Summary
Pandemic (H1N1) 2009 poses a serious global health threat. However, the global impact of this new pandemic remains uncertain. Past pandemics had different impacts on mortality which varied between countries. Several countries in South-east Asia have already developed their national pandemic preparedness plans. However, these plans have focused on surveillance for and response to the highly pathogenic avian influenza (H5N1), including the rapid containment of H5N1. The newly emerged pandemic (H1N1) 2009 is different from H5N1 in terms of severity and requires different approaches. There are several factors that can potentially affect the severity of pandemic (H1N1) 2009, including a population's vulnerability and response capacity. The pattern of severity appears to be changing with the spread of pandemic (H1N1) 2009, which can be conceptualized in a step-wise manner based on observation of the current situation. The overall impact of pandemic (H1N1) 2009 remains unknown and it is difficult to assess its severity. However, there is an urgent need to assess its potential severity based on the available data so that appropriate responses can be provided in order to mitigate its impact.
Keywords: Pandemic influenza, South-east Asia, Severity assessment
Background
Occasionally, a new subtype of influenza A virus emerges that can cause an influenza pandemic.1 To estimate the impact of a pandemic, lessons from past pandemics provide useful insights.2 However, the impacts of the three pandemics during the last century were varied. Spanish Flu (1918) had the most severe impact and an estimated 20–100 million people died worldwide.3, 4 Asian Flu (1957) and Hong Kong Flu (1968) had much lower impacts, although they still caused approximately 1 million deaths worldwide.5 The impact of a pandemic may differ between countries or even within a country. During the Spanish Flu pandemic, mortality was significantly higher in underdeveloped countries than in developed countries.2, 6
Currently, pandemic influenza A (H1N1) has raised global concern. As of 20 September 2009, more than 318,925 cases, including 3917 deaths, had been reported to the World Health Organization (WHO). The severity of pandemic (H1N1) 2009 remains largely unknown, due in part to the fact that the situation is still evolving, and it may increase when more vulnerable populations are affected. Conducting the severity assessment is also constrained by limited data, such as accurate estimates of case-fatality rates. WHO has issued guidelines for assessing the severity of an influenza pandemic.7 However, this is only a conceptual framework and does not provide detailed methods for the assessment. The WHO framework comprises three variables, including the virological and epidemiological characteristics of the pandemic (H1N1) 2009 virus, the vulnerability of a population and the capacity for response.
This article describes the possible severity of pandemic (H1N1) 2009 in South-east Asian countries based on the framework of the WHO guidelines. Ten member countries of the Association of South East Asian Nations (ASEAN) were included; the ASEAN region comprises approximately 560 million people and 4.5 million square kilometres. The 10 ASEAN member countries included in this study were Brunei, Cambodia, Indonesia, Lao People's Democratic Republic (PDR), Malaysia, Myanmar, the Philippines, Singapore, Thailand and Vietnam.
Capacity for response in South-east Asia
All ASEAN countries have already developed their national pandemic plans after H5N1 outbreaks began in 2003.8 It is apparent that avian influenza outbreaks were the driving force behind the development of their national pandemic plans. Massive external technical and financial support has been provided to ASEAN countries, especially those that have been severely affected by H5N1, such as Indonesia, Vietnam, Thailand, Cambodia and Lao PDR. In addition, because this region was an epicentre of recently emerging diseases, WHO developed guidelines in 2005 entitled ‘Asian Pacific Strategy on Emerging Infectious Disease’ (APSED) to strengthen the general capacity to respond to emerging diseases, including pandemic influenza. This strategic framework has helped countries in the Asian-Pacific region to strengthen their communicable disease surveillance and response capacities, including the capacity to respond to pandemic influenza. Under APSED, each country now has a better capability and capacity to respond to emerging diseases. However, in spite of all these efforts in recent years, there are certain critical gaps in the capacity to respond to a major public health threat, such as pandemic influenza. In recent years, the general response capacity at central level has improved significantly, while that at local level remains suboptimal. Other emerging disease threats, including severe acute respiratory syndrome and H5N1, have caused focal outbreaks in which some support could be provided from central level. Since pandemic influenza affects virtually all areas in each country with a minimum time lag, support from central level may not be provided during a pandemic.
