Abstract
Recent terrorist and epidemic events have underscored the potential for disasters to generate large numbers of casualties. Few surplus resources to accommodate these casualties exist in our current health care system. Plans for “surge capacity” must thus be made to accommodate a large number of patients. Surge planning should allow activation of multiple levels of capacity from the health care facility level to the federal level. Plans should be scalable and flexible to cope with the many types and varied timelines of disasters. Incident management systems and cooperative planning processes will facilitate maximal use of available resources. However, resource limitations may require implementation of triage strategies. Facility-based or “surge in place” solutions maximize health care facility capacity for patients during a disaster. When these resources are exceeded, community-based solutions, including the establishment of off-site hospital facilities, may be implemented. Selection criteria, logistics, and staffing of off-site care facilities is complex, and sample solutions from the United States, including use of local convention centers, prepackaged trailers, and state mental health and detention facilities, are reviewed. Proper pre-event planning and mechanisms for resource coordination are critical to the success of a response.
1. Introduction
The terrorist attacks of 2001 and the threat of large-scale infectious disease outbreaks such as severe acute respiratory syndrome and pandemic influenza have revealed potentially large gaps in the ability of the health care system to find either the capacity or the special capabilities to cope with disasters that severely injure or infect a large number of victims.1., 2. Although much current planning revolves around large-scale terrorist or epidemic events, the recent Rhode Island nightclub fire demonstrates that even a moderate-sized incident may generate large numbers of victims whose care requires supplemental staff and specialized resources and overwhelms local capabilities.3 There is an urgent need for communities and regions, not just individual health care facilities, to develop tiered, scalable, and flexible surge capacity plans to provide care for a large volume of patients. These plans must reflect local hazards and other variables (eg, climate, travel and tourism patterns, population).
Surge capacity is not a new concept, as auxiliary hospitals have been used in smallpox and pandemic influenza events,4 and field hospitals are a core component of military casualty care. However, the challenges of planning are many in the face of frequent emergency department (ED) crowding5 and a loss of 38,000 hospital beds (4.4%) nationwide between 1996 and 2000,6 including a 20% decrease in ICU capacity between 1995 and 2001.7
This article reviews options for patient care surge capacity for hospital patients. These strategies do not exist in isolation but must be part of a comprehensive public health and emergency management plan for outpatient and inpatient care. In addition to the resources available to the authors, a MEDLINE search was conducted to identify articles of interest using search terms “surge capacity,” “disasters + hospital,” “disaster planning + hospital,” “field hospital,” and “surge + disasters” since 1966. Articles that seemed primarily related to surge capacity were reviewed and hand-searched for additional references.
2. Definitions
There are 3 broad areas in which an augmented or “surge” response may be required during a disaster. “Public health surge capacity” refers to the overall ability of the public health system to manage a large incident by increased capacity for patient care and for multiple other patient- and population-based activities (Table 1 ). “Health care facility–based” and “community-based patient care surge capacity” relate to making available adequate resources for the delivery of acute medical care to large numbers of patients (Table 1). “Surge capability,” by contrast, refers to more specialized resources for specific patient groups (eg, burns; Table 1).8
Table 1.
Definitions.
| Term | Definition |
|---|---|
| Surge capacity | Ability to manage a sudden, unexpected increase in patient volume (ie, numbers of patients) that would otherwise severely challenge or exceed the current capacity of the health care system |
| Surge capability | Ability of the health care system to manage patients who require specialized evaluation or interventions (eg, contaminated, highly contagious, or burn patients) |
| Public health surge capacity | Ability of the public health system to increase capacity not only for patient care but also for epidemiologic investigation, risk communication, mass prophylaxis or vaccination, mass fatality management, mental health support, laboratory services, and other activities |
| Facility-based surge capacity | Actions taken at the health care facility level that augment services within the response structure of the health care facility; may include responses that are external to the actual structure of the facility but are proximate to it (eg, medical care provided in tenting on the hospital grounds). These responses are under the control of the facility's incident management system and primarily depend on the facility's emergency operations plans. |
| Community-based surge capacity | Actions taken at a community level to supplement health care facility responses. These may provide for triage and initial treatment, nonambulatory care overflow, or isolation (eg, off-site “hospital” facility). These responses are under the control of the jurisdictional response (eg, public health, emergency management) and represent a public effort to support and augment the health care system. |
These terms refer not only to the physical space but also the organizational structure, medical and ancillary staff, support (eg, nutrition, mental health), supply, information systems, pharmaceuticals, and other resources required to support public health and patient care efforts.
