Abstract
Background
Many US hospitals lack the capacity to house safely a surge of potentially infectious patients, increasing the risk of secondary transmission. Respiratory protection and negative-pressure rooms are needed to prevent transmission of airborne-spread diseases, but US hospitals lack available and/or properly functioning negative-pressure rooms. Creating new rooms or retrofitting existing facilities is time-consuming and expensive.
Methods
Safe methods of managing patients with airborne-spread diseases and establishing temporary negative-pressure and/or protective environments were determined by a literature review. Relevant data were analyzed and synthesized to generate a response algorithm.
Results
Ideal patient management and placement guidelines, including instructions for choosing respiratory protection and creating temporary negative-pressure or other protective environments, were delineated. Findings were summarized in a treatment algorithm.
Conclusion
The threat of bioterrorism and emerging infections increases health care's need for negative-pressure and/or protective environments. The algorithm outlines appropriate response steps to decrease transmission risk until an ideal protective environment can be utilized. Using this algorithm will prepare infection control professionals to respond more effectively during a surge of potentially infectious patients following a bioterrorism attack or emerging infectious disease outbreak.
Terrorist attacks using biologic agents pose a substantial threat to the safety, health, and security of US citizens. As the 2001 anthrax attacks illustrated, only a small amount of agent is required to have a tremendous impact in terms of morbidity, costs, and mental health effects.1 These consequences would likely have been exponentially greater if the terrorists had utilized an agent that causes a communicable disease because this could have resulted in the rapid spread of secondary infections.1 According to the Centers for Disease Control and Prevention (CDC), terrorists are likely to choose an agent that would result in the greatest terror or mass casualties.2 In this regard, infectious agents that are spread via airborne droplet nuclei, such as smallpox, have the potential for a massive public health impact.2
Any infectious disease spread by droplet nuclei, such as smallpox, Mycobacterium tuberculosis (TB), and Severe Acute Respiratory Syndrome (SARS), poses a threat to the health of other patients, staff, and visitors in the hospital setting. There is no single way to protect susceptible persons from transmission; it is recommended that a combination of methods be used.3 For hospitalized patients, airborne precautions are used to decrease health care-associated spread of airborne-spread diseases.4, 5 This category of isolation precautions consists of protective measures designed to remove as many of the droplet nuclei from the air as possible and eliminate the risk of inhalation by susceptible people.4, 5 Airborne precautions consist of engineering controls, such as the use of a negative-pressure environment, and the use of personal protective equipment in the form of respirators.5
One major challenge to airborne precautions adherence is the well-documented lack of negative-pressure rooms available in hospitals.6, 7, 8, 9 In addition, research conducted in the early 1990s indicates that many rooms designed to be negative pressure do not consistently function as required.6, 10 In a more recent (1996) study conducted in 10 St. Louis hospitals, this finding was reaffirmed: only 51% of the negative-pressure rooms tested functioned properly.11 Even the monitoring systems installed to verify continuously that negative pressure was maintained were found to be faulty. When smoke testing was conducted to verify negative-pressure functioning in rooms with a continuous monitoring system, only 50% were found to actually be negative pressure.12 Nonfunctioning negative-pressure rooms are believed to contribute to health care-associated outbreaks of TB6 and could therefore be an exposure risk for other infectious agents, such as smallpox and SARS.
Despite the lack of properly functioning negative-pressure rooms, the need for health care facility negative-pressure rooms continues to increase. This was illustrated by the recent outbreak of SARS in Toronto, Canada. As the number of SARS cases increased, the need for negative-pressure facilities increased at an almost parallel rate.13 In response, Mount Sinai Hospital in Toronto was forced to expand its number of negative-pressure beds 7-fold, and future expansions are under consideration.13 It has been estimated that Canada's 3 to 4 month outbreak of SARS cost $1.5 to $2 billion.14 US hospitals can learn from Toronto's SARS experience and examine the potential consequences of a bioterrorism attack using smallpox or an outbreak of SARS in which many additional negative-pressure rooms or protected environments may be required to help contain disease spread. This includes anticipating the growing need for additional negative-pressure rooms or alternative protective environments.
Long-term solutions include the construction of new negative-pressure rooms or units, purchasing portable isolation units that can be quickly assembled, maintaining or repairing current rooms, or retrofitting existing rooms.15, 16, 17 Unfortunately, these options are extremely costly and require extensive time and planning.15, 16 In the interim, decisions must be made concerning how and where to house safely the potentially infectious patients.
