Abstract
Background
Minimally invasive hysterectomy may require the use of morcellation to remove the uterus. In the presence of unexpected sarcoma, morcellation risks disseminating malignant cells and worsening survival outcomes. As a consequence, in 2014 the US Food and Drug Administration (FDA) issued a black box warning against the use of power morcellator for the treatment of uterine fibroids. However, the proportion of unexpected sarcoma at the time of hysterectomy for presumed benign indication remains unclear.
Objective
To estimate the incidence of sarcoma among women undergoing hysterectomy for benign indication in Olmsted County, Minnesota, between 1999 and 2013.
Methods
We conducted a population-based study including all hysterectomies performed for benign indication in Olmsted County women between 1/1/1999 and 12/31/2013. Cases were identified using the medical records-linkage system of the Rochester Epidemiology Project, and data were abstracted by a gynecologist who reviewed the complete medical records of each woman who underwent hysterectomy. An expert pathologist reviewed the pathologic slides of each sarcoma to ensure the accuracy of the diagnosis. Incidences of sarcoma (overall and by type of sarcoma) were estimated both overall and stratified by menopausal status, indication for surgery, and uterine weight as a rate per 100 persons.
Results
A total of 4,232 hysterectomies were performed during the study period. Among them, we identified 16 sarcomas, of which 11 (69%) were suspected pre-operatively and 5 (31%) were unexpected. Of the total number of hysterectomy, 3,759 (88.8%) were performed for benign indication. Among those, the incidence of unexpected sarcoma was 0.13% (5/3,759 [95% CI, 0.04 to 0.31%]). Uterine fibroids comprised 27.3% (n=1,025) of all hysterectomies for benign indication and was the indication most commonly associated with diagnosis of unexpected sarcoma. The incidence of unexpected sarcoma among surgeries for uterine fibroids was 0.35% (3/851) for premenopausal women and 0.57% (1/174) for peri/postmenopausal, and all 4 unexpected sarcomas were leiomyosarcoma. The incidence of unexpected sarcoma progressively increased with higher uterine weight with an incidence of 0.03% (1/2,993) among women with a uterine weight <250 grams versus 15.4% (2/13) with a uterine weight >=2,000 grams.
Conclusions
Unexpected uterine sarcoma was low in all women undergoing hysterectomy for benign indication (0.13% or 1 in 752 surgeries), while increased in women with uterine fibroids (0.39% or 1 in 256 surgeries). Peri-post-menopausal women, women with large uteri, and age ≥45 were risk factors for sarcoma.
Keywords: hysterectomy, uterine fibroids, uterine sarcoma, morcellation, Olmsted County
CONDENSATION:
In patients who undergo hysterectomy for uterine fibroids, the incidence of uterine sarcoma is 0.6%; age ≥45 and uterine weight are associated with risk of uterine sarcoma.
Introduction
Hysterectomy is the most common major gynecologic surgery performed in the United States, with over 600,000 hysterectomies performed each year for benign indications1,2. Among those, uterine fibroids represent the most frequent indication, accounting for approximately 30–40% of all benign hysterectomies1. By contrast, uterine sarcomas are rare and aggressive tumors, accounting for approximately 1% of the female tract malignancies3, and with an incidence of 3–7 per 100,000 women4. During the last decades, the surgical approach to hysterectomy shifted from open laparotomy to minimally invasive (laparoscopic-assisted or robotic-assisted), which is preferred by most women because it is less invasive, associated with lower rate of complications, and has faster recovery5,6. Minimally invasive approach may require the use of morcellation to facilitate the extraction of the specimens from the vagina or through the small port incisions, especially in the presence of a large uterus with fibroids. This process of morcellation carries the risk of disseminating benign or malignant disease7–10. In the latter case, dissemination of malignant tissue would increase risk of recurrence and shorten survival11.
In the last four years, the use of morcellation has come under scrutiny because of a hysterectomy case where a leiomyosarcoma (LMS) presumed to be a benign fibroid was incidentally morcellated12. As a consequence, the FDA “warned against” the use of uterine power morcellation, issuing “contraindications” for its use in “peri- and post-menopausal” women, and in patients with “suspected or known malignancy”13. Also, the FDA reported a meta-analysis which estimated that the rates of unexpected sarcoma and LMS at the time of surgery for presumed benign fibroids were 1 in 352 surgeries (0.28%) and 1 in 498 surgeries (0.20%), respectively14. Several studies reported the incidence of unexpected sarcoma among women who underwent hysterectomy with an indication of uterine fibroids, ranging from 0.00–0.49%15. Given the varying incidence reported by those studies, we conducted a population-based study aimed to estimate the incidence of unexpected sarcoma (overall and by type of sarcoma) among women who underwent hysterectomy for benign indication. We also stratified the incidence of unexpected sarcoma by factors that may increase the risk of sarcomas, such as menopausal status, indication for surgery, and uterine weight.
