv. 2020 2020.2003.2005.20030502. [Google Scholar]