Previous publications have outlined appropriate planning and response steps for bioterrorism and emerging infections.8, 13, 15 However, these publications either assume that negative-pressure rooms are available and functioning or that patients will be transported immediately to appropriate facilities. They do not identify alternative options for responding in suboptimal situations, such as when a negative-pressure environment is not available. Although alternative arrangements for a negative-pressure environment are not completely protective, they do offer some degree of protection and help reduce disease transmission risk.16, 17 In addition, a clear algorithm is needed to outline the order of response steps that should be implemented to maximize existing protective environments until ideal isolation can be established.
Purpose statement: This article's purpose is to provide infection control professionals (ICP), health care epidemiologists, or hospital disaster planners an algorithm for patient management following a bioterrorism attack or naturally occurring infectious disease outbreak that is airborne spread, such as smallpox, SARS, and TB. This algorithm will guide users on proper patient management and placement to decrease secondary exposure risk.
It should be noted that this algorithm is designed for patient management during small airborne infectious disease outbreaks following a bioterrorism attack or emergence of a new pathogen involving a slow trickle of patients, such as the early onset of SARS in Canada.14 If a large-scale bioterrorism attack that results in hundreds or thousands of victims occurred, different response strategies would be required, such as the creation of very large negative-pressure areas or physically isolated areas for contagious patients. Examples of such systems have been delineated in the literature.18
The algorithm and guidelines in this article should be used as part of a facility's disaster planning efforts because many of the recommendations require advanced planning to implement. ICPs and hospital epidemiologists play a critical role in hospital disaster planning, but a multidisciplinary approach should be utilized. Decisions regarding placement for potentially infectious patients should be coordinated among the ICP, hospital epidemiologist, administration, facilities engineering professionals, and others.
Methods
A literature review was conducted using the following key terms in Medline, PubMed, and CINAHL databases: negative pressure, ventilation, filtration, respiratory isolation, and airborne isolation. In addition, the snowballing technique (identifying relevant references from the reference list of other publications) and expert consultation were utilized. Only English language research articles in peer-reviewed journals, national organization publications, and book chapters that discuss methods of and provide empirical evidence related to airborne isolation and/or establishing negative air pressure for rooms/areas were utilized. Editorials, articles published in nonpeer reviewed journals or those that address negative pressure unrelated to room air balance, and non-English language articles were excluded. Abstracts and titles were screened, and only those that met the aforementioned criteria were considered. From a total of 86 titles and abstracts, only 13 met the criteria. Searching the reference lists of these and consulting environmental health experts resulted in an additional 11 relevant publications, for a total of 24 articles.
Data from the 24 relevant articles were extracted; specifically, details of patients/samples, intervention, study type, study quality, and results were recorded in a spreadsheet. Studies were grouped by topic and quality of evidence, with randomized controlled trials assumed to provide the best evidence. Nonrandomized and other study designs were considered to provide less reliable evidence. Next, components were compiled into a visual step-by-step process. After the initial analysis was completed, the findings were discussed with content experts, and minor adjustments were made when applicable.
Results
Based on information identified in the literature review, a response algorithm for airborne infection isolation patient management and placement was developed (see Fig 1). This algorithm can be used by all health care facilities that need to manage safely and isolate patients with diseases or conditions that can be transmitted via airborne droplet nuclei. For entities that do not have adequate numbers of properly functioning negative-pressure rooms, this algorithm provides guidance for temporary solutions regarding room selection and creation of safer environments for staff, patients, and visitors.
Fig 1.
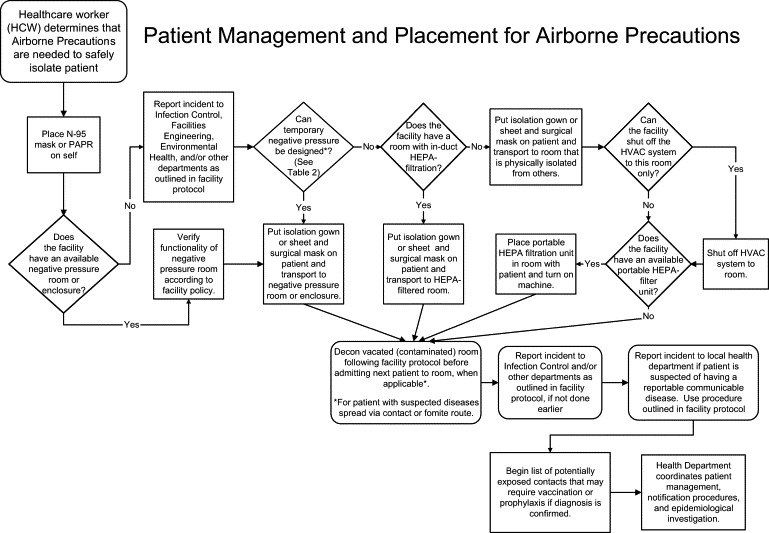
Patient management and placement for airborne precautions
Droplet nuclei are small airborne particles (≤5 μ in size) that are expelled when infected patients sneeze or cough.5, 17, 19 Eventually, these particles will settle to the ground, but they can remain suspended in the air for hours unless they are removed by ventilation or filtration.19 As long as droplet nuclei are airborne, they remain a risk to nearby susceptible people, who can inhale the particles and become infected. Airborne precautions encompass a category of measures needed to prevent the spread of organisms that can be transmitted by airborne droplet nuclei.4, 5 See Table 1 for a list of diseases and conditions that require airborne precautions and how long they are needed.