Materials and Methods
We conducted a population-based study using the Rochester Epidemiology Project (REP), a unique medical records-linkage system established in 1966 and including the health records of virtually all residents of Olmsted County, Minnesota, regardless of insurance status16,17. The REP includes the health care information of a dynamic cohort of over 500,000 unique individuals who resided in Olmsted County from 1966 up to the present day17. Participants who do not provide permission to use their medical records for research are excluded from research studies (<3% of the overall population)17. The institutional review board (IRB) of both Mayo Clinic (#15–003573) and Olmsted Medical Center (032-omc-15) approved the present study.
Using the REP medical records-linkage system, a REP database specialist identified all hysterectomies performed among residents of Olmsted County from 1/1/1999 to 12/31/2013 using the International Classification of Diseases, Ninth Revision (ICD-9) procedures codes for hysterectomy. To confirm the hysterectomies and to obtain the clinical data, the complete medical records of each woman who underwent a hysterectomy was extensively reviewed by one of three gynecologists (F.M., J.C., L.T.) following a specifically designed abstracting form. Prior to review, all data abstractors agreed on definitions and interpretation of each collected variables, and conflicts were resolved by consensus. We defined peri-menopausal status as women who were still having bleeding (normal or abnormal menstrual pattern), but perimenopause was documented in the clinical notes. Uterine weight was obtained from the pathology report.
Uterine sarcomas were identified by reviewing the pathologic reports of all hysterectomies performed during the time period of the study. To ensure the accuracy of diagnosis of uterine sarcoma, an expert pathologist (Y.H.) re-reviewed the pathologic slides.
The incidence of sarcomas among all hysterectomies and the incidence of unexpected sarcomas among hysterectomies for benign conditions are expressed as a rate or percentage per 100 hysterectomies. Incidences of unexpected sarcomas (overall and by type of sarcoma) were stratified by age, menopausal status (pre- vs. peri-/post), indication for surgery (uterine fibroids vs. other benign indication), and uterine weight. A ninety-five percent confidence interval for each incidence rate was constructed using an exact test for a binominal parameter. Fisher’s exact test was used to compare incidences between groups and Cochran-Armitage trend was used to test for a trend in incidences across ordinal age and uterine weight categories. All calculated p-values were two-sided and p-values less than 0.05 were considered statistically significant.