3. Incident management
Surge capacity planning must address static and dynamic events throughout a variety of timelines requiring different types of resources.9 For example, a large-scale airborne anthrax attack will rapidly overwhelm intensive care resources such as ventilators. A smallpox outbreak may develop more slowly and place longer-term demands on hospitals, isolation facilities, and the workforce. Effective planning thus requires comprehensive resource coordination and control to allow for a flexible response.
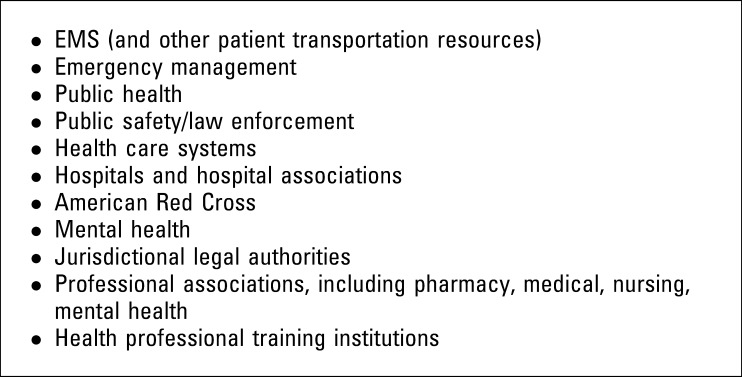
From the local health care facility to the state and federal level, surge capacity decisionmaking must take place within an incident management system that involves key stakeholders (Figure 1 ). An example of a functional health incident management system is the Medical and Health Incident Management System.10 This system provides a framework for all facets of a jurisdictional or multijurisdictional health response to a disaster, including public health initiatives, patient care delivery, and epidemiologic response.
Figure 1.
Key community and regional stakeholders.
Internally, health care facilities accredited by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) are required to use an incident management system11 (eg, the Hospital Emergency Incident Command System)12 that integrates with that of the community.
Response to a large-scale disaster may be improved when health care facilities and other stakeholder groups agree on a mechanism for their needs and resources to be represented at the jurisdictional or regional level (eg, area hospitals designate a single “clearinghouse” hospital to coordinate resources and response). Roles and responsibilities of each stakeholder group must be understood and documented before an event occurs.
One of the most difficult aspects of managing a public health incident is that health care systems are usually private rather than public enterprises. They have no jurisdictional boundaries and are not under any governmental or municipal operational authority or control. Because of their regulatory and policy authority, departments of public health are expected to assume responsibility for coordination of disaster medical care, but often expertise in clinical care and daily involvement with health care systems is minimal. Close cooperation of health care facilities with public health, especially in pre-event planning, is thus of paramount importance to any large-scale disaster patient care response.
4. Health care facility–based surge capacity
The initial facility-based “surge in place” response (Table 1) occurs on notification of a multiple-casualty event. Most victims of chemical and explosion events will present within the first 6 hours to hospital EDs.13 Rapid clearance of the ED is accomplished by expediting the disposition of patients and clearing the ED of ambulatory patients. Elective procedures and admissions should be held or cancelled. The facility may elect a graded response, which provides for different actions to be taken according to the number of casualties expected. According to the type of incident, additional emergency patient screening areas may be required if the volume of patients overwhelms the resources of the ED.14
Each inpatient unit may be assigned by the disaster plan to automatically accept a predetermined number of patients from the ED who do not yet have beds (eg, 2 per nursing unit, or 110% unit census). Health care facilities should be prepared to discharge inpatients to make beds available for incoming casualties. The discharge function should receive immediate attention when the health care facility disaster plan is activated. Identification of patients eligible for early discharge is an inexact science, but patients who are clinically stable and whose inpatient requirements are limited to a few parenteral medications may be appropriate candidates. Preplanning with ancillary health care services (eg, nursing homes, home health) is essential for these early discharges. A discharge holding area (eg, lounge, cafeteria area) may allow these patients to be moved from their rooms while awaiting appropriate transportation, home care, and pharmacy arrangements.
After expedited discharges, the next most immediate resource for patient care capacity comes from the adaptation of existing capacity. Private rooms may be converted to double rooms, and patients may be placed in halls.15., 16. Closed areas may be reopened if staffing and supplies allow. Health care facilities may find that patient care areas typically reserved for postanesthesia care, chest pain observation, gastroenterology procedures, pulmonary and cardiac catheterization suites, and outpatient surgery areas provide the best opportunities to increase critical care capacity.
Generally, approximately 10% to 20% of a hospital's operating bed capacity can be mobilized within a few hours using these strategies, with an additional 10% from conversion of “flat space” areas such as lobbies, waiting rooms, classrooms, conference facilities, physical therapy areas, and hallways. Inova Health System's 4 hospitals in northern Virginia, for example, made 343 additional beds (of 1,500 total) and 43 operating rooms available within 3 hours of the 2001 Pentagon attack. The District of Columbia made available 200 beds from their existing 2,904 staffed beds. Thus, for any given facility, surge capacity planning should incorporate the availability of about 20% to 30% of operating beds for immediate or near-term patient use. Some institutions may have significantly different numbers according to their elective admission rates, critical case resources, and availability of additional staffed beds. ICU bed availability is likely to be significantly lower.