One of the most important responses to mitigate the impact of pandemic (H1N1) 2009 is the surge capacity in the healthcare system. Although the majority of people infected by pandemic (H1N1) 2009 have self-limiting infections, some have developed very severe forms of illness, such as severe viral pneumonia, acute respiratory distress syndrome and multiple organ failure. Preliminary data indicated that approximately 20% of hospitalized cases required care in an intensive care unit.9 In order to prevent such severe cases, early treatment is crucial. In Mexico, it has been suggested that late treatment was associated with a higher fatality rate.10 The lack of healthcare facilities and personnel in several South-east Asian countries could be a limiting factor for early treatment. Table 1 summarizes the overall hospital bed capacity and available medical personnel in each country. Several South-east Asian countries do not have adequate surge capacity to care for a large number of patients. The lack of resources for fundamental health care is certainly problematic in terms of providing early treatment to cases. It has also been shown that there are other gaps related to providing adequate medical care; these have come to light from community surveys of health-seeking behaviours.11, 12, 13, 14 The socio-economic level and a lack of knowledge regarding severe signs of illness were associated with the health-seeking behaviours for children with pneumonia.
Table 1.
Summaryof healthcare-facility-related indicators (number per 10,000).
| Country | Year | Hospital beds per population | Density of nurses and midwives | Density of physicians |
|---|---|---|---|---|
| Brunei Darussalam | 2002 | 30 | 61.0 | 11.5 |
| Cambodia | 2000 | 1 | 8.7 | 1.6 |
| Indonesia | 2003 | - | 8.4 | 1.4 |
| Lao PDR | 2004 | 12 | 9.7 | 3.5 |
| Malaysia | 2002 | 19 | 17.9 | 7.0 |
| Myanmar | 2004 | 7 | 10.3 | 3.7 |
| Philippines | 2002 | 13 | 59.5 | 11.2 |
| Singapore | 2003 | 32 | 45.8 | 15.3 |
| Thailand | 2000 | - | 27.7 | 3.6 |
| Vietnam | 2002 | 26 | 7.6 | 5.6 |
National population was adjusted to the population of each year (United Nation Population Division).
For the early treatment of cases, stockpiles of antivirals are obviously necessary. The current stockpiled levels of antivirals are not adequate to cover a large number of patients. In some areas, the small stocks of antivirals have already been depleted during the early stage of the pandemic. Another critical element of the healthcare system's capacity to mitigate the impact of pandemic (H1N1) 2009 is its capacity to treat very severe cases. In Spain, approximately 75% of patients in intensive care units due to pandemic (H1N1) 2009 have survived.15 However, unless proper intensive care facilities with adequate equipment, such as mechanical ventilators, are provided, many of the severe cases, especially primary viral pneumonia cases, may be fatal. Several hospitals in the rural areas of South-east Asia do not have the capacity to provide intensive care, primarily due to the lack of equipment and trained medical personnel. The mortality impact can be higher in areas with limited intensive care facilities.
Vulnerable population in South-east Asia
The epidemiological and clinical descriptions of pandemic (H1N1) 2009 have revealed several factors that are associated with severe outcomes, including pre-existing medical conditions, obesity, pregnancy and children.9, 16, 17 Deaths due to seasonal influenza are mainly seen among infants or elderly people.18 During the three influenza pandemics in the last century, excess mortality was observed to be greater in the younger population,5, 19, 20 although most deaths still occurred among elderly people. This illustrated differences in age distribution between populations for seasonal influenza and pandemic influenza. For pandemic (H1N1) 2009, the mortality impact by age group is similar to the previous pandemics. As reported in some studies,21, 22 high mortality rates were observed for those aged between 40 and 59 years. The mortality impact among elderly people appears to be lower, possibly because they already have some level of antibody protection against pandemic (H1N1) 2009, which has been shown by a seroepidemiological study.23 Thus, the younger population has been experiencing a higher impact due to pandemic (H1N1) 2009.
