Version Changes
Revised. Amendments from Version 2
The manuscript has been revised and the following changes made to address the comments raised by reviewers accordingly:
Further consultations with the statistician have been made.
Methods section, second paragraph: formula for sample size calculation, the square part that appeared as 2 has been changed to superscript 2
Results section, the first paragraph, specifying the variables, has been moved to the methods section.
Results section, second paragraph: Further clarification has been made on the use of the median as the cut-off between high and low IFAS knowledge ( Arega Sadore et al., 2015). It has been clarified that the null hypothesis referred to here is not about this study but about the statistical test of normality, Shapiro-Wilk W test.
Conclusion: First sentence "...pregnant women had high IFAS..." has been revised to "...pregnant women had high IFAS knowledge…”
We wish to clarify that this was a cross-sectional study, looking at the counselling status and knowledge on iron and folic acid supplementation (IFAS) among pregnant women in Kiambu County. We agree that there was no control group. We wish to clarify that it was not an intervention study and we were not providing counselling services in the study but were simply looking at the counselling status as it were in the health facilities: whereby some of the pregnant women had been counselled on various components of IFAS whereas others had not been counselled at all on various IFAS components. So there was not control group since it was a one-time observation study but some of the pregnant women did not receive any counselling. The fact that some had been counselled while others had not, formed the basis for all our comparisons and associations in this study.
Abstract
Background: The increased demand for iron and folic acid during pregnancy is not met through diet due to insufficiency or reduced bioavailability of nutrients among women from low income countries. Thus, iron and folic acid supplementation (IFAS) is a promising interventional strategy for control of anaemia during pregnancy. Kenya adopted the global IFAS intervention with a target of 80% coverage by 2017, however, the compliance remains low. Increasing awareness, counselling, communication and community education on IFAS have improved compliance among pregnant women. Thus, we aimed to determine: IFAS knowledge, availability, practices, and content of IFAS counselling among pregnant women attending health facilities in Kiambu County, Kenya.
Methods: A cross-sectional study involving 364 pregnant women aged 15-49 years. A two stage cluster sampling, including one sub-county and five public health facilities were used. A pre-tested, structured questionnaire consisting of socio-demographic data, maternal knowledge and counselling on IFAS was used. An observation checklist was used to observe practices and content of antenatal counselling session in each facility. Data was analysed using STATA in which descriptive and inferential statistics were computed.
Results: Of 364 respondents, less than half (40.9%) scored high on knowledge on IFAS. Women who were counselled on duration of IFAS intake, side effects, and their mitigation were more likely (p <0.005) to have high IFAS knowledge. Although all the health facilities had varied IFAS posters displayed, none had key IFAS counselling documents.
Conclusion: Less than half of the pregnant women had high IFAS knowledge, IFAS documents were scarce in health facilities, IFAS counselling information in different health facilities was limited and varied, and content of counselling was associated with levels of knowledge on IFAS. This underscores the need to strengthen focused and targeted IFAS counselling for pregnant women and standardization of counselling messages to improve compliance and pregnancy outcomes.
Keywords: Pregnancy, Iron and folic acid supplementation, Knowledge, Counselling information, Anaemia
Introduction
Nutritional status during conception and pregnancy is a predictor of maternal and infant outcomes 1. Pregnancy increases metabolic activity including demand for macro and micro nutrients, particularly iron and folic acid. The levels of body stores for most critical nutrients, particularly iron and folate, are usually suboptimal by the time of conception among most women in developing countries, thus their requirement is greater resulting in a need for supplementation. This implies that a slight decrease in haemoglobin levels in pregnant women can cause anaemia which can result in severe and often fatal consequences especially if not addressed early 2. The consequences include increased risk of mortality, morbidity, postpartum haemorrhage, and poor birth outcomes, including foetal growth retardation, preterm births and low birthweight 3– 5.
Anaemia in pregnancy is a leading cause of global burden of disease 2 with iron deficiency anaemia being responsible for more than half of the cases. The global prevalence of anaemia in pregnancy ranges from 41.8–43.8% with the greatest (61.3%) burden being found in Africa then South East Asia at 52.5% 6, 7. Africa has the highest prevalence of anaemia among both pregnant and non-pregnant women while Asia has the largest absolute number of women with anaemia, forming 38% of the global total 8. In Kenya, anaemia in pregnancy remains a public health problem, with the prevalence being persistently high, currently at 55.1% 2, 7, 9 resulting in estimated 10% maternal deaths and 20% perinatal deaths 10.
Iron and folic acid supplementation (IFAS) is one of the most affordable and effective global intervention strategy for control of anaemia in pregnancy with resultant benefits of reduced maternal-child morbidity and mortality 10– 12. This is necessitated by the fact that the high body’s nutrient demand in pregnancy is not met by regular diet because of insufficient amounts and/or low bioavailability in diets 5. Following the WHO guidelines 13, Kenya adopted IFAS programme targeting to achieve 80% coverage by 2017 10. Indeed, the IFAS tablets are currently routinely provided through all public health facilities during antenatal care, free of charge for daily use throughout pregnancy. However, the government’s effort to provide IFAS for free notwithstanding, compliance remains low over the years. Reports show that only about 8% pregnant women take IFAS for more than 90 days 14– 17. Studies indicate that poor compliance hinders IFAS success with subsequent poor maternal-child outcomes 12, 18, 19.
Many factors are substantially associated with the non-use of IFAS including: ineffective management, limited funding, stock-outs, maternal age, maternal literacy, spouse literacy, wealth index, frequency of antenatal care (ANC), comprehensive knowledge of anaemia, and quality of counselling on IFAS during pregnancy 20, 21, among others. At the heart of these factors lies lack of demand from health sectors and beneficiaries 22. Studies have shown that increasing awareness on IFAS, appropriate counselling, focused communication and community education among pregnant women improve IFAS compliance 23– 26. Information and training on importance of supplementation during pregnancy is associated with better IFAS utilization 20, 27 in terms of longer duration 28 and increased compliance 29, eventually leading to more effective supplementation 30. There is need to develop appropriate counselling strategies to address this poor compliance.