Table 1.
Disease/condition requiring airborne isolation precautions4
| Infection/condition | Duration of precautions |
|---|---|
| Chickenpox (Varicella) | Maintain precautions until all lesions are crusted. For exposed susceptible individuals, begin precautions 10 days after exposure and continue until 21 days after last exposure (up to 28 days if VZIG given). |
| Herpes Zoster (Varicella-Zoster) (Localized in immunocompromised patient or disseminated) | Maintain precautions for duration of illness. Susceptible health care workers should not enter the room if other immune caregivers are available. |
| Measles (rubeola), all presentations | Maintain precautions for duration of illness. |
| Severe Acute Respiratory Syndrome (SARS) | Maintain precautions for duration of illness. |
| Smallpox (Variola) | Maintain precautions until all lesions are crusted. Susceptible health care workers should not enter the room if other immune caregivers are available. |
| Tuberculosis (Pulmonary (confirmed or suspected) or laryngeal disease) | Discontinue precautions only after patient is on effective therapy, is clinically improving, and has 3 consecutive negative sputum smears collected on different days or TB is ruled out. |
| Viral hemorrhagic fever | Maintain precautions for duration of illness. Airborne precautions for VHFs are not reflected in HICPAC's isolation guidelines, but more recent research indicates the need to implement these precautions when feasible. In mass casualty events in which negative pressure is not available, strict adherence to isolation precautions outlined by the JAMA consensus article will help reduce the risk of transmission.33 |
The first group of infection control measures related to airborne precautions involves engineering controls to redirect, remove, or filter infectious particles from the air. This is accomplished by the use of ventilation and filtration or a combination of these measures.10, 20
The second group of airborne precautions infection control measures involves protection of susceptible persons. Precautions include wearing appropriate respiratory protection,5, 20 having immune staff care for infected patients when applicable (eg, staff immunized against the patient's disease), limiting patient transport, and restricting the number of staff going into airborne isolation rooms.4, 5 Protective measures for airborne precautions, such as appropriate respiratory protection, have been well delineated in the literature.4, 5, 18, 20
The algorithm in Fig 1 outlines response steps needed to address both groups of airborne precautions infection control measures: decreasing the bioburden of infectious particles in the air and reducing the risk to susceptible people. The results from the literature review are summarized in the order depicted on the response algorithm, starting with the most protective measures and working toward the least. The algorithm and the results section delineate the appropriate order in which the steps should be instituted to provide the best protection by reducing the risk of secondary spread.
Choosing respiratory protection
As soon as a patient is suspected of having an airborne-spread disease, protective measures must be implemented. Respiratory protection is the first protective measure. Health care workers should wear an N-95 mask or powered air purifying respirator (PAPR) when in the patient's room. A surgical mask should be placed on patients who are to be transported.5, 20
Room placement
Ideally, infected patients are placed in an airborne infectious isolation room (AIIR) that meets specific engineering controls that limit or prevent the spread of infectious particles to people outside the room.4, 5, 20, 21 AIIRs decrease the health care-associated transmission risk by redirecting contaminated air in the patient's room to the outside environment and/or filtering it before recirculation. This protects susceptible staff, patients, and visitors outside the AIIR against exposure to the infectious aerosols. However, staff and visitors who enter AIIRs must wear N-95 respirators or PAPRs to protect themselves from inhaling aerosolized infectious particles.5
Requirements for AIIRs include the following: (1) negative air pressure (in which the air flows from the adjacent corridor into the patient's isolation room), (2) a minimum of 6 to12 air changes per hour, (3) room air exhausted directly to the outside or filtered through a high-efficiency particulate air (HEPA) filter before recirculation, and (4) keeping the door to the room closed except when entering/leaving the room.4, 10, 20, 22 Whenever possible, an isolation room with an anteroom is preferable because it will further decrease the risk of droplet nuclei escaping from the infected patient's room.5, 20, 22 It does not matter whether the anteroom is positive or negative pressure in relation to the corridor, but it must be positive pressure in relation to the isolation room to be effective.20
If a negative-pressure room is available, its functioning should be verified, and the patient should be transported to the room as soon as possible.6, 12 An isolation gown or linen sheet should be placed on the patient before transfer from the room, making sure to cover as much as the patient as possible.4, 5, 23 Covering the patient before transport reduces the risk of cross contamination from the patient. In addition, a surgical mask should be placed on the patient before transport.5 If a traditional AIIR is not available, the use of a negative-pressure enclosure, such as a tent or booth, is the next best option.18, 20 Many portable tent or booth setups are commercially available, but they are cost prohibitive for many hospitals.15, 16 A less expensive alternative has been delineated in the literature but requires preplanning.18
What should be done if there are no available negative-pressure rooms or enclosures and your facility does not have prearranged plans for rapid creation of such? When feasible, the patient should be transferred to a facility with a functioning negative-pressure room as soon as possible,20, 23 but, in the interim, response steps must be implemented to protect hospital staff, patients, and visitors. If traditional negative-pressure rooms or enclosures are not available, appropriate patient placement for airborne precautions must be a multidisciplinary decision among the ICP, health care epidemiologist, facilities engineering, environmental health and safety, administration, medical staff, and others.