Protocols must be in place for revision of staff work hours (eg, 12-hour shift standard in disasters), callback of off-duty personnel, use of nonclinical staff (eg, nurse administration, continuous quality improvement coordinator) in clinical roles as appropriate, reallocation of outpatient staff resources (eg, cancel subspecialty clinics and reallocate staff), and use of solicited (former employees, retirees) and unsolicited volunteers. Credentialing of nonemployees should be consonant with institutional bylaws and legislative and accrediting body regulations.17 Untraditional patient care providers such as family members and nonprofessional personnel (eg, city employees) should be considered. Partnerships can be established before an event, with local Medical Reserve Corps18 and other preidentified service organizations.
Specialty patient care surge capability (eg, burns, pediatrics) may be created to address patient needs temporarily but ideally only pending transfer to a specialty center with adequate resources. Consulting with experts from a hospital's usual referral centers may be helpful in planning for these situations.
Temporary external shelters (eg, tents or mobile trailers) for patient holding may be an option. Their practicality will be influenced by the need to have staff familiar with their operation, climate, and the ability to ensure that the shelter(s), the required exterior space for their placement, and any needed infrastructure support (eg, water, utilities) are available. In cases in which the standard of care must be adjusted because of a lack of resources, immediate requests for assistance and patient transfers should be made to allow the best standard of care possible to be applied across the community or region.
5. Community-based surge capacity
A community planning process that integrates regional health care facilities is critical to develop a systematic process to increase health care capacity.19 The individual health care facility represents the “first tier” of response. The mission for the facility is to take steps to increase facility capacity by revising staffing and patient care practices as outlined in the previous sections. Should these responses prove inadequate, the “second tier” of resources—other local health care facilities—is activated.
Barbera and Macintyre8 describe a tiered system that allows facilities to organize before an incident and understand their role within their jurisdiction (Table 2 ). At each level, resources and a coordination mechanism are available. If the resources at one level are inadequate, the next tier is activated, and so on. An incident management system must be in place that incorporates each of these tiers. The definitions for each tier may vary because health care facilities may organize within a jurisdiction (eg, county or city) or span several jurisdictions, depending on their geography.
Table 2.
Tiers of health care disaster response.
| Response Tier | Response Scope | Response Role |
|---|---|---|
| Tier 1 | Individual health care facility | Facility-based “surge in place” response |
| Tier 2 | Health care coalition | Multiple facility response using facility and coalition agreements/plans |
| Tier 3 | Jurisdictional incident management | Community response, coordination at emergency operations center |
| Tier 4 | Regional incident management | Cooperation between jurisdictions/coalitions |
| Tier 5 | State response | Support to jurisdictions |
| Tier 6 | Federal response | Support to state |
Cooperative regional planning by health care facilities allows for more streamlined response and requests for resources. Cooperative agreements should include staff and supply sharing and describe a process for communication and resource request or reallocation during an incident. A mechanism for interacting with jurisdictional authorities should be described and practiced. Transfer agreements should be in place within the region so that patients can be moved from one facility to another (although some contagions may alter these referral plans). Interregional agreements are also encouraged and may be facilitated by state health authorities.
Movement of casualties to areas that have adequate resources is one of the key functions of the cooperative system. In most disasters, health care facilities only a few miles from the incident receive few casualties, and those closest may be overwhelmed.20 A communications coordination point can facilitate local casualty redistribution by ambulance, bus, and other means. It is important that decisionmakers at the regional level have access to accurate information about hospital capacity so that early, appropriate requests for assistance can be made. Regional patient redistribution should occur when required. In certain cases, particularly in a localized outbreak of a highly contagious disease, resources may need to be brought to the area rather than transferring patients out.
The National Disaster Medical System is a federal program that can provide medical response to a disaster area in the form of teams, supplies, equipment, patient movement from a disaster site to unaffected areas of the nation, and definitive medical care at participating hospitals in unaffected areas.21., 22. The National Disaster Medical System thus may provide a national surge capacity for large disasters. Concerns exist that National Disaster Medical System resources might be limited or nonexistent in contagious illness and other disasters that may affect multiple sites or that may occur during a major military contingency.
Community measures to provide the public with adequate health information and mental health support will be in significant demand23., 24. after a disaster. These responses may reduce the need for patient care surge capacity by preventing the health care system from being submerged under a deluge of patients who may not be ill but have concerns and seek further information or evaluation.