Counselling is one of the strategies for Social Behaviour Change and Communication (SBCC). Social behaviour change and communication is an evidence based communication style aimed at influencing observable, measurable actions so as to improve the health of individuals and communities 31, 32. The use of Behaviour Change and Communication (BCC) strategies including counselling to improve health outcomes over the years cannot be overemphasized 33. The BCC strategies are particularly effective when designed and implemented locally: tailored to the local context realities and locally accepted, owned and driven 34. In Kenya, various strategies have been integrated to different programmes to develop and disseminate evidence based communication campaigns to influence behaviour change on diverse health issues including communicable diseases control especially HIV/AIDS, child welfare services, non-communicable diseases control, health promotion, various maternal issues and nutrition and supplementation programmes, among many others. For example, Malaria Trac 2014 showed a strong correlation between exposure to Interpersonal Communication and net use behaviour 35.
Counselling applies interpersonal communication at different levels to influence individual and collective behaviours that promote health. These can occur by producing changes in a wide range of behaviours including knowledge, attitudes and social norms, practices and many others 36, 37. For the behaviour change to occur and have these changes fully internalized, clients need to move from the level of information to motivation and then progress to experimenting with behaviour change 38. Thus counselling provides an excellent opportunity for interacting with the client through interpersonal communication to achieve behaviour change.
Various factors affect delivery and uptake of counselling messages, related to either the service-provider, health facility or client. In order to deliver quality counselling for behaviour change, basic counselling skills, communication skills and therapeutic approach are key 39. Service-provider factors include: knowledge, skilfulness, ability to translate conceptual ideas into the local context and interpersonal communication skills, among other counselling skills 40. Health facility factors include infrastructure and equipment, workload, availability of IEC materials and job aids such as counselling cards, flyers, and posters. Client related factors include their perception, accessibility and affordability of the services 41. To ensure that quality counselling is provided and sustained, ongoing training and supervision of service-providers as well as routine assessment of practices and content of counselling messages given is essential.
Previous Kenyan studies have shown limited knowledge about anaemia or the importance of taking IFAS 2, 29, 42, 43. Information on the quality of counselling in association to maternal knowledge on IFAS in Kenya is scarce. Thus, the aim of this study was to: (1) determine maternal knowledge on iron and folic acid supplementation (2) determine availability of IFAS counselling documents in health facilities (3) assess practices and content of IFAS counselling information provided to antenatal women in health facilities and (4) determine the association between content of counselling information and level of maternal knowledge on IFAS.
Methods
This was a cross-sectional study conducted between June and October 2016 involving 364 pregnant women, from Kiambu County, Kenya. Using two stage cluster sampling, one Sub-County (Lari) and five of its major public health facilities (Lari, Githirioini, Kagwe, Kagaa, and Kinale) were selected for the study. The Sub-County was selected on the basis of having existing functional community units (with active community health volunteers in health care activities implying completeness in health care provision at level one of health care service delivery). The study population consisted of all pregnant women who attended antenatal care in the selected health facilities who were: aged 15–49 years, below 33 weeks in their pregnancy gestation, not suffering from any chronic illness and who provided informed consent to participate in the study.
The minimum sample size was 285, as determined using Fisher’s formula (1999) [n = Z2pq/e 2] for a cross-sectional study, using the prevalence of IFAS compliance obtained from Thika hospital, Kiambu County among women attending ANC clinic, where n is the minimum sample score (z = 1.96), p is the presumed prevalence of IFAS compliance (24.5%), q (1-p) is the proportion of non-compliance and e is the margin of error (e = 0.05). A non-response rate of 30% was factored in and added to the minimum sample to make a total sample of 370. The study achieved a sample size of 364 which is 98.5% response rate. A structured interviewer-administered questionnaire ( Supplementary File 1) consisting of 24 closed ended questions including; 11 on socio-demographic data, 9 on maternal knowledge and 4 on counselling content on IFAS, was developed, pre-tested and used for data collection in this study. In addition, an observation checklist ( Data set 2) was used to determine availability of IFAS counselling documents in each health facility as well as counselling practices and content of information covered during an antenatal counselling session. To address any potential bias in data collection, training of four research assistants on research ethics and protocol and quality data collection was done at Kiambu level 5 hospital where the research questionnaires were pretested. To ensure reliability of the questionnaire, a test re-test method was adopted in pre-testing, whereby a repeat pre-test was conducted after two weeks, and Cohen’s kappa statistic was used to measure the level of agreement of the results from the two pre-tests. The questions which were tested and re-tested included: on socio-demographic data: age, education level, occupation, income, gestation, parity and gravidity; on maternal knowledge: benefits of IFAS, frequency of taking IFAS, duration of taking IFAS, possible side effects of IFAS, how to manage the side effects, food sources that increase blood levels, consequences of not getting enough iron/folate, and signs and symptoms of anaemia. All the questions repeated had a kappa value of above 0.7 after comparison thus the questionnaire was considered reliable, hence all the questions were retained. To ensure validity of the questionnaire, it was shared and discussed with experts from the Ministry of Health, division of nutrition, and the study supervisors. The feedback obtained from these experts and pre-testing results was used to refine the tool and improve its quality to ensure the questions were able to test what was intended.
The trained research assistants administered questionnaires to all pregnant women who met the inclusion criteria and consented to participate in the study at the health facilities selected for the study. Filling of the observation checklist was done by the researcher. One counselling session was observed in each health facility. To control for Hawthorne effect, discretion was applied whereby the investigator did not out-rightly inform the nurse that she was being observed but rather objectively recorded details of the counselling session on a notebook then immediately after filled the checklist objectively by stepping out of the antenatal room. The variables of this study were as follows: outcome was maternal knowledge on IFAS; the predictors of maternal IFAS knowledge were: socio-demographic characteristics, practices and content of counselling on IFAS; and availability of counselling documents was an effect modifier.