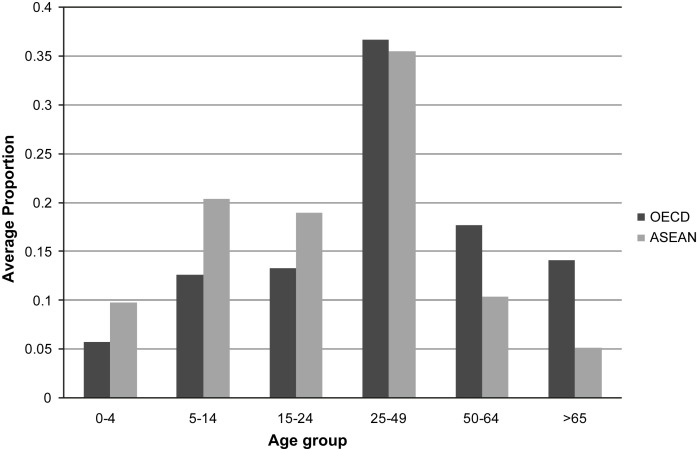
Fig. 1 shows a comparison of the population proportions by age groups between the ASEAN countries and countries in the Organization for Economic Cooperation and Development (OECD; Australia, Japan, Republic of Korea, UK and USA). ASEAN countries have significantly higher proportions of their populations in the 0–4, 5–14 and 15–24 age groups than the OECD countries (P < 0.01). These age group differences can potentially alter the differences in severity outcomes between these countries. Fertility rates in South-east Asian countries are also generally high; for instance, 3.3% fertility rates were reported in Cambodia, Lao PDR and the Philippines. In these countries, the numbers of pregnant women and young infants are high, and both groups are believed to be associated with severe infections.
Figure 1.
Comparison of age group (years) distributions between Association of South-east Asian Nations (ASEAN) and selected Organization for Economic Cooperation and Development (OECD) countries.
The estimated prevalence of chronic medical conditions is also important in order to estimate pandemic severity. These conditions include obesity, chronic respiratory conditions and diabetes mellitus, which have been reported to be risk factors for severe infection during this pandemic.17 Other communicable diseases, such as tuberculosis and human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), can also be important determinants of severity, although no data showing such associations are available to date.
Table 2 summarizes the prevalence of these pre-existing conditions in South-east Asian countries. This shows some unique patterns of prevalence. For example, there is a high prevalence of obesity in Malaysia, and the prevalences of HIV and tuberculosis are high in Cambodia. It has not been established to what extent these conditions may affect the severity of pandemic (H1N1) 2009. Each country should give priority to protecting and treating these high-risk groups in order to mitigate the overall impact. It is also essential to provide the necessary information to the population regarding pandemic (H1N1) 2009, including information about how to prevent infection, particularly among high-risk groups.
Table 2.
Disease prevalence (percentage of population) by country.
| Asthmaa | Diabetesb | Obesityc | HIV/AIDSc | Tuberculosisd | |
|---|---|---|---|---|---|
| Brunei Darussalam | 9.3 | <1 | 1.0 | ||
| Cambodia | 4.3 | 1.2 | 14.7 | 6.7 | |
| Indonesia | 1.1 | 2.0 | 2.4 | 1.1 | 2.5 |
| Lao PDR | 2.5 | 1.2 | 1.0 | 2.9 | |
| Malaysia | 4.8 | 9.9 | 14.4 | 3.9 | 1.3 |
| Myanmar | 2.8 | 9.8 | 1.7 | ||
| Philippines | 6.2 | 7.6 | <1 | 4.3 | |
| Singapore | 4.9 | 10.1 | 6.8 | 1.6 | 0.3 |
| Thailand | 6.5 | 6.9 | 11.4 | 2.0 | |
| Vietnam | 2.9 | 4.2 | 2.3 |
Prevalence of clinical asthma, 2001: Global Initiative of Asthma.
Prevalence estimates of diabetes mellitus, 2007: International Diabetes Federation.
Prevalence of adults (≥15 years), 2006: World Health Organization/World Health Organization Statistical Information System (WHO/WHOSIS).
Prevalence of tuberculosis, 2006: WHO/WHOSIS.
Recent epidemiological situation of pandemic (H1N1) 2009 in South-east Asia
According to an update by the European Centre for Disease Prevention and Control, as of 16 September 2009, the cumulative number of fatal cases in South-east Asia had reached 293. The highest number of fatal cases was reported in Thailand (n = 153), followed by Malaysia (n = 76) and the Philippines (n = 28). The number of fatal cases is still considered small in other South-east Asian countries. In fact, Thailand and Malaysia have better response capacities than countries such as Cambodia, Lao PDR and Myanmar. However, the situation in South-east Asia is still evolving and the severity pattern in each country may change over time. It has been assumed that approximately 20–30% of the total population may be ill during the first season of this pandemic. Such large outbreaks are yet to occur in most of the South-east Asian countries. Some epidemiological reports have indicated the significance of school-related outbreaks that can trigger outbreaks in the wider community.24, 25, 26 Therefore, this study attempted to conceptualize the evolving severity patterns as a step-wise spread (Table 3 ).
