Abstract
Background
The Eating Disorder Examination – Questionnaire Short (EDE-QS) was developed as a 12-item version of the Eating Disorder Examination Questionnaire (EDE-Q) with a 4-point response scale that assesses eating disorder (ED) symptoms over the preceding 7 days. It has demonstrated good psychometric properties at initial testing. The purpose of this brief report is to determine a threshold score that could be used in screening for probable ED cases in community settings.
Methods
Data collected from Gideon et al. (2016) were re-analyzed. In their study, 559 participants (80.86% female; 9.66% self-reported ED diagnosis) completed the EDE-Q, EDE-QS, SCOFF, and Clinical Impairment Assessment (CIA). Discriminatory power was compared between ED instruments using receiver operating characteristic (ROC) curve analyses.
Results
A score of 15 emerged as the threshold that ensured the best trade-off between sensitivity (.83) and specificity (.85), and good positive predictive value (.37) for the EDE-QS, with discriminatory power comparable to other ED instruments.
Conclusion
The EDE-QS appears to be an instrument with good discriminatory power that could be used for ED screening purposes.
Keywords: EDE-QS, Eating disorders, Screening, ROC analysis, Discriminant validity
Background
The Eating Disorder Examination Questionnaire (EDE-Q [1];), derived from the Eating Disorder Examination (EDE [2];), is one of the most widely used and extensively validated self-report instruments for eating disorder (ED) assessment. However, the lengthy administration time of the EDE-Q and the 28-day period over which it captures symptoms may be problematic when monitoring session-by-session outcomes in the context of clinical practice and treatment. Consequently, researchers have developed modified versions of this tool [3]. One such version is the 12-item EDE-QS, which was recently developed employing Rasch’s analysis among individuals with EDs receiving specialist treatment [4]. The EDE-QS removes the open-ended responses to behavioural items and also narrows the reference timeframe from the past 28-days to the past 7-days. Alongside its brevity, this timeframe was adopted to improve recall potential, and positions the EDE-QS as a routine outcome-monitoring instrument for individuals in treatment to aid clinical decision-making via improved and regular feedback [5].
The EDE-QS has demonstrated good internal consistency, test-retest reliability, convergent validity and sensitivity in a mixed sample of individuals with probable ED and individuals probably not having an ED, recruited from a university and a charity [4]. Its brevity and psychometric properties provide preliminary support for the use of the EDE-QS as a screening tool for people with EDs in community settings. However, a threshold value was not established for the EDE-QS questionnaire, as it was not originally developed as a screening instrument. Cut-off scores are important for facilitating the detection of individuals likely to be experiencing threshold EDs and differentiating these individuals from those who are unlikely to have ED symptoms. Existing instruments (such as the original EDE-Q) are either too long to be practical to use for screening purposes, do not capture each disorder across the ED spectrum (for instance, SCOFF does not assess BED symptoms), or have inadequate psychometric properties in some populations (e.g. SCOFF in overweight women) [6]. Therefore, the aim of this brief report was to establish and evaluate a cut-off point on the EDE-QS that could be utilized by researchers and clinicians when identifying probable ED cases in community settings.
Method
Participants and procedures
A total of 559 people, who were recruited from a university and through a charity that offers support for eating disorders, participated in the EDE-QS validation part of the study first reported by Gideon et al. [4]. The same data are used for the secondary analysis reported in the current study. The majority of participants were women (80.86%) aged between 18 and 34 years (92.31%). Seventy-eight percent of the participants identified as White and 88.90% had tertiary (post-secondary school) education. Fifty-four (9.66%) participants self-reported currently having an ED diagnosis (i.e. they responded with Yes to the question “Do you currently suffer from an eating disorder (anorexia nervosa, bulimia nervosa, binge eating disorder, eating disorder not otherwise specified)?”). Of these, 7 (13%) met criteria for restrictive anorexia nervosa (AN-R); two (4%) for binge eating/purging AN subtype (AN-BP); eight (15%) for bulimia nervosa (BN); 10 (19%) for binge eating disorder (BED); and 27 (50%) for other specified feeding and eating disorders (OSFED) based on their responses on the EDE-Q and their Body Mass Index (BMI). Mean BMI in the total sample was 22.35 (SD = 4.61), with 12% of participants classified as underweight, 72% as average-weight, 12% as overweight, and 3% as obese. Underweight individuals were not excluded from the subsample of participants who self-reported currently not having an ED diagnosis. Detailed information about recruitment processes and data collection have been presented elsewhere [4]. In brief, an invitation to participate was distributed to a large university in London, UK, and the study was advertised via the Beat - Beating Eating Disorders website, a UK’s eating disorder charity that offers support to people with current or former ED difficulties and their families. Participants provided informed consent and completed an online survey.