Temporary negative pressure
As an interim measure, temporary negative pressure can be obtained by 1 of 4 methods. Table 2 provides detailed instructions on how to achieve temporary negative pressure with interventions ordered by preference. All methods of establishing temporary negative pressure should be utilized as interim protective measures only. Patients should be transported to a room with verified negative-pressure functionality as soon as possible to provide the best protection against infection transmission.
Table 2.
Methods of establishing temporary negative pressure
| Methods to obtain temporary negative pressure (in order of preference): |
| (1) Bleed air∗ from the room through a fixed room air recirculation system |
| (2) Bleed air∗ from the room through a portable room air recirculation system |
| (3) Use a centrifugal blower to exhaust air outside from the patient's room (the unit must be set up to exhaust air out through a window†) |
| (4) Use a specifically designed air cleaner to exhaust air outside from the patient's room (the unit must be set up to exhaust air out through a window†) |
| (5) Use floor and/or window fans to exhaust air outside the patient's room‡ |
Remove appropriate amount of air volume to achieve negative pressure (to remove more air than flows into the room).
The window must be >25 feet away from air intakes, other open windows, or be more than 100 yards from another occupied building or high-risk area.
See Fig 2 for visual depiction of appropriate fan set-up.
Bleeding air from the room through fixed or portable room air recirculation systems or using a centrifugal blower to exhaust air directly to the outside from the patient's room are the best options for achieving temporary negative pressure (See Table 2 for more information).20 Room air recirculation units are more effective than exhausting air outside using a centrifugal blower and are, therefore, preferable.20 If room air recirculation units are not available and a centrifugal blower will be used to create negative pressure, the unit must be set up to exhaust air out through a window.19, 20 As with standard negative-pressure rooms, the door to the room must be kept closed.17 As an alternative to a centrifugal blower, some air cleaners can also be utilized, but they must be designed specifically for this purpose.20
Traditional floor or window fans can also be used to create temporary negative pressure, although this should only be done as a last resort because it is the least effective option and can actually contribute to transmission if set up incorrectly (See Table 2 and Fig 2 for more information).3 Used alone to create wind in a room, fans only serve to recirculate airborne infectious particles; this could actually increase rather than decrease the risk of transmission.3 However, fans are effective at redirecting infectious particles and thus decreasing the room's bioburden if they are positioned correctly.3 Figure 2 provides a visual depiction of appropriate fan setup and some necessary instructions. Because fresh air generally comes from outdoors and is directed in through open windows or doors (something that is not feasible in most hospitals), the use of a floor or window fan to help increase circulation or redirect infectious particles from the contaminated room may not be a viable option.
Fig 2.