In regard to analyses, maternal knowledge was computed by summing up all relevant 40 Likert scale items (5 on benefits, 7 on possible side-effects of IFAS, 6 on managing side effects, 6 on effects of iron/folate deficiency, 7 on features of anaemia, 7 on dietary sources that increase blood levels, one item on frequency and one item on duration of IFAS). A correct answer for each item was scored as “1” and “0 for the incorrect response. All the scores for each respondent were summed up to determine the respondents’ level of knowledge. The frequencies of the observation checklist items were entered and data summarized into percentages. A cross tabulation of the data was then carried out against socio-demographic characteristics and content of counselling information offered at health facilities to determine their relationship.
Data from questionnaires was entered into SPSS version 20.0 and exported to STATA version 13.0 then the descriptive and inferential statistics were computed ( Dataset 1 38). Eight of the questionnaires had missing data and were not included in the analysis. Univariate and multivariate binary logistic regression analysis was performed in order to identify the association between maternal IFAS knowledge and content of counselling information. All variables with P<0.05 during the univariate analysis were fitted in the multivariate analysis to identify variables independently associated with maternal IFAS knowledge. A 95% CI with respective odd ratios was used to assess the statistical significance of association among variables. The significance level was set at p <0.05. Descriptive statistics and binomial exact 95% confidence interval (95%CI) of proportions were used for reporting.
Ethical approval of the study protocol was sought and granted by Kenyatta National hospital/University of Nairobi Ethics and Research Committee (KNH-ERC/A/90 protocol number – P706/11/2015). Research permit was obtained from the National Commission for Science, Technology and Innovation (NACOSTI/P/18/81499/2231). Authority to conduct the study was obtained from Kiambu County, Lari Sub-county authorities and health facilities involved. All study participants provided verbal and written informed consent. The minors (below 18 years of age) who agreed to participate in the study provided verbal and signed assent and their parents provided an informed consent on their behalf. The STROBE cross sectional reporting guidelines were used for reporting ( Supplementary File 2) 40.
Results
Socio-demographic characteristics and knowledge on IFAS among respondents
Of the 364 respondents, 67.7% were aged 19–29 years, with the mean age of 25 years. Whereas 37.4% of the respondents had attained upper primary education, only 40.4% had completed secondary education and beyond. A majority (84.1%) of the respondents were married, and had 1–2 children (77.6%). Regarding economic activity, the respondents reported being housewives (27.4%), self-employed (25.1%), casual labourers (22.4%), and on formal employment (2.8%), respectively. Furthermore, only 7.8% of them reported earning more than 100 USD per month.
The distribution of the knowledge scores yielded a mean of 6.24 (SD=3.64) and a median of 6.00. Since the mean was slightly different from the median in this distribution, it shows that the distribution of the knowledge scores was not exactly normal. A further test of normality was done to determine the distribution of maternal knowledge scores using Shapiro-Wilk W test. The results of the test were statistically significant (W=0.961, p<0.001), which showed that the distribution of maternal knowledge scores was not exactly normal (rejecting the null hypothesis that distribution of maternal knowledge scores was normal). Thus, the median was used as the cut-off between high and low IFAS knowledge as in the study by Arega Sadore and colleagues 44. Those who scored above the median value were classified as having high IFAS knowledge, while those who scored below the median value were classified as having low IFAS knowledge 45.
The level of knowledge on IFAS among respondents was varied, with only 40.9% scoring an overall high. About two-thirds (67.3%) of them had heard of IFAS. Among those who scored high for IFAS knowledge, the highest percentage was among those on formal employment (70%) and aged above 40 years (66.7%) ( Table 1).
Table 1. Socio-demographic characteristics and level of knowledge on iron and folic acid supplementation (IFAS) among respondents.
| Socio-demographics
Characteristics |
Level of IFAS
knowledge |
||
|---|---|---|---|
| Overall
n (%) |
Low
n (%) |
High
n (%) |
|
|
Age in years (n=356):
≤ 18 19 – 29 30 – 39 40 – 49 |
28 (7.9) 241 (67.7) 84 (23.6) 3 (0.84) |
23 (82.1) 151 (62.7) 38 (45.2) 1 (33.3) |
5 (17.9) 90 (37.3) 46 (54.8) 2 (66.7) |
|
Marital Status(n=364):
Married Single Widow/Separated/Divorced |
306 (84.1) 54 (14.8) 4 (1.1) |
173 (56.5) 39 (72.2) 3 (75.0) |
133 (43.5) 15 (27.8) 1 (25.0) |
|
Education Level (n=361):
Lower primary Upper primary Secondary incomplete Secondary complete Tertiary |
8 (2.2) 135 (37.4) 72 (19.9) 125 (34.6) 21 (5.8) |
3 (37.5) 86 (63.7) 44 (61.1) 67 (53.6) 12 (57.1) |
5 (62.5) 49 (36.3) 28 (38.9) 58 (46.4) 9 (42.9) |
|
Occupation (n=362):
Formal employment Self-employed Casual labourer Housewife Students Unemployed Farming |
10 (2.8) 91 (25.1) 81 (22.4) 99 (27.4) 11 (3.0) 55 (15.2) 15 (4.1) |
3 (30.0) 51 (56.0) 54 (66.7) 53 (53.5) 9 (81.8) 36 (65.5) 7 (46.7) |
7 (70.0) 40 (44.0) 27 (33.3) 46 (46.5) 2 (18.2) 19 (34.6) 8 (53.3) |
|
Number of children (n=237):
1 – 2 3 – 4 5+ |
184 (77.6) 46 (19.4) 7 (3.0) |
101 (54.9) 23 (50.0) 3 (42.9) |
83 (45.1) 23 (50.0) 4 (57.1) |
|
Average income (n=351):
≤ 10,000 Above 10,000 |
325 (92.6) 26 (7.4) |
199 (61.2) 10 (38.5) |
126 (38.8) 16 (61.5) |
| Overall maternal IFAS knowledge | 364 (100) | 215 (59.1) | 149(40.9) |
Availability of IFAS counselling documents at the health facilities
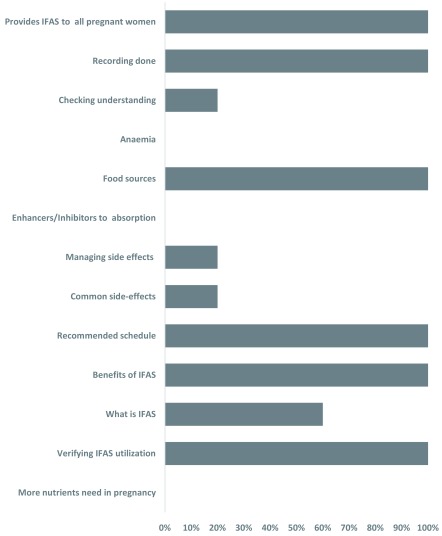
All health facilities displayed diverse posters with information about IFAS at different service delivery points. Among the five facilities, only two displayed the IFAS national policy guidelines, while none had IFAS information, communication and education (IEC) materials, including health workers’ counselling guides, mothers’ calendars or brochures/leaflets on IFAS, among others ( Figure 1 and Dataset 2 38).
