Abstract
Adult-onset Still’s disease is a rare inflammatory disorder characterised by fever, arthritis and rash. It can present in a number of ways and is associated in 5% of cases with parenchymal lung involvement. We present the case of a 37-year-old man who initially presented with fever, weight loss and pancytopaenia. He gradually deteriorated requiring non-invasive ventilation with a Computerised tomography of his chest showing bilateral nodular infiltrates. An open lung biopsy showed acute fibrinous organising pneumonia, which responded well to corticosteroid treatment. He then re-presented over three years later with a similar systemic illness although with less severe lung involvement. Following extensive further investigations, he was diagnosed with Adult-onset Still’s disease fulfilling the Yamaguchi criteria. We feel this case is important due to the rare association of Adult-onset Still’s disease and interstitial lung disease. More specifically, we are not aware of any published cases of Adult-onset Still’s disease with acute fibrinous organising pneumonia.
Keywords: clinical, interstitial lung disease, other rheumatology, respiratory medicine, rheumatology
Case presentation
Our patient was a Caucasian man who initially presented aged 33 with a seven-week history of gradually worsening fevers, night sweats, lethargy and 6 kg weight loss. He had no significant medical history, was on no regular medications and worked in Information Technology. Admission blood tests showed a total white cell count (WCC) of 2.38 (109/L), neutrophils of 1.5 (109/L), lymphocytes of 0.6 (109/L), haemoglobin of 10.4 (g/dl) and platelets of 209 (109/L) (which subsequently dropped to 135). Liver enzymes showed an alanine aminotransferase (ALT) of 59 (IU/L), bilirubin of 32 (µmol/L) and alkaline phosphatase (ALP) of 57 (IU/L). His c-reactive protein (CRP) was 44 (mg/L) and ferritin elevated at 728 (µg/L). Computerised tomography (CT) of the chest showed multiple bilateral lung nodules and splenomegaly. Due to his fever and imaging appearances (Figure 1), he was treated with broad-spectrum antibiotics for possible atypical pneumonia. Multiple investigations including several blood cultures were performed to look for an infective cause of the fever all of which were negative. Autoimmune screen was unremarkable. He continued to deteriorate despite antibiotics developing type-1 respiratory failure requiring non-invasive ventilation. His blood tests also worsened becoming pancytopaenic with worsening liver enzymes (ALT increased to 262 IU/L) and CRP increasing to 205 (mg/L). Bronchoscopy with transbronchial biopsies and washings were non-diagnostic. Due to a lack of a clear diagnosis, he was intubated and transferred to a tertiary care centre for a surgical lung biopsy which showed acute fibrinous and organising pneumonia, noting a prominent reactive interstitial lymphoid infiltrate (Figure 2). Following this, he was given intravenous methylprednisolone for five days and started to improve clinically. This was followed by a reducing course of prednisolone starting at 30 mg once a day. He remained asymptomatic for over two years with approximately 18 months off corticosteroids.
Figure 1.
CT chest appearances on initial presentation showing multiple soft tissue nodules.
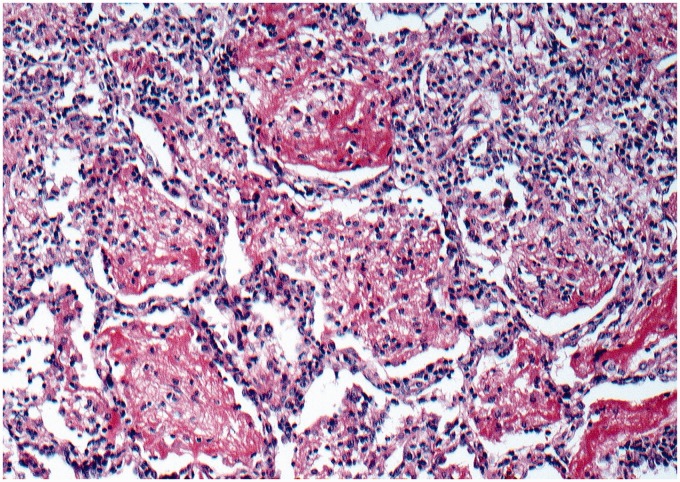
Figure 2.
Histology showing buds of granulation tissue filling alveolar spaces as well as variable amounts of fibrin and organisation. There is an associated moderately intense reactive interstitial lymphoid infiltrate (H&E ×100).
He then re-presented aged 37 approximately 4 years after his initial presentation. On this occasion, he gave a one-week history of night sweats, fevers, fatigue and arthralgia. From the patient’s point of view, he felt this was likely a recurrence of his initial illness. Initial blood tests showed pancytopaenia with a haemoglobin of 10.8 (g/dl), WCC of 2 (109/L) and platelets of 119 (109/L). His ALT was 106 (IU/L), ALP 199 (IU/L), bilirubin 154 (µmol/L) and CRP 150 (mg/L). He then developed rapidly worsening liver function tests and jaundice. A CT abdomen and pelvis showed hepatosplenomegaly and he had a marked hyperferritinaemia (>6000). Bilateral lung nodules were again noted on the CT but improved compared with his previous admission. A bone marrow biopsy showed no evidence of macrophage activation or T-cell lymphoma. A liver biopsy showed intrahepatic cholestasis and atypical lymphocytes in the liver sinusoids. He was treated with broad-spectrum antibiotics to cover for underlying infection and 40 mg prednisolone was restarted empirically as it was felt he was again deteriorating. Following the restart of steroids, he improved relatively quickly, as he had previously, and was discharged from hospital.