Outpatient care systems may see higher volumes of patients because of disaster-related early hospital discharges, visits by patients who were less seriously ill or injured, and visits by patients who are experiencing indirect effects of the event (eg, asthma symptoms from dust). Stresses on home care services from disaster-related hospital discharges can also be expected. Home care agencies and clinics must have surge plans that may include canceling or delaying appointments or visits, increasing staffing, or expanding or limiting services in conjunction with the community response plans.
Public health agencies may need to facilitate home care and family-based care or recommend modifications to the health care framework of the community to meet the needs of the incident (eg, opening screening clinics). One of the goals of ambulatory care surge capacity development is to reduce pressure on the hospitals, allowing them to concentrate on nonambulatory care.
6. Off-site patient care
If a large number of ambulatory “walking wounded” or “potentially exposed” victims are generated by an event, triage and initial treatment sites may be immediately needed to relieve pressure on the emergency transportation and care system. For every casualty injured or infected, hundreds more may seek evaluation.25., 26. Such sites may also be required when the local health care infrastructure is severely damaged. For example, auxiliary care sites have been proposed to cope with health care facility damage after earthquakes.27 Many localities rely on emergency medical services (EMS) to organize triage and initial treatment sites. A process to provide health care workers from other agencies, special teams, or less-affected facilities to the scene should be in place to reduce convergent volunteerism.28
Materials for these sites may be predeployed with response agencies. Supplies should be standardized when possible to facilitate use by mutual aid providers. These sites usually must be rapidly deployed to be effective and may be staffed for hours to days.
Nonambulatory patients should be accommodated within the existing health care infrastructure as much as possible (see facility-based surge capacity above), with patient transfer as a later step. In select situations, usually in the setting of a contagious disease epidemic, but sometimes in the setting of a hospital evacuation or other circumstance, these mechanisms will be inadequate, and an off-site hospital facility may be required. Each hospital accredited by JCAHO is required to plan for such facilities.11 The need for such a facility should be anticipated as early as possible according to patient load, hospital capacity, and event data. The authority to initiate an off-site facility and the administrative, staffing, logistic, and legal issues should be detailed and drilled in advance. Public health will also potentially need sites in the community for outpatient care and vaccination or prophylaxis, and it is important that the same sites not be considered for conflicting missions. Because of economies of scale, it may be appropriate to plan for a few larger off-site facilities in a region than for many smaller ones, which may require cooperative agreements between public health entities. Rural hospitals that must provide off-site care because of facility evacuation or capacity overflow are particularly challenged by a lack of bed capacity, staff, and transportation resources.