Figure 1. Observed counselling practices and content of counselling information provided.
These are the counselling practices and content of counselling information provided to pregnant women by health care providers, as observed during an antenatal counselling session at each health facility, by the researcher.
Observed counselling practices and content of information on IFAS at health facilities
A provider-client interaction observed during an antenatal counselling session in each health facility revealed that health care providers provided IFAS services to all pregnant women without discrimination, regardless of their haemoglobin levels. Verification of IFAS utilization and recording of IFAS services was done in all the health facilities. However, evaluation on the comprehension of the counselling content provided to clients only took place in one facility. Furthermore, counselling women on side-effects of IFAS and their management was only done in one facility. Despite the universal provision of IFAS to all antenatal women, they were not given information on the causes, features or consequences of anaemia in any of the health facilities. Moreover, the counselling did not include; the enhancers/inhibitors of iron/folate absorption, and the fact that there is increased nutritional requirement during pregnancy, in any of the health facilities ( Figure 1 and Dataset 2 38).
Relationship between IFAS counselling content and maternal knowledge on IFAS
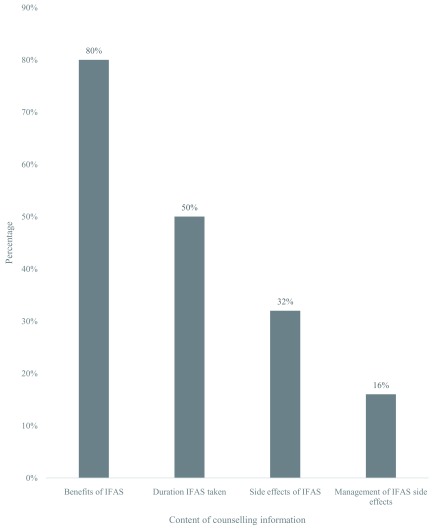
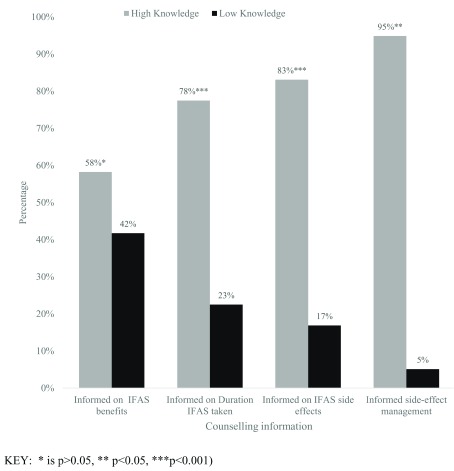
The proportion of pregnant women provided with counselling information on various aspects of IFAS is shown in Figure 2. While most (80%) of the women were informed of the benefits of IFAS, half (50%) were informed on supplementation duration, a third (32%) on side-effects and only 16% on management of side-effects. The content of IFAS counselling was associated with the level of maternal IFAS knowledge. Among the respondents who received information on the benefits of IFAS, only 58.2% scored high for IFAS knowledge. However, those counselled on the side effects and the duration of IFAS supplementation demonstrated high knowledge scores of 83.1% and 77.5%, respectively. In addition, respondents who received information on the management of IFAS side effects demonstrated the highest (95%) knowledge score ( Figure 3).
Figure 2. Content of counselling information provided on iron and folic acid supplementation (IFAS).
This refers to the proportion of pregnant women counselled on various aspects of the content of IFAS counselling information, according to the women’s interviews.
Figure 3. Relationship between counselling information and level of iron and folic acid supplementation (IFAS) knowledge.
The proportion of pregnant women provided with IFAS counselling information on: benefits, supplementation duration, side-effects and management of side-effects were tabulated against the level of IFAS knowledge. For each content of counselling information provided, the level of IFAS knowledge was scored and categorized as high and low, both adding up to the total 100% of the respondents who were counselled on each specific content of counselling information.
Further analysis with multivariate logistic regression revealed that counselling on the duration of IFAS supplementation, its side effects and their management were the predictors of maternal IFAS knowledge. Respondents counselled on the duration of IFAS supplementation were 6.3 times more likely (AOR=6.27; 95%CI, 3.24 – 12.16; P<0.001) to have high knowledge scores. Furthermore, counselling information on IFAS that included side effects was more likely (AOR=4.5; 95%CI, 2.01 – 10.07; P<0.001) to contribute to high knowledge scores among the respondents. The respondents who were counselled on management of IFAS side-effects were 10.3 times more likely (AOR=10.31; 95%CI, 2.10 – 50.59, P=0.004) to have high knowledge scores compared to those who were not counselled. However, respondents who were counselled on the benefits of IFAS, did not show any statistical (AOR=1.48; 95%CI, 0.63 – 3.51, P=0.368) difference on the knowledge score compared to those not counselled ( Figure 3).