The study is reported following the Strengthening the Reporting of Observational studies in Epidemiology (STROBE statement) recommendations18.
Results
A total of 4,232 women had hysterectomies performed in Olmsted County, MN during the time period of the study. Of these 4,232 women, 450 underwent hysterectomy where malignancy was found on pathologic examination and 23 had a pregnancy-related indication (Figure 1). The remaining 3,759 (88.8%) women had a hysterectomy for benign indications.
Figure 1.
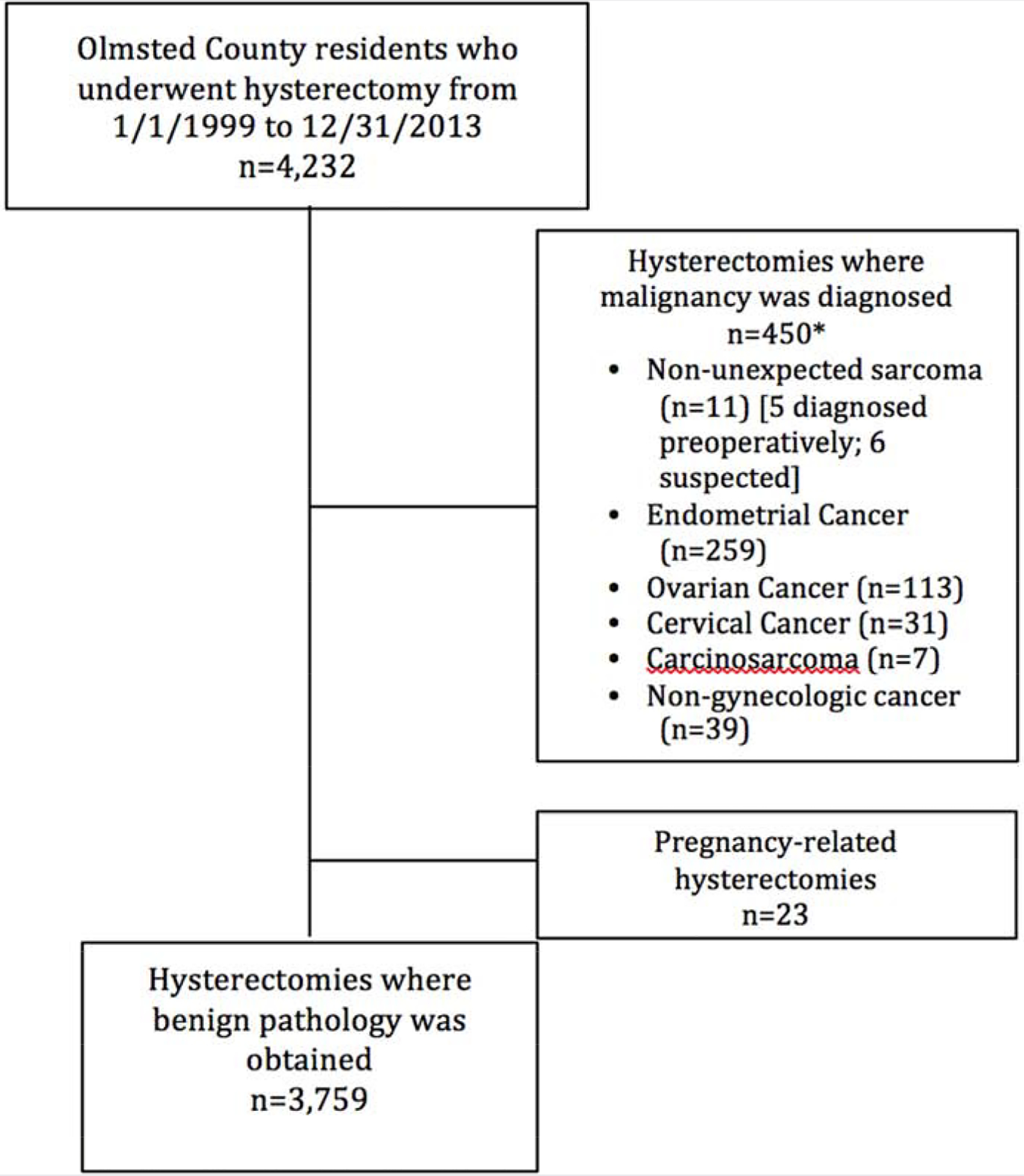
Flow chart of the study population
*10 women had synchronous cancers.
Among the total 4,232 women with hysterectomy, we identified 16 sarcomas (6 LMS, 4 low-grade endometrial stromal sarcoma (ESS), 3 high-grade ESS, 2 adenosarcoma, and 1 rhabdomyosarcoma), of which 11 were suspected preoperatively (5 pre-operative diagnosis of sarcoma, 6 pelvic mass of unknown origin) and 5 were unexpected. Patients’ and tumor characteristics of 16 women with a sarcoma are reported in Table 1. All the 16 women were white. The mean (SD) age at diagnosis of sarcoma was 54.6 (10.6), and the median BMI was 32.5 (range 22.9–48.6). Preoperative imaging was obtained for 15 of the 16 women (94%): 8 had pelvic ultrasound, 4 computed tomography (CT) scan, 1 magnetic resonance imaging (MRI), 1 ultrasound and MRI, and 1 ultrasound and CT scan. Preoperative endometrial biopsy was performed in 4 of 16 patients. In total, preoperative diagnosis of sarcoma was found in 5 of 16 (31%) women, 1 with a CT guided biopsy on an asymptomatic women with incidental finding of uterine mass; 3 with a preoperative endometrial biopsy (1 LMS, 1 adenosarcoma, 1 rhabdomyosarcoma) on patients with postmenopausal bleeding; and 1 with a myomectomy on a women with presumed benign fibroids. The majority of the 16 women (81%) underwent an open abdominal approach, 1 was performed with laparoscopic-assisted vaginal approach, and the 2 remaining were performed vaginally (one of them was converted to robotic-assisted for staging after the intraoperative frozen section diagnosis of low-grade ESS). Of the 16 women with sarcoma, one with a low-grade ESS who had an intraoperative dilation and curettage of the uterus showing benign endometrium underwent manual morcellation. After 5 years of follow-up, she remained alive and disease-free.
Table 1.