Measures
Eating disorder examination-questionnaire short
The EDE-QS was developed by Gideon et al. [4] as a 12-item version of the EDE-Q (see below) with a response scale ranging from 0 to 3, that captures essential symptoms of AN, BN and BED. The response scale was shortened during the development of the EDE-QS to reduce the cognitive demand and because respondents were not making full use of the 0–6 scale (some original categories were not used consistently with respondents’ ED severity), as observed in Rasch analysis results [see 4]. Scores of items are summed, ranging from 0 to 36 and higher scores indicate greater ED symptoms. ED symptoms are reported for the preceding seven days. Cronbach’s alpha obtained in this sample was .91 [4] indicating excellent internal consistency.
Ede-q
The most recent version of the full EDE-Q [7] is a 28-item measure of ED symptoms and behaviors. Scores on each of four subscales (Restraint, Eating Concerns, Shape Concerns, Weight Concerns) and a Global score may be derived from items assessing core attitudinal features. Participants provide their answers on a scale from 0 to 6, with higher scores indicating greater frequency and/or severity of ED psychopathology over the previous 28 days. The EDE-Q has been validated in various clinical and non-clinical samples [8]. Previous studies showed a cut-off score for “probable” ED amongst young women of 2.3 (in conjunction with the occurrence of binge eating and/or excessive exercise) [9], and a clinical cut-off of a global EDE-Q score ≥ 2.8 [6]. In the current study sample, Cronbach’s alpha was .96 for the global score and .84, .86, .93 and .88 for the Restraint, Eating Concern, Shape Concern, and Weight Concern subscales, respectively.
Scoff
The SCOFF [10] is a 5-item measure used to screen for EDs in primary care. Items tap into key symptoms of AN and BN with a dichotomous (Yes/No) response scale. The number of “Yes” responses are summed to create a total score, with a score ≥ 2 indicative of an ED. The SCOFF has been found to have good psychometric properties in international community samples [11]. Cronbach’s alpha in the current sample was .64 [4].
Clinical impairment assessment
The CIA (CIA 3.0) [12] was designed to measure psychosocial impairment associated with key ED features in the past 28 days. Sixteen items are answered on a 4-point Likert-type scale summed to compute the global score, with higher scores indicating greater perceived impairment. The CIA has previously been used for ED instrument validation [13, 14] since clinical impairment has shown to be higher among ED clinical samples relative to healthy controls [15], thus supporting the instrument’s criterion validity [16]. The CIA has robust psychometric properties [12]. In the present sample, Cronbach’s alpha was .96.
Data analysis
The R package “epiR” was used to obtain sensitivity (the proportion of true cases correctly identified by the test), specificity (the proportion of true non-cases correctly identified by the test), positive predictive values (PPV; the proportion of individuals with positive test results who have an ED), and negative predictive values (NPV; the proportion of individuals with negative test results who do not have an ED). The PPVs and NPVs depend upon the prevalence of the disorder (e.g. if the prevalence is < 10% then PPV can be < 0.5) thus there is no defined criterion for classifying PPV or NPV as “acceptable,” or “good” [17]. The package “pROC” was used to compute the Area Under the Curve (AUC; the surface area under the curve which describes the relationship between sensitivity and specificity) statistic and confidence intervals (CI). AUC can obtain values from 0 to 1, with AUC of 0.50 classified as non-informative; between 0.50 and 0.70 as less accurate; between 0.70 and 0.90 as moderately accurate; between 0.90 and 1 as highly accurate; and AUC = 1 is considered as perfect [18]. Two participants (0.36%) with missing values in the question about current ED diagnosis were excluded from the analyses (their Global EDE-Q scores were in a 30th and 38th percentile, indicating their removal would not markedly impact analyses as they did not have extreme results in this variable). Complete data were available for all other variables. Summation scores are more sensitive to missing data than other scoring methods [19], but as there were no missing data for the EDE-QS, summation was considered to be appropriate for this study. Global cut-off scores calculated as the average of item scores are also derived and presented in Table 1 in case of a necessary use by future researchers or clinicians, although for the simplicity in the following text we limit our discussion to global summation scores.