Table 3.
Hypothetical pandemic influenza spread and occurrence of severe cases in the community.
| Stage | Epidemiological characterization | Affected people | Morbidity | No. of severe cases |
|---|---|---|---|---|
| 1 | Imported cases from affected country | Mostly healthy adult or young | Sporadic | Limited |
| 2 | Small outbreaks related to imported cases | Mostly healthy adult or young | Sporadic | Limited |
| 3 | Some school outbreaks | School-aged children | Small | Small |
| 4 | Outbreaks spreading to community | All age groups including those with risk factors | Medium | Medium |
| 5 | Widespread community outbreak | All age groups including most vulnerable population | Large | Large |
This model explains school outbreaks as a probable trigger of community spread, followed by transmission into households and the general community. Once pandemic (H1N1) virus has spread widely in the community, those individuals with certain risk factors could be affected and the number of severe cases can be assumed to increase. When the virus reaches the most vulnerable populations, the impact of this pandemic could be much greater. Therefore, it is important to monitor the situation closely and urgently improve the preparedness and response capacities in all areas.
Conclusion
Since the spread of community transmission may occur discretely rather than simultaneously, it is necessary to make preparations and responses to this pandemic at all levels. This analysis included several indicators that may potentially lead to larger negative impacts, including the overall population structure, populations at increased risk, and hospital capacity and health professional resources. Many areas of South-east Asia have not yet experienced a widespread community transmission of pandemic (H1N1) 2009. It is important for each country in South-east Asia to develop the best strategy possible to mitigate the impact of pandemic (H1N1) 2009 in the community using the resources available. These mitigation strategies should include health educational activities for the public and improving response capacities in healthcare systems.
Acknowledgements
The work presented in this study was partly funded by the Sasagawa Peace Foundation, Japan. The authors are indebted to Akiko Hashimoto, Department of Virology, Tohoku University Graduate School of Medicine, and Miako Yofu of the Sasagawa Peace Foundation for arranging the data. This paper was developed from a lecture presented at The Lancet Conference on Influenza in the Asia Pacific, Beijing, China, 22–23 August 2009.
Ethical approval
None sought.
Funding
None declared.
Competing interests
None declared.
References
- 1.Belshe R.B. The origins of pandemic influenza – lessons from the 1918 virus. N Engl J Med. 2005;353:2209–2211. doi: 10.1056/NEJMp058281. [DOI] [PubMed] [Google Scholar]
- 2.Murray C.J., Lopez A.D., Chin B., Feehan D., Hill K.H. Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918–20 pandemic: a quantitative analysis. Lancet. 2006;368:2211–2218. doi: 10.1016/S0140-6736(06)69895-4. [DOI] [PubMed] [Google Scholar]
- 3.Patterson K.D., Pyle G.F. The geography and mortality of the 1918 influenza pandemic. Bull Hist Med. 1991;65:4–21. [PubMed] [Google Scholar]
- 4.Johnson N.P., Mueller J. Updating the accounts: global mortality of the 1918–1920 “Spanish” influenza pandemic. Bull Hist Med. 2002;76:105–115. doi: 10.1353/bhm.2002.0022. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen-Van-Tam J.S., Hampson A.W. The epidemiology and clinical impact of pandemic influenza. Vaccine. 2003;21:1762–1768. doi: 10.1016/s0264-410x(03)00069-0. [DOI] [PubMed] [Google Scholar]
- 6.Cox N.J., Subbarao K. Global epidemiology of influenza: past and present. Annu Rev Med. 2000;51:407–421. doi: 10.1146/annurev.med.51.1.407. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Considerations for assessing the severity of an influenza pandemic. Wkly Epidemiol Rec. 2009;84:197–202. [PubMed] [Google Scholar]
- 8.Coker R., Mounier-Jack S. Pandemic influenza preparedness in the Asia-Pacific region. Lancet. 2006;368:886–889. doi: 10.1016/S0140-6736(06)69209-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Hospitalized patients with novel influenza A (H1N1) virus infection – California, April–May, 2009. MMWR Morb Mortal Wkly Rep. 2009;58:536–541. [PubMed] [Google Scholar]
- 10.Perez-Padilla R., de la Rosa-Zamboni D., Ponce de Leon S., Hernandez M., Quiñones-Falconi F., Bautista E. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361:680–689. doi: 10.1056/NEJMoa0904252. [DOI] [PubMed] [Google Scholar]
- 11.Jordan H.T., Prapasiri P., Areerat P., Anand S., Clague B., Sutthirattana S. A comparison of population-based pneumonia surveillance and health-seeking behavior in two provinces in rural Thailand. Int J Infect Dis. 2009;13:355–361. doi: 10.1016/j.ijid.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 12.National Statistics Office and ORC Macro. Philippines National Demographic and Health Survey 2003. 2004.