Patients’ and tumor characteristics of Olmsted County, Minnesota women diagnosed with uterine sarcoma (n=16) from 1/1/999 to 12/31/2013.
| Diagnosis | Age at diagnosis (years) | BMI (kg/m2) | Menopausal status at diagnosis | Symptoms | Preoperative endometrial biopsy | Preoperative imaging | Surgical approach | Morcellation | FIGO 2009 staging for uterine sarcoma | Tumor grade | Largest tumor dimension (cm) | Uterine weight (grams) | Vital status | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Indication: Uterine fibroids | |||||||||||||||
| 1 | LMS | 55 | 34 | Post | Pelvic pressure | Not performed | Ultrasound | Open | No | IB | Grade 1 | 14 | 1325 | DOD after 6 months | |
| 2 | LMS | 45 | 29 | Pre | Heavy menstrual bleeding | Not performed | Ultrasound | Open | No | IB | Grade 3 | 8.5 | 1150 | NED after 12 years | |
| 3 | LMS | 50 | 35 | Pre | Heavy menstrual bleeding | Not performed | Ultrasound | Open | No | IVA | Grade 4 | 15 | 2290 | NED after 1 years | |
| 4 | LMS | 46 | 38 | Pre | Heavy menstrual bleeding | Not performed | Ultrasound | Open | No | IB | Unknown | 18 | 2641 | NED after 4 years | |
| Indication: Pelvic organ prolapse | |||||||||||||||
| 5 | Low-Grade ESS | 76 | 32 | Post | Pelvic Organ Prolapse | Not performed | No | Vaginal | No | IA | Low Grade | 3.5 | 175 | NED after 4 years | |
| Indication: Uterine mass of unknown origin suspicious for malignancy | |||||||||||||||
| 6 ƚ | Adenosarcoma | 64 | 49 | Post | Pelvic pain | Not performed | Ultrasound, CT scan | Open | No | IA | Unknown | 4 | 230 | NED after 12 years | |
| 7 | ESS | 59 | 23 | Post | Pelvic pain | Not performed | CT scan | Open | No | IVB | High Grade | 10 | 650 | DOD after 4 months | |
| 8 | Low-Grade ESS | 43 | 27 | Pre | Unknown | Not performed | Ultrasound, MRI | Vaginal converted to robotic for staging | Yes | IB | Low Grade | 7.5 | 275 | NED after 5 years | |
| 9 | ESS | 53 | Unknown | Post | Pelvic pain | Not performed | Ultrasound | Open | No | IIA | Low Grade with focal areas of High Grade | 15 | 1,075 | DOD after 4 years | |
| 10 | ESS | 65 | 40 | Post | Post-menopausal bleeding | Yes: no abnormal pathology | CT scan | Open | No | IB | High grade | 14 | 1,490 | DOD after 3.years | |
| 11 ‡ | Low-Grade ESS | 52 | 30 | Post | Post-menopausal bleeding | Not performed | Ultrasound | Open | No | IA | 3 | 3 | 140 | DOD after 4 years | |
| Indication: pre-operatively diagnosed uterine sarcoma | |||||||||||||||
| 12 | Adenosarcoma | 58 | 24 | Post | Post-menopausal bleeding | Yes: diagnosis of sarcoma | MRI | Open | No | IA | Low Grade | 7 | 270 | NED after 6 years | |
| 13 | Low-Grade ESS | 34 | 30 | Pre | Heavy menstrual bleeding | Not performed | Ultrasound | Open | No | IB | Low Grade | 20 | 1501 | NED after 10 years | |
| 14 | LMS | 61 | 32 | Post | Post-menopausal bledding | Yes: diagnosis of sarcoma | Ultrasound | Open | No | IVB | Grade 4 | 9.5 | 840 | DOD after 3 months | |
| 15 | Rhabdomyosarcoma | 60 | 28 | Post | Post-menopausal bleeding | Yes: diagnosis of sarcoma | CT scan | LAVH | No | IB | Unknown | 7.5 | 273 | DOD after 2 years | |
| 16 | LMS | 47 | 39 | Pre | Incidental finding on imaging | Not performed | CT scan | Open | No | IVB | Grade 1 | 9.5 | 585 | NED after 11 years | |
DOD: Dead of disease; ESS: Endometrial stromal sarcoma; CT: Computed tomography; LAVH: laparoscopic-assisted vaginal; LMS: Leiomyosarcoma; MRI: Magnetic resonance imaging; NED, no evidence of disease.
A frozen section biopsy changed the surgical approach
A cervical biopsies indicated malignancy
Uterine weight was substantially larger for women with LMS and ESS. The median uterine weight for all 16 women was 745 grams (range 140–2641), with median of 1237 grams (range 585–2641) for women with LMS and median of 650 grams (range 140–1501) for women with ESS. The three women with adenosarcoma and rhabdomyosarcoma had uterine weights of 230 to 273.