Table 1.
Mean (SD) of clinical impairment, EDE-Q scores, and eating disorder behaviour for self-reported eating disorder cases (n = 54) and non-cases (n = 503) in the current study and normative data reported by Mond et al. (2004)
| Current study | Normative data | ||||
|---|---|---|---|---|---|
| Self-reported ED cases (n=54) | Self-reported ED non-cases (n=503) | ED cases | ED non-cases | ||
| Mean (SD) | Mean (SD) | t | Mean (SD) | Mean (SD) | |
| Clinical impairment | 28.67(12.44) | 8.24(8.47) | 12.15** | ||
| Global EDE-Q | 3.99(1.39) | 1.67(1.32) | 12.25** | 3.09(0.83) | 1.30(0.96) |
| Restraint | 3.67(1.69) | 1.52(1.46) | 9.47** | 2.65(1.48) | 1.19(1.21) |
| Eating concerns | 3.40(1.54) | 0.97(1.22) | 11.26** | 2.02(0.95) | 0.49(0.74) |
| Weight concerns | 4.23(1.43) | 1.86(1.59) | 12.04** | 3.68(1.08) | 1.49(1.20) |
| Shape concerns | 4.64(1.44) | 2.31(1.63) | 11.90** | 4.01(0.98) | 2.03(1.38) |
| OBE | 44.4% | 12.1% | 4.63** | 25.0% | 2.2% |
| SBE | 5.5% | 9.7% | -1.23 | 25.0% | 6.0% |
| Excessive exercisinga | 27.8% | 6.4% | 3.43* | 58.3% | 8.2% |
Note. ED – eating disorders; OBE – objective binge eating (≥ 4 episodes in the last 28 days); SBE – subjective binge eating (≥ 4 episodes in the last 28 days)
a ≥ 20 times in the last 28 days
* p < .01
** p < .001
Using the self-reported ED diagnosis variable, the number of true positive, false positive, true negative, and false negative cases were determined separately for every possible cut-off score on the EDE-QS, and for the previously established range of cut-off scores on the EDE-Q (from 1.3 to 2.9) [20] and all possible SCOFF scores (from 0 to 5) [21]. Sensitivity and specificity rates were calculated for each of the possible cut-off score in these instruments, and PPV and NPV were also obtained. For the purpose of the current study, only findings for cut-off scores that yielded the highest levels of discriminatory parameters are reported, as the aim was to detect a cut-off score with high sensitivity, specificity and PPV. In addition to this, discriminatory parameters were also derived among female participants solely (n = 452).
Results
Comparison of ED symptom levels between study subgroups
In the absence of assignment of “ED case” status on the basis of clinical interview, preliminary analysis was conducted to confirm the validity of the “clinical” and “non-clinical” group identification, which was based on self-reported ED diagnosis. In Table 1, two groups were compared according to clinical impairment level, EDE-Q scores, and eating disorder behavior assessed by the EDE-Q. These include objective binge eating episodes (eating unusually large amount of food and having sense of losing control over eating), subjective binge eating episodes (having sense of losing control over eating without eating unusually large amount of food), and excessive exercising as a means of controlling weight or shape. Normative data for EDE-Q scores and prevalence of eating disorder behavior were also reported in Table 1 to ease comparison with present findings. As can be seen, participants with a self-reported ED had markedly elevated levels of ED symptoms when compared with the non-ED group, levels comparable to (but higher than) those of community cases of ED among young adult women identified by means of interview assessment in previous research.