Discussion
The objectives of this study were to assess maternal knowledge on iron and folic acid supplementation, availability of IFAS counselling documents in health facilities, practices and content of IFAS counselling information provided to pregnant women in health facilities and determine the association between content of counselling information and level of maternal knowledge on IFAS. The study was based at the antenatal clinic where IFAS services are provided. Health care providers, specifically nurses, working in those antenatal clinics are expected to provide IFAS counselling information together with the supplements as part of Focused Antenatal Care (FANC) to all pregnant women attending antenatal care in all public health facilities in Kenya. The Ministry of Health, through the Division of Nutrition, where micronutrient deficiency control and supplementation programmes fall, is supposed to facilitate quality counselling on IFAS by providing the appropriate job aids including IEC materials and counselling guides on IFAS.
The findings of the study showed: (i) less than 50% of the pregnant women had high IFAS knowledge level; (ii) apart from IFAS posters, other counselling guides were scarcely available in the health facilities; (iii) limited IFAS counselling information was provided to pregnant women who attended antenatal care even though they were all provided with IFAS supplements in all health facilities (iv) the content of counselling varied in different health facilities and was associated with the level of IFAS knowledge. This underscores the need to strengthen implementation of counselling for the pregnant women regarding nutrition and its importance on pregnancy outcome. Health care providers (HCPs) should be supported by the health systems to escalate counselling of pregnant women every time they meet them.
The findings reveal that less than half of the pregnant women had high IFAS knowledge level despite about two-thirds (67.3%) having heard of IFAS. This is probably associated with the lack of individualized message sharing and counselling of pregnant women on IFAS by the HCPs. In addition, emphasis on the critical role IFAS plays in pregnancy may be lacking, including support for the women with tools such as brochures. This reveals that many pregnant women do not have the details about IFAS. This could also mean that we have a huge number of women who are either ignorant of IFAS or who do not know about the supplements given to pregnant women. This is evidenced by observation performed during the counselling session where the nurse informed the mother the purpose of the supplement but not its name. Similar findings have been reported with folic acid knowledge studies in Pakistan (43%) 46 and the United Arab Emirates where, even though 79.1% had heard of folic acid, 46.6% had accurate knowledge on role of folic acid 47. This calls for more appropriate strategies to give mothers detailed IFAS information of why, when and how, beginning with actual names, importance, supplementation duration, maintaining supplementation, side-effects/challenges, and more importantly how to handle these side-effects/challenges, to increase maternal knowledge on IFAS and its compliance. Generally, high IFAS knowledge has been associated with better IFAS compliance 20. Hence, the need to constantly seek to improve counselling approaches so as to improve maternal knowledge on IFAS.
Scarcity of IFAS counselling documents was observed in health facilities. Though IFAS counselling was provided in all facilities and varied IFAS posters displayed at different service points, the national policy guidelines were available in only two out of the five health facilities, while health workers’ counselling guides, IFAS calendars and brochures/leaflets were not available in any of the health facilities. This paucity of IFAS counselling documents in health facilities may have led to non-standardized counselling between health facilities as well as incomplete and ineffective counselling for pregnant women. This is evidenced by the findings of the counselling session observed where it was only in one health facility that the nurse provided counselling information on IFAS side-effects and their management, and evaluated comprehension of counselling content offered to the client. Research indicates that health education plays a key role in determining uptake of health interventions 48, 49. However, their effectiveness is hampered by lack of relevant guides and job aids. Health workers need to be provided with requisite skills, especially counselling and interpersonal skills, and job aids to provide effective health education to clients 50. These include policy and counselling guides to ensure standardized health messages 48. As part of health education, materials for clients to take home should also be provided for their references. These guides should be regularly updated and availed on time for them to be useful. Subsequently, ensuring HCPs have the right tools on what to communicate to clients will enhance effective communication which is one of the key counselling skills essential for behaviour change including knowledge and practice.
Limited IFAS counselling information was provided to the pregnant women who attended antenatal care but they were all provided with IFAS supplements in all the health facilities. The content of counselling varied in different health facilities. Despite the universal provision of IFAS to all antenatal women, they were not counselled on the causes, features or consequences of anaemia. Moreover, counselling information on; the enhancers/inhibitors of iron/folate absorption, and the fact that there is increased nutritional requirement during pregnancy, was not provided in any of the health facilities. This is consistent with research reports that a great percentage of maternal anaemia occurs due to insufficient intake of bioavailable dietary iron particularly in developing countries 51, 52. It is therefore very important to ensure proper choices of food that promote iron and folate absorption among pregnant women by providing effective counselling and information on the food interactions and practices. This non-standardized counselling in health facilities resulting from lack of counselling guides may in turn have contributed to low level of IFAS knowledge and compliance as found in studies among respondents whose primary source of information was health care providers 21, 30, 53, 54. Accompanying communication with supplementation greatly improved compliance and decreased anaemia prevalence among adolescents in Tanzania 26. Research findings have reported limited knowledge/lack of information among health care providers in many aspects of education and counselling in Kenya as a set-back that adversely affects IFAS utilization 9 and needs to be addressed. This calls for standardization of IFAS counselling messages provided to pregnant women.
The content of counselling differed in the health facilities as discussed above and was associated with the level of IFAS knowledge. As far as content of IFAS counselling in relation to maternal knowledge is concerned, except those informed on benefits, all the other counselling aspects showed a very high difference among those who had low and high IFAS knowledge. Research indicates that experiencing side-effects is one of the reasons for low IFAS compliance 20. As most women stop taking iron-folate tablets due to side effects, it is important that pregnant women are effectively counselled and provided with accurate, detailed information on the side-effects and how to effectively manage them to ensure adherence to IFAS 6, 20, 50. Lack of counselling on the side-effects could be due to either lack of information by HCPs or their wrong attitude. While some HCPs may imagine that by mentioning side-effects of IFAS, pregnant women will not take the supplements, on the contrary, detailed counselling on the same yielded higher levels of knowledge. If women are counselled on the expected side-effects and their management and reassured they will subside with time, they are less likely to react negatively to side-effects. This was evidenced in an Indonesia study where women were not bothered by side-effects because they had been warned of their likely occurrence 55. This contrasts many studies that have shown side-effects as a major hindrance to IFAS compliance. Realistically, it seems like the actual problem is the quality of counselling as indicated in other studies 50, 56. Thus, it is important that HCPs should be well informed to enable them provide women with relevant information and conduct effective, quality counselling on IFAS to ensure compliance 20. This can be implemented by formally involving community health workers more in the IFAS programme for closer follow-up and counselling of the pregnant women at community level, as demonstrated in other studies 55.