Among the 3,759 women with hysterectomy for a benign indication, the mean (SD) age at hysterectomy was 47.0 (11.1) years and the mean (SD) BMI was 29.0 (6.7) kg/m2. The majority were white (n=3,513, 93.5%), followed by black (n=86, 2.3%) and Asian (n=61, 1.6%). The majorities were performed vaginally (2,280, 60.6%), followed by open abdominal approach (1,030, 27.4%), and minimally invasive approach (laparoscopic, laparoscopic-assisted vaginal approach, and robotic)(449, 11.9%). We identified 5 unexpected sarcomas among these 3,759 women, for an incidence of 0.13% (95% CI, 0.04 to 0.31%), including 4 LMS and 1 Low-Grade ESS (Table 2). Thus, in our cohort, the incidence of unexpected LMS was 0.11% (4/3759), whereas the incidence of low-grade ESS was 0.03% (1/3759). The incidence of unexpected sarcoma was not observed to be significantly higher in peri/post-menopausal women compared with pre-menopausal women (0.18% (2/1116) vs. 0.11% (3/2643), p=0.64).
Table 2.
Incidence of unexpected uterine sarcoma based on preoperative surgical indication and menopausal status, among 3,759 hysterectomies performed for benign indications among residents of Olmsted County, Minnesota, from 1/1/1999 to 12/31/2013.
| Stratum | N (%) with unexpected sarcoma within each stratum | |||
|---|---|---|---|---|
| Indication for hysterectomy | Menopausal status | LMS | Low-Grade ESS | Total [95% CI] |
| Uterine fibroids | Pre (N=851) | 3 (0.35%) | 0 | 3 (0.35%) [0.07 – 1.03%] |
| Peri-/Post (N=174) | 1 (0.57%) | 0 | 1 (0.57%) [0.01 – 3.16%] | |
| Total (N=1025) | 4 (0.39%) | 0 | 4 (0.39%) [0.11 – 1.00%] | |
| Other benign indications | Pre (N=1792) | 0 | 0 | 0 (0%) [0.00 – 0.21%] |
| Peri-/Post (N=942) | 0 | 1* (0.11%) | 1 (0.11%) [0.00 – 0.59%] | |
| Total (N=2734) | 0 | 1* (0.04%) | 1 (0.04%) [0.00 – 0.20%] | |
| All benign indications | Pre (N=2,643) | 3 (0.11%) | 0 | 3 (0.11%) [0.02 – 0.33%] |
| Peri-/Post (N=1,116) | 1 (0.09%) | 1* (0.09%) | 2 (0.18%) [0.02 – 0.65%] | |
| Total (n=3,759) | 4 (0.11%) | 1* (0.03%) | 5 (0.13%) [0.04 – 0.31%] | |
LMS: Leiomyosarcoma; ESS: Endometrial stromal sarcoma.
Diagnosed in a patient who underwent hysterectomy for pelvic organ prolapse.
None of the High-Grade ESS, Adenosarcoma, and Rhabdomyosarcoma were unexpected.
After stratification by indication of surgery, the majority of unexpected sarcoma (4 out of 5, 80%) was diagnosed among the 1,025 patients who underwent hysterectomy for presumed benign fibroids, with an incidence of unexpected sarcoma of 0.39%. All 4 unexpected sarcoma diagnosed after surgery for benign fibroids were LMS. Also, in this subgroup of women with an indication of benign fibroids, the incidence of unexpected sarcoma was higher for peri-/postmenopausal compared to premenopausal women, although the difference was not statistically significant (0.57% (1/174) vs. 0.35% (3/851), p=0.53).
The age-stratified risk of unexpected sarcoma increased with increasing age (p=0.037, Table 3), with all age groups ≥ 45 years having higher risk than the overall risk of 0.13% or 1 in 752, except for the age group 65–74 years in which we did not identify any unexpected sarcoma. No unexpected sarcoma occurred in women under age 45 years.
Table 3.
Incidence of unexpected sarcoma by age among women undergoing hysterectomy for benign indications in Olmsted County, Minnesota, from 1/1/1999 to 12/31/2013 (n=3,759).
| Age at hysterectomy (years) | N (%) with unexpected sarcoma within each age stratum | ||
|---|---|---|---|
| LMS | Low-Grade ESS | Total | |
| <35 (N=357) | 0 | 0 | 0 |
| 35–44 (N=1368) | 0 | 0 | 0 |
| 45–54 (N=1333) | 3 (0.22%) | 0 | 3 (0.22%) |
| 55–64 (N=365) | 1 (0.27%) | 0 | 1 (0.27%) |
| 65–74 (N=233) | 0 | 0 | 0 |
| ≥ 75 (N=103) | 0 | 1 (0.97%) | 1 (0.97%) |
LMS: Leiomyosarcoma; ESS: Endometrial stromal sarcoma.