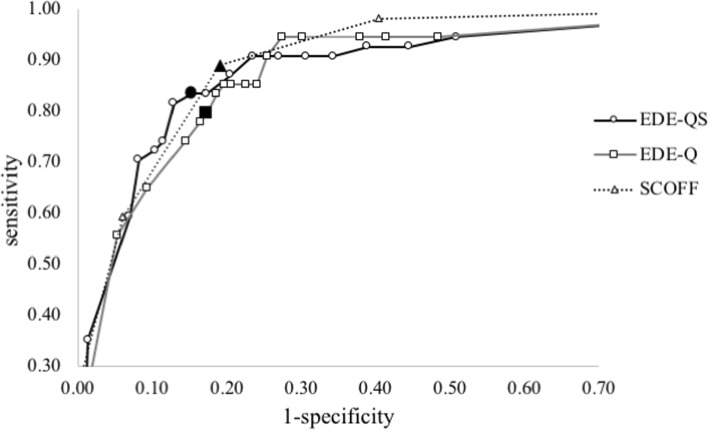
Comparison between measures
As shown in Fig. 1 and Table 2, the EDE-Q and EDE-QS demonstrated good, and the SCOFF excellent, discriminatory power according to the AUC statistic (AUC > .90) [18]. The EDE-Q showed an optimal sensitivity (.80) and specificity (.83) at a cut-off score of 2.8, where the PPV and NPV reached 33 and 97%, respectively. Similarly, with the cut-off score of ≥2, the SCOFF obtained a PPV and NPV of 34 and 99%, respectively. The EDE-QS demonstrated an optimal sensitivity (.83) and specificity (.85) at a total score cut-off of 15. At this cut-off, the NPV was very high (98%), as with the EDE-Q and SCOFF, while the PPV of 37% was higher than that for the EDE-Q (33%) or SCOFF (34%). Similar results were observed in the female subsample, with numerical differences in statistics of approximately 0.02 (higher sensitivity and PPV, lower specificity). Also, at a cut-off score of 15 on the EDE-QS, the proportion of probable ED cases in the total sample was 21.82%, which is somewhat lower than the rates yielded by the EDE-Q (23.26%) and SCOFF (25.58%), and closer to the proportion of participants’ self-reported ED diagnosis (9.66%).
Fig. 1.
Relationship between sensitivity and specificity at different cut-off scores. Black-colored markers indicate cut-off scores of 15, 2.8, and 2 for EDE-QS, EDE-Q, and SCOFF, respectively
Table 2.
Summary statistics for various global score thresholds on the EDE-Q, EDE-QS (summation/average), and SCOFF
| Cut-off | Rate of probable ED (%) | Se(95%CI) | Sp(95%CI) | PPV(95%CI) | NPV(95%CI) | AUC(95%CI) |
|---|---|---|---|---|---|---|
| EDE-Q | ||||||
| 2.6 | 25.94 | .85(.73–.93) | .80(.77–.84) | .32(.24–.40) | .98(.96–.99) | 88(.84–.93) |
| 2.7 | 24.87 | .83(.71–.92) | .81(.78–.85) | .32(.25–.41) | .98(.96–.99) | |
| 2.8 | 23.26 | .80(.66–.89) | .83(.79–.86) | .33(.25–.42) | .97(.95–.99) | |
| EDE-QS | ||||||
| 13/1.0 | 26.83 | .87(.75–.95) | .80(.76–.83) | .31(.24–.39) | .98(.96–.99) | 89(.84–.93) |
| 14/1.1 | 23.61 | .83(.71–.92) | .83(.79–.86) | .34(.26–.43) | .98(.96–.99) | |
| 15/1.2 | 21.82 | .83(.71–.92) | .85(.81–.88) | .37(.28–.46) | .98(.96–.99) | |
| 16/1.3 | 19.50 | .81(.69–.91) | .87(.84–.90) | .40(.31–.50) | .98(.96–.99) | |
| SCOFF | ||||||
| 2 | 25.58 | .89(.77–.96) | .81(.77–.84) | .34(.26–.42) | .99(.97–.99) | .90(.87–.94) |
Note. ED eating disorders, Se Sensitivity, Sp Specificity, PPV Positive Predictive Value, NPV Negative Predictive Value, AUC Area Under the Curve, CI Confidence Interval
Comparison of alternative EDE-QS cut-off points
An EDE-QS score of 13 (but not 14 or 15) was within 1 SD of the mean score among participants who did not report an ED diagnosis, indicating that scores above 13 are likely to serve as cut-off points, if guided by suggestions in previous studies [20, 22]. Also, when utilizing the formula for detection of the criterion of clinical significance [23], defined as the mid-point between mean values of non-cases and cases, the result was 13.97. However, sensitivity was the same for cut-off points of 14 and 15, while specificity was greater with a cut-off point of 15. When comparing mean CIA total scores between self-reported ED cases and non-cases according to each of these proposed cut-off points, the difference was greatest with a cut-off point of 15 (Mdiff = 20.05; 14: Mdiff = 19.32; 13: Mdiff = 18.53).