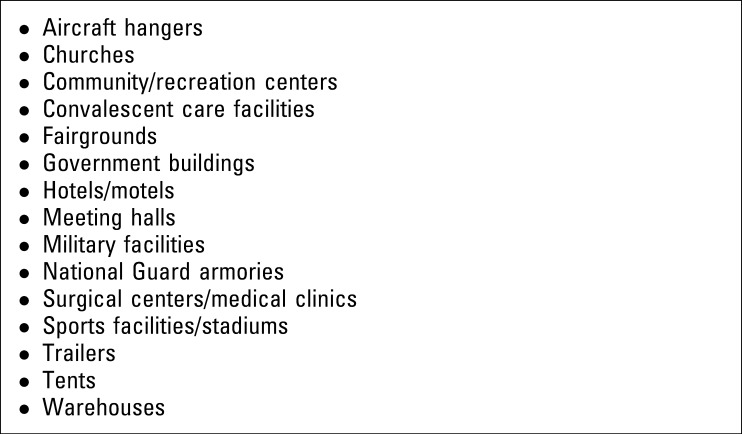
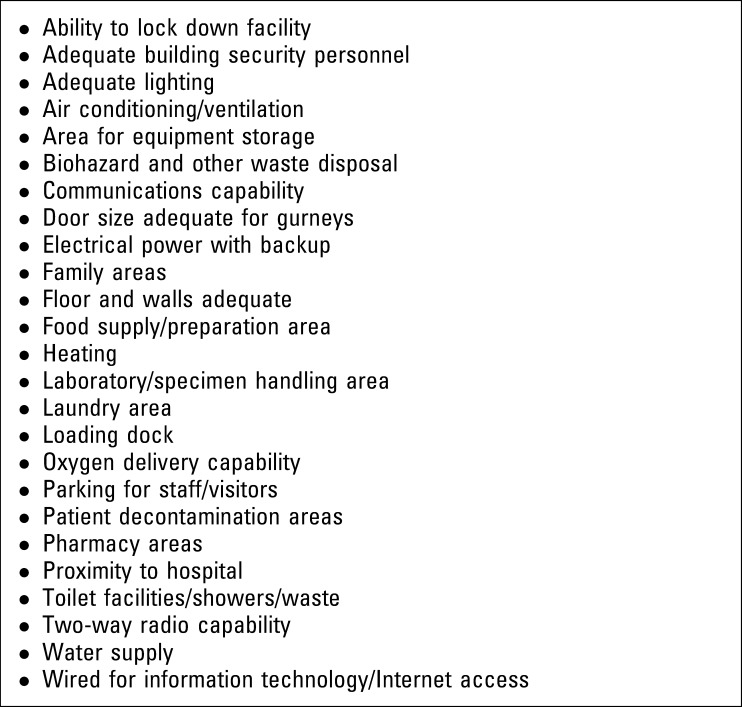
Many possible locations for an off-site hospital facility can be considered (Figure 2 ). The selection of an appropriate site is an imprecise science. Figure 3 lists factors that may be reasonable to consider in the evaluation of a possible site.29 Some items may be of lesser importance, depending on the event and its timing (eg, wide doors when the facility will treat only ambulatory patients or heating capability during summer months). A spreadsheet can be developed with these items on one axis, allowing multiple potential sites to be “graded” and compared. This approach has been demonstrated to be useful in a site-selection exercise, using a 0 to 5 rating scale (bad to good) for each category and was used to evaluate sites for the Athens 2004 Summer Olympics (Col. R. Gum, MC, USA, personal communication, November 2003).29 Ideally, the facility would be publicly owned and rapidly available. Agreements for use of the facility should be in place in advance. The timeframe for converting the facility to patient care use should be understood.
Figure 2.
Potential alternative care sites.
Figure 3.
Factors to consider in alternative care site selection.
Site suitability will change according to the type of event. For example, a hotel may be an excellent choice for less acutely ill patients but may not be appropriate for sicker patients who would be more easily observed and cared for in a single large room (“ward”). Mobile facilities, although avoiding stigma issues, may present logistic challenges, such as availability of plumbing and water, and may have high incremental costs per bed. Surgical centers and other outpatient health care facilities should also be considered and may be more suitable sites to provide critical care than more austere environments.
Guidelines specifying the level of care to be provided and the patient admission and discharge criteria for the facility should be developed and can facilitate planning. Basic nursing care, intravenous fluids, nasogastric feeds, medications (including gravity-administered intravenous medications), and bedside laboratory testing may be the limit of care that can reasonably be provided, with more advanced care provided at the health care facility as part of the “surge in place” response. Field critical care30 poses significant obstacles because even oxygen provision for more than a small number of patients presents logistic issues that should carefully be considered and may be unsolvable.31
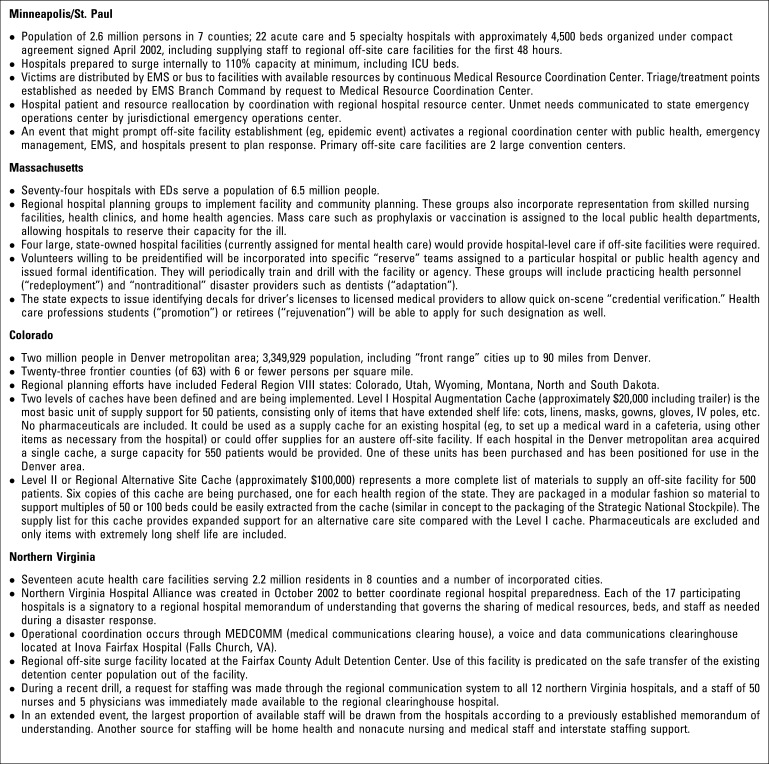
Guidance and templates from the US Army Soldier and Biological Chemical Command have been particularly helpful for planning off-site facility operations.32., 33. Examples of local and regional strategies that are being implemented are noted in Figure 4 .