Stratification by uterine weight showed that higher uterine weights were directly associated with an increase in the incidence of unexpected sarcoma (p<0.001, Table 4). The incidence of unexpected sarcoma was 0.03% (1/2,993) among women with a uterine weight <250 grams versus 14.3% (2/14) with a uterine weight ≥2,000 grams. Because the number of unexpected sarcomas was low, we performed a secondary analysis including all sarcomas (n=16) to estimate the incidence of sarcoma among all hysterectomies (n=4,232) stratified by uterine weight (Supplementary Table 1). Similar to the incidence of unexpected sarcoma, the incidence of any sarcoma progressively increased among all hysterectomy with increasing uterine weight from 0.09% among women with uterine weight < 250 grams to 0.7%, 1.4%, 6.3%, 11.1%, and 14.3%, among women with uterine weight 250–499, 500–999, 1000–1499, 1500–1999, and ≥2000 grams, respectively (p<0.001). Interestingly, all 6 LMS diagnosed in our cohort had uterine weight ≥500 grams, with 4 of them being ≥1000 grams.
Table 4.
Incidence of unexpected sarcoma by uterine weight among women undergoing hysterectomy for benign indications in Olmsted County, Minnesota, from 1/1/1999 to 12/31/2013 (n=3,759).
| Uterine Weight (grams)* | N (%) with unexpected sarcoma within each weight stratum | ||
|---|---|---|---|
| LMS | Low-Grade ESS | Total | |
| <250 (N=2993) | 0 | 1 (0.03%) | 1 (0.03%) |
| 250–499 (N=404) | 0 | 0 | |
| 500–999 (N=203) | 0 | 0 | |
| 1000–1499 (N=63) | 2 (3.17%) | 0 | 2 (3.17%) |
| 1500–1999 (N=9) | 0 | 0 | |
| ≥ 2000 (N=13) | 2 (15.38%) | 0 | 2 (15.38%) |
Data available for n=3,685 [98.0% of the total number of benign hysterectomies (n=3,759)
Discussion
The present population-based study showed that the incidence of unexpected sarcomas in Olmsted County among all women undergoing hysterectomy for a benign indication is 0.13% or 1 in 752, which is between the incidences reported by two other large series (range of incidences of 1 in 454 and 1 in 1,124) in Michigan19 and Texas20, respectively. Among women undergoing hysterectomy for uterine fibroids, the incidence of unexpected sarcomas was 0.39% or 1 in 256, which is higher than anticipated based on prior reports14,15. One reason is that indication of “benign uterine fibroids” among post-menopausal women was reported in one of our cases. However, fibroids should not be symptomatic after menopause and thus, women presenting with symptoms should be suspected for possible cancer. If we consider only premenopausal women, our unexpected sarcoma incidence rates are 0.11% (or 1 in 881) and 0.35% (or 1 in 283) among women undergoing hysterectomy for any benign indication and for uterine fibroids, respectively. Importantly, no unexpected sarcoma occurred in women under age 45 years. Moreover, compared to other studies, the higher incidence of unexpected sarcomas among women with indication of uterine fibroids estimated in our study can be related to the lower proportion of hysterectomies for uterine fibroids which represent the denominator, accounting for only 27.3% of the total number of hysterectomies for benign indication. The lower proportion of hysterectomies for uterine fibroid in our study may be due to the large use in Olmsted County of non-surgical treatment of fibroids such as myomectomy, levonorgestrel-releasing intrauterine system, magnetic resonance-guided focused ultrasound, and uterine artery embolization. Of note, none of the women treated for uterine fibroid with conservative management in Olmsted County during the time period of the study were diagnosed with an unexpected sarcoma.
As expected, similar to Brohl et al21 we demonstrated that the risk of unexpected sarcoma increases with age. In particular, the risk of unexpected sarcoma was higher for women ≥ 45 years old compared to women at younger age, with no unexpected sarcoma diagnosed among women <45 years of age. This finding is reassuring for the population of infertile women, in which conservative management of uterine fibroids can be offered at low risk of delaying a diagnosis of sarcoma.