This study had several limitations. The assessment of counselling and knowledge levels was done at one point in time by asking pregnant women whether they were counselled or not and the content of the counselling. Only one counselling session was observed in each health facility. This is a limitation of cross-sectional designs. In addition, this study relied heavily on verbal reports on IFAS, which may have introduced some recall bias and subjectivity. However, this challenge was circumvented through proper training of interviewers and double questioning that enabled identification of any inconsistencies in the reports. The study involved pregnant women who are under high hormonal influence leading to mood changes as well as pregnancy associated fatigue which may affect response and consistency. This was mitigated through message sharing, clarification, reassurance and psychosocial support of the respondents. Furthermore, participation in the study was purely voluntary and respondents were asked whether they were comfortable answering the questions and they were at liberty to discontinue. This ensured that their rights were respected and was in compliance with the ethical requirement of non-coercion. Finally, although important associations between counselling and knowledge levels are demonstrated in this study, this was a cross-sectional descriptive study whose results cannot be used to make causal inferences. Also, generalizations of the study findings to other areas may be difficult since the study involved one sub-county.
Conclusion
Findings from this study indicate that less than half of the pregnant women had high IFAS knowledge, IFAS documents were scarce in health facilities, there was limited and varied IFAS counselling information in different health facilities and content of counselling was associated with levels of knowledge on IFAS among pregnant women. Counselling information on the duration of IFAS supplementation, IFAS side effects and their management were significantly associated with high levels of knowledge on IFAS among pregnant women. This underscores the need to strengthen focused and targeted counselling for women attending antenatal clinic to improve compliance and pregnancy outcomes. The researchers recommend provision of IFAS documents and IEC materials to peripheral health facilities, standardization of counselling content provided on IFAS and formal involvement of community health workers in the IFAS programme for closer follow-up and counselling of the pregnant women at community level. Further, intervention studies are recommended that allow for causal inferences.
Consent
Verbal and written informed consent was provided by all the study participants before recruitment into the study.
Data availability
The data underlying this study is available from Open Science Framework Dataset 1: Knowledge and counselling, Dataset 2: Observation checklist-counselling. DOI https://doi.org/10.17605/osf.io/x8tj3 33. This dataset is available under a CCO 1.0 Universal license
Dataset 1. Counselling information and knowledge on iron and folic acid supplementation (IFAS)This is the data set used for analysis using STATA version 13. It contains the information on socio-demographic information of study respondents, IFAS knowledge and counselling information, as per the attached questionnaire ( Supplementary File 1).
Dataset 2. Observation checklist: counselling practices and content of informationThis data set contains a table showing the counselling practices and content of counselling information, as observed during an antenatal counselling session, as well as available iron and folic acid supplementation (IFAS) counselling documents in each health facility.
Acknowledgements
Our gratitude to all study participants in Lari Sub-County for their time and willingness to share their experiences. We thank the Sub-County management team for their support especially by the Public Health Officer in-charge of the community health strategy. We are grateful for the dedicated performance of the field and data management staff.
Funding Statement
This research was supported by African Academy of Sciences (AAS) through a Consortium for Advanced Research Training in Africa (CARTA) grant as part of the DELTAS Africa initiative [107768/Z/15/Z]. The DELTAS Africa Initiative is an independent funding scheme of the AAS’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust (UK) [107768/Z/15/Z] and the UK government. CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Carnegie Corporation of New York [B 8606.R02], Sida [54100029], the DELTAS Africa Initiative [107768/Z/15/Z]. "The statements made and views expressed are solely the responsibility of the fellow”.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 3; peer review: 2 approved, 1 approved with reservations]
Supplementary material
Supplementary File 1: Study questionnaire.
Supplementary File 2: Completed STROBE reporting checklist.
Supplementary File 3: Author responses and the changes made in this version following the reviewers’ comments.
References
- 1. Gunaratna NS, Masanja H, Mrema S, et al. : Multivitamin and iron supplementation to prevent periconceptional anemia in rural tanzanian women: a randomized, controlled trial. PLoS One. 2015;10(4):e0121552. 10.1371/journal.pone.0121552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mulambah CS, Siamba DN, Ogutu PA, et al. : Anaemia in pregnancy: Prevalence and possible risk factors in Kakamega County, Kenya. Sci J Public Health. 2014;2(3):216–222. 10.11648/j.sjph.20140203.23 [DOI] [Google Scholar]
- 3. Mohajan HK: Food and Nutrition Scenario of Kenya. American Journal of Food and Nutrition. 2014;2(2):28–38. Reference Source [Google Scholar]
- 4. MoH: IFAS Dialogue guide for health care providers. Division of Nutrition ed. Nairobi;2012. Reference Source [Google Scholar]