Figure 4.
System examples.
Generally, planning should be modular, perhaps in 50-patient increments. Staffing, supplies, food, and administrative needs will be driven by the number of modules activated. Documentation, order mechanisms, treatment protocols, pharmacy, and laboratory resources should be planned as much as possible and drilled. Contingencies for making all or part of the facility an isolation area should be in place. Incorporation of state and federal assets (eg, Disaster Medical Assistance Teams) should be anticipated if these resources are available.
Plans should also address transportation to and from the site. Untraditional forms of transport may be needed because EMS assets will be challenged to meet the needs of the disaster, as well as the ongoing needs of the community.
Staff, especially those providing nursing care, are likely to be the key restriction on the number of patients who can be accommodated. In the epidemic setting, health care facilities may be unable to staff their own facilities, let alone off-site facilities, especially because their workers become ill or are unavailable because of family obligations. A plan for staffing the facility for the first few days should be arranged, ideally with a local medical reserve corps or by a hospital coalition. Planning for long-term staffing should begin as soon as a decision is made to activate the facility and is likely to be an ongoing effort.
There are many unresolved regulatory issues regarding the establishment of an off-site hospital. Certain public health regulations may or may not apply, depending on whether the facility is an extension of the hospital or under public health authority, which should be determined ahead of time. Liability coverage, narcotics handling, patient records, reimbursement for staff time and expenses, and the use of licensed and unlicensed volunteers are all issues that deserve mention and will require guidance or legislative efforts at the state and federal level.
7. Limitations and triage
Disaster planning is often not a high priority for health care facilities, despite JCAHO11 and federal grant requirements, often because of the precarious financial situation of many institutions.34 Thirty-two percent of hospitals operated at a deficit in 2002, and this number is expected to increase.6 Furthermore, any disaster, particularly one involving a contagious organism, has the potential to financially cripple involved health care entities because of increased costs (including staff time) that are exacerbated by decreased revenues from cancelled elective appointments and procedures.
Because of limited available surplus resources,35 developing significant surge capacity while maintaining usual standards of care may be difficult, especially for critical care and isolation capacity. Current federal hospital funding programs will not provide a significant increase in capacity. For example, the amount of funding received by the average hospital under the current Health Resources and Services Administration grant will not purchase the equipment in use in a single critical care room or pay to retrofit one airborne infection isolation room. Thus, creative use of “low-tech” solutions is required and may provide efficient care but will not meet the quotidian standard of care (eg, using pulse oximetry and inexpensive oxygen-flow ventilators rather than standard ICU equipment or using inexpensive in-room high-efficiency particulate air filtration rather than purpose-built isolation rooms). Considering dual use in future facility planning (eg, building oxygen supply into meeting rooms) has been explored in limited settings36 and would be of great benefit but often is cost prohibitive.
In some facilities in which beds are available, staffing is insufficient because of nursing shortages, which may be exacerbated during a disaster.37
A number of potential catastrophic events exist for which the health and medical response will rapidly consume available resources. Managing expectations in these situations is a significant issue for the medical community, as well as for political leadership and the general public. Triage of resources will have to occur, and patients will be provided with an adjusted standard of care. This standard may evolve during an incident. It is critical that the public understand that preparedness does not necessarily equate to availability of standard medical care during a disaster. Although triage concepts have been discussed in the medical literature,38., 39., 40. operational systems for health care facility–based triage, particularly of inpatients, are lacking. A system of triage in which those with the best survival probability are offered available resources that could be implemented uniformly would be of great value, particularly for epidemic events.
In conclusion, although general information exists on components of surge capacity, further research and functional exercising are required to better identify the strengths and weaknesses of particular strategies. Such efforts will benefit greatly from the progress that is being made integrating public health and health care into emergency preparedness planning and response.
Planning for patient care surge capacity requires an immense health care facility and community effort by entities with little historical emergency planning experience. Formation of health care facility cooperative agreements and integration with public health and emergency management planning are key first steps in formulating an effective response. Involvement of political leaders is encouraged because, during a health care emergency, many of the decisions have significant political impact, and these authorities must understand the issues and trust the input of public health and health care agencies.
Incident management systems, until recently foreign concepts to many public health and private health care systems, are a necessary component of any effective disaster response. Operational plans must take into consideration the communities' resources, hazards, climate, and other unique factors. Proper planning and drilling for multiple contingencies are important and will help drive changes in response, equipment, and training.
We must be prepared to use all the resources available to ensure the best care possible for the greatest number of individuals. Although this method has always been the goal of disaster medicine, terrorism and the specter of evolving infectious diseases present us with new challenges. With a health care system that is often operating at or over capacity daily, we will never have the resources to be prepared for every disaster, but with appropriate partnerships, incident management systems, and a tiered response framework, we can be prepared to respond to any challenge.