A new finding is the impact of large uteri on sarcoma rates. To our knowledge, this is the first study estimating the incidence of sarcoma by uterine weight. In fact, although previous studies demonstrated that a sarcoma could be present also in the presence of small uteri19,22, none of them reported the total number of uteri in each weight category, precluding any estimate of the incidence of sarcoma by uterine weight. From a practical standpoint, the preoperative prediction of uterine weight can be accurately performed either by a bimanual examination or by ultrasound using the prolate ellipsoid formula23 or its simplified version24 [weight (g) = uterine length × maximum width × anteroposterior diameter × 0.52].
Our study has several strengths. First, by using the medical records linkage system of the REP we were able to study a large population-based cohort that spanned 15 years. This allowed us also to avoid the referral bias of patients referred to a gynecologic oncologist for a suspected sarcoma. Second, since the REP includes all medical facilities in Olmsted County it is unlikely that a patient with sarcoma would have been missed while living in the county. Third, reviewing the pathologic slides to confirm the accuracy of the diagnosis of sarcoma allowed us to differentiate among types of uterine sarcoma and determine an accurate incidence of unexpected sarcoma that without confirmation would have been affected by risk of misclassification of sarcoma due to the changes in the diagnostic criteria for uterine smooth muscle tumor over the last decades26. Fourth, the full medical records of all hysterectomies were manually reviewed by a gynecologist, thus reducing potential bias introduced by differences in the interpretation of the collected variables. This allowed for higher diagnostic accuracy compared with the use of administrative data or to inaccuracy of procedure coding.
The present study also has a number of limitations. First, the low number of sarcomas in our cohort and the resulting lack of statistical power did not allow us to perform further risk-stratification and to identify predictors of unexpected sarcoma. Second, since the majority (>95%) of women resident in Olmsted County are white, the results of our study are not generalizable to populations with different ethnic, social, and economic characteristics; however, results obtained using REP database have generally been consistent with the entire United States population27. Third, in our cohort not all patients with uterine sarcoma underwent preoperative biopsy and imaging, raising concerns on whether these procedures should be always included in the preoperative assessment of women undergoing hysterectomy for benign disease. However, since these procedures have low sensitivity in diagnosis of uterine sarcoma25, they were not routinely used in the preoperative assessment of women undergoing hysterectomy for a benign indication. Preoperative diagnostic techniques continue to improve and routine use will be more common.
Our study has substantial implications for public health. Because there are not reliable markers that allow us to distinguish between uterine fibroids and sarcomas during the preoperative management, the age-specific and uterine weight-specific risks of unexpected sarcomas should be used for preoperative informed consent and counseling of women with presumed uterine fibroids. The risk of unexpected sarcoma should be balanced with the increased risk of surgical complications associated with preventing the use of minimally invasive procedures28. New technologies to allow diagnosis of sarcoma in the preoperative setting and to minimize the risk of dissemination of malignant cells are warranted to preserve the benefits of minimally invasive surgery in the large incidence of women with benign uterine fibroids.
Supplementary Material
AJOG at a Glance example:
A. Why was this study conducted?
To estimate the incidence of sarcoma among women undergoing hysterectomy for benign indication in a population-based cohort.
B. What are the key findings?
The present study shows that the incidence on sarcoma is low among women undergoing hysterectomy for a benign indication (1 in 752 surgeries), but increased in women with presumed uterine fibroids (1 in 256 surgeries). Menopausal status, uterine weight, and age are risk factors for sarcoma.
C. What does this study add to what is already known?
The present study reaffirms that the risk of sarcoma in women with uterine fibroids is not negligible (1 in 256 surgeries). Age-specific and uterine-weights specific risk stratification can be used for preoperative informed consent and counseling of women with presumed uterine fibroids.
Funding/Support:
This publication was made possible by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures: None reported.