- 5. Elder LK: Issues in programming for maternal anaemia. Mother Care. 2000. [Google Scholar]
- 6. Bilimale A, Anjum J, Sangolli HN, et al. : Improving adherence to oral iron supplementation during pregnancy. Australas Med J. 2010;3(5):281–290. 10.4066/AMJ.2010.291 [DOI] [Google Scholar]
- 7. Waweru J, Mugenda OM, Kuria E: Anaemia in the context of pregnancy and HIV/AIDS: a case of Pumwani maternity hopital in Nairobi Kenya. Afr J Food Agric Nutr Dev. 2009;9:748–763. 10.4314/ajfand.v9i2.19226 [DOI] [Google Scholar]
- 8. USAID: SPRING NUTRITION TECHNICAL BRIEF: A simple method for making a rapid, initial assessment of the consumption and distribution of iron-folic acid supplements among pregnant women in developing countries.2014. Reference Source [Google Scholar]
- 9. MoH: National Iron and Folic Acid Supplementation; Communication Strategy, 2013-2017. Division of Nutrition ed. Nairobi;2013. Reference Source [Google Scholar]
- 10. MoH: National Policy Guideline on combined iron and folic acid (IFA) supplementation for pregnant mothers in Kenya. Division of Nutrition ed. Nairobi;2013. Reference Source [Google Scholar]
- 11. MoH: Accelerating reduction of iron deficiency anaemia among pregnant women in Kenya: Plan of action 2012-2017.Division of Nutrition ed. Nairobi;2012. Reference Source [Google Scholar]
- 12. Müngen E: Iron supplementation in pregnancy. J Perinat Med. 2003;31(5):420–426. 10.1515/JPM.2003.065 [DOI] [PubMed] [Google Scholar]
- 13. WHO: Guideline: Daily Iron and Folic Acid Supplementation in Pregnant Women.Geneva: World Health Organization,2012. [PubMed] [Google Scholar]
- 14. MoPHS: Kenya nutrition bulletin. Division of Nutrition ed., Nairobi;2012;2 Reference Source [Google Scholar]
- 15. MoPHS: National Nutrition Action Plan 2012-2017.Division of Nutrition ed. Nairobi;2012. Reference Source [Google Scholar]
- 16. KNBS, Macro ICF: Kenya Demographic and Health Survey (KDHS) 2008-09.Nairobi: Kenya National Bureau of Statistics;2010. Reference Source [Google Scholar]
- 17. KNBS, Macro ICF: Kenya Demographic and Health Survey 2014.Nairobi: Kenya National Bureau of Statistics;2015. Reference Source [Google Scholar]
- 18. Pena-Rosas JP, Viteri FE: Effects of routine oral iron supplementation with or without folic acid for women during pregnancy. Cochrane Database Syst Rev. 2006; (3):CD004736. 10.1002/14651858.CD004736.pub2 [DOI] [PubMed] [Google Scholar]
- 19. Yip R: Iron deficiency: contemporary scientific issues and international programmatic approaches. J Nutr. 1994;124(8 Suppl):1479S–1490S. 10.1093/jn/124.suppl_8.1479S [DOI] [PubMed] [Google Scholar]
- 20. Gebremedhin S, Samuel A, Mamo G, et al. : Coverage, compliance and factors associated with utilization of iron supplementation during pregnancy in eight rural districts of Ethiopia: a cross-sectional study. BMC Public Health. 2014;14:607. 10.1186/1471-2458-14-607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nisar YB, Dibley MJ, Mir AM: Factors associated with non-use of antenatal iron and folic acid supplements among Pakistani women: a cross sectional household survey. BMC Pregnancy Childbirth. 2014;14(1):305. 10.1186/1471-2393-14-305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. MCSP: MCSP Nutrition Brief. Community-Based Distribution of Iron-Folic Acid Supplementation: Evidence and Program Implications. MCSP;2017. Reference Source [Google Scholar]
- 23. Popa AD, Niţă O, Graur Arhire LI, et al. : Nutritional knowledge as a determinant of vitamin and mineral supplementation during pregnancy. BMC Public Health. 2013;13:1105. 10.1186/1471-2458-13-1105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ghanekar J, Kanani S, Patel S: Toward better compliance with iron-folic acid supplements: understanding the behavior of poor urban pregnant women through ethnographic decision models in Vadodara, India. Food Nutr Bull. 2002;23(1):65–72. 10.1177/156482650202300109 [DOI] [PubMed] [Google Scholar]
- 25. Wendt A, Young M, Stephenson R, et al. : Antenatal care and counseling measures increase iron and folic acid receipt among pregnant women in Bihar, India (256.3). FASEB J. 2014;28(1_supplement). Reference Source [Google Scholar]
- 26. Muro GS, Gross U, Gross R, et al. : Increase in compliance with weekly iron supplementation of adolescent girls by an accompanying communication programme in secondary schools in Dar-es-Salaam, Tanzania. Food Nutr Bull. 1999;20(4):435–444. 10.1177/156482659902000408 [DOI] [Google Scholar]
- 27. Pal PP, Sharma S, Sarkar TK, et al. : Iron and Folic Acid Consumption by the Ante-natal Mothers in a Rural Area of India in 2010. Int J Prev Med. 2013;4(10):1213–1216. [PMC free article] [PubMed] [Google Scholar]
- 28. Yekta Z, Ayatollahi H, Pourali R, et al. : Predicting Factors in Iron Supplement Intake among Pregnant Women in Urban Care Setting. J Res Health Sci. 2008;8(1):39–45. [PubMed] [Google Scholar]
- 29. Maina-Gathigi L, Omolo J, Wanzala P, et al. : Utilization of folic acid and iron supplementation services by pregnant women attending an antenatal clinic at a regional referral hospital in Kenya. Matern Child Health J. 2013;17(7):1236–1242. 10.1007/s10995-012-1120-x [DOI] [PubMed] [Google Scholar]
- 30. Aguayo VM, Koné D, Bamba SI, et al. : Acceptability of multiple micronutrient supplements by pregnant and lactating women in Mali. Public Health Nutr. 2005;8(1):33–37. 10.1079/PHN2004665 [DOI] [PubMed] [Google Scholar]
- 31. Gathigi LN: Factors Influencing Utilization of Iron and Folic Acid Supplementation Services among Women Attending Antenatal Clinic at Nyeri Provincial Hospital Kenya. Jomo Kenyatta University of Agriculture and Technology, ITROMID;2011. Reference Source [Google Scholar]
- 32. Juma M, Oiye SO, Konyole SO: Predictors of optimum antenatal iron-folate supplementation in a low resource rural set-up in Eastern Kenya. J Public Health Epidemiol. 2015;7(11):337–345. 10.5897/JPHE2015.0770 [DOI] [Google Scholar]