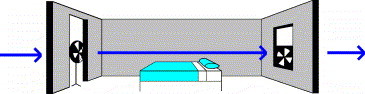
Appropriate placement of floor and/or window fans to facilitate removal of contaminated air. For visual clarity, the door appears open in the picture but should always remain closed, except when staff need to enter or exit the room. A floor or table fan should be placed near the doorway pointing toward the window fan. Never point a fan toward the patient's door because this can facilitate the spread of infectious particles into the corridor.3 A second fan must be utilized to help draw contaminated air from the room at the same rate at which the fan at the door is drawing air into the room.17 The fan in the window must be facing the outside of the building to direct air outward, and the window must be open. If the room's windows do not open, this fan system must not be utilized; the wind created by such a set-up may actually lead to an increased risk of transmission.3
Consult facilities engineering and/or environmental health and safety when considering establishing temporary negative pressure through any method of exhausting room air. Although this is an easy task to accomplish, the remainder of the facility can suffer from an air pressure imbalance if steps are not taken to replace the loss of air in the room.17 In addition, the room from which to exhaust contaminated air should be chosen carefully; if contaminated air is exhausted near intake vents, open windows, or nearby susceptible people, infection transmission can occur.10 The room chosen should meet the following criteria: (1) have a window that is ≥25 feet away from air intakes or other open windows and (2) be more than 100 yards from another occupied building or high-risk area.23
If any temporary method of obtaining negative pressure is utilized, it must be discontinued as soon as possible because it does not provide the correct mix of fresh air for comfort and poses a risk to those near the exhaust site.20 Various organizations and regulatory agencies, including the American Institute of Architects and the American Society of Heating, Refrigerating, and Air-Conditioning Engineers, provide guidelines and recommendations regarding safe exhaust of potentially contaminated air.20, 24, 25 These guidelines should be consulted prior to instituting temporary negative-pressure systems. Setting up temporary negative-pressure rooms/areas requires preplanning and a multidisciplinary approach. This must be included in hospital disaster planning efforts.
If negative pressure is not available and cannot be temporarily achieved, other interim measures need to be implemented to prevent the transmission of airborne-spread diseases. The heating, ventilation, and air conditioning (HVAC) systems of the patient's room and facility need to be evaluated to determine proper patient placement and filtration intervention needs. Ventilation systems that recirculate air pose a hazard if contaminated air exhausted from the room of infected patients is not filtered prior to discharging it into the general ventilation system and recirculating it to clean areas.3, 20 Contaminated air must either be discharged to the outside away from air intakes or filtered prior to recirculation.16, 19, 20 Filtration options consist of in-duct or portable filtration systems/units.16, 19
In-duct HEPA filter systems are more effective at removing infectious particles than portable filtration units and are, therefore, the preferred method of recirculating contaminated air.19, 20, 26 Although the efficacy of HEPA-filtration removal of some organisms believed to be spread by droplet nuclei, such as smallpox and SARS, has never been evaluated, research indicates that HEPA filters effectively remove other particles that are the same size as droplet nuclei, such as Aspergillus spores.20 Therefore, HEPA filters would most likely be effective at removing droplet nuclei and other particles in the 1 to 5 μ size range.
In the absence of negative-pressure rooms or in-duct HEPA filters, 2 interventions will help decrease the transmission risk of infections spread via droplet nuclei: (1) physical isolation of the patient and (2) use of portable HEPA-filtration units.9, 16, 20, 25 The first intervention, physical isolation, should be implemented regardless of whether portable filtration units are available. Physical isolation consists of placing potentially infectious individuals in a room as far away from others as possible and keeping the door to the room closed as much as possible.17 For patients with smallpox, physical isolation was historically accomplished through home isolation or the creation of smallpox wards or facilities.27 More recently, home quarantine (for contacts of SARS) and development of physically isolated wards (for patients with SARS) were again utilized to help prevent the spread of disease.14
In addition to physical isolation, engineering controls will decrease the air's bioburden that will in turn help prevent transmission.25, 26 The first engineering control is to shut down the HVAC system in the patient's room when possible. However, this should only be done if it will not affect the HVAC system to the rest of the hospital.21, 22
The final engineering control involves the use of portable HEPA-filtration units. Portable HEPA units work in 2 ways: (1) they filter airborne contaminants from room air, and (2) they help increase the number of air changes per hour, which further improves the number of airborne contaminants removed from the room.17 Although they are not 100% effective at removing infectious particles from the air, portable HEPA-filtration units provide more protection than the regular HVAC system alone, which only reduces particle concentrations by 34%.28 HEPA filtration units remove ≥99.97% of 0.3 μ size and 100% of larger size particles (such as droplet nuclei) from the air but require time to filter an entire room's air volume.19, 26, 29 A HEPA-filtration unit can clear 90% of particles in a 760 cubic foot room within 5 minutes compared with ≥120 minutes needed in a room without a HEPA-filtration unit, but clearance times also depend on the room's airflow rate.16 Portable filtration units do not eliminate secondary transmission risk to staff, visitors, or other patients either in or outside the room. However, portable HEPA units do decrease the droplet nuclei bioburden in the air, which reduces the risk of secondary transmission.26 Although not completely protective, this is far superior to using only the facility's standard HVAC system.17, 26
Many manufacturers recommend that portable HEPA-filtration units be placed in the center of the room, but this is not feasible in hospital settings. In addition, a 1995 study by Rutala et al illustrated that this is also not necessary.16 Rutala et al found that the filtration units were effective regardless of placement in the room.16 The overall portable filtration unit effectiveness depended on the air's bioburden of infectious particles, the facility's HVAC system, and the individual room's airflow rate and size.16 Therefore, portable filtration units should be placed as close to the patient as possible, without interfering with staff work flow or medical equipment in the room.29 In addition, health care providers should not stand between the patient and the portable HEPA unit's air intake because this can increase their exposure risk.16, 29
Disadvantages to the use of portable filtration units include physical obstruction, air drafts, and noise.16 In addition, the associated costs of purchasing and running one or more of these units may make them cost prohibitive for many hospitals. Prices range from $1000 to $2200 per unit and another $100 per year for filter replacements, and there is an uncalculated associated cost for electricity to power the machine(s).29, 30, 31 Although $1000 per machine is a relatively inexpensive investment for disaster preparedness, the actual cost to a hospital would be exponentially higher in a mass casualty incident, such as a large smallpox or SARS outbreak, when hundreds of such machines might be needed.