Outcome and follow-up
Repeat bone marrow biopsy when off steroid therapy showed a degree of macrophage activation but no overt haemophagocytosis or evidence of lymphoma. When attempting to wean the steroids again, he developed some non-specific symptoms of joint aches and pains and was restarted on steroids with a long-term plan to introduce methotrexate as a steroid sparing agent. The diagnosis of Adult-onset Still’s disease was made following the involvement of multiple medical specialities and he meets the Yamaguchi criteria. A next generation auto-inflammatory disorders gene panel was negative further supporting the diagnosis.
Discussion
Adult-onset Still’s disease is a multisystem auto-inflammatory syndrome often seen in young adults. It is classically characterised by the presence of fevers, arthritis and an evanescent pink rash.1,2 It is a rare disease with an estimated incidence of 0.16 per 100,000.3 The diagnosis is made clinically using the Yamaguchi criteria once infectious, neoplastic and autoimmune disorders have been excluded.2
The diagnosis of Adult-onset Still’s disease is often challenging due to its varied clinical presentations. A study of 57 patients by Gerfaud-Valentin et al. in 2014 suggested a mean time to diagnosis of four months.4 A case published in 2017 by Stella Pak and Cindy Pham shows similarities to our case where a 31-year-old man was diagnosed with Adult-onset Still’s disease three years after his initial presentation.5 This highlights the importance of considering the diagnosis in any patient with a suspected inflammatory condition of unknown aetiology.
Lung parenchymal involvement has been described as a rare feature of Adult-onset Still’s disease in around 5% of cases.6 Our case further highlights this rare association. A case series published in 2016 by Gerfaud-Valentin et al. discussed 30 cases of Adult-onset Still’s disease with parenchymal lung involvement. Of these patients 12 had acute respiratory distress syndrome, 5 had an organising pneumonia, 3 had an interstitial lung disease (ILD) that was thought likely to be an NSIP (non-specific interstitial pneumonia), 7 had an unclassified ILD, 2 had bronchiolitis and 1 had diffuse alveolar haemorrhage.6
Our patient was diagnosed with acute fibrinous and organising pneumonia which is a rare pattern of interstitial pneumonia characterised by the presence of organising pneumonia with intra-alveolar fibrin.7 It most likely reflects a more acute presentation of organising pneumonia and is therefore a pattern of interstitial pneumonia recognised by pathologists but not a specific idiopathic clinical entity.8 Indeed, most cases are secondary, with associations similar to those in typical cases of organising pneumonia, though with a poorer prognosis.9 We are unaware of any published reports of acute fibrinous and organising pneumonia being seen in Adult-onset Still’s disease but as its diagnosis requires a lung biopsy it may be that it is under reported. It is also of interest that in our case this association was only confirmed 4 years after presentation, a feature seen in non-specific interstitial pneumonia but not well described in acute fibrinous and organising pneumonia.10
In conclusion, this case highlights the importance of considering Adult-onset Still’s disease in patients with a presumed inflammatory disorder of unknown aetiology. We also highlight the rare association between Adult-onset Still’s disease and acute fibrinous and organising pneumonia, and the fact that an associated collagen vascular disease can manifest years after the pulmonary presentation of disease. We are unaware of any other published reports of this association.
Acknowledgements
None.
Declarations
Competing interests
None declared.
Funding
None declared.
Ethics approval
Consent form completed by patient.
Guarantor
Kuldeep Cheent.
Contributorship
RP, KC, LS and DC were involved in the clinical care of the patient. The manuscript was written by RP and KC. AGN provided the histology and accompanying description. All authors read and made amendments to the manuscript.
Provenance
Not commissioned. Externally peer reviewed.
ORCID iD
Robert Perry https://orcid.org/0000-0003-0149-6530
References
- 1.Bywaters EG. Stills disease in the adult. Ann Rheumat Dis 1971; 30: 121–133–121–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gerfaud Valentin M, Jamilloux Y, Iwaz J, Seve P. Adult-onset Still’s Disease. Autoimmun Rev 2014; 13: 708–722–708–722. [DOI] [PubMed] [Google Scholar]
- 3.Magadur-Joly G, Billaud E, Barrier JH, Pennec YL, Masson C, Renou P, et al. Epidemiology of adult Still’s disease: estimate of the incidence by a retrospective study in West France. Ann Rheumat Dis 1995; 7: 587–590–587–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gerfaud-Valentin M, Maucort-Boulch D, Hot A, Iwaz J, Ninet J, Durieu I, et al. Adult-onset Still’s disease: manifestations, treatment, outcome, and prognostic factors in 57 patients. Medicine 2014; 93: 91–99–91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pak S, Pham C. Delay in the diagnosis of Adult-onset Still’s Disease. Cureus 2017; 9: e1321–e1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gerfaud-Valentin M, Cottin V, Jamilloux Y, Hot A, Gaillard-Coadon A, Durieu I, et al. Parenchymal lung involvement in Adult-onset Still’s disease. Medicine 2016; 95: e4258–e4258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beasley MB, Franks TJ, Galvin JR, Gochuico B, Travis WD. Acute fibrinous and organizing pneumonia: a histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch Pathol Lab Med 2002; 126: 1064–1070–1064–1070. [DOI] [PubMed] [Google Scholar]
- 8.Travis WD, Costabel U, Hansell DM, King TEJr, Lynch DA, Nicholson AG, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Resp Crit Care Med 2013; 188: 733–748–733–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arnaud D, Surani Z, Vakil A, Varon J, Surani S. Acute fibrinous and organizing pneumonia: a case report and review of the literature. Am J Case Rep 2017; 18: 1242–1246–1242–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kono M, Nakamura Y, Yoshimura K, Enomoto Y, Oyama Y, Hozumi H, et al. Nonspecific interstitial pneumonia preceding diagnosis of collagen vascular disease. Resp Med 2016; 117: 40–47–40–47. [DOI] [PubMed] [Google Scholar]