Discussion
The EDE-QS demonstrated good discriminatory power, obtaining AUC, sensitivity, specificity and PPV estimates similar to those of the 28-item EDE-Q used in this study, and similar values were also reported in a study of young women in primary care [6]. Hence, reducing the number of items did not influence this instrument’s ability to differentiate between self-reported ED cases and non-cases. Similar discriminatory parameters where observed between the EDE-QS and the SCOFF as well, with a higher specificity but lower sensitivity produced by the EDE-QS. At the optimal cut-off point for the EDE-QS of 15, which yielded the best trade-off between sensitivity (.83) and specificity (.85) and the greatest divergence in clinical impairment between self-reported ED cases and non-cases, PPV was higher for the EDE-QS than for the SCOFF (.37 vs .34). A potential advantage of the EDE-QS is that it provides more information on specific ED behaviors and their severity, which could be more clinically useful and hence outweigh the cost of the additional time taken to complete few more items. For instance, the EDE-QS captures the frequency of binge eating and purging behavior, which is important for risk and health management.
It has been suggested [21] that when establishing cut-off points for ED screening tools, priority should be given to maximizing sensitivity (i.e. lowering the criteria for reaching ED level) rather than specificity, since the purpose of these instruments is to capture potential ED cases, the status of which could then be confirmed by means of further assessment, such as a clinical interview. Prioritizing sensitivity through the selection of a slightly lower cut-off point, while conducive to an over-inclusion of non-cases, would serve to ensure the inclusion of individuals experiencing or likely to experience clinically significant impairment associated with ED symptoms and could therefore be seen as good early intervention practice [24]. The current findings suggest that a cut-off point of 15 may be optimal when using the EDE-QS for screening purposes, although a slightly lower cut-off point may be preferable if optimizing sensitivity is the goal.
Limitations and directions for future research
Some limitations should be noted. First, as in most previous studies of screening measures for ED, men were under-represented in the current study sample. Importantly, previous research has suggested that, when compared to thresholds established for women, a lower cut-off score on ED measures may be required to identify clinically significant ED symptoms in men [25, 26]. As the number of males with EDs in the current study was insufficient to conduct separate gender segregated analyses, further research will be needed to identify appropriate cut-off points for the EDE-QS (and other screening instruments) for men. Second, participants’ age ranged between 19 and 34, calling into question the representativeness of this group for the general population, including adolescents and elderly people. Relatedly, only 15% were classified as overweight or obese which might signify the shortfall of participants who experience regular binge eating episodes. Third, ED cases were self-reported rather than independently identified which is why inferences concerning direct application of the EDE-QS as a screening instrument at this stage are necessarily tentative. Further directions for future research hence include validation in general population and primary care samples using clinical interview as a reference point. Furthermore, while the fact that the EDE-QS captures ED symptoms over the past 7 days may be strength in terms of facilitating participant recall, the use of this relatively short time period - far less than the period of 3 months specified in formal diagnostic criteria - underscores the point that the EDE-QS, like the EDE-Q, is not intended as and should not be used as a diagnostic instrument. Lastly, to examine the suitability of the further use of the EDE-QS as a single-factor measure of ED psychopathology, additional directions for future research include employing parallel analysis for examination of the factor structure since this method has been shown to be superior to scree-plot analysis [27], that was used in the initial EDE-QS development study [4].
Conclusion
In conclusion, as well as being a useful instrument for repeated assessments of people in treatment for an ED, the EDE-QS may be useful in screening for individuals likely to have clinically significant ED symptoms in non-clinical populations. In this study a cut-off score of 15 provided optimal validity coefficients.
Acknowledgements
Western Sydney University had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. Scott Griffiths is supported by a National Health and Medical Research Council Early Career Fellowship (grant number: 1121538) and receives honoraria from Elsevier in his capacity as Associate Editor for Body Image.