Footnotes
No grant or other funds supported the writing of this article. No products are mentioned in the article that the authors market or have investments in. Dr Barbisch is a principal in Global Deterrence Alternatives, which consults on issues such as these, but no recommendations within the paper support particular initiatives or products that are related to her venture.
Reprints not available from the authors.
References
- 1.Roccaforte J.D. The World Trade Center attack: observations from New York's Bellevue Hospital. Crit Care. 2001;5:307–309. doi: 10.1186/cc1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flomenbaum N. All the king's horses and all the king's men. Acad Emerg Med. 2003;10:646–649. doi: 10.1111/j.1553-2712.2003.tb00050.x. [DOI] [PubMed] [Google Scholar]
- 3.Dacey M.J. Tragedy and response: the Rhode Island nightclub disaster. N Engl J Med. 2003;349:1990–1991. doi: 10.1056/NEJMp038179. [DOI] [PubMed] [Google Scholar]
- 4.Schoch-Spana M. Hospital's full-up: the 1918 influenza pandemic. Public Health Rep. 2001;116:32–33. doi: 10.1093/phr/116.S2.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Derlet R., Richards J., Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001;8:151–155. doi: 10.1111/j.1553-2712.2001.tb01280.x. [DOI] [PubMed] [Google Scholar]
- 6.American Hospital Association. Hospital Statistics 2002. Chicago, IL: American Hospital Association; 2002.
- 7.Eastman P. Bioterrorism preparedness combating disease threats. EM News. 2003;25:58–60. [Google Scholar]
- 8.Barbera J, Macintyre A, eds. Medical Surge Capacity and Capability: A System Template for Managing Medical and Health Resources During Large-Scale Emergencies. Washington, DC: US Department of Health and Human Services. In press.
- 9.Koenig K.L., Dinerman N., Kuehl A.E. Disaster nomenclature: a functional approach: the PICE system. Acad Emerg Med. 1996;3:723–727. doi: 10.1111/j.1553-2712.1996.tb03498.x. [DOI] [PubMed] [Google Scholar]
- 10.Barbera J, Macintyre A. Medical and health incident management system: a comprehensive functional system description for mass casualty medical and health incident management [George Washington University Institute for Crisis, Disaster, and Risk Management Web site]. Available at: http://www.gwu.edu/∼icdrm. Accessed November 16, 2003.
- 11.Joint Commission on Accreditation of Healthcare Organizations . Joint Commission on Accreditation of Healthcare Organizations; Oakbrook Terrace, IL: 2001. The 2001 Joint Commission Comprehensive Accreditation Manual for Hospitals. [Google Scholar]
- 12.San Mateo County Emergency Medical Services Agency. Hospital Emergency Incident Command System III, January 1998. Available at: http://www.emsa.cahwnet.gov/dms2/heics3.htm. Accessed January 13, 2004.
- 13.Greenberg M.I., Hendrickson R.G. CIMERC: Drexel University Emergency Department Terrorism Preparedness Consensus Panel: report of the CIMERC/Drexel University Emergency Department Terrorism Preparedness Consensus Panel. Acad Emerg Med. 2003;10:783–788. [PubMed] [Google Scholar]
- 14.Schultz C.H., Mothershead J.L., Field M. Bioterrorism preparedness,: I: the emergency department and hospital. Emerg Med Clin North Am. 2002;20:437–455. doi: 10.1016/s0733-8627(02)00003-2. [DOI] [PubMed] [Google Scholar]
- 15.Viccellio P. ED overcrowding: right diagnosis, wrong etiology, no treatment. EM News. 2003;25:25. [Google Scholar]
- 16.SoRelle R. A real solution to overcrowding. EM News. 2003;25:1–10. [Google Scholar]
- 17.Joint Commission on Accreditation of Healthcare Organizations . Joint Commission on Accreditation of Healthcare Organizations; Oakbrook Terrace, IL: 2003. Comprehensive Accreditation Manual for Hospitals: Medical Staff Section MS.5.14.4.1: Disaster Privileging Standard. [Google Scholar]
- 18.US Department of Health and Human Services. Medical Reserve Corps. Available at: http://www.medicalreservecorps.gov. Accessed January 16, 2004.
- 19.Joint Commission on Accreditation of Healthcare Organizations. Health care at the crossroads: strategies for creating and sustaining community-wide emergency preparedness systems. Available at: http://www.jcaho.org/accredited+organizations/ambulatory+care/advisor/2003issue1/emergency+preparedness.pdf. Accessed January 16, 2004.