Other patient management issues
After the patient has been transported to another room, whether internally or externally, the room in which the patient was originally housed may require decontamination before the next patient can be safely admitted. Some diseases, such as SARS and smallpox, can be spread by hand-to-mouth transfer of infectious particles because of direct contact with patient secretions or contaminated materials (ie., contact) and airborne droplet nuclei; these patients require both airborne and contact precautions. One component of contact precautions is thorough environmental decontamination to prevent transmission.4, 5, 23 Therefore, all horizontal surfaces and inanimate objects in the contaminated vacated room must be decontaminated before the next patient is admitted.4 Hospital decontamination protocols should be followed. This will not apply to all patients. Decontamination is only needed for the rooms of patients on contact precautions in addition to airborne precautions.4, 5
Once the patient is housed in the safest environment possible, the ICP or hospital epidemiologist must be notified (unless they had been consulted during patient placement). In addition, other groups or departments identified by hospital infection control policies should also be notified at this time. Hospital reporting and notification policies and procedures should always be followed.
If the patient is suspected of having a reportable, communicable disease as defined by the facility's state department of health, this incident should be reported to the local health department.32 Hospital policy and state health department reporting regulations should always be followed.32 It is imperative that early, accurate, and complete reporting be made to the local health department. Efforts to include this critical aspect of public health must begin with early collaboration.
While awaiting diagnosis confirmation, it is prudent to begin a list of potentially exposed individuals. This will aid in the health department's epidemiologic investigation if a communicable disease, such as TB, SARS, or smallpox, is confirmed. Utilize CDC definitions of a “contact” to determine the list of potentially exposed individuals.32 The definition of a “contact” should be based on the specific suspected diagnosis because the definition can differ between infectious diseases.32
Discussion
Preventing the transmission of airborne-spread diseases remains a challenge for hospitals. A combination of protective measures aimed at decreasing the air's bioburden of infectious particles and reducing the risk to susceptible people must be employed. Engineering controls, such as the use of properly functioning negative-pressure rooms or enclosures, and infection control measures, such as respirator use, play a significant role in decreasing the spread of airborne-spread diseases. Unfortunately, many hospitals do not have adequate negative-pressure rooms available, and some of these rooms' airflow systems do not function properly. As the need for airborne precautions increases because of the risks of SARS, smallpox, and other bioterrorist or emerging infectious conditions, hospitals must develop plans to accommodate safely the potential surges of these patients.
Adequate numbers of properly functioning negative-pressure rooms or areas are the ideal to which all health care facilities must aspire. Hospital disaster planners must address ways to accommodate not only surge capacity for mass casualties but also, and more specifically, a surge of potentially airborne infectious patients. This includes development of a plan to mobilize negative-pressure beds or areas rapidly should such a need arise. This must be a priority for US hospitals. However, accommodations for new negative-pressure rooms or enclosures are costly; sources for such endeavors are outside this article's scope but must be addressed.
In the interim, alternative options are needed until new negative-pressure facilities can be created, repaired, or retrofitted or until a potentially infectious patient can be transferred to a facility with properly functioning negative pressure. The algorithm depicted in Fig 1 provides such guidance. Use of this algorithm should help prepare ICPs and hospital epidemiologists to respond better to a bioterrorism attack or airborne-spread infectious disease outbreak by providing guidelines for proper patient management and placement.
This article's algorithm is designed for patient management during the early onset of a bioterrorism attack or emerging infectious disease outbreak. It will be most helpful as a planning tool for ICPs and hospitals and as a response algorithm during a slow surge of potentially infectious patients. Under other scenarios, such as a large-scale bioterrorism attack that results in hundreds or thousands of victims, the usefulness of these recommendations may be limited. Hospitals must plan for both small and large infectious disease outbreak scenarios. This algorithm is one option for addressing these needs but is not the solution for all US hospital negative-pressure surge capacity issues.