- 13.Central Statistical Office and ORC Macro. Vietnam Demographic and Health Survey 2002. 2003.
- 14.National Institute of Public Health, National Institute of Statistics and ORC Macro. Cambodia Demographic and Health Survey 2005. 2006.
- 15.Rello J., Rodriguez A., Ibanez P., Socias L., Cebrian J., Marques A. Intensive care adult patients with severe respiratory failure caused by influenza A (H1N1)v in Spain. Crit Care. 2009;13:R148. doi: 10.1186/cc8044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Intensive-care patients with severe novel influenza A (H1N1) virus infection – Michigan, June 2009. MMWR Morb Mortal Wkly Rep. 2009;58:749–752. [PubMed] [Google Scholar]
- 17.Chowell G., Bertozzi S.M., Colchero M.A., Lopez-Garell H., Alpuche-Aranda C., Hernandez M. Severe respiratory disease concurrent with the circulation of H1N1 influenza. N Engl J Med. 2009;361:674–679. doi: 10.1056/NEJMoa0904023. [DOI] [PubMed] [Google Scholar]
- 18.Thompson W.W., Shay D.K., Weintraub E., Brammer L., Cox N., Anderson L.J. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 19.Simonsen L., Clarke M.J., Schonberger L.B., Arden N.H., Cox N.J., Fukuda K. Pandemic versus epidemic influenza mortality: a pattern of changing age distribution. J Infect Dis. 1998;178:53–60. doi: 10.1086/515616. [DOI] [PubMed] [Google Scholar]
- 20.Richard S.A., Sugaya N., Simonsen L., Miller M.A., Viboud C. A comparative study of the 1918–1920 influenza pandemic in Japan, USA and UK: mortality impact and implications for pandemic planning. Epidemiol Infect. 2009;137:1062–1072. doi: 10.1017/S0950268809002088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaillant L., La Ruche G., Tarantola A., Barboza P. Epidemiology of fatal cases associated with pandemic H1N1 influenza 2009. Euro Surveill. 2009;14 doi: 10.2807/ese.14.33.19309-en. pii=19309. [DOI] [PubMed] [Google Scholar]
- 22.de Silva U.C., Warachit J., Waicharoen S., Chittaganpitch M. A preliminary analysis of the epidemiology of influenza A(H1N1)v virus infection in Thailand from early outbreak data, June–July 2009. Euro Surveill. 2009;14 doi: 10.2807/ese.14.31.19292-en. pii=19292. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Serum cross-reactive antibody response to a novel influenza A (H1N1) virus after vaccination with seasonal influenza vaccine. MMWR Morb Mortal Wkly Rep. 2009;58:521–524. [PubMed] [Google Scholar]
- 24.Cruz-Pacheco G., Duran L., Esteva L., Minzoni A., Lopez-Cervantes M., Panayotaros P. Modelling of the influenza A(H1N1)v outbreak in Mexico City, April–May 2009, with control sanitary measures. Euro Surveill. 2009;14 pii=19254. [PubMed] [Google Scholar]
- 25.Nishiura H., Castillo-Chavez C., Safan M., Chowell G. Transmission potential of the new influenza A(H1N1) virus and its age-specificity in Japan. Euro Surveill. 2009;14 doi: 10.2807/ese.14.22.19227-en. pii=19227. [DOI] [PubMed] [Google Scholar]
- 26.Sypsa V., Hatzakis A. School closure is currently the main strategy to mitigate influenza A(H1N1)v: a modeling study. Euro Surveill. 2009;14 doi: 10.2807/ese.14.24.19240-en. pii=19240. [DOI] [PubMed] [Google Scholar]