- 20.Auf der Heide E. CV Mosby and Co; St. Louis, MO: 1989. Disaster Response. [Google Scholar]
- 21.Department of Health and Human Services. National Disaster Medical System. Available at: http://ndms.dhhs.gov. Accessed January 16, 2004.
- 22.Knouss R.F. National Disaster Medical System. Public Health Rep. 2001;116:49–52. doi: 10.1016/S0033-3549(04)50142-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Basrur SV. Toronto Public Health's Response to the Severe Acute Respiratory Syndrome Outbreak 2003: Report to the Toronto Board of Health. Toronto, Ontario, Canada: Toronto Board of Health; 2003.
- 24.Rosack J. Mental health effects of terrorism. Psychiatric News. January 4, 2002:4–5. [Google Scholar]
- 25.Okumura T., Suzuki K., Fukada A. The Tokyo subway sarin attack: disaster management,: part 2: hospital response. Acad Emerg Med. 1998;5:618–624. doi: 10.1111/j.1553-2712.1998.tb02471.x. [DOI] [PubMed] [Google Scholar]
- 26.Petterson J.S. Perception vs. reality of radiological impact: the Goiana model. Nuclear News. 1988;31:84. [Google Scholar]
- 27.Schultz C.H., Koenig K.I., Noji E.K. A medical disaster response to reduce immediate mortality after an earthquake. N Engl J Med. 1996;334:438–444. doi: 10.1056/NEJM199602153340706. [DOI] [PubMed] [Google Scholar]
- 28.Cone D.C., Weir S.D., Bogucki S. Convergent volunteerism. Ann Emerg Med. 2003;41:457–462. doi: 10.1067/mem.2003.107. [DOI] [PubMed] [Google Scholar]
- 29.Denver Health and the Rocky Mountain Regional Model for Bioterrorist Events (RMBT) Working Group. Contract 290-00-0014, Task Order Number 5, US Department of Health and Human Services, Agency for Healthcare Research and Quality. Available at: http://www.denverhealth.org/BioTerror/Tools.htm. Accessed January 17, 2004.
- 30.Kevetan V. Intensive care in a field hospital in an urban disaster area: are we ready? Crit Care Med. 2003;31:1589–1590. doi: 10.1097/01.CCM.0000059438.11968.B9. [DOI] [PubMed] [Google Scholar]
- 31.Rizzo A. “Deployable oxygen solutions for FEMA” briefing [appendix A]. Available at: http://www.denverhealth.org/bioterror/Document/DH2SupplyStaffing10-30-03.pdf. Accessed January 28, 2004.
- 32.Skidmore S., Wall W., Church J. US Department of Defense; Aberdeen Proving Ground, MD: 2003. Modular Emergency Medical System Concept of Operation for the Acute Care Center: Mass Casualty Strategy for a Biological Terror Incident. [Google Scholar]
- 33.Church J. US Department of Defense; Aberdeen Proving Ground, MD: 2003. Neighborhood Emergency Help Center: A Mass Casualty Care Strategy for Biological Terrorism Incidents. [Google Scholar]
- 34.Barbera J.A., Macintyre A.G., DeAtley C.A. John F. Kennedy School of Government, Harvard University; Boston, MA: 2001. Ambulances to Nowhere: America's Critical Shortfall in Medical Preparedness for Catastrophic Terrorism [BCSIA Discussion Paper 2001-15; Executive Session on Domestic Preparedness (ESDP) Discussion Paper 2001-07] [Google Scholar]
- 35.Bloem K. Treating the sick: capacity of the US Health Care System to respond to an epidemic. Public Health Rep. 2001;116(Suppl 2):34–35. doi: 10.1016/S0033-3549(04)50138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Project ER 1. Washington Hospital Center and MedStar Emergency. Available at: http://www.er1.org. Accessed January 16, 2004.
- 37.Joint Commission on Accreditation of Healthcare Organizations . Joint Commission on Accreditation of Healthcare Organizations; Oakbrook Terrace, IL: 2002. Health Care at the Crossroads: Strategies for Addressing the Evolving Nursing Shortage. [Google Scholar]
- 38.Burkle F.M. Mass casualty management of a large-scale bioterrorist event: an epidemiological approach that shapes triage decisions. Emerg Med Clin North Am. 2002;20:409–436. doi: 10.1016/s0733-8627(01)00008-6. [DOI] [PubMed] [Google Scholar]
- 39.Coupland R.M. Epidemiological approach to surgical wound management of the casualties of war. BMJ. 1994;308:1693–1697. doi: 10.1136/bmj.308.6945.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pesik N., Keim M.E., Iserson K.V. Terrorism and the ethics of emergency medical care. Ann Emerg Med. 2001;37:642–646. doi: 10.1067/mem.2001.114316. [DOI] [PubMed] [Google Scholar]