- 33. Kamau M: Iron and folic acid supplementation among pregnant women.2018. 10.17605/osf.io/x8tj3 [DOI] [Google Scholar]
- 34. von Elm E, Altman DG, Egger M, et al. : Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. PSI: Kenya Health Behaviour Change Initiatives: Communication Initiatives Experiences from Kenya. Nairobi;2014. Reference Source [Google Scholar]
- 36. Noar SM, Palmgreen P, Chabot M, et al. : A 10-year systematic review of HIV/AIDS mass communication campaigns: Have we made progress? J Health Commun. 2009;14(1):15–42. 10.1080/10810730802592239 [DOI] [PubMed] [Google Scholar]
- 37. Nguyen TS, Nguyen TLH, Pham TTV, et al. : Effectiveness of a short training program for community pharmacists to improve knowledge and practice of asthma counselling - A simulated patient study. Respir Med. 2018;144:50–60. 10.1016/j.rmed.2018.10.003 [DOI] [PubMed] [Google Scholar]
- 38. Elmendorf AE, Cabañero-Verzosa C, Lioy M, et al. : Behavior Change Communication for Better Health Outcomes in Africa: Experience and Lessons Learned from World Bank Financed Health, Nutrition and Population Projects. (Region HDSA ed.: The World Bank;2005. Reference Source [Google Scholar]
- 39. Dewing S, Mathews C, Cloete A, et al. : Lay counselors' ability to deliver counseling for behavior change. J Consult Clin Psychol. 2014;82(1):19–29. 10.1037/a0034659 [DOI] [PubMed] [Google Scholar]
- 40. Lettenmaier C, Kraft JM, Raisanen K, et al. : HIV communication capacity strengthening: a critical review. J Acquir Immune Defic Syndr. 2014;66 Suppl 3:S300–S305. [DOI] [PubMed] [Google Scholar]
- 41. Agbozo F: Qualitative assessment of counselling on infant and young child feeding provided by community health workers to caregivers at child welfare clinics in Ghana. Int J Commun Health. 2016;9:97–108. Reference Source [Google Scholar]
- 42. Cooper C: A Guide for Planning and Implementing Social and Behavior Change Communication Activities for Postpartum Family Planning. (Program TMaCHI ed. Baltimore, Maryland 21231-3492, USA: Jhpiego;2014. Reference Source [Google Scholar]
- 43. Thomas T, Passfield L, Coulton S, et al. : Effectiveness of a tailored training programme in behaviour change counselling for community pharmacists: A pilot study. Patient Educ Couns. 2016;99(1):132–138. 10.1016/j.pec.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 44. Arega Sadore A, Abebe Gebretsadik L, Aman Hussen M: Compliance with Iron-Folate Supplement and Associated Factors among Antenatal Care Attendant Mothers in Misha District, South Ethiopia: Community Based Cross-Sectional Study. J Environ Public Health. 2015;2015:781973. 10.1155/2015/781973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kamau MW, Mirie W, Kimani S: Compliance with Iron and folic acid supplementation (IFAS) and associated factors among pregnant women: results from a cross-sectional study in Kiambu County, Kenya. BMC Public Health. 2018;18(1):580. 10.1186/s12889-018-5437-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hisam A, Rahman MU, Mashhadi SF: Knowledge, attitude and practice regarding folic acid deficiency; A hidden hunger. Pak J Med Sci. 2014;30(3):583–588. 10.12669/pjms.303.4716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Al-Hossani H, Abouzeid H, Salah MM, et al. : Knowledge and practices of pregnant women about folic acid in pregnancy in Abu Dhabi, United Arab Emirates. East Mediterr Health J. 2010;16(4):402–407. 10.26719/2010.16.4.402 [DOI] [PubMed] [Google Scholar]
- 48. Alam A, Rasheed S, Khan NU, et al. : How can formative research inform the design of an iron-folic acid supplementation intervention starting in first trimester of pregnancy in Bangladesh? BMC Public Health. 2015;15:374. 10.1186/s12889-015-1697-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Matiri E, Pied E, Galloway R, et al. : Improving Iron-Folic Acid and Calcium Supplementation Compliance through Counseling, Reminder Cards, and Cell Phone Messages in Kenya. Maternal and Child Health Integrated Program (MCHIP);2017. Reference Source [Google Scholar]
- 50. Nisar YB, Alam A, Aurangzeb B, et al. : Perceptions of antenatal iron-folic acid supplements in urban and rural Pakistan: a qualitative study. BMC Pregnancy Childbirth. 2014;14:344. 10.1186/1471-2393-14-344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pasricha SR, Drakesmith H, Black J, et al. : Control of iron deficiency anemia in low- and middle-income countries. Blood. 2013;121(14):2607–2617. 10.1182/blood-2012-09-453522 [DOI] [PubMed] [Google Scholar]
- 52. Milman N: Oral iron prophylaxis in pregnancy: not too little and not too much! J Pregnancy. 2012;2012: 514345. 10.1155/2012/514345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Fiedler J, D'Agostino A, Sununtnasuk C: A rapid initial assessment of the distribution and consumption of iron–folic acid tablets through antenatal care in Nepal. Arlington, Virginia, JSI Research and Training Institute, Strengthening Partnerships, Results and Innovations in Nutrition Globally [SPRING],2014;12 Reference Source [Google Scholar]
- 54. Taye B, Abeje G, Mekonen A: Factors associated with compliance of prenatal iron folate supplementation among women in Mecha district, Western Amhara: a cross-sectional study. Pan Afr Med J. 2015;20:43. 10.11604/pamj.2015.20.43.4894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Shivalli S, Srivastava RK, Singh GP: Trials of Improved Practices (TIPs) to Enhance the Dietary and Iron-Folate Intake during Pregnancy- A Quasi Experimental Study among Rural Pregnant Women of Varanasi, India. PLoS One. 2015;10(9):e0137735. 10.1371/journal.pone.0137735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Titaley CR, Dibley MJ: Factors associated with not using antenatal iron/folic acid supplements in Indonesia: the 2002/2003 and 2007 Indonesia Demographic and Health Survey. Asia Pac J Clin Nutr. 2015;24(1):162–76. 10.6133/apjcn.2015.24.1.10 [DOI] [PubMed] [Google Scholar]