Sir,
In the recent review of the global epidemiology of meticillin-resistant Staphylococcus aureus (MRSA) by Stefani et al. [1], they showed that MRSA remains highly prevalent in hospitals, especially in America, Asia and Malta. In contrast, the prevalence of hospital-acquired MRSA has declined in Austria, France, Ireland, the UK and Greece [1]. However, another recent study that enrolled 14 hospitals in Europe, North America and South America over a 10-year period (1998–2007) demonstrated that the incidence of nosocomial bloodstream infections (BSIs) was increasing and that the increased incidence was mainly due to antibiotic-resistant bacteria (ARB), including MRSA [2]. In that study, the MRSA incidence density (events per 100 000 patient-days) increased from 3.1 to 11.7 with an annual increase of 10% in seven ARB-endemic hospitals [2]. In Taiwan, the annual report of the Taiwan Nosocomial Infections Surveillance system by the Department of Health of Taiwan showed that S. aureus was among the top three common pathogens causing BSIs in intensive care units, and more than 77% of S. aureus isolates were MRSA in 2011. These differences in MRSA incidence density may be due to geographical variation and their findings [1], [2] might not be generalised to other places, such as Asia. We therefore retrospectively assessed the trend in incidence of nosocomial MRSA BSIs at an ARB-endemic medical centre in Taiwan.
This study was conducted at National Taiwan University Hospital (NTUH), a 2500-bed, academically affiliated medical centre providing both primary and tertiary care in northern Taiwan. The number of annual patient-days at the hospital increased from 624 675 in 2000 to 763 372 in 2010. To determine the temporal trend in nosocomial BSIs due to MRSA at NTUH, data on disk diffusion susceptibilities of S. aureus to oxacillin among isolates recovered from 2000 to 2010 were retrieved from annual summary documents. Definitions of nosocomial infections followed National Nosocomial Infections Surveillance guidelines [3]. Isolates of each species from each patient recovered within 7 days were considered as a single isolate. Susceptibility testing for S. aureus followed Clinical and Laboratory Standards Institute (CLSI) guidelines [4]. Staphylococcus aureus ATCC 25923 was used as a control strain for routine disk susceptibility testing [4]. Meticillin resistance among the S. aureus isolates was routinely screened for by measuring the growth of each isolate on a trypticase soy agar plate containing 6 mg/L oxacillin plus 2% NaCl at 35 °C in ambient air for 24 h [4]. The χ 2 test was used for dichotomous variables. The χ 2 test for trend was used to assess temporal trends in incidence densities, and Poisson regression was used to determine yearly change in incidence density as a percentage with 95% confidence intervals (CIs). Data were analysed using SPSS v.11.0 (SPSS Inc., Chicago, IL) and R v.2.15.2.
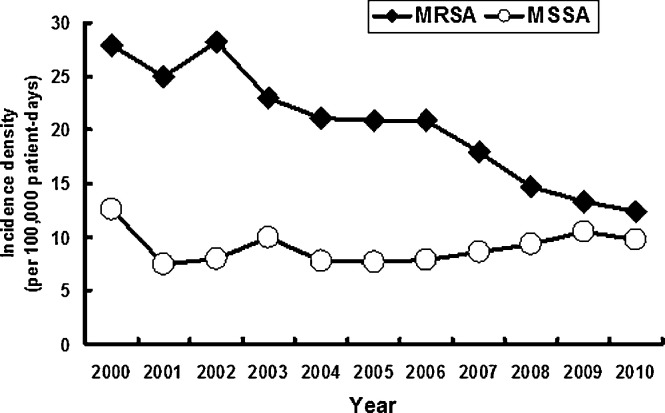
During the study period, a total of 21 233 nosocomial BSIs were identified. Of these BSIs, 2240 infections were caused by S. aureus, 69.1% of which (n = 1547) were due to MRSA. During the period 2000–2010, the incidence density of all nosocomial BSIs increased from 254.7 to 308.3 per 100 000 patient-days (P < 0.001), with an annual increase of 3.9% (95% CI 2.4–10.2%). The secular trends in incidence density of nosocomial MRSA and meticillin-susceptible S. aureus BSIs are shown in Fig. 1 . For MRSA, the incidence density significantly decreased from 27.9 to 12.3 per 100 000 patient-days, with an annual decrease of 8.5% (95% CI 7.0–10.8%) over the 10-year study period (P < 0.001). In addition, the ratio of MRSA isolates to all S. aureus isolates obtained from patients with nosocomial BSIs decreased from 68.8% in 2000 to 55.9% in 2010 (P = 0.01).
Fig. 1.
Secular trends in the incidence densities of nosocomial meticillin-resistant Staphylococcus aureus (MRSA) and meticillin-susceptible S. aureus (MSSA) bloodstream infections (P < 0.001 for MRSA and P = 0.91 for MSSA, χ2 test for trend).
In this study, we found that the incidence of nosocomial MRSA BSIs decreased even though there was an increase in the incidence of all nosocomial BSIs in Taiwan. Therefore, the total burden of nosocomial BSIs is most likely attributable to pathogens other than MRSA. This finding contrasts sharply with that reported by Ammerlann et al. [2] but is consistent with some European countries [1]. In response to the severe acute respiratory syndrome (SARS) epidemic in 2003, the infection prevention and control programme at NTUH was upgraded to include hand hygiene, antibiotic control policies, and an annual, intensive, project-based control programme. Implementation of these measures is one of the main reasons for the decrease in MRSA infections during the study period. In fact, the impact of these policies has been demonstrated to be directly associated with the decrease in rates of BSIs at NTUH [5].
In conclusion, these results show that the incidence of MRSA nosocomial BSIs decreased during the period 2000–2010 at NTUH and that the infection control measures at this hospital most likely played a major role in protecting against MRSA infections.
Funding: No funding sources.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1.Stefani S., Chung D.R., Lindsay J.A., Friedrich A.W., Kearns A.M., Westh K. Meticillin-resistant Staphylococcus aureus (MRSA): global epidemiology and harmonisation of typing methods. Int J Antimicrob Agents. 2012;39:273–282. doi: 10.1016/j.ijantimicag.2011.09.030. [DOI] [PubMed] [Google Scholar]
- 2.Ammerlaan H.S., Harbarth S., Buiting A.G., Crook D.W., Fitzpatrick F., Hanberger H. Secular trends in nosocomial bloodstream infections: antibiotic-resistant bacteria increase the total burden of infection. Clin Infect Dis. 2012;56:798–805. doi: 10.1093/cid/cis1006. [DOI] [PubMed] [Google Scholar]
- 3.Horan T.C., Andrus M., Dudeck M.A. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–332. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Clinical and Laboratory Standards Institute . CLSI; Wayne, PA: 2009. Performance standards for antimicrobial susceptibility testing; nineteenth informational supplement. Document M100-S19. [Google Scholar]
- 5.Chuang Y.C., Chen Y.C., Chang S.C., Sun C.C., Chen M.L., Hsu L.Y. Secular trends of healthcare-associated infections at a teaching hospital in Taiwan, 1981–2007. J Hosp Infect. 2010;76:143–149. doi: 10.1016/j.jhin.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]