Future initiatives need to evaluate the current numbers of negative-pressure rooms available in US hospitals, the total available occupancy, and the percentage of those that meet the functional standard. In addition, cost-effective approaches to development of large negative-pressure areas that can be mobilized rapidly after a bioterrorism attack or infectious disease outbreak must be identified. Furthermore, the best locations within or around the facility for the placement of isolation rooms/areas need to be determined. Hospital disaster plans must address these issues.
Saint Louis, Missouri
References
- 1.Mondy C., Cardenas D., Avila M. The role of an advanced practice public health nurse in bioterrorism preparedness. Public Health Nurs. 2003;20:422–431. doi: 10.1046/j.1525-1446.2003.20602.x. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Bioterrorism agents/diseases. 2004. Available from: http://www.bt.cdc.gov/agent/agentlist-category.asp. Accessed January 30, 2004.
- 3.Hodge D., Kass D. Reducing the spread of tuberculosis in your workplace. In: Charney W., editor. Vol 3. CRC Press; Boca Raton, FL: 1994. pp. 166–222. (Essentials of modern hospital safety). [Google Scholar]
- 4.Hospital Infection Control Practices Advisory Committee . Recommendations for isolation precautions in hospitals. In: Pfeiffer J.A., editor. APIC text of infection control and epidemiology. Association for Professionals in Infection Control and Epidemiology; Washington, DC: 2000. pp. 29A1–29A26. [Google Scholar]
- 5.Garner J.S. Guidelines for isolation precautions in hospitals. Am J Infect Control. 1996;24:24–31. doi: 10.1016/s0196-6553(96)90050-4. [DOI] [PubMed] [Google Scholar]
- 6.Fraser V.J., Johnson K., Primack J., Jones M., Medoff G., Dunagan W.C. Evaluation of rooms with negative-pressure ventilation used for respiratory isolation in seven Midwestern hospitals. Infect Control Hosp Epidemiol. 1993;14:623–628. doi: 10.1086/646654. [DOI] [PubMed] [Google Scholar]
- 7.Fuss E., Israel E., Baruch N., Roghmann M. Improved tuberculosis infection control practices in Maryland acute care hospitals. Am J Infect Control. 2000;28:133–137. [PubMed] [Google Scholar]
- 8.Grow R.W., Rubinson L. The challenge of hospital infection control during a response to bioterrorist attacks. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2003;1:215–220. doi: 10.1089/153871303769201860. [DOI] [PubMed] [Google Scholar]
- 9.Kellerman S.E., Simonds D., Banerjee S., Towsley J., Stover B., Jarvis W. APIC and CDC survey of Mycobacterium tuberculosis isolation and control practices in hospitals caring for children. Part II: patient and family isolation policies and procedures. Am J Infect Control. 1998;26:478–482. doi: 10.1016/s0196-6553(98)70019-7. [DOI] [PubMed] [Google Scholar]
- 10.Marier R.L., Nelson T. A ventilation-filtration unit for respiratory isolation. Infect Control Hosp Epidemiol. 1993;14:700–705. doi: 10.1086/646672. [DOI] [PubMed] [Google Scholar]
- 11.Dahl K.M., L'Ecuyer P.B., Jones M., Fraser V.J. Follow-up evaluation of respiratory isolation rooms in 10 Midwestern hospitals. Infect Control Hosp Epidemiol. 1996;17:816–818. doi: 10.1086/647244. [DOI] [PubMed] [Google Scholar]
- 12.Pavelchak N., Cummings K., Stricof R., Marshall E., Oxtoby M., London M. Negative-pressure monitoring of tuberculosis isolation rooms within New York State hospitals. Infect Control Hosp Epidemiol. 2001;22:518–519. doi: 10.1086/501943. [DOI] [PubMed] [Google Scholar]
- 13.Farquharson C., Baguley K. Responding to the severe acute respiratory syndrome (SARS) outbreak: lessons learned in a Toronto emergency department. J Emerg Nurs. 2003;29:222–228. doi: 10.1067/men.2003.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Health Canada. Chapter 5: Building capacity and coordination: National infectious disease surveillance, outbreak management, and emergency response. In: SARS in Canada. 2003:1-29. Available from: http://www.hc-sc.gc.ca/english/protection/warnings/sars/learning/EngSe30_ch5.htm. Accessed March 7, 2004.