Abbreviations
- ED
Eating disorders
- EDE-QS
Eating Disorder Examination Questionnaire Short
- EDE-Q
Eating Disorder Examination Questionnaire
- AN-R
Anorexia nervosa restrictive type
- AN-BP
Anorexia nervosa binge eating/purging type
- BN
Bulimia nervosa
- BED
Binge eating disorder
- OSFED
Other specified feeding and eating disorders
- BMI
Body mass index
- CIA
Clinical Impairment Assessment
- ROC
Receiver operating characteristic
- AUC
Area under the curve
- PPV
Positive predictive value
- NPV
Negative predictive value
Authors’ contributions
NG, LS and JM conducted and wrote the original study. KP performed the analyses. KP, DM, SG, JM, NG, LS and PH wrote the paper. All authors have read and approved the manuscript.
Funding
Funding for this study was provided by the Western Sydney University as a scholarship to corresponding author (KP).
Availability of data and materials
Original data is available as a supplementary file in the manuscript published by Gideon et al. (2016): 10.1371/journal.pone.0152744.s004
Ethics approval and consent to participate
Ethical approval for the original data collection was obtained from a National Health Service (NHS) ethics committee (reference number: 13/EE/0254). The type of consent was “implied” since participants provided consent by proceeding with the online survey, which had been approved by the ethics committee.
Consent for publication
Not applicable.
Competing interests
Professor Hay receives/has received sessional fees and lecture fees from the Australian Medical Council, Therapeutic Guidelines publication, and New South Wales Institute of Psychiatry and royalties/honoraria from Hogrefe and Huber, McGraw Hill Education, and Blackwell Scientific Publications, Biomed Central and PlosMedicine and she has received research grants from the NHMRC and ARC. She is Chair of the National Eating Disorders Collaboration Steering Committee in Australia (2012-) and Member of the ICD-11 Working Group for Eating Disorders (2012–2019) and was Chair Clinical Practice Guidelines Project Working Group (Eating Disorders) of RANZCP (2012–2015). In the past 5 years she has consulted for, conducted education of Psychiatrists, and prepared a report under contract for Shire Pharmaceuticals. All views in this paper are her own. Deborah Mitchison is an Editorial Board Member.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16(4):363–370. [PubMed] [Google Scholar]
- 2.Fairburn CG, Cooper Z, O'Connor M. The eating disorder examination. Int J Eat Disord. 1993;6:1–8. [Google Scholar]
- 3.Kliem S, Mossle T, Zenger M, Strauss B, Brahler E, Hilbert A. The eating disorder examination-questionnaire 8: a brief measure of eating disorder psychopathology (EDE-Q8) Int J Eat Disord. 2016;49(6):613–616. doi: 10.1002/eat.22487. [DOI] [PubMed] [Google Scholar]
- 4.Gideon N, Hawkes N, Mond J, Saunders R, Tchanturia K, Serpell L. Development and psychometric validation of the EDE-QS, a 12 item short form of the eating disorder examination questionnaire (EDE-Q) PLoS One. 2016;11(5):e0152744. doi: 10.1371/journal.pone.0152744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simon W, Lambert MJ, Busath G, Vazquez A, Berkeljon A, Hyer K, Granley M, Berrett M. Effects of providing patient progress feedback and clinical support tools to psychotherapists in an inpatient eating disorders treatment program: a randomized controlled study. Psychother Res. 2013;23(3):287–300. doi: 10.1080/10503307.2013.787497. [DOI] [PubMed] [Google Scholar]
- 6.Mond JM, Myers TC, Crosby RD, Hay PJ, Rodgers B, Morgan JF, Lacey JH, Mitchell JE. Screening for eating disorders in primary care: EDE-Q versus SCOFF. Behav Res Ther. 2008;46(5):612–622. doi: 10.1016/j.brat.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Fairburn CG, Beglin SJ. Eating disorder examination questionnaire. Cognitive behaviour therapy and eating disorders. 2008;309:313. [Google Scholar]