References
- 1.Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122(2 Pt 1):233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen SL, Ajao MO, Clark NV, Vitonis AF, Einarsson JI. Outpatient Hysterectomy Volume in the United States. Obstetrics and Gynecology. 2017;130(1):130–137. [DOI] [PubMed] [Google Scholar]
- 3.D’Angelo E, Prat J. Uterine sarcomas: a review. Gynecol Oncol. 2010;116(1):131–139. [DOI] [PubMed] [Google Scholar]
- 4.Hosh M, Antar S, Nazzal A, Warda M, Gibreel A, Refky B. Uterine Sarcoma: Analysis of 13,089 Cases Based on Surveillance, Epidemiology, and End Results Database. International Journal of Gynecological Cancer. 2016;26(6):1098–1104. [DOI] [PubMed] [Google Scholar]
- 5.Stewart EA, Nicholson WK, Bradley L, Borah BJ. The burden of uterine fibroids for African-American women: results of a national survey. J Womens Health (Larchmt). 2013;22(10):807–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. The Cochrane database of systematic reviews. 2009(3):CD003677. [DOI] [PubMed] [Google Scholar]
- 7.George S, Barysauskas C, Serrano C, et al. Retrospective cohort study evaluating the impact of intraperitoneal morcellation on outcomes of localized uterine leiomyosarcoma. Cancer. 2014;120(20):3154–3158. [DOI] [PubMed] [Google Scholar]
- 8.Morice P, Rodriguez A, Rey A, et al. Prognostic value of initial surgical procedure for patients with uterine sarcoma: analysis of 123 patients. European journal of gynaecological oncology. 2003;24(3–4):237–240. [PubMed] [Google Scholar]
- 9.Park JY, Park SK, Kim DY, et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecologic oncology. 2011;122(2):255–259. [DOI] [PubMed] [Google Scholar]
- 10.Seidman MA, Oduyebo T, Muto MG, Crum CP, Nucci MR, Quade BJ. Peritoneal dissemination complicating morcellation of uterine mesenchymal neoplasms. PloS one. 2012;7(11):e50058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bogani G, Cliby WA, Aletti GD. Impact of Morcellation on Survival Outcomes of Patients with Unexpected Uterine Leiomyosarcoma: A systematic review and meta-analysis. Gynecologic oncology. 2014. [DOI] [PubMed] [Google Scholar]
- 12.Rosenbaum L. N-of-1 Policymaking--Tragedy, Trade-offs, and the Demise of Morcellation. N Engl J Med. 2016;374(10):986–990. [DOI] [PubMed] [Google Scholar]
- 13.FDA. UPDATED Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm424443.htm. Nov. 24, 2014.
- 14.FDA. Quantitative Assessment of the Prevalence of Unsuspected Uterine Sarcoma in Women Undergoing Treatment of Uterine Fibroids. April 17, 2014; https://www.fda.gov/downloads/medicaldevices/safety/alertsandnotices/ucm393589.pdf. Accessed September 27, 2017.
- 15.Cui RR, Wright JD. Risk of occult uterine sarcoma in presumed uterine fibroids. Clinical Obstetrics and Gynecology. 2016;59(1):103–118. [DOI] [PubMed] [Google Scholar]
- 16.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ, 3rd. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.St Sauver JL, Grossardt BR, Yawn BP, et al. Data Resource Profile: The Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Plos Med. 2007;4(10):e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahnert N, Morgan D, Campbell D, Johnston C, As-Sanie S. Unexpected gynecologic malignancy diagnosed after hysterectomy performed for benign indications. Obstet Gynecol. 2015;125(2):397–405. [DOI] [PubMed] [Google Scholar]
- 20.Kho KA, Lin K, Hechanova M, Richardson DL. Risk of Occult Uterine Sarcoma in Women Undergoing Hysterectomy for Benign Indications. Obstet Gynecol. 2016;127(3):468–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brohl AS, Li L, Andikyan V, et al. Age-stratified risk of unexpected uterine sarcoma following surgery for presumed benign leiomyoma. Oncologist. 2015;20(4):433–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raine-Bennett T, Tucker LY, Zaritsky E, et al. Occult uterine sarcoma and leiomyosarcoma: Incidence of and survival associated with morcellation. Obstetrics and Gynecology. 2016;127(1):29–39. [DOI] [PubMed] [Google Scholar]
- 23.Kung FT, Chang SY. The relationship between ultrasonic volume and actual weight of pathologic uterus. Gynecol Obstet Inves. 1996;42(1):3538. [DOI] [PubMed] [Google Scholar]
- 24.Harb TS, Adam RA. Predicting uterine weight before hysterectomy: Ultrasound measurements versus clinical assessment. American Journal of Obstetrics & Gynecology. 193(6):2122–2125. [DOI] [PubMed] [Google Scholar]
- 25.Stewart EA. Differentiating uterine leiomyomas (fibroids) from uterine sarcomas. 2018; https://www.uptodate.com/contents/differentiatinguterine-leiomyomas-fibroids-from-uterine-sarcomas?search=unexpectedsarcoma&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2. Accessed October, 7, 2018.
- 26.Giuntoli RL, Gostout BS, DiMarco CS, Metzinger DS, Keeney GL. Diagnostic criteria for uterine smooth muscle tumors - Leiomyoma variants associated with malignant behavior. J Reprod Med. 2007;52(11):10011010. [PubMed] [Google Scholar]
- 27.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Multinu F, Casarin J, Hanson KT, et al. Practice Patterns and Complications of Benign Hysterectomy Following the FDA Statement Warning Against the Use of Power Morcellation. JAMA Surg. 2018:e180141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