- 15.Clayton A.J., Best H.R. Controlling the exotic diseases: 1. Isolation facilities. Can Med Assoc J. 1980;123:863–867. [PMC free article] [PubMed] [Google Scholar]
- 16.Rutala W.A., Jones S.M., Worthington J.M., Reist P.C., Weber D.J. Efficacy of portable filtration units in reducing aerosolized particles in the size range of Mycobacterium tuberculosis. Infect Control Hosp Epidemiol. 1995;16:391–398. doi: 10.1086/647136. [DOI] [PubMed] [Google Scholar]
- 17.Tepper B.S. Portable HEPA filtration for TB isolation in hospitals and clinics. In: Charney W., editor. Vol. 3. CRC Press; Boca Raton, FL: 1994. pp. 143–156. (Essentials of modern hospital safety). [Google Scholar]
- 18.Rosenbaum R.A., Benyo J.S., O'Connor R.E., Passarello B.A., Williams D.R., Humphrey B.D. Use of a portable forced air system to convert existing hospital space into a mass casualty isolation area. Ann Emerg Med. 2004;44:628–634. doi: 10.1016/j.annemergmed.2004.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller-Leiden S., Lobascio C., Nazaroff W.W., Macher J.M. Effectiveness of in-room air filtration and dilution ventilation for tuberculosis infection control. J Air Waste Manag Assoc. 1996;46:869–882. doi: 10.1080/10473289.1996.10467523. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention Guidelines for preventing the transmission of Mycobacterium tuberculosis in healthcare facilities, 1994. MMWR. 1994;43:1–132. [PubMed] [Google Scholar]
- 21.The American Institute of Architects and The Facilities Guidelines Institute . American Institute of Architects Press; Washington, DC: 2001. Guidelines for the design and construction of hospital and healthcare facilities, 2001. [Google Scholar]
- 22.Centers for Disease Control and Prevention Guidelines for environmental infection control in health-care facilities. MMWR. 2003;52:1–44. [Google Scholar]
- 23.Centers for Disease Control. Smallpox response plan and guidelines version 3.0. 2003. Available from: http://www.bt.cdc.gov/agent/smallpox/response-plan/index.asp-guidea. Accessed January 30, 2004.
- 24.American Society of Heating, Refrigerating, and Air-Conditioning Engineers, Inc. (ASHRAE). Ventilation for Acceptable Indoor Air Quality (ANSI Approved). (ASHRAE Standard No. 62-2004). Atlanta, GA: ASHRAE.
- 25.Seitz T.A., Decker J., Jensen P. National Institute for Occupational Safety and Health; Newark, NJ: 1996. Health hazard evaluation report 95-0031-2601. p. 1-8. [Google Scholar]
- 26.Conroy L.M., Franke J.E. An industrial hygiene approach to tuberculosis control. In: Charney W., editor. Vol. 3. CRC Press; Boca Raton, FL: 1994. pp. 105–222. (Essentials of modern hospital safety). [Google Scholar]
- 27.Henderson D.A., Inglesby T.V., Bartlett J.G., Ascher M.S., Eitzen E., Jahrling P.B. Smallpox as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. JAMA. 1999;281:2127–2137. doi: 10.1001/jama.281.22.2127. [DOI] [PubMed] [Google Scholar]
- 28.Jamriska M., Morawska L., Clark B.A. Effect of ventilation and filtration on submicrometer particles in an indoor environment. Indoor Air. 2000;10:19–26. doi: 10.1034/j.1600-0668.2000.010001019.x. [DOI] [PubMed] [Google Scholar]
- 29.Mead K., Johnson D.L. An evaluation of portable high-efficiency particulate air filtration for expedient patient isolation in epidemic and emergency response. Ann Emerg Med. 2004;44:635–645. doi: 10.1016/j.annemergmed.2004.07.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fisk W.J., Faulkner D., Palonen J., Seppanen O. Performance and costs of particle air filtration technologies. Indoor Air. 2002;12:223–234. doi: 10.1034/j.1600-0668.2002.01136.x. [DOI] [PubMed] [Google Scholar]
- 31.Kellerman S., Saiman L., Soto-Irizarry M., San Gabriel P., Larsen C., Besser A. Costs associated with tuberculosis control programs at hospitals caring for children. Pediatr Infect Dis J. 1999;18:604–608. doi: 10.1097/00006454-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Wharton M., Chorba T.L., Vogt R.L., Morse D.L., Buehler J.W. Case definitions for public health surveillance. MMWR. 1990;39:1–43. [PubMed] [Google Scholar]
- 33.Borio L., Inglesby T., Peters C.J., Schmaljohn A.L., Hughes J.M., Jahrling P.B. Hemorrhagic fever viruses as biological weapons: medical and public health management. JAMA. 2002;287:2391–2405. doi: 10.1001/jama.287.18.2391. [DOI] [PubMed] [Google Scholar]