- 8.Berg KC, Peterson CB, Frazier P, Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: a systematic review of the literature. Int J Eat Disord. 2012;45(3):428–438. doi: 10.1002/eat.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mond JM, Hay PJ, Rodgers B, Owen C, Beumont P. Validity of the eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther. 2004;42:551–567. doi: 10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- 10.Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. Bmj. 1999;319(7223):1467–1468. doi: 10.1136/bmj.319.7223.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Richter F, Strauss B, Braehler E, Adametz L, Berger U. Screening disordered eating in a representative sample of the German population: usefulness and psychometric properties of the German SCOFF questionnaire. Eat Behav. 2017;25:81–88. doi: 10.1016/j.eatbeh.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 12.Bohn K, Doll HA, Cooper Z, O'Connor M, Palmer RL, Fairburn CG. The measurement of impairment due to eating disorder psychopathology. Behav Res Ther. 2008;46(10):1105–10. doi: 10.1016/j.brat.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Welch E, Birgegård A, Parling T, Ghaderi A. Eating disorder examination questionnaire and clinical impairment assessment questionnaire: general population and clinical norms for young adult women in Sweden. Behav Res Ther. 2011;49(2):85–91. doi: 10.1016/j.brat.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 14.Zickgraf HF, Ellis JM. Initial validation of the nine item avoidant/restrictive food intake disorder screen (NIAS): a measure of three restrictive eating patterns. Appetite. 2018;123:32–42. doi: 10.1016/j.appet.2017.11.111. [DOI] [PubMed] [Google Scholar]
- 15.Vannucci A, Kass AE, Sinton MM, Aspen V, Weisman H, Bailey JO, Wilfley DE, Taylor CB. An examination of the clinical impairment assessment among women at high risk for eating disorder onset. Behav Res Ther. 2012;50(6):407–414. doi: 10.1016/j.brat.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jenkins PE. Psychometric validation of the clinical impairment assessment in a UK eating disorder service. Eat Behav. 2013;14(2):241–243. doi: 10.1016/j.eatbeh.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Williams P, Hand D, Tarnopolsky A. The problem of screening for uncommon disorders—a comment on the eating attitudes test. Psychol Med. 1982;12:431–434. doi: 10.1017/S003329170004678X. [DOI] [PubMed] [Google Scholar]
- 18.Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240(4857):1285–1293. doi: 10.1126/science.3287615. [DOI] [PubMed] [Google Scholar]
- 19.Downey RG, King CV. Missing data in Likert ratings: a comparison of replacement methods. J Gen Psych. 1998;125(2):175–191. doi: 10.1080/00221309809595542. [DOI] [PubMed] [Google Scholar]
- 20.Fairburn CG, Cooper D, Phil DP. Zafra, Doll D Phil HA, O’Connor ME, Bohn D Phil DP, Kristin, hawker DM, Wales JA, Palmer RL. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166(3):311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill LS, Reid F, Morgan JF, Lacey JH. SCOFF, the development of an eating disorder screening questionnaire. Int J Eat Disord. 2010;43(4):344–351. doi: 10.1002/eat.20679. [DOI] [PubMed] [Google Scholar]
- 22.Rø Ø, Reas DL, Stedal K. Eating disorder examination questionnaire (EDE-Q) in Norwegian adults: discrimination between female controls and eating disorder patients. Eur Eat Disord Rev. 2015;23(5):408–412. doi: 10.1002/erv.2372. [DOI] [PubMed] [Google Scholar]
- 23.Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59(1):12–19. doi: 10.1037/0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- 24.Jacobi C, Abascal L, Taylor CB. Screening for eating disorders and high-risk behavior: caution. Int J Eat Disord. 2004;36(3):280–295. doi: 10.1002/eat.20048. [DOI] [PubMed] [Google Scholar]
- 25.Liu CY, Tseng MC, Chen KY, Chang CH, Liao SC, Chen HC. Sex difference in using the SCOFF questionnaire to identify eating disorder patients at a psychiatric outpatient clinic. Compr Psychiatry. 2015;57:160–166. doi: 10.1016/j.comppsych.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 26.Smith KE, Mason TB, Murray SB, Griffiths S, Leonard RC, Wetterneck CT, Smith BER, Farrell NR, Riemann BC, Lavender JM. Male clinical norms and sex differences on the eating disorder inventory (EDI) and eating disorder examination questionnaire (EDE-Q) Int J Eat Disord. 2017;50(7):769–775. doi: 10.1002/eat.22716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Swami V, Barron D. Translation and validation of body image instruments: challenges, good practice guidelines, and reporting recommendations for test adaptation. Body Image. 2018;31:204–20. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Original data is available as a supplementary file in the manuscript published by Gideon et al. (2016): 10.1371/journal.pone.0152744.s004